Contrast enhanced ultrasonography (CEUS) to detect abdominal microcirculatory disorders in severe cases of COVID-19 infection: First experience
Abstract
In the hands of experienced examiners, the contrast enhanced sonography (CEUS) offers the possibility to analyze dynamic microcirculatory disturbances in real time dynamically without any risk for kidneys and thyroid gland even in severe progressing disease bedside. Based on severe COVID-19 infections, first experiences with abdominal CEUS examinations are presented. In the stage of an imminent organ failure with significantly reduced kidney and liver function, CEUS can be used to show a narrowing of the organ-supplying arteries, as well as a delayed capillary filling of vessels near the capsule, a regional reduced parenchymal perfusion or an inflammatory hyperemia with capillary hypercirculation. It is possible to quickly rule out organ infarction and to dynamically record the mesenteric arterial and venous blood flow.
1Introduction
First publications showed that COVID-19 patients often suffer from pneumonia [1–3] and pulmonary changes monitored by ultrasound [4, 5]. Older age, showing signs of sepsis on admission, underlying diseases like high blood pressure and diabetes and the prolonged use of noninvasive ventilation were important factors on the deaths of these patients [2]. Though sepsis is a disease with severe microcirculatory disorders [6, 7], up to now, there are no investigations of the abdominal microvasculature in COVID-19 patients.
Contrast enhanced ultrasound (CEUS) is increasingly used worldwide not only for the detection and characterization of parenchymal liver changes or the detection of liver tumors, but according to the current EFSUMB guidelines also in non-hepatic related diagnostic fields [8]. CEUS is also used to detect dynamic microcirculatory changes in pediatrics [9]. Using Sulphur-Hexafluoride Microbubbles as ultrasound contrast medium, there is no risk for severe side effects for the thyroid and kidneys and only a low allergic risk, which is in the range of other contrast media. However, special ultrasound equipment, the possibility of Contrast Harmonic Imaging (CHI) at low mechanical index (MI < 0.2) and experienced examiners are required [10]. Then, the diagnostic accuracy is in the range of contrast-enhanced computed tomography (ceCT) or contrast-agent-enhanced magnetic resonance imaging (MRI) with correspondingly good sound conditions [8, 11]. The demands on technology and examiners are even greater if CEUS is performed directly bedside on intensive care units during severe disease progression. This requires a considerable logistical effort in case of severe COVID-19 infections and examinations under special protective measures. CEUS is then used in the abdominal area for rapid dynamic assessment of the perfusion of abdominal organs down to the microcirculation pathway, the detection of inflammatory hyperemia or organ circulation disorders in case of impending organ failure, as well as the exclusion of infarcts or organ necrosis and the dynamic detection of mesenteric perfusion.
In the following clinical evaluation, first experiences using CEUS in patients with severe COVID-19 infections, during dynamic examination of abdominal organs bedside in intensive care units are presented.
2Material and methods
The indications for the ultrasound examinations including contrast agent sonography (CEUS) were based on decisions of the interdisciplinary board. In accordance with earlier intensive care unit examinations and the experience with intraoperative CEUS, such examinations are supported by the new EFSUMB Guidelines and many clinical trials [8, 12, 13].
In the case of COVID-19 infections, the requirements for examiners and ultrasound examinations can only be met to the highest standards of hygiene and only with high-performance ultrasound equipment with maximum mobility. In the present case, all examinations were performed by an experienced examiner (more than 20 years, more than 5000 examinations /year) with a mobile ultrasound unit with battery operation (LOGIQ S8) with the possibility to store dynamic digital cine-loops in DICOM format for CEUS in the PACS.
The abdomen was examined from the right side of the bed using a multi-frequency probe (C 1–6 MHz) with sterile protective measures, taking all protective measures from the right side of the bed. Initially, the abdominal organs were examined with the fundamental B-mode, then with color-coded duplex sonography (CCDS) with assessment of the hemodynamics of liver perfusion, mesenteric vessels and kidney perfusion. The extent of free fluid, the volume status was documented, urinary retention was ruled out and, including the intestine, regions of inflammation and abdominal changes were searched for. In determining the resistance index RI, guideline values of 0.5 to 0.7 were considered standard values for the renal arteries, the A. hepatica and the superior mesenteric artery. Significantly higher values were evaluated as an indication of flow against peripherally increased resistance, significantly lower values for RI as post-stenotic flow.
For CEUS, the transmission power was reduced, a low mechanical index (MI < 0.2) was selected for Contrast Harmonic Imaging (CHI) as Pulse Inversion Mode with high resolution for a depth up to 8 cm or amplitude amplified for a depth up to 15 cm. Thus, modified transcostal and subcostal scans were required for the complete evaluation of liver, kidneys and spleen. The injection of 1.5 to 2.4 ml of the ultrasound contrast medium, Sulphur-hexafluoride Microbubbles (SonoVue™, BRACCO, Italy) was performed via a central access with at least 10 ml NaCL as a bolus injection. Cine loops of CEUS of 10 to 15 s duration were dynamically documented after early arterial flooding after 10 to 15 s in double mode B-Mode/CEUS until the late phase of 5 min from the abdominal organs in sweep mode. The image storage in the PACS was performed after appropriate disinfection measures of probes and ultrasound equipment in the ultrasound center, in a special protection room. A delayed arterial contrast was assumed as a contrast at the earliest after 20 s, a portal venous contrast at the earliest after 50 s and a venous contrast beginning only after 90 s. Infarcts showed a segmental wedge-shaped perfusion deficit. Hyperemia as an expression of reactive inflammatory changes was associated with significant contrast agent enrichment within 10 to 15 s after bolus injection of the ultrasound contrast agent.
The ultrasound examinations were part of interdisciplinary case conferences and expert teams for the treatment of the COVID-19 infected patients and were correlated for clinical follow-up.
3Results
Up to now, 5 male patients between 51 and 74 years of age in a state of severe disease were examined; Table 1 shows the patients’ demographic and clinical data.
Table 1
Demographic and clinical data of the 5 patients included in the study
| Patient /age | Sex | Pulmonary | COVIC-19 Infection | Liver function | Kidney function |
| 74 years old | Male | Consolidation Intubated in intensive care | Since 3 weeks | Critical reduced Cholestasis | Dialysis |
| 52 years old | Male | Consolidation Intubated in intensive care | Since 2 weeks | Reduced | Reduced |
| 51 yaers old | Male | Consolidation Intubated in intensive care | Since 2 weeks | Reduced | Reduced |
| 68 yaers old | Male | Consolidation Intubated in intensive care | Since 3 weeks | Critically Reduced | Dialysis |
| 73 years old | Male | Consolidation Intubated in intensive care | Since 3 weeks | Critically reduced, cholestasis | Dialysis |
The abdominal ultrasound examinations including CEUS proved to be very time-consuming due to the special protective measures for the examiner and the disinfection of the ultrasound machine with 45 min up to 60 min. A battery operation with stand-by can significantly facilitate mobility, especially if a change of the patient’s side (right -y left) is required during primary acoustic examination from the right for dynamic examination of CEUS also of the spleen and left kidney under very severe acoustic conditions.
CCDS showed in all patients adjusted abdominal arterial vessels such as the hepatic artery, the mesenteric superior artery and the renal arteries with high values for RI > 0.7 in narrowed peripheral vessels with high resistance at high doses of catecholamine-containing medication. Venous flow was noticeable less reduced. In cases of beginning fibrosis of the liver tissue a reduced flow in the portal vein was found with a general lumen reduction of liver veins.
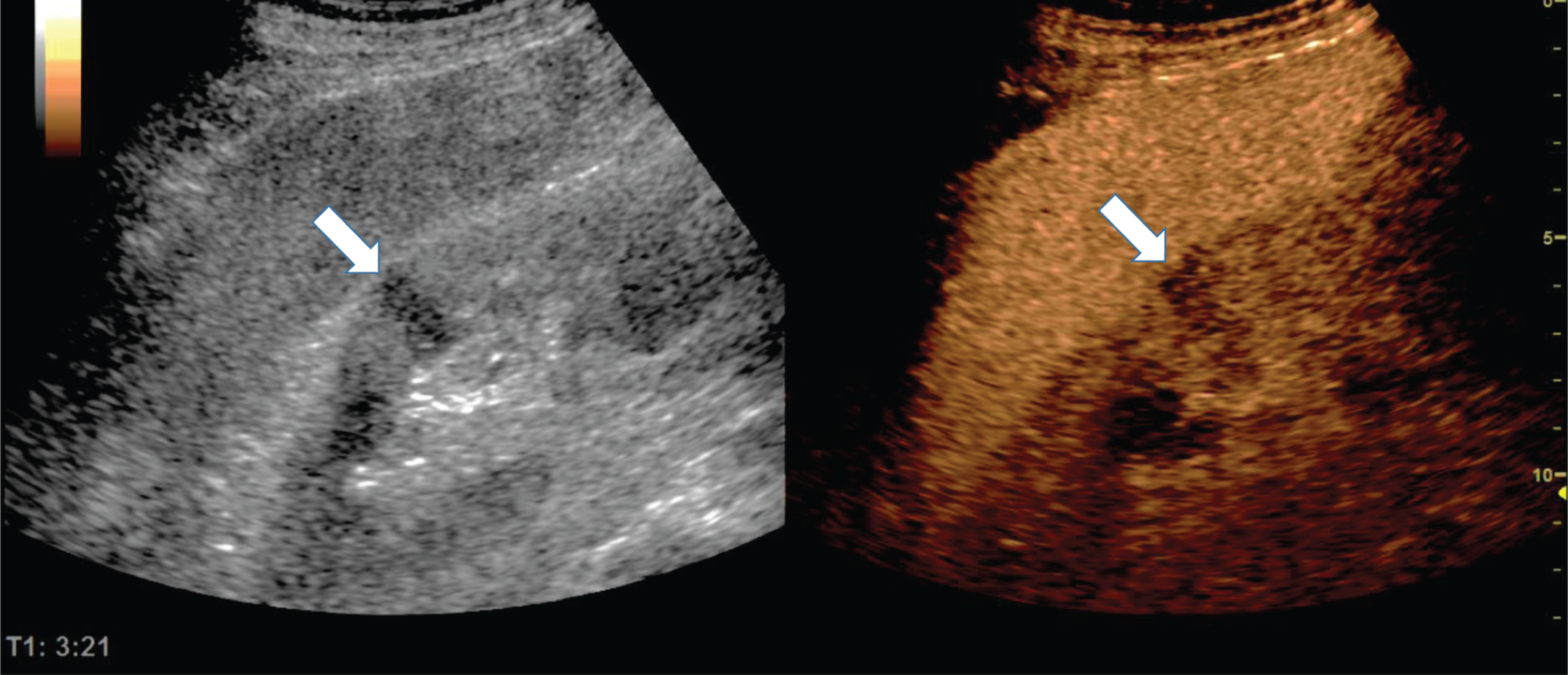
In the late phase, three minutes after the bolus injection of 2.4 ml ultrasound contrast agent an inhomogeneous enhancement of the liver and irregular hyperechogenic inflammatory signals of the lung (see arrow) were visible (Fig. 1).
Fig. 1
Representative CEUS images of liver and lung from a male 52 years old patient with COVID-19 disease of arrow with respiratory failure and inflammatory reaction of the lung with consolidations.
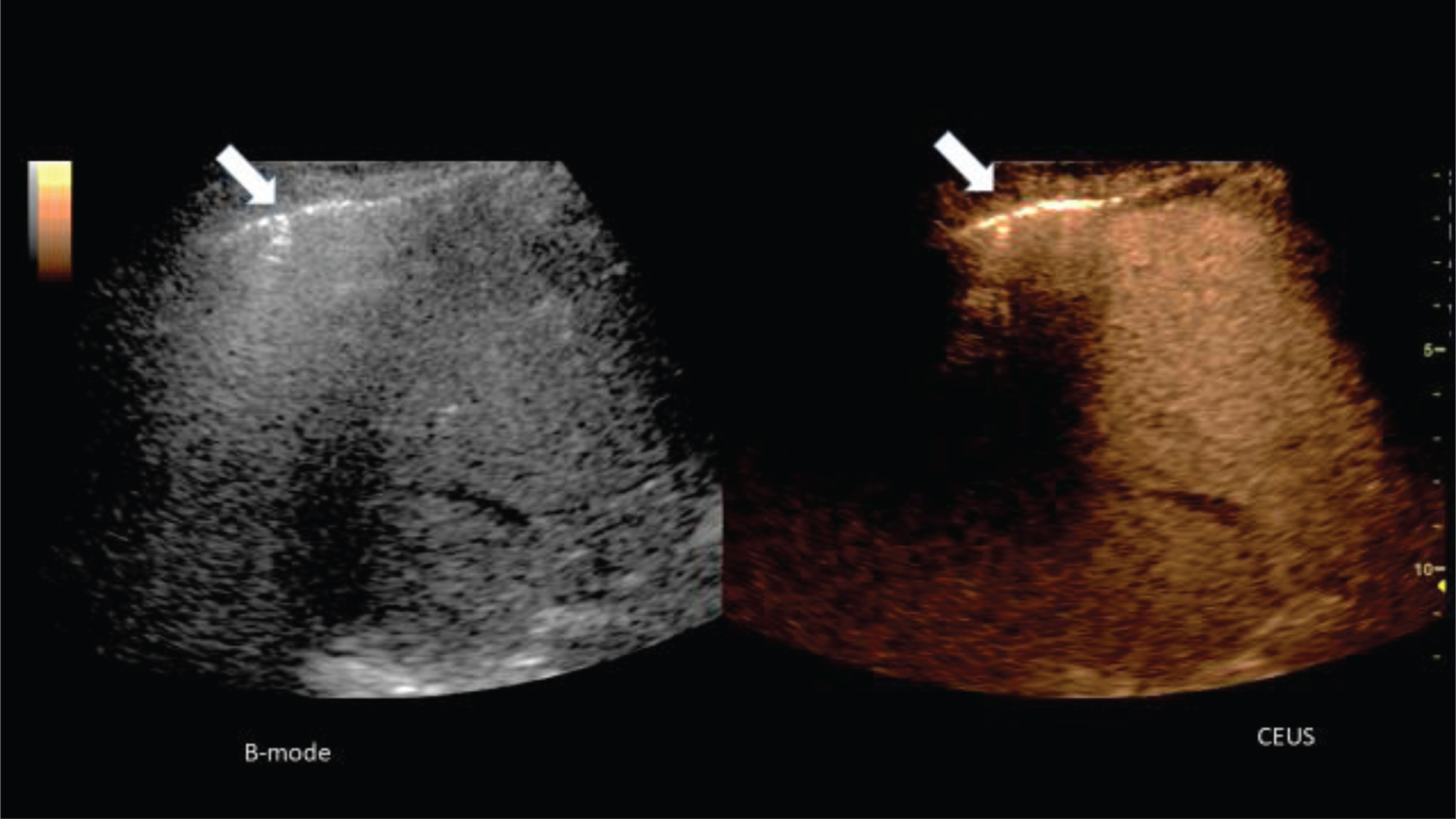
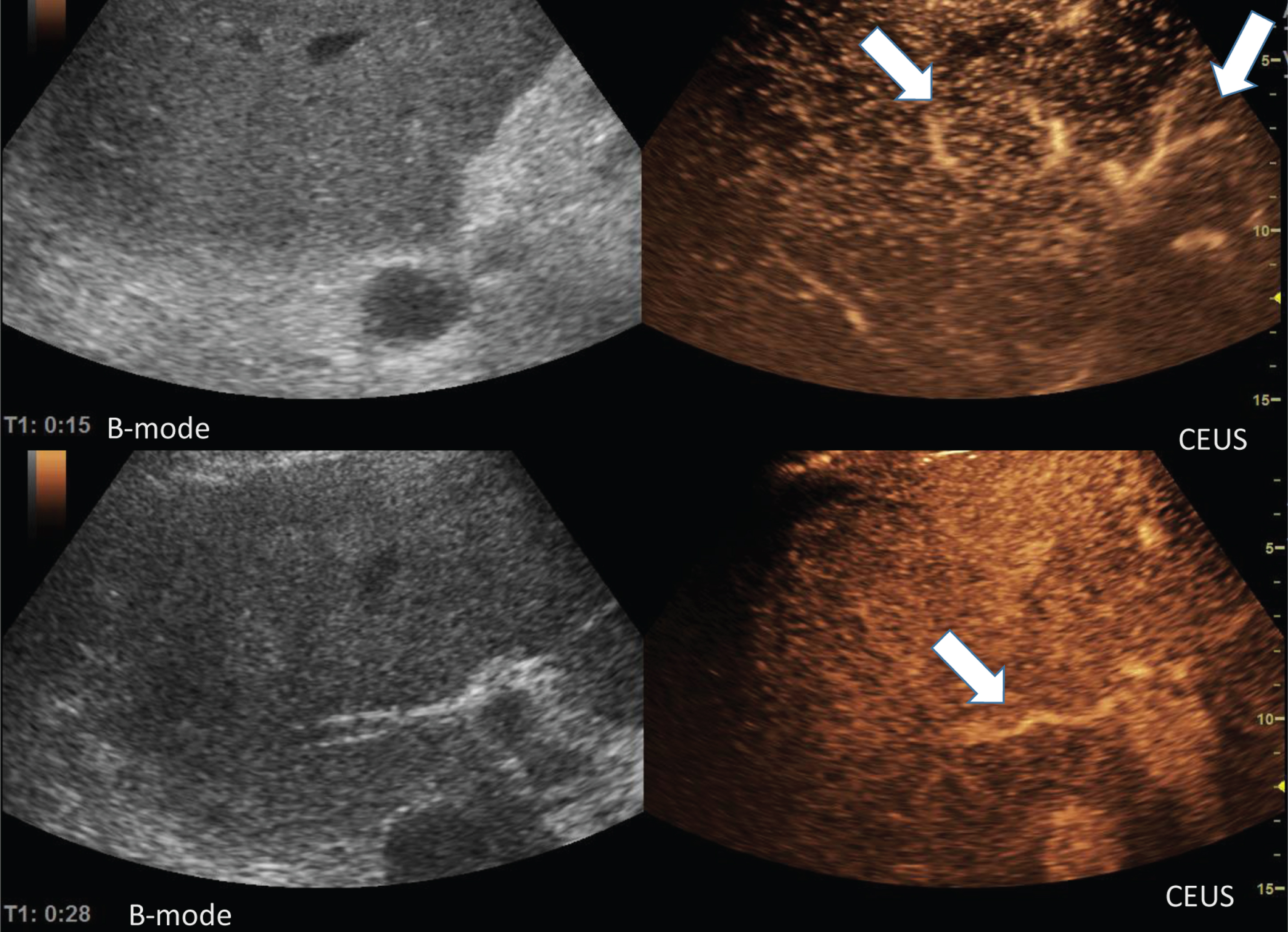
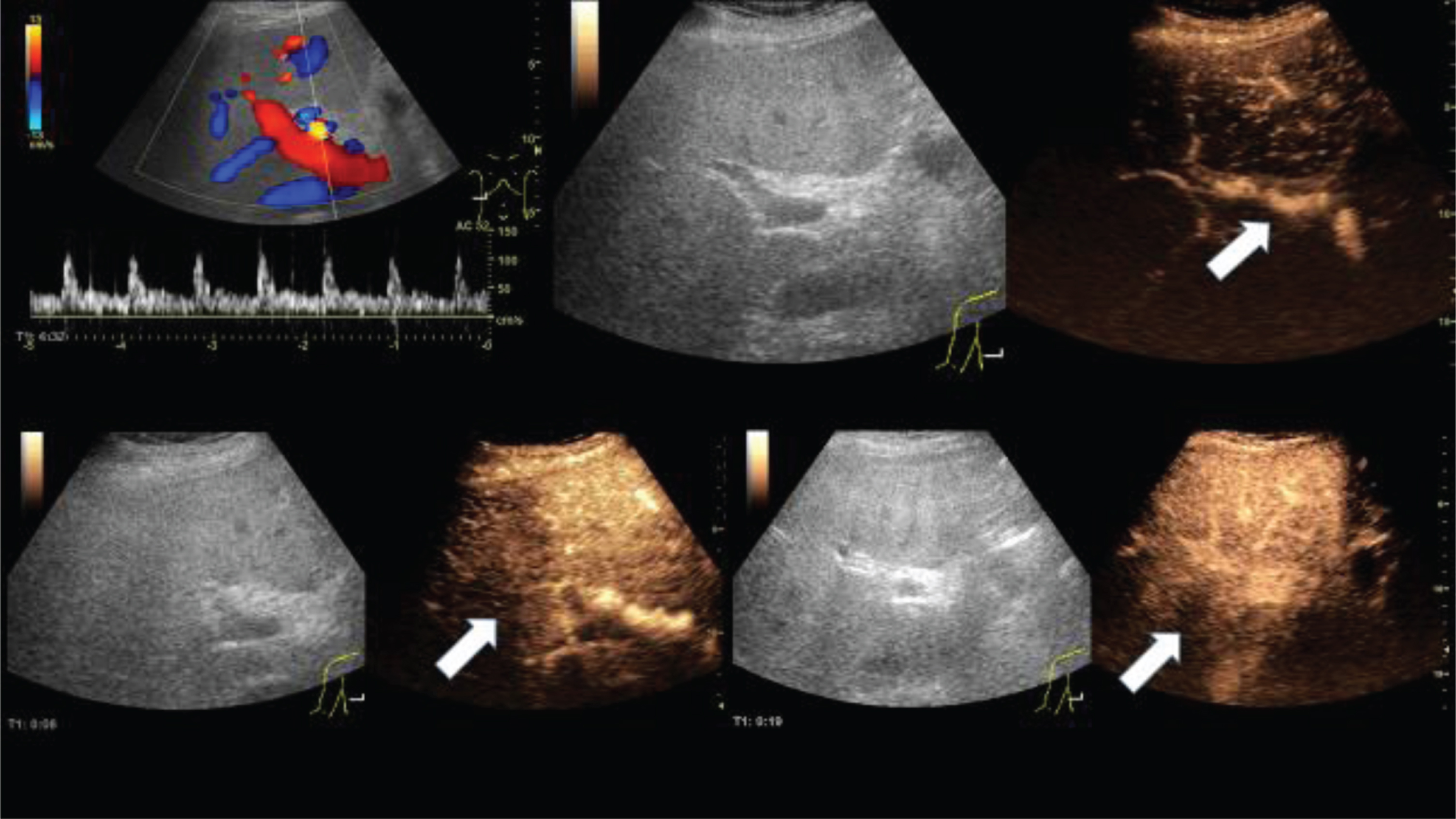
Figure 2 shows the liver during the early arterial phase (15 s and 28 s after bolus injection of the ultrasound contrast agent). An inhomogeneous enhancement of the liver with irregular intrahepatic lumen reduced arteries (arrows) occurred. In all patients with severe course of COVID-19 infections, the subcapsular contrast of liver and kidneys was delayed. The liver parenchyma was proportionally inhomogeneously contrasted like a map.
Fig. 2
Representative images of the microvasculature of the liver from a 51 years old male patient with COVID-19 disease.
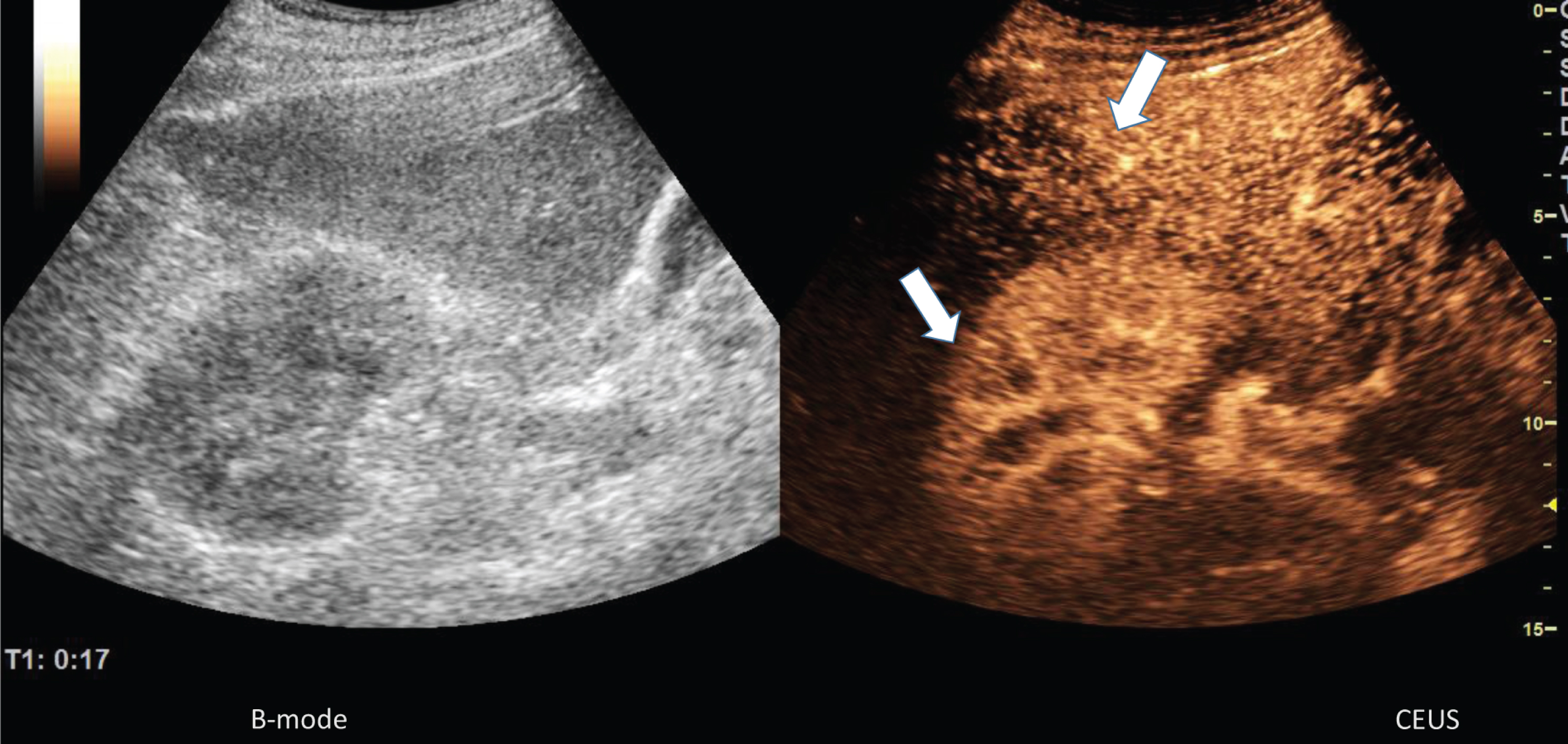
After bolus injection of 2.4 ml ultrasound contrast agent during the early arterial phase (17 s) an inhomogeneous hyperenhancement of the liver and the right kidney in the center and partially reduced microcirculation in the cortex (arrows) was visible (Fig. 3).
Fig. 3
Representative images of the microvasculature of the liver and kidney of a 68 years old male patient with COVID-19 disease.
Two minutes after bolus injection of 2.4 ml ultrasound contrast agent, a homogeneous enhancement of the enlarged spleen (Fig. 4), but reduced partial enhancement of the left kidney (see arrow). The small intestine was also sectionally reactively altered with hyperemia. Moderate splenomegaly (up to 13×6 cm) showed proportionately wedge-shaped perfusion deficits.
Fig. 4
Representative images of the microvasculature of the kidney of a 73 years old male patient with COVID-19 disease.
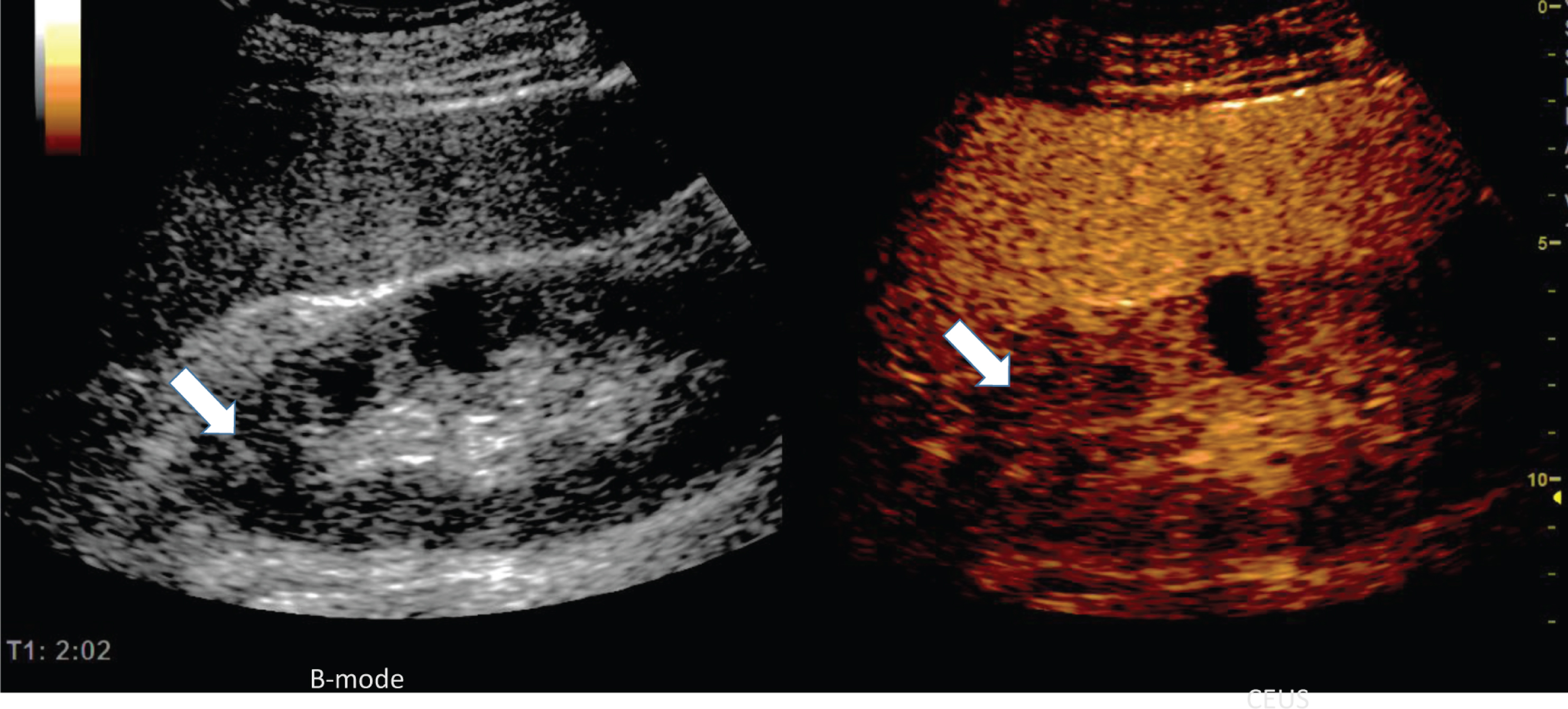
Three minutes after the bolus injection of 2.4 ml ultrasound contrast agent a homogeneous enhancement of the spleen, but segmental reduced enhancement of the left kidney was visible indicating an area of infraction (Fig. 5).
Fig. 5
Microvasculature of the kidney of a 74 years old male patient with COVID-19 disease.
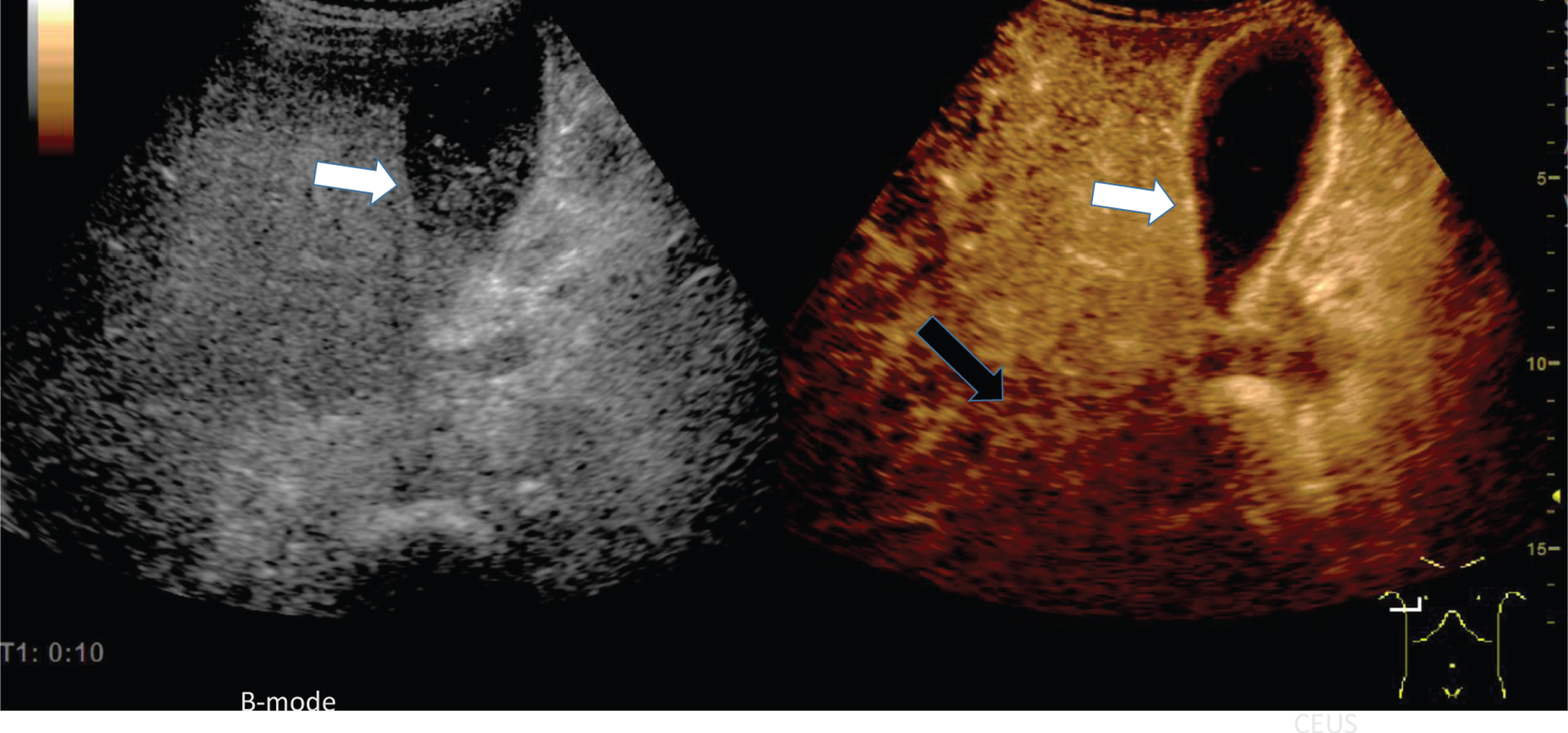
10 seconds after the bolus injection of 2.4 ml ultrasound contrast agent an early hyperenhancement of the wall of the gallbladder (white arrow) and of the surrounding liver tissue occurred corresponding to an inflammatory hyperemia (Fig. 6). In comparison to the liver tissue near the gallbladder a prolonged enhancement of the more peripheral liver tissue was visible (see black arrow). In case of acute cholecystitis, a distinct hyperemia of the gallbladder wall with edema and surrounding fluid was detectable.
Fig. 6
Inflammatory reaction of the gallbladder in a of a 73 years old male patient with COVID-19 disease.
After the bolus injection of 2.4 ml ultrasound contrast agent during the early arterial phase (8 s) and arterial phase (19 s) an inhomogeneous enhancement of the liver with irregular intrahepatic lumen reduced arteries (arrows), corresponding to Doppler signal with shorter systolic peak enhancement was found (Fig. 7).
Fig. 7
Microvasculature of the liver of a 52 years old male patient with COVID-19 disease.
4Discussion
In our experience, Contrast Enhanced Ultrasound Sonography (CEUS) is an excellent diagnostic tool for monitoring severe cases of intermediate care patients with early changes of abdominal microcirculatory disorders (8, 10, 14, 15]. CEUS can be an important diagnostic tool for monitoring capillary perfusion of abdominal organs [14, 15] and as these initial experiences suggest even in severe cases of COVID-19 infection. The advantage of CEUS with Sulphur-hexafluoride microbubbles as an ultrasound contrast agent is the dynamic assessment down to the capillary level strictly intravascular from the early arterial phase (10 to 15 s) to the late phase of 5 min [13]. Hyperemia is indicative of reactive inflammatory changes, and reduced perfusion indicated by a reduction of capillary outflow. Causes may be a clear vasospasm due to medication or micro-infarcts in the context of a septic clinical picture. Since CEUS with sulphur hexafluoride microbubbles is without risk for the kidneys [16], CEUS is also of great diagnostic importance in COVID-19 infections with imminent kidney failure. In our studies, the advantage of CEUS in comparison to X-ray contrast media could be shown, especially with regard to renal perfusion [17]. However, it seems to lead to a subcapsular impairment of the capillary liver blood flow and possible wedge-shaped perfusion deficits of the spleen. Reactive inflammatory changes not only affect the small intestine but can also lead to acute cholecystitis with edema, hyperemia and surrounding increased serous fluids. Although hemodynamic assessment by CCDS remains indispensable, CEUS allows a rapid and clear evaluation of arterial and venous organ perfusion of the liver, kidneys, spleen and mesentery. Small areas of reduced microvascularization or early infarctions of the kidneys are not visible in fundamental B-mode, but clearly detectable using dynamic CEUS [8, 17].
The time factor of CEUS bedside for COVID-19 infection with all hygienic measures for examiners and ultrasound equipment is certainly high at up to 60 minutes, but it is significantly below the set-up times for a CT examination of up to 2 hours with up to 4 accompanying persons required for storage, transport and intensive care. The hygiene measures for CT are also considerably more complex.
Contraindications for CEUS may include severe COPD with pulmonary hypertension, pulmonary arterial hypertension and acute cardiac perfusion deficit, which requires a strict indication for CEUS in Covid-19 infection with pulmonary embolism and myocarditis. A relative contraindication for CEUS is assured contrast agent intolerance to other contrast agents.
The limitation of CEUS bedside is that it requires a special mobile high-performance ultrasound technique, if possible, with battery operation, a very experienced examiner and ultrasound contrast medium with costs of up to 60 euros per 2.4 ml sulphur hexafluoride microbubbles. Nevertheless, the presented first results here open a new, very detailed view on changes in capillary abdominal organ perfusion in severe COVID-19 infection.
5Conclusion
CEUS can be an important part of a fast and effective bedside diagnosis in severe cases of COVID-19 infection, even taking into account all the complex measures, the required special ultrasound equipment and the necessary high level of experience of the examiner. These first results could be the first step for an optimized monitoring of abdominal microcirculatory disorders by CEUS in a situation of very severe Covid-19-infection, considering the situation of reduced liver function and kidney failure.
References
[1] | Zhang T , Sun LX , Feng RE . Comparison of Clinical and Pathological Features Between Severe Acute Respiratory Syndrome and Coronavirus Disease 2019. Zhonghua Jie He He Hu Xi Za Zhi. (2020) ;43: :E040. |
[2] | Yang X , Yu Y , Xu J , Shu H . Jia’an. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet. 2020. doi.org/10.1016/S2213-2600(20)30079-5 |
[3] | Han R , Huang L , Jiang H , Dong J , Peng H , Zhang D . Early Clinical and CT Manifestations of Coronavirus Disease 2019 (COVID-19) Pneumonia. AJR. (2020) ;215: :1–6. |
[4] | Peng QY , Wang XT , Zhang LN . Findings of lung ultrasonography of novel corona virus pneumonia during the 2019-2020 epidemic. Chinese Critical Care Ultrasound Study Group (CCUSG). Intensive Care Med. 2020. doi: 10.1007/s00134-020-05996-6 |
[5] | Zhang HW , Yu J , Xu HJ , Lei Y , Pu ZH , Dai WC , Lin F , Wang YL , Wu XL , Liu LH , Li M , Mo YQ , Zhang H , Luo SP , Chen H , Lyu GW , Zhou ZG , Liu WM , Liu XL , Song HY , Chen FZ , Zeng L , Zhong H , Guo TT , Hu YQ , Yang XX , Liu PN , Li DF . Corona Virus International Public Health Emergencies: Implications for Radiology Management. Acad Radiol. (2020) ;27: (4):463–7. |
[6] | Hariri G , Joffre J , Leblanc G , Bonsey M , Lavillegrand JR , Urbina T , Guidet B , Maury E , Bakker J , Ait-Oufella H . Narrative review: clinical assessment of peripheral tissue perfusion in septic shock. Ann Intensive Care. (2019) ;9: (1):37. |
[7] | Harrois A , Grillot N , Figueiredo S , Duranteau J . Acute kidney injury is associated with a decrease in cortical renal perfusion during septic shock. Crit Care. (2018) ;22: (1):161. doi: 10.1186/s13054-018-2067-0 |
[8] | Sidhu PS , Cantisani V , Dietrich CF , Gilja OH , Saftoiu A , Bartels E , Bertolotto M , Calliada F , Clevert DA , Cosgrove D , Deganello A , D’Onofrio M , Drudi FM , Freeman S , Harvey C , Jenssen C , Jung EM , Klauser AS , Lassau N , Meloni MF , Leen E , Nicolau C , Nolsoe C , Piscaglia F , Prada F , Prosch H , Radzina M , Savelli L , Weskott HP , Wijkstra H . The EFSUMB Guidelines and Recommendations for the Clinical Practice of Contrast-Enhanced Ultrasound (CEUS) in Non-Hepatic Applications: Update 2017 (Long Version). Ultraschall Med. (2018) ;39: (2):e2–e44. |
[9] | Krüger PC , Mentzel HJ . [Radiological evaluation of acute abdomen in children]. Radiologe. (2019) ;59: (2):146–53. |
[10] | Putz FJ , Verloh N , Erlmeier A , Schelker RC , Schreyer AG , Hautmann MG , Stroszczynski C , Banas B , Jung EM . Influence of limited examination conditions on contrast-enhanced sonography for characterising liver lesions. Clin Hemorheol Microcirc. (2019) ;71: (2):267–76. |
[11] | Furrer MA , Spycher SCJ , Büttiker SM , Gross T , Bosshard P , Thalmann GN , Schneider MP , Roth B . Comparison of the Diagnostic Performance of Contrast-enhanced Ultrasound with That of Contrast-enhanced Computed Tomography and Contrast-enhanced Magnetic Resonance Imaging in the Evaluation of Renal Masses: A Systematic Review and Meta-analysis. Eur Urol Oncol. 2019. DOI: 10.1016/j.euo.2019.08.013. |
[12] | Sidhu PS , Cantisani V , Dietrich CF , Gilja OH , Saftoiu A , Bartels E , Bertolotto M , Calliada F , Clevert DA , Cosgrove D , Deganello A , D’Onofrio M , Drudi FM , Freeman S , Harvey C , Jenssen C , Jung EM , Klauser AS , Lassau N , Meloni MF , Leen E , Nicolau C , Nolsoe C , Piscaglia F , Prada F , Prosch H , Radzina M , Savelli L , Weskott HP , Wijkstra H . The EFSUMB Guidelines and Recommendations for the Clinical Practice of Contrast-Enhanced Ultrasound (CEUS) in Non-Hepatic Applications: Update 2017 (Short Version). Ultraschall Med. (2018) ;39: (2):154–80. |
[13] | Dietrich CF , Averkiou M , Nielsen MB , Barr RG , Burns PN , Calliada F , Cantisani V , Choi B , Chammas MC , Clevert DA , Claudon M , Correas JM , Cui XW , Cosgrove D , D’Onofrio M , Dong Y , Eisenbrey J , Fontanilla T , Gilja OH , Ignee A , Jenssen C , Kono Y , Kudo M , Lassau N , Lyshchik A , Franca Meloni M , Moriyasu F , Nolsøe C , Piscaglia F , Radzina M , Saftoiu A , Sidhu PS , Sporea I , Schreiber-Dietrich D , Sirlin CB , Stanczak M , Weskott HP , Wilson SR , Willmann JK , Kim TK , Jang HJ , Vezeridis A , Westerway S . How to perform Contrast-Enhanced Ultrasound (CEUS). Ultrasound Int Open. (2018) ;4: (1):E2–E15. |
[14] | Lerchbaumer MH , Putz FJ , Rübenthaler J , Rogasch J , Jung EM , Clevert DA , Hamm B , Makowski M , Fischer T . Contrast-enhanced ultrasound (CEUS) of cystic renal lesions in comparison to CT and MRI in a multicenter setting. Clin Hemorheol Microcirc. 2020. DOI: 10.3233/CH-190764. |
[15] | Lerchbaumer MH , Kleemann T , Jung EM , Nagel S , Hamm B , Fischer T . Vascular pattern and diagnostic accuracy of contrast-enhanced ultrasound (CEUS) in spleen alterations. Clin Hemorheol Microcirc. 2020. DOI: 10.3233/CH-190758. |
[16] | Lamby P , Prantl L , Krüger-Genge A , Franke RP , Jung EM , Jung F . Clin Hemorheol Microcirc. Influence of Ultrasound Microbubbles on kidney oxygen tension. (2017) ;67: (3-4):211–4. |
[17] | Lamby P , Jung F , Graf S , Schellenberg L , Falter J , Platz-da-Silva N , Schreml S , Prantl L , Franke RP , Jung EM . Effect of Iodinated Contrast Media on Renal Perfusion: A Randomized Comparison Study in Pigs Using Quantitative Contrast-Enhanced Ultrasound (CEUS). Sci Rep. (2017) ;7: (1):13125. |




