The hierarchy of preventive measures to protect workers against the COVID-19 pandemic: A review
Abstract
BACKGROUND:
The high spread rate of coronaviruses, specifically severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has raised concerns about the spread of the disease in crowded occupational environments. The risk of occupational exposure to coronavirus depends on the type of industry and the nature of work. Currently, most countries are working for reactivating their economies and need to improve working conditions for a safe situation during the COVID-19 pandemic.
OBJECTIVE:
The present work aimed to investigate the current engineering and administrative control measures, which are necessary to protect workers against COVID-19 in workplaces.
METHODS:
The current strategies, including engineering control, administrative control, personal protective equipment, and their efficiencies, were reviewed and discussed.
RESULTS:
Reviewing the literature indicated that a collection of control approaches should be implemented for an effective control of the virus. Control measures could be selected based on the risk of exposure to COVID-19. The results also revealed that relying solely on a specific control measure could not effectively control the outbreak.
CONCLUSION:
In conclusion, employers and health professionals must continually monitor international and local guidelines to identify changes in recommendations to make their workplaces safer. Establishment of an expert team in any workplace for the implementation of more effective control measures is warranted, as well.
1Introduction
The novel coronavirus disease, known as COVID-19, is a cluster of acute respiratory effects caused by the SARS-CoV-2 virus, with a rapid outbreak among humans around the world [1]. To date, over 19 million people have caught COVID-19, with 712000 recorded global deaths by July 2020. At the beginning of the COVID-19 outbreak, various countries decided to disrupt several businesses, which led to substantial job losses. However, is it possible to disrupt all jobs until the situation improves? Absolutely not. Most countries are working to reactivate their economies and need to improve conditions for a safe activity during the COVID-19 pandemic. It is known that COVID-19 is primarily spread from a person to another, which raises concerns about its outbreak in crowded occupational environments. Yet, the risk of occupational exposure to coronavirus depends on the type of industry. According to the occupational risk pyramid introduced by the Occupational Safety and Health Administration (OSHA), job tasks can be divided into four exposure levels, including low, medium, high, and very high-risk tasks. Healthcare workers who perform aerosol-generating procedures, such as induction procedures, laboratory personnel handling, and specimen collection, as well as morgue workers who perform autopsies are at a very high-level risk of exposure to SARS-CoV-2. Support staff, healthcare delivery workers who must enter patients’ rooms, medical transport workers like ambulance operators, and mortuary workers are also considered as high exposure or high risk. The staff with possible contact to suspected or infected people within a six-feet distance have a medium risk of exposure. Lower exposure risk jobs are those with no requirement to contact with suspected people. Workers in the lower risk category have the least occupational contact with other coworkers or customers.
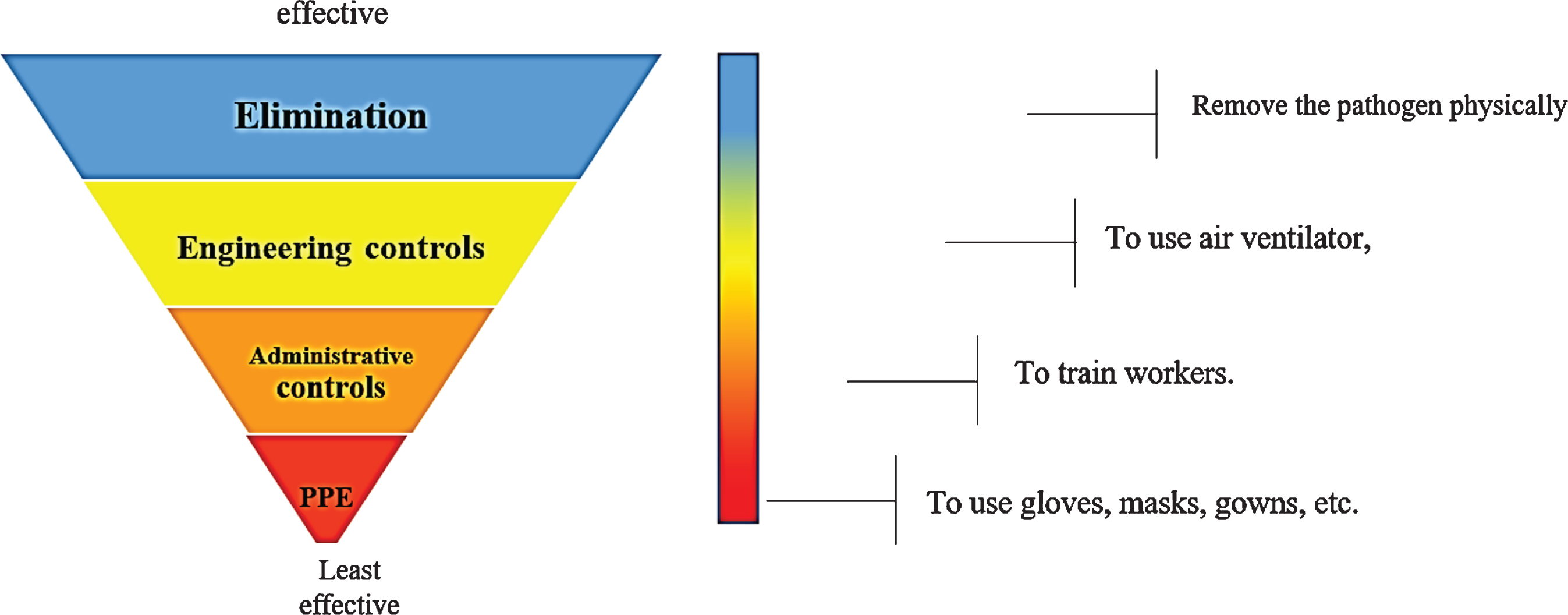
To reduce the influence of COVID-19 on workers in any workplace, some control measures should be taken based on the level of risk. It is worth mentioning that employers should reduce the risk of exposure to SARS-COV-2 based on their risk levels in their workplaces. They can decrease the number of lost days due to diseases and slow or stop the spread of COVID-19 by conducting risk management programs to make workplaces clean and hygienic [2]. The overall process of risk management of occupational hazards consists of four steps, including hazards identification, risk assessment, control measures, and monitor of controls [3]. Coronavirus is a biological hazard that needs to be controlled through a comprehensive program in any workplace. According to the study conducted by Rim et al., a number of measures, such as risk assessment, ventilation, training, and use of Personal Protective Equipment (PPE), could be applied to control biological hazards in workplaces [4]. Occupational safety and health experts use a framework known as the “hierarchy of controls” (Fig. 1), which means that the controls located at the first level are more effective. In other words, like other workplace hazards, elimination of coronavirus is more favorable compared to other control measures. However, it may not be always possible to eliminate COVID-19 from the workplace and, consequently, preventive efforts should be applied to minimize the probability of exposure to SARS-CoV-2. In addition, some measures must be taken to avoid new infections due to the spread of the virus. The engineering controls followed by administrative controls and PPE are the most effective ways to control the exposure to COVID-19 [5].
Fig. 1
The biological hazards control pyramid adapted from the US Center for Disease Control (CDC).
2Engineering controls to reduce occupational exposure to COVID-19
Since elimination or substitution of biohazards is not applicable in COVID-19, engineering controls are the most effective solution to reduce the exposure. Application of engineering controls helps minimize or prevent the exposure to COVID-19 without relying on workers’ behaviors. Engineering controls refer to a collection of measures that have priority in the control of hazards in workplaces. These measures are not recommended for workplaces with lower exposure risks to coronaviruses because of the relatively high running and maintenance costs. In fact, employers should use engineering controls to protect workers in high-risk jobs. Improvement of ventilation systems, use of high-efficiency air filters, and use of physical barriers are among the most effective engineering solutions to prevent the transmission of SARS-CoV-2.
2.1Efficient ventilation
At the time of writing the present article, three different modes of viral transmission were introduced for the spread of the respiratory droplets of coronaviruses. In this context, contact transmission via contaminated surfaces, transmission by large respiratory droplets (>10 microns), and transmission via airborne micro droplets (<5 microns) were among the main scenarios for SARS-CoV-2 transmission [6]. Although there has been controversy about the airborne transmission of SARS-COV-2, an increasing number of reports provided strong evidence in the role of aerosols in COVID-19 outbreak, especially in poorly ventilated environments [7–10]. Aerosols consist of small droplets, which can stay suspended in the air for a longer time compared to larger droplets [11]. One experimental study showed that SARS-CoV-2 remained active for up to three hours in indoor air under common conditions [12]. Several studies have also indicated that SARS-CoV-2 particles could stay airborne and travel long distances in indoor environments, depending on humidity and temperature [13]. Moreover, various investigations indicated that COVID-19 transmission could be especially significant in confined and crowded indoor spaces, such as workplaces [14, 15]. Thus, the American Society of Heating, Refrigeration, and Air-Conditioning Engineers (ASHRAE) has recommended the use of ventilation control measures regarding the potential airborne hazard. Ventilation is the process of supplying clean outdoor air to a building by mechanical or natural means [16, 17]. Ventilation systems normally exist in all workplaces to control harmful chemical agents or air conditioning. Ventilation is usually provided by Heating, Ventilation, and Air-Conditioning (HVAC). HVAC systems are the usual systems used in any workplace to provide comfortable conditions (humidity and temperature) and clean air in indoor environments. In the case of COVID-19, the current systems can be modified with a relatively low cost to enhance their efficiency and to limit the outbreak of the virus. In some workplaces such as hospitals and other healthcare centers, good ventilation systems can already be found to protect people against infectious agents [18]. Based on the literature review, some advice has been given to improve ventilation efficiency in outbreak conditions.
2.2Increasing the numbers of air exchanges
In order to eliminate any trace of infectious agents, increasing air supply and exhaust ventilation systems are necessary for all parts of the workplace. In buildings with mechanical ventilation systems, the time of the operation of the ventilation system is necessary to be expanded. For example, turning the ventilation system on before beginning the work and keeping it running for at least two hours after finishing the routine work could increase air exchanges and enhance the efficiency of ventilation. In demand-controlled systems, it is better to keep ventilation on 24.7 and lower the ventilation rates in the absence of workers. In systems with Demand-Control Ventilation (DCV), it has been recommended to disable the control because air supply can be reduced according to the temperature or occupancy. It has been also suggested to keep the ventilation systems running through the night and weekends in order to be sure about the complete removal of harmful contaminants. In this situation, the operation time should be expanded and the application of energy saving and control-demand systems should be avoided [19, 20].
2.3Avoiding air recirculation
Although air recirculation is an essential measure for saving energy, it should be avoided when there is a possibility to transport infectious contaminants through spaces. Virus particles maintained in return ducts could re-enter a working station when centralized ventilation units are equipped with recirculation sectors. Recirculation of air can lead to the distribu-tion of airborne contaminants from one point to the others who are connected to the same system. Therefore, for industries with such ventilation systems, the running should be done at 100%outdoor fresh air to avoid central recirculation during the COVID-19 pandemic. The results obtained from the previous studies regarding airborne transmission of bioaerosols, such as influenza and biological agents during terrorist attacks, indicated that air recirculation had to be stop-ped [21]. According to the Federation of European Heating, Ventilation and Air Conditioning Associations (REHVA), the recirculation dampers should be closed in spite of cooling or heating problems because the health of people is more important than thermal comfort. Therefore, in workplaces with cooling and heating problems, other local heating and cooling devices could be replaced to provide thermal comfort. The REHVA also stated that using high efficiency filters in recirculation units could not be a reason to open the recirculation dampers. Induction units and fan coils with local circulation have also been suggested to be turned off in order to prevent the resuspension of virus particles. Therefore, recirculation systems should be disabled by opening the outdoor air dampers and closing the recirculation dampers. In cases where it is not possible, the outdoor airflow should be maximized. Another alternative is the use of ultraviolet irradiation in workplaces to reactivate the virus in recirculation air [20].
2.4Increasing the use of outdoor air
Proper ventilation with outside air is an important practice for improving indoor air quality and protecting workers against COVID-19. Expanding the use of outdoor air could be achieved simply by opening the windows. Opening outdoor air dampers could also play an important role in getting outdoor air into the workplace. With turning thermostat settings to the ‘ON’ position, much air would move through the system, making the environment cleaner and safer for the personnel. The critical point is the amount of air supplied per person. It has been recommended to enlarge the social distance among workers in order to improve the ventilation cleaning effects.
2.5High-efficiency air filter
As mentioned earlier, air recirculation can transmit the virus within buildings in workplaces. Thus, if possible, it is necessary to filter the air before being distributed in the building. HVAC systems usually filter air before distribution through buildings in order to reduce the airborne transmission of viruses. Air filtration can be considered as a risk mitigation approach, but is not regarded as a solution by itself. High-Efficiency Particulate Air (HEPA) filters are a type of air cleaners manufactured by pleating fibrous media, such as microfiber glass, which have been proposed as the best filters against very fine particles. For high and very high-risk work activities such as Aerosol-Generating Procedures (AGPs), the use of HEPA filters can help control the suspended aerosols. The coronavirus has a diameter of about 0.125 microns (125 nanometers), which falls within the HEPA filter efficiency range of 0.01 microns (10 nanometers) and bigger. Many reports have wrongly stated that HEPA filters cannot filter the particles sizing 0.3 microns or lower and are thus not able to capture coronaviruses. However, the NASA study showed that HEPA filters were efficient almost 100%at 0.01 microns. Therefore, they could capture ultrafine particles below 0.3 microns, including coronavirus particles. Although HEPA filters are usually used in filtration systems of healthcare centers, such as hospitals, they could be utilized in other occupational settings. The Center for Disease Control (CDC) previously recommended the use of HEPA filters as a control strategy for SARS-CoV-1 in 2003. The CDC has also recently suggested the use of HEPA filters in air purifier respirators for the effective control of SARS-CoV-2 [22].
2.6Portable air cleaner
Portable air cleaners, known as air purifiers, are supplementary systems that can help remove parti-cles from the air with the same efficiency as the ventilation systems. In specific situations where the existence of ventilation cannot be improved, local air cleaning devices could provide more protection against SARS-COV2. The portable air cleaner must have HEPA filters to have a significant role in air cleaning. Electrostatic filtration-based devices with high efficiency in air cleaning could be introduced as a good alternative in situations where air cleaners are not applicable due to limited airflow. During the utilization of electrostatic filtration-based devices, it is better to be located close to the workers’ breathing zone to be more efficient. A schematic view of the proposed engineering controls based on improvement of the ventilation systems has been depicted in Fig. 2. Accordingly, collection of air cleaning systems has been proposed to be used to control the exposure to SARS-CoV-2. Considering the risk of exposure in workplaces, one or more systems could be applied to protect workers against COVID-19.
Fig. 2
A schematic view of the proposed engineering controls based on the improvement of ventilation systems.

2.7Physical barriers
Although maintenance of a two-meter social distance among co-workers is important to decrease the potential transmission of COVID-19, workers are often not able to keep this distance, especially in small businesses. Hence, these occupational settings should consider innovative approaches based on a barrier that could be purpose-made or improved according to the nature of works. These physical berries, which have been recommended for work activities with medium risk levels, help maintain a distance and decrease droplet transmission by limiting human-to-human interactions. Plastic shielding, mobile drawer, and partitions are good choices for providing a barrier among workers [23]. Various organizations have proposed the use of barriers, such as plexiglass, for a variety of industries. CDC and OSHA have also recommended the installation of physical barriers, such as clear plastic or plexiglass barriers, in pharmacies. World Health Organization (WHO) has also proposed the use of physical barriers in healthcare centers, such as pharmacy windows. Plexiglass is advantageous because it is more available, transparent, smooth, and easily cleanable. Polycarbonate and tempered glass are other options that are more durable but more expensive. Characteristics, such as impact resistance and scratches, should be considered before the installation of physical barriers. Another important point that should be taken into account when installing barriers is the ventilation requirements to prevent interference with HVAC systems.
3Administrative controls
The main goal of administrative controls is to minimize the exposure to SARS-CoV-2 through chan-ges in work procedures. Exposure to SARS-CoV-2 should be limited by decreasing the total number of workers in each work shift. Minimizing contact among workers by limiting face-to-face meetings and communications is one of the examples of administrative measures. Establishing extra shifts or alternative days may help maintain the full onsite work. Provi-ding workers with ongoing education and training programs is another useful action to limit their exposure. Training may highlight the importance of social distancing, protective behaviors, use of Respiratory Protective Equipment (RPE), and maintenance and disposal of masks.
4Personal protection equipment
Although engineering and administrative controls have been considered as effective alternatives in protecting workers from SARS-CoV-2 exposure, the use of PPE should be considered as an integral part of the control strategy. Workers in all risk groups need one or more PPE, including facemasks or respirators, face shields, goggles, gloves, and gowns, based on their job tasks as well as their risk levels. Healthcare personnel, such as those who work in hospitals or laboratories, should use all above-mentioned PPE. Workers in other occupational settings must also wear facemasks and gloves, and may even need additional protection. All types of PPE must be selected, ins-pected, maintained, and used properly to provide adequate protection. Among all PPE, the use of RPE and facemasks is very crucial because of their protection ability against breathing, coughing, or sneezing droplets. Many guidelines and recommendations on different aspects of PPE against SARS-CoV-2 exposure have been given in details elsewhere [24–26]. The N95 filtering face piece respirators and other respirators must be used under the written, comprehensive respiratory protection program according to the National Institute for Occupational Safety and Health (NIOSH). This program contains some essential aspects regarding RPE, such as donning, doffing, user seal check, and fit testing of respirators. Sealing and fitting the respirators affect the overall acquired protection. Fit testing is performed for tight-fitting respirators and checking their model and size with the user’s face based on OSHA’s respiratory protection standard, 29 CFR. OSHA has recently recommended initial fit testing for workers in high-risk and very high-risk jobs, including healthcare workers. The health specialist in any workplace must also justify the importance of performing a seal check after putting on the respirator to ensure getting an adequate seal.
5Conclusion
Different preventive measures have been proposed to control the transmission of coronaviruses in workplaces. Control measures should be selected based on the risk of exposure to SARS-CoV-2. Yet, a collection of control measures is more efficient and practical to protect workers against COVID-19. Moreover, employers and health professionals must continually monitor international and local guidelines to identify changes in recommendations and to make their workplaces safer. An expert team is also recommended to be established in any workplace for the implementation of more effective control measures.
Conflict of interest
None declared.
Funding
This work was supported by Shiraz University of Medical Sciences (Grant No. 22089).
Acknowledgment
The authors would like to thank Ms. A. Keivanshekouh at the Research Improvement Center of Shiraz University of Medical Sciences for improving the use of English in the manuscript.
References
[1] | Abd El-Aziz TM , Stockand JD . Recent progress and challenges in drug development against COVID-19 coronavirus (SARS-CoV-2)-an update on the status. Infection, Genetics and Evolution. (2020) :104327. |
[2] | Adams JG , Walls RM . Supporting the health care workforce during the COVID-19 global epidemic. Jama. (2020) ;323: (15):1439–40. |
[3] | Rout B , Sikdar B . Hazard identification, risk assessment, and control measures as an effective tool of occupational health assessment of hazardous process in an iron ore pelletizing industry. Indian Journal of Occupational and Environmental Medicine. (2017) ;21: (2):56. |
[4] | Rim K-T , Lim C-H . Biologically hazardous agents at work and efforts to protect workers’ health: a review of recent reports. Safety and Health at Work. (2014) ;5: (2):43–52. |
[5] | de Castro AB . ‘Hierarchy of Controls’: Providing a framework for addressing workplace hazards. AJN The American Journal of Nursing. (2003) ;103: (12):104. |
[6] | Organization WH. Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations: scientific brief, 27 March 2020. World Health Organization; 2020. |
[7] | Coleman KK , Nguyen TT , Yadana S , Hansen-Estruch C , Lindsley WG , Gray GC . Bioaerosol sampling for respiratory viruses in Singapore’s mass rapid transit network. Scientific Reports. (2018) ;8: (1):1–7. |
[8] | Knibbs LD , Morawska L , Bell SC . The risk of airborne influenza transmission in passenger cars. Epidemiology & Infection. (2012) ;140: (3):474–8. |
[9] | Li Y , Huang X , Yu I , Wong T , Qian H . Role of air distribution in SARS transmission during the largest nosocomial outbreak in Hong Kong. Indoor Air. (2005) ;15: (2):83–95. |
[10] | Nishiura H , Oshitani H , Kobayashi T , Saito T , Sunagawa T , Matsui T , et al. Closed environments facilitate secondary transmission of coronavirus disease 2019 (COVID-19). medRxiv. 2020. |
[11] | Ong SWX , Tan YK , Chia PY , Lee TH , Ng OT , Wong MSY , et al. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. Jama. (2020) ;323: (16):1610–2. |
[12] | Chin A , Chu J , Perera M , Hui K , Yen H-L , Chan M , et al. Stability of SARS-CoV-2 in different environmental conditions. medRxiv. 2020. |
[13] | Dietz L , Horve PF , Coil DA , Fretz M , Eisen JA , Van Den Wymelenberg K . novel coronavirus (COVID-19) pandemic: Built environment considerations to reduce transmission. Msystems. (2020) ;5: (2). |
[14] | Leclerc QJ , Fuller NM , Knight LE , Funk S , Knight GM , Group CC-W . What settings have been linked to SARS-CoV-2 transmission clusters? Wellcome Open Research. (2020) ;5: (83):83. |
[15] | Hamner L . High SARS-CoV-2 attack rate following exposure at a choir practice—Skagit County,Washington, March 2020. MMWR Morbidity and Mortality Weekly Report. 2020;69. |
[16] | Lewis D . Is the coronavirus airborne? Experts can’t agree. Nature. (2020) ;580: (7802):175. |
[17] | Morawska L , Cao J . Airborne transmission of SARS-CoV-2: The world should face the reality. Environment International. (2020) :105730. |
[18] | Phiri M . Health Building Note 00-01 General design guidance for healthcare buildings. Department of health. 2014. |
[19] | Federation of European Heating VaACA. COVID-19 Guidance: REHVA uA, https://www.rehva.eu/fileadmin/user_upload/REHVA_COVID19_guidance_document_ver2_20200403_1.pdf Af. |
[20] | ASHRAE; ASoHR-CApdoiaA, from: cJA, https://www.ashrae.org/file%20library/about/position%20documents/pd_infectiousaerosols_2020.pdf. |
[21] | Persily A , Chapman RE , Emmerich SJ , Dols WS , Davis H , Lavappa P , et al. Building retrofits for increased protection against airborne chemical and biological releases. National Institute of Standards and Technology, Gaithersburg, MD. (2007) . |
[22] | Christopherson DA , Yao WC , Lu M , Vijayakumar R , Sedaghat AR . High-Efficiency Particulate Air Filters in the Era of COVID-19: Function and Efficacy. Otolaryngology–Head and Neck Surgery. 2020:0194599820941838. |
[23] | Dyal JW . COVID-19 Among Workers in Meat and Poultry Processing Facilities—19 States, April 2020. MMWR Morbidity and Mortality Weekly Report. 2020;69. |
[24] | Livingston E , Desai A , Berkwits M . Sourcing personal protective equipment during the COVID-19 pandemic. Jama. (2020) ;323: (19):1912–4. |
[25] | Organization WH. Rational use of personal protective equipment (PPE) for coronavirus disease (COVID-19): interim guidance, 19 March 2020. World Health Organization; 2020. |
[26] | Hirschmann MT , Hart A , Henckel J , Sadoghi P , Seil R , Mouton C . COVID-19 coronavirus: recommended personal protective equipment for the orthopaedic and trauma surgeon. Knee Surgery, Sports Traumatology, Arthroscopy. (2020) ;28: (6):1690. |




