The factors of non-specific chronic low back pain in nurses: A meta-analysis
Abstract
BACKGROUND:
Numerous studies have investigated factors for non-specific chronic low back pain (NSCLBP) in nurses, and have reached different conclusions. Evidence-based recommendations are required for the prevention and treatment of NSCLBP in nurses.
OBJECTIVE:
This meta-analysis aimed to systematically review and quantify the factors of NSCLBP in nurses.
METHODS:
Eleven databases were searched. The odds ratios (OR) with 95% confidence intervals (CIs) were pooled using meta-analysis, and either a fixed-effect or random-effect model was used based on heterogeneity across included studies.
RESULTS:
Eighteen publications including 11,752 nursing staff were included. Being female (pooled estimate [95% CI], 1.56 [1.24–1.96];
CONCLUSIONS:
This is the first meta-analysis to quantify the risk factors for NSCLBP in nurses. Being female, married, working night shifts, overweight, working at least 10 years and dissatisfied with work are risk factors. High-quality prospective studies are required to validate the findings of this study.
1.Introduction
Non-specific chronic low back pain (NSCLBP) is characterized by muscle stiffness, tension, or pain localized between the gluteal folds and the costal margin, with or without referred leg pain, without a specific somatic origin, and with the course of the disease lasting more than 12 weeks [1]. With the development and application of diagnostic and therapeutic technologies and the aging population in some countries, the number of critically ill patients being treated by nurses has increased, creating a nursing environment where many physical, chemical, ergonomic, and other harmful factors coexist [2, 3]. These occupational hazards have caused acute and chronic damage to the health of nurses. NSCLBP in nurses in particular is a major health problem, with an increasing occurrence worldwide. The incidence of NSCLBP in nurses is reported to be 61–72% [4, 5, 6], and has resulted in frequent nursing staff resignations and absences due to ill health [7].
Nurses not only play a professional role in public health, such as in hospital communities, but they also play a key role in responding to various health challenges, including the coronavirus disease 2019 (COVID-19) pandemic. The occurrence of NSCLBP among nurses differs somewhat from that among workers in other occupations. First, the working environment of nurses involves a heavy workload and high technical requirements [8]. Second, NSCLBP in nurses is often caused by common nursing procedures such as assisting patients to turn over, administering intravenous treatment, or inserting indwelling urinary catheters [9]. NSCLBP in nurses affects their physical and mental health, and is detrimental to the development of the nursing team and the safety of patients.
From a physical point of view, some nursing operations, including catheterization or introducing a central venous catheter (CVC), require the nurse to maintain the same posture, such as sitting, leaning forward, or lifting weights, for a long time. This may overload the spine, and place the core muscles that maintain the stability of the spine (including the rectus abdominis muscle, abdominal obliques muscle, back muscles muscle and other muscle groups) in a state of tension for a prolonged period. The back muscles in particular are prone to fatigue. Over time, the body develops symptoms of NSCLBP [10, 11]. The development of NSCLBP in nurses may also be related to a biomechanical imbalance [12]. For example, the process of turning a patient or assisting a patient to turn may require excessive and simultaneous bending and turning, subjecting the lumbar spine to shearing forces. A study by Kim et al. [13] found that a continuous shearing force acting on rat L5-6 intervertebral discs for 1 to 2 weeks could induce intervertebral disc degeneration, which in turn leads to NSCLBP. Finally, from a medical point of view, NSCLBP may be caused by the gradual degeneration of joints and soft tissues over time due to repeated microtraumas, resulting from poor control of the spinal structure [14]. Excessive spine activity can also lead to potential spine deformation and nerve tissue compression damage, which can lead to NSCLBP. Biomechanical imbalance is the basis of spinal deformation and nerve tissue compression, and the NSCLBP that occurs after nerve tissue compression is a reflection of the former [15].
Numerous studies have investigated risk factors for NSCLBP in nurses, including physical, mental, and occupational considerations. However, the various studies reached different conclusions regarding risk factors. For example, Zhang et al. [16] found that the age, educational level, and the professional title of nurses had no effect on NSCLBP, whereas Wang et al. [17] found that these factors influenced the development of NSCLBP. Therefore, it is difficult to find a scientific and clinical consensus on the risk factors for NSCLBP among nurses. Smith et al. [18] demonstrated a significant association between increased age and body mass and golf-related NSCLBP in her meta-analysis. A further meta-analysis by Griffith et al. [19] found that posture exposure and force exposure were associated with NSCLBP. However, to our knowledge, no meta-analyses have explored the risk factors that influence NSCLBP in nurses.
In view of this existing research gap, the objective of this study was to perform a meta-analysis of the risk factors for NSCLBP in nurses. Moreover, the study comprehensively and objectively evaluated the relationship between the identified risk factors and NSCLBP in nurses, using big data to provide appropriate evidence-based insights for the prevention and treatment of NSCLBP in nurses.
2.Methods
2.1Search strategy
PubMed, ScienceDirect, Web of Science, Cochrane Library, EMBASE, CINAHL, MEDLINE, WANFANG, VIP Database, China Knowledge Resource Integrated Database, and SinoMed were searched. The retrieval time spanned from the establishment of the databases to March 2020. The search strategy combined medical subject headings (MeSH) and free words with “AND” and “OR” as the two logical operators. Key search terms included (nurse OR nurses OR nursing staff OR clinical nurse OR personnel, nursing OR nursing personnel OR registered nurses OR nurse, registered OR nurses, registered OR registered nurse) AND (low back pain OR lower back pain OR back pain OR non-specific low back pain OR Back Pain, Low OR Low Back Pains OR Lower Back Pains OR Pain, Lower Back OR Pains, Lower Back) AND (factors OR risk factors OR Prevalence). These search terms were used consistently across the different databases. Studies were retrieved by computer and manual retrieval methods, and the search languages were Chinese and English.
Table 1
Methodological quality assessment of the 18 studies
| Item | ⟀ | ⟁ | ⟂ | ⟃ | ⟄ | ⟅ | ⟆ | ⟇ | ⟈ | Score |
|---|---|---|---|---|---|---|---|---|---|---|
| Study | ||||||||||
| Jingwen Sun, 2018 |
|
|
|
|
|
|
|
|
| 8 |
| Xiulan Wang, 2016 |
|
|
|
|
|
|
|
|
| 7 |
| Limei Tang, 2018 |
|
|
|
|
|
|
|
|
| 8 |
| Changjun Liu, 2006 |
|
|
|
|
|
|
|
|
| 7 |
| Hongjing Lin, 2013 |
|
|
|
|
|
|
|
|
| 9 |
| Tianci Wang, 2015 |
|
|
|
|
|
|
|
|
| 9 |
| Jiaqi Zeng, 2020 |
|
|
|
|
|
|
|
|
| 9 |
| Junxiao Wu, 2019 |
|
|
|
|
|
|
|
|
| 9 |
| Mekonnen TH, 2019 |
|
|
|
|
|
|
|
|
| 9 |
| Mohammad Suliman, 2018 |
|
|
|
|
|
|
|
|
| 9 |
| Shwn-Huey Shieh, 2016 |
| ? |
|
|
|
|
|
|
| 8 |
| Mohd Ismail Ibrahim, 2019 |
|
|
|
|
|
|
|
|
| 9 |
| Junpei Yokota, 2019 |
|
|
|
|
|
|
|
|
| 9 |
| Payman Asadi, 2016 |
|
|
|
|
|
|
|
|
| 9 |
| Chuliporn Sopajareeya, 2009 |
|
|
|
|
|
|
|
|
| 7 |
| Moath Bin Homaid, 2016 |
|
| ? |
|
|
|
|
|
| 7 |
| Vera Yin Bing Yip, 2004 |
|
|
|
|
|
|
|
|
| 7 |
| Seyed Ehsan Samaei, 2017 |
|
|
|
| ? |
|
|
|
| 8 |
Note: (“
2.2Inclusion and exclusion criteria
Inclusion criteria: (1) subjects were registered nurses; (2) the literature reported the diagnostic criteria for NSCLBP (NSCLBP is characterized by muscle stiffness, tension, or pain localized between the gluteal folds and the costal margin, the pain is not caused by infection, trauma, or any other specific reasons, and with the course of the disease lasting more than 12 weeks); (3) samples of nursing staff and cases of NSCLBP were reported in the literature; (4) primary research reported the prevalence of NSCLBP among nurses working at different healthcare facilities using a 12-month recall period; and (5) the literature was published in peer-reviewed journals. Exclusion criteria: (1) unavailability of abstracts, full-text articles, and data; (2) incomplete, unclear, or incorrect information; and (3) duplicated evidence. The literature was independently screened by two trained researchers according to the inclusion and exclusion criteria. The extracted information included clinical information and the following data from the original literature: first author, year of publication, country, research type, research objective, and sample size. In case of disputes regarding the data, an agreement was reached through third-party discussion.
2.3Quality evaluation
The predominant type of research included in this analysis was the status survey. Quality assessment of status surveys was conducted according to the Joanna Briggs Institute evidence-based healthcare center in Australia (Table 1) [20]. In this assessment, nine items were scored, with a maximum score of 9 points awarded. If the evaluation result was YES, the score was 1; otherwise, the score was 0. Scores of 0–3, 4–6, and 7–9 were classified as low, medium, and high quality, respectively. The risk of cross-sectional research bias (Joanna Briggs Institute) was used to evaluate publication bias in the included literature. Following independent evaluation, the two researchers discussed the results and reached a consensus. In case of disagreement, a third researcher participated in the discussion.
2.4Statistical analysis
Odds ratios (OR) were used as effect indicators for counting data. Mean differences or standardized mean differences and 95% confidence intervals (CIs) were used as the effect indices of the data. The statistical software Review Manager 5.3 (Cochrane collaboration, Oxford, UK) was used in the meta-analysis to analyze the heterogeneity of the different studies.
Table 2
Basic information used for the sample plots
| Author | Year | Sample size | Prevalence of NSCLBP (%) | Mean age | Gender frequency (%) | Region | Tool | Factor | Publication bias | |
|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | |||||||||
| Jingwen Sun | 2018 | 1854 | 70.3 | 32.2 | 77 (4.1) | 1777 (95.8) | China | SRQ, NMQ | ⟀ ⟂ ⟃ ⟄ ⟅ ⟆ | Low |
| Xiulan Wang et al. | 2016 | 909 | 92.4 | 31.93 | – | China | SRQ | ⟁ ⟄ ⟅ | Low | |
| Limei Tang et al. | 2018 | 1279 | 91.01 | – | 80 (6.2) | 1199 (93.8) | China | SRQ, VAS | ⟀ ⟁ ⟂ ⟃ ⟆ | Low |
| Changjun Liu et al. | 2006 | 486 | 60.3 | 33.4 | 0 (0) | 486 (100) | China | SRQ | ⟇ ⟈ | Low |
| Hongjing Lin | 2013 | 344 | 54.65 | 29.47 | – | China | SRQ, RMDQ, ODI | ⟀ ⟁ ⟆ | Low | |
| Tianci Wang et al. | 2015 | 474 | 66.7 | 33.64 | 0 (0) | 474 (100) | China | SRQ, NRS | ⟀ ⟁ ⟆ | Low |
| Jiaqi Zeng et al. | 2020 | 627 | 79.6 | 28.93 | 38 (6.1) | 589 (93.9) | China | SRQ | ⟁ ⟄ ⟅ ⟇ | Low |
| Junxiao Wu et al. | 2019 | 648 | 63.0 | 31.0 | – | China | SRQ, VAS | ⟁ ⟈ | Low | |
| Tesfaye Hambisa Mekonnen et al. | 2019 | 422 | 63.6 | 31.39 | 189 (44.8) | 233 (55.2) | Ethiopia | SRQ, NMQ | ⟄ ⟅ ⟆ ⟇ | Low |
| Mohammad Suliman | 2018 | 384 | 69.0 | 32.59 | 127 (33.1) | 257 (66.9) | Jordan | SRQ, NRS | ⟂ ⟃ ⟄ | Low |
| Shwn-Huey Shieh et al. | 2016 | 788 | 72 | – | – | Taiwan | SRQ | ⟀ ⟁ ⟅ ⟆ ⟈ | Low | |
| Mohd Ismail Ibrahim et al. | 2019 | 1292 | 76.5 | – | 49 (3.8) | 1243 (96.2) | Malaysia | SRQ | ⟀ ⟁ ⟂ ⟃ ⟄ ⟅ ⟆ ⟇ | Low |
| Junpei Yokota et al. | 2019 | 1100 | 64.6 | 33.0 | 412 (37.5) | 688 (62.5) | Japan | SRQ, NRS | ⟁ ⟂ | Low |
| Payman Asadi et al. | 2016 | 350 | 70.3 | 32 | 34 (9.7) | 316 (90.3) | Iran | SRQ | ⟀ ⟁ ⟃ ⟆ ⟈ | Low |
| Chuliporn Sopajareeyaet al. | 2009 | 265 | 61.5 | 39.5 | 9 (3.4) | 256 (96.6) | Thailand | SRQ, NMQ | ⟀ ⟂ ⟃ ⟈ | Low |
| Moath Bin Homaid et al. | 2016 | 120 | 74.2 | 33.9 | 31 (25.8) | 89 (74.2) | Saudi Arabia | SRQ | ⟁ ⟂ ⟃ ⟅ ⟆ | Low |
| Vera Yin Bing Yip et al. | 2004 | 144 | 83.3 | 31.1 | 21 (14.6) | 123 (85.4) | Hong Kong | SRQ | ⟁ ⟂ ⟆ | Low |
| Seyed Ehsan Samaei et al. | 2017 | 243 | 69.5 | 33.6 | 30 (12.3) | 213 (87.7) | Iran | SRQ | ⟂ ⟃ | Low |
Note: ⟀ age; ⟁ years working as a nurse; ⟂ gender; ⟃ body mass index; ⟄ shift night work; ⟅ education background; ⟆ marital status; ⟇ job satisfaction; ⟈ physical exercise; SRQ: self-reported questionnaire; NMQ: Nordic Musculoskeletal questionnaire; VAS: Visual Analogue Scale; RMDQ: Roland-morris Disability Questionnaire; ODI: Oswestry Disablity Index; NRS: numerical rating scale; –: Not reported.
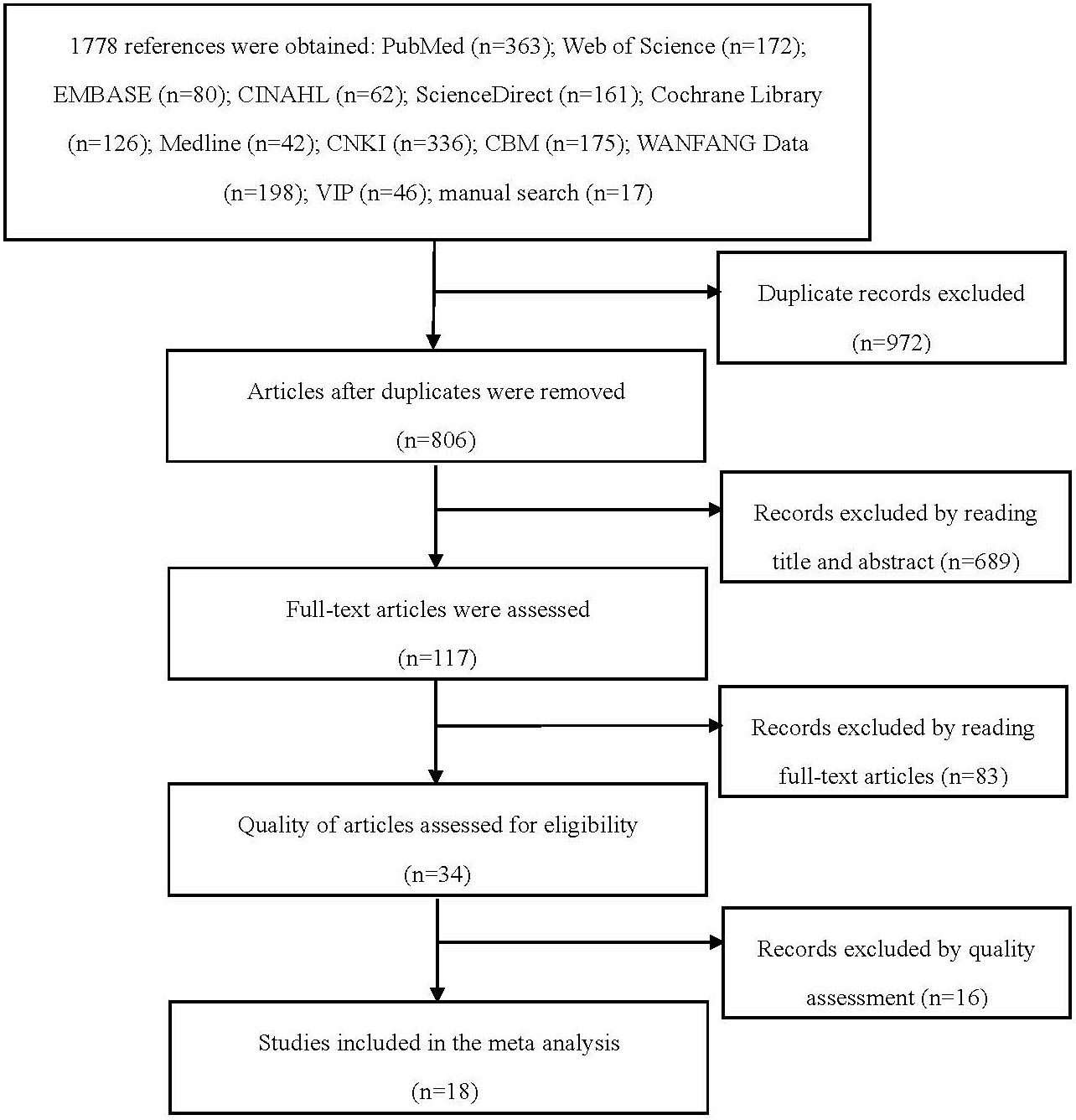
Figure 1.
Literature selection process and results.
corresponding 95% CI were calculated. Sensitivity analysis was used to evaluate the stability of the meta-analysis result, and the root of heterogeneity was evaluated by removing studies one by one, with changes in heterogeneity and combined effect size observed at the same time. If the heterogeneity changed after excluding a study, or the results changed, then that study was considered the possible source of the heterogeneity. In this case, the source of heterogeneity was further analyzed, in terms of experimental design, sample size, and evaluation criteria. If the results were not affected after exclusion a study, the results were considered relatively stable.
Figure 2.
Forest plot of the effect of gender on NSCLBP in nurses.
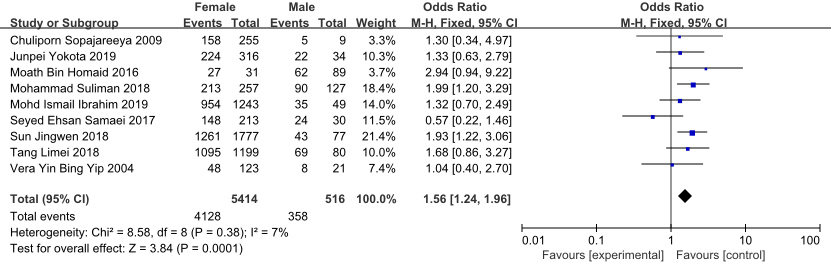
Figure 3.
Forest plot of the effect of BMI on NSCLBP in nurses.
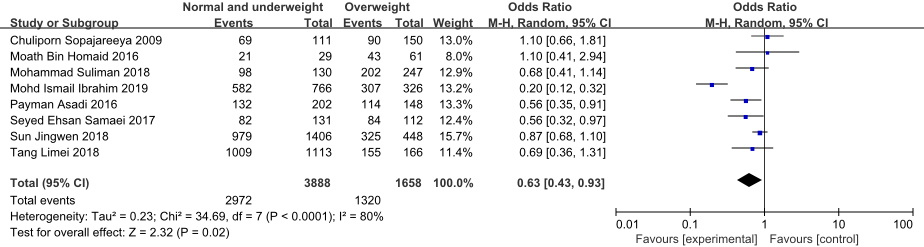
Figure 4.
Forest plot of the effect of education background on NSCLBP in nurses.
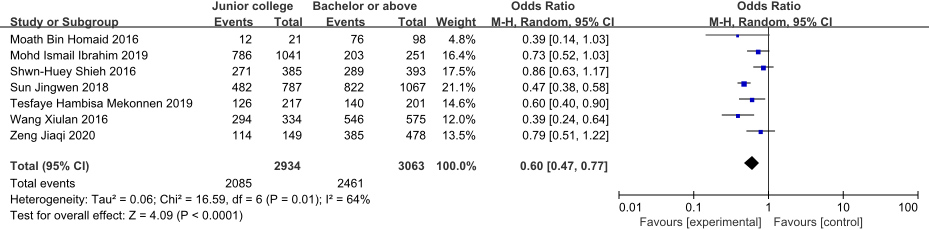
Figure 5.
Forest plot of the effect of marital status on NSCLBP in nurses.
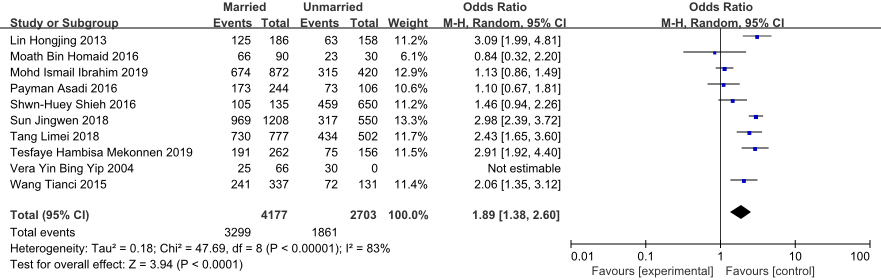
Figure 6.
Forest plot of the effect of shift night work on NSCLBP in nurses.
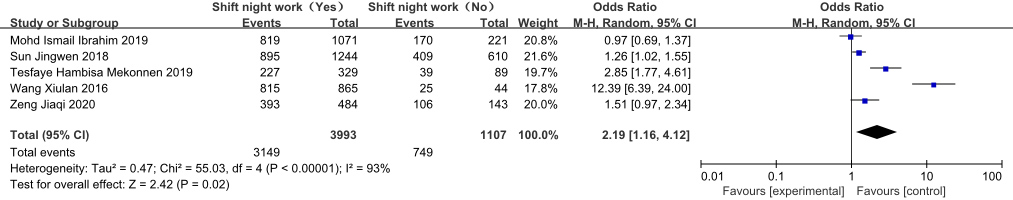
Figure 7.
Forest plot of the effect of job satisfaction on low back pain in nurses.
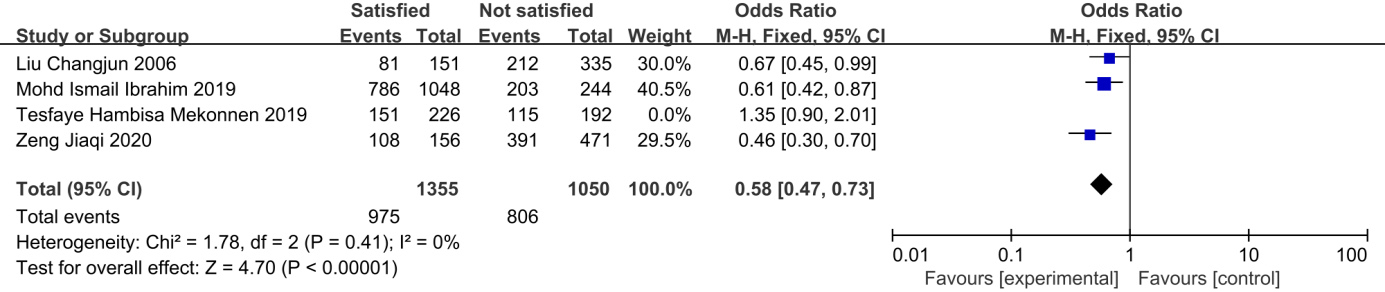
Figure 8.
Forest plot of the effect of years working as a nurse on NSCLBP in nurses.
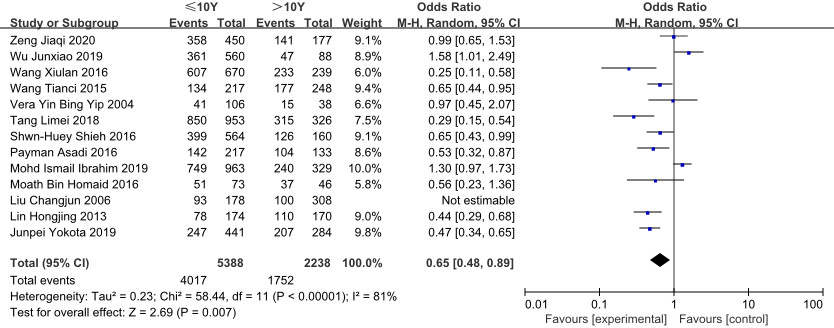
Figure 9.
Forest plot of the effect of age on low back pain in nurses.

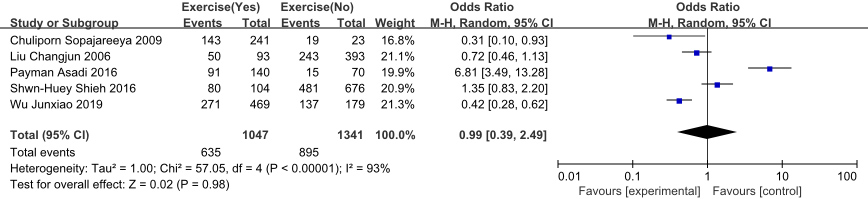
Figure 10.
Forest plot of the effect of physical exercise on NSCLBP in nurses.
3.Results
3.1Characteristics of included studies and publication bias
Following the search and selection procedure described, 18 articles were included, involving a total of 11,752 nursing staff (Fig. 1). The research designs of all included studies are cross-sectional studies. The characteristics of the included studies are summarized in Table 2.
3.2The results of the quality evaluation
Results of the Joanna Briggs Institute evidence-based assessment of the quality of the literature are summarized in Table 1. Five articles scored 7 points [17, 21, 22, 23, 24], four articles scored 8 points [25, 26, 27, 28], and nine articles scored 9 points [29, 30, 31, 32, 33, 34, 35, 36, 37]. Hence, all the included studies were regarded to be of sufficient quality to be included in the meta-analysis.
3.3The results of the meta-analysis
This meta-analysis showed that being female (pooled estimate of 1.56, 95% CI 1.24–1.96, I
Although the heterogeneity of the selected factors was greater than 50%, the sensitivity analysis revealed clear heterogeneity on the impact of job satisfaction on NSCLBP, arising from the study of Tesfaye et al. [33]. This may be because job satisfaction in this study was evaluated in the form of a scale, while other publications used subjective evaluation methods. After excluding this publication, it was found that no single study affected the results. Further sensitivity analyses found that no single study affected the results of the remaining factors assessed, suggesting that the results are stable.
4.Discussion
NSCLBP develops in nurses due to numerous causes, through the interaction of work, lifestyle, and environmental factors. NSCLBP leads to many nurses leaving their jobs, with a high disability rate, and has low rates of diagnosis and treatment in nurses [38]. NSCLBP greatly affects the health of nurses, and brings a heavy burden for their families and the wider society. Therefore, fully understanding the risk factors for NSCLBP in nurses is of crucial importance for the effective prevention of this condition.
This study of the demographic characteristics of nursing staff with and without NSCLBP groups revealed that nurses with NSCLBP tended to be overweight (
The findings suggest that nurses should be vigilant and protect themselves as much as possible by maintaining a reasonable posture at work and in everyday life, and allowing rest time after working to relieve muscle fatigue. Eating a balanced diet and maintaining a healthy weight are important to decrease the risk of NSCLBP. In addition, managers should pay particular attention to female and married nurses. Nurses with families should be offered flexible work-family arrangements to decrease the pressure and the risk of NSCLBP.
The analysis of the occupational characteristics among nursing staff with and without NSCLBP revealed that nurses with NSCLBP tended to be night shift workers (
Nurses with more than 10 years of work experience had a 0.65-fold higher risk of low back pain compared with those with
It is suggested that in clinical work, scientific nursing teams should be equipped according to the specific work intensity. Moreover, nursing managers should make reasonable scheduling adjustments, and limit the total number of night shifts to no more than three times per week to avoid the occurrence of NSCLBP due to the high frequency of night shifts [50]. Relevant managers should equip nurses with the necessary auxiliary facilities and equipment, especially in the intensive care unit (ICU), emergency department and operating room nurses, to reduce the physical demands. At the same time, we also recommend further research on the factors that lead to low job satisfaction, and how these factors affect nurses.
The OR value for age or physical exercise in this study was not statistically significant. There are two possible reasons for this. First, there is a considerable imbalance between the number of nurses aged over and under 40 years included in this analysis; second, most of the original literature divided ages into four stages: 20–29, 30–39, 40–49, and
There are several limitations to this study. Only two languages, Chinese and English, were searched, and other languages were not included. Also, due to the different factors investigated in the included literature, a limited analysis of each factor only was possible. Finally, although the OR values were combined with the random-effect model, false negative results may also be obtained.
5.Conclusion
Current evidence shows that being female, married, working night shifts, and being dissatisfied with work are risk factors for NSCLBP in nurses. Current evidence is not clear on the effect of age or physical exercise. High-quality prospective studies are needed to validate the findings of this study. This study provides a scientific basis for nursing managers and nurses to protect against NSCLBP. Based on these results, any interventional program for preventing or reducing NSCLBP among nursing staff should focus on improving the shift system, increasing the nurse-to-bed ratio in hospitals, particularly on the night shift, and providing flexible work-family arrangements for married females.
Acknowledgments
The authors thank Mr. Jiang JianZhong, the director of the library of The Second Hospital of Hebei Medical University, for his guidance regarding literature retrieval.
Conflict of interest
There are no conflicts of interest in the submission of this manuscript, and the manuscript has been read and approved by all authors for publication.
References
[1] | Association EGOS. Consensus of Chinese experts in the diagnosis and treatment of acute/chronic nonspecific low back pain. Chinese J Spine Spinal Cord. (2016) ; 26: (12): 1134–1138. doi: 10.3969/j.issn.1004-406X.2016.12.16. |
[2] | Alemayehu T, Worku A, Assefa N. Sharp injury and exposure to blood and body fluids among health care workers in health care centers of Eastern Ethiopia. Int J Occup Environ Med. (2016) ; 7: (3): 172–180. doi: 10.15171/ijoem.2016.714. |
[3] | Serranheira F, Smith D. Work-related musculoskeletal disorders in nursing: current knowledge and ongoing challenges for occupational health. Med Lav. (2014) ; 105: (5): 395–397. |
[4] | Soroush A, Shamsi M, Izadi N, Heydarpour B, Samadzadeh S, Shahmohammadi A. Musculoskeletal disorders as common problems among Iranian nurses: a systematic review and meta-analysis study. Int J Prev Med. (2018) ; 9: : 27. doi: 10.4103/ijpvm.IJPVM_235_16. |
[5] | Jin Y, Jia M, Xu F. Prevalence of low back pain in Chinese nurses a meta-analysis. Chinese Journal of Practical Nursing. (2013) ; 29: (20): 45–47. doi: 10.3760/cma.j.issn.1672-7088.2013.2013.20.016. |
[6] | Azizpour Y, Delpisheh A, Montazeri Z, Sayehmiri K. Prevalence of low back pain in Iranian nurses: a systematic review and meta-analysis. BMC Nurs. (2017) ; 16: : 50. doi: 10.1186/s12912-017-0243-1. |
[7] | Tian SZ, Tang LM, Yin LS. Influencing factors and protection of occupational low back pain in nurses. Chinese J Nurs. (2012) ; 47: (9): 856–858. doi: 10.3761/j.issn.0254-1769.2012.09.035. |
[8] | Wu Y, Zheng J, Liu K, Baggs JG, Liu J, Liu X, et al. The associations of occupational hazards and injuries with work environments and overtime for nurses in China. Res Nurs Health. (2018) . doi: 10.1002/nur.21882. |
[9] | Nourollahi M, Afshari D, Dianat I. Awkward trunk postures and their relationship with low back pain in hospital nurses. Work. (2018) ; 59: (3): 317–323. doi: 10.3233/WOR-182683. |
[10] | Barr KP, Griggs M, Cadby T. Lumbar stabilization: a review of core concepts and current literature, part 2. Am J Phys Med Rehabil. (2007) ; 86: (1): 72–80. doi: 10.1097/01.phm.0000250566.44629.a0. |
[11] | Barr KP, Griggs M, Cadby T. Lumbar stabilization: core concepts and current literature, part 1. Am J Phys Med Rehabil. (2005) ; 84: (6): 473–480. doi: 10.1097/01.phm.0000163709.70471.42. |
[12] | Young LJ, Lin OY, Chen DW, Lin Q. A biomechanical analysis of low back pain. Chinese J Tissue Eng Res. (2020) ; 24: (33): 5267–5271. doi: 10.3969/j.issn.2095-4344.2848. |
[13] | Kim J, Yang SJ, Kim H, Kim Y, Park JB, Dubose C, et al. Effect of shear force on intervertebral disc (IVD) degeneration: an in vivo rat study. Ann Biomed Eng. (2012) ; 40: (9): 1996–2004. doi: 10.1007/s10439-012-0570-z. |
[14] | Gold JE, Punnett L, Cherniack M, Wegman DH. Digital vibration threshold testing and ergonomic stressors in automobile manufacturing workers: a cross-sectional assessment. Ergonomics. (2005) ; 48: (1): 66–77. doi: 10.1080/00140130412331311408. |
[15] | Fournely M, Petit Y, Wagnac E, Evin M, Arnoux PJ. Effect of experimental, morphological and mechanical factors on the murine spinal cord subjected to transverse contusion: a finite element study. PLoS One. (2020) ; 15: (5): e232975. doi: 10.1371/journal.pone.0232975. |
[16] | Zhang L, Quan Y, Zhao M. Investigation of clinical nurses’ low back pain and analysis of influencing factors. Chinese Gen Pract Nurs. (2017) ; 15: (19): 2311–2313. doi: 10.3969/j.issn.1674-4748.2017.19.003. |
[17] | Wang XL, Ren JQ, Liu J. The status and influencing factors of low back pain of 909 nurses in three tertiary grade A hospitals. Chinese Nurs Manag. (2016) ; 16: (1): 61–64. doi: 10.3969/j.issn.1672-1756.2016.01.17. |
[18] | Smith JA, Hawkins A, Grant-Beuttler M, Beuttler R, Lee SP. Risk factors associated with low back pain in golfers: a systematic review and meta-analysis. Sports Health. (2018) ; 10: (6): 538–546. doi: 10.1177/1941738118795425. |
[19] | Griffith LE, Shannon HS, Wells RP, Walter SD, Cole DC, Côté P, et al. Individual participant data meta-analysis of mechanical workplace risk factors and low back pain. Am J Public Health. (2012) ; 102: (2): 309–318. doi: 10.2105/AJPH.2011.300343. |
[20] | Zhou Y, Gu Y, Hu Y, Xing W. The Joanna Briggs institute critical appraisal tools for use in systematic review: prevalence study and analytical cross-sectional study. J Nurs Training. (2018) ; 33: (3): 219–221. doi: 10.16821/j.cnki.hsjx.2018.03.007. |
[21] | Liu C, Lan Y, Wang M, Wang Z, Zhou D. A survey on low back pain and its influential factors among nurses. China Occupational Medicine. (2006) ; 193–195. |
[22] | Sopajareeya C, Viwatwongkasem C, Lapvongwatana P, Hong O, Kalampakorn S. Prevalence and risk factors of low back pain among nurses in a thai public hospital. J Med Assoc Thai. (2009) ; 92: (Suppl 7): S93–9. |
[23] | Yip VYB. New low back pain in nurses: work activities, work stress and sedentary lifestyle. J Adv Nurs. (2004) ; 46: (4): 430–40. doi: 10.1111/j.1365-2648.2004.03009.x. |
[24] | Bin Homaid M, Abdelmoety D, Alshareef W, Alghamdi A, Alhozali F, Alfahmi N, et al. Prevalence and risk factors of low back pain among operation room staff at a Tertiary Care Center, Makkah, Saudi Arabia: a cross-sectional study. Ann Occup Environ Med. (2016) ; 28: : 1. doi: 10.1186/s40557-016-0089-0. |
[25] | Tang L, Ning W, Sun H, Zhang Z, Tian S. Multi-center survey and analysis of influencing factors of clinical nurses’ occupational low back pain. Chinese J Modern Nurs. (2018) ; 24: (27): 3292–3295. doi: 10.3760/cma.j.issn.1674-2907.2018.27.017. |
[26] | Sun J. The prevalence and relative factors of occupational low back pain among nurses in Zibo City. Master degree [dissertation]. Qingdao (MI): Shan Dong University; (2018) . |
[27] | Samaei SE, Mostafaee M, Jafarpoor H, Hosseinabadi MB. Effects of patient-handling and individual factors on the prevalence of low back pain among nursing personnel. Work. (2017) ; 56: (4): 551–561. doi: 10.3233/WOR-172526. |
[28] | Shieh SH, Sung FC, Su CH, Tsai Y, Hsieh VC. Increased low back pain risk in nurses with high workload for patient care: a questionnaire survey. Taiwan J Obstet Gynecol. (2016) ; 55: (4): 525–529. doi: 10.1016/j.tjog.2016.06.013. |
[29] | Wu JX. Occupational risk factors of low back pain in nurses. China Occup Med. (2019) ; 46: (2): 194–197. doi: 10.11763/j.issn.2095-2619.2019.02.011. |
[30] | Wang T, Liu Y, Li Q, Guan G, Xu M. The investigation and analysis of the status of nursing staff’s occupational low back pain and related risk factors. Chinese Gen Pract Nurs. (2015) ; 13: (26): 2651–2653. doi: 10.3969/j.issn.1674-4748.2015.26.046. |
[31] | Zeng J, Yuan Q, Tian L, Wang L, Gui H, Li Y, et al. Occupational low back pain in nurses: the influencing factors. J Nurs Sci. (2020) ; 35: (3): 60–63. doi: 10.3870/j.issn.1001-4152.2020.03.060. |
[32] | Lin H. The investigation and analysis of professional low back pain in clinical nursing staff. Master degree [dissertation]. Changchun (MI): Jilin University; (2013) . |
[33] | Mekonnen TH. Work-related factors associated with low back pain among nurse professionals in East and West Wollega Zones, Western Ethiopia, 2017: a cross-sectional study. Pain Ther. (2019) ; 8: (2): 239–247. doi: 10.1007/s40122-019-0129-x. |
[34] | Suliman M. Prevalence of low back pain and associated factors among nurses in Jordan. Nurs Forum. (2018) ; 53: (4): 425–431. doi: 10.1111/nuf.12269. |
[35] | Yokota J, Fukutani N, Nin K, et al. Association of low back pain with presenteeism in hospital nursing staff. J Occup Health. (2019) ; 61: (3): 219–226. doi: 10.1002/1348-9585.12030. |
[36] | Asadi P, Monsef Kasmaei V, Zia Ziabari SM, Zohrevandi B. The prevalence of low back pain among nurses working in Poursina hospital in Rasht, Iran. J Emergency Pract Trauma. (2016) ; 2: (1): 11–15. doi: 10.15171/jept.2015.01. |
[37] | Ibrahim MI, Zubair IU, Yaacob NM, Ahmad MI, Shafei MN. Low back pain and its associated factors among nurses in public hospitals of Penang, Malaysia. Int J Environ Res Public Health. (2019) ; 16: (21). doi: 10.3390/ijerph16214254. |
[38] | Chen L, Guo H, Meng L. Study for the influencing factors and preventive measures of occupational low back pain in nurses. Journal of Nurses Training. (2017) ; 32: (12): 1082–1085. doi: 10.16821/j.cnki.hsjx.2017.12.008. |
[39] | Kalichman L, Li L, Kim DH, Guermazi A, Berkin V, O’Donnell CJ. Facet joint osteoarthritis and low back pain in the community-based population. Spine. (2008) ; 33: (23): 2560–2565. doi: 10.1097/BRS.0b013e318184ef95. |
[40] | Trinkoff AM, Le R, Geiger-Brown J, Lipscomb J, Lang G. Longitudinal relationship of work hours, mandatory overtime, and on-call to musculoskeletal problems in nurses. Am J Ind. Med. (2006) ; 49: (11): 964–971. doi: 10.1002/ajim.20330. |
[41] | Awosoga O, Steinke C, Nord C, Doan J, Varsanyi S, Meadows J, et al. Exploring the role of shift work in the self-reported health and wellbeing of long-term and assisted-living professional caregivers in Alberta, Canada. Hum Resour Health. (2020) ; 18: (1): 70. doi: 10.1186/s12960-020-00515-6. |
[42] | Hernlund E, Svedbom A, Iverg Rd M, Compston J, Cooper C, Stenmark J. Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos. (2013) ; 8: : 136. doi: 10.1007/s11657-013-0136-1. |
[43] | Maria S, Witt-Enderby PA. Melatonin effects on bone: potential use for the prevention and treatment for osteopenia, osteoporosis, and periodontal disease and for use in bone-grafting procedures. J Pineal Res. (2014) ; 56: (2): 115–125. doi: 10.1111/jpi.12116. |
[44] | Jradi H, Alanazi H, Mohammad Y. Psychosocial and occupational factors associated with low back pain among nurses in Saudi Arabia. J Occup Health. (2020) ; 62: (1): e12126. doi: 10.1002/1348-9585.12126. |
[45] | Alexopoulos EC, Burdorf A, Kalokerinou A. A comparative analysis on musculoskeletal disorders between Greek and Dutch nursing personnel. Int Arch Occup Environ Health. (2006) ; 79: (1): 82–88. doi: 10.1007/s00420-005-0033-z. |
[46] | Thiese MS, Lu M, Merryweather A, Tang R, Ferguson SA, Malloy EJ, et al. Psychosocial factors and low back pain outcomes in a pooled analysis of low back pain studies. J Occup Environ Med. (2020) ; 62: (10): 810–815. doi: 10.1097/JOM.0000000000001941. |
[47] | Eriksen W, Bruusgaard D, Knardahl S. Work factors as predictors of intense or disabling low back pain; a prospective study of nurses’ aides. Occup Environ Med. (2004) ; 61: (5): 398–404. doi: 10.1136/oem.2003.008482. |
[48] | Freimann T, P Suke M, Merisalu E. Work-Related psychosocial factors and mental health problems associated with musculoskeletal pain in nurses: a cross-sectional study. Pain Res Manag. (2016) ; (2016). doi: 10.1155/2016/9361016. |
[49] | Bazazan A, Dianat I, Bahrampour S, et al. Association of musculoskeletal disorders and workload with work schedule and job satisfaction among emergency nurses. Int Emerg Nurs. (2019) ; 44: (5): 8–13. doi: 10.1016/j.ienj.2019.02.004. |
[50] | Wu M, Cao W. Association between shift work and musculoskeletal symptoms among nursing personnel in Zhejiang. Zhejiang Medical Education. (2015) ; 14: (4): 25–28. |




