Improving physical health monitoring and interventions in a learning disabilities forensic psychiatric secure service
Abstract
BACKGROUND:
Patients in psychiatric inpatient settings are at increased risk of developing physical health complications due to the structure of inpatient wards, the metabolic side-effects of antipsychotic medications and socioeconomic factors. Robust physical health monitoring and interventions are paramount in reducing this health inequality.
OBJECTIVE:
To improve the quality of physical health interventions in the ward environment and empower patients to follow healthy lifestyle guidance to reduce their risk of metabolic syndrome.
METHODS:
Patient weight and waist circumference data were collected at baseline and weekly throughout the 8-week intervention period. A questionnaire was recorded from baseline to week-5 to assess patient understanding. Two Plan-Do-Study-Act (PDSA) cycles were completed: (1) Series of weekly psychoeducation sessions and group exercise and (2) Implementation of healthy living diaries.
RESULTS:
Our data did not demonstrate any definitive impact upon the waist circumference and weight of participants. However, analysis of the questionnaires showed a consistent trend in knowledge improvement.
CONCLUSION:
Whilst our aim of reducing patient weight and waist circumference was not realised, there was a significant impact on participant’s knowledge, demonstrating a subjective benefit of our interventions. Our project also highlighted inconsistencies in physical health measurements and data collection, providing vital information for further quality improvement measures.
1.Background
The increasing physical health needs of psychiatric in-patient populations are of growing concern [1]. This is particularly important because socio-economic backgrounds, psychiatric medications as well as diet and lifestyle on the ward, can predispose patients to weight gain, insulin resistance and ultimately cardiovascular disease [2]. This is seen in the alarming statistic that psychiatric patients have a higher mortality rate and lower life expectancy than non-psychiatric patients [3]. This quality improvement project aimed to address these needs through patient education and engagement on the benefits of healthy lifestyles. Through this programme, we aimed to see a decrease in patient weight and waist circumference in order to reduce the risk factors for developing metabolic syndromes such as diabetes mellitus [4]. Seeing as long-standing diabetes can have numerous detrimental effects on the body, by intervening at an earlier stage, we hoped to preserve and improve patient physical health and mitigate their need for additional anti-glycaemic medication [5]. We also hoped these effects would be far-reaching and go beyond the patients’ in-patient admissions, equipping them with the knowledge and resources to make informed decisions about their health in the community.
2.Objective
This project aimed to improve physical health initiatives on the selected forensic inpatient wards through a patient education programme. We used weight and waist circumference measurements to monitor the patients’ physical response to the program. It was predicted that during the 8-week intervention period (October 2019–December 2019), 60% of inpatients in the three selected learning disability forensic inpatient wards at risk of developing type 2 diabetes, or with a current diagnosis of type 2 diabetes, would have experienced a reduction in weight and waist circumference.
3.Methods
We recruited patients from Kent and Medway Forensic learning disability wards. All included patients underwent two rounds of interventions which aimed to encourage weight loss through improved knowledge of healthy eating and exercise.
The first Plan-Do-Study-Act (PDSA) cycle, conducted through weeks one to four, consisted of weekly small group teaching sessions on healthy diet and exercise, of which the last session included a particular emphasis on diabetes. Each session focused on a specific aspect of healthy eating and included a 15-min practical exercise at the end designed to teach the participant some physical exercises. Prior to commencing the interventions, we held meetings with the ward staff and patients to detail the goals, structure and topics of each session.
For the second PDSA cycle, we made a food and exercise diary that was to be completed for the remaining four weeks by both the patients and the staff and was intended to help consolidate and apply their knowledge from the first four weeks. We created two diaries for each participant; one was to be completed by the ward staff with details of healthy behaviour changes adopted and suggested improvements. The other diary was to be completed by each patient and was formatted to be easy to complete with icons and small phrases for healthy choices made during each week.
We collected baseline data on each participant before commencing our two rounds of interventions. This information was collected by the ward staff weekly and was recorded on the electronic patient records as standard. Data extracted included weight and waist circumference for each participant. We then extracted this data each week for the remaining weeks of the project. During the first PDSA cycle, we also collected questionnaire data on subjective knowledge of ideal nutrition and exercise as well as diabetes after each session. To increase uptake in our patients, all of whom had a learning disability diagnosis, we formatted the questionnaire into an easy read format and based it on a visual Likert scale [6], with emotive face icons representing each score on the scale of one to five. The completed questionnaires were compiled at the end of the project and the available data recorded.
4.Results
The goal of 60% of patients showing a weight reduction was achieved at week 1, week 3 and week 5. The goal was only met once for WC at week 7 (Fig. 1). It is important to view the results alongside the considerable amount of missing data and measurement errors we found upon data collection due to the inconsistency in the method and frequency at which staff took measurements. Though there was a high decrease in overall weight loss at week 1 (85.71%), only 7/18 patients had enough data to be analysed at week 1.
Fig. 1.
Two run charts showing the overall percentage of participating patients with some loss in their (a) weight and (b) waist circumference each week. Median value = 50%. Goal = 60%.
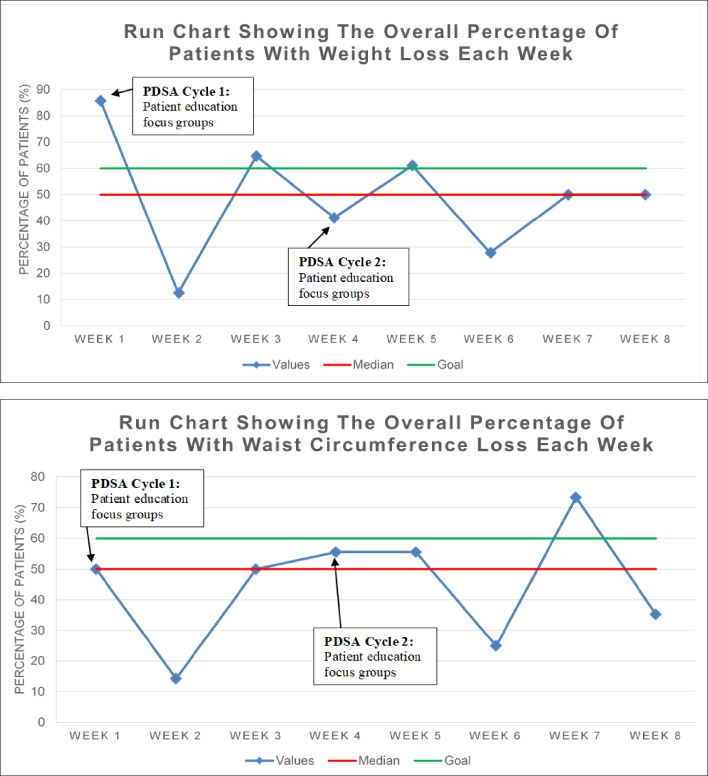
6/18 patients had weight loss and 12/18 patients had reduced WC from their baseline measurement to final measurement at week 8. Much of this reduction was insignificant. One patient had a 14.04% WC decrease but stark jumps in their weekly WC recordings inconsistent with reasonable fluctuations make this an anomalous result. Some patients did not have a baseline recording prior to the start of the project and therefore their first available measurement was used as the baseline. For example, for most patients on Brookfield Centre, their weight and WC measurements began at week 2 and 3, respectively.
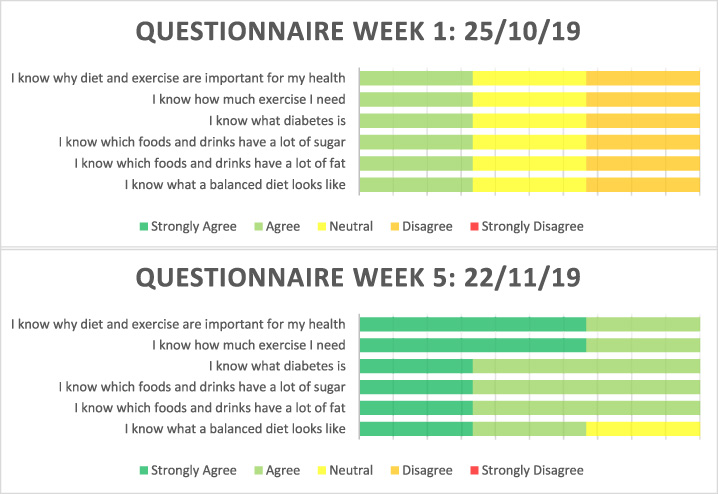
Unfortunately, only three patients on Riverhill ward completed the questionnaire for more than 2 weeks thus only their responses could be considered. It is evident that the psychoeducation sessions aided in improving their knowledge from week 1 to week 5 of the project, particularly in knowing why diet and exercise are important and how much exercise they need (Fig. 2).
Fig. 2.
Charts comparing the knowledge check questionnaire responses from week 1 to week 5 by the three patients on Riverhill ward.
5.Conclusion
Whilst there was no significant quantitative reduction in parameters of metabolic health from this project, the collection of this data enabled many alternative improvements in the quality of physical health interventions within the service.
Firstly, discussions of our intervention and results with staff demonstrated that there is significant work still to be done on ensuring optimal physical health assessment and treatment in psychiatric settings. Secondly, the impact of the education session intervention on patient levels of understanding indicates education sessions are a valuable resource for improving physical health and is a potential avenue for future research and development. Future studies should include longitudinal follow up to examine this hypothesis as due to the short-term nature of our project the true effect of our interventions could be misevaluated. Further reflection on this outcome enabled us to acknowledge the value of qualitative data in quality improvement and how strict quantitative aims can distract us from important alternative lessons and outcomes being obtained through the process, this is an area quality improvement projects must explore to ensure we are providing the best care [7].
Gaining learning from the process of QI, rather than just the outcomes, was additionally important in identifying areas that required improvement that had not previously been identified by internal actors. A key example of this was in demonstrating the inaccuracies in the recording and measuring of physical health indicators and providing suggestions into how a future QI project could target this. To avoid discrepancies in the future, it was recommended that WC can be measured at the umbilical level as it is a validated site and provides ease for staff [8,9].
Whilst being able to distance ourselves was a benefit of being an external influence, this also presented challenges during our project. Feedback from staff members highlighted that as external members our understanding of ward structures and team dynamics were limited and our interventions could have improved with greater involvement of regular staff members. Quality improvement teams must look into how to optimise a mixture of internal and external actors to ensure efficient and effective projects.
Many techniques must be utilised to improve physical health in psychiatric settings, however having these independent and separate projects can cause significant burden on staff and a lack of consistency in implementation. Therefore, future work must look into how to streamline the multitude of QI interventions to provide successful, sustainable and replicable interventions to improve physical health in psychiatric inpatient services. To reach the required change, ambitious thinking and the restructuring of services will need to be explored, whilst this will require sustained work and effort, it is essential to providing equality in health outcomes.
Acknowledgements
The authors thank Dr Emmanuella Akande and Kent Low Secure Forensic Service.
Conflict of interest
None to report.
References
[1] | Irene C, Martin D, Ferriter M. Improving the physical health of long-stay psychiatric in-patients. Advances in Psychiatric Treatment. (2004) ;10.2: :107–15. |
[2] | Hjorth P, Davidsen AS, Kilian R, Eriksen SP, Jensen SO, Sørensen HØ Improving the physical health of long-term psychiatric inpatients. Australian & New Zealand Journal of Psychiatry. (2014) ;48: (9):861–70. |
[3] | Hert MD, Correll CU, Bobes J, Cetkovich-Bakmas M, Cohen D, Asai I Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry. (2011) ;10: (1):52–77. |
[4] | Rothberg AE, McEwen LN, Kraftson AT, Ajluni N, Fowler CE, Nay CK Impact of weight loss on waist circumference and the components of the metabolic syndrome. BMJ Open Diabetes Research and Care. (2017) ;5: (1):1. |
[5] | Llorente MD, Victoria U. Diabetes, psychiatric disorders, and the metabolic effects of antipsychotic medications. Clinical Diabetes. (2006) ;24.1: :18–24. |
[6] | Robinson J , Likert Scale. In: Michalos AC (ed), Encyclopedia of Quality of Life and Well-Being Research. Dordrecht: Springer; 2014. |
[7] | Berenholtz SM, Needham DM, Lubomski LH, Goeschel CA, Pronovost PJ. Improving the quality of quality improvement projects. Jt Comm J Qual Patient Saf. (2010) ;36: (10):468–73. |
[8] | Lemoncito MV, Paz-Pacheco E, Lim-Abrahan MA, Jasul Jr G, Isip-Tan IT, Sison CM. Impact of waist circumference measurement variation on the diagnosis of metabolic syndrome. Risk. (2010) ;8: :9–12. |
[9] | Shi W, Neubeck A, Gallagher R. Measurement matters: A systematic review of waist measurement sites for determining central adiposity. Collegian. (2017) ;24: (5):513–23. |




