Improving the quality of inpatient discharge summaries
Abstract
BACKGROUND:
Discharge summaries (DCS) are vital in facilitating handover to community colleagues. Unfortunately, at Whittington Health, General Practitioners (GPs) found it difficult to identify relevant information in DCS, and use of medical jargon meant patients did not understand details of their admission. With this quality improvement project, the team aimed to improve DCS to enhance patient-centered care.
OBJECTIVE:
The aim of this quality improvement project (QIP) was to improve the quality of DCS by critiquing the ones produced within our trust and implementing various interventions.
METHODS:
Multiple Plan-Do-Study-Act (PDSA) cycles were completed. A multi-disciplinary meeting was conducted to identify the needs of each party in a DCS. A new template was subsequently launched. Teaching was conducted and educational leaflets were disseminated hospital-wide. Quality of written communication was audited quarterly, and evaluated against quality indicators. Problems with DCS were identified via GP and patient feedback, and these became the focus of subsequent PDSA cycles.
RESULTS:
From March 2019 to February 2020, all the audited categories improved, with an overall improvement from 67% to 92%. We also received positive feedback from GPs.
CONCLUSIONS:
Quality of DCS can be improved with appropriate interventions, leading to improved patient care. A similar PDSA cycle could be utilized elsewhere to achieve similar results.
1.Background
DCS are a vital tool in ensuring the smooth transfer of patient care from inpatient to community settings. The Academy of Medical Royal Colleges has published guidance on the formatting and content of DCS which can provide a succinct, safe handover to community colleague [1]. In 2018, the Professional Records Standards Body published expected standards of information through integrated clinical IT systems [2]. This includes a concise summary of the admission, any completed investigations, and a detailed list of medications. Previous literature has shown that high quality DCS can reduce readmissions to hospital [3], improve attendance at outpatient appointments [4], and avoid medication errors [5].
In addition, DCS should provide patients with a comprehensible overview of their admission, including any follow up plans [1]. Previous QIPs have found that increasing lay terminology and avoiding medical terminology and acronyms improved patient and carer satisfaction [6].
Feedback from local GPs stated that our trust’s DCS were often convoluted and contained irrelevant information. Furthermore, patients informed us that they were unable to grasp a clear understanding of their care, as their DCS were long and contained unfamiliar medical language. They were consequently left with unanswered questions following discharge.
Previous studies have shown that regular feedback and structured teaching for junior doctors can improve the quality of their DCS [7]. Therefore, we designed a wide-reaching and high impact project by critiquing the DCS that our trust produced and implementing a range of interventions, with the aim of improving their quality, and subsequently patient care and satisfaction.
2.Methods
In November 2018, a multi-disciplinary meeting was held with medical consultants, GPs, Healthwatch, IT, junior doctors and patients in order to identify the needs of each party in a DCS. The views of patients and GPs were emphasized to highlight key elements required in discharge documentation, whilst balancing the time required for doctors to write them. Patients fed back that they wanted jargon free terminology so they could understand their care journey and follow up.
A new electronic template was created in June 2019 that incorporated feedback from all parties. A baseline audit was carried out, with DCS randomly selected from all 10 wards at the Whittington Hospital to remove selection bias. Important categories were evaluated using a 3 point-scale, scoring 0, 1 or 2 depending on the quality of information written, which included the use of jargon free language, presentation of information, and conciseness of content. The categories evaluated included co-morbidities, investigations, information for patient, GP actions, medications and named consultant. The score for each category was expressed as a percentage, and the overall quality of the DCS was determined by the average score, with each category being weighted equally.
Specific interventions were taken to increase awareness of this QIP. The consultant leading the project conducted teaching sessions during Grand Rounds and Patient Safety Forums for junior doctors to educate them on techniques for writing DCS. The team also created leaflets and posters, which were distributed throughout the hospital. Departmental representatives were nominated to monitor compliance, and emails were regularly sent to junior doctors who wrote excellent DCS to improve their engagement.
Subsequently, multiple PDSA cycles were implemented. The team met up quarterly and audited a sample of DCS from each specialty, with the design of the DCS being continuously updated following feedback from GPs and patients. The quarterly results were communicated internally, and any changes to the criteria conveyed via trust email.
3.Results
The initial audit in March 2019 revealed that, overall, DCS were 67% compliant with the quality indicators. Specifically, only 46% were compliant for the “investigations” section and only 32% had provided adequate “information for patient” (Table 1).
With repeated PDSA cycles, the compliance with quality indicators was found to improve (Table 1 and Fig. 1). Most notably, the “information for patient” section improved from 32% compliant to 91% and the “investigations” section improved from 46% to 71%. Safety netting advice was found to improve from 41% to 54% within three months. Overall, sampled DCS increased from 67% to 91% compliant with the quality indicators.
Fig. 1.
General improvement in DCS compliance with quality indicators on repeated PDSA cycles.
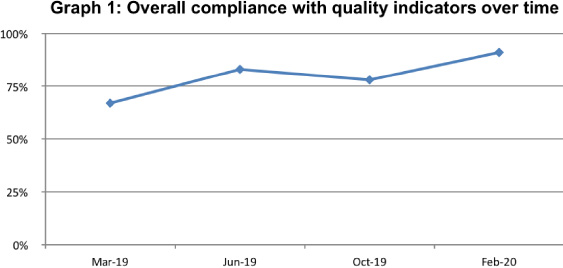
Table 1
Results by quality indicators
| Mar-19 | Jun-19 | Oct-19 | Feb-20 | |
| Co-morbidities | 86% | 96% | 94% | 94% |
| Investigations | 46% | 79% | 60% | 71% |
| Patient info | 32% | 64% | 58% | 91% |
| GP actions | 82% | 85% | 85% | 94% |
| Medications | 82% | 94% | 93% | 99% |
| Named consultant | 73% | 77% | 75% | 100% |
| AVERAGE | 67% | 83% | 78% | 91% |
[i] Table 1 shows the compliance of DCS subsections with quality indicators on repeated PDSA cycles.
4.Discussion
This project was successful in its aim for DCS to achieve an average score of 90% against the agreed quality standards. The results show that sustainable improvements can be achieved through continued education and working closely with the IT department.
It is evident that DCS provide an essential line of communication between primary and secondary care, as well as with patients themselves. However, it is clear that the information which GPs and patients require in DCS is very different. The introduction of the ‘information for patients’ section, consisting of clear, non-medical terminology, resulted in a significant improvement in the quality of the DCS and received positive feedback from GPs. Our project also built on the work of Earnshaw et al., who suggested that moving the ‘Information for The Patient’ section to the front page of the summary could further improve accessibility of lay terminology for patient understanding [6]. We rearranged the sections of the summary to put this information first, which received excellent feedback from patients and GPs.
The junior doctor education around appropriate documentation of investigations, such as the inclusion of relevant information that was appropriately summarized, was successful. This showed that continued education can produce sustained results [8,9], which is consistent with findings from our background research.
A key strength of the project was the initial MDT meetings that were held to establish quality indicators, as this ensured that interventions addressed key issues for the DCS recipients. The main limitation of this study was the subjectivity of the marking criteria. There was also potential for bias given that the summaries were marked by the project team.
The issues we encountered included making the DCS framework appropriate for use by all clinical inpatient teams, which limited some of our interventions. For example, it was suggested that the ‘Treatment Escalation Plan/DNACPR’ section was made compulsory, which may have improved the scores for recording this information. However, as the paediatric ward also uses this framework, it was felt that this would not be appropriate and could distress parents. A solution to this would be trialing software options which would allow departments to tailor the summaries to their specific needs. This could be explored in future projects. We also identified that summaries from departments with fewer junior medical staff were less likely to score highly, suggesting that our interventions were more effectively targeting foundation trainees, rather than higher trainees or consultants. This could be improved in future by incorporating DCS teaching into the induction for new senior staff, or by identifying teaching opportunities with a broader range of clinical staff in attendance. Lastly, the project could be improved further by objectively measuring patient outcomes, such as missed follow-up appointments.
5.Conclusion
This project was successful in its aims and has been able to bring about sustainable changes. It has shown the importance of tailoring DCS towards both GPs and patients, and provides evidence for other trusts on the effectiveness of including an ‘information for patients’ section. The future implications of this project would be for DCS to include other specialist sections, such as a ‘therapies section’, and to be tailored to meet specific departmental needs.
Conflict of interest
None to report.
Funding
The authors received no financial support for the research, authorship and publication of this article.
References
[1] | Professional Records Standards body. Guidance on the NHS Standard Contract Requirements on Discharge Summaries and Clinic Letters and on Interoperability of Clinical IT Systems. PRSB, 2018. www.england.nhs.uk/wp-content/uploads/2018/09/interoperability-standard-contract-guidance.pdf [Accessed 20 April 2021]. |
[2] | Academy of Medical Royal Colleges. Standards for the Clinical Structure and Content of Patient Records. AoMRC, 2013. www.aomrc.org.uk/wp-content/uploads/2016/05/Standards_for_the_Clinical_Structure_and_Content_of_Patient_Records_0713.pdf [Accessed 11 April 2021]. |
[3] | Salim Al-Damluji M, Dzara K, Hodshon B, Punnanithinont N, Krumholz H, Chaudhry S Association of discharge summary quality with readmission risk for patients hospitalized with heart failure exacerbation. Circulation: Cardiovascular Quality and Outcomes. (2015) ;8: (1):109–11. |
[4] | Darragh P, Bodley T, Orchanian-Cheff A, Shojania K, Kwan J, Cram P. A systematic review of interventions to follow-up test results pending at discharge. Journal of General Internal Medicine. (2018) ;33: (5):750–58. |
[5] | Caleres G, Bondesson Å, Midlöv P, Modig S. Elderly at risk in care transitions when discharge summaries are poorly transferred and used – a descriptive study. BMC Health Services Research. (2018) ;18: :770. |
[6] | Earnshaw C, Pedersen A, Evans J, Cross T, Gaillemin O, Vilches-Moraga A. Improving the quality of discharge summaries through a direct feedback system. Future Healthcare Journal. (2020) ;7: (2):149–54. |
[7] | Talwalkar J, Ouellette J, Alston S, Buller G, Cottrell D, Genese T A structured workshop to improve the quality of resident discharge summaries. Journal of Graduate Medical Education. (2012) ;4: (1):87–91. |
[8] | Otto M, Sterling M, Siegler E, Eiss B. Assessing origins of quality gaps in discharge summaries: A survey of resident physician attitudes. Journal of Biomedical Education. (2015) ;2015: :1–7. |
[9] | Axon R, Penney F, Kyle T, Marsden J, Zhao Y, Moran W A hospital discharge summary quality improvement program featuring individual and team-based feedback and academic detailing. The American Journal of the Medical Sciences. (2014) ;347: (6):472–7. |




