Proactive care post-discharge to reduce 30 day readmissions to hospital
Abstract
BACKGROUND:
Healthwatch England estimated emergency readmissions have risen by 22.8% between 2012–13 and 2016–17. Some emergency readmissions could be avoided by providing patients with urgent out of hospital medical care or support. Sovereign Health Network (SHN) comprises of three GP practices, with a combined population of 38,000.
OBJECTIVE:
We will decrease the number of SHN patients readmitted within 30 days of discharge from Portsmouth Hospitals Trust following a non-elective admission (excluding Emergency Department attendance) by 40–60% by July 2020.
METHODS:
Four Plan, Do, Study, Act (PDSA) cycles were used to test the administrative and clinical processes. Our Advanced Nurse Practitioner reviewed all discharge summaries, added alerts to records, and proactively contacted patients either by text, telephone or home visit.
RESULTS:
92 patients aged 23 days to 97 years were admitted onto the recent discharge scheme. Half of discharge summaries were received on the day of discharge, whilst 29% of discharge summaries were received more than 24 hours post-discharge, and one was received 11 days post-discharge. Following our interventions, there were 55% less than expected readmissions during the same time period.
CONCLUSION:
To allow proactive interventions to be instigated in a timely manner, discharge summaries need to be received promptly. The average readmission length of stay following a non-elective admission is seven days. Our proactive interventions saved approximately 102.9 bed days, with potential savings of 1,775 bed days over a year. We feel the results from our model are promising and could be replicated by other Primary Care Networks to result in larger savings in bed days.
1.Background
National Health Service (NHS) England defines an emergency admission to be “when admission is unpredictable and at short notice because of clinical need [1]”. Some emergency admissions are clinically appropriate and unavoidable, others could be avoided by providing alternative forms of urgent care or by providing appropriate support earlier to prevent a person becoming unwell enough to require an emergency admission.
Healthwatch England has estimated emergency readmissions have risen by 22.8% between 2012–13 and 2016–17 [1]. NHS Digital has recently released data regarding readmission rates within 30 days of discharge from hospital. Over the last six years the readmission rate in England has gone up every year, Fareham and Gosport Clinical Commissioning Group (FGCCG) on the south coast of England has however consistently remained lower than the national rate [2].
Sovereign Health Network (SHN) comprises of three GP practices — Highlands Practice, Jubilee Surgery and Whiteley Surgery and is located within FGCCG. All three practices provide services under general medical services (GMS) contracts and the network has a combined population of approximately 38,000 patients.
A 2014 systematic review of randomised control trials identified that interventions to prevent readmissions were more effective when they had multiple components, such as including more than one person involved in the delivery of the intervention or increasing patients’ ability to care from themselves [3].
A 2019 study from the Midlands found that geriatric ( >65 years) medical patients in receipt of a follow-up from a community nurse within 48hrs of discharge (telephone + ∕− home visit) were almost twice as likely to avoid a 30-day readmission compared to patients where no attempt was made. The decrease was statistically significant and could not be explained by differences between the two groups of patients [4].
2.Objective
The aim of this study was to decrease the number of SHN patients readmitted within 30 days of discharge from Portsmouth Hospitals Trust (PHT) following a non-elective admission (excluding Emergency Department attendance) by 40–60% by July 2020.
3.Methods
A Quality Improvement (QI) team was formed consisting of important stakeholders including the SHN Clinical Director, SHN Management Lead, SHN Project Officer, a GP (SHN QI Lead) and an Advanced Nurse Practitioner. A process map was developed with the involvement of key stakeholders and the implementation team met weekly.
Baseline measurement data provided by FGCGG estimated that from 1st January to 31st December 2019 there were 461 SHN patients readmitted within 30 days of discharge, an average of 8.9 per week.
Plan-Do-Study-Act (PDSA) cycles were used to trial the improvement interventions. PDSA cycles 1a–1c were ‘non-live’ cycles, with the aim of testing the different administration processes that needed to take place. PDSA cycle 2 was a ‘live’ cycle putting in place clinical interventions.
PDSA cycle 1a: our initial intervention was to test the model of care. The administration team in each practice added the names of patients who had been discharged from Portsmouth Hospitals Trust onto an appointment book within a shared database. This allowed us to ascertain how many patients were being discharged, how many of these were elective admissions, how many were non-elective admissions and ensure that the discharge summary was correctly attached to the patients’ records.
PDSA cycle 1b: once we were confident that the administration team were able to correctly identify patients who had been discharged following a non-elective admission, the team then began to add the patient details to a tracking spreadsheet.
PDSA cycle 1c: in this cycle we introduced our Advanced Nurse Practitioner into the work stream. During this cycle there were still no clinical interventions taking place, the purpose was to test the red, amber, green (RAG) rating system and develop ideas about the sorts of interventions our Advanced Nurse Practitioner would put in place.
PDSA cycle 2: this was our first ‘live’ cycle. Interventions included adding an alert to the patients’ medical records, sending the patient a text message with safety-netting information, telephoning the patient, conducting a home visit, reviewing the patient during a Care Home ward round, or arranging a face-to-face appointment with a GP or Practice Nurse. Due to the COVID-19 pandemic, Sovereign Health Network commenced their business continuity plan on 16th March 2020 and all non-essential activity was deprioritised. From this date no new patients were admitted onto the scheme, however it remained fully operational until the last patient reached 30 days post-discharge.
Example case study: 91 year old male admitted to hospital for 11 days following a fall and symptoms of heart failure. His discharge summary was received two days after discharge, it was reviewed and on day four post-discharge a telephone call was made to the wife and son to ensure they had support at home with a package of care. A referral to the Extended Primary Care Team for social support was made and the family was provided with information about the discharge project and who to contact if they had any concerns. A further telephone review was made on day 18 post-discharge; they confirmed that intensive input was being received from the Rapid Therapy Team. Had contact not been made to ensure the correct support and referrals were in place; he potentially could have been readmitted if they were not able to cope at home.
4.Results
Patients were admitted onto the scheme from 24th February until 16th March 2020, with the last patient being discharged from the scheme 30 days later on 11th April 2020.
During this time period, 92 patients were admitted onto the scheme, 44 from Highlands Practice, 30 from Jubilee Surgery and 18 from Whiteley Surgery. The age of the patients ranged from 23 days to 97 years with a mean age of 54 years.
The length of stay for the index admission ranged from 0 to 191 days. Excluding the outlier, the index admission of length of stay was 0–51 days, with a mean of 4.4 days and a median of 2 days—this highlights that over 50% of index admissions were for two days or less.
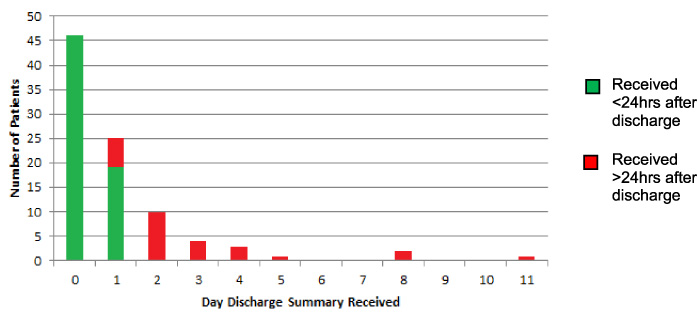
Exactly half of discharge summaries were received on the day of discharge, however 29% of discharge summaries were received more than 24 hours post-discharge, and one was received 11 days post-discharge (see Fig. 1).
Fig. 1.
Day discharge summary received post index admission.
The actual number of 30-day readmissions over the duration of the project was 12 (see Fig. 2), this was 14.7 fewer (55% less) than the predicted number of 30-day readmissions based on the data provided by FGCCG.
Fig. 2.
Number of readmissions by day post-discharge.
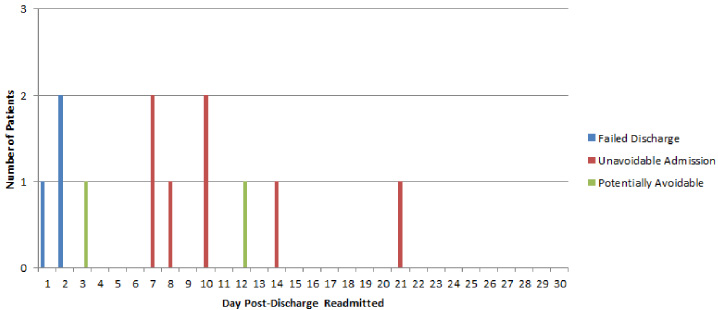
Of the 12 patients that were re-admitted we felt that only two of them were potentially avoidable in that they could have been prevented by interventions in primary care. One patient was re-admitted with right iliac fossa pain secondary to an ovarian cyst on day three post-discharge, but we did not receive the original discharge summary until day four. The other patient was readmitted on day 12 post-discharge with colitis, but we did not receive the original discharge summary until day 11.
We felt three patients had failed discharges; two were readmitted with falls and their index admissions were falls. The third patient who was known to have severe chronic obstructive pulmonary disease on home oxygen therapy was readmitted with hospital acquired pneumonia.
Seven patients were thought to have had unavoidable readmissions. This included patients with sepsis, a patient who was COVID positive, a child receiving chemotherapy and patients with infections that were not responding to antibiotics that had been prescribed in the community.
5.Conclusion
The average readmission length of stay following a non-elective admission is seven days. Our proactive interventions would therefore have saved approximately 102.9 bed days, with potential savings of 1,775 bed days over a year.
Although all three practices use the same clinical system (EMIS Web), we encountered a number of Information Technology issues. All three practices use different systems for viewing their incoming documents, this meant that the discharge summaries for Jubilee Surgery patients had to be sent in a different format by the administration team otherwise they could not be viewed by the Advanced Nurse Practitioner. The intention is for the other two practices to upgrade their document viewing system so they are all aligned.
To allow proactive interventions to be instigated in a timely manner, discharge summaries need to be received promptly. The NHS Standard Contract requirements on Transfer of Care documentation the key requirements of the provider are following inpatient or day case care of A&E attendance, to issue a Discharge Summary to the patient’s GP within 24 hours.
We would be in favour of receiving live data of PHT discharges to further develop this scheme so we can continue to support patients in a timelier manner following discharge.
Despite the recent discharge scheme only running for a relatively short period of time due to the COVID-19 pandemic, we feel that the results from our model are promising and could be replicated by other Primary Care Networks (PCNs) to result in larger savings in bed days.
Conflict of interest
None to report.
References
[1] | Department of Health and Social Care (2018). Reducing emergency admissions (session 2017–19, HC 833). Retrieved from: https://www.nao.org.uk/wp-content/uploads/2018/02/Reducing-emergency-admissions.pdf. |
[2] | NHS Digital (2020. Data set 3.2 Emergency readmission within 30 days of discharge from hospital [online] Available from: https://digital.nhs.uk/data-and-information/publications/statistical/ccg-outcomes-indicator-set/march-2020/domain-3-helping-people-to-recover-from-episodes-of-ill-health-or-following-injury-ccg/3-2-emergency-readmissions-within-30-days-of-discharge-from-hospital. |
[3] | Leppin AL, Gionfriddo MR, Kessler M Preventing 30-day hospital readmissions: A systematic review and meta-analysis of randomized trials. JAMA Intern Med. (2014) ;174: :1095–107. |
[4] | Vernon D, Brown JE, Griffiths Reducing readmission rates through a discharge follow-up service. Future Health J Jun. (2019) ;6: (2):114–7. |




