Broad spectrum antibiotic stewardship by quality improvement methods
Abstract
BACKGROUND:
With the majority of antibiotics being prescribed in primary care it is of utmost importance that antimicrobial stewardship principles are adhered to in order to slow down the incidence of antimicrobial resistance.
OBJECTIVE:
Broad spectrum antibiotic prescribing is often seen as a proxy marker of increasing resistance within a population and so it is important that they are used sparingly, to avoid drug-resistant bacteria developing.
METHOD:
In Tameside and Glossop a novel approach, using quality improvement methods, was employed to allow the behaviour change to be sustained for a longer period. Practices submitted monthly broad spectrum usage data, and if over a set target they were required to submit a “deep dive”.
RESULTS:
A 10.6% reduction of broad spectrum antibiotic usage was seen over the 2019-20 financial year.
CONCLUSION:
Over time the number of practices submitting a deep dive reduced and clinicians saw the deep dive as method to peer review their prescribing. Putting the practice staff in control of their own prescribing, allowed for a better method to sustain the improvement.
1.Background
Antimicrobial resistance (AMR) is an increasingly serious threat to global public health. Although we are now more informed on the economic burden of resistance than in previous years, there is still a distance required to go to fully understand the exact implication of this burden [1].
The threat of AMR is multifactorial including, a lack of investment in antibiotic development and antibiotic overuse. When used appropriately to treat actual bacterial infections, antibiotic use generate benefits by expediting infection clearance and recovery from associated illness, whilst generating public benefits by reducing the spread of infection across the rest of the population. However, their use can select for bacteria with resistance, hence reducing the effectiveness of future antibiotic use [2].
Around 71% of all antibiotics are prescribed in primary care in England [3]. Antibiotic quality premium (QP) targets have been set by NHS England to help reduce antibiotic consumption. Since 2013, QP targets encompassed a method to incentivise clinical commissioning groups (CCGs) to encourage behaviour change and reduce antibiotic consumption [4]. Prescribing data from England show a reduction of about 2.7 million antibiotic items between 2014/15 and 2016/17 [4]. These have now largely been replaced with a target to reduce antibiotics consumption via the ‘Tackling Antimicrobial Resistance 2019 to 2024: The UK’s 5-year national action plan [5,6]’.
The NHS Oversight Framework replaced the Clinical Commissioning Group (CCG) Improvement and Assessment Framework (IAF). It was intended as a focal point for joint work, support and dialogue between NHS England and NHS Improvement, clinical commissioners, providers and sustainability and transformation partnerships and integrated care systems. The NHS Oversight Framework 2019/20 contained 2 antimicrobial resistance (AMR) related indicators with set targets that have been used in NHS improvement and assurance schemes for CCGs since 2015 [3].
The indicators are:
reduction in the number of antibiotics prescribed in primary care to be equal to or below value of 0.965 antibacterial items per Specific Therapeutic Group Age-sex Weightings-Related Prescribing Units (STAR-PU) (12 months);
number of co-amoxiclav, cephalosporins and quinolones as a percentage of the total number of selected antibacterials prescribed in primary care to be 10% or below.
The ‘5-year plan’ states that sub-optimal use of antimicrobials in human medicine is one of the main drivers of AMR. Sub-optimal use not only increases time to cure and perhaps treatment failure, but drives resistance at an alarming rate. The ‘5-year plan’ specifies a reduction target of antimicrobial use in humans by 15% by 2024. Part of this action plan is to strengthen stewardship programmes ensuring antimicrobials are only used when appropriate and clinically indicated or required.
The antibiotic prescribing trends in Tameside and Glossop are monitored monthly, when ePACT data from the NHS BSA becomes available. Upon studying our broad spectrum consumption trends over the course of a year, following the cessation of monitoring as part of a QP target, it seemed broad spectrum usage increased since not being monitored as part of the QP. Co-amoxiclav, cephalosporins and quinolones are broad spectrum antibiotics that can be used when others have failed. It is important that they are used sparingly, to avoid drug-resistant bacteria developing [7].
However, the CCG as a whole for antibiotic prescribing was below the target of 0.965 STAR-PU and broad spectrum antibiotics use still below the 10%. In order to reduce resistance, it is imperative to at least maintain, if not reduce this momentum. The task of reducing and staying below these targets would be difficult. The principles of AMS are the real reason that true behaviour change can be sustained. It was felt that if a strategy can be employed, whereby clinicians can monitor and take more responsibility for their prescribing actions, rather than seeing it as a target, the reduction would be able to be maintained for a longer period of time.
2.Methods and interventions
Every practice had previously sent two participants to a 2-hour QI-basics session for a similar project on reduction of trimethoprim prescribing in over 70 year olds to ensure clinically appropriate prescribing to treat urinary tract infection.
The CCG rewarded practices with 67 pence per patient, on the practice list if they participated. The payment was for submission of prescribing system data and participation, including submission of a detailed ‘deep dive’ if the practice was over the set target, not for achieving the set goal. The payment was around £1675 per year for a practice with a list size of 5000. Even though participation was optional, all the practices chose to take part.
The CCG average items per 1000/patients/month was calculated using OpenPrescribing and EMIS/SystemOne search data. A CCG average worked out at 3.2/1000 patients with a 10% reduction applied, the target was set at 2.88/1000 patients. This was the goal that we wanted all practices to reach.
A search was set up centrally on EMIS and SystemOne allowing the Practices to access and run the search easily and a guide with simple instructions, on how to run the search, was sent to all practices.
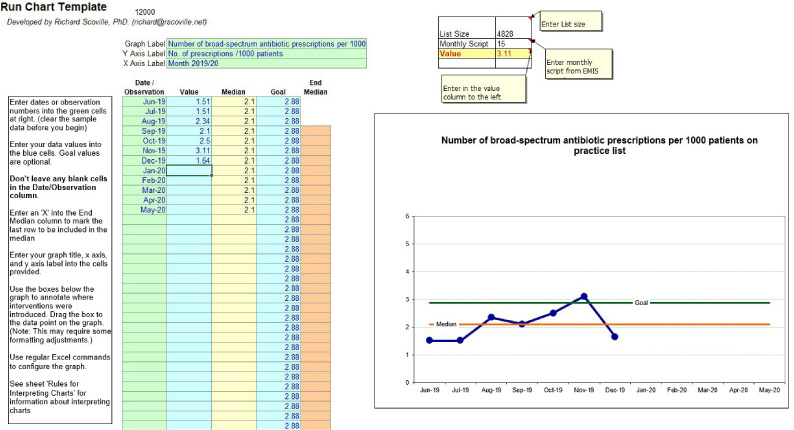
Practices were required to run the search by the 7th of each month and plot the data into a run chart template before submitting the data. Fig. 1 shows a sample of the run chart.
Fig. 1.
An example run chart that was required to be completed by practices each month. The template was set up so that practice staff were only required to input their list size and the number of prescriptions for broad spectrum antibiotics issued every month into the required boxes.
If the value, submitted by the practice, was above the predefined threshold, the practice was required to undertake a case notes review or “deep-dive”, which was reviewed by the Antibiotic Specialist Pharmacist. This was used to provide feedback on methods to reduce inappropriate broad spectrum prescribing. The process was repeated each month, with a view that the deep dives would become less frequent as time went on – indicating reduction in prescribing, but more importantly, instilling principles of good AMS.
Sustainability was achieved by ensuring ease of the task and by using a locally commissioned service to provide a monetary incentive. This meant the data was relatively easy to collect and submit.
This method of data collection and intervention had been employed previously for reduction in trimethoprim prescribing for a previous QP target. The practices had become accustomed to this way of working and submitting data. The change was successful and issues relating to the method had been rectified with the reduction project.
3.Results
In one year (Mar 19 to Mar 20), 10.6% reduction in broad spectrum consumption across the CCG, as seen in Fig. 2.
Fig. 2.
The year on year rolling (takes into account seasonal variation) growth per quarter. The red line showing the trend in Tameside and Glossop, shows negative growth – meaning there is a reduction in broad spectrum items issued when compared to the average for Greater Manchester.
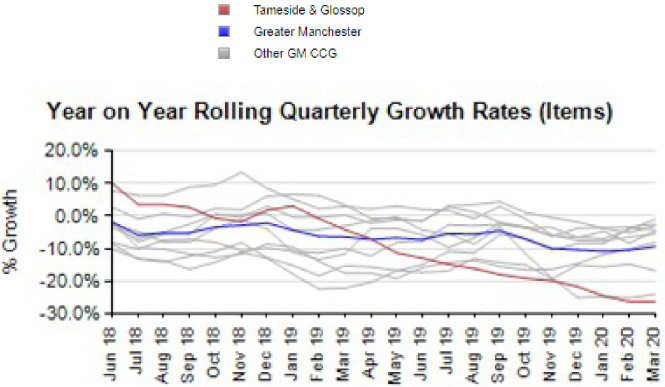
The only intervention made, with regards to broad spectrum prescribing, in this time period was the requirement to submit run chart data and input with regards to appropriate prescribing strategies from the Antibiotic Specialist Pharmacist, if above the predefined threshold as described.
Post-March 2020 the pressures related with COVID-19 and the uncertainty around diagnosis saw increased levels of all antibiotics. The increased levels of antibiotic prescribing was also related to remote working and attempting to figure out a completely new method of consultation.
4.Discussion
It was seen that, with time, the practices and the staff involved saw the deep dives as a way for them to peer review their prescribing, rather than a tool for criticism. This allowed the reduction, and essentially, the appropriate broad spectrum prescribing to be maintained over time.
Putting the practice staff in control of their own prescribing, allowed for a better method to sustain the improvement. It is often difficult to maintain such profound improvements in antibiotic prescribing.
The COVID-19 pandemic saw some increase in overall prescribing, in line with the national trend. However, within Tameside and Glossop CCG the areas of increase have been identified quickly and action taken to ensure antibiotic prescribing, as a whole, is of a more appropriate nature. This has namely been with interventions undertaken by the Antibiotic Specialist Pharmacist, whereby prescribing data has been used to identify practices that may require some assistance to manage antibiotic prescribing. The methods used were individualised together with the clinicians to ensure sustainability.
The rates of antibiotic and broad spectrum have stayed below those of previous years, so there has been some sustained reduction in real terms, despite the challenges faced due to the pandemic.
5.Conclusion
Early identification of potentially unwarranted increases with regards to prescribing can help with long term sustainability of the improvement achieved. It is also beneficial to individual practices if their prescribing is queried by an individual seen as an extended member of the wider team.
It was found that many practices were perplexed when they received the Chief Medical Officer (CMO) letter a few years earlier, as the increased rates of prescribing had been identified and rectified by the time the letter was received. Perhaps, as the most up to date data hadn’t been used to identify the practices that received the CMO letter, the practices in Tameside & Glossop didn’t see it as a timely intervention, so there wasn’t the desired impact that was expected from a national perspective.
General Practice in England has, since 2004, been receiving performance-related pay in the form of the Quality and Outcomes Framework [8]. This pays for the achievement of targets. For this project the payment was for engagement in a QI process, including gathering and understanding data and using this to influence future prescribing. We were pleased to say this had the positive benefit on prescribing behaviour without the need for a target to be achieved.
6.Limitations
Some baseline knowledge of QI methods is required for those involved in the data collection and reporting, so some training is needed. This was overcome by providing a session at the beginning of the improvement task.
The monetary incentive required to encourage participation was built in as part of a locally commissioned service. This may not be the case across the country but can help to drive down inappropriate use of broad spectrum antibiotics, as seen here.
Ensuring the deep dive is completed with sufficient information can be a challenge, as it’s done retrospectively. Having a template to complete this task has helped with some consistency in the information provided.
With time it has been seen that the personnel involved have become accustomed to the methods of working with this improvement project. It is important to ensure buy-in from all parties at the onset and give them clear feedback on a regular basis.
7.Conflict of interest
None to report.
References
[1] | Smith R, Coast J. The true cost of antimicrobial resistance. BMJ. (2013) ;346: :f1493-f1493. |
[2] | Jit M, Ng D, Luangasanatip N, Sandmann F, Atkins K, Robotham J Quantifying the economic cost of antibiotic resistance and the impact of related interventions: Rapid methodological review, conceptual framework and recommendations for future studies. BMC Medicine. (2020) ;18: (1). |
[3] | Department of Health and Social Care. English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) Report 2019 to 2020. London: Public Health England; 2020. |
[4] | Anyanwu P, Tonkin-Crine S, Borek A, Costelloe C. Investigating the mechanism of impact of the Quality Premium initiative on antibiotic prescribing in primary care practices in England: A study protocol. BMJ Open. (2019) ;9: (8):e030093. |
[5] | Department of Health and Social Care. UK 5-year action plan for antimicrobial resistance 2019 to 2024. London: Global and Public Health Group, Emergency Preparedness and Health Protection Policy Directorate; 2019. |
[6] | Contained and controlled: the UK’s 20-year vision for antimicrobial resistance [Internet]. London: Department of Health and Social Care; 2019 [cited 27 April 2021]. Available from: https://www.gov.uk/government/publications/uk-20-year-vision-for-antimicrobial-resistance. |
[7] | Prescribing measures for NHS TAMESIDE AND GLOSSOP CCG | OpenPrescribing. Openprescribing.net. 2021 [cited 21 April 2021]. Available from: https://openprescribing.net/ccg/01Y/measures/?tags=antimicrobial. |
[8] | NHS England – GP Contract [Internet]. England.nhs.uk. 2021 [cited 27 April 2021]. Available from: https://www.england.nhs.uk/gp/investment/gp-contract/. |




