Changes in neurorehabilitation management during the COVID-19 pandemic: A scoping review
Abstract
BACKGROUND:
The SARS-CoV-2 infection (COVID-19) has generated a threat to global health, determining the need for healthcare for large numbers of people in an extremely short time
OBJECTIVE:
To investigate the management changes in the neurorehabilitation services during the COVID-19 pandemic.
METHODS:
An electronic search was conducted in September 2021 by 2 independent reviewers in the following databases: MEDLINE (PubMed), the Physiotherapy Evidence Database, and the Cochrane Database of Systematic Reviews. All studies on organizational and welfare changes resulting from the COVID-19 pandemic in neurorehabilitation services were included. Screening of titles, abstracts, and full texts and data extraction were undertaken independently by pairs of reviewers.
RESULTS:
The summary of results was reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for scoping reviews.
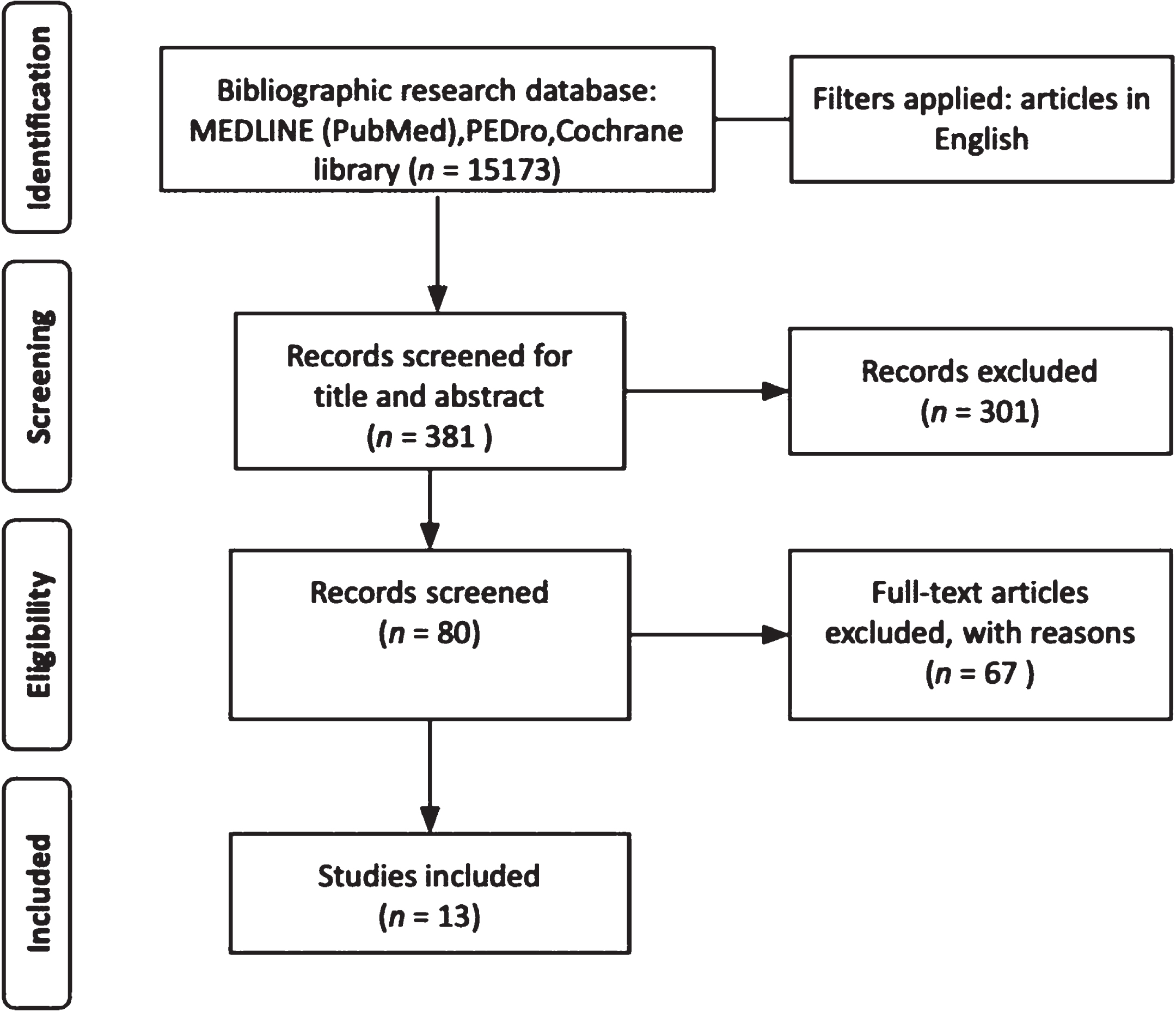
Electronic searches after the screening of title and abstract identified 80 studies, 13 studies met the inclusion criteria. A narrative summary of results of all included studies were reported in a tabular format.
CONCLUSIONS:
Different organizational models were adopted in neurorehabilitation during the COVID-19 pandemic impacting the therapies time frame, the physical and mental health of healthcare professionals and the caregiver’s workload. There is still uncertainty about the effectiveness of these new therapeutic strategies on the management of neurorehabilitation services and future studies should explore the effect on the patients’ needs.
1Introduction
The SARS-CoV-2 infection (COVID-19) has generated a threat to global health, determining the need for healthcare for large numbers of people in an extremely short time (Bartolo et al., 2020; World Health Organization, 2021a). It overwhelmed emergency departments, infectious disease, pulmonary and intensive care units. Therefore, health services became more rigorous while imposing radical changes in organization and operating procedures (World Health Organization, 2020a).
After COVID-19 global emergency was declared, a strategic preparedness and response plan was introduced by the World Health Organization (WHO) (World Health Organization, 2020b). This strategy was aimed to provide the technical and operational response pillars to support countries to control transmission of the virus, to save lives, and to safeguard susceptible individuals such as the elderly, people with disabilities and with multiple comorbidities or chronic diseases. As reported by WHO, the governments, waiting for effective therapies, have reacted by adopting national COVID-19 action plan with standard measures, such as quarantine and restrictions to travel and mobility (World Health Organization, 2021b). However, unlike in the past, this health emergency has arisen in a globalized and interconnected society unlike any other; defined by populations that tend to congregate in highly urbanized and overcrowded environments, with easy movement between continents (Dobson & Carper, 1996; World Health Organization, 2021b).
Within this perspective, neurorehabilitation services have struggled in the very same way in the need to remodel their operating procedures. Indeed, neurorehabilitation is a complex medical process that offers a coordinated interdisciplinary care program with measures that aid individuals who experience disability to achieve and maintain optimal function in interaction with their environment, for maximum independence and social reintegration (Caltagirone et al., 20221; Khan Fary et al., 2015). In Europe, neurorehabilitation services started to quickly reorganize their internal structure and care delivery by trying to guarantee access to the patients with recent disease onsets, which, if left untreated, could have resulted in disability, including those who contracted the SARS-CoV-2 virus (Treger et al., 2020). Initially, non-urgent medical activities were postponed to give priority to the reorganization of intensive care units (Leocani et al., 2020). At the same time, it maintained a therapeutic-rehabilitative contact with people suffering from chronic and/or degenerative neurological diseases, which have seen the postponement of all outpatient and day hospital services, to avoid worsening of the conditions and quality of life (Maccarone & Masiero, 2021). For example, in Italy, there was a notable decrease of over 50% in hospitalizations, possibly due to fear of contagion and the social isolation that comes with a hospital stay (Lazzerini & Putoto, 2020).
After about two months of lockdown, it became evident that the COVID-19 disease would still be circulating for months. For this reason, specific actions and adaptation strategies were taken to ensure a return to previous levels of healthcare, ensuring safety and access to treatment, especially in neurorehabilitation (Leocani et al., 2020).
This scoping review aimed to map the scientific literature that clarifies the organizational and welfare changes resulting from the COVID-19 pandemic in neurorehabilitation services.
2Methods
The current scoping review was prepared by referring to the “2020 version of JBI Manual for Evidence Synthesis Chapter 11: Scoping Review” available fromhttps://synthesismanual.jbi.global and following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (the PRISMA-ScR) (Peters et al., 2020).
2.1Search strategy and eligibility criteria
Electronic databases searched in September 2021 were MEDLINE (PubMed), Physiotherapy Evidence Database, and the Cochrane Database of Systematic Reviews. The terms used for this search were: Coronavirus, Covid-19, Sars-cov-2, neurological disorder*, neurological disease*, rehabilitation, neurorehabilitation and management. These terms were combined using the Boolean AND and OR operators. Search terms were modified for each database and appropriate subheadings were used for each database that was searched (for details see the Appendix).
Controlled and non-controlled clinical trials (i.e., randomized or non-randomized trials), retrospective studies, case reports, case series, observational studies, reviews and systematic reviews have been included. Studies published until September 2021, in English without any restrictions in terms of country, sex and age of participants were accepted. All articles focused on rehabilitation and neurological rehabilitation were selected. Only patients with neurological diseases, caregivers who assisted this type of patients and healthcare professionals working in hospitals or rehabilitation/neurorehabilitation facilities were included.
2.2Study selection and data collection process
The search strategy results were uploaded and managed through Zotero, online software of the Corporation for Digital Scholarship, which was developed by a global community for collecting, organizing, citing and sharing research. Duplicates were automatically removed; records were screened first by title and abstract and second by full-text reading. Both phases were conducted by starting with a pre-screening team meeting to discuss inclusion and exclusion criteria. To test the consistency of extracting and reporting methods, 18 h of training were carried out by the peer-reviewers in three online meetings. The reviewers independently screened the articles; disagreements were resolved through discussion and consensus. Further details of this review process are better illustrated in the PRISMA flow diagram (Fig. 1).
Fig. 1
PRISMA flow diagram of studies selected for the present study.
2.3Data extraction and synthesis
The same authors independently extracted the following relevant features of the included studies: 1) author; 2) publication year; 3) study type; 4) diagnosis; 5) participants; 6) objective; 7) intervention characteristics; 8) intervention duration; 9) outcomes; 10) setting; and 11) country. Thus, the selected articles have been grouped and synthesized in different thematic areas such as i) organizational models adopted in neurorehabilitation during the COVID-19 pandemic; ii) changes in the choice of therapeutic strategies; iii) consequences of new measures on patients, healthcare professionals and caregivers.
3Results
After the screening by title and abstract, 80 articles were assessed for eligibility, 13 articles were found suitable for this scoping review (Assenza et al., 2021; Dalise et al., 2021; Farí et al., 2022; Gorini et al., 2020; Kim et al., 2021; Lee et al., 2021; Manacorda et al., 2021; Salvia et al., 2020; Santamato et al., 2021; Spielmanns et al., 2021; Summaka et al., 2021; Sutter-Leve et al., 2021; Yogev-Seligmann & Kafri, 2021). 37 studies were inconsistent with the research question, and the other 30 did not meet the inclusion criteria (6 studies did not include neurological rehabilitation; 11 studies included a different population; 13 studies with a different study design). A summary of results of all included studies have been synthesized in a tabular format reporting the following information: name of primary author and publication year, study type, participants, and intervention (Table 1).
Table 1
Description of the included studies
| First author, year | Study type | Participants | Intervention |
| Assenza et al., 2021 | Observational transversal study | Patients (n = 169) | Online questionnaire on telerehabilitation |
| 25 adult patients; 144 children. | |||
| Cerebral palsy, genetic disorders, neuromuscular diseases, stroke, acute brain injury, spinal cord injury, Parkinson disease, and multiple sclerosis. | |||
| Healthcare workers (n = 50) | |||
| Physical therapists, speech therapists, neurodevelopmental therapists, occupational therapists, psychologists. | |||
| Children’s caregivers (n = 144) | |||
| Dalise et al., 2021 | Cross-sectional observational study | Patients (n = 134) | Telephonic interview |
| Stroke, focal dystonia, Parkinson disease, multiple sclerosis, peripheric causes, traumatic brain injury, paraparesis, sub aracnodal hemorrhage, Mielec diseases. | |||
| Farí et al., 2022 | Retrospective study | Healthcare workers (n = 68) | Online questionnaire |
| Physicians, nurses, and physical therapists | |||
| Gorini et al., 2020 | Multicentre cross-sectional study | Healthcare workers (n = 650) | Online survey |
| Physicians, nurses, and administrative staff. | |||
| Kim et al., 2021 | Prospective, open-label, single-arm pilot study | Patients (n = 21) Parkinson disease, parkinsonism. | Home-based exercise with mobile app |
| Lee et al., 2021 | Qualitative Study | Caregivers (n = 25) | Individual semi-structured interviews |
| Manacorda et al., 2021 | Observational study | Patients (n = 2722) | Questionnaire online |
| Multiple sclerosis | |||
| Salvia et al., 2020 | Observational study | Patients (n = 253) | Analysis of reorganization of neurorehabilitation activities |
| Stroke, traumatic brain injury, spinal cord injury, Parkinson disease, multiple sclerosis. | |||
| Clinical professionals (n = 722) | |||
| Other hospital workers (n = 232) | |||
| Santamato et al., 2021 | Multicentric cross-sectional study | Patients (n = 151) | Phone-based survey |
| Stoke, traumatic brain injury | |||
| Spielmanns et al., 2021 | Retrospective cohort study | Patients (n = 27) | Analysis of reorganization of neurorehabilitation activities |
| With or without nosocomial COVID-19 infection and neurological comorbidities | |||
| Summaka et al., 2021 | Cross-sectional study | Patients (n = 118) | Online survey |
| Tetraplegia, paraplegia, hemiplegia, paresis. | |||
| Sutter-Leve et al., 2021 | Phenomenological study | Caregivers (n = 11) | Semi-structured interview Questions in person or over the telephone |
| Yogev-Seligmann &Kafri, 2021 | Observational study | Patients (n = 142) Parkinson disease | Web-based survey |
The included studies were conducted in the United States (Sutter-Leve et al., 2021), Republic of Korea (Kim et al., 2021), Italy (Assenza et al., 2021; Dalise et al., 2021; Farí et al., 2022;Gorini et al., 2020; Manacorda et al., 2021; Salvia et al., 2020; Santamato et al., 2021), China (Lee et al., 2021), Lebanon (Summaka et al., 2021), Israel (Yogev-Seligmann & Kafri, 2021) and Switzerland (Spielmanns et al., 2021). There were 12 observational studies (Assenza et al., 2021; Dalise et al., 2021; Farí et al., 2022; Gorini et al., 2020; Lee et al., 2021; Manacorda et al., 2021; Salvia et al., 2020; Santamato et al., 2021; Spielmanns et al., 2021; Summaka et al., 2021; Sutter-Leve et al., 2021; Yogev-Seligmann & Kafri, 2021), and one clinical trial (Kim et al., 2021).
3.1Organizational models adopted in neurorehabilitation during the COVID-19 pandemic
Two studies were found regarding the choices and changes made by rehabilitation facilities attempting the containment of infection spread in hospital settings. Despite slight differences, the main actions undertaken in the two hospitals were: use of personal protective equipment, isolation, staff training and increased hygiene and disinfection policies (Salvia et al., 2020; Spielmanns et al., 2021). Both studies have compared the length of hospitalizations and the amount and effectiveness of the treatments during the Covid-19 period to the 2019 data. The first study (Salvia et al., 2020) found significant reductions in hospital admissions, shorter length stays and dramatic reductions in outpatients care when comparing their results with previous data from 2019. Nonetheless, the authors have reported unaffected inpatient treatment duration and effectiveness in the delivered therapies. On the contrary, the second study (Spielmanns et al., 2021) had reported longer length stays, a decrease in the duration of therapies and decremental improvements, as a result of the implemented hygiene policies. Overall, the length of hospitalization got contrasting results, on the one hand, a decrease was reported (Salvia et al., 2020) and on the other hand, an increase in hospitalization days (Spielmanns et al., 2021) was registered.
3.2Changes in the choice of therapeutic strategies
Following the interruption of outpatient activities, Assenza et al. 2021 investigated the use of telerehabilitation as an alternative tool to provide access to therapy in a home setting. The studied population were 25 adult patients, 144 children’s caregivers and 50 therapists. It was found that all respondents reported a medium-high level of positive perception and a high level of satisfaction with the telerehabilitation approach, especially in subjects under the age of 40. And adult patients needed assistance from the caregiver to perform the proposed exercises. Moreover, the sample of healthcare workers has perceived telerehabilitation as a useful tool to improve the sense of competence of patients and caregivers in relation to disability and to increase therapeutic goals. Besides, all caregivers of treated children have perceived telerehabilitation as a support tool, but they have shown skepticism about the actual achievement of therapeutic goals.
Similarly, Kim et al. 2021 investigated the use of new technologies to evaluate the effects of home exercise management in 21 patients with Parkinson’s disease and parkinsonism. Participants showed a significant increase in the amount and intensity of the weekly exercise. The study also reported a decrease in a sedentary life, depression, and an improvement in the quality of life. In general, the participants expressed good satisfaction with the usability of the app.
3.3Consequences of new measures
3.3.1Patients
Five studies (Assenza et al., 2021; Dalise et al., 2021; Santamato et al., 2021; Summaka et al., 2021; Yogev-Seligmann & Kafri, 2021) investigated the impact and consequences of the interruption of rehabilitation in patients with chronic disabilities or neurological diseases. Patients were interviewed through online surveys (Manacorda et al., 2021; Summaka et al., 2021; Yogev-Seligmann & Kafri, 2021) or telephone interviews (Dalise et al., 2021; Santamato et al., 2021) and a total of 3125 people were interviewed. In general, all patients experienced a decrease in perceived well-being, independence, daily life activities and social participation. Additionally, patients undergo feelings of fear, depression, anxiety, and a worsening of perceived symptoms. Specifically, in patients with neurological diseases, a decrease in family cohesion was observed (Yogev-Seligmann & Kafri, 2021). In addition, people with moderate and severe disabilities experienced a deterioration in their health (Manacorda et al., 2021). Likewise, patients with neurological diseases have complained about an increase in somatic manifestations and emotional and behavioural responses, with an increase in risk behaviour (Assenza et al., 2021; Santamato et al., 2021; Summaka et al., 2021).
3.3.2Healthcare professionals
Two studies (Farí et al., 2022; Gorini et al., 2020) observed the impact of COVID-19 disease on a total of 718 healthcare professionals through online surveys. Gorini et al. 2020 reported a change in the daily workload and found that healthcare workers perceived that they are more at risk of contracting the virus than their family members. But the greatest concern was about being a transmission vehicle. Furthermore, Farí et al. 2021 reported an increase in levels of depression, anxiety, emotional exhaustion, and depersonalisation, especially in women.
3.3.3Caregivers
Two articles analyzed a total of 180 people, including 25 caregivers assisting newly-onset stroke patients at home (Lee et al., 2021) and 11 caregivers of stroke patients in rehabilitation facilities (Sutter-Leve et al., 2021). Lee et al. 2021reported an increase in caregivers’ workload and a decrease in their physical and psychological well-being. Similarly, Sutter-Leve et al. 2021 registered that caregivers who had hospitalized relatives experienced concern about their relatives’ care and progress and had difficulty communicating with the members of the rehabilitation team. Moreover, the same study also reported high levels of uncertainty about home management after discharge from the hospital. The authors conclude that clear and timely communication with healthcare professionals and the support of relatives and friends facilitated the maintenance of low levels of stress on caregivers’ health (Sutter-Leve et al., 2021).
4Discussion
This scoping review aimed to address the changes and strategies adopted by the neurorehabilitation services during the first wave of COVID-19 and included studies conducted on average between March and June 2020. The early detection and management of COVID-19 positive cases through swab screening and serological testing in patients and employees, has helped to significantly decrease the spread of the virus within neurorehabilitative services (Salvia et al., 2020). Even though, the containment measures taken to limit the hazard risk of contagion have enhanced safety on a high level, neurorehabilitation therapies in terms of frequency and intensity have been modified (Salvia et al., 2020). With the latter, being particularly negative in cases where a decrease in the therapy time frame has happened, and an as consequence, affecting the patients’ recovery. Particularly, in patients with sub-acute stroke, where it is well recognized that earlier and multidisciplinary therapeutic training leads to higher recovery (Iosa et al., 2021; Veerbeek et al., 2014). Additionally, there have been reported other factors that may have affected rehabilitation services, such as reduced therapeutic alliance and social isolation, and a decrease of group activities (Spielmanns et al., 2021).
The COVID-19 disease has certainly imposed more challenges to the neurorehabilitation services, specifically, increasing the frequency of hospitalizations in average. The established recommendations suggested optimizing the time and to identify the main objectives for carrying out early hospital discharges (Bartolo et al., 2020). However, even in this specific situation, the available data are insufficient and contrasting.
An approach followed by the neurorehabilitation services to compensate for the interruption of outpatient therapies was to implement telerehabilitation services. In this way, neurorehabilitation facilities were able to reorganize in a timely manner the treatments of patients with neurological diseases (Assenza et al., 2021). Telerehabilitation has been assessed with a positive impact, in terms of satisfaction and positive perception by the treated population. However, the lack of adequate training and the sudden activation of an unknown treatment method may increase skepticism about the actual benefit of this approach in improving the therapeutic objectives (Bettger et al., 2020). Further, in the current research only two articles were evaluated on this subject, for this reason, the results cannot be generalized to the whole population with neurological pathologies, the latter being so heterogeneous. Altogether, telerehabilitation could be suggested as an alternative method to facilitate therapy timeframes and continuity of care, not only during a health emergency but also in everyday life. But before adopting this method, some considerations must be followed: its pros and cons, its acceptance, availability of technological resources and availability of the caregiver, if required (Klaic & Galea, 2020).
The repercussions of COVID-19 at the beginning of the pandemic were not only on healthcare workers and patients but also on their caregivers. For healthcare professionals, the spread of the virus had a strong impact. Higher levels of stress, anxiety and depression have been reported on healthcare professionals who assisted COVID-19 patients (Gray et al., 2019). Moreover, the interruption of the patients’ neurorehabilitative activities has also resulted in decreased independence, an increased need for care and have worsened the perception of symptoms (Assenza et al., 2021; Santamato et al., 2021; Summaka et al., 2021; Yogev-Seligmann & Kafri, 2021). In addition, the restrictions imposed on visitors to access the rehabilitation facilities have generated concern and uncertainty in all caregivers. Consequently, caregivers have expressed the feeling of being unprepared and not competent to manage the patient at home (Sutter-Leve et al., 2021). On account of the data being extrapolated from various studies based on self-reported perceptions, the responses can be influenced by social or personal aspects of the participants (Assenza et al., 2021; Manacorda et al., 2021; Santamato et al., 2021; Summaka et al., 2021; Yogev-Seligmann & Kafri, 2021).
Regarding the psychological consequences on the affected population during the COVID-19 pandemic, high increases of emotional distress have been reported. Particularly, the constant checks for symptoms and infection policies aggravated the general anxiety in the population (World Health Organization Regional Office for Europe, 2020). The main source of psychological burden was primarily the fear of being infected, and secondly to become a vehicle for the transmission of the virus (Kisely et al., 2020). The feeling of emotional exhaustion and emptiness during an emergency has been highly exacerbated in the working environment, increasing the risk of burnout (Lasalvia et al., 2021) and pathological depersonalization (Farí et al., 2022). In general, it has been reported that all patients demonstrated good resilience resources (Dalise et al., 2021), but specifically, fragile patients were found to be more susceptible to psychological distress (Dalise et al., 2021; Manacorda et al., 2021; Santamato et al., 2021; Summaka et al., 2021; Yogev-Seligmann & Kafri, 2021). However, there is no available information on the patients’ psychological status before the pandemic.
Lastly, communication coping strategies were crucial on the neurorehabilitation services during COVID-19. During the beginning of the pandemic, caregivers faced several communication challenges. Specifically, when reaching the neurorehabilitation team, to ask for updates on the health status of their loved ones. And often perceived themselves as an extra burden to the members of the care team (Sutter-Leve et al., 2021). In response, the neurorehabilitation services put in practice the suggestions given by caregivers and scheduled phone calls, video conferences and recorded videos to compensate for this gap. Furthermore, to show the way in which therapy sessions were performed, and to provide a view of the gained progress (Sutter-Leve et al., 2021). Another important factor that remained essential during inpatient neurorehabilitation care, was the help given by friends and family members (Hanson et al., 2019). During the lockdown, a decrease in medical and rehabilitation support was related to poor judgment on the positive aspects of caregiving (Assenza et al., 2021).
5Study limitations
This scoping review presents several limitations. Firstly, all the above studies were observational designs based on surveys and questionnaires. Secondly, the variability and the heterogeneity of the reported interventions did not allow a comparison among the groups and limit the evaluation effectiveness of the interventions. Primary research regarding the unexpected impact of COVID-19 on the effectiveness of the strategies adopted by the neurorehabilitation services still currently lacking. Hence, the current scoping review has included studies in which modifications have been reported regarding the impact of the pandemic on rehabilitation settings as a secondary outcome.
6Conclusions
The unforeseen impact of the COVID-19 pandemic on neurorehabilitation services has profoundly altered its organization and therapeutic strategies. Consequently, therapeutic interventions during the first wave were remodeled to identify short-term achievable goals while reducing the risk of spreading the virus. Implementation of home remote assistance and training through information technologies was fundamental for healthcare professionals, patients, and caregivers. The latter, being of utmost importance in healthcare, specifically when patients became ready for hospital discharge; in cases where patients were unable to access outpatient rehabilitation services; or when consulting the patient’s status or achieved progress.
Future studies should investigate the potential of telerehabilitation applicability, not only during health emergencies, but also as a tool for monitoring patient and caregiver compliance, and strengthening patient and caregiver support networks. Specifically, studies monitoring the impact of the successive waves of COVID-19 on healthcare professionals, caregivers, and patients are needed.
Conflict of interest
The authors declare that there is no conflict of interest.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Funding
The authors report no financial support.
References
1 | Assenza, C. , Catania, H. , Antenore, C. , Gobbetti, T. , Gentili, P. , Paolucci, S. , Morelli, D. ((2021) ). Continuity of Care During COVID-19 Lockdown: A Survey on Stakeholders’ Experiencen With Telerehabilitation. Frontiers in Neurology, 11: (January), 1–10. https://doi.org/10.3389/fneur.2020.617276 |
2 | Bartolo, M. , Intiso, D. , Lentino, C. , Sandrini, G. , Paolucci, S. , Zampolini, M. , Alfonsi, E. , Antonucci, G. , Baricich, A. , Casu, G. , Ciancarelli, I. , Cisari, C. , De Tanti, A. , Estraneo, A. , Ferraro, F. , Gandolfi, M. , Invernizzi, M. , Iolascon, G. , Martinuzzi, A. ,. . . Trompetto, C. ((2020) ). Urgent Measures for the Containment of the Coronavirus (Covid-19) Epidemic in the Neurorehabil itation/Rehabilitation Departments in the Phase of Maximum Expansion of the Epidemic. Frontiers in Neurology, 11: (April), 1–6 https://doi.org/10.3389/fneur.2020.00423 |
3 | Bettger, J.P. , Thoumi, A. , Marquevich, V. , De Groote, W. , Rizzo Battistella, L. , Imamura, M. , Delgado Ramos, V. , Wang, N. , Dreinhoefer, K. E. , Mangar, A. , Ghandi, D. B. C. , Ng, Y.S. , Lee, K. H. , Tan Wei Ming, J. , Pua, Y.H. , Inzitari, M. , Mmbaga, B. T. , Shayo, M. J. , Brown, D. A. ,. . . Stein, J. ((2020) ). COVID-19: Maintaining essential rehabilitation services across the care continuum. BMJ Global Health,5: (5), 1–7. https://doi.org/10.1136/bmjgh-2020-002670 |
4 | Caltagirone, C. , Piras, F. , & Imbriani, P. (20221). Handbook of Neurorehabilitation and Principles of Neurology. Giunti Psychometrics. |
5 | Dalise, S. , Tramonti, F. , Armienti, E. , Niccolini, V. , Caniglia-Tenaglia, M. , Morganti, R. , & Chisari, C. ((2021) ). Psycho-social impact of social distancing and isolation due to the coVid-19 containment measures on patients with physical disabilities. European Journal of Physical and Rehabilitation Medicine, 57: (1), 158–165. https://doi.org/10.23736/S1973-9087.20.06535-1 |
6 | Dobson, A. P. , & Carper, E. R. ((1996) ). Infectious Diseases and Human population History, BioScience 46: (2), 115–126. |
7 | Farí, G. , de Sire, A. , Giorgio, V. , Rizzo, L. , Bruni, A. , Bianchi, F. P. , Zonno, A. , Pierucci, P. , Ranieri, M. , & Megna, M. ((2022) ). Impact of COVID-19 on the mental health in a cohort of Italian rehabilitation healthcareworkers. Journal of Medical Virology 94: (1), 110–118 https://doi.org/10.1002/jmv.27272 |
8 | Gorini, A. , Fiabane, E. , Sommaruga, M. , Barbieri, S. , Sottotetti, F. , La Rovere, M. T. , Tremoli, E. , & Gabanelli, P. ((2020) ). Mental health and risk perception among Italian healthcare workers during the second month of theCovid-19 pandemic. Archives of Psychiatric Nursing 34: (6), 537–544. https://doi.org/10.1016/j.apnu.2020.10.007 |
9 | Gray, P. , Senabe, S. , Naicker, N. , Kgalamono, S. , Yassi, A. , & Spiegel, J. M. ((2019) ). Workplace-based organizational interventions promoting mental health and happiness among healthcare workers: A realist review. International Journal of Environmental Research and Public Health, 16: (22). https://doi.org/10.3390/ijerph16224396 |
10 | Hanson, K. T. , Carlson, K. F. , Friedemann-Sanchez, G. , Meis, L. A. , Van Houtven, C. H. , Jensen, A. C. , Phelan, S. M. , & Griffin, J. M. ((2019) ). Family caregiver satisfaction with inpatient rehabilitation care. PLoS ONE 14: (3), 1–13. https://doi.org/10.1371/journal.pone.0213767 |
11 | Iosa, M. , Morone, G. , Antonucci, G. , & Paolucci, S. ((2021) ). Prognostic factors in neurorehabilitation of stroke: A comparison among regression, neural network, and cluster analyses. Brain Sciences, Brain Sciences 11: (9). https://doi.org/10.3390/brainsci11091147 |
12 | Khan Khan Fary , Amatya Bhasker , Mannan Hasheem , & Rathore Farooq Azam . ((2015) ). Neurorehabilitation in Developing Countries: Challenges and the Way Forward, Phys Med Rehabil Int 2: (9), 1–13. |
13 | Kim, A. , Yun, S. J. , Sung, K. S. , Kim, Y. , Jo, J. Y. , Cho, H. , Park, K. , Oh, B. M. , & Seo, H. G. ((2021) ). Exercise management using a mobile app in patients with parkinsonism: Prospec-tive, open-label, single-arm pilot study. JMIR MHealth and UHealth 9: (8), 1–12. https://doi.org/10.2196/27662 |
14 | Kisely, S. , Warren, N. , McMahon, L. , Dalais, C. , Henry, I. , & Siskind, D. ((2020) ). Occurrence, prevention, and manage- ment of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ (Clinical Research Ed.) 369: , 1642–. https://doi.org/10.1136/bmj.m1642 |
15 | Klaic, M. , & Galea, M. P. ((2020) ). Using the Technology Accep- tance Model to Identify Factors That Predict Likelihood to Adopt Tele-Neurorehabilitation. Frontiers in Neurology 11: (December). https://doi.org/10.3389/fneur.2020.580832 |
16 | Lasalvia, A. , Amaddeo, F. , Porru, S. , Carta, A. , Tardivo, S. , Bovo, C. , Ruggeri, M. , & Bonetto, C. ((2021) ). Levels of burn-out among healthcare workers during the COVID-19 pandemic and their associated factors: A cross-sectional study in a ter- tiary hospital of a highly burdened area of north-east Italy. BMJ Open 11: (1), 1–12. https://doi.org/10.1136/bmjopen-2020-045127 |
17 | Lazzerini, M. , & Putoto, G. ((2020) ). COVID-19 in Italy: momen-tous decisions and many uncertainties. The Lancet Global Health, 8: (5), e641–e642. https://doi.org/10.1016/S2214-109X(20)30110-8 |
18 | Lee, J. J. , Tsang, W. N. , Yang, S. C. , Kwok, J. Y. Y. , Lou, V. W. Q. , & Lau, K. K. (2021). Qualitative Study of Chinese Stroke Caregivers’ Caregiving Experience during the COVID-19 Pandemic. Stroke, April, 1407-1414. https://doi.org/10.1161/STROKEAHA.120.032250 |
19 | Leocani, L. , Diserens, K. , Moccia, M. , & Caltagirone, C. ((2020) ). Disability through COVID-19 pandemic: neurorehabilitation cannot wait. European Journal of Neurology 27: (9), e50–e51. https://doi.org/10.1111/ene.14320 |
20 | Maccarone, M. C. , & Masiero, S. ((2021) ). The Important Impact of COVID-19 Pandemic on the Reorganization of a Rehabilitation Unit in a National Healthcare System Hospital in Italy: Lessons 601 From Our Experience. American Journal of Physical Medicine & Rehabilitation 100: (4), 327–330. https://doi.org/10.1097/PHM.0000000000001707 |
21 | Manacorda, T. , Bandiera, P. , Terzuoli, F. , Ponzio, M. , Brichetto, G. , Zaratin, P. , Bezzini, D. , & Battaglia, M. A. ((2021) ). Impact of the COVID-19 pandemic on persons with multiple sclero- sis: Early findings from a survey on disruptions in care and self-reported outcomes. Journal of Health Services Research and Policy 26: (3), 189–197. https://doi.org/10.1177/1355819620975069 |
22 | Peters, M. D. J. , Marnie, C. , Tricco, A. C. , Pollock, D. , Munn, Z. , Alexander, L. , McInerney, P. , Godfrey, C. M. , & Khalil, H. ((2020) ). Updated methodological guidance for the conduct of scoping reviews.JBI Evidence Synthesis 18: (10), 2119–2126. https://doi.org/10.11124/JBIES-20-00167 |
23 | Salvia, A. , Morone, G. , Iosa, M. , Balice, M. P. , Paolucci, S. , Grasso, M. G. , Traballesi, M. , Nocentini, U. , Formisano, R. , Molinari, M. , Rossini, A. , & Caltagirone, C. ((2020) ). An Italian Neu rorehabilitation Hospital Facing the SARS-CoV-2 Pandemic: Data From 1207 Patients andWorkers. Frontiers in Neurology 11: (October), 1–7. https://doi.org/10.3389/fneur.2020.584317 |
24 | Santamato, A. , Facciorusso, S. , Spina, S. , Cinone, N. , Avvantaggiato, C. , Santoro, L. , Ciritella, C. , Smania, N. , Picelli, A. , Gasperini, G. , Molteni, F. , Baricich, A. , & Fiore, P. ((2021) ). Discontinuation of botulinum neurotoxin type-A treatment during COVID-19 pandemic: An Italian survey in post stroke and traumatic brain injury patients living with spasticity. European Journal of Physical and Rehabilitation Medicine 57: (3), 424–433. https://doi.org/10.23736/S1973-9087.20.06478-3 |
25 | Spielmanns, M. , Pekacka-Egli, A. M. , Cecon, M. , Witassek, F. , Schoendorf, S. , Lutz, D. , & Hermann, M. ((2021) ). COVID-19 Outbreak During Inpatient Rehabilitation: Impact on Settings and Clinical Course of Neuromusculoskeletal Rehabilitation Patients. American Journal of Physical Medicine & Rehabilitation, 100: (3), 203–208. https://doi.org/10.1097/PHM.0000000000001686 |
26 | Summaka, M. , Zein, H. , Naim, I. , & Fneish, S. ((2021) ). Assess ing the psychological impact of COVID-19 outbreak and its related factors on Lebanese individuals with physical disabilities. Disability and Health Journal 14: (3), 101073. https://doi.org/10.1016/j.dhjo.2021.101073 |
27 | Sutter-Leve, R. , Passint, E. , Ness, D. , & Rindflesch, A. ((2021) ). The caregiver experience after stroke in a covid-19 environment: A qualitative study in inpatient rehabilitation. Journal of Neurologic Physical Therapy 45: (1), 14–20. https://doi.org/10.1097/NPT.0000000000000336 |
28 | Treger, I. , Lutsky Treger, L. , & Friedman, A. ((2020) ). Organization of acute patients’ transfer to rehabilitation services during coVid-19 crisis.European Journal of Physical and Rehabilitation Medicine 56: (3). https://doi.org/10.23736/S1973-9087.20.06324-8 |
29 | Veerbeek, J. M. , Van Wegen, E. , Van Peppen, R. , Van Der Wees, P. J. , Hendriks, E. , Rietberg, M. , & Kwakkel, G. ((2014) ). What is the evidence for physical therapy poststroke? A systematic review and meta-analysis. PLoS ONE 9: (2). https://doi.org/10.1371/journal.pone.0087987 |
30 | World Health Organization. (2020a). Ensuring A Safe Environment For Patients And Staff In COVID-19 Health-Care Facilities (Issue October). https://apps.who.int/iris/bitstream/handle/10665/336257/WHO-2019-nCoV-HCF_assessment-Safe_environment-2020.1-eng.pdf?sequence=1&isAllowed=y |
31 | World Health Organization. (2020b). Operational Planning Guidelines to Support Country Preparedness and Response. https://www.who.int/publications/i/item/draft-operational-planning-guidance-for-un-country-teams |
32 | World Health Organization. (2021a). Considerations for imple-menting and adjusting public health and social measures in the context of COVID-19: interim guidance (Issue June). https://www.who.int/publications/i/item/considerations-in-adjusting-public-health-and-social-measures-in-the-context-of-covid-19-interim-guidance |
33 | World Health Organization. (2021b). Looking back at a year that changed the world: WHO’s response to COVID-19 (Issue January). https://www.who.int/publications/m/item/looking-back-at-a-year-that-changed-the-world-who-s-response-to-covid-19 |
34 | World Health Organization Regional Office for Europe. (2020). Long-stay mental health care institutions and the COVID-19 crisis: identifying and addressing the challenges for better response and preparedness. https://www.euro.who.int/en/health-topics/noncommunicable-diseases/mental-health/publications/2020/long-stay-mental-health-care-institutions-and-the-covid-19-crisis-identifying-and-addressing-the-challenges-for-better-response-and-preparedness-2020 |
35 | Yogev-Seligmann, G. , & Kafri, M. ((2021) ). COVID-19 social dis-tancing: negative effects on people with Parkinson disease and their associations with confidence for self-management. BMC Neurology 21: (1), 1–8. https://doi.org/10.1186/s12883-021-02313-6 |
Appendices
Appendix: Search terms for the databases
Search strategy in MEDLINE/PubMed:
(((((“coronavirus” [MeSH Terms] OR “coronavirus” [All Fields] OR “coronaviruses” [All Fields] OR (“covid 19” [All Fields] OR “covid 19” [MeSH Terms] OR “covid 19 vaccines” [All Fields] OR “covid 19 vaccines” [MeSH Terms] OR “covid 19 serotherapy” [All Fields] OR “covid 19 serotherapy” [Supplementary Concept] OR “covid 19 nucleic acid testing” [All Fields] OR “covid 19 nucleic acid testing” [MeSH Terms] OR “covid 19 serological testing” [All Fields] OR “covid 19 serological testing” [MeSH Terms] OR “covid 19 testing” [All Fields] OR “covid 19 testing” [MeSH Terms] OR “sars cov 2” [All Fields] OR “sars cov 2” [MeSH Terms] OR “severe acute respiratory syndrome coronavirus 2” [All Fields] OR “ncov” [All Fields] OR “2019 ncov” [All Fields] OR ((“coronavirus” [MeSH Terms] OR “coronavirus” [All Fields] OR “cov” [All Fields]) AND 2019/11/01:3000/12/31[Date - Publication])) OR (“sars cov 2” [MeSH Terms] OR “sars cov 2” [All Fields] OR “sars cov 2” [All Fields])) AND ((“neurologic manifestations” [MeSH Terms] OR (“neurologic” [All Fields] AND “manifestations” [All Fields]) OR “neurologic manifestations” [All Fields] OR “neurologic” [All Fields] OR “nervous system” [MeSH Terms] OR (“nervous” [All Fields] AND “system” [All Fields]) OR “nervous system” [All Fields] OR “neurological” [All Fields] OR “neurologically” [All Fields]) AND “disease*” [All Fields])) OR ((“neurologic manifestations” [MeSH Terms] OR (“neurologic” [All Fields] AND “manifestations” [All Fields]) OR “neurologic manifestations” [All Fields] OR “neurologic” [All Fields] OR “nervous system” [MeSH Terms] OR (“nervous” [All Fields] AND “system” [All Fields]) OR “nervous system” [All Fields] OR “neurological” [All Fields] OR “neurologically” [All Fields]) AND “disorder*” [All Fields])) AND (“rehabilitant” [All Fields] OR “rehabilitants” [All Fields] OR “rehabilitate” [All Fields] OR “rehabilitated” [All Fields] OR “rehabilitates” [All Fields] OR “rehabilitating” [All Fields] OR “rehabilitation” [MeSH Terms] OR “rehabilitation” [All Fields] OR “rehabilitations” [All Fields] OR “rehabilitative” [All Fields] OR “rehabilitation” [MeSH Subheading] OR “rehabilitation s” [All Fields] OR “rehabilitational” [All Fields] OR “rehabilitator” [All Fields] OR “rehabilitators” [All Fields])) OR (“neurological rehabilitation” [MeSH Terms] OR (“neurological” [All Fields] AND “rehabilitation” [All Fields]) OR “neurological rehabilitation” [All Fields] OR “neurorehabilitation” [All Fields] OR “neurorehabilitative” [All Fields])) AND (“manage” [All Fields] OR “managed” [All Fields] OR “management s” [All Fields] OR “managements” [All Fields] OR “manager” [All Fields] OR “manager s” [All Fields] OR “managers” [All Fields] OR “manages” [All Fields] OR “managing” [All Fields] OR “managment” [All Fields] OR “organization and administration” [MeSH Terms] OR (“organization” [All Fields] AND “administration” [All Fields]) OR “organization and administration” [All Fields] OR “management” [All Fields] OR “disease management” [MeSH Terms] OR (”disease” [All Fields] AND “management” [All Fields]) OR “disease management” [All Fields])
Search strategy in the WHO COVID-19 database:
‘SARS-CoV-2’ OR ‘COVID-19’
‘COVID-19’ AND neurological disease* OR neurological disorder*




