Improving the delivery of acute NIV at Kings Mill Hospital: A closed loop quality improvement project
Abstract
BACKGROUND:
The British Thoracic Society (BTS) Acute Non-Invasive Ventilation (NIV) standards state all patients who require acute NIV should be initiated on NIV within two hours of hospital admission. The delivery of acute NIV is a time critical intervention as prompt application of acute NIV substantially reduces mortality for patients with acute hypercapnic respiratory failure.
OBJECTIVE:
This audit aimed to assess the number of patients for whom there is a delay in the initiation of acute NIV. We also assessed the outcome of admission for patients started on acute NIV.
METHODS:
Data was collected on patients admitted to Kings Mill Hospital for acute NIV between 1/2/2019 and 31/3/2019. Awareness and knowledge of acute NIV was highlighted as an area for improvement. E-learning packages on ‘Acute NIV’ were designed and sent to medical-staff. The audit was repeated for patients admitted for acute NIV between 1/2/2020 and 31/3/2020 and analysed using chi-square tests.
RESULTS:
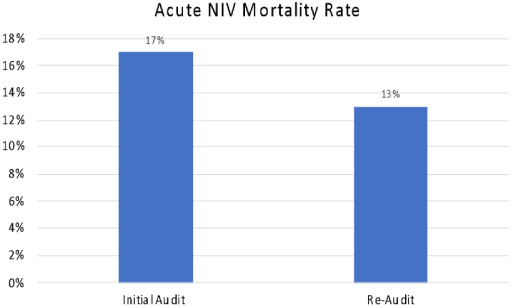
25 patients were included in the initial audit and 30 patients in the re-audit. Prior to intervention 31% of patients had a delay in the initiation of acute NIV, which increased to 77% post-intervention (p < 0.0001). Prior to intervention there was a mortality rate of 17% and a mortality rate of 13% post-intervention (p > 0.05).
CONCLUSION:
Further work is required to ensure the sustained delivery of acute NIV to BTS standards, however variable achievements in the targets does not seem to have a significant adverse effect on patient outcomes.
1.Background
Acute hypercapnic respiratory failure (AHRF) occurs when there is insufficient alveolar ventilation to maintain a normal arterial pCO2 and can lead to acute respiratory acidosis [1]. Acute respiratory acidosis is conventionally defined as a pH < 7.35 and pCO2 > 6.5 kPa. If acute respiratory acidosis persists following 30 min of optimal medical therapy, then these values are used as a threshold for considering the use of acute NIV [1].
Acute non-invasive ventilation (NIV) was first recommended by the BTS in response to trials which demonstrated that acute NIV delivered improved patient outcomes compared to invasive mechanical ventilation in the treatment of acute respiratory acidosis secondary to acute exacerbations of AECOPD [1,2]. These trials also illustrated the feasibility of delivering acute NIV in emergency departments, admissions wards or even general medical wards with adequate staff training and specialist support [3]. NICE guidance for COPD has recommended that all hospitals admitting patients with AECOPD have acute NIV available, with acute hospitals establishing dedicated services to deliver this treatment [4].
Unfortunately, national audits have repeatedly raised concerns that benefits shown in trials are not translating into real clinical practice [1]. The British Thoracic Society (BTS) has found overall mortality rates in patients started on acute NIV are increasing and also finding significant regional variations in patient outcomes [4]. The National Confidential Enquiry into Patient Outcome and Death (NCEPOD) analysed data of 432 patients treated with acute NIV to identify how acute NIV treatment could be improved and published their findings in the ‘Inspiring Change’ study [4]. These findings informed the BTS Quality Standards for Acute NIV in Adults [5]. Quality Statement 4 of these standards focussed upon the timely delivery of acute NIV: ‘Patients who meet evidence-based criteria for acute NIV should start NIV within 60 min of the blood gas result associated with the clinical decision to provide NIV and within 120 min of hospital arrival for patients who present acutely [5]’. Prompt delivery of acute NIV in patients with AHRF reduces patient mortality as treatment delay can lead to worsening acidosis, which is associated with a poorer outcome [6]. The BTS recommends that when a blood gas is consistent with AHRF and respiratory acidosis, patients should receive 30 min of standard medical therapy [7]. If AHRF and respiratory acidosis persist, then acute NIV with targeted oxygen therapy should be initiated without delay [5]. The target time limits set out in Quality Statement 4 aims to highlight that recognition and correct management of AHRF are time critical events. The BTS considers these targets to allow sufficient time for triage, blood gas, clinical review, medical management and planning for acute NIV [5,8]. This quality improvement project therefore aims to evaluate the performance of Kings Mill Hospital against Quality Statement 4.
2.Objective
The British Thoracic Society (BTS) Acute Non-Invasive Ventilation (NIV) standards state all patients who require acute NIV should be initiated on NIV within 120 minute of hospital admission [5]. The delivery of acute NIV is a time critical intervention as prompt application of acute NIV substantially reduces the mortality for patients with AHRF [9].
This quality improvement project (QIP) therefore sought to achieve the following aims:
To assess and improve the timely delivery of acute NIV.
To assess the outcome of admission for patients who are started on acute NIV.
Using guidance from the British Thoracic Society, the following criteria was established in order to assess the timely delivery of acute NIV [5]:
All patients meeting evidence-based criteria for acute NIV and treated with acute NIV, their first blood gas measurement is performed within 60 min of hospital arrival.
All patients meeting evidence-based criteria for acute NIV are treated with acute NIV within 60 min of the blood gas result associated with the clinical decision to provide NIV.
All patients meeting evidence-based criteria for acute NIV are treated with acute NIV within 120 min of hospital arrival.
A delay in any of these 3 criteria will be classified as a delay in the timely delivery of acute NIV.
Data was collected retrospectively, with cases defined as patients treated with acute NIV for AHRF. The audit period for the first audit cycle included patients admitted to Kings Mill Hospital between 1st February 2019 and 31st March 2019 and the audit period for the second cycle included patients admitted between 1st February 2020 and 31st March 2020. Patients under the age of 18, treated with continuous positive airways pressure (CPAP), <48 hours post extubation or required NIV later on in admission were excluded from the project.
3.Methods
At Kings Mill Hospital there is already a dedicated acute NIV service in which acute NIV can be initiated in the emergency department prior to transfer to the respiratory wards. In order to improve the quality of care, we aimed to focus on the timely delivery of acute NIV. An important factor in achieving this is to improve standards in the emergency department where recognition of the need for acute NIV takes place. Our intervention focused upon education of staff in the emergency department. Specialist e-learning packages on ‘Acute NIV’ and ‘Adult Oxygen Therapy’ were designed and sent to all medical and nursing staff working in the emergency department and in acute medicine. The electronic nature of this teaching reduces barriers to access and allows medical staff flexibility in terms of when it is accessed and the opportunity to revisit the modules at their convenience. A poor uptake of the e-learning packages was an anticipated issue. In response, we planned for acute NIV leads to send out regular email reminders of the need for staff to complete this training.
Data was collected retrospectively from patient medical records. A list of all patients initiated on NIV during the data collection periods was obtained from the NIV ward at Kings Mill Hospital and patient medical notes were requested. Relevant measures were then obtained from patient medical records and documented on specially designed proformas. The measures recorded included: admission time, date of first pre NIV blood gas measurement, time of first pre NIV blood gas measurement, time NIV commenced, date NIV commenced, outcome of admission and patient demographics. See SMART Aims for study dates, inclusion criteria and exclusion criteria.
4.Results
25 and 30 patients were included in the first and second audit cycles respectively. In the first audit cycle 12 (48%) patients were male and had a mean age of 75. In the second audit cycle 10 (33%) patients were male and had a mean age of 69. Prior to intervention, 8 (32%) patients had a delay in the delivery of acute NIV and this increased to 23 (77%) patients post intervention (p < 0.0001) (see Fig. 1). Prior to intervention 4 (17%) patients died whilst in hospital and post intervention 4 (13%) patients died whilst in hospital (see Fig. 2).
Fig. 1.
A bar chart to show the proportion of patients who had a delay in the delivery of acute NIV in the initial and the re-audit.
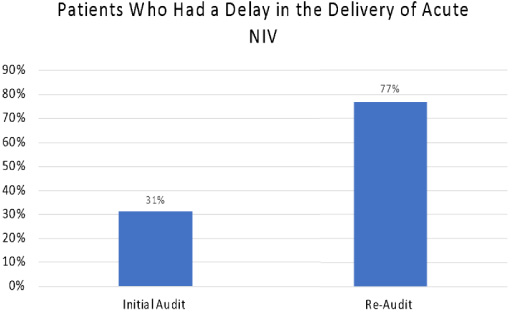
Fig. 2.
A bar chart to show the mortality rate amongst patients initiated on acute NIV in the initial and the re-audit.
From these figures, it is clear to see there was a significant increase in the number of patients who had a delay in the delivery of acute NIV following the implementation of e-learning packages. It is highly unlikely that delivery of e-learning packages caused this increased delay. An important confounding factor which cannot be ignored is the impact of the coronavirus pandemic on the timely delivery of acute NIV. The later part of the second audit cycle period coincided with the first wave of the UK coronavirus pandemic. The following factors therefore may have adversely impacted the timely delivery of acute NIV: increased patient numbers attending the emergency department; reduced ability to provide NIV due to increased personal protective equipment requirements for aerosol generating procedures, staff sickness and failure to recognise the need for acute NIV.
5.Conclusion
From the data we have presented, it is clear further work is needed to improve the timely delivery of acute NIV at Kings Mill Hospital. Well defined outcomes, strict criteria used for defining delay in acute NIV, clear inclusion/exclusion criteria and controlling for seasonal variation are strengths of our project design. The small sample sizes are a weakness of this quality improvement project, however significance calculations are still valid. Although lack of education into NIV was legitimately identified as an area for improvement following the first audit cycle there are likely multiple other factors which require addressing and further work is required. Firstly, we need to be sure that education is an area for improvement that has been adequately addressed. In future work it would be beneficial to understand the proportion of clinical staff who have actually completed the e-learning modules and then work to increase this proportion. Additionally, we had a very strict 3 rule criteria for defining if a patient had a delay in delivery of acute NIV. Further work to identify at which stages the delays occur, whether that be admission to gas time, gas to mask time or a combination would help to identify areas for improvement. Finally, it is possible that patients may have only had a slight delay in the delivery of acute NIV and that this delay was negligible in terms of affecting outcomes. Reassuringly however, the observed increase in acute NIV delay did not lead to an observed increase in mortality.
Conflict of interest
None to report.
References
[1] | Davidson AC, Banham S, Elliott M, Kennedy D, Gelder C, Glossop A BTS/ICS guideline for the ventilatory management of acute hypercapnic respiratory failure in adults. Thorax. (2016) ;71: (Suppl 2):ii1–ii35. |
[2] | Guideline B. Non-invasive ventilation in acute respiratory failure. Thorax. (2002) ;57: (3):192–211. |
[3] | Plant PK, Owen JL, Elliott MW. One year period prevalence study of respiratory acidosis in acute exacerbations of COPD: implications for the provision of non-invasive ventilation and oxygen administration. Thorax. (2000) ;55: (7):550–4. |
[4] | Juniper MC, Ellis G, Protopapa KL, Smith N. Inspiring Change: A report on acute non-invasive ventilation. Br J Hosp Med. (2017) ;78: (9):497–502. |
[5] | Davies M, Allen M, Bentley A, Bourke SC, Creagh-Brown B, D’Oliveiro R British Thoracic Society Quality Standards for acute non-invasive ventilation in adults. BMJ Open Respiratory Research. (2018) ;5: (1). |
[6] | Lightowler JV, Wedzicha JA, Elliott MW, Ram FS. Non-invasive positive pressure ventilation to treat respiratory failure resulting from exacerbations of chronic obstructive pulmonary disease: Cochrane systematic review and meta-analysis. BMJ. (2003) ;326: (7382):185. |
[7] | Roberts CM, Stone RA, Buckingham RJ, Pursey NA, Lowe D. Acidosis, non-invasive ventilation and mortality in hospitalised COPD exacerbations. Thorax. (2011) ;66: (1):43–8. |
[8] | O’driscoll BR, Howard LS, Earis J, Mak V. BTS guideline for oxygen use in adults in healthcare and emergency settings. Thorax. (2017) ;72: (Suppl 1):ii1–ii90. |
[9] | Davies MG, Juniper MC. Lessons learnt from the National confidential enquiry into patient outcome and death: Acute non-invasive ventilation. Thorax. (2018) ;73: (10):904–7. |




