Improving the visibility and communication of treatment escalation plans in Somerset NHS foundation trust
Abstract
BACKGROUND:
Advance care treatment escalation plans (TEPs) are often lost between healthcare settings, leading to duplication of work and loss of patient autonomy.
OBJECTIVE:
This quality improvement project reviewed the usage of TEP forms and aimed to improve completeness of documentation and visibility between admissions.
METHODS:
Over four months we monitored TEP form documentation using a standardised data extraction form. This examined section completion, seniority of documenting clinician and transfer of forms to our hospital electronic patient record (EPRO). We added reminders to computer monitors on wards to improve EPRO upload.
RESULTS:
Initial data demonstrated that 95% of patients (n = 230) had a TEP, with 99% of TEPs recording resuscitation status. However, other sections were not well documented (patient capacity 57% completion and personal priorities 45% completion, respectively). Only 11.9% of TEPs documented consultant involvement. Furthermore, only 44% of TEPs with a do not attempt resuscitation (DNACPR) decision were uploaded. Following this, we added reminders to computer monitors explaining how to upload TEP decisions to EPRO, which increased EPRO uploads to 74%.
CONCLUSION:
Communication of TEPs needs improving across healthcare settings. This project showed that the use of a physical reminder can greatly improve communication of treatment escalation decisions. Furthermore, this intervention has inspired future projects aiming at making communication more sustainable through the use of discharge summaries.
1.Background
Treatment escalation plans (TEPs) document the discussion and agreement with a patient about appropriate ceilings of care, including DNACPR decisions. These are widely used across the NHS in keeping with national guidance [1].
The NCEPOD report ‘Time to Intervene’ identified multiple cases in which patients were resuscitated beyond the level of care agreed in their TEP form [2]. This is not only harmful to the patient but can be distressing for loved ones. Poor documentation of TEPs, lack of communication between healthcare providers and poor visibility of these decisions across primary and secondary care all contribute towards inappropriate resuscitation of patients [2,3]. The COVID-19 CQC ‘Protect, Respect, Connect’ identified the need for comprehensive documentation of TEPs across integrated care systems [3]. National guidance states that it is the health care professional responsible for a DNACPR decision who is responsible for ensuring this is communicated effectively to other healthcare staff, both in primary and secondary care [1]. There is currently no national guidance over how this can be achieved with great variability between Trusts across the UK [4].
Previous local projects have increased the proportion of inpatients with appropriate TEPs, making it a mandatory part of admission clerking, improved the formatting of the TEP form itself and educated the public on the importance and benefits of an appropriate TEP [5–8].
2.Objective
TEPs are currently completed on paper and, ideally, the original is given to the patient on discharge. These are often lost and inpatient paper notes are not readily available, so not immediately visible on subsequent admissions. Our aim was for all TEPs to be uploaded onto the hospital electronic records alert system (EPRO) by June 2020, improving accessibility to those involved with patient care across the Trust, including on re-admission. This reduces the risk of iatrogenic harm and improves patient autonomy, whilst also preventing duplication of work and the risk of litigation.
3.Methods
This project was junior doctor-led, conducted at Somerset NHS Foundation Trust. To inform our first PDSA cycle, we completed a pre-intervention audit looking into the proportion of patients with TEP forms, whether capacity was documented, seniority of the doctors endorsing TEPs and proportion of TEPs uploaded onto EPRO. From these data we produced a driver diagram and identified interventions.
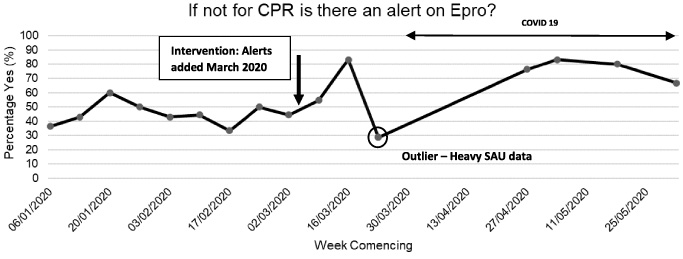
We sent out multiple emails to junior doctors across the trust and stuck alert stickers onto all ward computers used by doctors, prompting them to upload TEPs on to EPRO and explaining how to do so. To track our improvements, we set up a run chart (Fig. 1) where we randomly sampled 10-20 patients each week, recording the same data collection fields previously sampled in our pre-intervention audit. Upon completion of this intervention, we presented our data to Trust executives to increase awareness of the problem and increase support for our second PDSA cycle by including TEPs in discharge summaries and developing an electronic version of the form and automatic upload to GP electronic records. This second cycle is currently ongoing and beyond the scope of this paper, but we hope will encourage lasting and more sustainable improvement.
Fig. 1.
Run diagram of patient’s TEP form sampling and upload to EPRO. Intervention of alerts and emails is denoted by arrow. Circled data point shows outlier influenced by heavy surgical admission data. COVID-19 pandemic is documented.
4.Results
In October 2019, we completed a preintervention audit of 230 inpatients. We found that the vast majority of patients had a TEP present in their notes (95.2%, n = 219∕230) and 99% of these forms indicated a clear decision regarding resuscitation. However, only 57% (n = 125∕217) of forms documented capacity, 45% (n = 98∕219) documented a patient’s priorities and only 11.9% (n = 26∕218) were signed or countersigned by a consultant. We also identified that only 44% of patients, in whom a DNACPR decision had been made, had this alert uploaded to EPRO.
We sampled TEP completion weekly, as demonstrated in Fig. 1 and made our intervention of email and desktop reminders in March 2020. Following this intervention, we saw an immediate increase in TEP uploads from approximately 45% to 80%. Unfortunately, our post-intervention data were skewed by one sample taken from the surgical admissions unit (SAU) in the week of the 23rd March 2020. However, this highlighted an area for more intensive intervention. With the mass redeployment of doctors during the COVID-19 pandemic, data collection was paused and only resumed in late April. Despite this pause, our intervention remained in place and we observed a continued increase in TEP uploads when data collection resumed. The total percentage of forms being uploaded to EPRO, excluding the outlying SAU data, increased from 44.9% (n = 83∕185) to 74% (n = 73∕98) post-intervention.
While collecting the data we observed problems with our interventions. Raising awareness about uploading TEPs onto EPRO only had an effect for a limited amount of time and the stickers on computers began to fall off. This may be why at the end of our data collection we observed a slight reduction in the number of uploads, indicating a need for a more sustainable solution.
5.Discussion
Like other projects, nearly all our TEPs indicate a clear decision about resuscitation status with capacity and patient priorities being poorly completed [7,9]. However, we are unaware of any project that has aimed to increase the visibility of DNACPR decisions within the hospital, with most focusing on improving documentation. Using a sticker in clinical areas with email follow up was a cheap and initially effective intervention. This increased the visibility of TEPs during that admission and on subsequent re-admissions. Whilst unable to quantify, increasing visibility for patients on re-admission is likely to improve patient safety and autonomy as well as reducing duplication of work.
A limitation of our study is that the COVID-19 pandemic occurred just after our intervention was instigated. The pandemic placed an enormous strain on critical care services and therefore clear decisions regarding escalation of care and resuscitation were required for all patients on admission. This likely influenced our results as increased significance was placed on visibility of DNACPR decisions during COVID-19.
Our project had a big impact on improving initial visibility of DNACPR decisions on Epro. However, as our email intervention became more distant, and our sticker reminders begin to fall off we saw Epro uploads fall. This highlights the need for a more sustainable solution. By presenting this project to the Trust executive team we have gained financial and political support for this project’s aims. To make TEP form upload more reliable it must be part of an automated system. One solution to this is including TEP forms as a mandatory part of discharge summaries. This would have the added benefit of improving communication of TEPs to primary care. Previous observational studies indicate up to 50% of patients with DNACPR decisions in place are discharged home, identifying the need for robust continuity of treatment escalation decisions [10]. Unfortunately, this is both a timely and financially costly process due to current IT system limitations, but by presenting our first PDSA cycle and drawing attention to the CQC need for comprehensive documentation of TEP decisions across integrated care systems, we hope future changes can have more lasting effects [3].
6.Conclusion
This project demonstrated that vital treatment escalation decisions are being inadequately communicated between healthcare settings. The use of a physical reminders can greatly improve communication of treatment escalation decisions but have limited time of impact. By completing this work, we have increased the profile of TEP communication which is leading to new projects with more sustainable solutions.
Conflict of interest
None to report.
References
[1] | BMA, Resus Council (UK), RCN. Decisions Relating to Cardiopulmonary Resuscitation, 3rd edn., 2016. |
[2] | National Confidential Enquiry into Patient Outcome and Death ‘Time to Intervene’, 2012. |
[3] | Quality Care Commission. Protect, respect, connect—decisions about living and dying well during COVID-19, 2020. |
[4] | Freeman K, Field RA, Perkins GD. Variation in local trust do not attempt cardiopulmonary resuscitation (DNACPR) policies: A review of 48 English healthcare trusts. BMJ Open. (2015) ;5: (1):e006517. doi:10.1136/bmjopen-2014-006517. PMID: 25586369; PMCID: PMC4298091. |
[5] | Dahill M, Powter L, Garland L, Mallett M, Nolan J. Improving documentation of treatment escalation decisions in acute care. BMJ Quality Improvement Reports. (2013) ;2: (1):u200617.w1077. |
[6] | Sayma M, Nowell G, O’Connor A, Clark G, Gaukroger A, Proctor D Improving the use of treatment escalation plans: A quality-improvement study. Postgraduate Medical Journal. (2018) ;94: (1113):404–10. |
[7] | Harkness M, Wanklyn P. Cardiopulmonary resuscitation: Capacity, discussion, and documentation. QJM. (2006) ;99: (10):683–90. doi:10.1093/qjmed/hcl095. Epub 2006 Sep 20. PMID: 16990292. |
[8] | Castle N, Owen R, Kenward G, Ineson N. Pre-printed ‘do not attempt resuscitation’ forms improve documentation? Resuscitation. (2003) ;59: (1):89–95. doi:10.1016/s0300-9572(03)00176-x. PMID: 14580738. |
[9] | Butler JV, Pooviah PK, Cunningham D, Hasan M. Improving decision-making and documentation relating to do not attempt resuscitation orders. Resuscitation. (2003) ;57: (2):139–44. doi:10.1016/s0300-9572(03)00029-7. PMID: 12745181. |
[10] | Fritz Zoë B McC, Heywood Richard M., Moffat Suzanne C, Bradshaw Lucy E, Fuld Jonathan P. Characteristics and outcome of patients with DNACPR orders in an acute hospital; an observational study. Resuscitation. (2014) ;85: (1):104–8, ISSN 0300-9572. |




