Impact of the COVID-19 pandemic on dispensing medicines in the community pharmacy
Abstract
BACKGROUND:
The world has faced an unprecedented challenge since COVID-19 emerged as a pandemic, which has led to quarantine and disruptions in drug services. During the pandemic, drug use habits and availability changed, causing a shift in behaviors and, in turn, medicine misuse. In Iraq, this is a major problem because many medicines can be easily obtained.
OBJECTIVE:
The study aims to describe the pattern of dispensing medications during the pandemic and to evaluate the biochemical and pathological consequences.
METHOD:
The analytical, observational, cross-sectional study was performed via a compiled questionnaire for 400 random pharmacists, and the analysis and interpretation of the biochemical changes and medical reports.
RESULTS:
Results revealed that dispensing of medications since the COVID-19 outbreak has increased by 74%, and the demand for medicines seems higher than required in comparison to the periods before the pandemic, while 60% of the dispensed medicines were taken just in case needed. In addition, the availability of medicines decreased by 61%, and the dispensing of common medicines increased due to the belief in their prophylactic action. Several biochemical abnormalities and pathological consequences were recorded due to the irrational use of medicines, and the highest percentage (12%) was seen in hepatic and liver enzymatic dysfunction and 8% for the endocrine and hormonal abnormalities.
CONCLUSION:
It can be concluded that most of the dispensed medicines were not used on a therapeutic or scientific basis during the pandemic.
1.Introduction
The world has faced an unprecedented challenge when coronavirus (COVID-19) emerged as a pandemic [1]. In comparison to Middle East respiratory syndrome (MERS) and severe acute respiratory syndrome (SARS), COVID-19 was the more rapidly spreading disease and in a short time became a pandemic. In January 2020, the World Health Organization (WHO) declared the outbreak as a Public Health Emergency of International Concern, and developed to new dimensions with a higher death ratio. This virus has put a massive burden on the healthcare system and a turning point for the initiation of a global health crisis of an unprecedented nature and scale [2]. The high potential of this extensive dissemination led to the quarantine of several cities in different countries.
Since the beginning of this pandemic, a lot of assumptions, and even allegations or rumors about treatment have emerged. In addition, several medicines were proposed and are still under research. However, the WHO and Centers for Disease Control and Prevention (CDC) warned about using medicines and said people must follow the treatment guidelines that help guide healthcare providers caring for patients with COVID-19. These guidelines are updated as research develops and as presented in Table 1.
Table 1
Management of patients with COVID-19 based on disease severity (taken from: https://www.covid19treatmentguidelines.nih.gov/about-the-guidlines)
| Disease severity | Panel’s recommendations |
| Not hospitalized, mild to moderate COVID-19 | For patients who are not at high risk for disease progression, provide supportive care and symptomatic management. |
| For patients who are at high risk of disease progression (as defined by the FDA EUA criteria for treatment with anti-SARS-CoV-2 monoclonal antibodies), use one of the following combinations: | |
| ∙ Bamlanivimab plus etesevimab | |
| ∙ Casirivimab plus imdevimab | |
| Hospitalized but does not require supplemental oxygen | There are insufficient data to recommend either for or against the routine use of remdesivir. For patients at high risk of disease progression, the use of remdesivir may be appropriate. |
| Hospitalized and requires supplemental oxygen | Use one of the following options: |
| ∙ Remdesivir (e.g., for patients who require minimal supplemental oxygen) | |
| ∙ Dexamethasoneplus remdesivir (e.g., for patients who require increasing amounts of supplemental oxygen) (BIII) | |
| ∙ Dexamethasone (e.g., when combination therapy with remdesivir cannot be used or is not available) | |
| Hospitalized and requires oxygen delivery through a high-flow device or noninvasive ventilation | Use one of the following options: |
| ∙ Dexamethasone | |
| ∙ Dexamethasoneplus remdesivir | |
| For patients who were recently hospitalizedf with rapidly increasing oxygen needs and systemic inflammation: | |
| ∙ Add tocilizumab to one of the two options above | |
| Hospitalized and requires invasive mechanical ventilation or ECMO | ∙ Dexamethasone |
| For patients who are within 24 h of admission to the ICU: | |
| ∙ Dexamethasoneplus tocilizumab |
[i] FDA EUA: Food and Drug Administration, Emergency Use Authorization. ECMO: Extracorporealmembrane oxygenation. ICU: Intensive care unit.
Access to drug services, like any other services, was disrupted by lockdown, social distancing and other restrictions during the pandemic [3,4]. Furthermore, community pharmacies are being affected by shortages of staff, disorganized services and drug availability, in turn this crisis originates urgent requirements to expand drug services, for protection of vulnerable individuals and minimizing the additional strain on the healthcare systems [1].
The current widespread of virus without enough data and an undiscovered cure led to a rush to find a way for protection or a magic treatment without adequate safety causing public confusion and panic. For instance, the media announced that hydroxychloroquine or chloroquine may have an effective role in treatment of COVID-19, stimulating inappropriate use and stockpiling. In addition, some people are confused by widely circulated myths or rumors on social media into taking scientifically-unproven substances and even poisonous therapy for coronavirus, such as ingesting methanol (alcohol) or bleach, taking a hot bath or exposure to high temperatures, and taking vitamins [1,5].
1.1.Effect of rumors during the COVID-19 pandemic
Health rumors are usually misleading resulting in severe consequences and unfavorable behaviors, particularly in a public crisis. Throughout the COVID-19 outbreak, health rumors have led to a salient purchase craze for different medicines and medical appliances and even misuse of some medicines that could have adverse effects on people’s health [4]. Consequently, the world experienced a shortage in availability of medicines and personal protective equipment (PPE) including face masks.
1.2.Misuse of medicines during the COVID-19 pandemic
Drug misuse is taking illegal drugs or medicines in a way not recommended by a physician or the manufacturer and the term is used to describe the improper or unscientific use of medicine rather than for what it is prescribed. Misuse is also defined as the intentional use of a product, over the counter (OTC) or prescribed medicines, by an individual for a purpose not in compliance with the authorized drug information [6].
During the COVID-19 pandemic, numerous drugs were used randomly by the patients such as analgesics, anticoagulants, steroids, hydroxychloroquine and other antibiotics that might cause severe adverse effects and different biochemical abnormalities and pathological consequences if used without supervision.
1.2.1.Causes of misuse
Because of the fear that people lived in during the onset of corona pandemic, they began to use several medicines randomly and without medical advice, which consequently led to harmful effects due to this misuse.
A salient purchase craze led by allegations and rumors during the COVID-19 pandemic.
Since the early times of outbreak, drug use habits, availability and prices have altered, making a shift in public behaviors regarding both prescribed and OTC medicines.
Due to the unprecedented conditions, the majority of people relied on pharmacists or home clinics managed by nurses to identify the required medicines, and with this constant concern, many people have resorted to bringing medical supplies, such as a medical oxygen bottle to the home to be used in treating the infected patients with this virus.
Also, because of the absence of specific regulations in Iraq, it is difficult to control the availability and prices of medicines and medical equipment, which prompted the Iraqis to search for easy temporary solutions, such as buying supplements, chronic disease medications, and even medical oxygen bottles, despite the three or four times their prices, to keep them at home, because they believe it is safer than going to hospitals.
In this regard, healthcare professionals, including pharmacists, should be aware of potential prescription drugs diversion, recognize misuse cases, consider the possibility of polydrug misuse, and prevent it where possible.
1.3.Role of community pharmacies during the COVID-19 pandemic
The pharmacists are always the most accessible health care providers; especially during the era of COVID-19 and considered on the frontline of public health service that have direct contact with the patients [7]. In many countries, pharmacies remain open and accessible to the public even during lockdown restrictions to manage the coronavirus disease [8]. Pharmacist’s availability and their direct contact with people, facilitating early detection of symptoms or referring to physicians, and they participated in numerous administrative measures that prevent or slow down the prevalence of the virus. Alternatively, pharmacists are responsible for dispensing medications and promoting their rational use by appropriate practice, providing safe healthcare and advice according to the official standards and also offering emotional support [9].
The aim of this study is to describe the pattern of dispensing medications in the midst of the COVID-19 pandemic via estimating the current status of drug dispensing in community pharmacies and to illustrate how a piece of information or health rumor can affect the dispensing of specific medicines and appliances and whether this has any potential side effects. This was conducted through a questionnaire with community pharmacists who lived through a certain period of the pandemic to assess changes in consumption and demand, prices and availability or shortages of medicines and PPE in Iraqi pharmacies retrospectively based on their recorded data systems. The study was designed as an analytical, observational, cross-sectional study by constructing a questionnaire that was validated before data collection according to the evaluation of a panel of experts in the field to ensure the included items are adequately assessing what the construct is intended to measure. Moreover, the study evaluated the biochemical and pathological consequences associated with the irrational use of these medicines via the analysis and interpretation of the biochemical and medical reports.
2.Subjects and method
The study was performed during the peak of COVID-19 pandemic from the beginning of June until the end of December 2020. A validated, compiled questionnaire included closed- and open-ended questions, was self-administered electronically using a Google Form to pharmacists working in different community pharmacies in different locations around the country. Pharmacists to be eligible in the study should be working in the pharmacy for not less than 1 year and have lived through the pandemic and its predecessor for a comprehensive comparison. The number of completed responses was 400, which represents a confidence level of 95% with a 5% margin of error.
The study was designed to include the followings:
• The duration spent working in the pharmacy.
• The location of the pharmacy whether it in the city center, peripheral or rural areas.
• Type or method of dispensing medicines in the pharmacy, whether it is in a medical center, a private clinic, or depending on by-hand prescriptions.
• Age of patients who come to ask for medicines.
• The changes in the amount of medications dispensed during COVID-19 outbreak.
• The changes in the availability and prices of medications.
• Types of common drugs dispensed regularly.
• Reason for taking these medicines.
• The demand for Vitamin C, Vitamin D, zinc, Chloroquine (antibiotics), antivirals, seasonal flu vaccine if has increased due to the belief of the prophylactic action or not.
• The demand for lidocaine gel due to belief of its prophylactic action.
• The demand for anticoagulants and antiplatelets without prescription.
• The efforts of pharmacists in patient education and providing advice during the pandemic.
• In addition to the reported biochemical changes and pathological consequences as serious side effects associated with the consumption of medications during the pandemic, depending on the recorded data system of the medical centers.
The results in this work were interrogated and the data were collected and analyzed statistically by cross-tabulation to be expressed as percentages or means ± standard deviation using SPSS and Excel Microsoft program.
3.Results and discussion
The results revealed that the location of the pharmacy, whether it is in the city center or in peripheral or rural areas makes no difference in the dispensing of the medicines. Whilst the results regarding the age of patients showed that 85% of patients who visited pharmacies were 20–60 years old, this may be due to the quarantine and the vulnerability of older or smaller individuals which restricted their movement. The amount of medications dispensed since COVID-19 outbreak has increased by 74%. Whereas 50.3% of pharmacists agreed that the demand of medicines seems higher than required in comparison to the periods before the pandemic and 60% of the dispensed medicines were taken by patients just in case needed and not for a real need or reason (Fig. 1). In addition, the availability of medicines and PPE were recorded by participants as a sharp decrease (61%) and difficult to be provided with a high cost where available (67%) (Fig. 2).
Fig. 1.
(a) The demand of medications dispensed since COVID-19 outbreak. (b) Age of patients come to pharmacies. (c) Evaluation of the demand of the dispensed medicines. (d) Reasons for demand of the medicines.
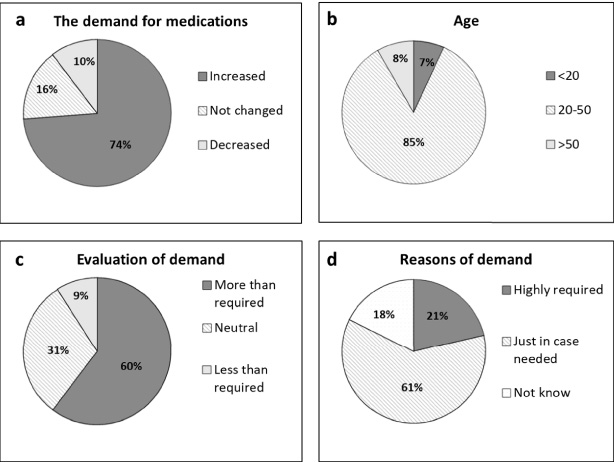
Fig. 2.
The changing in availability and cost of medicines during the COVID-19 pandemic.
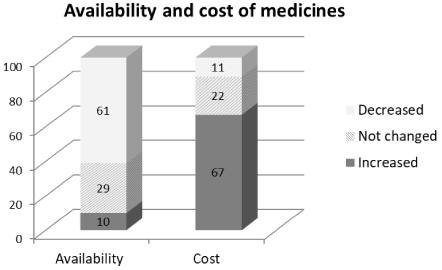
The demand for medicines seems more than required because of concern that these medicines will not be available in the coming days due to their frequent use or because of the prevention of movement between countries or cities and the exchange of resources, in turn, people started obtaining these medicines and storing them so that the required medicines would remain available for them in the coming days when they need them.
Some people bought medicines and used them to protect themselves from the Corona virus and they consider it a way of protection. Other people who show symptoms of seasonal influenza took these medicines, thinking that they are infected with the Coronavirus. Considering these reasons, several types of medications kept rising in their prices and reduction in the availability. This was not a case in Iraq only; previous studies have shown there were limited increases in prices of pertinent medicines and PPE seen in over 90% of pharmacies among a range of studied Asian countries particularly in Bangladesh [10,11]. The results show increased use of immune boosters such as vitamins and PPE across the studied countries, as well as a rise in prices of antimicrobials, analgesics and vitamin C in Malaysia, India and Vietnam. In addition, a shortage of a number of medicines was found especially in the case of antimalarials and antibiotics alongside the PPE in Bangladesh, Malaysia, India, and Pakistan [10].
The shortage is mainly owing to the highly irrational use of medicines, increase in consumption with decrease in production due to low affordability of manufacturers and closing, and difficulty of approaching workplaces by workers during quarantine.
It is common knowledge that a particular perception, especially in an emergency situation, leads to a change in health behaviors. Nevertheless, various and complicated factors are responsible for changing perception and encouraging people in making health-related decisions [4,12].
The tendency of conformity behaviors increases during any crisis. Social behaviors or decisions are also “contagious”. Studies regarding purchase craze have identified three types of conformity behaviors. The first sort is due to the family’s and neighbors’ pressure, while the second one is a blind conformity purchase derived by curiosity. The third sort is a rational choice conformity in which the purchase behaviors are stimulated by the rational balance between benefit, cost and time [13].
Drug use habits have altered due to the COVID-19 pandemic, leading to a shift in people’s behaviors for both prescription and OTC medicines.
3.1.Type of medicines that have been often dispensed during lock down
According to the responses of participants in the questionnaire, the dispense of several types of medications were recorded as being high and some drugs were often dispensed and mostly required, among them:
3.1.1.Analgesics, cold and flu and cough medications
During the pandemic era, people did not differentiate between being infected with coronavirus or seasonal flu virus so dispensing of these drugs increased to 60% for analgesics and 72% for cold and flu or cough medications (Fig. 3). This was to relieve the fever, headache, myalgia, sore throat, cough and other associated symptoms. For instance: paracetamol, non-steroidal antinflammotry drugs (NSAID), phenylephrine, and bromhexine are reported to be often dispensed.
Fig. 3.
Type of medicines that have been often dispensed during lock down.
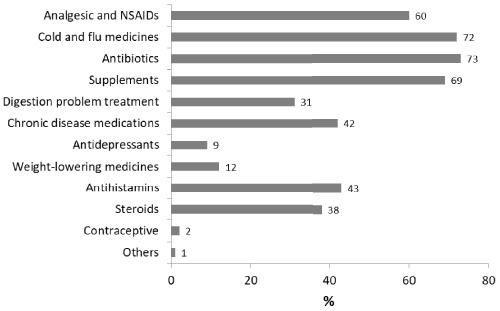
3.1.2.Antibiotics
A high percentage (73%) was recorded for dispensing antibiotics as a lot of people started to use them just in case they have infection (Fig. 3). Use of antibiotics in inappropriate way, as occurred during epidemic periods, can cause resistance. Infections caused by antibiotic-resistant germs are difficult, and sometimes impossible, to treat. In most cases, antibiotic-resistant infections require extended hospital stays and costly and toxic alternatives [14].
Among antibiotics that were mostly dispensed are Azithromycin (a macrolide antibiotic), Ceftriaxone (a third-generation cephalosporin antibiotic), meropenem (an intravenous β-lactam antibiotic),
Antibiotics misuse by the public has been globally reported during COVID-19 pandemic, despite the discouraging instructions by the WHO, especially for mild cases. While The National Institute for Health and Care Excellence (NICE) guidelines recommend that “Do not use antibiotics for preventing or treating COVID-19 patients and it should be used only when there is a strong clinical suspicion of bacterial infection,” treatment guidance from the “National Institutes of Health” also recommends that when antimicrobials have been used, there must be a daily reassessment to reduce the adverse effects due to unnecessary antibiotics [15]. Antibiotics were dispensed massively during the corona pandemic without proper clinical indications and in some instances for long duration this supports the idea of antibiotic misuse. Antibiotics in most Iraqi community pharmacies are easily accessible upon official physician prescription or upon patient request; this can be a major cause behind the highly antibiotic misuse happening among the population. In addition, the choice of antibiotics is usually not depending on bacterial culture or the severity of symptoms, but rather new and broad-spectrum antibiotics were preferred, which also result in antibiotic misuse. Generally, antibiotics have no role or benefit in treatment of viral infections [16].
The broad-spectrum antibiotic, azithromycin, is highly concerning. Azithromycin, a licensed, widely available antibiotic with antiviral and immunomodulatory actions, has been suggested as a treatment for COVID-19. Consequently, it was highly requested by people when they think they have been infected with the COVID-19. Azithromycin usage has been found high in primary care during the COVID-19 pandemic, however its irrational use and for long terms is contributing to antimicrobial resistance and side effects happening [17,18]. The common side effects include: headache, nausea, vomiting, diarrhea; and stomach pain. It also should be used with caution in some patients with liver problems or taking other medications.
3.1.3.Antihistamines
The dispensing of antihistamines was found to be 43% more frequent than usual (Fig. 3). The use of antihistamines has widely spread as they are mostly used for runny nose and sneezing, and because some people thought that they are able to restore the sense of smell and taste after losing when becoming infected with coronavirus. In this instance, the action of antihistamine may have no effect because, in most cases, loss of smell or taste will return relatively quickly after the relief from illness.
Some antihistamines were found to restore the loss of smell, and this concurs more with reduction of nasal inflammation than of nasal patency [19,20]. Several side effects are associated with the use: headache, dry mouth, feeling sick and drowsiness.
3.1.4.Steroids
Steroids act as anti-inflammatory agents and are mainly used for those needing respiratory support. Most people tend to use steroids, especially dexamethasone, as a prophylaxis to avoid COVID-19 infection, while after the infection they use it for relieving dry cough symptoms. So, their consumption increased to about 38% during the pandemic (Fig. 3).
Many side effects include: gastric upset, increased appetite leading to a significant weight gain, bacterial, viral, and fungal infections may progress more easily, osteoporosis, hypertension, fluid and sodium retention and hormonal changes [21]. Steroid therapy is considered a double-edged sword, although it is recommended for the treatment of viral pneumonia, it appears to reduce immunity. It is predisposing patients to secondary bacterial and fungal infections, such as Mucormycosis, thus impacting morbidity and mortality, particularly in uncontrolled diabetes mellitus and other immunosuppressive conditions [22].
Recent data from several studies has strongly supported the use of corticosteroids in treating COVID-19 only in patients requiring oxygen supplementation with severe symptoms. Steroids must be administered orally or intravenously depending on the severity of disease, “as hydrocortisone, dexamethasone or methylprednisolone, at a 6 mg dose of dexamethasone for 5 to 10 days” under supervision [23,24]. Misunderstanding and misinformation about corticosteroids can lead to their misuse and consequently, to adverse effects.
3.1.5.Chronic disease medications
Patients with chronic diseases urged to purchase their medicines in high quantities (42%) to be enough for a long time and stored them just in case closing pharmacies and before lockdown so they ensured them during quarantine (Fig. 3). This could lead to squandering medicines as they may reach the expiration date before being used or lost or even misused by other individuals.
3.1.6.Antidepressant
People experienced high levels of stress and depression as well as anxiety disorders during the pandemic. The unpredictable nature of the COVID-19, sudden changes in the future’s plans, lack of personal freedoms and concern for own or relatives’ health and well-being followed by house confinement for indefinite periods with substantial financial losses are among causes of stress associated with pandemic [25]. A previous study found the prevalence of depression during the pandemic was 7 times higher than that estimated globally in 2017, suggesting a primitive impact of the outbreak on mental health [26]. Another study has revealed a substantial elevation in the prevalence and burden of depression and anxiety disorders due to this pandemic [27]. Thus, demand for this type of medicines has relatively increased and found to be 9% (Fig. 3).
3.1.7.Digestion problems and weight loss medicines
Some medicines that are used for digestion problems and weight loss were found often dispensed during onset of COVID-19 pandemic, 31% and 12% respectively (Fig. 3). Many studies have demonstrated changes in people’s health related behaviors, including dietary behaviors, and sleep and physical activity. It is reported that individuals have engaged with high stress eating and less exercise during the pandemic, making a difficulty in weight management and digestion problem [28]. Previous data obtained from electronic health records have found that 39% of included patients have gained weight during the pandemic.
In addition to eating behavior during the pandemic, there was a stress, which is associated with increased levels of cortisol, in turn leading to increase intake of foods, alongside with that the body metabolizes food slowly under stress.
3.1.8.Contraceptives
It is important to build links between pandemic and women’s health; as infectious outbreaks and home quarantine have the potential to destroy family planning programs; and there was an increase in unplanned pregnancies during the outbreak [29]. In this regard, some respondents to our questionnaire have reported a slight increase in the demand for contraceptives (2%) (Fig. 3).
3.1.9.Others
Some medicines were also reported to some extent as an increase in consumption and suggested to be used within treatment lines without official approval at the time of the study; the most important one was Ivermectin. Ivermectin is an antiparasitic drug, and studies have reported that it has an inhibitory effect on the replication of SARS-CoV-2 in vitro, leading to its being resonated widely in the global press [30]. Nevertheless, its optimal antiviral dose has not been determined, and the preliminary data do not illustrate a clear and comprehensive understanding of its effect in COVID-19. However, its effectiveness as an antivirus is still controversial, whilst latest studies have concluded that ivermectin has no benefit in the treatment of COVID-19 or needs very high and dangerous doses and for very long time [31,32].
In addition to the above mentioned, a lot of different medicines recorded a rise in their demand when participants in the questionnaire were asked about their consumption during quarantine whether increased or decreased or not changed. Among these are;
3.2.The demand for specific medications during the pandemic
3.2.1.Supplements (vitamin C, vitamin D and zinc)
Individuals are usually looking for a way to potentially protect themselves or to mitigate the effects of infection with COVID-19, via consumption of supplements and so their consumption was often (69%) (Fig. 3).
There are many vitamins necessary for boosting the immune system. Vitamin C is known to potentiate the immunity because of its high antioxidant effects and anti-inflammatory, vitamin C supplementation can also support respiratory defense mechanisms, and has antihistamine properties which might improve flu like symptoms and reduce the severity and duration of infections, making it an attractive target for COVID-19 [33]. Therefore, the dispense of vitamin C has increased in a trial to improve immunity (87%) (Fig. 4). While standard doses of vitamin C are generally harmless, high doses can cause a number of side effects, including nausea, cramps, and an increased risk of kidney stones.
Fig. 4.
The demand for specific medications during the pandemic.
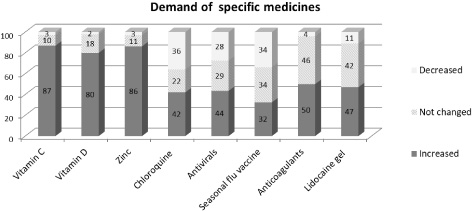
While vitamin D demand increased to 80% during the pandemic (Fig. 4). Vitamin D can modulate the adaptive and innate immune responses as well as to its action in disrupting cellular infection of the virus via interaction with angiotensin converting enzymes [34]. In addition, vitamin D acts directly on enveloped viruses and properly modulates and regulates the immunity and oxidative responses to viral infection. It is proposed that deficiency of vitamin D could increase the severity and frequency of infection with COVID-19. Hence, vitamin D supplementation is recommended to strengthen immunity to fight against COVID-19 [35].
Misuse of vitamin D will cause vitamin D intoxication (VDI), a well-known cause of hypercalcemia in children and leads to serious kidney, heart, and neurological problems.
Considering the demand for Zinc, it has increased to a high percentage, as 86.2% of responses confirmed that the demand has increased (Fig. 4). Zinc acts as antiviral, immunomodulator, and regulator of the inflammatory response. Till now there is not enough data to validate the beneficial role of zinc as an adjuvant therapy in COVID-19. However, zinc is suggested to have a role in preventing viral entry and blocking the replication via inhibition of the viral RNA-dependent RNA polymerase and interferes with the viral processing of polyproteins. Zinc also acts as an immunity modulator and stimulates the production of IFNα by leukocytes (43–48).
Acute toxicity with Zinc supplements could lead to gastrointestinal abnormalities (nausea, vomiting, persistent diarrhea, abdominal cramps), and renal syndromes, hematemesis, and haematuria. Meanwhile, chronic Zinc overdose may result in neurological disorders, sideroblastic anemia, myelodysplastic syndrome and granulocytopenia.
It has been also observed that increased consumption of vitamins and minerals was because of their easy availability, relatively low prices and widespread advertising.
A study found that consumption of vitamins and minerals was the highest among medical and related-education people indicating their awareness or a need for a protective measure against infection [36,37]. In addition, it has been shown that increased supplement use was recorded during the pandemic in Asia, America, Europe and Turkey [38].
Overall, previous studies have demonstrated that the supplementation vitamin C and vitamin D with zinc could mitigate viral respiratory infections. These supplementations can be characterized as widely available and safe with relatively low cost that can be helpful in coping with their increased demand during onset of the immune responses in viral infection, as well to reduce the risk of its severe progression [39].
However, accurate evaluation of the actual need, careful supplement selection, with appropriate dose and correct use can ensure superior benefits with less side effects occurring. Therefore, it is essential to inform people correctly and advise them to get the right sources of information [35].
3.2.2.Hydroxychloroquine and chloroquine
During the onset of the pandemic there was a rush to find a magic drug even without adequate guarantee of safety, and with the sources of therapy-related misinformation this has caused public confusion and panic. The announcement of using Hydroxychloroquine and chloroquine as potential cure for COVID-19 “game changers”, is an example that prompts improper stockpiling and their misuse by the community. Consequently this resulted in substantial shortages of these drugs and affected conditions for which they have been proven effective such as arthritis or lupus patients [1]. Their demand was recorded high at the beginning of the emergence of the pandemic as most people, even medical staff, hurried to buy them without prescription and store them just in case needed (42%) (Fig. 4). Hydroxychloroquine or chloroquine treatment has reported high rates of different cardiovascular adverse events, particularly QT prolongation, cardiac arrhythmias, cardiomyopathy and heart failure. Furthermore, they may lead to severe consequences particularly for those with cardiac disorders so carefulness must be considered when used as off label indications [18].
Findings from early studies have shown that taking hydroxychloroquine with azithromycin had promising results however data is very limited regarding benefit or safety profiles of the combination. Evidence has suggested doing adequate cardiac assessments before starting using this combination [1,18].
FDA has revoked the emergency use authorization to use hydroxychloroquine and chloroquine in the treatment of COVID-19 based on analysis and scientific data. This outcome was consistent with other recent data showing that the suggested doses of these medicines are unlikely to inhibit or kill the coronavirus [40–42].
3.2.3.Antiviral and flu vaccines
Some people believe that these medicines could provide a prophylaxis against COVID-19, so their demand increased. While these are not indicated for coronavirus and so have no role, and dispensing them may just be a waste. The demands for antiviral and flu vaccines have just increased to 43.5% and 32.5 respectively (Fig. 4).
Among these medicines are; remdesivir (Veklury®), oseltamivir phosphate (Tamiflu®), zanamivir (Relenza®), peramivir (Rapivab®), and baloxavir marboxil (Xofluza®).
Tamiflu is one of the common antivirals that are mistakenly used by some people as prophylaxis against COVID-19. It is an oral antiviral drug approved to treat acute and uncomplicated type A and B influenza in patients whose flu symptoms have lasted less than two days. Similarly, the seasonal vaccine has been also consumed due to belief of its action against coronavirus. However, some trails suggested that influenza vaccination could lower the risk and severity of COVID-19 testing and improve patients’ clinical outcomes [41,43]. Data from previous studies has believed that the use of some antivirals for treatment of COVID-19 is accumulating and more studies are needed to confirm the clinical benefits and safety [1].
3.2.4.Anticoagulants or antiplatelets
The demand for anticoagulants and antiplatelets, especially Aspirin, has increased during the pandemic as more than half of participants confirmed that (Fig. 4). Some people just used them without prescription or without laboratory analysis. People thought that it was beneficial to use aspirin as prophylaxis in coronavirus infection is accompanied by increased thrombotic risk and hypercoagulability in critically ill patients. However, it could be harmful and may cause peptic ulcer, sensitive reactions and it may increase the risk of heart attack and bleeding.
Low doses of aspirin are recommended to prevent arterial thromboembolism in patients who are at high risk of atherosclerotic cardiovascular disease. Use of aspirin could be also associated with reducing intensive care unit admission and mechanical ventilation, and mortality in hospitalized patients infected with COVID-19 [44]. Aspirin’s protective role in COVID-19 could be considered in cases of vascular thrombosis with no history of cardiovascular disorders or acute lung injury. However more trials are needed to provide adequate conclusions [45].
In addition, anticoagulants demand has increased according to the responses of our questionnaire even for the un-hospitalized patients and without laboratory analysis. An overwhelming number of literature over the past several months have suggested a high risk of thromboembolism associated with coronavirus infection. This might be due to exaggerated inflammatory responses leading to activation of the coagulation cascades and endothelial injuries. To date, there are no definite guidelines that highlight the use of anticoagulants in COVID-19. Some published guidelines recommend use of heparin only in patients of highly suspected or diagnosed with developing macrothrombi such as pulmonary embolism (PE) or deep vein thrombosis (DVT) [46].
3.2.5.Lidocaine gel
The demand for lidocaine in about 47% of pharmacies has increased during the pandemic. The use of lidocaine spread after allegations posted on social media that this drug acts as prophylaxis during epidemic and can be used in replacement of masks, so the demand for its use increased. People started to buy the gel and use it inside their nose believing that this would prevent catching the viruses. According to scientific literatures, lidocaine gel does not work against virus through the nose. In general, lidocaine is a local analgesic and anti-arrhythmic and effective in inhibiting cough and enhancing respiratory symptoms in severe asthma, in addition to its anti-inflammatory actions. Studies suggested that nebulized lidocaine can be used to improve consequences in COVID-19 patients, reduce cytokine release, protect lungs and prevent progression of the disease when being administered as an adjunctive treatment via inhalation for severe respiratory symptoms in hospitalized patients infected with coronavirus. This is the correct way for lidocaine if it is used and not as mentioned that it is used topically on the nose to avoid infection with COVID-19 [47].
Misusing of lidocaine can cause side effects such as mild burning, swelling, tingling, changes in skin color or skin redness where applied [48].
3.3.The reported biochemical changes and pathological consequences
According to the collected results, several biochemical and pathological consequences were recorded after consumption of these medicines, relying on medical reports and the history of medications taken as a follow-up for the visited patients (Fig. 5). The highest percentage was recorded with hepatic and liver enzymatic dysfunction (12%); this is suggested due to antiviral drugs, such as remdesivir, that have been proposed to cause organ dysfunction, with hypoalbuminemia and reduced potassium levels as well as increased transaminases levels (liver enzymes). High bilirubin levels were also seen and associated with steroid use. While endocrine and hormonal abnormalities (8%), such as hyperparathyroidism, Cushing syndrome, irregular menstruation, hair loss, obesity, and hyperglycemia, were also recorded. These changes were associated mostly with steroids, particularly dexamethasone injections due to hormonal release changes and metabolism alteration [49]. Renal dysfunction and kidney stones were found to be 7%, which could be attributed to vitamin D overdose that happened frequently in patients with histoplasmosis, hyperparathyroidism and lymphoma and could be explained by elevated calcium levels. Moreover, some antivirals could cause nephrotoxicity and renal injury, probably through direct renal tubular toxicity [50].
Fig. 5.
The reported biochemical and pathological consequences.
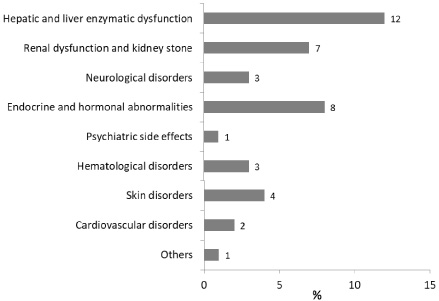
Whereas 4 percent represents skin related disorders such as acne and skin rash, which are presumably due to steroid and antibiotics use, respectively, and nose skin burning due to irrational use of lidocaine gel. Hematological side effects, including iron deficiency anemia, bleeding and changes in red blood cells count, were reported in only 3% of patients, owing mainly to aspirin and antiviral uses without medical supervision or follow-up. The same percentage was seen for neurological disorders such as muscle weakness, myasthenia gravis and dyskinesia; this is possibly due to hydroxychloroquine and chloroquine use [49]. The latest drugs use, particularly when administered in combination with azithromycin, was also associated with cardiovascular disorders which represent 2% to include QT prolongation, cardiac hypertrophy and congestive heart failure via alteration of the action potential and cellular excitability [18]. In addition, hydroxychloroquine and chloroquine were expected to cause some psychiatric side effects (1%) such as psychosis, irritability, depression, insomnia, anxiety and confusion. The neuropsychiatric side effects might be contributed to acetylcholine dysfunction or inhibition of neuronal calcium currents and dopamine excess. Other side effects such as gastric disturbances, could be mainly related to misuse of weight-lowering agents, antidepressants and antihistamines or infections due to steroid use. Most of these consequences are associated with the irrational use of medications or their use without medical supervision, which may result in serious and dangerous consequences if left without management. So the risks and benefits of medications should be considered before dispensing to patients.
3.4.The efforts of pharmacists during the pandemic
Pharmacists have an important role during the pandemic; they educate people about drugs and advise them about their harmful effects. The role of the pharmacist is to ensure the safe and effective use of medicines. Also, pharmacists participate with other medical staff in controlling diseases by monitoring and improving treatment methods, or studying the results of laboratory analyses. They also had a key role in educating people against the wrong or unscientific use of medicines to avoid misuse, especially during the pandemic, and what are the symptoms that require referring the patient to the physician to confirm the infection [51,52]. In this regard, and according to the questionnaire, efforts of pharmacists have increased (76%) during the pandemic to educate people in comparison to previous times.
A public misunderstanding of the information, people’s beliefs in rumors and conformity behavior caused purchase craze behaviors during the onset of the pandemic. However, some pieces of prevalent information are inaccurate or completely wrong that individuals become easily misinformed and can perform wrongful health behaviors. In order to protect people from infodemic (an overabundance of information or believing the rumors or myths), it is necessary to provide efficient health communication to eliminate the widespread infodemic [1,4].
Depending on the scope of practice and specialty, pharmacists could play a substantial role in the community and contribute in fighting against the misunderstanding and combating medication misinformation by providing the medical advice, managing minor ailments, treating medication-related problems and early identifying and appropriate referral of suspected cases [1,9].
However, the increase in the utilization of some medications, their shortage in their availability and rise in their prices is a big concern that requires addressing alongside misinformation with undesirable consequences that can occur from the pandemic. Community pharmacists could play a key role in protecting the public health by providing evidence-based advice, other preventative measures of medication misuse in addition to help and address some of the unintended consequences of irrational use of drugs.
4.Conclusion
The results obtained from this study showed that there is a misuse of some medications in the subjects involved in this study in Iraq that are not used on a therapeutic basis and without physician supervision. Most of the reasons to use these drugs are to protect from the Corona virus and store them just in case they are needed.
The use of some medicines, such as antibiotics, steroids, antihistamines, anticoagulants, and some supplements, in an unscientific way or without medical advice may cause multiple problems and serious biochemical and pathological consequences, especially liver enzymatic dysfunction and endocrine and hormonal abnormalities, that cannot be controlled.
4.1.Recommendation
Pharmacists’ roles can be activated more to reduce drug misuse and can be involved in different activities that effectively detect and prevent drug adverse effects and misuse. Policy efforts should be put in place to make some medications such as antibiotic prescriptions less easy to be obtained and thus would limit their indiscriminate dispensing.
A lot of public awareness and educational campaigns about the side effects associated with the misuse of drugs are required to avoid using these drugs without scientific or therapeutic need or in a way that does not follow the instructions.
Acknowledgements
The authors would like to thank their colleagues and pharmacy students for their help in this study.
Conflict of interest
There is no conflict of interest.
References
[1] | Erku DA When fear and misinformation go viral: pharmacists’ role in deterring medication misinformation during the “infodemic” surrounding COVID-19. Research in Social and Administrative Pharmacy. (2021) ;17: (1):1954–63. |
[2] | Hasen G Medicines dispensing practice during the era of COVID-19 pandemic: a commentary. Journal of Pharmaceutical Policy and Practice. (2021) ;14: (1):1. |
[3] | Leahy LG, Caverly SE. COVID-19: changing the landscape of substance use. Journal of the American Psychiatric Nurses Association. (2022) ;28: (1):5–8. |
[4] | Zhang L How the health rumor misleads people’s perception in a public health emergency: lessons from a purchase craze during the COVID-19 outbreak in China. International Journal of Environmental Research and Public Health. (2020) ;17: (19):7213. |
[5] | W.W.H.O. Coronavirus Disease (COVID-19) Advice for the Public: Myth Busters. 2020. [cited 2022]. |
[6] | Saleh SK. Misuse of appetite- stimulant drugs in Babylon. Iraqi Journal of Pharmaceutical Sciences. (2012) ;21: (2):31–4. |
[7] | Ali E Pharmacists and COVID-19. Journal of Pharmaceutical Policy and Practice. (2020) ;13: :36. |
[8] | Ashiru-Oredope D Needs assessment and impact of COVID-19 on pharmacy professionals in 31 commonwealth countries. Journal of Pharmaceutical Policy and Practice. (2020) ;13: (1):1–11. |
[9] | Liao Y Role of pharmacists during the COVID-19 pandemic in China–Shanghai experiences. Journal of the American College of Clinical Pharmacy. (2020) ;3: (5):997–1002. |
[10] | Godman B Rapid assessment of price instability and paucity of medicines and protection for COVID-19 across Asia: findings and public health implications for the future. Frontiers in Public Health. (2020) ;8: :585832. |
[11] | Rome BN, Avorn J. Drug evaluation during the Covid-19 pandemic. New England Journal of Medicine. (2020) ;382: (24):2282–4. |
[12] | Waters EA, McQueen A, Cameron LD. 11 perceived risk and its relationship to health-related decisions and beha avior The Oxford Handbook of Health Communication, Behavior Change, and Treatment Adherence. Oxford Academic; (2013) . p. 193. |
[13] | Duo Q Conformity behavior during a fire disaster. Social Behavior and Personality: An International Journal. (2016) ;44: (2):313–24. |
[14] | Lin J Mechanisms of antibiotic resistance. Frontiers in Microbiology. (2015) ;6: :34. |
[15] | Garg SK. Antibiotic misuse during COVID-19 pandemic: a recipe for disaster. Indian Journal of Critical Care Medicine: Peer-Reviewed, Official Publication of Indian Society of Critical Care Medicine. (2021) ;25: (6):617. |
[16] | Elsayed AA Antibiotic misuse and compliance with infection control measures during COVID-19 pandemic in community pharmacies in Egypt. International Journal of Clinical Practice. (2021) ;75: (6):e14081. |
[17] | Butler CC Azithromycin for community treatment of suspected COVID-19 in people at increased risk of an adverse clinical course in the UK (PRINCIPLE): a randomised, controlled, open-label, adaptive platform trial. The Lancet. (2021) ;397: (10279):1063–74. |
[18] | Chorin E The QT interval in patients with COVID-19 treated with hydroxychloroquine and azithromycin. Nature Medicine. (2020) ;26: (6):808–9. |
[19] | Cheng H Identification of a coumarin-based antihistamine-like small molecule as an anti-filoviral entry inhibitor. Antiviral Research. (2017) ;145: :24–32. |
[20] | Guilemany JM The loss of smell in persistent allergic rhinitis is improved by levocetirizine due to reduction of nasal inflammation but not nasal congestion (the CIRANO study). International Archives of Allergy and Immunology. (2012) ;158: (2):184–90. |
[21] | Hodgens A, Sharman T Corticosteroids. StatPearls [Internet], 2020. |
[22] | Ahmadikia K The double-edged sword of systemic corticosteroid therapy in viral pneumonia: a case report and comparative review of influenza-associated mucormycosis versus COVID-19 associated mucormycosis. Mycoses. (2021) ). |
[23] | Cano EJ Impact of corticosteroids in coronavirus disease 2019 outcomes: systematic review and meta-analysis. Chest. (2021) ;159: (3):1019–40. |
[24] | Organization WH. Corticosteroids for COVID-19: Living Guidance, 2 September 2020. World Health Organization; (2020) . |
[25] | Huremović D. Social distancing, quarantine, and isolation Psychiatry of Pandemics. Springer; (2019) . pp. 85–94. |
[26] | Bueno-Notivol J Prevalence of depression during the COVID-19 outbreak: a meta-analysis of community-based studies. International Journal of Clinical and Health Psychology. (2021) ;21: (1):100196. |
[27] | Santomauro DF Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. The Lancet. (2021) ;398: (10312):1700–12. |
[28] | Bullard T Impact of the COVID-19 pandemic on initial weight loss in a digital weight management program: a natural experiment. Obesity. (2021) ;29: :1434–38. |
[29] | Ferreira-Filho ES Contraception and reproductive planning during the COVID-19 pandemic. Expert Review of Clinical Pharmacology. (2020) ;13: (6):615–22. |
[30] | Caly L The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro. Antiviral Research. (2020) ;178: :104787. |
[31] | Peterson C Ivermectin-an antiviral drug for the COVID-19 pandemic? (2023) ;11: (46):7–18. |
[32] | Bibbins-Domingo K, Malani PNJJ. At a Higher Dose and Longer Duration, Ivermectin Still Not Effective Against COVID-19. JAMA; (2023) . |
[33] | Zhong X An evaluation of the protective role of vitamin C in reactive oxygen species-induced hepatotoxicity due to hexavalent chromium in vitro and in vivo. Journal of Occupational Medicine and Toxicology. (2017) ;12: (1):1–12. |
[34] | Aranow C. Vitamin D and the immune system. Journal of Investigative Medicine. (2011) ;59: (6):881–6. |
[35] | Çimke S, Gürkan DY. Determination of interest in vitamin use during COVID-19 pandemic using Google Trends data: infodemiology study. Nutrition. (2021) ;85: :111138. |
[36] | Puścion-Jakubik A Consumption of food supplements during the three COVID-19 waves in Poland—focus on zinc and vitamin D. Nutrients. (2021) ;13: (10):3361. |
[37] | Khabour OF, Hassanein SF. Use of vitamin/zinc supplements, medicinal plants, and immune boosting drinks during COVID-19 pandemic: a pilot study from Benha city, Egypt. Heliyon. (2021) ;7: (3):e06538. |
[38] | Aysin E, Urhan M. Dramatic increase in dietary supplement use during Covid-19. Current Developments in Nutrition. (2021) ;5: (Supplement_2):207. |
[39] | Souza ACR Zinc, vitamin D and vitamin C: perspectives for COVID-19 with a focus on physical tissue barrier integrity. Frontiers in Nutrition. (2020) ;7: :295. |
[40] | Rentsch CT Effect of pre-exposure use of hydroxychloroquine on COVID-19 mortality: a population-based cohort study in patients with rheumatoid arthritis or systemic lupus erythematosus using the OpenSAFELY platform. The Lancet Rheumatology. (2021) ;3: (1):e19–e27. |
[41] | Huang K Influenza vaccination and the risk of COVID-19 infection and severe illness in older adults in the United States. Scientific Reports. (2021) ;11: (1):1–6. |
[42] | Belayneh A. Off-label use of chloroquine and hydroxychloroquine for COVID-19 treatment in Africa against WHO recommendation. Research and Reports in Tropical Medicine. (2020) ;11: :61. |
[43] | Conlon A Impact of the influenza vaccine on COVID-19 infection rates and severity. American Journal of Infection Control. (2021) ;49: (6):694–700. |
[44] | Paranjpe I Association of treatment dose anticoagulation with in-hospital survival among hospitalized patients with COVID-19. Journal of the American College of Cardiology. (2020) ;76: (1):122–4. |
[45] | Ahmed HAS Rationales and uncertainties for aspirin use in COVID-19: a narrative review. Family Medicine and Community Health. (2021) ;9: (2):1–9. |
[46] | Chandra A Anticoagulation in COVID-19: current concepts and controversies. Postgraduate Medical Journal. (2021) ;98: :395–402. |
[47] | Bailey M Perioperative lidocaine infusions for the prevention of chronic postsurgical pain: a systematic review and meta-analysis of efficacy and safety. Pain. (2018) ;159: (9):1696–704. |
[48] | Keane K Does instillation of lidocaine gel following flexible cystoscopy decrease the severity of post procedure symptoms? A randomised controlled trial assessing the efficacy of lidocaine gel post flexible cystoscopy. Irish Journal of Medical Science . (2021) ;190: (4):1–7. |
[49] | Zadeh NM Mechanism and adverse effects of COVID-19 drugs: a basic review. Int J Physiol Pathophysiol Pharmacol. (2021) ;13: (4):102. |
[50] | Izzedine H, Launay-Vacher V, Deray GJAJOKD. Antiviral drug-induced nephrotoxicity. Am J Kidney Dis .. (2005) ;45: (5):804–817. |
[51] | Cadogan CA, Hughes CM. On the frontline against COVID-19: community pharmacists’ contribution during a public health crisis. Research in Social and Administrative Pharmacy. (2021) ;17: (1):2032–5. |
[52] | Sheppard J, Thomas CB. Community pharmacists and communication in the time of COVID-19: applying the health belief model. Research in Social and Administrative Pharmacy. (2021) ;17: (1):1984–7. |




