The effects of physical training without equipment on pain perception and balance in the elderly: A randomized controlled trial
Abstract
BACKGROUND: Research supports a link between exercise and falls prevention in the older population.
OBJECTIVES: Our aims were to evaluate pain perception and balance skills in a group of elderly subjects and to examine the consequences of a standardized equipment-free exercise program intervention on these variables. The study utilized a randomized controlled trial method.
METHODS: 92 subjects were recruited from a rural Sicilian village (Resuttano, Sicily, Italy). Subjects were randomly split into two groups, an experimental group (EG; n = 49) and a control group (CG; n = 43). Qualified fitness instructors delivered the standardized physical exercise program for the EG whilst the CG did not receive this exercise intervention. The Berg Balance Scale and the Oswestry Disability Index were administered in both groups before (T0) and after the intervention (T1).
RESULTS: At T1, the EG group significantly improvement in balance (p < 0.0001) and pain perception (p < 0.0001). No significant differences were found within the CG both in BBS and ODI, respectively.
CONCLUSIONS: Our findings suggest that a 13-weeks standardized exercise equipment-free program is effective in improving balance and perception of pain in the elderly. This type of intervention can consequently provide a low cost strategy to counteract the rate of disability in elderly.
1Introduction
According to the World Health Organization (WHO) and the American College of Sport and Medicine (ACSM), the population’s aging process is a win for humanity but it is also a challenge for societies and organizations [1, 2]. Falls have been identified to be the first cause of injury-related declines in health which consequently lead to higher levels of morbidity and mortality in the elderly [3]. In the case of hip fractures, the resultant hospitalization of patients leads to major social costs [4]. Moreover, 20% of patients with hip fractures die within a year as a result of the injury [5]. The aging process and related chronic diseases that affect older adults lead to balance disorders in this population [6–11]. A correlation between low cognitive status and reduced balance abilities furthermore exists [12]. Research importantly suggests that the effects of physical activity (PA) are particularly useful in older individuals with chronic diseases [13–16]. Decline in physical functioning pre-disposes older adults to poor quality of life and falls [17]. Modifiable factors in this scenario are muscle strength, balance proprioception and functional abilities which all can be improved through exercise [18–20]. A multicomponent PA, such as ballroom dancing was demonstrated by Bianco et al. [21] to improve balance and consequently through this, can prevent falls in the elderly. This in turn can also reduce perceived musculoskeletal pain which has been associated with low levels of balance skills [22]. In 2012, Irmak, A et al., showed that a exercise software programs may help to reduce perceived pain among office workers [23]. There were strengthening, stretching and posture exercises for all body parts which were suitable for office environment [23]. However, not all types of exercises are suitable to improve balance with an outcome of fall prevention [24, 25]. The aim of the study was therefore to evaluate balance levels and pain levels perceived in a large cohort of elderly subjects and consequently to investigate dose-response effects on these factors using a standardized equipment-free exercise program.
2Materials and methods
2.1Participants and procedures
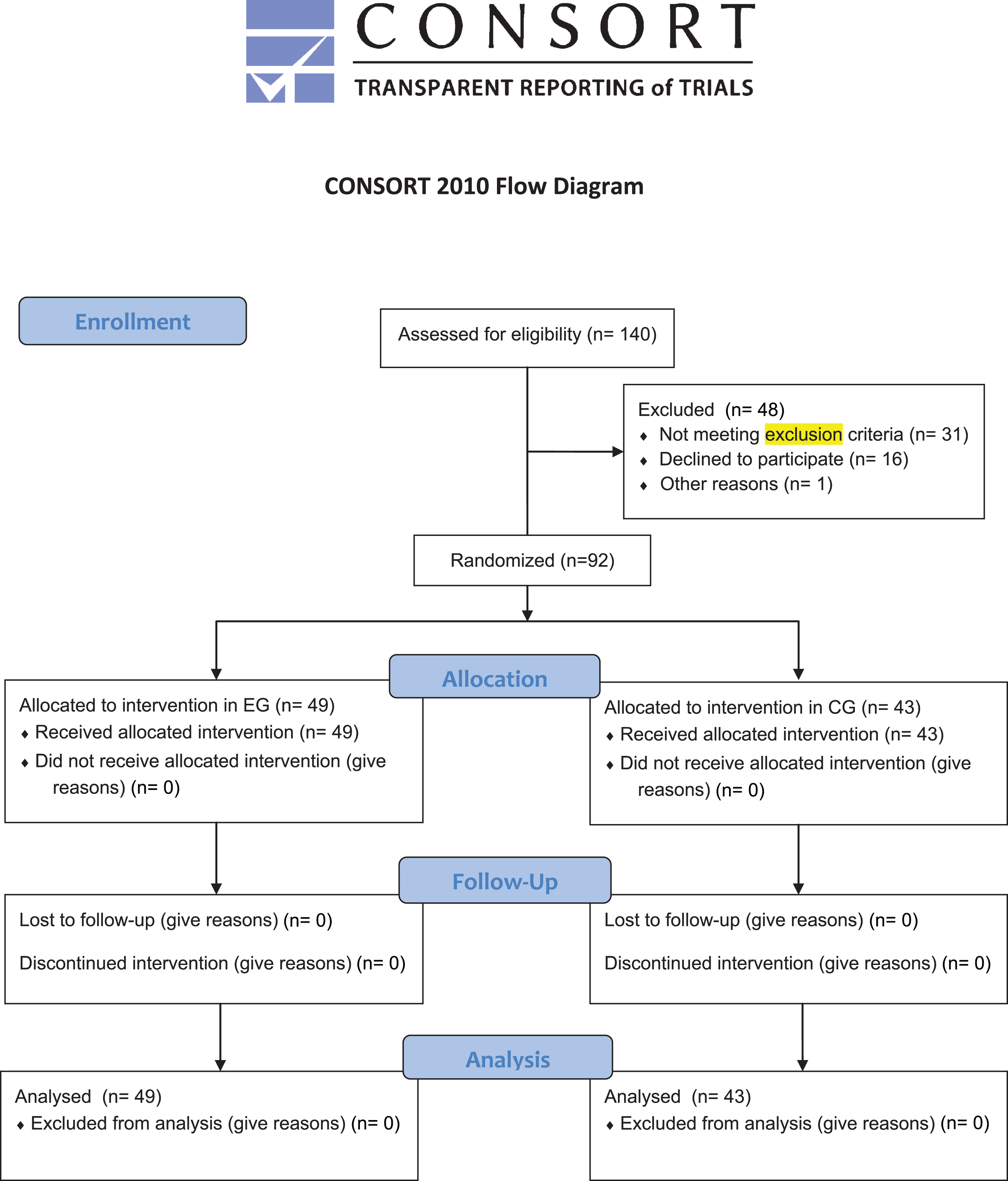
Prior to the start of the standardized exercise program, the Sport and Exercise Sciences Research Unit of University in collaboration with the Posturalab Research Institute of the University of Palermo carried out a screening procedure and a PA study in a rural village of Sicily (Resuttano); Italy. This prior study was carried out in compliance with the Declaration of Helsinki and the principles of the Italian data protection act (196/2003). The study design was approved by the departmental research committee (Consiglio di Dipartimento SPPF Prot. n. 285/2015; punto all’ordine del giorno numero 12) with the ethical committee approval number: 285-2015/MEDF-02/11. The selected population sample was invited to a first screening in which eligibility was evaluated based on age (minimum of 50 yrs, maximum of 85 yrs), disease-free state and no history of regular exercise. Exclusion criteria comprised conditions which prohibited moderate PA: 1) High pressure, 2) participants not having a positive diagnosis for any serious disease, 3) not ex-professional athletes, 4) no prosthesis). 140 subjects were initially screened, with 31 subjects not meeting all exclusion criteria and two subjects declining participation. Participants eligible for the study were however also excluded if they were either unable to commit to a 75% exercise program attendance or if adherence to the program dropped below this threshold during the intervention. Consequently, 92 subjects were included in the study and randomly assigned into two groups, the experimental group (EG; n = 49, 23 males, 26 females) and the control group (CG; n = 43, 19 males, 24 females). Subjects were randomized by a 1:1 ratio were the allocation sequence was PC generated (Diagram 1). The Consolidated Standards of Reporting Trials (CONSORT) Statement was set as a standard [26]. The project began in March 2015 and ended in July 2015. In this period two screening procedures were administered by an examiner blinded to group assignment at the following times: prior to the study (T0, baseline) and 13 weeks after the completion of the exercise intervention (T1). The EG group carried out a standardized equipment-free exercise program, whilst the CG group did not receive this intervention or any other study related treatment. Anthropometric characteristics of all participants were collected through a stadiometer (Seca 22±1 mm approximation, Hamburg, Germany).
Diagram 1
CONSORT 2010 Flow Diagram.
2.2Standardized equipment-free exercise intervention
The EG group was trained for the duration of 13 weeks by qualified fitness instructors. Due to the large number of subject in the EG group, the exercise intervention was performed twice in two parallel groups. Consequently, 25 standardized training sessions were carried out twice weekly each lasting 70 min (Table 2). The intervention was based on joint mobility, cardiovascular exercise, strengthening of core stability, proprioceptive training and eye-hand/eye-foot coordinative exercises. Both exercise training central phases were administered considering the principle of workload progression, from the first week up to the last week of each phase, respectively [19, 27–33].
Table 1
Descriptive anthropometric characteristics of participants
| Total sample | EG | CG | |
| Subjects | 92 | 49 | 43 |
| Age, yrs (SD) | 68.07 (5.01) | 67.32 (6.39) | 68.93 (2.51) |
| Weight, kg (SD) | 71.75 (12.15) | 72.88 (13.41) | 70.46 (10.53) |
| Height, cm (SD) | 158.5 (8.51) | 154.69 (8.38) | 162.83 (6.36) |
Table 2
Exercise protocol training
| Warm-up (10/15 minutes) | |||
| From standing posture, participants executed a standard sequence of exercises including: | |||
| •Two sets of eight repetitions of circling movements of shoulders (forward and backward) with bended arms | |||
| •Two sets of six repetitions of CC and AC circling movements of pelvis with hands to hips | |||
| •Two sets of six repetitions of left and right trunk rotations | |||
| •Two alternate sets of eight repetitions of CC and AC circling movements of feet | |||
| •Four sets of eight repetitions of FEM | |||
| •1 minute of free-walking | |||
| •Four sets of eight repetitions of FEM | |||
| Central phase for 1th –7th Weeks | |||
| Exercises | Objectives and hints | Time (m) | Repetitions |
| Diaphragmatic breathing exercises | 5 | ||
| Pre training, mobilization pelvis and principal joints | Retroversion, anterior tilt and rotation of pelvis; mobilization of the spine and larger joints | 10 | |
| The Hundred with bent leg | Exercise to increase torso stability and abdominal strength. | 5 | 4 repetitions of 30 s with 2 min of recovery between repetitions |
| Single Leg Circles with bent leg | Stabilization basin (minimum excursion of the circle), mobilization of the hip (maximum range of the circle). A breathing cycle for each circle | 5 | 5 repetitions for pelvis stabilization - 5 repetitions for mobilization of the hip |
| Spine Stretch with crossed legs | Lengthening of the muscles of the back legs, torso and neck; mobilization of the spine | 5 | 5 repetitions+5 repetitions with 2 min of recovery between repetitions; breathing out, bring your upper body forward contracting your abdominals and avoiding the bending of the spine |
| Single Leg Stretch with bent leg | Stabilization of the pelvis, strengthening the abdominals and hip flexors of the neck | 5 | 20 repetitions |
| Diaphragmatic breathing exercises | 5 | ||
| Central phase for 8th – 13th Weeks | |||
| Exercises | Objectives and hints | Time (m) | Repetitions |
| Diaphragmatic breathing exercises | 5 | ||
| Pre training, mobilization pelvis and principal joints | Retroversion, anterior tilt and rotation of pelvis; mobilization of the spine and larger joints | 5 | |
| The Hundred | Exercise to increase torso stability and abdominal strength. | 10 | 6 repetitions of 30 s with 2 min of recovery between repetitions |
| Roll Up | Mobilization of the spine. Strengthening the abdominals, the kinetic chain back and hamstring muscles. | 5 | 5 repetitions. Exhale and contract the abdominals |
| Single Leg Circles with one leg straight | Stabilization basin (minimum excursion of the circle), mobilization of the hip (maximum range of the circle). A breathing cycle for each circle | 5 | 5 repetitions for pelvis stabilization - 5 repetitions for mobilization of the hip |
| Spine Stretch with one leg straight | Lengthening of the muscles of the back legs, torso and neck; mobilization of the spine | 5 | 5 repetitions+5 repetitions with 2 min of recovery between repetitions; breathing out, bring your upper body forward contracting your abdominals and avoiding the bending of the spine |
| Rolling Like a Ball | Self-massage of the spine, activation of the abdominal muscles | 5 | 5/6 repetitions |
| Single Leg Stretch | Stabilization of the pelvis, strengthening the abdominals and hip flexors of the neck | 5 | 20 repetitions |
| Diaphragmatic breathing exercises | 5 | ||
| Cool down (10/15 minutes) |
| It included a standard sequence of stretching exercises: |
| •From a kneeling position, slowly go back on heels and hold for 20–30 seconds; practice the exercise twice and then return to the starting position |
| •From a SP, bend the knee, put the hands around the knee, and pull it toward the body, hold for 20–30 seconds with both hands; practice the exercise twice and then return to the starting position |
| •From NSP, bend the whole body forward slowly for 20–30 seconds; practice the exercise twice |
| •From NSP, with both arms over the head and clasped fingers, stretch the entire body for 20–30 seconds; practice the exercise twice |
| •From NSP, with both arms over the head and with clasped fingers, stretch all body for 20–30 seconds by TUB right and left alternatively; practice the exercise twice |
Abbreviations: CC, clockwise; AC, anticlockwise; FEM, flexion–extension movements of lower and upper limbs; SP, supine posture; NSP, neutral standing with legs slightly apart; TUB, twist the upper body to the left and right raising both arms over the head alternatively.
2.3Outcome measurements
The Berg Balance Scale (BBS), to evaluate the balance, and the Oswestry Disability Index (ODI), to evaluate the perception of general musculoskeletal pain, were administered in both groups prior at T0 and T1 (i.e. 14 weeks after T0). An examiner blinded to the patients’ group assignment performed all evaluations at the following times:
2.4The Berg Balance Scale (BBS)
This test consists of 14 items that quantitatively evaluate balance and risk of falling. The total score is obtained by summing the scores of each item [34]. The test is rated through the examiner’s observation of individual test performance. Each item is scored from 0 to 4, with 0 corresponding to the lowest performance level and 4 corresponding to a normal performance.
2.5The Oswestry Disability Index
The Oswestry Disability Index (ODI) is a tool to measure a subject’s permanent functional disability. The test is considered the ‘Gold Standard’ of low back functional outcome tools [35]. The test comprises 10 items with an overall achievable score of 50. For each section the total score possible is 5: if the first statement is marked, the section score is “0”, corresponding to a minimal disability; if the last statement is marked the section score is “5”, correspond to a maxim disability. The overall score can also be expressed as a percentage which consequently translates into a percentage ofdisability [35].
2.6Statistical analysis
All data were coded using Microsoft Excel. The statistical analysis was performed through StatSoft’s STATISTICA software (Windows, Vers. 8.0; Tulsa, OK, USA) and GraphPad Prism software (Windows, Vers. 5.0; La Jolla, CA, USA). Before and after the exercise intervention, a Wilcoxon matched pairs test (P < 0.05) was used to detect significant differences in the BBS Index and ODI results.
3Results
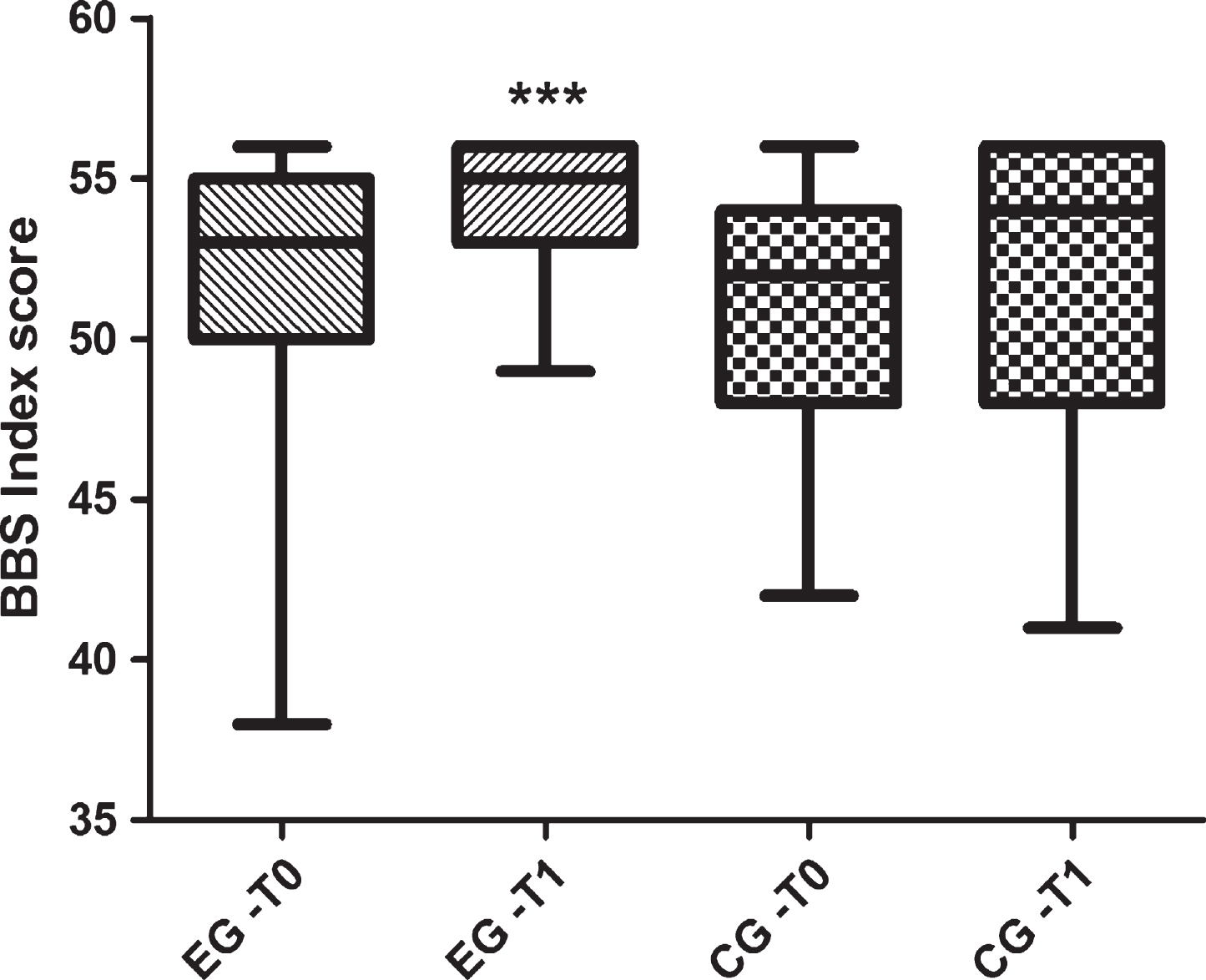
As previously said, the cohort was constituted by 92 subjects and assigned into two groups, EG (n = 49, 23 males, 26 females) and the control group CG (n = 43, 19 males, 24 females). Baseline demographics did not significantly differ between groups (Table 1). BBS scores at T0 were 51.83±4.17 and at T1 they were 54.36±2.15 for the EG group. The CG at T0 achieved BBS scores of 51.09±3.89 which did not change thereafter (T1; 51.67±4.49) (Table 3 and Fig. 1). ODI results prior and post intervention were 9.87±6.39 and 4.75±3.41 and 6.74±3.5 and 7.02±3.72 for the EG and the CG respectively (Table 3 and Fig. 2). Only the EG group demonstrated significant improvements in balance skills (p < 0.0001) as well as a significant reduction in levels of perceived pain (p < 0.0001).
Table 3
Descriptive Scores obtained in the Berg Balance Scale and in the Oswestry Disability Index
| EG (49) | CG (43) | |||||
| T0 | T1 | p | T0 | T1 | p | |
| BBS | 51.83±4.17 | 54.36±2.15 | <0.0001 | 51.09±3.89 | 51.67±4.49 | ns |
| ODI | 9.87±6.39 | 4.75±3.41 | <0.0001 | 6.74±3.5 | 7.02±3.72 | ns |
Fig.1
Scores obtained in the Berg Balance Scale (score range from 0 up to 56).
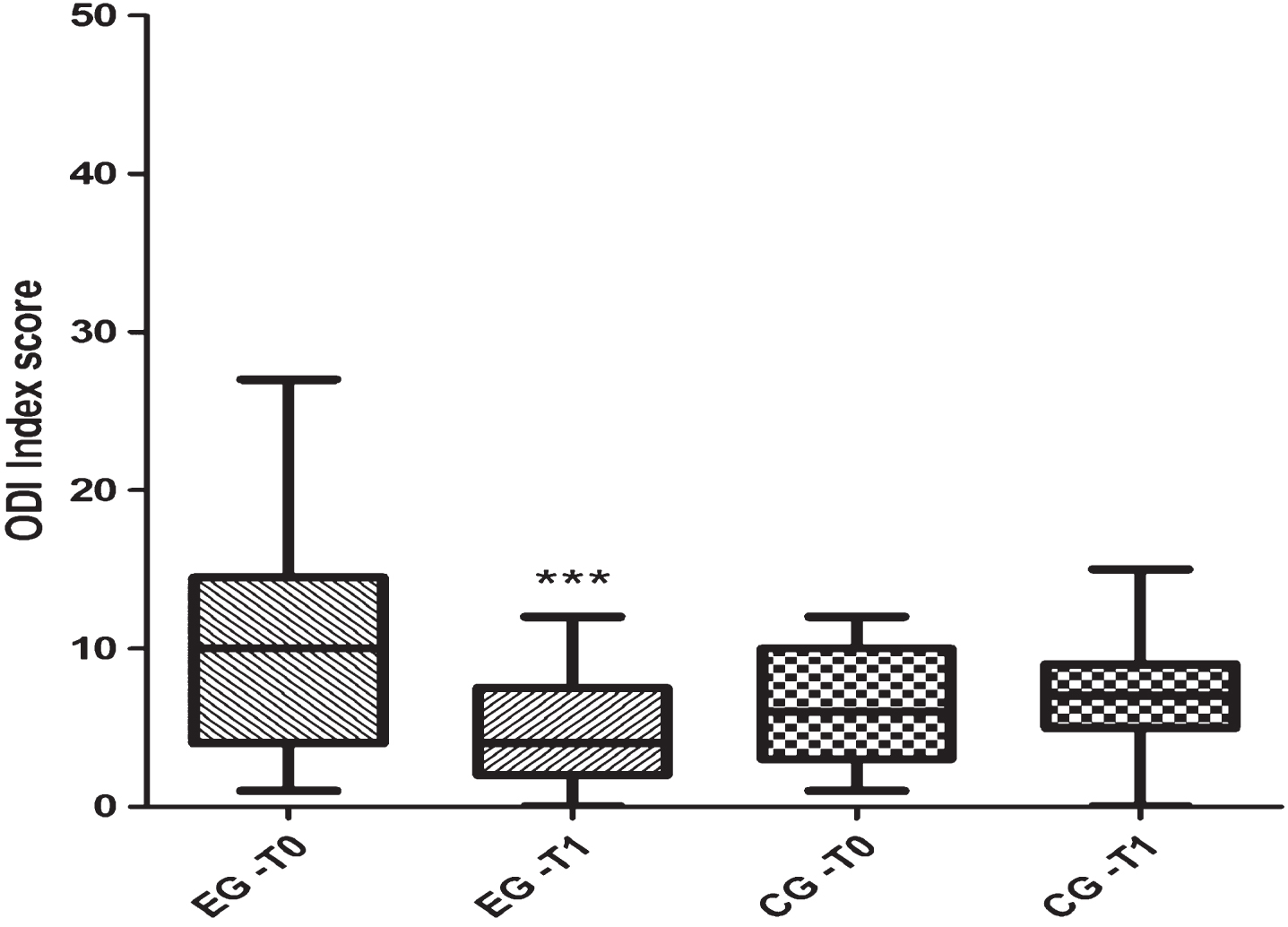
Fig.2
Scores obtained in the Oswestry Disability Index (score range from 0 up to 50).
4Discussion
Regular PA in the elderly population is fundamental as it positively influences most common diseases [36]. The present study demonstrates the effectiveness of a standardized equipment-free exercise program on dynamic balance skills and pain perception. Its importance is based on the use of body weight only exercises which can be performed in sports and non-sports environments and which effectiveness can improve the quality of life in the elderly by reducing the risk of falls. Moreover, this standardized exercise regime does not rely on specialized expensive resistance machines whilst arguably reducing the socio-economic impact of falls by reducing the rate of required hip-replacements and consequent costs. Recent research suggests that exercise interventions can also be beneficial to improve cognitive health by directly enhancing brain metabolism and plasticity [37]. Supporting this, Rahe et al. [38] demonstrated positive effects when combining cognitive training with additional PA. Our results also ascertain the sensibility of the BBS to detect improvements in people with a good level of balance. Whilst other balance protocols might be more accurate [9, 20, 39, 40] the BBS is valid and reliable but also a cost effective tool to measure different levels of balance when investigating large subject groups. The presently employed standardized equipment-free protocol comprised a number of exercises that are spinal and pelvic–lumbar stabilizing [41]. Hodges and Richardson [42] demonstrated m.transversus abdominus to be invariably the first muscle that is activated in many movements. A delayed contraction of this muscle indicates a deficit in motor control and an inefficient muscular spinal stabilization [42] which in turn can lead to the perception of musculoskeletal pain [42]. Unsgaard-Tondel et al. [43] demonstrated that an improved level of strength of m. transversus abdominis is associated with clinically important pain reductions [43]. Stubbs et al. [21] furthermore stated an increase in stability to translate into less perceived musculoskeletal pain. This is consistent with our findings as levels of perceived musculoskeletal pain were reduced in the EG group only. As suggested by Famula et al. [44], a high level of PA during adolescence positively influences the balance in old age. Body balance disorders more often affect elderly subjects who were less active at a young age [44]. Famula et al. [41] in this context asserted the importance of different types of PA which develop coordinative abilities. In the elderly, the maintenance of body balance skills at a relatively high level using specific exercise programs is vital [19, 45]. A good evaluation is required to select the best approach and to determine its effects. The ODI is an objective measurement tool that is used for evaluating the effects of the treatment, as it reveals the overall severity of impediments to daily living and physical activities [46]. The ODI predict disability caused by pain in the general population but it does not measure disability in the context of high-demanding activities such as sports [47]. The International Classification of Functioning, Disability, and Health (ICF) defines disability as following: “Disability is an umbrella term, covering impairments, activity limitations, and participation restrictions [48] and research suggests that patients with low back pain (LBP) have impaired levels of daily activities [49]; and more activities of daily living of the subjects with LBP are reduced due to the chronic pain and disability may occur. In addition, subjects reported less physical activity practice [50]. The present study demonstrated an improvement in ODI levels which in turn caused an improvement in quality of life as a result of a reduction of perceived pain. The main limitation of this investigation is the lack of standardized recommendation for balance scores that further distinguished between trained and untrained individuals as well as individuals with a history of adolescent training and individuals who only in later stages of their life engaged in a structured exercise regime. The present study demonstrates that a standardized 13-week exercise program based on joint mobility, cardiovascular exercise, strengthening core stability and proprioceptive training, can improve balance skills and reduce pain perception. Consequently, the exercise program can be recommended to practitioners starting to work with elderly inactive populations without the requirement of equipment and it can be applied to large subject groups. Further experimental research is required to confirm this mechanism of effectiveness, but the exercise could provide a low cost strategy to reduce and/or to slow down disability levels.
Conflict of interest
None to report.
Acknowledgments
We are grateful to all “Comune di Resuttano” community. In particular the project “Geromotricità I e II Edizione” was possible thanks to: 1) The Research Unit involved (Dott. Alessandro Valenza, Dott. Jessica Brusa, Dott. Luigia Caito, Dott. Giordano Rosa, Dott. Valerio Giustino, Dott. Jessica Albanese, Dott. Giovanna Panzica, Dott. Gloria Calabria, Dott. Monia Nigrelli; 2) The Mayor Dott. Rosario Carapezza; 3) The Mayor Deputy for Sport activities Giuseppe Claudio Bianco; 4) All members of the administrative staff involved.
REFERENCES
[1] | WHO global report on falls prevention in older age. Geneva Switzerland: World Health Organization. (2007) . |
[2] | ACSM: American College of Sports Medicine position stand. Progression models in resistance training for healthy adults. Med Sci Sports Exerc (2009) ;41: :687–708. |
[3] | Stenhagen M , Nordell E , Elmstahl S . Falls in elderly people: A multifactorial analysis of risk markers using data from the Swedish general population study ‘Good ageing in Skane’. Aging Clin Exp Res (2013) ;25: :59–67. |
[4] | Wiktorowicz ME , Goeree R , Papaioannou A , Adachi JD , Papadimitropoulos E . Economic implications of hip fracture: Health service use, institutional care and cost in Canada. Osteoporos Int (2001) ;12: :271–278. |
[5] | Zuckerman JD . Hip fracture. N Engl J Med (1996) ;334: :1519–1525. |
[6] | Lawlor DA , Patel R , Ebrahim S . Association between falls in elderly women and chronic diseases and drug use: Cross sectional study. BMJ (2003) ;327: :712–717. |
[7] | Thiem U , Klaassen-Mielke R , Trampisch U , Moschny A , Pientka L , Hinrichs T . Falls and EQ-5D rated quality of life in community-dwelling seniors with concurrent chronic diseases: A cross-sectional study. Health Qual Life Outcomes (2014) ;12: :2. |
[8] | Yu PL , Qin ZH , Shi J , Wu ZL , Sun ZQ . [Study on the relationship between chronic diseases and falls in the elderly]. Zhonghua Liu Xing Bing Xue Za Zhi (2009) ;30: :1156–1159. |
[9] | Martines F , Messina G , Patti A , Battaglia G , Bellafiore M , Messina A , Rizzo S , Salvago P , Sireci F , Traina M , Iovane A . Effects of tinnitus on postural control and stabilization: A pilot study. Acta Medica Mediterranea (2015) ;31: :907–912. |
[10] | Madigan M , Rosenblatt NJ , Grabiner MD . Obesity as a Factor Contributing to Falls by Older Adults. Curr Obes Rep (2014) ;3: :348–354. |
[11] | Patti A , Mammina C , Cataldo MC , Montalto MA , Alden T , Palma R , Bianco A , Palma A . Relationship between hypertension and accidental falls: The potential positive effects of physical exercise on blood pressure. Journal of Biological Research (Italy) (2015) ;88: :113–114. |
[12] | Stijntjes M , Pasma JH , van Vuuren M , Blauw GJ , Meskers CG , Maier AB . Low cognitive status is associated with a lower ability to maintain standing balance in elderly outpatients. Gerontology (2015) ;61: :124–130. |
[13] | Chase CA , Mann K , Wasek S , Arbesman M , Systematic review of the effect of home modification and fall prevention programs on falls and the performance of community-dwelling older adults. Am J Occup Ther (2012) ;66: :284–291. |
[14] | Hale LA , Mirfin-Veitch BF , Treharne GJ . Prevention of falls for adults with intellectual disability (PROFAID): A feasibility study. Disabil Rehabil (2016) ;38: :36–44. |
[15] | Patil R , Uusi-Rasi K , Tokola K , Karinkanta S , Kannus P , Sievanen H . Effects of a Multimodal Exercise Program on Physical Function, Falls, and Injuries in Older Women: A 2-Year Community-Based, Randomized Controlled Trial. J Am Geriatr Soc (2015) ;63: :1306–1313. |
[16] | Moreira RF , Foltran FA , Albuquerque-Sendin F , Mancini MC , Coury HJ . Comparison of randomized and non-randomized controlled trials evidence regarding the effectiveness of workplace exercise on musculoskeletal pain control. Work (2012) ;41: (Suppl 1):4782–4789. |
[17] | Stenhagen M , Ekstrom H , Nordell E , Elmstahl S . Falls in the general elderly population: A 3- and 6- year prospective study of risk factors using data from the longitudinal population study ‘Good ageing in Skane’. BMC Geriatr (2013) ;13: :81. |
[18] | Maitre J , Jully JL , Gasnier Y , Paillard T . Chronic physical activity preserves efficiency of proprioception in postural control in older women. J Rehabil Res Dev (2013) ;50: :811–820. |
[19] | Patti A , Bianco A , Paoli A , Messina G , Montalto MA , Bellafiore M , Battaglia G , Iovane A , Palma A . Effects of pilates exercise programs in people with chronic low back pain: A systematic review. Medicine (Baltimore) (2015) ;94: :e383. |
[20] | Sahin N , Bianco A , Patti A , Paoli A , Palma A , Ersoz G . Evaluation of knee joint proprioception and balance of young female volleyball players: A pilot study. J Phys Ther Sci (2015) ;27: :437–440. |
[21] | Bianco A , Patti A , Bellafiore M , Battaglia G , Sahin FN , Paoli A , Cataldo MC , Mammina C , Palma A . Group fitness activities for the elderly: An innovative approach to reduce falls and injuries. Aging Clin Exp Res (2013) ;26: (2):147–52. |
[22] | Stubbs B , Schofield P , Patchay S , Leveille S . Musculoskeletal pain characteristics associated with lower balance confidence in community-dwelling older adults. Physiotherapy (2015) ;102: (2):152–8. |
[23] | Irmak A , Bumin G , Irmak R . The effects of exercise reminder software program on office workers’ perceived pain level, work performance and quality of life. Work (2012) ;41: (Suppl 1):5692–5695. |
[24] | Battaglia G , Bellafiore M , Bianco A , Paoli A , Palma A . Effects of a dynamic balance training protocol on podalic support in older women. Pilot Study. Aging Clin Exp Res (2010) ;22: :406–411. |
[25] | Campbell AJ , Robertson MC , Gardner MM , Norton RN , Tilyard MW , Buchner DM . Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ (1997) ;315: :1065–1069. |
[26] | Schulz KF , Altman DG , Moher D . Group C: CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. PLoS Mede (2010) ;7: :e1000251. |
[27] | Bischoff HA , Roos EM . Effectiveness and safety of strengthening, aerobic, and coordination exercises for patients with osteoarthritis. Curr Opin Rheumatol (2003) ;15: :141–144. |
[28] | Romanazzi M , Galante D , Sforza C . Intralimb joint coordination of the lower extremities in resistance training exercises. J Electromyogr Kinesiol (2015) ;25: :61–68. |
[29] | Penzer F , Duchateau J , Baudry S . Effects of short-term training combining strength and balance exercises on maximal strength and upright standing steadiness in elderly adults. Exp Gerontol (2015) ;61: :38–46. |
[30] | Battaglia G , Bellafiore M , Caramazza G , Paoli A , Bianco A , Palma A . Changes in spinal range of motion after a flexibility training program in elderly women. Clin Interv Aging (2014) ;9: :653–660. |
[31] | Paoli A , Bianco A . What Is Fitness Training? Definitions and Implications: A Systematic Review Article. Iran J Public Health (2015) ;44: :602–614. |
[32] | Paoli A , Bianco A . Not all exercises are created equal. Am J Cardiol (2012) ;109: :305. |
[33] | Patti A , Bianco A , Paoli A , Messina G , Montalto MA , Bellafiore M , Battaglia G , Iovane A , Palma A . Pain Perception and Stabilometric Parameters in People With Chronic Low Back Pain After a Pilates Exercise Program: A Randomized Controlled Trial. Medicine (Baltimore) (2016) ;95: :e2414. |
[34] | Berg KO , Maki BE , Williams JI , Holliday PJ , Wood-Dauphinee SL . Clinical and laboratory measures of postural balance in an elderly population. Arch Phys Med Rehabil (1992) ;73: :1073–1080. |
[35] | Fairbank JC , Couper J , Davies JB , O’Brien JP . The Oswestry low back pain disability questionnaire. Physiotherapy (1980) ;66: :271–273. |
[36] | Vaes AW , Cheung A , Atakhorrami M , Groenen MT , Amft O , Franssen FM , Wouters EF , Spruit MA . Effect of ‘activity monitor-based’ counseling on physical activity and health-related outcomes in patients with chronic diseases: A systematic review and meta-analysis. Ann Med (2013) ;45: :397–412. |
[37] | Bamidis PD , Vivas AB , Styliadis C , Frantzidis C , Klados M , Schlee W , Siountas A , Papageorgiou SG , A review of physical and cognitive interventions in aging. Neurosci Biobehav Rev (2014) ;44: :206–220. |
[38] | Rahe J , Becker J , Fink GR , Kessler J , Kukolja J , Rahn A , Rosen JB , Szabados F , Wirth B , Kalbe E . Cognitive training with and without additional physical activity in healthy older adults: Cognitive effects, neurobiological mechanisms, and prediction of training success. Front Aging Neurosci (2015) ;7: :187. |
[39] | Scoppa F , Capra R , Gallamini M , Shiffer R . Clinical stabilometry standardization: Basic definitions–acquisition interval–sampling frequency. Gait Posture (2013) ;37: :290–292. |
[40] | Oyarzo CA , Villagran CR , Silvestre RE , Carpintero P , Berral FJ . Postural control and low back pain in elite athletes comparison of static balance in elite athletes with and without low back pain. J Back Musculoskelet Rehabil (2014) ;27: :141–146. |
[41] | Endleman I , Critchley DJ . Transversus abdominis and obliquus internus activity during pilates exercises: Measurement with ultrasound scanning. Arch Phys Med Rehabil (2008) ;89: :2205–2212. |
[42] | Hodges PW , Richardson CA . Inefficient muscular stabilization of the lumbar spine associated with low back pain. A motor control evaluation of transversus abdominis. Spine (Phila Pa 1976) (1996) ;21: :2640–2650. |
[43] | Unsgaard-Tondel M , Lund Nilsen TI , Magnussen J , Vasseljen O . Is activation of transversus abdominis and obliquus internus abdominis associated with long-term changes in chronic low back pain? A prospective study with 1-year follow-up. Br J Sports Med (2012) ;46: :729–734. |
[44] | Famula A , Nowotny-Czupryna O , Czupryna K , Nowotny J . Previous physical activity and body balance in elderly people. Biol Sport (2013) ;30: :311–315. |
[45] | Barnett A , Smith B , Lord SR , Williams M , Baumand A . Community-based group exercise improves balance and reduces falls in at-risk older people: A randomised controlled trial. Age Ageing (2003) ;32: :407–414. |
[46] | Kong YS , Jang GU , Park S . The effects of prone bridge exercise on the Oswestry disability index and proprioception of patients with chronic low back pain. J Phys Ther Sci (2015) ;27: :2749–2752. |
[47] | Zamani E , Kordi R , Nourian R , Noorian N , Memari AH , Shariati M . Low back pain functional disability in athletes; conceptualization and initial development of a questionnaire. Asian J Sports Med (2014) ;5: :e24281. |
[48] | Jimenez Bunuales MT , Gonzalez Diego P , Martin Moreno JM . [International classification of functioning, disability and health (ICF)]. Rev Esp Salud Publica (2002) ;76: :271–279. |
[49] | Soysal M , Kara B , Arda MN . Assessment of physical activity in patients with chronic low back or neck pain. Turk Neurosurg (2013) ;23: :75–80. |
[50] | Koes BW , van Tulder M , Lin CW , Macedo LG , McAuley J , Maher C . An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J (2010) ;19: :2075–2094. |




