The effect of a structured personalized ergonomic intervention program for hospital nurses with reported musculoskeletal pain: An assigned randomized control trial
Abstract
BACKGROUND:
Intervention programs for hospital nurses with musculoskeletal pain present a challenge for the health professions.
OBJECTIVE:
To examine the effect of a structured personalized ergonomic intervention program for hospital nurses with musculoskeletal pain.
METHODS:
In a randomised controlled trial, 31 nurses from one central hospital with musculoskeletal pain were observed at work. A multi-stage study that included the Nordic Musculoskeletal Questionnaire, Karasek’s questionnaire, The Rapid Entire Body Assessment, and an intervention program was completed with 14 nurses, while the remaining 17 were assigned to a control group. The intervention program was carried out by one physiotherapist and included four meetings over three months. The control group received only instruction sheets. Data on body posture and frequency and intensity of pain were collected before and at three months after the termination of the intervention program.
RESULTS:
Compared with the control group, the intervention group showed an improvement in REBA scores and in posture that is considered risk factor for work-related musculoskeletal discomfort disorders [p < 0.001], but there were no significant differences in the number of body parts in pain or in the level of musculoskeletal pain.
CONCLUSIONS:
The intervention was shown to be effective in reducing risk factors for work-related musculoskeletal disorders over a short follow-up period. A long-term study is required to determine if this effect is preserved over a longer period and to determine whether the intervention can reduce musculoskeletal symptoms.
1Introduction
Work-related musculoskeletal disorders (WRMSD) are musculoskeletal injuries caused or exacerbated by various forms of exposure within the work environment [1]. Nurses are at significant risk of such injuries, including low back pain (LBP) (30–60%), neck pain (33–53%), and shoulder pain (30–48%) [2–4]. The resulting discomfort and pain can contribute to an inability to perform tasks appropriately, decreased productivity, and an increase in disability compensation claims [5–7].
Biomechanical risk factors include repetitive tasks that require prolonged static forces or awkward work positions [8–10], for example, in nurses, this can occur when lifting and carrying patients and from prolonged tasks [3, 7, 9]. Previous interventional studies have described different intervention methods including using educational models, the distribution of printed guidance material and/or coaching within the framework of “Back Schools” [11, 12], or reduced stress with the use of special equipment [13–17]. Physical exercise programs have also been attempted to reduce musculoskeletal pain in nurses [18–20]. In a systematic literature review, ergonomic interventions such as improved technical performance of transfers and reduced frequency of manual lifting were found to be preferable to changing general health behaviours [21]. The literature also shows that an integration of the various approaches may be even more preferable [18, 21, 22].
Although it has been shown that primary and secondary work prevention programs are limited in their effectiveness [23], there is no agreement on the appropriate interventional program for nurses to reduce biomechanical strain. This notion is presented in the review of Bos et al. [21], who tried to evaluate the effects of occupational interventions for primary prevention of musculoskeletal symptoms in healthcare workers. This research demonstrated that there was a beneficial effect of occupational interventions for physical discomfort, technical performance of transfers and frequency of manual lifting, but there was insufficient evidence to explain absenteeism due to musculoskeletal discomfort, fatigue, perceived physical load, knowledge of risk factors at work, and ergonomic principles.
A limitation of previous studies is that they do not attempt to determine the various biomechanical strains for individual nurses and do not address specific personal models to facilitate change. Motor learning theories suggest [24] that people achieve maximal progress at the workplace when intervention is guided by principles of motor learning. “Motor learning” refers to a set of internal processes associated with practice or experience leading to relatively permanent changes in motor behaviour [25]. This approach takes into account the characteristics of the learner (e.g., age, strength, posture, speed), the type of work (e.g., complexity, task organization in the various wards), and the structure of work practices (e.g., similarity between the contexts of practice and those at the work place) before determining the most appropriate personally tailored program, including suggestions to decrease ergonomic stress and exercises to minimize symptoms in the remaining areas of stress.
In the following study we used a comprehensive ergonomic model (referring to the work place, the worker, and the task, to help workers learn the correct movement patterns) integrating motor learning principles according to the 4 stages model (I- evaluation of ground setting, II- basic intervention, III- progressive intervention, IV- the follow up stage) [25], in order to determine whether a comprehensive and personalized ergonomic interventional program can reduce the biomechanical workload and introduce personalized exercise to reduce associated musculoskeletal complaints. Specifically, the research questions are: (a) compared with the level before the intervention, will there be a significant decrease after the structured intervention program in the level of biomechanical workload as expressed by body postures that are considered risk factors for work-related musculoskeletal disorders and musculoskeletal pain (time effect)? (b) Will there be a significantly larger improvement in body postures and in musculoskeletal pain among hospital nurses who participated in the intervention than among the nurses of the control group of hospital nurses who did not attend the intervention program [timeXgroup]?
2Materials and methods
This is an assigned, randomized, controlled trial. The study was approved by the institutional review board of the Meir Hospital. Following a full explanation of the procedure, a valid consent form was completed by all participants in the study.
The authors selected a study population according to inclusion and exclusion criteria (see “Study Population” and Fig. 1), and then randomly assigned the study population into the intervention and the control group. A demographic questionnaire was used to collect data from all participants regarding gender, age, education, self-reported health status, medications, work experience and status (full/part time job). Study participants were photographed prior to and post-intervention while performing the same specific task, which was defined as the most strenuous task experienced at work. While performing the task, the nurse was asked to state when it felt most strenuous. At this moment the nurse was asked to stay still and the photograph was taken. Results were scored according to Rapid Entire Body Assessment (REBA) [26–28] instructions to assess participants’ body postures (see “Tools” section). Prior to intervention and six months after the start of the intervention (three months after the last session of the intervention), both study and control groups completed the self-administered questionnaires (The Standardized Nordic Questionnaire [29] and The Job Content Questionnaire [30] (also known as Karasek’s questionnaire and in this paper will be referred to by this name)).
2.1Study population
The study population included 31 female registered nurses from one medical centre located in a large geographic area in Israel. Inclusion criteria were as follows: A minimum of half-time work (18 hours per week) for at least one year; reports of musculoskeletal pain (at least one body region) regardless of use of pain medications; and agreement to participate in the interventional study. Exclusion criteria were nurses with previously defined job restrictions and pregnancy.
The initial questionnaire was completed by 411 nurses, of which 86 reported musculoskeletal pain. Sixteen nurses were excluded because of pregnancy or a previously recognized permanent disability. Of the 70 remaining nurses, 34 refused to participate. The self-administrated questionnaires that were returned by the 36 remaining nurses were randomly assigned to two groups by drawing numbers of participants out of ‘a hat’; 18 were assigned to the intervention group and 18 into the control group.
Four nurses from the intervention group and one nurse from the control group failed to complete either the intervention or the follow up.
Three months later, intervention group participants were invited to the physiotherapy group hall to attend three group meetings (in addition to the individual intervention they had) once a week for three consecutive weeks. Each meeting was about 45 minutes long. During the three meetings the participants were taught segmental stabilizing exercises according to their individual reported complaints of pain and common work situations. The control group received instruction sheets which included explanations of the principles of good work posture as well as when and how to perform exercises during the work shift.
2.3.1Tools
2.3.1.1. Rapid Entire Body Assessment (REBA). The REBA was used to assess body postures that are considered risk factors for work-related musculoskeletal disorders during work. REBA has been developed to fill a need for a practitioner’s field tool that is sensitive to the type of work postures found in health care and other service industries [26, 27]. REBA is based on a structured observation posture (in this study it is based on a photograph of the most strenuous task as defined by the nurses). The overall REBA score is assembled in three stages: (a) Analysing the posture relating to the trunk, neck, and legs. This analysis produces nine possible scores, to which a load and force score is added. (b) Analysing the posture of the upper arms, lower arms, and wrists, producing nine possible scores, to which a coupling score is added. For the present study, the calculation of this section was carried out for the dominant hand. It is acceptable to select the arm to be assessed [26, 27], (c). The two scores are combined and an activity score is added to generate the final REBA score. The overall rating scale ranges from 1 [minimal] to 15 [maximal], corresponding to “negligible” to “extremely high” risk factors for work-related musculoskeletal disorders, which represents the categorical REBA Decision Score [27].
Participants were interviewed and asked to describe their most difficult task. This specific task was photographed while it was being performed [the pictures were taken in a way that captured the dominant side], then analysed as described above. This observation method has been shown to be reliable and valid [28]. Face and content validity was also reported for pre- and post-ergonomic intervention and for achieving changes in work practices [31].
Two physiotherapists performed the REBA analysis independently of each other. One of the physiotherapists was blind to the participant’s group assignment; the other was not. The final rating was determined by agreement between the analysts.
2.3.1.2. The Standardized Nordic Questionnaire for the Analysis of Musculoskeletal Symptoms (SNQ) [29]. Prior to and post-intervention, the nurses completed the SNQ, which contains 36 questions on pain and discomfort in 12 different body parts, with a total score ranging from 36 to 72 (the sum of all painful joints). The SNQ has been reported as a reliable tool for a variety of different worker populations. Its validity has been demonstrated by a high match (80%) between the results of the SNQ and the participants’ clinical history [29]. The level of pain for each of the 12 body parts was further evaluated by the Numeric Rating Scale [32]. The Numeric Rating Scale measures a subjective perception of pain which ranges from 0 to 10 and gives the whole numeric scale for rating the intensity of pain.
2.3.1.3. The Job Content Questionnaire (will be referred as Karasek’s questionnaire) [30]. Participants also completed Karasek’s questionnaire designed to assess the level of job decision-making latitude and psychological demands prior to and post- intervention. The questionnaire includes 14 statements that describe the dimensions of the job content in two main categories: Five statements relate to the level of psychological demands at work and nine statements relate to the level of control, discretion, and decision making. For each question a 5-point Likert scale was used, ranging from 1 (very little) to 5 (very much) to evaluate the amount of agreement or disagreement with each of the statements. The tool was previously found to be reliable, with Cronbach’s α> 0.7, and validity was established by showing high correlations with other tools (such as the Work Environment Scale (WES) and the Maslach Burnout Inventory (MBI)) (r = 0.70–0.81) [30].
Prior to the intervention, each participant also completed a personal data questionnaire regarding age, body mass index (BMI), rates of smoking, and job-related information, which included years of experience in both the job and the specific ward, and hours of work, including reporting on shift work.
2.3.1.4. Structured intervention program. The postures of participants in the intervention group were evaluated by REBA (Stage I-Ground) and received coaching in four meetings. All the meetings were conducted by one authorized physiotherapist with more than 5 years of experience who worked at the same hospital where the study was conducted. The physiotherapist was familiar with work and regulations in the different departments as part of her routine work. To increase fidelity, the physiotherapist attended a course given by an occupational therapist with a Ph.D. degree (one of the developers of the prevention ergonomic model), and received regular personal supervision sessions during the interventionphase.
The four meetings were structured as follows: The first meeting of the intervention took place in the ward (Stage II-Basic intervention). In that meeting a job analysis was performed for the specific nurse in the given ward. The nurses performed the five most frequent tasks at their workstation during working hours, and the therapist performed basic interventions suited to those five tasks. The first intervention included an oral explanation of how to perform tasks properly, analysis of the body postures that are considered risk factors for work-related musculoskeletal disorders, and prescriptive exercises. Special emphasis was placed on correct body postures during work, organisation of the work environment, and use of aid accessories. Correct body posture during work included avoiding rotational movements and awkward and uncomfortable body positions, after which ergonomic solutions were recommended. Common interventions to reduce ergonomic stress included working as closely as possible to the patient, lifting with bended knees, and asking for help for difficult tasks. Proper organization of the work environment included adjusting the intravenous infusion stand to the height of the nurse when changing infusions, widening the space between cribs in the nursery to allow improved body position when taking care of babies, and lowering the storage position of heavy equipment. The third principle involved the use of aid accessories.
After three months, all participants were invited to attend three educational/coaching group meetings. All the meetings were held during working hours (approximately five nurses per group), once a week for three consecutive weeks. Each meeting was about 45 minutes long. During these three meetings the participants were taught segmental stabilizing exercises according to their individual reported pain and common work situations [33–35] (Stage III-Progressive intervention). A list of exercises was recommended for releasing physical stress in those who had been in uncomfortable positions over prolonged periods of time. Each session paid special attention to, and included explanations about the anatomy and physiology of body regions (back, neck, upper extremities, and lower extremities). The first educational/coaching meeting focused on the lower back, the second on the upper back, shoulder girdle, and neck, and on the upper and lower extremities, and the third included instructions for exercises to address difficulties that 5 participants had reported with work tasks. Equipment used during these sessions included Thera-Band and balls that were designed for stretching, flexibility, and increase of strength for the limbs and trunk with personal adaptations. These meetings were developed on the basis of studies that investigated the benefits of physical activity programs for WRMSD [36–38] instructed by and monitored under the direct supervision of the physiotherapist to ensure correct technique, safety, and proper exerciseintensity.
The control group received instruction sheets that included explanations about the principles of proper work performance and when and how to perform exercises during the work shift. The sheets were given to the control group by the same physiotherapist who conducted the intervention, but without any oral explanation. The control group received the instruction sheets at the same time when the intervention group received the first intervention.
Six months after the start of the intervention (and three months after the last session of the intervention) both study and control groups were re-evaluated by the self-administered questionnaires (SNQ and Karasek’s questionnaire). Further, the groups were photographed again performing the same task identified during the pre-test and another REBA analysis was conducted to assess the level of their biomechanical workload (Stage IV-follow-up for the study group).
2.4Statistical analysis
Means and standard deviations of bio-demogra-phic variables, pain level, Karasak’s Questionnaire, and REBA were reported. Frequency of pain in the last week was calculated for each of the 12 body regions of the SNQ.
Sample size was calculated for testing the difference between means with 80% power and 5% significance, assuming that the ratio between the intervention group and control group = 1. Pooled variance = 2 and the expected difference of time effect was 1.5. The required sample included a total of 30 participants (15 in each group). Sample size was analysed using the Win-Pepi program. When the actual analysis was performed, the statistical power was 89% (sample size was 14 for intervention group and 17 for the control group, SD = 2.38 and 2.06 for intervention and control respectively, mean difference of 4.22 and α= 0.01).
To verify maximum reliability between the two evaluators in this study (two physiotherapists performed the analysis independently of each other), maximum reliability was achieved through the following process: For the pre-intervention assessment, there was full agreement on 32 cases out of 36. In two cases, there was a difference of 2 points, and in two other cases, the difference was 1 point. For the post-intervention assessment, there was full agreement between the analysts on 29 cases out of 31. For the two remaining cases (both from the control group) the difference was 1 point.
Two separate paired t-tests (one for the intervention group and one for the control group) were used to analyse the first hypothesis, testing the difference in the risk factor scores for body postures and musculoskeletal pain before and after the structured intervention program (time effect). A group t-test was used to analyse the second hypothesis, testing the difference in the risk factor scores for body postures and musculoskeletal pain between hospital nurses who participated in the intervention and the control group of hospital nurses who did not attend the intervention program (timeXgroup).
Statistical analysis was performed by a blinded statistician. Data were analyzed using IBM SPSS for Windows, version 19.
3Results
There were 31 participants who completed the study. Their age range was 30 to 64 with an average age of 50 (S.D. ± 9.2) years, an average total work time of 35.5 (S.D. ± 14.8) hours per week, and an average seniority in the specific ward of 16 (S.D. ± 9) years. There was no significant difference between the intervention and control groups in age, BMI, rates of smoking, occupational characteristics, levels of stress, control and autonomy in performing their job, or the baseline total number and type of musculoskeletal pain.
Thirty-nine nurses who either refused to participate or to complete the process were compared with the rest of the study population. There were no significant differences in age, total number of working years, or the total number of reported regions ofmusculoskeletal pain. The descriptive statistics of study participants are presented in Table 1.
The nurses who participated were involved in direct patient care in nine different wards: deliveryroom, labour room, nephrology, premature baby ward, internal medicine, surgery, oncology, urology,and intensive care. Difficult tasks that nurses descri-bed, and which were subsequently analysed with REBA, were related to tasks such as patient handling, awkward positions induced by restricted space in the ward environment, long periods of bending while sterilizing wound dressings, and changing urinary catheters and nasogastric tubes.
The frequency of LBP was the highest (44.32%), followed by neck (34.45%), shoulder (25/17%), wrist (24.37%), and knee (23.30%) pain. The frequency of pain in other body regions was less than 20% (Fig. 2).
Pain level reported (n = 31) ranged from 0–10 (numerical rating scale). The lowest mean score of pain level was for the forearm [0.55 (S.D. ± 1.73)], and the highest mean score was for the lower back [6.55(S.D. ± 2.16)]. The level of psychological demands and control at work ranged from 1–5 (Likert scale, 5 = high stress and low control). The lowest mean score of Karasek’s questionnaire was 2.71 (S.D. ± 0.61) and the highest score was 4.64 (SD ± 1.00). There was no significant difference in the scores on Karasek’s questionnaire before and after the intervention.
The first hypothesis was partially confirmed, there was a significant decrease in body posture scores after the structured intervention program (time effect among intervention group, n = 14) compared with the level before the intervention. The average REBA score before intervention was 6.35 (S.D. ± 2.76), and after intervention decreased to 2.07 (S.D. ± 1.14) (t = 5.75, p < 0.001). Among the control group, there were no significant differences before and after the intervention. The average REBA score before intervention was 7.17 ± 3.6, and after intervention was 6.35(S.D. ± 3.46) (t = 1.69, p = NS).
There were no significant differences in either the sum of body parts reported as uncomfortable or in level of musculoskeletal pain before and after the intervention in either group.
The second hypothesis was partially confirmed, there was a significant improvement in body postures of hospital nurses who participated in the intervention compared with the control group of hospital nurses who did not attend the intervention program (t = –4.42, p < 0.001). There was no significant difference in either the number of body parts with discomfort or in level of musculoskeletal pain between the two groups.
Figures 3 and 4 illustrate an overall decrease in REBA scores after the intervention in the study group (Fig. 3). This trend did not occur in the control group (Fig. 4).
In summary, there was a significant different in the REBA scores, and hence the body postures that are considered risk factors for work-related musculoskeletal disorders, before and after the structured intervention program. Nurses who participated in the intervention showed a significantly lower REBA score (that is, lower risk body postures) compared to the controls.
4Discussion
The major finding of this study is that a personal intervention program based on identifying individual ergonomic risk factors decreased the REBA scores for high risk postures six months after the start of a three-month intervention program. The decreased REBA scores for high risk postures in the intervention group were seen among all subjects. This differs to the control group in which some participants showed worse REBA scores at the end of the study.
The difference in scores between the intervention and control groups can be attributed to several factors. The interventions took place inside the ward so changes could be implemented within the usual work environment (e.g., adjusting the intravenous infusion stand to the height of the nurse when changing infusions, widening the space between cribs in the nursery to allow improved body position when taking care of babies, lowering the storage position of heavy equipment, and practicing the use of aid accessories). The study did not include a budget for acquiring new devices, so nurses were taught to use the available devices. For example, the nurses were advised to use a stool with wheels when treating patients in a low sitting position, to use wheeled tables to move various objects rather than to carry them by hand, and to use a stool (without wheels) when reaching for medications stored on high shelves. A practice run was performed within the work environment, and staff were encouraged to increase work awareness through cooperative feedback.
Our results are consistent with other studies which demonstrate the effectiveness of some uniform ergonomic interventions for nurses [21, 22, 28, 39]. It is unclear whether our individual approach is preferable. Both programs can be used together in order to enable on the one hand, a uniform ergonomic intervention, and on the other hand, specially designed, tailored intervention. Both address specific onsite ergonomic training and enable performance of a specially designed exercise programme according to nurses’ individual pain characteristics. Further studies are warranted to compare the effect of different programs to determine whether using them in conjunction with each other may have an added benefit.
The results also showed that a reduction in the biomechanical workload did not reduce musculoskeletal pain. This is consistent with other short-term studies that found that a change in behaviour did not necessarily result in pain reduction [40–45].
There are some limitations of our study. Firstly, the study had a short time frame. A longer follow-up period may either demonstrate a reduction in musculoskeletal pain, as has been reported in other studies using different methodologies [45–50] or may show that nurses come back to their previous ways of performing their jobs because they perceive no benefit following the prescribed changes.Secondly, there was no involvement in the ward with other staff members or with the administration in charge of variables that may cause stress.. This may explain the fact that the Karasak questionnaire scores were unchanged before and after the intervention. These findings are similar to those found by Martin et al. 2009 [48]. Thirdly, there was a low response rate by the nurses. Although there were no significant differences in bio-demographic variables between those who did and those who did not participate, we cannot rule out a response bias. The assigned randomized control methodology demonstrates that the methods improved working habits, but extrapolation to other cohorts may be unwarranted because the interventions are more likely to be successful in volunteers. The therapist who provided the intervention to the nurses was not blinded to participant group assignments. Another possible bias might occur while taking the photos by choosing to take a picture of the best posture after theintervention.
Although there was only one care provider, there was no risk of performance bias as far as the treatment is concerned because the control group received only written material. The intervention lasted only four meetings and outcome measures were collected three months after the last session of the intervention for both study and control groups. Larger studies with higher response rates in other settings, including male participants, fully blinded, and for a longer follow-up period are warranted.
In conclusion, the intervention program, which was based on Ratzon and Jarus’s four phases [25],used motor learning processes and considered ergo-nomic principles, led to a reduction in the REBA scores. Structured, personalized intervention programs for hospital nurses with musculoskeletal pain presents a challenge for the health professions to help nurses attain and maintain their roles while learning how properly to prevent WRMSDs.
Conflict of interest
None to declare.
References
[1] | Bureau of Labour statistics-U.S.D.L. Lost working Injuries and Illnesses: Characteristics and Resulting Time Away from Work. Washington, D.C(2002) :2–196. |
[2] | Bos E , Krol B , VanDerStar L , Groothoff J . Risk factors and musculoskeletal complaints in non-specialized nurses, IC nurses, operation room nurses and X-ray technologists. Int Arch Occup Environ Health (2007) ;80: (3):198–206. |
[3] | Carugno M , Pesatori A , Ferrario M , Ferrari A , Silva F , Martins A , Bonzini M . Physical and psychosocial risk factors for musculoskeletal disorders in Brazilian and Italian nurses. Cad Saude Publica (2012) ;28: (9):1632–1642. |
[4] | Sembajwe G , Tveito T , Hopcia K , Kenwood C , O’Day E , Stoddard A , Sorensen G . Psychosocial stress and multi-site musculoskeletal pain: A cross-sectional survey of patient care workers. Workplace health Saf (2013) ;61: (3):117–125. |
[5] | Bernar BP , Fine LJ . Musculoskeletal disorders and workplace factors. A critical review of epidemiologic evidence for work related musculoskeletal disorders of the neck, upper extremity and low back. U.S. Department of Health and human service. Orth Cli of N Am (1996) ;27: :679–709. |
[6] | Bruce PB . Musculoskeletal disorders and workplace factors. A Critical review of epidemiologic evidence for work related musculoskeletal disorders of the neck, UE and low back. Retrieved National Institution for Occupational Safety and Health Publication; (1997) :97–141. |
[7] | Waters T , Collins J , Galinsky T , Caruso C . NIOSH research efforts to prevent musculoskeletal disorders in the healthcare industry. Orth Nur (2006) ;25: :380–389. |
[8] | Ratzon NA , Jarus T . Musculoskeletal symptoms among dentists in Relation to Work Posture. Work: A Journal of Prevention, Assessment and Rehabilitation (2000) ;15: :153–158. |
[9] | Smedley J , Inskip H . Risk factors for incident neck and shoulder pain in hospital nurses. Occup Environ Med (2003) ;60: :864–869. |
[10] | Sadeghian , Farideh , et al. Predictors of incident and persistent Neck/Shoulder pain in iranian workers: A Cohort Study. PLoS One (2013) ;8: (2):e57544. |
[11] | Lahad A , Malter A , Berg AO , Dayo R . The effectiveness of four interventions for the prevention of low back pain. JAMA (1994) ;272: (16):1286–1291. |
[12] | Linton SJ , VanTulder MW . Preventive interventions for back and neck pain problems: What is the evidence? Spine (2001) ;26: (7):778–787. |
[13] | Engkvist IL . Evaluation of an intervention comprising a no lifting policy in Australian hospitals. Appl Ergon (2006) ;37: (2):141–148. |
[14] | Yassi A , Khokhar J , Tate R , Cooper J , Snow C , Vallentyne S . The epidemiology of back injuries in nurses at a large canadian tertiary care hospital: Implications for Prevention. Occup Med (1995) ;45: (4):215–220. |
[15] | Waters TR , Rockefeller K . Safe patient handling for rehabilitation professionals. Rehab Nurse (2010) ;35: (5):216–222. |
[16] | Nelson A , Matz M , Chen F , Siddharthan K , Lloyd J , Fragala G . Development and evaluation of a multifaceted ergonomics program to prevent injuries associated with patient handling tasks. Intern J Nurs Stud (2006) ;43: (6):717–733. |
[17] | Nelson A , Harwood K , Tracey C , Dunn K . Myths and facts about safe patient handling in rehabilitation. Rehabil Nurs (2008) ;33: (1):10–17. |
[18] | Ewert T , wert T , Limm H , Wessels T , Rackwitz B , von Garnier K , Freumuth R , Stucki G . The comparative effectiveness of a multimodal program versus exercise alone for the secondary prevention of chronic low back pain and disability. Phy Med & Reh (2009) ;1: (9):798–808. |
[19] | Szeto G , Wong T , Law R , Lee E , Lau T , So B , Law S . The impact of a multifaceted ergonomic intervention program on promoting occupational health in community nurses. Appl Ergon (2012) ;44: :414–422. |
[20] | Skargren E , Oberg B . Effects of an exercise program on musculoskeletal symptoms and physical capacity among nursing staff. Sca J of Reh Med (1996) ;6: (2):122–130. |
[21] | Bos E , Krol B , Vanderstar L , Groothoff J . The effects of occupational interventions on reduction of musculoskeletal symptoms in the nursing profession. Ergonomics (2006) ;49: (7):706–723. |
[22] | Svensson A , Stroyer J , Ebbehoj E , Schultz-Larsen K , Marott J , Mortensen O , Suadicani Multidimensional intervention and sickness in assistant nursing students. Occ Med (2009) ;59: (8):563–569. |
[23] | Goldgruber J , Ahrens D . Effectiveness of workplace health promotion and primary prevention interventions: A review. J Public Heal (2010) ;18: (1):75–88. |
[24] | Schmidt T , Lee T . Motor Learning and Performance, 5E With Web Study Guide: From Principles to Application. Hum Kinet (2013) ;24: :91–146. |
[25] | Ratzon NA , Jarus T . Prevention of workers’ musculoskeletal disorders: A Four- Stage Model. In: Söderback I ed, International Handbook of Occupational Therapy Interventions. New York, Springer: Dordrecht Heidelberg London; (2009) :507–514. |
[26] | Coyle A . Comparison of the rapid entire body assessment and the New Zealand manual handling hazard control record, for assessment of manual handling hazards in the supermarket industry. Work (2005) ;24: (2):111–116. |
[27] | Hignett S , Mctamney L . Rapid entire body assessment [REBA]. App Ergo (2000) ;31: (2):201–205. |
[28] | Janowitz IL , Gillen M , Ryan G , Rempel D , Trupin L , Swig L , Blanc P . Measuring the physical demands of work in hospital setting: Design and implementation of an ergonomics assessments. App Ergo (2006) ;37: (5):640–658. |
[29] | Kuorinka I , Jonsson B , Kilbom A , Vinterberg H , Biering-Sørensen F , Andersson G , Jorgensen K . Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. App Ergo (1987) ;18: (3):233–237. |
[30] | Karasek RA . Job demands, job decision latitude and mental strain: Implications for job redecision. Adm Sci Qua (1997) ;24: :285–308. |
[31] | McAtamney L . RULA and REBA in the real world. Proceedings of 11th conference of the New Zealand ergonomics society, New Zealand, November, (2002) :15–25. |
[32] | Ferraz MB , Quaresma MR , Aquino LRL , Atra E , Tugwell P , Goldsmith CH . Reliability of Pain Scales in the Assessment of Literate and Illiterate Patients with Rheumatoid Arthritis. J Rheumatol (1990) ;17: :1022–1024. |
[33] | Tortora GA , Grabowski SR . Principles of Anatomy and Physiology. 7th. Ed. Harper Collins College Publishers; (1992) . |
[34] | Konijnenberg HS , De Wilde NS , Gerritsen AA , Van Tulder MW , de Vet HC . Conservative treatment for repetitive strain injury. Scand J W , Enviro (2001) :299–310. |
[35] | Stanton N , Hedge A , Brookhuis K , Salas E , Hendrick H . Handbook of human factors and ergonomics method. CRC Press (2005) :8–10. |
[36] | Coury HJ , Moreira RF , Dias NB , Evaluation of the effectiveness of workplace exercise in controlling neck, shoulder and low back pain: A systematic review. Brazilian J PhysTher (2009) ;13: (6):461–479. |
[37] | Verhagen AP , Karels C , Bierma-Zeinstra SM , Burdorf L , Feleus A , Dahaghin S , Vet HCW , Koes BW . Ergonomic and physiotherapeutic interventions for treating work-related complaints of the arm, neck or shoulder in adults. Cochrane Database Syst Rev (2006) :3. |
[38] | O’Sulivan PB . Lumbar segmental “instability”: Clinical spesentation and specific stabilizing exercise management. Man Th (2000) ;5: (1):2–12. |
[39] | McCaffery M , Beebe A . Pain: Clinical Manual for Nursing Practice. Baltimore: V.V. Mosby Company. National Research Council, 2001–Musculoskeletal Disorders and the Workplace: Low Back and Upper Extremities . Washington, D.C.: National Academy Press; (1993) . |
[40] | National Research Council: Musculoskeletal disorders and the workplace: Low lack and upper extremities. National Academy Press. (2001) . |
[41] | Rackwotz B , Debie R , Limm H , VonGarnier K , Ewart T , Stucki G . Segmental stabilizing exercises and low back pain. What is the evidence? A systematic review of randomized controlled trials. Clin Reh (2006) ;20: (7):553–567. |
[42] | Collins JW , Wolf L , Bell J , Evanoff B . An evaluation of a “best practice musculoskeletal Injury prevention program in nursing homes. Inj Prev (2004) ;10: (4):206–211. |
[43] | Fanello S , Jousset N , Roquelaure Y , Frampas-Chotard V . Evaluation of a training program for the prevention of lower back pain among hospital employees. Nat Heal Ser (2002) ;4: (1-2):51–54. |
[44] | Johnsson C , Carlsson R , Lagerstrom M . Evaluation of training in patient handling and moving skills among hospital and home care personnel. Ergonomics (2002) ;45: (12):850–862. |
[45] | Lagerstrom M , Hagberg M . Evaluation of a 3 year education and training program For nursing personnel at a Swedish hospital. Am Ass of Occ Heal Nur (1997) ;45: (2):83–92. |
[46] | Peterson EL , McGlothlin JD , Bleu CL . The developments of an ergonomics training program to identify, evaluate, and control musculoskeletal disorders among nursing assistants at a state-run veterans’ home. J of Occl and Env HygD (2004) ;1: :10–16. |
[47] | Videman T , Rauhala H , Asp S . Patient-handling skill, back Injuries and back pain: An intervention study in nursing. Spine (1989) ;14: (2):148–156. |
[48] | Martin PJ , Harvey JT , Culvenor JF , Payne WR . Effect of a nurse back injury prevention intervention on the rate of injury compensation claims. J of Saf Res (2009) ;40: (1):13–19. |
[49] | Oldervoll LM , Ro M , Zwart JA , Svebak S . Comparison of two physical exercise programs for the early intervention of pain in the neck, shoulders and lower back in female hospital staff. J of Reh Med (2001) ;33: (4):156–161. |
[50] | Rasotto C , Bergamin M , Simonetti A , Maso S , Bartolucci GB , Ermolao A , Zaccaria M . Tailored exercise program reduces symptoms of upper limb work-related musculoskeletal disorders in a group of metalworkers: A randomized controlled trial. Manual Therapy (2015) ;20: (1):56–62. |
Figures and Tables
Fig.1
Random allocation sequence and participant flow.
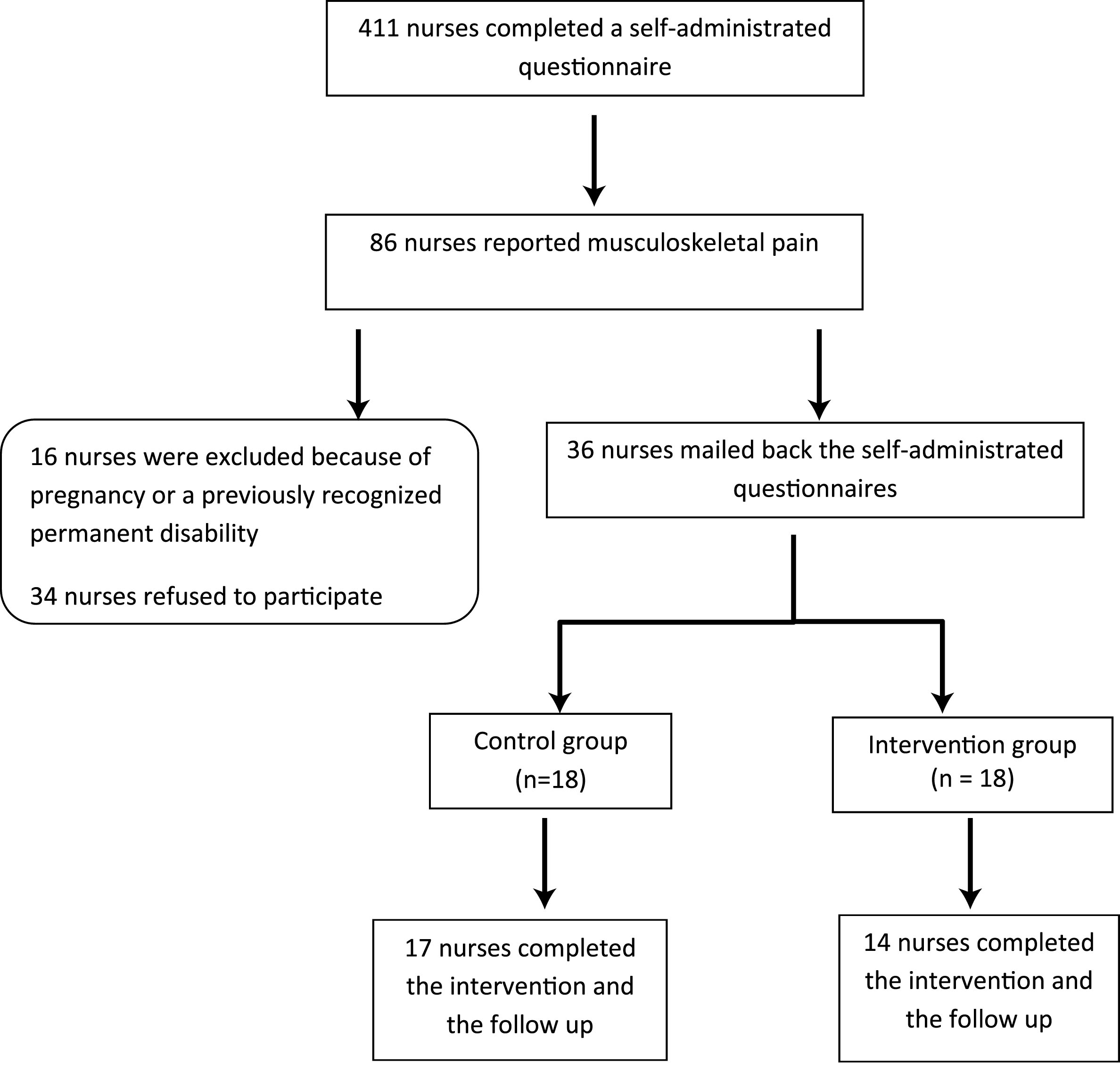
Fig.2
Frequency (%) of pain reported in the last week by participants [N = 31].
![Frequency (%) of pain reported in the last week by participants [N = 31].](https://content.iospress.com:443/media/wor/2016/54-2/wor-54-2-wor2340/wor-54-wor2340-g002.jpg)
Fig.3
Distribution of REBA scores for the intervention group before and after intervention [N = 14].
![Distribution of REBA scores for the intervention group before and after intervention [N = 14].](https://content.iospress.com:443/media/wor/2016/54-2/wor-54-2-wor2340/wor-54-wor2340-g003.jpg)
Fig.4
Distribution of REBA scores for the control group before and after intervention [N = 17].
![Distribution of REBA scores for the control group before and after intervention [N = 17].](https://content.iospress.com:443/media/wor/2016/54-2/wor-54-2-wor2340/wor-54-wor2340-g004.jpg)
Table 1
Descriptive statistics of demographic variables for the intervention and control group
| Variable | Mean | Std. Deviation | T | P | |
| Age (years) | Intervention (n = 14) | 51.28 | 7.55 | 1.075 | 0.29 |
| Control (n = 17) | 47.7 | 10.38 | |||
| BMI (weight/height2) | Intervention (n = 14) | 24.71 | 3.31 | –0.773 | 0.44 |
| Control (n = 17) | 25.75 | 3.99 | |||
| Working experience | Intervention (n = 14) | 26.71 | 10.20 | 0.421 | 0.67 |
| as a nurse (years) | Control (n = 17) | 25.11 | 10.74 | ||
| Working experience | Intervention (n = 14) | 18.64 | 8.63 | 0.732 | 0.47 |
| in the department (years) | Control (n = 17) | 16.08 | 10.43 | ||
| Working hours per week | Intervention (n = 14) | 33.28 | 7.53 | – | 0.29 |
| Control (n = 17) | 40.00 | 22.37 | 1.071 |
Table 2
Descriptive statistics of the REBA variable
| REBA before | REBA after | REBA difference (before-after) | |||||||||
| Mean | SD | 95% CI | Mean | SD | 95% CI | Mean | SD | 95% CI | Min | Max | |
| Intervention | 6.35 | 2.76 | 4.76–7.95 | 2.07 | 1.14 | 1.41–2.73 | 4.28 | 2.78 | 2.67–5.89 | 1 | 10 |
| Controls | 7.17 | 3.60 | 5.32–9.03 | 6.35 | 3.46 | 4.57–8.13 | 0.82 | 2.00 | –0.20–1.85 | –3 | 4 |




