Working dilemmas in care for breastfed newborns: An exploratory study in a single center in Taiwan
Abstract
BACKGROUND:
Clinical medical staff should be aware of and examine the correlation between breastfeeding and neonatal hospitalization. Additional attention should be paid to work dilemmas experienced by the nursing staff caring for newborns to avoid exposing newborns to hospitalization risk.
OBJECTIVE:
The present study investigated the working dilemmas by neonatal nurses caring for breastfed newborns and risk of newborn hospitalization.
METHODS:
This hospital-based study in Taiwan surveyed 84 neonatal nurses using a structured questionnaire entitled “Working Dilemmas in Clinical Care for Breastfed Newborns.”
RESULTS:
Collected data were analyzed statistically (descriptive analysis, chi-square test, and t test) using Statistical Package for the Social Sciences (SPSS) software. Neonatal intensive care unit (NICU) staff noted that breastfed newborns showed a high risk of hospitalization and nursery staff highlighted a lack of manpower and time. NICU staff experienced more working dilemmas (117.460±12.260) than nursery staff (87.410±15.820) when caring for breastfed newborns (t = 1.080, P < 0.001). NICU staff reported a higher risk of hospitalization in breastfed newborns and experienced more working dilemmas caring for these patients compared with nursery staff, who reported a lack of manpower and time.
CONCLUSION:
Our findings highlight the working dilemmas by neonatal nurses and can serve as a foundation for further critical studies.
1Introduction
Breastfeeding is the best source of nutrition for infants, to help reducing morbidity and mortality in children under five years of age, longer breastfeeding time, children have lower risk of infection and chronic diseases, and higher intelligence [1]. The baby-friendly hospital initiative (BFHI) promotes skin-to-skin contact between babies and their mothers and breastfeeding by practicing rooming-in. The BFHI was introduced in 1991 by the World Health Organization (WHO) and United Nations Children’s Fund as a comprehensive program to implement the Ten Steps to Successful Breastfeeding (Ten Steps) and the International Code of Marketing of Breastmilk Substitutes [2]. More than 600 BFHI hospitals offer maternity care for nearly 30% of women who give birth in the United States (US) [3]. The National Health Agency promotes breastfeeding policies by providing support to pregnant women from the prenatal stage to discharge. In 2018, the exclusive breastfeeding rate of infants and children aged <6 months in Taiwan was 46.2%, which is close to the WHO’s 2025 target value of 50% [4]. Various hospitals have made substantial efforts to promote the BFHI in response to the evaluation of maternal and child-friendly hospitals.
Among the ten most crucial measures required for maternal and child-friendly hospital certification in Taiwan, 24-h parent–child rooming is the least widely implemented [5]. In practice, exhaustion is very common in postpartum women, and those who have undergone a cesarean section are particularly prone to postpartum fatigue due to surgery followed by performing infant care activities [6]. In addition, meeting the requirements of the maternal and child-friendly hospital (e.g., 24-h parent–child rooming) following the exhausting process of labor may cause additional stress for many women [7].
Burnham et al. [8] interviewed maternity nurses at hospitals in Mississippi and reported the factors influencing the success or failure of BFHI implementation. Thus, these experiences encouraged the maternity nurses to learn and adapt. Nurses provide most of the direct care for women and their newborns, as defined in the Ten Steps. Successful BFHI implementation requires a rich understanding of nursing experience. As more US hospitals aim to implement BFHI, learning from facilities that have succeeded is vital and previous studies have discussed the developments required for BFHI success [9, 10].
Studies have demonstrated the benefits of baby-friendly practices (e.g., increased breastfeeding rate). Exclusively breastfed newborns tend to receive less milk and water than babies fed using other methods in the first week after birth [11–13]. A lack of appropriate supervision can increase the risk of injury in newborns. For example, the mother may fall asleep and cause the baby to fall off the bed or accidentally suffocate the baby [14, 15]. Some studies [16–20] have reported that breastfeeding can cause jaundice and weight loss. BFHI requires that rooming-in must be implemented in a safe environment; mothers feel that they cannot get appropriate rest when they agree to rooming-in after the delivery of their babies, which leads to further exhaustion. In addition, the lack of breast milk during the first stage of breastfeeding may increase the admission rate of newborns. Neonatal clinical care requires additional attention to avoid the exposure of newborns to hospitalization risk [21]. Therefore, the present study surveyed neonatal nurses at a medical center in central Taiwan to examine the clinical care working dilemmas by neonatal intensive care unit (NICU) and nursery nursing staff in terms of breastfeeding and newborn hospitalization.
2Methods
2.1Study design and setting
This was a descriptive cross-sectional study using convenient sampling of neonatal nurses from 26 November 2019 to 20 January 2020 at a medical center in central Taiwan.
2.2Participants
A total of 84 neonatal nurses at the NICU and nursery unit participated in this study. The staff work load between the two clinical areas as the provision of 1:4 (NICU) and 1:8 (nursery unit) nurse to patient ratios. The inclusion criteria of the participants were: (1) having obtained a practical or registered nurse license and working in a pediatric unit; (2) ability to communicate in Chinese and Taiwanese and read Chinese; (3) having cared for or taking care of either breastfed newborns aged < 5 days or roomed-in breastfed newborns with jaundice, hypoglycemia, or weight loss; and (4) willing to participate in the study. Nursing staff who failed to provide written informed consent were not eligible to participate in the present study.
2.3Data collection
Participants were given a questionnaire from the NICU and nursery unit by the visiting researcher, and were asked to complete the questionnaire themselves and return it to the researcher at a convenient time. The order of the questionnaire collection was used as the code.
2.4Measurements
The questionnaire used in the present study comprised two sections: (1) demographic data of nursing staff, including sex, age, educational level, marital status, whether they had children, and seniority (in terms of nursing work); and (2) Dilemmas in Clinical Care for Breastfed Newborns [22], which is detailed subsequently. Relevant literature from Taiwan and other countries served as the theoretical basis of this study and the foundation of the drafted questionnaire items and scales [9, 23, 24]. A structured questionnaire was compilated for data collection. The Scale of Working Dilemmas in Clinical Care for Breastfed Newborns section comprised 27 items rated on a 5-point Likert scale, with a maximum total score of 135, where a high the total score indicated greater clinical care working dilemmas. For example, “I believe that babies are subject to increased hospitalization or prolonged hospitalization risks when family members reject the use of baby formula to supplement breastfeeding”, “I think that not using a pacifier during the hospitalization will make it difficult for the nursing staff to take care of them and increase the working hours”, “I think that newborns within five days are likely to be hospitalized due to insufficient breastfeeding”, “I think that the nurses who work in the rooming-in constantly teach mothers to breastfeed at any time, but some mothers still cannot provide enough milk”, “I think that conflicts with breast milk occur when the mother is unable to provide enough breast milk and the baby is hospitalized” and “I think that providing breastfeeding knowledge and skills to pregnant women is time-consuming and is feasible only when there is enough manpower and time in clinical settings”. Five Taiwanese clinical experts, including one pediatric resident physician, two experienced nursing staff, and two clinical nursing teachers, were invited to verify the validity of this scale. The content validity index of this scale was 0.910 [22], with internal consistency confirmed by a Cronbach’s α-value of 0.960 [22]. The data collection process involved the researcher sending a questionnaire to the units. The questionnaire was completed within 10–15 min.
2.5Samples size calculation
We postulated that working dilemma with neonatal nurses through breastfeeding and neonatal hospitalization were moderately correlated (r = 0.300; statistical power = 80.0%). A two-tailed hypothesis test was conducted for the population correlation coefficient using a preset α-value of 0.050, and a minimum sample size of 84 was found to be required [25].
2.6Ethical considerations
This study was approved by the Institutional Review Board of Changhua Christian Hospital, Changhua, Taiwan (IRB No.: 190911). The researcher explained research objectives to the participants, who signed a consent form in person. The participants were asked to seal the completed questionnaire in a paper envelope prior to submission. The survey was conducted anonymously and the participant information remained confidential.
2.7Statistical analysis
All statistical data were analyzed using Statistical Package for the Social Sciences (SPSS) version 22.0. The demographic variables used distribution for participants using descriptive statistics. Proportions were compared by chi-square test. For inferential statistics, the demographic characteristics of participants and working dilemmas were analyzed using F test, the mean between NICU and nursery unit nursing staff were compared using t test. The questionnaire was personally sent to participants by a researcher who checked that all the questionnaires were completed and returned and no data were missed. The resulting content validity index was 0.920, confirming the questionnaire was appropriate and applicable. The reliability of this research was assessed using Cronbach’s α to assess internal consistency. Cronbach’s α was 0.961. For all statistical tests, P < 0.05 indicated significance.
3Results
3.1Demographic characteristics of participants
Among a total of 84 nursing staff who participated in the present study, all (100%) were female. The majority of the participants were age < 30 years (n = 46; 54.8%), graduated from university (n = 65; 77.4%), unmarried (n = 51; 60.7%), had no children (n = 56; 66.7%), and 29 (34.5%) of had seniority of > 10 years (Table 1). There were no significant differences in the demographic variables of the NICU staff (n = 45) and nursery staff (n = 39), as indicated by the chi-square test results. Differences in working dilemmas administering clinical care to breastfed newborns were compared between intensive care neonatal nurses and nursery staff as following.
Table 1
Demographic variables of the study participants
| Variable | Total nursing | NICU | Nursery | P-value |
| staff n % | staff n (%) | staff n (%) | ||
| Sex | 1.000 | |||
| Female | 84 (100.0) | 45 (100.0) | 39 (100.0) | |
| Male | 0 (0) | 0 (0) | 0 (0) | |
| Age | 0.665 | |||
| <30 years | 46 (54.8) | 24 (53.3) | 22 (56.4) | |
| 30–40 years | 23 (27.4) | 14 (31.1) | 9 (23.1) | |
| >40 years | 15 (17.9) | 7 (15.6) | 8 (20.5) | |
| Education level | 0.120 | |||
| Junior college | 19 (22.6) | 15 (33.3) | 4 (10.3) | |
| University | 65 (77.4) | 30 (66.7) | 35 (89.7) | |
| Married | 0.554 | |||
| Yes | 33 (39.3) | 19 (42.2) | 14 (35.9) | |
| No | 51 (60.7) | 26 (57.8) | 25 (64.1) | |
| Children | 0.643 | |||
| Yes | 28 (33.3) | 16 (35.6) | 12 (30.8) | |
| No | 56 (66.7) | 29 (64.4) | 27 (69.2) | |
| Seniority | 0.178 | |||
| <1 year | 3 (3.6) | 0 (0) | 3 (7.7) | |
| 1–4 years | 28 (33.3) | 17 (37.8) | 11 (28.2) | |
| 5–10 years | 24 (28.6) | 11 (24.4) | 13 (33.3) | |
| >10 years | 29 (34.5) | 17 (37.8) | 12 (30.8) |
3.2Analysis of the demographic characteristics of participants and working dilemmas
The results of the F test showed that the demographic characteristics on the age, marital status, whether they had children, and seniority (in terms of nursing work) were not significantly different among the participants with working dilemmas. Educational level was significant predictor (F = 7.390, P < 0.01) of working dilemmas (Table 2).
Table 2
Analysis of the demographic characteristics of participants and working dilemmas
| Variables | Working dilemmas | |||
| Mean±SD | F | P-value | ||
| Age | 1.719 | 0.186 | ||
| <30 years | 103.739±17.350 | |||
| 30–40 years | 108.173±24.255 | |||
| >40 years | 95.666±22.506 | |||
| Education level | 7.390 | 0.008* | ||
| Junior college | 114.368±16.180 | |||
| University | 100.338±20.691 | |||
| Married | 0.757 | 0.387 | ||
| Yes | 105.939±22.650 | |||
| No | 101.941±10.114 | |||
| Children | 0.096 | 0.757 | ||
| Yes | 104.500±23.364 | |||
| No | 103.017±19.177 | |||
| Seniority | 1.536 | 0.212 | ||
| <1 year | 80.666±26.388 | |||
| 1–4 years | 106.821±17.384 | |||
| 5–10 years | 102.333±18.972 | |||
| >10 years | 103.655±23.351 | |||
SD standard deviation. *P < 0.01.
3.3Highest-rated items in the working dilemmas in clinical care for breastfed newborns scale
Neonatal nurses were divided according to the unit they served into NICU staff and nursery staff. The highest-rated item in the Working Dilemmas in Clinical Care for Breastfed Newborns scale by the NICU staff was “I believe that babies are subject to increased hospitalization or prolonged hospitalization risks when family members reject the use of baby formula to supplement breastfeeding” (score, 4.680±0.460), whereas the highest-rated item by the nursery staff was “I think that providing breastfeeding knowledge and skills to pregnant women is time-consuming and is feasible only when there is enough manpower and time in clinical settings” (score, 4.250±0.880).
3.4Analysis of the working dilemmas in clinical care for breastfed newborns scale results
The results of the t test for the responses on the Working Dilemmas in Clinical Care for Breastfed Newborns scale showed significant differences (t = 1.080, P < 0.001) between NICU (117.460±12.260) and nursery staff (87.410±15.820). The NICU staff reported greater clinical working dilemmas when caring for breastfed newborns than nursery staff (Fig. 1; Table 3).
Fig. 1
Comparison of working dilemmas in caring for breastfed newborns.
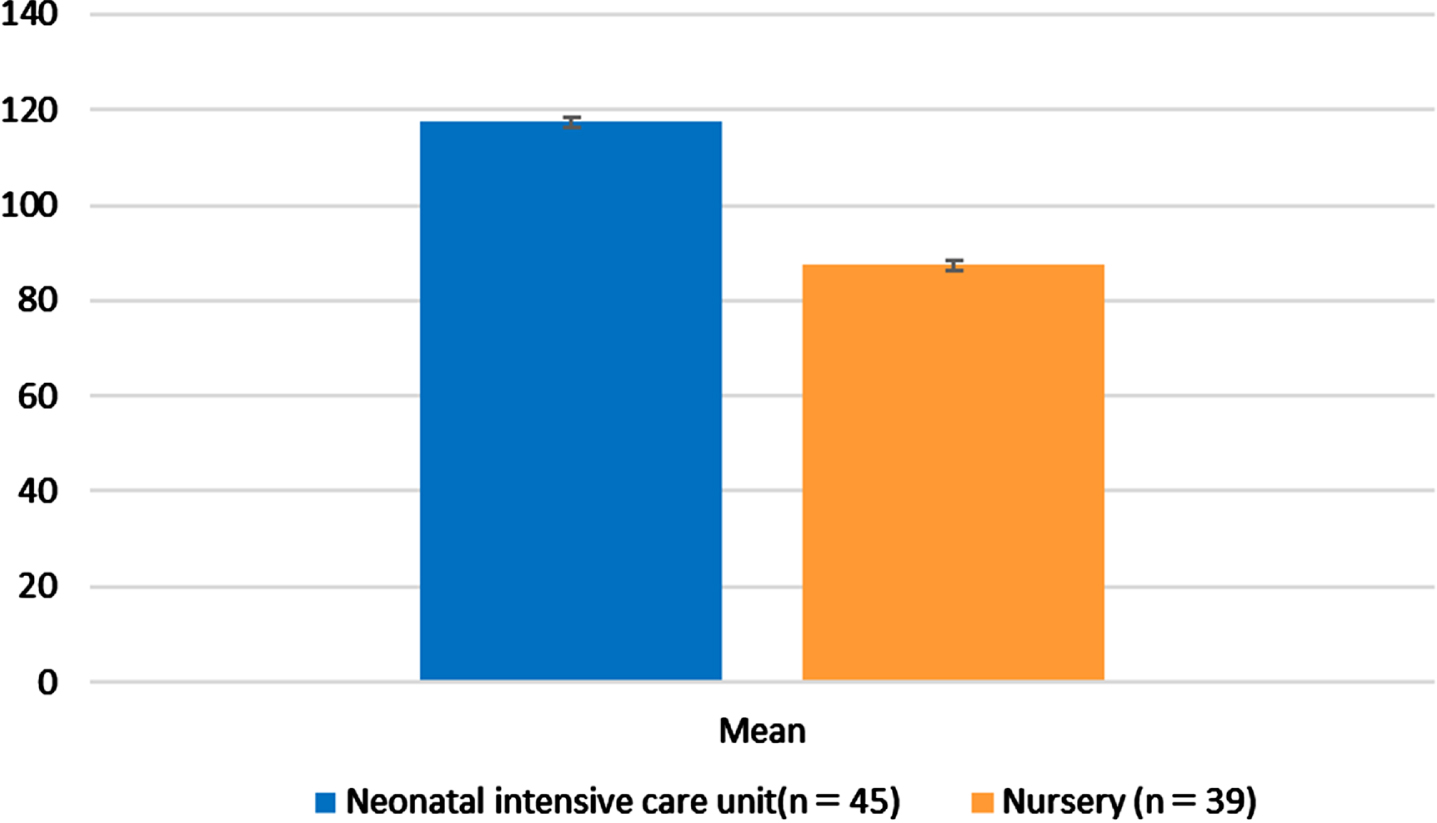
Table 3
Comparison of working dilemmas in caring for breastfed newborns between NICU staff and nursery staff
| Variables | Mean±SD | t | P-value |
| Hospital unit | 1.080 | 0.000** | |
| NICU (n = 45) | 117.460±12.260 | ||
| Nursery (n = 39) | 87.410±15.820 |
SD standard deviation. **P < 0.001.
4Discussion
In the present study, the highest-rated item in the Working Dilemmas in Clinical Care for Breastfed Newborns scale by the NICU staff was “I believe that babies are subject to increased hospitalization or prolonged hospitalization risks when family members reject the use of baby formula to supplement breastfeeding.” Chen et al. [26] also found similar results and reported that poor feeding practices can cause excessive weight loss and exclusive breastfeeding is a major risk factor for hyperbilirubinemia. In agreement with our findings, Fradkin et al. [27] reported that neonatal hyperbilirubinemia is commonly caused by inadequate breastfeeding. Flaherman et al. [28] showed that provision of a small amount of baby formula to breastfed newborns did not affect the breastfeeding rate within one month of birth and reduced the risk of hospitalization. These findings focus on clinical care working dilemmas based on the experience of the hospital providing postnatal care. It is possible that these issues can be resolved by providing adequate milk during rooming-in, which may reduce the risk of neonatal hospitalization due to hypoglycemia, weight loss, and hyperbilirubinemia.
In the present study, nursery staff reported that providing knowledge and skills for breastfeeding pregnant women is time-consuming and only feasible in settings with sufficient time and staff. Wieczorek et al. [29] found that nursing staff following the BFHI are required to dedicate additional time and effort toward clinical care, which can increase their workload. This finding concurs with the results of the present study. Walsh et al. [30] revealed that time is the most crucial resource required to implement BFHI and support breastfeeding women. Time pressure has become a problem for medical professionals, as confirmed by the findings of the present study, and is supported by the finding that it is time-consuming for nursing staff to impart breastfeeding knowledge and skills to breastfeeding women. Therefore, a lack of time or manpower in a clinical setting may result in failure to provide effective assistance with feeding, inadequate milk intake in newborns, clinical care dilemmas for nursing staff, and even neonatal hospitalization.
Therefore, this study to reflect the work dilemmas of the two units. The NICU staff work as a newborn hospitalization unit, the newborn hospitalization in this study refers to the newborns who are breastfed in rooming-in within 5 days after birth, to occurrence of jaundice, hypoglycemia and body weight loss and then need to be admitted in the hospital. The nursery staff work to care and feed newborns without jaundice, hypoglycemia and body weight loss. The challenges faced by the clinical care dilemma are different. NICU staff are facing high-risk newborns, so they face more clinical difficulties and care pressures. This echoes the literatures, such as NICU staff undertake related care tasks including feeding [31], respiratory care [32] and neonates requiring intensive medical care [33, 34]. However, the nursery staff are faced with healthy newborns, and the challenge is time pressure as pointed out in the literatures [29, 30], such as health education on breastfeeding knowledge and repeated teaching of breastfeeding skills, so it takes time. From the above, it can be seen that this study presents the differences in the work of the two units.
This study (Table 2) was significantly predictor of working dilemmas echoes the education level. The results showed that graduated from junior college had higher scores of working dilemmas than university graduated, which is consistent with the literature pointing out that education level and occupational category are influencing factors of job burnout [35] and work experience [36]. Higher emotional, social, family support and educational programs could have a positive impact with nursing staff [37, 38]. Improving work environment factors can enhance nursing staff’s comfort and improving organizational well-being [39], there is including nursing staff who can express their opinions; thus, nurse managers should provide such a working environment [40]. It is also hoped that the clinical working dilemmas of the NICU staff and nursery staff will be taken attention, including relevant professional training and courses, human resources and related their health and well-being for further exploring.
The results of the present study provide an understanding of the working dilemmas and concerns of the hospital unit staff when implementing the BFHI. In terms of clinical care for breastfed newborns, NICU staff reported that breastfed newborns have a high risk of hospitalization, whereas the nursery staff highlighted a lack of manpower and time.
A comparison of the results of the Working Dilemmas in Clinical Care for Breastfed Newborns scale between NICU staff and nursery staff (Fig. 1; Table 3) revealed a significant difference between the nursing staff in the two units. The staff of the NICU showed a significantly greater agreement with the “Working Dilemmas in Clinical Care for Breastfed Newborns” than the nursery staff. Thus, from a clinical care point of view, future studies focusing on these factors are required to address nursing care dilemmas experienced by neonatal nurses.
The strengths of the present study include that the findings identified working dilemmas by neonatal nurses in clinical care. The present study aimed to elucidate the problems related to caring for breastfed newborns and highlighted the additional time and efforts required for nursing staff to implement BFHI, which inspires further critical thinking. In particular, implementing BFHI requires the allocation of sufficient time and human resources, assignment of sufficient pediatric care, and reduced tension between mothers and their newborns.
The present study has one limitation related to the data collection with convenience sampling used to resolve the lack of time and manpower. This study considered the statistical power when estimating the required sample size and confirmed that the results derived from the sample should reflect the working dilemmas in care for breastfed newborns between NICU staff and nursery staff. Nevertheless, the present study only included one children’s hospital in central Taiwan, which may reduce the generalizability of the results. Future studies that include samples from different geographical areas, urban and rural, to enhance comprehensiveness of the obtained results are required. In clinical setting, to explore of the reason for the increased working dilemmas in the NICU compared to nursery staff word give more depth to results.
5Conclusion
The present study revealed that NICU staff experienced more working dilemmas caring for breastfed newborns than nursery nursing staff. Our findings revealed the working dilemmas by nursing staff to implement clinical care and serve as a foundation for further critical studies.
Ethical approval
Ethical permission was obtained from the Institutional Review Board of Changhua Christian Hospital, Changhua, Taiwan (IRB No.: 190911).
Informed consent
Informed consent was obtained from all participants before their participation in the study.
Conflict of interest
The authors have no conflict of interest to disclose.
Acknowledgments
The authors thank the participants for their time and valuable contribution.
Funding
This study was funded by the Department of Nursing, Da-Yeh University, Research Room PX407.
References
[1] | Hsieh PC , Ho YJ . Exploration of the Correlation between Social Support and Breastfeeding Attitudes of Postpartum Women. Cheng Ching Medical Journal. (2023) ;19: :49–61. doi: 10.3015/CCMJ. |
[2] | United Nations Children’s Fund. The baby-friendly hospital initiative. 2005(cited 2021 Jan 12). Available from https://www.unicef.org/nutrition/index_24806.html. |
[3] | Baby-friendly USA. Find à baby-friendly facility. 2020(cited 2021 May 1). Available from https://www.babyfriendlyusa.org/for-parents/find-a-baby-friendly-facility/. |
[4] | The Ministry of Health and Welfare. Nationwide breastfeeding rate survey. 2018(cited 2021 May 1).Available from https://www.hpa.gov.tw/Pages/Detail.aspx?nodeid=3804&pid=11264. |
[5] | Cai ZH , Peng TC , Lai HL , Wang SF . Influential factors related to rooming-in care. VGH Nurs. (2016) ;33: :283–92. doi: 10.6142/VGHN.33.3.283. |
[6] | Lai YL , Hung CH , Stocker J , Chan TF , Liu Y . Postpartum fatigue, baby-care activities, and maternal–infant attachment of vaginal and cesarean births following rooming-in. Appl Nurs Res. (2015) ;28: :116–20. doi: 10.1016/j.apnr.2014.08.002. |
[7] | Tsai SS , Yang MS , Wang HH . The efficacy of rooming-in in the context the physical and mental health of new mothers. Hu Li Za Zhi J Nurs. (2016) ;63: :119–25. doi: 10.6224/JN.63.3.119. |
[8] | Burnham L , Gambari A , Beliveau P , Ustianov J , Parker MG , Merewood A . Perspectives of nurses in Mississippi on implementation of the baby-friendly hospital initiative. J Obstet Gynecol Neonatal Nurs. (2021) ;50: :392–401. doi: 10.1016/j.jogn.2021.02.010. |
[9] | Cunningham EM , Doyle EI , Bowden RG . Maternity nurses’ perceptions of implementation of the ten steps to successful breastfeeding. MCN. Am J Matern Child Nurs. (2018) ;43: :38–43. doi: 10.1097/NMC.0000000000000392. |
[10] | Lundeen S , Sorensen S , Bland M , George S , Snyder B . Nurses’ perspectives on the process of attaining baby-friendly designation. Nurs Women’s Health. (2016) ;20: :277–87. doi: 10.1016/j.nwh.2016.03.004. |
[11] | Chen CF , Hsu MC , Shen CH , Wang CL , Chang SC , Wu KG , et al., Influence of breast-feeding on weight loss, jaundice, and waste elimination in neonates. Pediatr Neonatol. (2011) ;52: :85–92. doi: 10.1016/j.pedneo.2011.02.010. |
[12] | Chang RJ , Chou HC , Chang YH , Chen MH , Chen CY , Hsieh WS , et al., Weight loss percentage prediction of subsequent neonatal hyperbilirubinemia in exclusively breastfed neonates. Pediatr Neonatol. (2012) ;53: :41–4. doi: 10.1016/j.pedneo.2011.11.008. |
[13] | Flaherman VJ , Schaefer EW , Kuzniewicz MW , Li SX , Walsh EM , Paul IM . Early weight loss nomograms for exclusively breastfed newborns. Pediatrics. (2015) ;135: :e16–23. doi: 10.1542/peds.2014-1532. |
[14] | Barbaglia M , Finale E , Noce S , Vigo A , Arioni C , Visentin R , et al., Skin-to-skin contact and delivery room practices: a longitudinal survey conducted in Piedmont and the Aosta Valley. Ital J Pediatr. (2019) ;45: :95. doi: 10.1186/s13052-019-0688-9. |
[15] | Killion MM Skin-to-skin care and rooming-in: safety considerations MCN. Am J Matern Child Nurs. (2017) ;42: :115. doi: 10.1097/NMC.0000000000000320. |
[16] | Boskabadi H , Rakhshanizadeh F , Zakerihamidi M . Evaluation of maternal risk factors in neonatal hyperbilirubinemia. Arch Iran Med. (2020) ;23: :128–40. |
[17] | Hassan B , Zakerihamidi M . The correlation between frequency and duration of breastfeeding and the severity of neonatal hyperbilirubinemia. J Matern -Fetal Neonatal Med. (2018) ;31: :457–63. doi: 10.1080/14767058.2017.1287897. |
[18] | Huang HC , Yang HI , Chang YH , Chang RJ , Chen MH , Chen CY , et al., Model to predict hyperbilirubinemia in healthy term and near-term newborns with exclusive breast feeding. Pediatr Neonatol. (2012) ;53: :354–8. doi: 10.1016/j.pedneo.2012.08.012. |
[19] | Miyoshi Y , Suenaga H , Aoki M , Tanaka S . Determinants of excessive weight loss in breastfed full-term newborns at a baby-friendly hospital: a retrospective cohort study. Int Breastfeed J. (2020) ;15: :19. doi: 10.1186/s13006-020-00263-2. |
[20] | Yang WC , Zhao LL , Li YC , Chen CH , Chang YJ , Fu YC , et al., Bodyweight loss in predicting neonatal hyperbilirubinemia 72 hours after birth in term newborn infants. BMC Pediatr. (2013) ;13: :145. doi: 10.1186/1471-2431-13-145. |
[21] | Anderson PO . Breastfeeding and respiratory antivirals: coronavirus and influenza. Breastfeed Med. (2020) ;15: :128. doi: 10.1089/bfm.2020.29149.poa. |
[22] | Syue JC Discussion on factors related to breastfeeding and neonatal hospitalization by nursing staff. 2020 (cited 2020 July 1). Available from https://hdl.handle.net/11296/qxws35. |
[23] | Chu KH , Sheu SJ , Hsu MH , Liao J , Chien LY . Breastfeeding experiences of Taiwanese mothers of infants with breastfeeding or breast milk jaundice in certified baby-friendly hospitals. Asian Nurs Res. (2019) ;13: :154–60. doi: 10.1016/j.anr.2019.04.003. |
[24] | McRae MJ . Exclusive breastfeeding, 24-hour rooming-in, and the importance of women’s informed choices. Nurs Women’s Health. (2019) ;23: :309–15. doi: 10.1016/j.nwh.2019.05.003. |
[25] | Thiemann S , Kraemer HC How Many Subjects? Statistical Power Analysis in Research. Newbury Park, CA: Sage; 1987. |
[26] | Chen YJ , Chen WC , Chen CM . Risk factors for hyperbilirubinemia in breastfed term neonates. Eur J Pediatr. (2012) ;171: :167–71. doi: 10.1007/s00431-011-1512-8. |
[27] | Fradkin EC , Lafferty MA , Greenspan JS , Aghai ZH . Neonatal intensive care unit admissions before and after the adoption of the baby friendly hospital initiative. J Matern-Fetal Neonatal Med. (2022) ;35: :657–62. doi: 10.1080/14767058.2020.1730796. |
[28] | Flaherman VJ , Narayan NR , Hartigan-O’Connor D , Cabana MD , McCulloch CE , Paul IM . The effect of early limited formula on breastfeeding, readmission, and intestinal microbiota: a randomized clinical trial. Jurnalul Pediatrului. (2018) ;196: :84–90.e1. doi: 10.1016/j.jpeds.2017.12.073. |
[29] | Wieczorek CC , Schmied H , Dorner TE , Dür W . The bumpy road to implementing the Baby-Friendly Hospital Initiative in Austria: a qualitative study. Int Breastfeed J. (2015) ;10: :3. doi: 10.1186/s13006-015-0030-0. |
[30] | Walsh AD , Pincombe J , Henderson A . An examination of maternity staff attitudes towards implementing Baby Friendly Health Initiative (BFHI) accreditation in Australia. Matern Child Health J. (2011) ;15: :597–609. doi: 10.1007/s10995-010-0628-1. |
[31] | Huang YT , Tseng SF , Chiu YT , Lee MY , Chen LC . Reducing the incidence of feeding intolerance in premature infants in the neonatal intensive care unit. Hu Li Za Zhi J Nurs. (2022) ;69: :77–84. doi: 10.6224/JN. |
[32] | Huang YT , Lee MY , Liao HY , Chang CC . Increasing the rate of completion of the therapeutic hypothermia procedure in the NICU. Hu Li Za Zhi J Nurs. (2020) ;67: :72–80. doi: 10.6224/JN.202008_67(4).09. |
[33] | Huang YT , Jiang HY , Li CM , Lee MY , Chen LC . Improve the completion rate of ECMO placement assistance for nurses in the NICU. Hu Li Za Zhi J Nurs. (2023) ;70: :70–7. doi: 10.6224/JN.202302_70(1).10. |
[34] | Wang LY , Chen Yl , Fann GL . Nursing experience of caring for anewborn with congenital pulmonary airway malformation. NationalTaiwan University Hospital Journal of Nursing. (2023) ;19: :61–72. doi: 10.6740/ntuhjn.202301_19(1).0007. |
[35] | Abareshi F , Salimi F , Farnia F , Fallahi M , Rastaghi S . The impact of mental workload, work-related and socio-demographic factors on job burnout among emergency medical staff. Work. (2022) ;72: :1269–77. doi: 10.3233/wor-210001. |
[36] | Afshari D , Nourollahi-darabad M , Chinisaz N . Demographic predictors of resilience among nurses during the COVID-19 pandemic. Work. (2021) ;68: :297–303. doi: 10.3233/wor-203376. |
[37] | Izadi N , Saraie M , Aminian O , Forouzan N . Occupational stress and job performance among Iranian hospital nurses: A cross-sectional survey. Work. (2023) ;74: :1437–45. doi: 10.3233/wor-211015. |
[38] | Nemati R , Moradi A , Marzban M , Farhadi A . The association between moral distress and mental health among nurses working at selected hospitals in Iran during the COVID-19 pandemic. Work. (2021) ;70: :1039–46. doi: 10.3233/wor-210558. |
[39] | Mannocci A , Marigliano M , La Torre G . An assessment of organizational well-being, organizational health, and work-related stress: A cross-sectional study of nurses involved with COVID-19 interventions. Work. (2023) ;75: :29–39. doi: 10.3233/wor-220274. |
[40] | Yağar F , Dökme Yağar S . The effects of organizational silence on work engagement, intention to leave and job performance levels of nurses. Work. (2023) ;75: :471–8. doi: 10.3233/wor-210192. |




