Mercury air, urine monitoring and health effects on occupationally exposed dental healthcare workers in Delhi, India
Abstract
BACKGROUND:
Mercury (Hg) is a toxic heavy metal with multiple uses in various medical devices. Hg is used in dentistry as a restorative material. Such use creates significant exposure to dental practitioners. Hence, it is important to assess the risk created by Hg use in healthcare.
OBJECTIVE:
To quantify airborne Hg vapour exposure and Hg levels in dental healthcare workers, and determine the association of various symptoms and diseases to Hg exposure.
METHODS:
Air monitoring of Hg vapours were conducted in dental clinics and amalgam rooms. Urine samples were collected from occupationally exposed dental healthcare workers and urine Hg levels were measured. A cross-sectional health survey was conducted in 23 healthcare units of Delhi to determine an association between Hg exposure and various health effects.
RESULTS:
Hg vapour concentration ranged from 0.96μg/m3 to 15μg/m3, the highest concentration was recorded in the amalgam room (15μg/m3). Urine Hg levels in healthcare workers (0.51±0.17μg/L) were higher than the control (0.29±0.05μg/L). A cross-sectional health survey revealed a significant prevalence of confusion, forgetfulness, muscle spasm, and tremors by the respondents.
CONCLUSION:
Hg concentration in dental clinics may hover above the prescribed safe levels posing a definitive health risk to healthcare workers. Urinary Hg measurements did not reveal an excess of body burden except in one case. Since Hg bio accumulates, it is probable as these workers grow older, they may end up with a higher body burden of Hg that may lead to a variety of adverse health outcomes.
1Introduction
Mercury (Hg) is a toxic heavy metal which exists as metallic, inorganic, and organic species. It is released into the atmosphere as vapours released by elemental mercury (Hg (0)) from both anthropogenic and natural sources. Hg is deposited in water bodies and soil by precipitation, where microbial actions convert it into methyl mercury. The methyl mercury efficiently enters the marine food web through phytoplankton [1].
According to a 2007 estimate by the World Health Organization (WHO), healthcare facilities are responsible for up to 5% of the Hg waste that ends up in the environment [2]. The United States Environmental Protection Agency (USEPA) (2002) report revealed that 13% of all atmospheric Hg emissions in the US were caused by medical waste incinerators [3]. Thermometers, sphygmomanometers, medicines (Merbromin), vaccines (Thiomersal), gastrointestinal tubes, and electrical devices are common mercury-containing medical devices used in healthcare institutions [4]. The average elemental mercury content of a mercury thermometer is between 0.5 and 1.5 g, while that of a typical sphygmomanometer is between 80 and 100 g [5]. Hg contamination has a significant impact on the environment, considering that a single thermometer is enough to contaminate an 8.1-hectare lake, giving rise to adverse health risks for the general population [6]. Also, Hg is extensively used in dentistry as a restorative material. A previous study has documented that the average person with dental amalgam gets 10 times as much daily Hg exposure as the average person without any amalgam filling [7]. The healthcare industry is one of the largest reservoirs of Hg because hundreds of metric tonnes of Hg are used annually to manufacture dental amalgam, sphygmomanometers, and mercury thermometers [8].
Since elemental Hg has a relatively low vapour pressure (1.8μgHg) and is very volatile at ambient temperature, it can easily reach hazardous levels in the air during restorative procedure (trituration, mulling, condensation, carving, and polishing) and removal of restorative material [9]. Therefore, exposure to Hg in a poorly ventilated room could cause significant health risks to not only healthcare workers but also to patients and their families. Previous studies have reported that occupational exposure to Hg in dentists and dental assistants leads to irritation, headaches, neurobehavioral consequences (memory loss, depression, behavioural abnormalities, sleep, and personality alterations), and arthralgias [10–12]. Also, a study in nursing professionals has suggested certain associations between Hg exposure and Parkinson, Alzheimer, arthritis, negative effects on the thymus gland, and the psychomotor development of nurses’ children[13, 14].
Owing to the significant health risk posed by Hg in healthcare, the main objectives of this study were, (1) to quantify exposure to airborne Hg vapour, (2) to investigate urine Hg levels in occupationally exposed dental healthcare workers, and (3) to determine the association of various symptoms and diseases as a result of Hg exposure.
2Materials and methods
2.1Study area
The study was conducted in dental units of 22 healthcare establishments in Delhi, India. Hospitals from both government and private sectors were selected based on the relevance outlined in the scope of the study. A total of 17 hospitals with more than 500 beds were selected namely, All India Institute of Medical Science (AIIMS), Maulana Azad Institute of Dental Sciences (MAIDS), G.B. Pant Hospital, Lok Nayak Hospital, Safdarjung Hospital, ESI Basai Darapura, RML Hospital, Lady Harding Medical College, Deen Dayal Upadhyay Hospital, GTB Hospital, Baba Saheb Ambedkar Hospital, Rajan Babu TB Hospital, LRS Institute of TB, Sir Ganga Ram Hospital, Apollo Hospital, St. Stephens Hospital, and Hindu Rao Hospital. 5 hospitals with 52 to 100 beds were selected namely, ESI Jhilmil, Sitaram Bhartiya Institute of Science and Research, Aruna Asaf Ali Hospital, Swami Dayanand Hospital, and Charak Palika Hospital.
2.2Air monitoring of mercury vapours
In June 2014, a total of two air samples were collected in the Maulana Azad dental treatment areas, and one sample was collected from a private hospital (St. Stephens Hospital). In March 2015, a total of eight samples were collected in the Maulana Azad dental treatment areas. All samples were area samples and were not collected in the breathing zone. Additionally, none of the samples were collected for an entire work shift. Sampling time ranged from 107 minutes to 252 minutes. All samples were collected and analysed according to Method number 6009 of the United States National Centre for Occupational Safety and Health (NIOSH) Manual of Analytical Methods [15].
2.3Urine mercury investigations
20 ml of aliquot of urine was collected in a metal-free container (Tarsons) and further analysis was made with the help of Inductively Coupled Plasma-Mass Spectrometry (ICP-MS) Agilent (In House Method). Urine samples were collected from 65 healthcare workers occupationally exposed to Hg from MAIDS and 32 controls without occupational exposure. Participants were selected after considering inclusion and exclusion criteria. Only apparently healthy individuals were included in the study and individuals under treatment for tuberculosis, cancer, and chronic heart, lung, or kidney ailments were excluded. Also, pregnant, and lactating women were not included as these conditions might modify the results.
2.4Cross-sectional health survey
A cross-sectional health survey was conducted in the selected healthcare units, using a convenient sampling technique. Visual inspection was also carried out which enabled the team to anticipate/ identify potential sources of Hg exposure, identifying locations for taking personal and area samples. A total No. of 632 healthcare workers was randomly selected for the study purpose from various healthcare units. These hospitals were visited to let the participating healthcare workers fill in a general health survey form.
2.5Statistical analysis
The data collected in the form of a questionnaire was analysed using SPSS version 20 statistical software. Comparison of mean and standard deviation among the group was calculated using an unpaired t-test. Pearson’s chi-square test was used to determine the association of diseases with Hg exposure.
3Results
3.1Air monitoring of mercury vapours
Data regarding Hg vapours are tabulated in Table 1. In samples collected in June 2014, concentrations ranged from 2.4μg/m3 to 15μg/m3. In samples collected in March 2015, concentrations ranged from 0.96μg/m3 to 4.0μg/m3. These concentrations are lower than those observed in June 2014 at Maulana Azad Dental Units which ranged from 2.4μg/m3 to 15μg/m3. The American Conference of Governmental Industrial Hygienist Threshold Limit Value (TLV) for elemental Hg is 25μg/m3 [16]. The concentrations observed as a result of the sampling that was conducted were all below the TLV; however, it is important to note that none of these samples were collected for an entire eight-hour shift and thus should not be compared to the TLV for the purposes of determining potential overexposure.
Table 1
Mercury vapour sampling results
| June 2014 samples | |||
| S. No. | Location | Sampling duration | Concentration |
| 1 | Maulana Azad Dental Clinic | 252 minutes | 2.4μg/m3 |
| 2 | St. Joseph’s Hospital Dental Clinic | 107 minutes | 2.4μg/m3 |
| 3 | Maulana Azad Amalgam Room | 150 minutes | 15μg/m3 |
| 4 | COEH Office (Control sample) | 147 minutes | <0.31μg/m3 |
| March 2015 samples | |||
| 1 | Maulana Azad Dental Clinic | 206 minutes | 0.96μg/m3 |
| 2 | Maulana Azad Amalgam Room | 172 minutes | 2.4μg/m3 |
| 3 | Maulana Azad Dental OPD Clinic | 278 minutes | 2.1μg/m3 |
| 4 | Maulana Azad Amalgam Room | 302 minutes | 3.5μg/m3 |
| 5 | Maulana Azad Dental OPD Clinic | 275 minutes | 2.1μg/m3 |
| 6 | Maulana Azad Amalgam Room | 250 minutes | 4.0μg/m3 |
| 7 | Maulana Azad Dental OPD Clinic | 248 minutes | 2.5μg/m3 |
| 8 | Maulana Azad Dental OPD Clinic | 259 minutes | 1.8μg/m3 |
3.2Urine mercury investigations
A total of 65 healthcare workers and 32 controls participated in the sampling analysis of urine Hg levels. The results are tabulated in Table 2. The mean value of urinary Hg in healthcare workers and controls are 0.51±0.17μg/L and 0.29±0.05μg/L respectively. All the Hg levels were below the reference range (5.0μg/L) except one sample (11.2μg/L).
Table 2
Urinary Hg levels in healthcare workers and controls
| Healthcare workers (μg/L) | Controls (μg/L) | |
| N | 65 | 32 |
| Mean | 0.51 | 0.29 |
| Std. error of mean | 0.17 | 0.05 |
| Median | 0.2 | 0.2 |
| Std. deviation | 1.4 | 0.28 |
| Range | 11 | 1.4 |
| Minimum | 0.2 | 0.2 |
| Maximum | 11.2 | 1.6 |
3.3Details of population under study
The details of the participants selected for the study are tabulated in Table 3. 632 healthcare workers were selected for the survey. As regards gender distribution, 114 were males and 518 were females. A total of 67.1% subjects were using Hg-containing instruments during their work, out of which 33.3% reported direct exposure to Hg vapours. 47% of subjects were using Hg-containing thermometers in hospitals, 65% were using Hg-containing BP Apparatus, and another 12 per cent used fluorescent lamps, only 3 per cent were using dental amalgam containing elemental mercury.
Table 3
Details of population under study
| Frequency (n) | Percentage (%) | |
| Gender distribution | ||
| Male | 114 | 18.0 |
| Female | 518 | 82.0 |
| Total | 632 | 100.0 |
| Use of mercury containing instrument/ equipment | ||
| Yes | 424 | 67.1 |
| No | 173 | 27.4 |
| No answer | 35 | 5.5 |
| Exposure to mercury vapours | ||
| Yes | 141 | 22.3 |
| No | 435 | 68.8 |
| No answer | 56 | 100 |
| Frequency of use of instruments containing mercury | ||
| Rarely | 194 | 30.7 |
| Usually | 183 | 28 |
| Frequently | 201 | 31.8 |
| No answer | 54 | 8.5 |
| Use of mercury containing instruments | Yes percentage | |
| Thermometers | 47 | |
| BP Apparatus | 65 | |
| Fluorescent Lamps | 12 | |
| Dental Amalgam | 13 | |
3.4Cross-sectional health survey
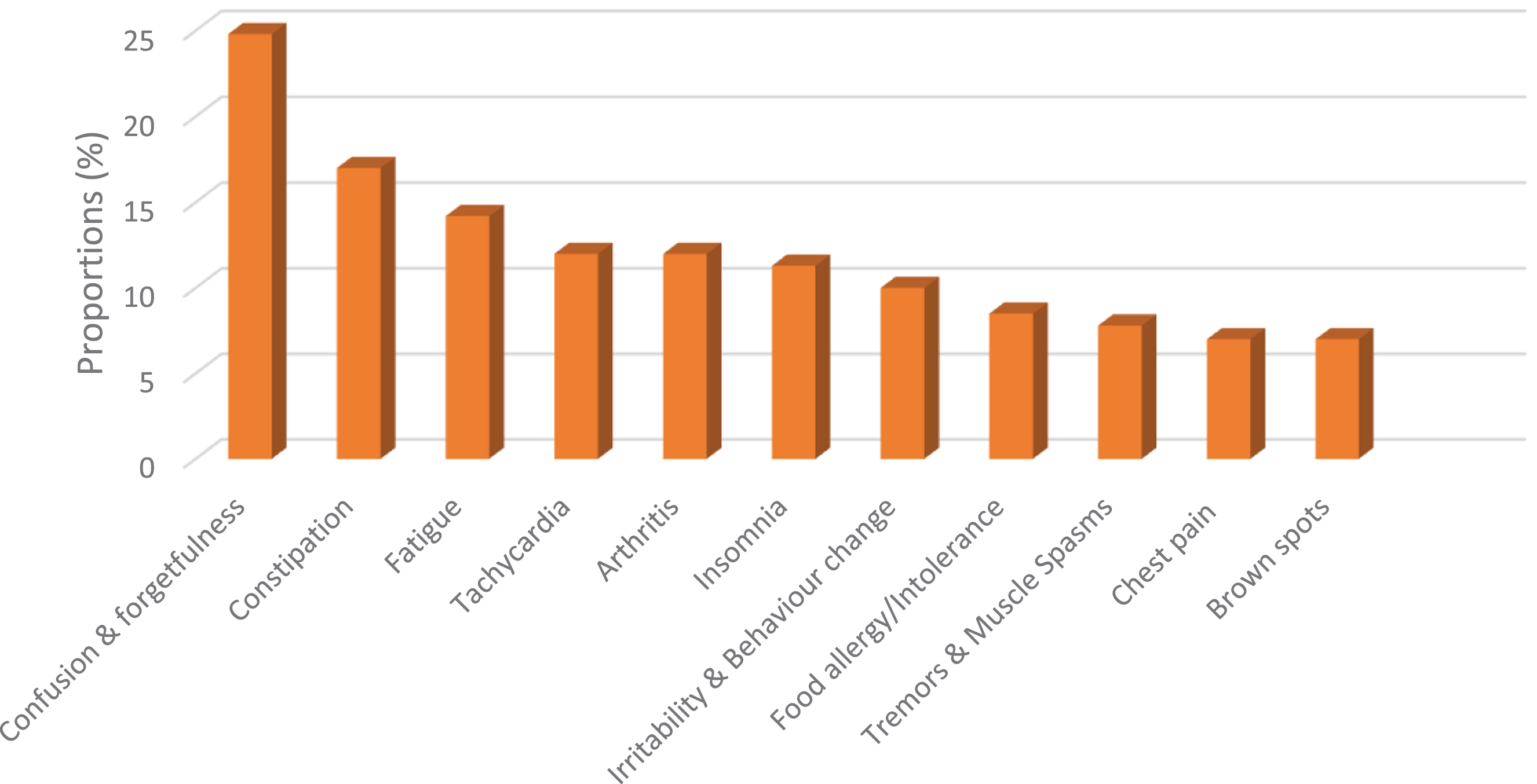
A cross-sectional health survey was conducted among healthcare workers to determine if there is any association between Hg exposure and adverse health effects. Out of 632 participants, 141 were occupationally exposed to Hg vapours. Among the exposed group, 35 (24.8%) reported confusion and forgetfulness, 24 (17%) experienced chronic constipation, 20 (14.2%) had fatigue, 17 (12%) had tachycardia, 17 (12%) had arthralgia, 16 (11.3%) had insomnia, 14 (10%) suffered from irritability and change in behaviour, 12 (8.5%) had food allergy/Intolerance, 11 (7.8%) experienced tremors and muscle spasms, 10 (7%) reported unidentified chest pain with normal ECG and X-ray, and another 10 (7%) reported having dark spots under the eyes. Figure 1 highlights these results. Among the various health effects, confusion and forgetfulness, chronic constipation, fatigue, arthralgia, insomnia, irritability and change in behaviour, food allergy/Intolerance and chest pain were statistically significant(p-value < 0.05).
Fig. 1
Distribution of health condition reported by healthcare workers occupationally exposed to Hg.
4Discussion
This is one of the first studies in dental healthcare units that provide information about Hg vapours concentration in dental clinics, and urinary Hg levels in occupationally exposed healthcare workers in Delhi. Furthermore, a questionnaire-based cross-sectional study was conducted to see if there is any association between Hg exposure and symptoms related to various organ systems.
In our study, air monitoring of Hg vapours was conducted by a certified industrial hygienist to assess the ambient air quality in the workplace which affects the healthcare worker as well as the patients. Air monitoring was done in the dental clinic and amalgam room. Hg vapour concentration ranged from 0.96μg/m3 to 15μg/m3. These values are higher than the control (<0.31μg/m3), but were lower than the TLV of OSHA, ACGIH, and NIOSH. Hg vapour concentration higher than 10μg/m3 poses a risk, especially to pregnant women [17]. Thus, the Hg vapour in the workroom air of the dental clinic represents a significant inhalational risk to workers. The amalgam room is of particular concern due to the nature of work that takes place in this area. The highest concentration observed from the pools of samples was in the amalgam room (15μg/m3). The study by Mousavi et al. showed Hg concentration in dental office atmosphere was within OSHA standards whereas [18] in our study Hg vapours were higher in the dental workplace compared to the control, but were lower than TLV of OSHA, ACGIH, and NIOSH. A similar observation of higher Hg concentration in dental offices, but within the standard level was documented by Shirkhanloo et al. [19]. The natural ventilation produced by the airflow from the open windows and the fans in operation in the area has an impact on the Hg concentrations in the air of the dental clinic. As a result, depending on how much outside air is coming in through the open windows, concentrations might change substantially. During our sampling procedures, we were not able to estimate concentrations without natural ventilation (closed windows); nonetheless, it is plausible to assume that without this ventilation, average concentrations would rise significantly.
Urinary heavy metal levels have been used to show prior exposure since urine is the primary method by which many metals are eliminated from the human body [20]. In the present study, we measured urinary Hg levels in 65 occupationally exposed healthcare workers and 32 controls. Non-occupational exposure of Hg in the population is mainly through food i.e., vegetables and seafood including shellfish [21]. Selecting control within the same population eliminates the confounding factor of non-occupational exposure and creates a baseline for comparison. Urine Hg levels in occupationally exposed healthcare workers (0.51±0.17μg/L) were higher than the control (0.29±0.05μg/L) but were within the legally permissible range. Most of the urine Hg values were below 1μg/L. The highest value in one case was 11.2μg/L, a dentist working with Hg in the amalgam room.
The statistical analysis of data from the health survey revealed a significant prevalence of confusion, forgetfulness, muscle spasm, and tremors by the respondents. The prevalence of unexplained arthritis, fatigue, and insomnia was also statistically significant. This may be due to Hg exposure during the handling of elemental Hg while preparing amalgam. There were also complaints related to pulmonary and cardiovascular dysfunctions, i.e., chest pain, rapid pulse, and irritability. In a Norwegian study, the dental assistants significantly reported more neurological symptoms, psychosomatic symptoms, memory loss, concentration difficulties, fatigue, and sleep disturbances than the reference group of assistant nurses. Memory loss seemed to be most important [22].
4.1Study limitations
In our study, we were unable to collect air samples for the entire eight-hour shift and thus should not be compared to the TLV for the purposes of determining potential overexposure. Also, we were not able to estimate concentrations without natural ventilation (closed windows). Another limitation of our study is that we were only able to perform air monitoring and urine examination for Hg from only 1 healthcare establishment compared to the 22-healthcare established which were included in the cross-sectional survey.
5Conclusion
We can conclude from our study that the Hg concentration in dental clinics may be above the prescribed safe levels posing a definitive health risk to dental healthcare workers. To reduce the impact of Hg vapours proper ventilation of the clinics should be maintained. Another crucial finding is that the urine Hg investigation did not reveal an excess of body burden except in one case that was handling elemental Hg. Since Hg has a bio-accumulative nature, it could well be that as these workers get older, they may exhibit higher body burden of Hg that may lead to a variety of adverse health outcomes. Following this study, a crusade was started to get rid of Hg from Delhi’s healthcare facilities and eventually Delhi became the first city in India to announce a “Mercury-free Healthcare.”
Ethics approval
This study was conducted after approval from the Ethical Committee of Maulana Azad Medical College.
Informed consent
Written informed consent was obtained from all participating subjects.
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
No organized funding source was used to conduct the study.
Acknowledgments
None to report.
References
[1] | Zhang Y , Soerensen AL , Schartup AT , Sunderland EM A global model for methylmercury formation and uptake at the base of marine food webs, Global Biogeochem Cycles. (2020) ;34: (2). |
[2] | WHO. Exposure to mercury: a major public health concern. WHO, Public Health Environment International. 2007. |
[3] | USEPA. Eliminating Mercury in Hospitals: Environmental Best Practices for Health care facilities [Internet]. 2002 Nov [cited 2022 Oct 26]. Available from: https://19january2017snapshot.epa.gov/www3/region9/waste/archive/p2/projects/hospital/mercury.pdf. |
[4] | Obrist D , Kirk JL , Zhang L , Sunderland EM , Jiskra M , Selin NE A review of global environmental mercury processes in response to human and natural perturbations: Changes of emissions, climate, and land use, Ambio. (2018) ;47: (2):116–40. |
[5] | Janev Holcer N , Maričević M , Miočić-Juran A The use of mercury-based medical devices across Croatian healthcare facilities. Arh Hig Rada Toksikol [Internet]. 2012 Mar 1 [cited 2022 Oct 26];63: (1):41–7.Available from: https://pubmed.ncbi.nlm.nih.gov/22450205/. |
[6] | Álvarez-Solorza I , Upegui-Arango LD , Borja-Aburto V , González-González N , Fischer F , Bustamante-Montes LP Perception and knowledge of mercury by occupationally exposed healthcare personnel, J Contin Educ Health Prof. (2022) ;42: (1):e19–26. |
[7] | Tuček M , Bušová M , Čejchanová M , Schlenker A , Kapitán M Exposure to mercury from dental amalgam: actualcontribution for risk assessment, Cent Eur J Public Health. (2020) ;28: (1):40–3. |
[8] | Nimmagadda A , Stanley I , Karliner J , Orris P Global substitution of mercury-based medical devices in the health sector, Water and Sanitation-Related Diseases and the Changing Environment: Challenges, Interventions, and Preventive Measures. (2019) 189–96. |
[9] | Senanayake SJ , Gunawardena NS Knowledge, attitudes and practicesregarding handling mercury containing medical devices among nursesin a tertiary care paediatric hospital in Sri Lanka, Work. (2016) ;55: (2):311–9. |
[10] | Chaari N , Kerkeni A , Saadeddine S , Neffati F , Khalfallah T , Akrout M [Mercury impregnation in dentists and dental assistants in Monastir city, Tunisia]. Rev Stomatol Chir Maxillofac [Internet]. 2009 Jun [cited 2022 Oct 26];110: (3):139–44.Available from: https://pubmed.ncbi.nlm.nih.gov/19419743/. |
[11] | Naimi-Akbar A , Sandborgh-Englund G , Ekbom A , Ekstrand J , Montgomery S Cognitive function among sons of women who worked in dentistry. Scand J Work Environ Health [Internet]. 2012 [cited 2022 Oct 26];38: (6):546–52. Available from: https://pubmed.ncbi.nlm.nih.gov/22517488/. |
[12] | Peshin SS , Halder N , Jathikarta C , Gupta YK Use of mercury-based medical equipment and mercury content in effluents of tertiary care hospitals in India. Environ Monit Assess [Internet]. 2015 Mar 1 [cited 2022 Oct 26];187: (3). Available from: https://pubmed.ncbi.nlm.nih.gov/25716525/. |
[13] | Bahcecik N , Ozturk H The occupational safety and health in hospitals from the point of nurses, Coll Antropol. (2009) ;33: (4):1205–14. |
[14] | Palacios N , Fitzgerald K , Roberts AL , Hart JE , Weisskopf MG , Schwarzschild MA ,et al A prospective analysis of airborne metal exposures and risk of Parkinson disease in the nurses’ health study cohort. Environ Health Perspect [Internet]. 2014 [cited 2022 Oct 26];122: (9):933–8.Available from: https://pubmed.ncbi.nlm.nih.gov/24905870/. |
[15] | NIOSH. Method 6009: Mercury. NIOSH Manual of Analytics [Internet]. 1994 Aug [cited 2022 Oct 26].Available from: https://www.cdc.gov/niosh/docs/2003-154/pdfs/6009.pdf. |
[16] | American Conference of Governmental Industrial Hygienists TLVs and BEIs. Threshold Limit Values for Chemical Substances and Physical Agents and Biological Exposure Indices. In Cincinnati, OH; 2008. p. 37. |
[17] | Moienafshari R , Bar-Oz B , Koren G Occupational exposure to mercuryWhat is a safe level? Can Fam Physician. (1999) ;45: :43–5. |
[18] | Zavvar Mousavi H , Rouhollahi A , Shirkhanloo H Determination of mercury concentration in the air of dental clinics and the urines of their personnel with cold vapor atomic absorption spectrometry. Iranian Journal of Toxicology [Internet]. 2009 Dec 10 [cited 2023 Jan 16];2: (4):287–91. Available from: https://ijt.arakmu.ac.ir/article-1-66-en.html. |
[19] | Shirkhanloo H , Fallah Mehrjerdi MA , Hassani H Identifying occupational and nonoccupational exposure to mercury in dental personnel, Arch Environ Occup Health. (2017) ;72: (2):63–9. |
[20] | Zhang T , Ruan J , Zhang B , Lu S , Gao C , Huang L ,et al. Heavy metals in human urine, foods and drinking water from an e-waste dismantling area: Identification of exposure sources and metal-induced health risk, Ecotoxicol Environ Saf. (2019) ;169: :707–13. |
[21] | Mawari G , Kumar N , Sarkar S , Daga MK , Singh MM , Joshi TK ,et al. Heavy metal accumulation in fruits and vegetables and human health risk assessment: Findings From Maharashtra, India, Environ Health Insights. (2022) ;16: :117863022211191. |
[22] | Moen B , Hollund B , Riise T Neurological symptoms among dental assistants: a cross-sectional study, J Occup Med Toxicol. (2008) ;3: :10. |




