Prevalence and risk factors of thumb pain in Italian manual therapists: An observational cross-sectional study
Abstract
BACKGROUND:
Work-related musculoskeletal disorders (WMSDs) affect physical therapists with loss of health status and social costs. MSD is a relevant problem in upper limb extremities, especially when associated with manual techniques.
OBJECTIVE:
The study aims to investigate the prevalence and risk factors associated with thumb pain in Italian physiotherapists who perform manual therapy.
METHODS:
A self-administered questionnaire was sent by email, exploring demographics, thumb mobility, job, thumb pain, manual techniques, aggravating factors, management strategies and consequences of thumb pain.
RESULTS:
The survey was sent to 523 manual therapists, 219 of which fully completed it. 49.3% of respondents experienced thumb pain at least once in the previous 12 months and 70.8% at least once in their lifetime. Statistically significant associations suggest that within 12 months manual therapists with more than 5 years of experience are less likely to report thumb pain (6–10 years of work: OR = 0.408, 95% CI: 0.215–0.775; 11–20 years of work: OR = 0.346, 95% CI: 0.139–0.859), whereas those who performs trigger point pressure release (OR = 1.832, 95% CI: 1.005–3.340), trigger point ischemic compression (OR = 2.999, 95% CI: 1.184–7.597) and fascial neuro-connective manipulation (OR = 3.086, 95% CI: 1.346–7.077) are more likely to experience it. In terms of lifetime prevalence, female manual therapists and those who perform trigger point ischemic compression are more likely to suffer from thumb pain (females: OR = 2.569, 95% CI: 1.339–4.930; trigger point ischemic compression: OR = 2.878, 95% CI: 1.319–6.281).
CONCLUSIONS:
Special attention should be paid to prevention during manual skills training, since inexperience exposes manual therapist to a higher risk of developing thumb pain.
1Introduction
The World Health Organisation (WHO) considers work-related musculoskeletal disorders (WMSDs)as all musculoskeletal disorders that are induced or aggravated by work and the circumstances ofits performance [1]. This definition considers both chronic and acute problems, with or without a cause-effect relationship. Regardless of the challenge in coming to a comprehensive definition, WMSD have a high impact on society, in terms of loss of health status and social costs, as the International Labour Organization (ILO) statistics and databasesshow [2].
The economic impact on businesses and social costs borne by European countries because of WMSDs are a cause of concern due to their extent. Even though the European Agency for Safety and Health at Work (EU-OSHA) finds it difficult to assess and compare WMSD costs, some studies have estimated the cost of work-related upper-limb musculoskeletal disorders (WRULDs) between 0.5% and 2% of Gross National Product (GNP) [1]. Despite the enormous cost for society, WRULD prevention is a recent branch of research, mostly focused on office workers [3, 4]. As a result, WRULD prevention among healthcare workers is not widely investigated [3, 4].
Most physical therapists’ WMSDs are located in upper limb extremities [5–18]. Percentages seem to be higher when related to an extensive use of manual techniques [5, 7, 8, 11, 14, 16, 18]. This finding prompted a study on physical therapists to thoroughly examine work-related wrist/hand area complaints. In terms of on thumb pain, the reported one-year prevalence ranges from 11.1% to 83% [7, 10, 12, 14, 19, 20].
There were no prior studies investigating prevalence and risk factors associated with thumb pain in Italian physiotherapists who perform manual therapy. Moreover, Master’s degree recognized by International Federation of Orthopaedic Manipulative Physical Therapists (IFOMPT) in Italy is a relatively new branch of specialisation (beginning in 2003) [21, 22].
The aim of this study was to analyse associations between demographic information [5, 7, 20, 23], work setting and habits [6, 7, 13, 14, 17, 18, 23], performance of manual techniques [5, 7, 8, 11, 14, 16, 18, 20, 23] and strategies to cope with pain and disability [7, 8, 10, 19, 20] due to thumb pain, in order to support or reject previous conflicting findings.
2Methods
2.1Procedure
This observational study was designed as a web-based cross-sectional survey, as per the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) guidelines [24].
Factors investigated in former studies were taken into consideration to draw up the questionnaire, but every item was originally conceived in Italian, considering the participants’ origin [5, 10, 14, 19, 23, 24]. At the beginning, face and content validity of the questionnaire were made: 10 manual physical therapists (reference sample), who met the inclusion criteria described in the following paragraph, were requested to answer the survey to test comprehension and interpretation of questions. After positive feedback, to determine the reliability of the survey responses, the same 10 manual physical therapists completed the questionnaire again two weeks later. Test-retest percentage of agreement was calculated and found to average 97% (90% – 100% range). The area of the questionnaire most susceptible to discrepancy was the demographics section (notably height and weight reports). These 10 respondents were then excluded from the next steps of the study.
A brief introduction and the link to the online form of the self-administered questionnaire were sent by email to each participant early in February 2013, along with a link for informed consent. Google Forms was used to create the survey. After 2 months, in order to avoid double responses, as per CHERRIES guidelines, a reminder with the same structure as the first email was electronically sent to all participants, encouraging those who already completed the survey not to answer again. Data were automatically and anonymously collected by the program until the beginning of June 2013 (timeframe of 4 months altogether) in an electronic database (Excel spreadsheet), and only the project manager could access the information. Anonymity was granted by associating a numeric code to each reply received.
2.2Participants
Because one of the aims of the study was to identify which manual techniques represent a risk factor in the development of thumb pain, participants were recruited among Italian physiotherapists with a Master’s Degree recognized by IFOMPT (International Federation of Orthopaedic Manipulative Physical Therapists) [21, 22]. This choice ensured a relatively homogeneous educational background of the participants and widespread knowledge and application of various manual techniques from such educational background. The total number of participants was 523.
2.3Instrumentation
The survey was 2-webpage long taking up about 10–15 minutes to be completed. The questionnaire was composed of 24 closed-ended questions. They were organised into 8 main areas: Demographics (5 questions about sex, age, handedness, weight and height), thumb mobility (2 questions about presence of hypermobility of thumb and joints involved in hypermobility), job (5 questions about years of work experience, current work setting, current work area, working hours per day, working days per week), thumb pain (6 questions about lifetime prevalence, lifetime side of pain, lifetime pain intensity, one-year prevalence, one-year side of pain, one-year pain intensity), manual techniques (2 questions about the kind of manual techniques regularly performed and manual techniques causing pain), aggravating factors and management strategies used to deal with pain (3 questions about aggravating circumstances, management strategies used to deal with pain and of electro-physical therapy effectiveness) and 1 question about consequences of thumb pain. In particular, in the last question respondents were asked to state if their thumb pain caused impairment of Activity of Daily Living and of Instrumental Activity of Daily Living (ADL/IADL) [27, 26], sports, work or prompted them to change job.
The participants indicated painful manual techniques only if they stated that they perform at least one manual technique listed, and they had to indicate which electro-physical agents significantly improved symptoms if they stated that they sought for electro-physical therapies as strategy to deal with pain (adaptive questions).
No previous literature findings investigated frequency of use or effectiveness of electro-physical agents for thumb pain relief: This was the only item not based on questions retrieved in former studies.
The complete form of the survey, translated into English, is provided in Appendix 1.
2.4Data analysis and statistics
The baseline demographic and clinical characteristics were summarized as count and percentage (%), mean with standard deviation (SD), range [R], or median with interquartile range (25–75 percentiles).
Chi square test or Fisher’s exact test was carried out to compare categorical variables, in particular to evaluate any association between presence/absence of pain and categorical demographic or clinicalcharacteristics.
Statistically significant variables at univariate analysis were fitted in a forward stepwise (conditional) logistic regression model to determine if the presence of pain was associated with other characteristics, with adjustment for potential confounding factors such as age and sex.
A multivariate analysis was applied to determine which characteristics were associated with the presence of pain.
For variables statistically associated with pain, differences in NRS score (median values) were explored by using the non-parametric Mann-Whitney or Kruskal-Wallis tests.
Data were expressed as Odds Ratio (OR) and 95% Confidence Interval (CI).
Statistical analysis was computed using Statistical Package for Social Science (SPSS version 20, IBM, USA).
All statistical tests were two-sided and the significance level (alpha error) was set at 0.05.
3Results
3.1Sample demographics and thumb mobility
The questionnaire was sent to 523 manual therapists, 224 of which responded, with a response rate of 42.8%. Due to incomplete data, 5 questionnaires were excluded (n = 219).
Most respondents were male (58.9%), mostly between 21 and 30 years old (60.3%). The sex of respondents closely reflected the composition of the whole sample of physiotherapists with the Master’s degree in manual therapy in Italy in the past 9 years (generally speaking 59.3% males and 40.7% females). The dominant limb was the right one in 93.6% of cases. The normal range of body mass index (BMI from 18.5 to 24.9) was the most represented (76.3% of the sample).
In terms of thumb mobility, self-assessed hypermobility, without distinction as to one or both hands, was declared mostly in metacarpophalangeal joint (42.7%) by 34.2% of respondents.
A complete overview of demographic and thumb mobility data is available in Fig. 1.
3.2Job characteristics and manual techniques
42.0% of respondents started to work recently, between 0 and 5 years ago, and 38.4% between 6 and 10 years ago. In almost all cases (95.9%) one of the current working areas was orthopaedics. Manual therapists who worked at private outpatient clinics were 65.8%, followed by 34.7% working in private inpatient clinics. Respondents worked an average of 40.31 (SD = 11.36) hours a week (range: 8–81). Figure 1 summarizes all job characteristics.
More commonly practiced manual techniques were: Traction (86.8%), trigger point ischemic compression (84.9%), central posterior-anterior mobilization (84.0%), unilateral posterior-anterior mobilization (78.5%) and massage (65.8%). The use of trigger point ischemic compression technique caused pain in 59.7% of cases, followed by trigger point pressure release (46.9%) and massage (36.8%). See Fig. 2 for more information.
3.3Thumb pain
49.3% (n = 108) of respondents experiencedthumb pain at least once in the last 12 months (one-year prevalence), 55.6% (60/108) of which in theright hand, 36.1% (39/108) in both and 8.3% (9/108) in the left one. Lifetime prevalence, i.e. pain experienced at least once in the entire life, of thumb pain, was 70.8% (n = 155), 55.5% (86/155) of which on the right hand, 38.1% (59/155) on both and 6.4% (10/155) on the left one. Numeric Rating Scale (NRS) was chosen to assess pain intensity in the survey. The average rating of thumb pain referred to one-year prevalence was 4.27 (SD 1.99). The mean NRS value experienced during the entire career was 4.13 (SD 1.9).
Respondents who experienced thumb pain reported consequences in the private sphere and working environment. Looking at one-year pain prevalence, impairment of Activity of Daily Living and of Instrumental Activity of Daily Living (ADL/IADL) were stated in 9.3% (10/108) of cases followed by 5.6% (6/108) temporary suspension of work, 4.6% (5/108) career change and 2.8% (3/108) impairment/temporary suspension of sport. As far as pain is concerned, impairment of ADL / IADL was stated in 9% (14/155) of cases, followed by 5.2% (8/155) temporary suspension of work, 4.5% (7/155) career change and 2.6% (4/155) impairment/temporary suspension of sport. IT should be noted that more than one answer was allowed in this section of the questionnaire.
Aggravating factors for therapists that experienced pain in the last year were continuing to work with a sore thumb (66.7%), followed by working in the same position for long periods (64.8%). Their management strategies were: Altering practice techniques (69.4%) and changing position frequently (57.4%). Electro-physical agents were used as treatment to manage pain in 20.4% (22/108) of cases, and a substantial improvement was perceived mainly when using laser therapy (14 out of 22).
Aggravating factors and the implementationof pain management strategies to deal with painwere also explored among those who experienced thumb pain at least once in the entire career. The most remarkable aggravating factor was working in the same position for long periods (65.2%) followed by continuing to work with a sore thumb (61.9%). The most common pain management strategiesused to deal with lifetime pain were altering practicetechniques (71.0%) and changing position frequently (54.2%). Electro physical agents were used as treatment to manage pain only in 18.7% (29/155) of cases and a subjective substantial improvement was perceived mainly when using laser therapy (19 out of 29). Table 1 shows a summary of aggravating factors and managementstrategies.
3.4Pain association with demographics, thumb mobility and job characteristics
Considering one-year prevalence of thumb pain, a statistically significant association was found with the experience of physical therapists, quantified in number of years of work (p = 0.035), and further analysis of the association between years of work and differences in NRS yielded a positive result (p = 0.013). Those who had been working for 11 to 20 years reported higher intensity of pain (median: NRS 5.50; range: 3.00–6.25), followed by those who had been working for 6 to 10 years (median: NRS 5.00; range: 4.00–6.00), then others (for 0 to 5 years, median: NRS 4.00; range: 2.00–5.00; for more than 20 years, median: NRS 4.00; range: 2.00–7.00).
No significant association between demographics, thumb mobility and job characteristics to lifetime prevalence of thumb pain was found at multivariate analysis.
Further information on significant association with differences in NRS is provided in Table 2. Associations not reported in Table 2 were not significant.
3.5Pain association with manual techniques
One-year prevalence of thumb pain was associated with performing trigger point ischemic compression (p = 0.006). NRS were significantly higher (p = 0.05) in those who did not perform trigger point ischemic compression (median: NRS 6.00; range: 3.50–7.50) than in those who practised it (median: NRS 4.00; range: 3.00–5.25).
In terms of lifetime prevalence of thumb pain, no statistically significant association was found at multivariate analysis.
The complete set of data about significant associations with differences in NRS is available in Table 2.
3.6Pain association with aggravating factors and management strategies
No aggravating circumstance were found to be associated with differences in NRS, either in one-year pain prevalence or in lifetime pain prevalence.
In the last 12 months physical therapists were more likely to decide for electro-physical therapies as a management strategy when NRS was significantly higher (p = 0.007).
Considering the entire career, respondents were more likely to opt for a reduction in the number of working hours or hours on patients (p = 0.001), for functional taping (p = 0.039) and for electro-physical therapies (p = 0.003), when NRS was found to be significantly higher.
Table 2 shows significant associations between differences in NRS and aggravating factors and management strategies.
3.7Consequences of thumb pain
Analysing the last 12 months, a statistically significant difference in NRS was detected regarding the impairment of ADL / IADL (p = 0.015). In particular, median NRS was 6.00 (range: 4.50–8.00) for those who reported an impairment of ADL / IADL; for the others NRS was 4.00 (range: 3.00–5.50).
In terms of lifetime prevalence, a statistically significant difference in NRS was detected regarding the impairment of ADL / IADL (p < 0.001), and also regarding a leave of absence from work (p = 0.001). NRS was 6.50 (range: 5.00–7.25) for those who reported an impairment of ADL / IADL; for the others NRS was 4.00 (range: 2.50–5.00). Median NRS was 7.00 (range: (5.00–7.75) in those who opted to temporarily stop working and 4.00 (range: 3.00–5.00) in those who did not stop because of pain.
An overview of significant data is available in Table 2.
3.8Protective and risk factors
Multivariate analysis performed on thumb pain experienced in the last year (as a dependent variable) showed some significant associations. In particular, physical therapists that had been working for 6 to 20 years were 60% less likely to develop thumb pain than colleagues who had been working for less than 5 years (6–10 years of work: OR = 0.408, 95% CI: 0.215–0.775, p = 0.006; 11–20 years of work: OR = 0.346, 95% CI: 0.139–0.859, p = 0.022). No difference in probability to have thumb pain resulted between professionals who had been working for less than 5 years and physiotherapists who had been working for more than 20 years. The risk of having pain was up to three times higher in physiotherapists who practice trigger point pressure release (OR 1.832, 95% CI: 1.005–3.340, p = 0.048), trigger point ischemic compression (OR 2.999, 95% CI: 1.184–7.597, p = 0.021) and fascial neuro-connective manipulation (OR 3.086, 95% CI: 1.346–7.077, p = 0.008).
The results from multivariate logistic model showed that, considering entire career as a dependent variable, significant risk factors that lead to thumb pain are sex and trigger point ischemic compression. Females had 2.6 greater risk than males of developing thumb pain (OR 2.569, 95% CI: 1.339–4.930, p = 0.005). Furthermore, physiotherapists who perform trigger point ischemic compression are almost three times more likely to have pain rather than subjects that do not use this technique (OR 2.878, 95% CI: 1.319–6.281, p = 0.008).
Further information is provided in Table 3.
4Discussion
4.1Thumb pain prevalence
The sample size of the present study was in line with previous ones in this area [7–9, 12–15, 19, 20]. The present study showed that thumb pain is a disorder that highly affects Italian physiotherapists who perform manual therapy with a lifetime prevalence of 70.8%, comparable with 65% prevalence underlined by McMahon et al., 2006 [23] in a sample of Australian physiotherapists, and with one-year prevalence of 49.3%, slightly greater than previous findings [7, 14, 20].
The average intensity of pain referred to one-year prevalence, measured by Numerical Rating Scale (NRS), was of moderate severity (4.27; SD 1.99), very close to the score of 3.75 (SD 1.9) obtained in a survey [19] that used another 11-point scale (Visual Analogue Scale) to measure thumb pain.
4.2Demographics, thumb mobility and pain
Younger physical therapists seems to suffer of thumb pain more often over a period of 12 months (68.5%), probably as consequence of less experience in dosing force or positioning hands and fingers while they perform manual techniques. This result confirms previous findings [7] and should be interpreted as a suggestion to be more careful during the teaching and learning process of manual techniques, to prevent musculoskeletal disorders possibly related to them.
Thumb pain experienced at least once in the entire career is strongly associated with sex (p = 0.005). Indeed, multivariate analysis showed that females were 2.6 times more at risk of developing thumb pain in their career than males. The results from this study seems to be in contrast with other studies according to which males are 1.5 to 2.2 times more likely to develop thumb pain [7, 23]. Previous findings were explained stating that males are more at risk because they perform manual techniques more often than females [7]. Our study does not seem to corroborate this. A possible explanation of the different results could come from the different composition of the sample. In this study all participants, both males and females, are specialised in manual therapy, therefore it can be assumed that both sexes use the same amount of the same manual techniques. Number and type of techniques being equal, the incidence of pain work-related musculoskeletal disorders [5, 12, 13, 15] in females seems to be higher due a less resistant physical structure.
Moreover some authors suggested that females are more at risk of developing thumb pain because of a more prevailing general hypermobility [28], but no strong association between hypermobility and musculoskeletal pain has yet been demonstrated [29].
Contrary to previous ones, the present study [20, 23, 28], has not shown any statistically significant association of thumb pain with BMI, handedness or joint hypermobility. Even if in one former study the self-assessment of joint hypermobility was considered acceptable [23], reliability of this measurement across many therapists may be poor, because the question might be interpreted differently by each professional. So caution is needed in drawing conclusions about this specific item of thequestionnaire.
4.3Job factors and pain
Years of work experience were significantly associated with thumb pain. In particular, those who had been working for fewer years reported thumb pain more frequently in the last 12 months (p = 0.035). Multivariate analysis showed that physical therapists who had been working from 6 to 20 years were 60% less likely to develop thumb pain than professionals who had been working for less than 5 years or more than 20. This could be explained assuming that more experienced physiotherapists have probably refined their practice technique and adopted ergonomic body position more regularly, reducing exposition to overloading in thumb joints. Indeed recent researches have outlined that younger physiotherapists are not trained enough about ergonomics [30] and that an interdisciplinary approach in teaching this subject may improve results [31].
Between 6 and 20 years of work, pain intensity seems to be positively correlated to the number of years of work and those who had been working from 11 to 20 years experienced more pain (median: NRS 5.50; range: 3.00–6.25), followed by those who had been working from 6 to 10 years (median: NRS 5.00; range: 4.00–6.00). The increase in median pain intensity can be related to the aging process of the articular complex (bones, cartilages and soft tissues), that contribute to inflammation [32, 33], possibly caused by minor injuries, like accidental sprains or strains due to inability to stabilise the joints of the thumb when performing manual techniques [23]. Reduction in pain intensity after 20 years of work may be due to better technical skills, fewer hours spent on patients and/or decreased use of manual techniques to prevent pain onset. No previous studies about physiotherapists found any significant association between job experience and thumbpain.
Instead, previous studies found an association between work setting, work area and thumb pain. In particular, private practice and outpatient clinics are related to higher prevalence of thumb pain [7, 10, 14, 23], and risk of developing it is reported to be 2.8 times in those who work in private practice [7] and 3.2 times in professionals working in outpatient orthopaedic clinics [23].
4.4Manual techniques and pain
Some manual techniques were found to be related to thumb pain in previous studies [7, 20, 23]. They specifically involve the thumb, requiring high level of finger pressure (until 235 N [35]) and producing maintained hyperextension of joints [19, 23]. A higher risk of developing thumb problems is consistent with performing trigger point therapy (OR 2.3) [23], massage (OR 2.1) [23] manipulations and mobilisations (OR from 3.42 to 7.7) [7, 16]. As regards one-year prevalence of thumb pain, this study highlighted an association with trigger point ischemic compression (p = 0.006) that was significantly associated with differences in NRS (p = 0.05): Pain intensity was found to be higher (median: NRS 6.00, range: 3.50–7.50) in physiotherapists who do not perform it than in those who do (median: NRS 4.00, range: 3.00–5.25). This seemingly contradictory result may be explained by the fact that this technique causes such strain that physical therapists already suffering from thumb pain probably tend to avoid it. It should be noted that the association was considered significant, even with a p value of 0.05, because of the great difference in median NRS.
The massage, that in previous studies was considered to be strongly associated with thumb pain [25, 34], showed no significant association in this investigation.
4.5Disability and participation restriction
This study found out that thumb pain is significantly associated, both at 12 months and in the entire career, with impairment in ADL/IADL. As expected, those who feel more pain tend to experience more difficulties in daily activities than others.
If we consider the entire life, contrary to previous findings [19], while more intense pain was associated with temporary work suspension, career change was not.
4.6Aggravating and reducing pain
No aggravating factors, such as working in the same position for long periods, continuing to work with a sore thumb, unavailable adjustable massage tables/beds and psychological distress/high workload were found to be significantly associated with thumb pain both at 12 months and in the entire career. Different results were found in past studies, indicating that high psychological demands significantly increased (OR 3.37) the risk of developing thumbpain [16].
Physical therapists reporting pain in the last 12 months are generally keen on using electro-physical therapies to treat their disorder (p = 0.007), but statistical analysis showed no preference in the type of therapy used.
If we consider the lifespan, among treatment by electro-physical therapies (p = 0.003), physiotherapists with more pain tend to use functional taping (p = 0.039) and to reduce working hours or hours spent on patients (p = 0.001). This last management strategy is a potential source of job loss, especially considering that most respondents work in private practice/outpatient clinics: Not fulfilling patients’ requests in reasonable time could lead them to seek for another professional, with consequent economic loss.
Previous studies reported significant associations with reducing working hours or hours spent on patients, but not with taping [19]. As no former studies investigated the choice of electro-physical agents as treatment method for physical therapists, no comparison can be made.
4.7Limits of the study
This study presents some limitations that need to be stated.
Even if respondents were more than a third of the number of physiotherapists who, at the moment of the survey, had a specialization in manual therapy from an Italian university, the analysed sample was limited with regard to size and age.
The sample is a convenience one, considering only manual therapists that earned a master’s degree in manual therapy from 2003 to 2011 and which was compliant with IFOMPT educational standards at university. Excluding physiotherapists educated in non-standardised private courses of manual therapy, the resulting sample was homogeneous and very specific, allowing results with a relevant statistical weight. This made it possible to draw clear conclusions on the population of physiotherapists specialized in manual therapy at university. At the same time, the sample represents a limitation requiring caution when trying to infer the results to the whole population of Italian physiotherapists practising manual therapy.
Moreover, as this is a cross-sectional study, it was possible only to describe associations between thumb pain and the issues investigated, without establishing cause-effect relationships.
Finally, it should be considered that questionnaires like this one are intrinsically affected by recall biases. The data obtained through a self-administered survey and self-assessment procedures are potentially less accurate than objective measurements and may generate over/under-estimated responses by physiotherapists [36]. However WMSDs are conditions commonly evaluated by subjective reports, often in absence of objective data or clinical tests [37].
5Conclusion
Thumb pain is predominant in Italian physiotherapists, affecting more female physiotherapists who use manual techniques specifically involving the thumb and requiring high level of finger pressure and maintained positions. The disorder seems to be more present during the first years and after twenty years of work.
5.1Implications for practice
It may be appropriate to raise awareness among physical therapists and trainees on work-related thumb pain, introducing ergonomic pre- and post-graduation trainings, focused on correct practice of manual techniques.
5.2Implication for research
Further prospective studies are needed to investigate risk factors (cause-effect relationships), with the purpose of developing more effective prevention programmes and educing health costs due to work-related upper-limb musculoskeletal disorders.
Conflict of interest
The authors do not believe there are any conflicts of interest.
Acknowledgments and ethical issues
Authors are grateful to Cristina Parente for her support in revising the English form of the paper. Informed consent for publication in print and electronic form was obtained from participants and all procedures were conducted pursuant to the Declaration of Helsinki. There was no external source of funding for this paper.
References
[1] | Hagberg M , Violante FS , Bonfiglioli R , Descatha A , Gold J , Evanoff B , et al . Prevention of musculoskeletal disorders in workers: Classification and health surveillance – statements of the Scientific Committee on Musculoskeletal Disorders of the International Commission on Occupational Health. BMC Musculoskeletal Disorders (2012) ;13: :109. |
[2] | International Labour Organisation. Frequency rate of non-fatal occupational injury by sex and occupation (%) [Homepage on the Internet]. International Labour Organisation (ILO); 1996-2011 [updated 2011; cited 2015 Jun 25]. Available from: http://www.ilo.org/ilostat/faces/help_home/data_by_subject/subject-details/indicator-details-by-subject?indicator=INJ_NFTL_SEX_OCU_RT&subject=INJ&_afrLoop=25513560410249&datasetCode=YI&collectionCode=YI&_adf.ctrl-state=142xj2qmno_482. |
[3] | Canadian Centre for Occupational Health and Safety.Work-related Musculoskeletal Disorders (WMSDs) [Homepage on the Internet]. Canadian Centre for Occupational Health and Safety; 2004 [updated 2014 Jan 08; cited 2014 Mar 22]. Available from: http://www.ccohs.ca/oshanswers/diseases/rmirsi.html. |
[4] | Schneider E , Irastorza X , Copsey S . OSH in figures: Work-related musculoskeletal disorders in the EU – facts and figures. Luxembourg Publications Office of the European Union; (2010) . |
[5] | Bork BE , Cook TM , Rosecrance JC , Engelhardt KA , Thomason ME , Wauford IJ , Worley RK . Work-related musculoskeletal disorders among physical therapists. Phys Ther (1996) ;76: (8):827–35. |
[6] | Holder NL , Clark HA , DiBlasio JM , Hughes CL , Scherpf JV , Harding L , et al . Cause, prevalence, and response to occupational musculoskeletal injuries reported by physical therapists and physical therapist assistants. Phys Ther (1999) ;79: (7):642–52. |
[7] | Cromie JE , Robertson VJ , Best MO . Work-related musculoskeletal disorders in physical therapists: Prevalence, severity, risks, and responses. Phys Ther (2000) ;80: (4):336–51. |
[8] | West DJ , Gardner D . Occupational injuries of physiotherapists in North and Central Queensland. Aust J Physiother (2001) ;47: (3):179–86. |
[9] | Rugelj D . Low back pain and other work-related musculoskeletal problems among physiotherapists. Appl Ergon (2003) ;34: (6):635–9. |
[10] | Glover W , McGregor A , Sullivan C , Hague J . Work-related musculoskeletal disorders affecting members of the Chartered Society of Physiotherapy. Physiotherapy (2005) ;91: (3):138–47. |
[11] | Campo M , Weiser S , Koenig KL , Nordin M . Work-related musculoskeletal disorders: A prospective cohort study with 1-year follow-up. Phys Ther (2008) ;88: (5):608–19. |
[12] | Adegoke BO , Akodu AK , Oyeyemi AL . Work-related musculoskeletal disorders among Nigerian physiotherapists. BMC Musculoskeletal Disorders (2008) ;9: :112. |
[13] | Alrowayeh HN , Alshatti TA , Alijadi SH , Fares M , Alshamire MM , Alwazan SS . Prevalence, characteristics, and impacts of work-related musculoskeletal disorders: A survey among physical therapists in the State of Kuwait. BMC Musculoskeletal Disorders (2010) ;11: :116. |
[14] | Rozenfeld V , Ribak J , Danziger J , Tsamir J , Carmeli E . Prevalence, risk factors and preventive strategies in work-related musculoskeletal disorders among Israeli physical therapists. Physiother Res Int (2010) ;15: (3):176–84. |
[15] | Nordin NA , Leonard JH , Thye NC . Work-related injuries among physiotherapists in public hospitals: A Southeast Asian picture. Clinics (Sao Paulo) (2011) ;66: (3):373–8. |
[16] | Grooten WJ , Wernstedt P , Campo M . Work-related musculoskeletal disorders in female Swedish physical therapists with more than 15 years of job experience: Prevalence and associations with work exposures. Physiother Theory Pract (2011) ;27: (3):213–22. |
[17] | Caragianis S . The prevalence of occupational injuries among hand therapists in Australia and New Zealand. J Hand Ther (2002) ;15: (3):243–41. |
[18] | Darragh AR , Campo M , King P . Work-related activities associated with injury in occupational and physical therapists. Work (2012) ;42: (3):373–84. |
[19] | Wajon A , Ada L . Prevalence of thumb pain in physical therapists practicing spinal manipulative therapy. J Hand Ther (2003) ;16: (3):237–44. |
[20] | Van de Velde K , Cattrysse E . Work-related thumb pain in physiotherapists: Prevalence, risk factors and prevention, an observational study. It J Physiotherapy (2013) ;3: (4):145–53. |
[21] | International Federation of Orthopaedic Manipulative Physical Therapists (IFOMPT). MOs and RIGs – Learning Institution: Italy [Internet]. IFOMPT; 2008 [cited 2014 Dec 30]. Available from: http://www.ifompt.com/MOs+and+RIGs/Learning+Institutions/Italy.html. |
[22] | Bologna Secretariat. Bologna process – European Higher Education Area: Towards shared descriptors for Bachelors and Masters [Internet]. Romanian Bologna Secretariat; 2010 [cited 2014 Apr 1]. Available from: http://www.ehea.info/article-details.aspx?ArticleId=110. |
[23] | McMahon M , Stiller K , Trott P . The prevalence of thumb problems in Australian physiotherapists is high: An observational study. Aust J Physiother (2006) ;52: (4):287–92. |
[24] | Eysenbach G . Improving the quality of Web surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J Med Internet Rese (2004) ;6: (3):34. |
[25] | Jang Y , Chi CF , Tsauo JY , Wang JD . Prevalence and risk factors of work-related musculoskeletal disorders in massage practitioners. J Occup Rehabil (2006) ;16: (3):425–38. |
[26] | Bookman A , Harrington M , Pass L , Reisner E . Family Caregiver Handbook: Finding elder care resourcesin Massachusetts. Cambridge, MA: Massachusetts Institute of Technology; (2007) . |
[27] | Roley SS , DeLany JV , Barrows CJ , Brownrigg S , Honaker D , Sava DI , et al. Occupational therapy practice framework: Domain & practice, 2nd edition. Am J Occup Ther (2008) ;62: (6):625–83. |
[28] | Snodgrass SJ , Rivett DA , Chiarelli P , Bates AM , Rowe LJ . Factors related to thumb pain in physiotherapists. Aust J Physiother (2003) ;49: (4):243–50. |
[29] | Mulvey MR , Macfarlane GJ , Beasley M , Symmons DP , Lovell K , Keeley P , et al. Modest association of joint hypermobility with disabling and limiting musculoskeletal pain: Results from a large-scale general population-based survey. Arthritis Care Res (Hoboken) (2013) ;65: (8):1325–33 . |
[30] | Adam K , Strong J , Chipchase L . Readiness for work injury management and prevention: Important attributes for early graduate occupational therapists and physiotherapists. Work (2014) ;48: (4):567–78. |
[31] | Barbosa LH , Pinheiro MH . Teaching ergonomics to undergraduate physical therapy students: New methodologies and impressions of a Brazilian experience. Work (2012) ;41: (Suppl 1):4790–4. |
[32] | Houard X , Goldring MB , Berenbaum F . Homeostatic mechanisms in articular cartilage and role of inflammation in osteoarthritis. Curr Rheumatol Rep (2013) ;15: (11):375–. |
[33] | Zhu Y , Armstrong JL , Tchkonia T , Kirkland JL . Cellular senescence and the senescent secretory phenotype in age-related chronic diseases. Curr Opin Clin Nutr Metab Care (2014) ;17: (4):324–8. |
[34] | Albert WJ , Currie-Jackson N , Duncan CA . A survey of musculoskeletal injuries amongst Canadian massage therapists. J Bodyw Mov Ther (2008) ;12: (1):86–93. |
[35] | Snodgrass SJ , Rivett DA , Robertson VJ . Manual forces applied during posterior-to-anteriori spinal mobilisation: A review of the evidence. J Manipulative Physiol Ther (2006) ;29: (4):316–29. |
[36] | Viikari-Juntura E , Rauas S , Martikainen R , Kuosma E , Riihimäki H , Takala EP , et al . Validity of self-reported physical work load in epidemiologic studies on musculoskeletal disorders. Scand J Work Environ Health (1996) ;22: (4):251–9. |
[37] | Guo HR , Tanaka S , Cameron LL , Seligman PJ , Behrens VJ , Ger J , et al . Back pain among workers in the United States: National estimates and workers at high risk. Am J Ind Med (1995) ;28: (5):591–602. |
Figures and Tables
Fig.1
Summary of demographics, thumb mobility and job characteristics of the sample (n = 219).
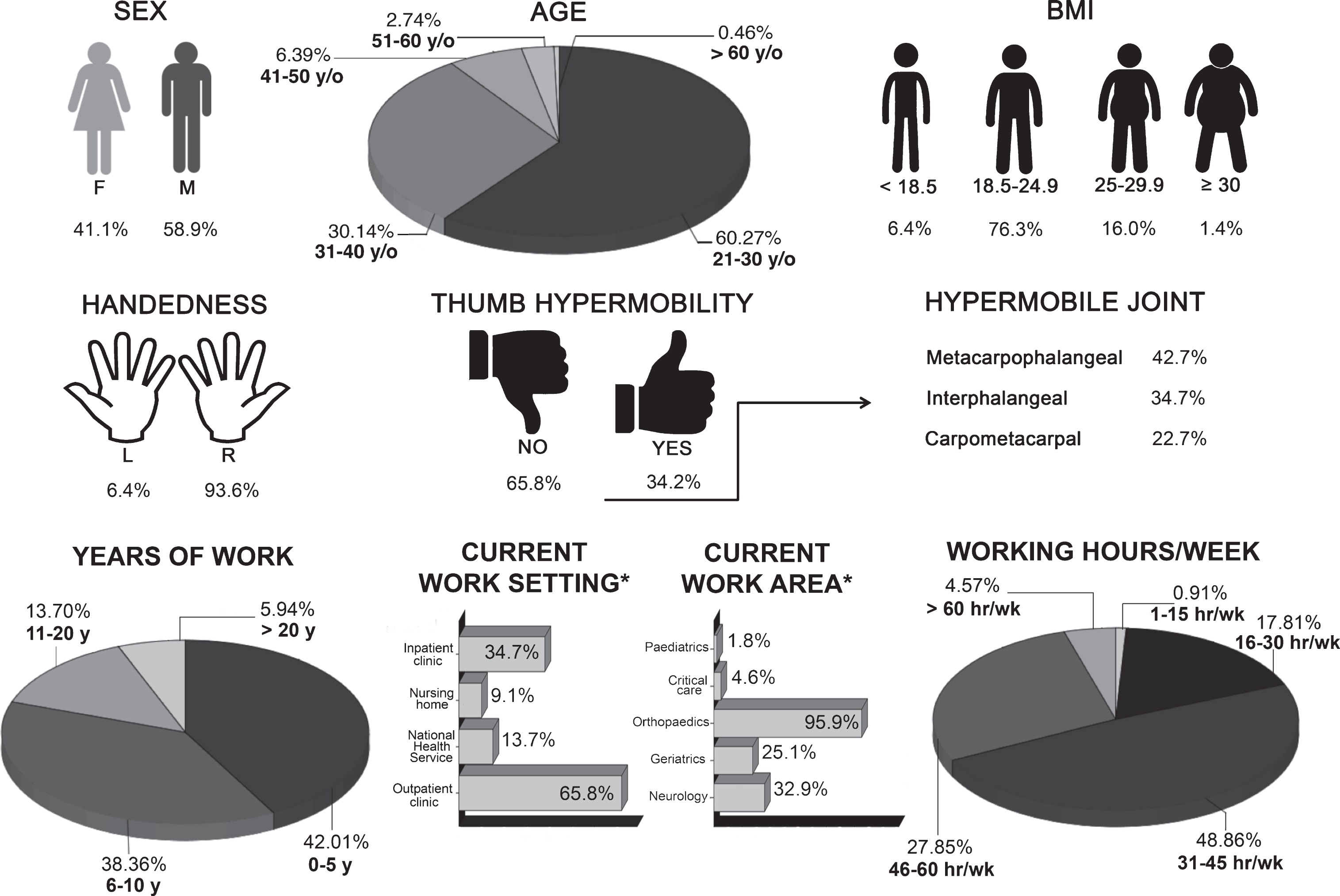
Fig.2
Performed and painful manual techniques: compared percentages. PA = postero-anterior; HVLA = high velocity low amplitude.
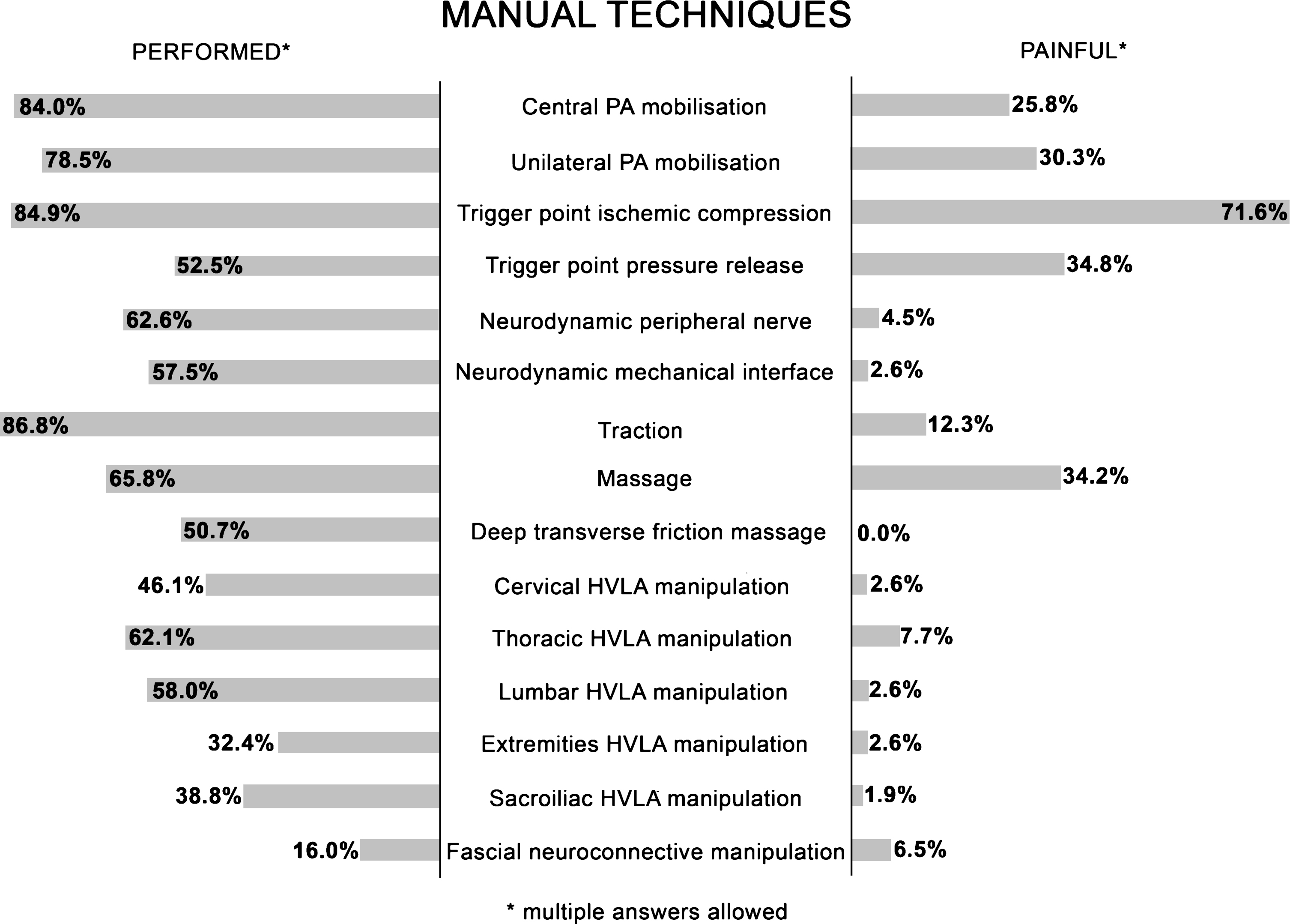
Table 1
Aggravating factors and management strategies
| Last year | Lifetime | ||
| Aggravating circumstances* | Working in the same position for long periods | 70 (64.8%) | 101 (65.2%) |
| Continuing to work when the thumb is painful | 72 (66.7%) | 96 (61.9%) | |
| Adjustable massage table/bed unavailable | 38 (35.2%) | 50 (32.3%) | |
| Psychological distress/High job demands | 13 (12.0%) | 22 (14.2%) | |
| Management strategies* | Altering practice techniques | 75 (69.4%) | 110 (71.0%) |
| Changing position frequently | 62 (57.4%) | 84 (54.2%) | |
| Performing stretching before treatment | 34 (31.5%) | 43 (27.7%) | |
| Introducing breaks into the work schedule | 30 (27.8%) | 39 (25.2%) | |
| Functional taping | 23 (21.3%) | 29 (18.7%) | |
| Electrophysical therapies | 22 (20.4%) | 29 (18.7%) | |
| Seeking intervention from a physical therapist colleague | 11 (10.2%) | 16 (10.3%) | |
| Static splinting or bracing | 6 (5.6%) | 10 (6.5%) | |
| Reducing working hours or hours on patients | 8 (7.4%) | 9 (5.8%) | |
| Medications | 1 (0.9%) | 4 (2.6%) | |
| Joint/soft tissue injection | 1 (0.9%) | 1 (0.6%) | |
| Seeking intervention from a medical specialist | 0 (0.0%) | 0 (0.0%) | |
| Electrophysical therapies which substantially improved symptoms*, § | Laser therapy | 14 (63.6%) | 19 (65.5%) |
| Tecar therapy | 8 (36.4%) | 09 (31.0%) | |
| Therapeutic ultrasound | 3 (13.6%) | 07 (24.1%) | |
| Electrotherapy | 0 (0.0%) | 0 (0.0%) | |
| Magnetic therapy | 0 (0.0%) | 0 (0.0%) |
*Multiple answers allowed. §Among those who reported using electro-physical therapies as management strategy. Results are expressed as count (percentage frequency).
Table 2
Summary of differences in pain measured by Numerical Rating Scale (expressed as median NRS 25th – 75th percentile, p value) of investigated factors significantly associated with thumb pain in the last year and in lifetime
| Last year | Lifetime | |||||
| Age | 21–30 y/o | n.s | 0.34 | n.i. | ||
| 31–40 y/o | ||||||
| Over 40 y/o | ||||||
| Sex | Males | n.i. | n.s | 0.50 | ||
| Females | ||||||
| Job factor | 0–5 years of work | 4.00 (2.00–5.00) | 0.013* | n.i. | ||
| 6–10 years of work | 5.00 (4.00–6.00) | |||||
| 11–20 years of work | 5.50 (3.00–6.25) | |||||
| Over 20 years of work | 4.00 (2.00–7.00) | |||||
| Manual techniques | Trigger point ischemic compression (vs not performed) | No | 6.00 (3.50–7.50) | 0.05* | n.s | 0.14 |
| Yes | 4.00 (3.00–5.25) | |||||
| Trigger point pressure release (vs not performed) | No | n.s | 0.81 | n.i. | ||
| Yes | ||||||
| Fascial neuroconnective manipulation | No | n.s | 0.06 | n.i. | ||
| (vs not performed) | Yes | |||||
| Management strategies to deal with pain | Electrophysical therapies | No | 4.00 (2.00–5.00) | 0.007* | 4.00 (2.00–5.00) | 0.003* |
| Yes | 5.00 (4.00–7.00) | 5.00 (4.00–7.00) | ||||
| Reducing working hours or hours on patients | No | n.i. | 4.00 (3.00–5.00) | 0.001* | ||
| Yes | 7.00 (5.50–8.00) | |||||
| Functional taping | No | n.i. | 4.00 (2.00–5.00) | 0.039* | ||
| Yes | 4.00 (4.00–6.00) | |||||
| Consequences of pain | ADL/IADL impairment | No | 4.00 (3.00–5.50) | 0.015* | 4.00 (2.50–5.00) | <0.001* |
| Yes | 6.00 (4.50–8.00) | 6.50 (5.00–7.25) | ||||
| Temporary suspension of work | No | n.i. | 4.00 (3.00–5.00) | 0.001* | ||
| Yes | 7.00 (5.00–7.75) | |||||
* = statistically significant; n.s. = not significant; n.i. = not investigated.
Table 3
Multivariate logistic regression: risk and protective factors in the development of thumb pain in the last year and in lifetime
| Dependent variable: thumb pain in the last year | Dependent variable: thumb pain in lifetime | ||||
| Protective factors | 6–10 years of work (vs 0–5 years) | 0.408 (0.215–0.775) | 0.006* | n.i. | |
| 11–20 years of work (vs 0–5 years) | 0.346 (0.139–0.859) | 0.022* | n.i. | ||
| Risk factors | Trigger point ischemic compression (vs not performed) | 2.999 (1.184–7.597) | 0.021* | 2.878 (1.319–6.281) | 0.008* |
| Trigger point pressure release (vs not performed) | 1.832 (1.005–3.340) | 0.048* | n.i. | ||
| Fascial neuroconnective manipulation (vs not performed) | 3.086 (1.346–7.077) | 0.008* | n.i. | ||
| Sex (vs male) | n.i. | 2.569 (1.339–4.930) | 0.005* | ||
* = statistically significant; n.i. = not investigated. Results are expressed as Odds Ratio (95% Confidence Interval), p value.




