Employment and accommodation needs and the effect of COVID-19 on men and women with traumatic brain injury
Abstract
BACKGROUND:
Traumatic brain injury (TBI) impacts an individual’s workforce involvement post-injury. Support services and workplace accommodations that can help with work re-integration post-TBI may differ based on a person’s sex and gender. The added impact of COVID-19 remains under-explored.
OBJECTIVE:
We aimed to investigate the support services and workplace accommodation needs and the impact of COVID-19 on work and mental health for persons with TBI, considering sex and gender.
METHODS:
A cross-sectional online survey was distributed. Descriptive and regression analyses were applied to uncover sex and gender differences, along with content analysis for open-ended responses.
RESULTS:
Thirty-two persons with TBI (62% women, 38% men) participated. Physiotherapy, occupational therapy, and counselling services were indicated as the most needed services by women and men. Modified hours/days and modified/different duties were the most needed workplace accommodations. Mental challenges impacting well-being was a highlighted concern for both men and women. Women scored poorer on the daily activity domain of the Quality of Life after Brain Injury – Overall Scale (p = 0.02). Assistance with daily activities was highlighted by women for a successful transition to work, including housekeeping and caregiving. Men were more likely than women to experience change in employment status because of COVID-19 (p = 0.02). Further, a higher percentage of men expressed concern about the inability to pay for living accommodations, losing their job, and not having future job prospects.
CONCLUSION:
Findings reveal important differences between men and women when transitioning to work post-TBI and emphasize the need for sex and gender considerations.
1Introduction
Although work is known to provide a sense of identity, prevent isolation, and improve quality of life [1], persons with disabilities remain underemployed in the workforce [2]. Traumatic brain injury (TBI), which impacts 50 million people per year worldwide [3] and is defined as an ‘alteration in brain function, or other evidence of brain pathology, caused by an external force’ [4], involves complex impairments that often impact employment [5]. An environment that does not fit the needs and abilities of an individual [6], including their biological (i.e., sex) and sociocultural characteristics (i.e., gender) can hinder employment post-injury. The Canadian Institutes of Health Research defines sex as encompassing human biological attributes, and gender as socially constructed roles, behaviours, expressions, and identities of women, men, and gender-diverse persons [7].
Currently, there are inconsistent findings on whether sex and gender are determinants of employment post-TBI [8], while age [9], injury severity [10, 11], education level [11, 12] and employment status pre-injury [11, 12] consistently reported to be associated with being employed after injury. At the same time, men have been found to more likely be employed post-injury [13] and women have been observed to work fewer hours after injury [14, 15] even though paid employment is closely linked to greater life satisfaction for women [15]. Employment differences between men and women post-TBI remain poorly understood. Employment may be influenced by unmet sex- and gender-based support needs of men and women for work re-integration [16], as existing disparity for women in unmet service needs is known for the general population [17] and meaningful employment for women with TBI disproportionately includes balancing employment with caregiving and homemaker roles [18].
Similarly, the importance of employment for men post-TBI often stems from their perceived roles as breadwinners and embodied masculine identities [19], which might be challenging to maintain post-injury [20, 21]. Occupational roles and associated identities of men and women with TBI can be strongly entangled with their sex and gender. When disrupted, they influence employment post-injury [19], emphasizing the need to understand sex and gender differences when transitioning to work post-TBI. In this paper, the terminology transition to work will be used to encompass working for the first time, starting a new job, or returning to the same or similar job (i.e., re-integration), unless specified in the literature or by research participants as return-to-work (RTW). Despite the observed inequities in employment post-TBI and known gendered predispositions, understanding this difference by examining the sex- and gender-based needs for men and women during recovery has never been explored.
A key facilitator to employment in TBI is having workplace accommodations [22, 23], which may be required for long periods following RTW post-injury [24]. Workplace accommodations can include accessibility aids and/or modifications to tasks or schedules to facilitate an employee reaching their potential at work. Research reports that the most useful TBI-related workplace accommodations include a gradual RTW and job modifications that are environment- (e.g., dimmer lighting, private office rather than cubicle) and context- (e.g., modified hours or duties) specific [25, 26]. However, it is unknown whether accommodation needs differ between men and women with TBI, given the gendered nature of TBI manifestations, recovery, and outcomes, and therefore filling this knowledge gap should be the next priority.
The coronavirus disease 2019 (COVID-19) pandemic has added further burden to the recovery of individuals with TBI, including increased mental health challenges, social isolation, and increased cognitive impairments [27]. Although there are reports that individuals with TBI experienced more stability during the pandemic, it was also highlighted that individuals were more likely to be unemployed before the pandemic or categorized as essential workers, thus generally experiencing fewer changes during the pandemic [27]. Further, although research on COVID-19 demonstrates that men and women’s employment are affected differently by the pandemic [28, 29], especially given that employment sectors can be highly segregated by sex and gender [30] and possess different pandemic restrictions, it is unknown the extent to which these disparities may be accentuated in men and women with TBI. Current studies have not addressed sex- and gender- considerations in the TBI population during the pandemic [31, 32]. This gap is important to address, considering the burden of the pandemic can compound the prevailing consequences of TBI and its sex- and gendered predispositions.
As such, considering the importance of understanding sex and gender differences for assessing and tailoring the employment and workplace accommodations that meet the needs of men and women with TBI, and in deconstructing the burden of the pandemic in this population, the study aimed to investigate, through a sex and gender lens: (1) support services needs in persons with TBI, (2) transition to work and accommodation needs in TBI and (3) the impact of COVID-19 on employment and well-being (i.e., mental health) in persons with TBI.
2Methods
The research study was approved by the research ethics boards (REBs) of the Toronto Rehabilitation Institute – University Health Network (TRI-UHN) (REB # 20-5724) and the University of Toronto (REB # 40439). The reporting of study procedures and findings followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies, for cross-sectional studies, specifically.
2.1Study design
An online cross-sectional survey was designed to investigate the support service needs, accommodations for transition to work, and the impact of COVID-19 in persons with TBI, by sex and gender. The study was conducted from November 2020 to February 2022.
2.2Recruitment and procedures
Study recruitment was facilitated through a multi-pronged approach, including (1) a list was provided by TRI-UHN centralized recruitment (CR) for contacting former TRI – University Centre Brain Injury Unit in-patients (admitted from 2017 to 2019) who had indicated interest in participating in future research; (2) an online version of the study flyer was circulated to local, provincial, and national brain injury organizations, and disability and/or employment focused organizations for advertisement; (3) the study flyer was additionally shared on social media outlets and (4) through a snowball sampling technique, in which interested participants were permitted to contact peers, community, and/or friends who have a TBI to share information about the study.
Interested potential participants underwent a short telephone eligibility screening by a study researcher (SH), who subsequently obtained written or electronic informed consent from eligible individuals. Self-referred individuals were additionally screened via the Ohio State University Traumatic Brain Injury Identification Methods (OSU TBI-ID) short-form to determine their lifetime history of TBI [33]. The OSU TBI-ID short-form is the shortest version of the OSU TBI-ID, a structured interview grounded on the Centre for Disease Control and Prevention case definitions and recommendations for TBI observation [34]. The construct validity, test/retest, and inter-rated reliability of the summary indices derived from the OSU TBI-ID have been supported [35, 36]. The OSU TBI-ID considers to be the gold standard for research and clinical purposes in capturing self-reported TBI [34]. Individuals who did not experience loss of consciousness (LOC) and responded ‘no’ to being dazed or experiencing memory loss from the injury on the OSU TBI-ID short-form were reported as having ‘no history of TBI’ and as such were not eligible for study inclusion. All consented study participants were provided with a unique link via email to self-administer the study survey online though the UHN Research Electronic Data Capture (REDCap) system. Participants who completed the study survey received a $50 e-gift card for their time.
2.2.1Eligibility criteria
Eligible participants included English-speaking persons who met the following criteria: (1) were within the age range of 18 to 65 years old (inclusive) at the time of study participation, (2) were injured at least 12 months prior, (3) resided in a community setting within Canada, and (4) previously worked full, part-time, or casually with a TBI in the last five years or are currently employed in any capacity, or on a medical leave with a current employer due to the TBI. We excluded participants who were (1) self-employed and (2) required a substitute decision maker at the time of study participation.
2.3Survey design and data collection
The study survey was created by SH and reviewed for comprehension and usability by SL, AC, and SM. The survey was pilot-tested by research colleagues and by two female adults with lived experience with an acquired brain injury. The semi-structured survey, completed online via REDCap, was approximately 30 to 45-minutes in length, composed of multiple-choice, Likert scale, and open-ended questions and the following four sections (Supplement 1):
2.3.1Demographics
This component included multiple-choice and/or open-ended questions on the individual’s sex, gender, age, education level, ethnicity or race, marital status, date of TBI, cause of TBI, level of LOC, level of post-traumatic amnesia, and dates of inpatient and/or outpatient acquired brain injury programs attended, if any. Sex, gender, age, and education level were independent variables considered in the analyses.
2.3.2Quality of Life after Brain Injury – Overall Scale (QOLIBRI – OS)
The Quality of Life after Brain Injury – Overall Scale (QOLIBRI – OS) is a six-item condensed version of the original QOLIBRI [37], that provides a summary measure to assess health-related quality of life domains that are impacted by TBI, including how satisfied an individual is with physical, cognitive, psychological, social, and daily life domains [38]. All areas are rated on a five-point Likert scale of (1) ‘not at all’, (2) ‘slightly’, (3) ‘moderately’, (4) ‘quite’, and (5) ‘very’. The mean score for each life domain were additionally converted to percentages by subtracting one from the mean and then multiplying by 25. Zero percent indicated the lowest score and 100% the highest score. The QOLIBRI – OS has previously exhibited good reliability and construct validity in TBI populations and strongly correlates with the total score of the full QOLIBRI 27-item scale measure [38]. The QOLIBRI – OS was used to measure how individuals were satisfied with health-related quality of life domains both prior to COVID-19 and during the present time. Only the latter was used in the analysis given some participants acquired their TBI during the COVID-19 pandemic.
2.3.3Statistics Canada – Canadian Survey on Disability (CSD) questions
The Canadian Survey on Disability (CSD) 2017 created by Statistics Canada and in collaboration with Employment and Social Development Canada, is the most recent national survey of Canadians aged 15 years or older who experience activity limitations because of a health condition and who live-in private dwellings [39]. The survey collects information on disability, equity and inclusion, health, society and community, and work, income, and spending [39]. Questions retrieved from the CSD 2017 included multiple-choice questions and free-text fields on general health, the use of various therapies and social service supports details, employment status, and requirements and unmet needs for accommodations at work. For these questions, the generic term ‘health condition’ was changed to ‘traumatic brain injury’ to capture TBI-related challenges.
Health support service types were assessed as dependent variables and included physiotherapy, massage therapy or chiropractic treatments, speech therapy, occupational therapy, counselling services from a psychologist, psychiatrist, psychotherapist or social worker, support group services, drop-in center services or telephone information or support lines and tutoring. Types of workplace accommodations were additionally considered and involved modified or different duties, working from home, modified hours or days or reduced work hours, human support, technical aids, computer, laptop or tablet with specialized software or other adaptations, communication aids, modified or ergonomic workstation, special chair or back support and specialized transportation.
Further, a total of five open-ended questions were created to provide an opportunity for participants to elaborate (i.e., typed by participants on REDCap) on the types of therapies, social support services, and accommodations that would have been beneficial for community integration and employment, including reasons as to why these services may not have been provided (Supplement 1).
2.3.4Statistics Canada – impacts of COVID-19 questions
Changes in employment status and mental health status due to the COVID-19 pandemic were assessed using items from a survey series developed by Statistics Canada to understand the impact of COVID-19 on the physical and mental well-being of Canadian persons as well as their social, post-education, and employment environments [40, 41]. The collection series primarily involves questions on disability, economic accounts, health, income and expenditure accounts, mental health and well-being, education, training and learning, and labour [40, 41]. Questions retrieved from the series included multiple-choice and five-point Likert scale questions on the impacts of COVID-19 and were modified to primarily inquire on work status and mental health for adult persons with TBI.
2.4Sample size determination
A sample size of equal to and/or greater than 30 persons is deemed appropriate for pilot studies [42]. With respect to sample-to-variable ratio, a minimum of five respondents in survey research must be reflected for each independent variable in the statistical analysis model [43]. The main independent variable in our analyses was sex and gender, while considering education and age in the model. Provided this, a sample size of 30 individuals for the study survey would be considered adequate.
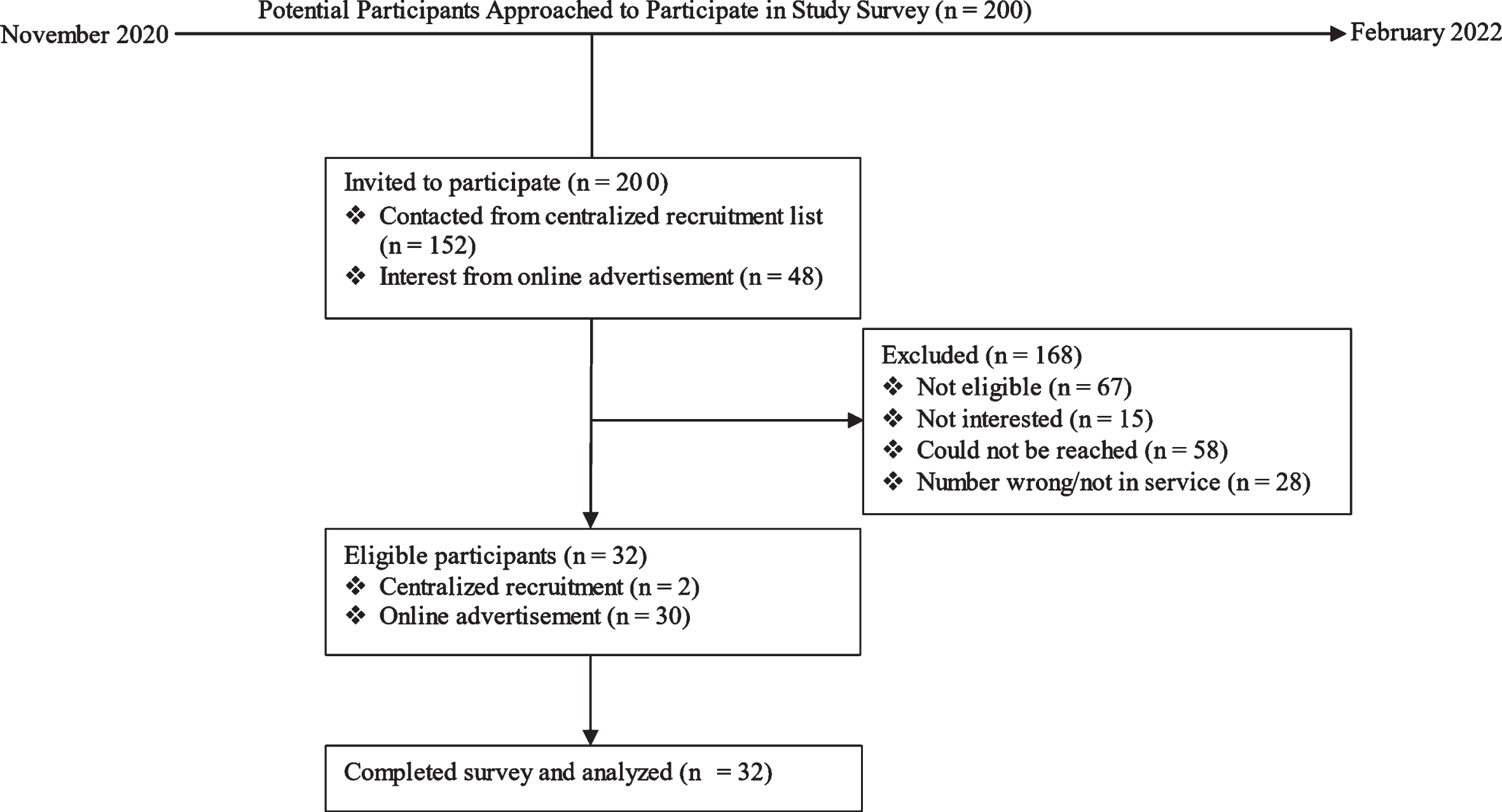
Fig. 1
Flowchart of the total number of participants approached and eligible for survey completion.
2.5Data analysis
Descriptive statistics were calculated for continuous and categorical variables of defined sample characteristics. Frequency distributions and percentages were additionally used to report sex and gender group differences in outcome variables. Between-group comparisons for sex and gender were completed using the Mann-Whitney U test or independent t-test to understand whether differences exist on described dependent variables between men and women with TBI. Binary or ordinal logistic regression analyses were computed for any statistically significant dependent variables observed in the performed non-parametric and parametric tests. Further, Quasi-Poisson regression analyses were used to evaluate the relationship between the number of workplace accommodations needed and those received by men and women. No missing data was present in the analysis. The significance level was set at less than 0.05 for all analyses. Analysis of quantitative data was computed via the R Project for Statistical Computing software, version 4.1.2.
Open-ended questions were analyzed using qualitative description [44] and a conventional content analysis approach, which is used for study designs that describe a phenomenon with limited existing literature and theory [45]. Study author (SH) first read through the data in its entirety and repeatedly; then created codes from elaborations provided in the free-text response fields by highlighting the exact words that exemplified central concepts; and finally identified common categories among the generated codes, noting down supporting quotes. A peer-review approach by author SM was utilized, in which SH and SM met to discuss generated codes and categories, ensuring that a final consensus was made.
3Results
3.1Sample profile
A total of 32 participants completed the study survey (see Fig. 1). Thirty participants were recruited from online advertisement and two from the list provided by CR. Table 1 provides an overview of the characteristics of participants included in the study. The sample consisted of 62.5% (n = 20) of female persons, in which all female persons identified themselves as women and 37.5% of male persons (n = 12), in which all male participants identified themselves as men. Given this, the designation of men and women will be used to report the results. The median age was 37.0 years (interquartile range, IQR = 16.25), with a range of 20 to 64 years old. Fifty-three percent (n = 17) of respondents were married or were in common law relationships. Participants had the opportunity to select race and/or all ethnicities that were applicable, and as such, this category aggregates to greater than 100%. Eighty-four percent (n = 27) of participants identified their race as white. No participants identified their race as black. Most participants either held a post-secondary education diploma or bachelor’s degree as their highest level of education. Though 27 respondents indicated they were employed at the time of their TBI, only 20 participants (62.5%) were employed at the time of survey completion with combined occupations in health, and occupations in sectors of education, law, social, community and government services, constituting 40% of held employments. Further, those employed during the study period indicated working a median of 38.75 hours per week (IQR = 26.50) (range two to 60 hours/week), of which 90% of those working part-time (i.e., less than 30 hours/week), indicated their TBI as the primary reason. Motor vehicle collisions (e.g., truck, automobile, motorcycle, bicycle, pedestrian) comprised approximately 34% of TBI mechanism of injury, followed by fall and sports-related injuries (combined 37.6%).
Table 1
Personal characteristics of study participants
| Variable | Overall | Male | Female | p-value | |
| Age (median years, IQR) | 37.0, 16.3 | 34.5, 16.8 | 38.5, 15.5 | 0.879 | |
| Level of education, n (%) | 0.004* | ||||
| High school diploma | 2 (6.3) | 1 (8.3) | 1 (5.0) | ||
| Post-secondary education diploma | 12 (37.5) | 8 (66.7) | 4 (20.0) | ||
| Bachelor’s degree | 11 (34.4) | 2 (16.7) | 9 (45.0) | ||
| University certificate/diploma above bachelor’s level | 1 (3.1) | 0 (0.0) | 1 (5.0) | ||
| Advanced degree | 6 (18.8) | 1 (8.3) | 5 (25.0) | ||
| Ethnicity or race, n (%)† | |||||
| White | 27 (84.4) | 9 (75.0) | 18 (90.0) | 0.27 | |
| North American | 2 (6.3) | 0 (0.0) | 2 (10.0) | ||
| European | 9 (28.1) | 2 (16.7) | 7 (35.0) | ||
| Aboriginal | 1 (3.1) | 0 (0.0) | 1 (5.0) | ||
| Latin American | 2 (6.3) | 1 (8.3) | 1 (5.0) | ||
| South Asian | 2 (6.3) | 2 (16.7) | 0 (0.0) | ||
| West Indian | 1 (3.1) | 0 (0.0) | 1 (5.0) | ||
| Marital status, n (%) | 0.44 | ||||
| Never married | 11 (34.4) | 4 (33.3) | 7 (35.0) | ||
| Married/living with someone/common law | 17 (53.1) | 5 (41.7) | 12 (60.0) | ||
| Divorced/separated | 3 (9.4) | 2 (16.7) | 1 (5.0) | ||
| Widowed and not remarried/living with someone | 1 (3.1) | 1 (8.3) | 0 (0.0) | ||
| TBI cause, n (%) | 0.36 | ||||
| Motor vehicle collision | 11 (34.4) | 5 (41.7) | 6 (30.0) | ||
| Fall | 6 (18.8) | 2 (16.7) | 4 (20.0) | ||
| Sports-related | 6 (18.8) | 3 (25.0) | 3 (10.0) | ||
| Interpersonal violence (other than gunshot) | 1 (3.1) | 1 (8.3) | 0 (0.0) | ||
| Work related injury | 4 (12.5) | 0 (0.0) | 4 (20.0) | ||
| Other | 4 (12.5) | 1 (8.3) | 3 (15.0) | ||
| Employment sector, n (%) | 0.17 | ||||
| Business, finance &administration occupations | 3 (15.0) | 2 (50.0) | 1 (6.3) | ||
| Natural and applied sciences &related occupations | 2 (10.0) | 1 (25.0) | 1 (6.3) | ||
| Health occupations | 4 (20.0) | 0 (0.0) | 4 (25.0) | ||
| Occupations in education/law/social, community &government services | 4 (20.0) | 0 (0.0) | 4 (25.0) | ||
| Occupations in art, culture, recreation &sport | 2 (10.0) | 0 (0.0) | 2 (12.5) | ||
| Sales &service occupations | 3 (15.0) | 0 (0.0) | 3 (18.8) | ||
| Trades, transport, and equipment operators &related occupations | 1 (5.0) | 1 (25.0) | 0 (0.0) | ||
| Natural resources, agriculture &related production occupations | 1 (5.0) | 0 (0.0) | 1 (6.3) |
Abbreviations: N – number, IQR – interquartile range. †Ethnicity or race category does not sum to 100% due to nature of survey question to select all that apply. p-value reported for white race only. *p < 0.05.
3.2Quality of life and health support
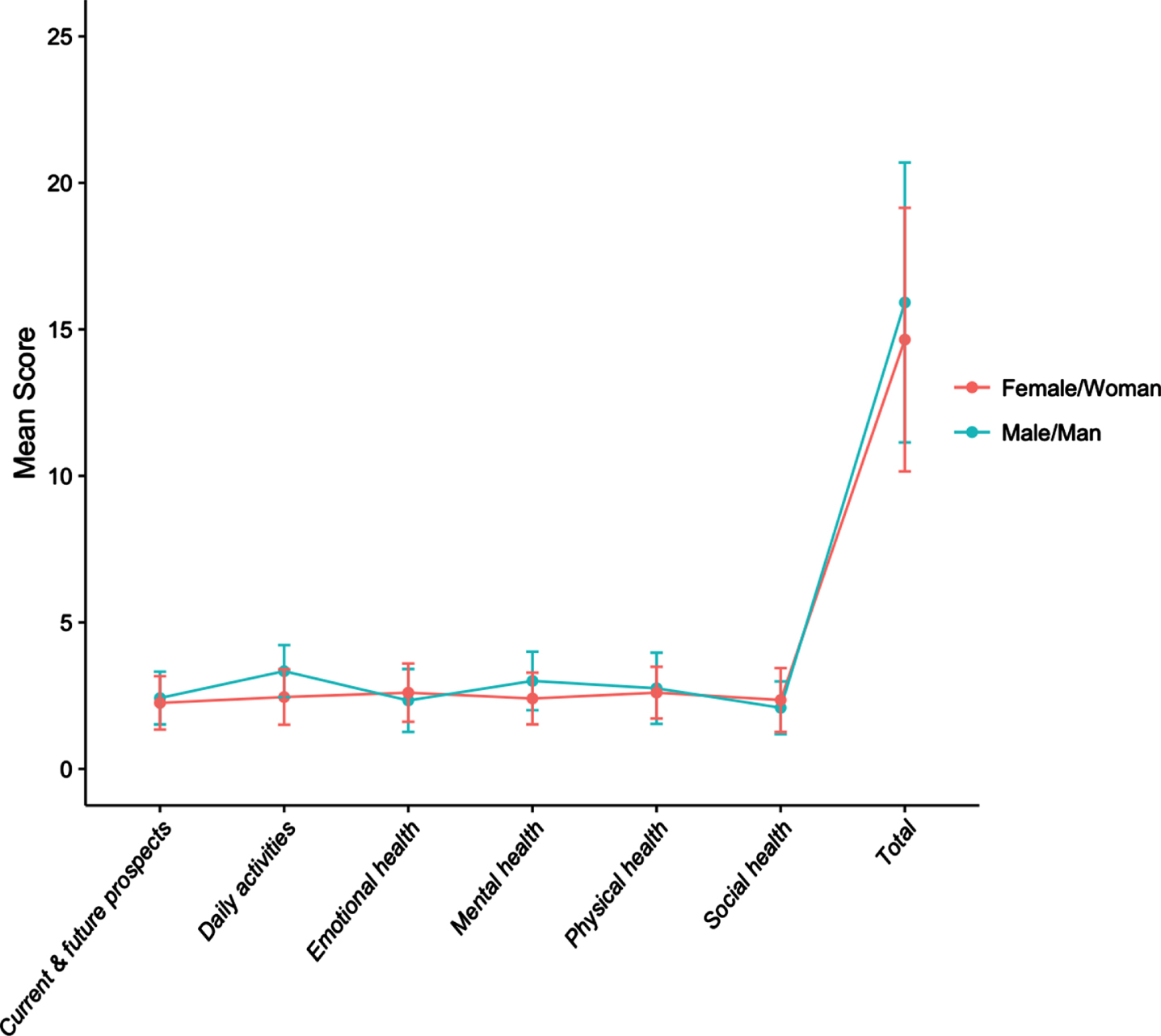
A score of less than 50% was observed in all health-related domains of the QOLIBRI – OS, including satisfaction with physical health, mental/cognitive health (i.e., concentration, memory, thinking), emotional health (i.e., feelings and emotions), ability to carry out daily activities, personal and social life, and current situation and prospects. When stratified by sex and gender, scores of men differed from that of women in domains of daily activities and mental health, though the difference was only significant for the daily activities’ domain (Mann-Whitney U test, p = 0.02; ordinal logistic regression analysis, odds ratio (OR) = 5.44, 95% confidence interval (CI) = 1.32, 22.39, p = 0.02) (Supplement 2). Figure 2 demonstrates the total and subscale mean scores of the QOLIBRI – OS by sex and gender. Examining the relationship between the total score for each participant and sex and gender revealed a lack of significant association (independent t-test, t = 0.75, CI = – 2.17, 4.70, p = 0.46).
Fig. 2
Total and subscale mean score of QOLIBRI – OS by sex and gender.
Among the reported support services, categories of physiotherapy, massage therapy or chiropractic treatments and counselling services from a psychologist, psychiatrist, psychotherapist or social worker were the most indicated services received on a regular basis for both men and women (Supplement 3). Further, categories of physiotherapy (40.0%), counselling services (30.0%), and occupational therapy (30.0%) were the most indicated as needed by women on a regular basis in the 12 months preceding the survey completion but were not received, whereas most men (66.7%) indicated not needing any further support services, followed by expressed needs of counselling services (33.3%), occupational therapy (16.7%), physiotherapy (16.7%) and support group services (16.7%). Seven participants commented on other types of services that were needed but not received that were not presented in the survey. Examples included lack of specialists in TBI care with expertise in concussion management; sleep problems and hormonal changes; endocrinologist; neck specialist; audiologist; home services to assist with organization; and vision therapy. No statistically significant difference was found by sex and gender for support services needed or received (Supplement 2, Mann-Whitney U test, p > 0.05).
3.3Employment and accommodations
Approximately 90% of individuals specified that due to their TBI, they took a leave of absence from work for one month or more (84.4%), had to change the amount of work that they do (78.1%), had to change the kind of work that they do (50.0%), had to change jobs (34.4%), and began working from home (28.1%). Further, approximately 84% of respondents indicated that their TBI made it difficult to change jobs or advance in their present employment. Reasons for this included difficulty adapting to a new work environment (92.6%); TBI limited the number of hours that can be worked (74.1%); discrimination or stigma because of TBI (51.9%); difficulty to obtain required supports or accommodations (40.7%); TBI limited the ability to search for a job (33.3%); and other reasons (44.4%) (e.g., anxiety, needing more schooling to change careers, inconsistency in health).
Eighty-four percent of respondents indicated that they disclosed to their employer about their TBI and approximately 53% reported that their employer is aware of the needed workplace accommodations. Among the reported accommodations, modified hours or days or reduced hours and/or modified or different work duties were the most often needed and received accommodations for both men and women (Fig. 3). Further, 28.1% indicated the need for other types of accommodations to be able to work, such as low-level light-emitting diode lighting instead of fluorescent lighting, listening to music to eliminate external stimuli, and short breaks hourly or following cognitively taxing tasks to allow for dark and minimal stimulation. No statistically significant difference was found by sex and gender for accommodations needed or received (Supplement 2, Mann-Whitney U test, p > 0.05).
Fig. 3
The types of accommodations (a) needed and (b) received as indicated by participants and by sex and gender.
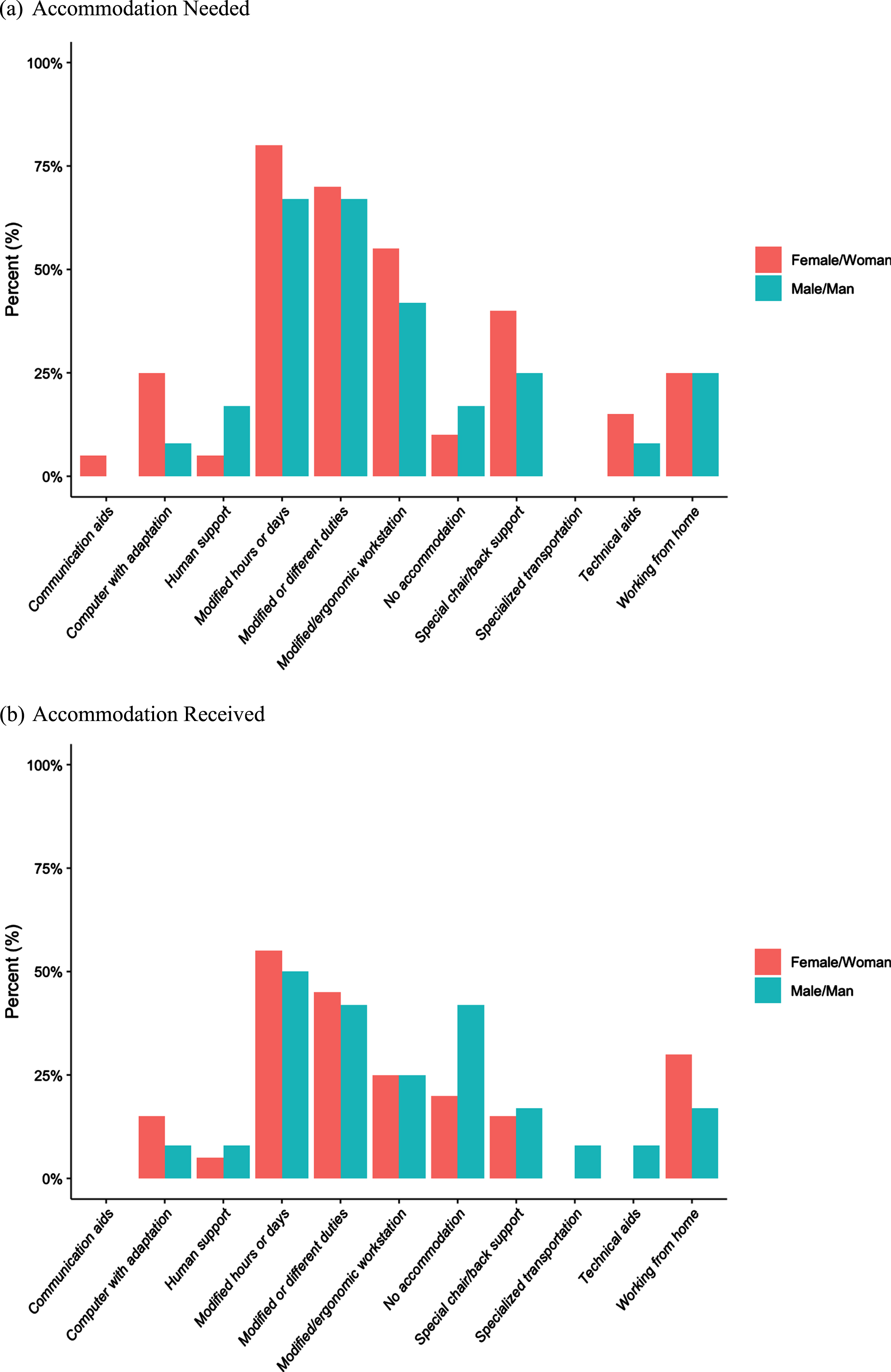
A Quasi-Poisson regression analysis was conducted to test the relationship between the number of accommodations needed and those received and whether relevant variables such as sex and gender, age or education were significantly associated with the number of accommodations needed and/or received. Results showed a significant association between the number of accommodations needed and those received (OR = 1.19, CI = 1.03, 1.38, p = 0.02). However, when stratified by sex and gender we observed that this relationship remained significant only for men (OR = 1.73, CI = 1.24, 2.41, p = 0.01). Examining the number of accommodations needed and received individually, the findings indicated that although sex and gender, age, and education were not associated with the number of accommodations needed, education (OR = 1.39, CI = 1.08, 1.79, p = 0.02) was shown to significantly influence the number of accommodations received.
3.4Impact of COVID-19
Fig. 4
Level of concern on impact of COVID-19 pandemic for male/man (a) and female/woman (b) persons.
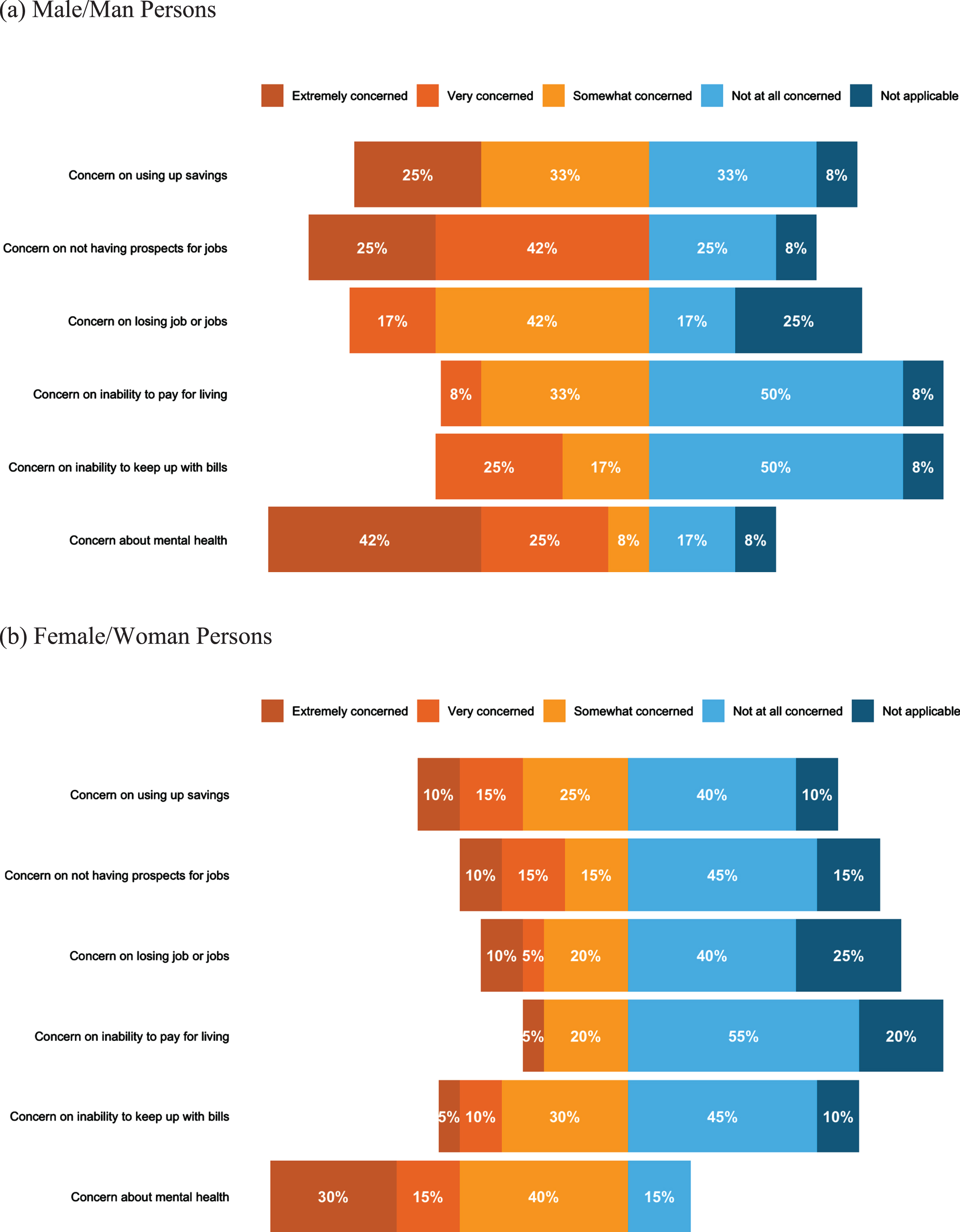
Twenty-two study participants (68.0%) indicated being employed at the beginning of March 2020 (15 women, seven men). As a result of the COVID-19 pandemic, four participants indicated they were still working but working less often (12.5%); six individuals indicated they either lost their jobs, lost a job that was supposed to start in the future, no longer have employment prospects, or currently looking for work (combined 18.8%); and 22 persons indicated no change in their employment status (68.8%). Further, of the 22 individuals who experienced no change in their employment status, 17 persons were women (77.3%). An association between sex and gender and changes in work status during the COVID-19 pandemic (Mann-Whitney U test, p = 0.01) was shown, with men less likely to experience no change in work status during the pandemic (binary logistic regression analysis, OR = 0.63, CI = 0.44, 0.90, p = 0.02). There were no significant differences in age or educational level and employment status due to the pandemic (Supplement 2).
With respect to mental health status since the COVID-19 pandemic, 13 respondents rated their mental health as fair or poor (combined 68.8%). As compared to before COVID-19, 31.2% indicated feeling much or somewhat better now, 21.9% indicated feeling about the same, and 46.9% indicated feeling somewhat or much worse now. Further, when asked about how concerned individuals were on the impact of the COVID-19 pandemic on paying for living accommodation, keeping up with other bills and payments, using-up savings, losing job or jobs, not having prospects for a job in the near future, and their mental health, a higher percentage of men were particularly concerned about the inability to pay for living accommodations, losing job or jobs, and not having prospects for a job in the future compared to women (Fig. 4). Further, a large percent of both men (75.0%) and women (85.0%) were concerned about their mental health during the COVID-19 pandemic, with 67% of men reporting being extremely and very concerned compared to 45% of women (Fig. 4).
3.5Qualitative findings
Two overarching themes were identified from the study’s open-ended questions: (1) barriers to receiving proper support services and accommodations, including limited finances, unsupportive emotional and physical work environments, lack of TBI knowledge, restrictive insurance policies, and COVID-19 amplified challenges; and (2) necessities for adequate transition to community and work, involving access to expertise while transitioning to community; help with daily activities as part of gradual RTW plan; and immediate access to resources, follow-up and clinician engagement.
3.5.1Barriers to receiving proper support services and accommodations
Limited finances. Ten respondents (all women) commented on expensive costs and limited finances as deterrents for receiving the therapies or support services that were needed. For example, a participant indicated:
I have neck pain and upper neck and body strain. It’s a daily issue. I have daily head pressure, nausea and dizziness that comes and goes. I can’t move too quickly, can’t stand or sit for long periods of time, and I definitely cannot look at computers or mobile devices for extended time. I have a problem with my eyes, especially the right one. I have no income, so there isn’t much I can get help with ... I have already spent over $10,000 in massage, physiotherapy, chiropractic care, etc. it has all slightly helped, but no real alleviation of all ills (ID 025, woman).
Another participant voiced concern regarding purchasing needed accommodations while working from home and said, ‘It was pricey [employment accommodation] and then we were working from home with COVID. It just didn’t seem feasible to spend the money on renovations when we did not know what the future would hold’ (ID 005, woman).
Unsupportive emotional and physical work environments. Nine study participants (five men, four women) elaborated on the impact of an unsupportive employer or abrasive workplace culture in receiving the needed support services and accommodations, across a continuum of lack of understanding to harassment or stigmatization. For instance, a participant said, ‘I did not receive mental health support because, despite disclosing my challenges, I did not explicitly ask for it and my employer did not think it was their responsibility to take care of this area. Further, I went back to work too quickly because my employer was eager to get me working again as they lose a lot of income when I am not working’ (ID 014, woman). A second individual voiced the need for a supportive manager that accepts their impairments and accommodates for their needs and said the following, ‘A non-judgmental supervisor when I benefit from sunglasses, or noise canceling headphones for noisy locations. I’m now unemployed as the [employer] felt the two years of harassment wasn’t a big deal, even though they found it in their own investigations to be true’ (ID 032, man). Participants shared their experiences of stigmatization following disclosure of their disability or the need for modifications. For example, a participant said ‘I don’t feel it [TBI] is well understood, and any employer I have opened-up to about this, it has gone very negatively. I was laid off from a job of four years when I disclosed that flying which was a big part of my job was difficult and made me feel very ill, and I was let go from the job less than three months later’(ID 023, man).
Further, four participants (one man, three women) expressed the lack of physical support in the workplace, including the cost and feasibility (i.e., nature of the job) that accompany the implementation of their needed accommodations by their employer. A participant said, ‘That extra academic support [smaller class size and educational assistant (EA)] would make a world of difference. However, both class size and EA support come down to the cost of education and becomes a political issue. So, I’m not sure these supports would ever be considered’ (ID 026, woman).
Lack of TBI knowledge. Eight participants (four men, four women) discussed that lack of TBI knowledge or awareness of available resources by either persons with TBI, health care providers, or employers as barriers to receiving appropriate help. For example, an individual described the lack of proper TBI knowledge they personally have for handling their recovery and said, ‘I’m not educated enough on the types of concussion recovery I should be doing, I’m just living life and not really dealing with my issues in a proper way’ (ID 023, man). A second individual underscored this point in addition to their employer’s knowledge gap on TBI trajectory and shared the following ‘These [accommodations] were not provided to the extent they should have been from a lack of understanding from myself and the employer how long the effects of the TBI could last’ (ID 012, woman). Further, a participant highlighted the need for ‘a one-stop-shop portal’ to know what services are available and which can be beneficial to TBI survivors.
Restrictive insurance policies. Seven individuals (one man, six women) described restrictive insurance policies that limited the ability to receive support services and accommodations. For example, an individual explained ‘It was a [Insurance X] rehabilitation program and so basic needs were met (technically), but anything else above or beyond or out of the box thinking wasn’t possible’ (ID 021, woman). A second participant reiterated the following ‘[Insurance X] doesn’t provide nanny care, even though it was my full-time job when I was injured and someone else needs to fill in for me. I am currently working on getting a cleaner through them, but it is very difficult to do so (I’ve been asking for over a year)’ (ID 015, woman). An individual additionally highlighted that since the insurance company does not view their TBI as requiring accommodations they can only RTW when at full capacity, as directed by their employer.
COVID-19 amplified challenges. Finally, six persons (three men, three women) indicated the additional challenges that the COVID-19 pandemic had on their TBI, specifically with a lack of continuity in care, difficulty in booking and accessing support services, and hesitancy in inquiring on needed workplace accommodations. To illustrate this, one person indicated ‘COVID makes it hard to be in as frequent or meaningful contact with doctors and other healthcare professionals’ (ID 013, man). A second individual expressed the fear of asking for the needed modifications during COVID-19 due to the repercussions it may have on their employment and said, ‘... did not ask for further reduction in hours due to onset of COVID-19 pandemic; layoffs were happening, and companies were running lean on manpower; security of employment felt at risk’ (ID 016, woman). In addition to the challenges experienced during the pandemic, one individual also shared the positive impacts of COVID-19 and said:
When COVID hit, the world had to slow down. So, in a weird way, this was nice for me. Finally, the world was moving at a slower pace. Because of my TBI, I had already learned to be grateful and look for everyday blessings. So, the isolation and changes brought on by COVID didn’t really affect my mental health in a negative way. The social pressures and strains on relationships were no longer there when I had to say “no”. i.e., everyone was to stay home with COVID, so the reason didn’t have to be because of my TBI anymore. The COVID lockdowns also meant I could pace and plan my therapies more (ID 026, woman).
3.5.2Necessities for adequate transition to community and work
Access to expertise while transitioning to community. Thirteen participants (five men, eight women) expressed the need for mentorship from someone who understands TBI, to provide them with proper guidance instead of having to navigate the transition on their own. For example, an individual described the following ‘Throughout this journey, there really hasn’t been any one person coordinating what needs to be done other than me. I have been learning on the fly over the past 7 years and it can be overwhelming. We are kind of left on our own to find out things’ (ID 003, man). This point was communicated several times, including needing a clinician who has expertise in concussion management, a case manager to help find the proper therapies needed, connections with employers that have previously hired employees with TBI, a mentor to help explain to family and work what TBI recovery entails including expectations and abilities, someone to explain the process of long-term disability and RTW, and a shadowing opportunity with a survivor who has coped with TBI in the past. A participant underscored this further and described needing, ‘... a professional who would have a hands-on role in helping me return to former activities I enjoyed or finding replacement activities I enjoy’ (ID 013, man).
Help with daily activities as part of gradual RTW plan. Nine persons (two men, seven women) explained the need for help with everyday challenges post-TBI, including adjusting both at home and at work. Individuals indicated ‘I cannot imagine going back to work until I can function normally at home’ (ID 006, woman) and ‘I would have liked to have more help with my kids and care for my home (cleaning)’ (ID 015, woman). Two additional women also described requiring day-to-day assistance including housekeeping, help with groceries, and child caregiving including maintaining active extra-curricular activities for children. Other persons expressed the importance of a gradual RTW plan for balancing the demands of work and homelife. For instance, a woman participant noted ‘... someone who could have been more involved in my corner to help with putting balance into perspective and to help eliminate the guilt of going off work because of the daily symptoms that it was creating and the lack of involvement at home and everything I was missing out on in my children’s life because I felt guilty, I wasn’t feeling 100% and guilty if I wasn’t working pretending I was fine when I really wasn’t’ (ID 027, woman).
Nine people (three men, six women) expressed that an explicit, gradual RTW plan would help with maintaining employment productivity and success, including a slower transition post-injury, time off as needed, reduced hours over a longer period, and less workload to provide an appropriate amount of time for recovery and for adjustment to cognitive demands of work-related tasks. A participant stressed that transition to work should be a step-by-step process to adequately assess needs and ensure that needs are met:
A good return to work plan would be critical including initial expectations, retraining, and hours to be worked. I would also include a formal regular review to understand how things may or may not be progressing. How I am actually feeling physically and mentally, does the RTW plan need to be adjusted and how the Manager and Supervisor see things. Additionally, reporting structure would be very important until it was determined if I was still capable of performing the role competently, and finally a complete reset in terms of performance, start as if it was day one. It would also be prudent to have a qualified OT [Occupational Therapist] with understanding of concussions and RTW available to properly assess the plan and any physical work environment (ID 003, man).
Immediate access to resources, follow-up and clinician engagement. Four individuals (one man, three women) spoke of the need for immediate access to support services and/or accommodations post-TBI for proper recovery. One participant described the following ‘I wish I had received physiotherapy earlier than I started so I would have been able to work towards healing faster. I wish my doctor had recommended other resources sooner instead of waiting for it to get better itself... ’ (ID 029, woman). A second participant reiterated this point and described the inability to receive therapies promptly given she was diagnosed with TBI one-month post-injury. Another person described wishing to have received help immediately during hospitalization from a social worker for herself and her family members. This point was further highlighted for access to accommodations as well, in which a participant stated ‘It’s not so much the type [of accommodations] for as it is the timing. The accommodations came too late, which extended and increased my symptoms’ (ID 020, man).
Further, four study participants (all women) described the importance of frequent follow-ups, including the engagement of clinicians during the individual’s transition to community and work. An individual reported the following ‘I would have liked to have had more advice at the time of the injury. I would have liked for there to have been follow-up. I would have liked to be connected to resources. I would have liked help deciding how to adjust to my new life and accept and grieve the loss of my old goals’ (ID 009, woman). This was explained by a second woman, who highlighted that it would have been beneficial to have an occupational therapist (OT) engage in their transition to work and said ‘The occupational therapist was going to meet with my boss, but never did. That could have been helpful. Also, I think it would be helpful for me to have a check-up with the occupational therapist at three months, six months, and 12 months back to work. At first, I was just so determined to get back to work, and not be a statistic, but lately I have been feeling like I may not have the energy and wherewithal to keep up the pace and handle all the variables long term’ (ID 005, woman). Another woman reported that continuous engagement from an OT, including in the workplace would have helped with developing strategies for undertaking tasks at work. Similarly, the same individual expressed that engagement from a physiotherapist would have assisted with ‘lingering vestibular issues’ and increase ‘exercise and stamina’, which would have mitigated the impact of ‘dizziness with work-related movements’ and ‘longer shifts’ at work for the individual (ID 025, woman).
4Discussion
This study investigated the sex and gender differences in support services and workplace accommodation needs of men and women with TBI. The research further provided critical information about how the COVID-19 pandemic impacts men and women’s employment and mental health post-TBI.
Findings from the survey showed that men and women’s quality-of-life was impacted post-injury across health-related domains of physical health, mental health, ability to carry out daily activities, personal and social life, and current situation and prospects. While the total QOLIBRI – OS score was not significantly different for men and women as consistently observed in previous research [46], men scored significantly better in the daily activities’ domain than women. Requiring help with daily activities was also identified in our qualitative findings as a gap and an area of necessity for appropriate community re-integration. Specifically, women expressed requiring help with housekeeping, grocery shopping, and caregiving responsibilities, emphasizing sex and gender implications for women in balancing domestic life in conjunction with transition to work post-injury. The cumulative workload and double burden for women who are transitioning to work and undertaking gendered responsibility influence RTW sustainability [47]. This trend requires recognition and assistance by health care providers and employers to proactively promote job sustainability for women with TBI by considering their gendered needs, without withdrawing from either responsibility [47]. This finding substantiates previous literature in the acquired brain injury population, on women navigating different challenges according to their gender, and the emotional distress experienced in the inability to meet gendered expectations and perform gendered roles (e.g., managing household, caregiving) while adapting after a life-changing injury [48], as traditional gender roles for men primarily involve undertaking tasks in the workplace and domestic life and family are often viewed as a support systems rather than as an additional burden [47].
Although sex and gender differences in needed support services were not observed, findings from the survey highlighted that both men and women with TBI needed regular participation in physiotherapy, massage therapy or chiropractic treatments, occupational therapy, and counselling services from a psychologist, psychiatrist, psychotherapist, or social worker post-injury. Additionally, our qualitative findings underscored the need for an undisrupted continuum of care for persons with TBI, starting with immediate access to support services and resources post-injury and leading to consistent follow-up with clinician engagement, such as OT involvement in the workplace to assess the work environment and related tasks for the development of suitable strategies. The difficulty experienced by persons with TBI in navigating the healthcare system and finding appropriate rehabilitation post-injury has been previously documented [49], with the lack of continuum in care profoundly hindering community re-integration. This gap accentuates the need for designated personnel to coordinate rehabilitation for persons with TBI with an ongoing follow-up period with clinicians, while recognizing the chronic effects of TBI and its influence on life post-injury [49, 50]. Past research has complemented our findings and showed that communications between employers and OTs can benefit the vocational rehabilitation programmes of persons with TBI, stressing the usefulness of OT involvement for both individuals with TBI and their employers in providing the reflection and tools needed for TBI re-integration [51].
While access to expertise to guide re-integration, target injury-related clinical manifestations (e.g., sleep issues, hormone disruptions, neck injury), and explain transition to work practices was shown to be notably needed in our qualitative findings, the accessibility of services for persons with TBI is cost depended, as also identified in our findings by women. Though some therapies are governmentally funded in Ontario (e.g., physiotherapy), others can be partly funded (e.g., occupational therapy), or require flexible insurance plans or complete out of pocket payments by individuals (e.g., counselling services). As such, accessibility to needed services is heavily reliant on the cause of TBI (e.g., access to automobile insurance or Workplace Safety and Insurance Board), availability of extended health insurance plans, and employment status and income. These factors have been shown to be influenced by sex and gender [13, 52, 53] and thus may disproportionally impact men and women with TBI, placing the financial burden on survivors and circumstantially limiting the sustainability of service participation. As such, understanding men and women’s personal life and valued goals and expectations can enable the provision of resources and support services that are needed.
In accordance with a recent study [25], our findings demonstrated that the most needed accommodations to help with transition to work in persons with TBI were modified hours or days or reduced hours and modified or different work duties in both men and women. However, in many cases workplace accommodations remain unavailable due to limitations in employers’ resources [51] or may not fit the specific needs of individuals post-injury [54]. For men with TBI, our results showed that each additional number of accommodations needed was associated with 73% more of accommodations received. Education was also shown to influence the number of accommodations received. These findings are novel and a further understanding of who may be receiving more accommodations post-injury is needed, to uncover potential workplace inequities that should be addressed. Further, a gradual RTW plan was highlighted in our qualitative findings as a facilitator to transitioning to work. The idea of a gradual RTW plan for persons with TBI that involves, for example, beginning with few hours or days and gradually increasing when feasible for the individual has been discussed previously [25]. However, while those types of accommodations are recognized as facilitators to transitioning to work post-TBI [50], our findings revealed that not all individuals received the needed help, partly due to restrictive insurance policies. As such, attention is needed for developing a standardized method of creating a transition to work plan for individuals with TBI, that involves key parties (e.g., employers, clinicians, persons with TBI, insurance companies), considers personal and workplace factors, and involves periodical reassessment given the changing nature of TBI [25]. An unsupportive emotional and physical work environment can also diminish accommodations. As such, the importance of workplace factors (e.g., job stability, supportive managers/co-workers) on disclosure decision-making [55] can help with securing accommodations [56], while eliminating the fear of stigmatization [57].
The added challenges prompted by the COVID-19 pandemic on persons with TBI have been the focus of recent research [27]. Though most individuals in our study were employed prior to the pandemic, which contrasted with previous findings [27], the majority similarly experienced no change in their employment status following COVID-19 [27]. A sex and gender difference was additionally demonstrated with men more likely to experience change in their employment status due to the pandemic compared to women. This could potentially be explained by the high percentage of women occupying employment in health, education, and sales and service [58] and as such be regarded as essential workers [29], with their occupations less likely to exhibit status change. At the same time, our study showed that a larger percentage of men were concerned about employment and financial security. This also supports the gendered expectations of men as financial providers [21] and the stress that may ensue in meeting this expectation post-injury and during COVID-19. Further disruptions to the continuum of needed care and the fear of disclosing disability needs, given COVID-19 layoffs and decreased job opportunities were also expressed in our findings and in previous research [59]. The COVID-19 pandemic has also increased the mental health challenges post-TBI [27]. However, research on this remains scarce in TBI, particularly across sex and gender. As such, our research provides a platform for the exploration of the interplay between COVID-19, transition to work, and the added mental health challenges experienced by men and women with TBI. Given both men and women with TBI expressed unequivocal concern about their mental health during the pandemic, this is an area of focus that deserves attention for rehabilitation follow-up and involvement and from employers (e.g., compensation, accommodation), as new onset mental health disorders (e.g., anxiety, depression) can limit RTW sustainability as observed in individuals with musculoskeletal injuries [60].
4.1Limitations
While this exploratory study uniquely reports on important differences between men and women post-TBI for community participation, including the added impact of COVID-19, it also has limitations. First, given that this was an observational cross-sectional study survey, it is difficult to determine the cause of the change and needs, making the associations identified difficult to interpret. Additionally, given the size of the sample, the precision of analytical outputs may be impacted. Second, some study participants had their TBI sustained during the COVID-19 pandemic, which may have influenced the extent to which COVID-19 solely impacted their employment and mental well-being, compared to individuals who had their TBI years prior and may have had more time for transitioning to community and work. Third, survey responses were susceptible to response, recall, and social desirability biases due to the nature of the study design. Fourth, although most participants indicated their race as white (84%), the remainder did not indicate their race, and only reported their ethnicity. As such, even though no participants identified themselves as black, it is difficult to know whether this was the case. Fifth, despite our efforts to recruit across sex and gender, we did not have any study participants that identified as gender-diverse individuals. Future research should examine how community participation post-TBI including during unprecedent times for LGBTQ2S+ individuals may be impacted.
5Conclusion
This study explored the support services and workplace accommodation needs of men and women with TBI and the added impact of COVID-19 on work and well-being. Our findings suggest that while there were similarities in the needed support services and workplace accommodations post-injury between men and women, differences existed in women needing help with daily activities for transition to work, with the need in help strongly entrenched in gendered roles; women exhibiting less change in employment status during the COVID-19 pandemic; and men displaying concern over job security and finances during the pandemic, with areas of concern related to their gendered identity and role expectations. These described differences highlight gender equity considerations that should be recognized by health care providers, employers, and persons with TBI during recovery and transition to community participation practices. Further, a high percentage of both men and women experienced concern in mental well-being, suggesting the need to address this concern in rehabilitation and in the community, including in the workplace post-TBI. As such, it is critical that researchers consider gender implications in community integration practices. Efforts must be made to pay attention to lived experiences of men and women with TBI during and after COVID-19, which should be formulated with the best of intentions to improve productivity and RTW and reduce inequalities between men and women with TBI.
Ethical approval
This study was reviewed and approved by the research ethics boards (REBs) of the TRI-UHN (REB # 20-5724) and the University of Toronto (REB #40439).
Informed consent
Informed consent was obtained from all research participants involved in this study.
Conflict of interest
The authors report no conflict of interest.
Acknowledgments
The authors would like to extend their appreciation to individuals who participated in this research study and shared their knowledge and challenges they’ve experienced. They would further like to acknowledge the land of which the University of Toronto operates on - the Huron-Wendat, the Seneca, and the Mississaugas of the Credit and of which the University Health Network operates on - the Huron-Wendat, the Haudenosaunee, and the Mississaugas of the Credit. Today, this place is still home to many Indigenous people from across Turtle Island and the authors are grateful to have the opportunity to work on this land.
Funding
This study was supported by a Canadian Institutes of Health Research and Social Sciences and Humanities Research Council (CIHR-SSHRC) Partnership Grant, ‘Healthy and Productive Work’, held by S. Lindsay (SSHRC—895-2018-4002; CIHR—01561-000) and a SSHRC Institutional Explore Grant (SIG 511431). Additional support was from a CIHR grant (#CGW-126580) and was supported in part by the Canada Research Chairs Program in Traumatic Brain Injury in Underserved Populations and Canada Research Chair in Neurological Disorders and Brain Health. Sara Hanafy is additionally supported by the Toronto Rehabilitation Institute Student Scholarship.
Supplementary Materials
[1] The supplementary files are available from https://dx.doi.org/10.3233/WOR-220437.
References
[1] | Saunders SL , Nedelec B . What work means to people with work disability: A Scoping Review. J Occup Rehabil. (2014) ;24: :100–10. https://doi.org/10.1007/s10926-013-9436-y. |
[2] | A demographic, employment and income profile of Canadians with disabilities aged 15 years and over, 2017. In: Statistics Canada. (2018) . https://www150.statcan.gc.ca/n1/pub/89-654-x/89-654-x2018002-eng.htm. Accessed 5 Jan 2022 |
[3] | Maas AIR , Menon DK , David Adelson PD , et al. Traumatic brain injury: Integrated approaches to improve prevention, clinical care, and research. Lancet Neurol. (2017) ;16: (12):987–048. https://doi.org/10.1016/S1474-4422(17)30371-X. |
[4] | About brain injury: Brain injury overview. In: Brain Injury Association of America. https://www.biausa.org/brain-injury/about-brain-injury/basics/overview. Accessed 5 Jan 2022. |
[5] | Little DM , Cook AJ , Morissette SB , et al. Considerations for return to work following traumatic brain injury. Handbook of Clinical Neurology. 1st ed Elsevier B.V.; (2015) , pp. 465–79. http://dx.doi.org/10.1016/B978-0-444-62627-1.00027-5 |
[6] | Towards a common language for functioning, disability and health: ICF. In: World Health Organization. 2002. http://www.who.int/classifications/icf/training/icfbeginnersguide.pdf. Accessed 22 Mar. |
[7] | Science is better with sex and gender. In: Canadian Institutes of Health Research. (2019) . https://cihr-irsc.gc.ca/e/51310.html Accessed 5 Jan 2022. |
[8] | Saltychev M , Eskola M , Tenovuo O , et al. Return to work after traumatic brain injury: Systematic review. Brain Inj. (2013) ;27: (13-14):1516–27. http://doi.org/10.3109/02699052.2013.831131. |
[9] | Renner C , Hummelsheim H , Kopczak A , et al. The influence of gender on the injury severity, course and outcome of traumatic brain injury. Brain Inj. (2012) ;26: (11):1360–71. https://doi.org/10.3109/02699052.2012.667592. |
[10] | Grauwmeijer E , Heijenbrok-Kal MH , Haitsma IK , et al. Employment outcome ten years after moderate to severe traumatic brain injury: A prospective cohort study. J Neurotrauma. (2017) ;34: (17):2575–81. https://doi.org/10.1089/neu.2016.4846. |
[11] | Scaratti C , Leonardi M , Sattin D , et al. Work-related difficulties in patients with traumatic brain injury: A systematic review on predictors and associated factors. Disabil Rehabil. (2017) ;39: (9):847–55. https://doi.org/10.3109/09638288.2016.1162854. |
[12] | Donker-Cools BHPM , Wind H , Frings-Dresen MHW . Prognostic factors of return to work after traumatic or non-traumatic acquired brain injury. Disabil Rehabil. (2016) ;38: (8):733–41. https://doi.org/10.3109/09638288.2015.1061608. |
[13] | Howe EI , Andelic N , Perrin PB , et al. Employment probability trajectories up to 10 years after moderate-to-severe traumatic brain injury. Front Neurol. (2018) :9: :1051. https://doi.org/10.3389/fneur.2018.01051. |
[14] | Corrigan JD , Lineberry LA , Komaroff E , et al. Employment after traumatic brain injury: Differences between men and women. Arch Phys Med Rehabil1. (2007) ;88: (11):1400–09. https://doi.org/10.1016/j.apmr.2007.08.006. |
[15] | O’Reilly K , Wilson N , Peters K . Narrative literature review: Health, activity and participation issues for women following traumatic brain injury. Disabil Rehabil. (2018) ;40: (19):2331–42. https://doi.org/10.1080/09638288.2017.1334838. |
[16] | Lindsay S , Cagliostro E , Albarico M , et al. A systematic review of the role of gender in securing and maintaining employment among youth and young adults with disabilities. J Occup Rehabil. (2018) ;28: :232–51. https://doi.org/10.1007/s10926-017-9726-x. |
[17] | Socías ME , Koehoorn M , Shoveller J . Gender inequalities in access to health care among adults living in British Columbia, Canada. Womens Health Issues. (2016) ;26: (1):74–9. http://doi.org/10.1016/j.whi.2015.08.001. |
[18] | Nalder E , Fleming J , Cornwell P , et al. Sentinel events during the transition from hospital to home: A longitudinal study of women with traumatic brain injury. Arch Phys Med Rehabil. (2016) ;97: :S46–53. https://doi.org/10.1016/j.apmr.2014.07.428. |
[19] | Stergiou-Kita M , Mansfield E , Sokoloff S , et al. Gender influences on return to work after mild traumatic brain injury. Arch Phys Med Rehabil. (2016) ;97: :S40–5. http://doi.org/10.1016/j.apmr.2015.04.008. |
[20] | Baldeo N , Souza AD , Haag HL , et al. A thematic analysis of patients’ and their informal caregivers’ gendered experiences in traumatic brain injury. Disabil Rehabil. (2022) ;0: :1–10. https://doi.org/10.1080/09638288.2022.2071483. |
[21] | D’Souza A , Fabricius A , Amodio V , et al. Men’s gendered experiences of rehabilitation and recovery following traumatic brain injury: A reflexive thematic analysis. Neuropsychol Rehabil. (2020) ;32: (3):337–58. https://doi.org/10.1080/09602011.2020.1822882. |
[22] | Colantonio A , Salehi S , Kristman V , et al. Return to work after work-related traumatic brain injury. NeuroRehabilitation. (2016) ;39: (3):389–99. https://doi.org/10.3233/NRE-161370. |
[23] | Matérne M , Lundqvist LO , Strandberg T . Opportunities and barriers for successful return to work after acquired brain injury: A patient perspective. Work. (2017) ;56: (1):125–34. https://doi.org/10.3233/WOR-162468. |
[24] | Libeson L , Downing M , Ross P , et al. The experience of return to work in individuals with traumatic brain injury (TBI): A qualitative study. Neuropsychol Rehabil. (2020) ;30: (3):412–29. https://doi.org/10.1080/09602011.2018.1470987. |
[25] | Gourdeau J , Fingold A , Colantonio A , et al. Workplace accommodations following work-related mild traumatic brain injury: What works? Disabil Rehabil. (2020) ;42: (4):552–61. https://doi.org/10.1080/09638288.2018.1503733. |
[26] | Stergiou-Kita M , Mansfield E , Colantonio A . Injured workers’ perspectives on how workplace accommodations are conceptualized and delivered following electrical injuries. J Occup Rehabil. (2014) ;24: (2):173–88. https://doi.org/10.1007/s10926-013-9463-8. |
[27] | Morrow EL , Patel NN , Duff MC . Disability and the COVID-19 pandemic: A survey of individuals with traumatic brain injury. Arch Phys Med Rehabil. (2021) ;102: (6):1075–83. https://doi.org/10.1016/j.apmr.2021.01.064. |
[28] | Kolakowsky-Hayner SA , Goldin Y . Sex and gender issues for individuals with acquired brain injury during COVID- A commentary. Arch Phys Med Rehabil. (2020) ;101: (12):2253–5. https://doi.org/10.1016/j.apmr.2020.08.004. |
[29] | Carli LL . Women, gender equality and COVID-19. Gend Manag. (2020) ;35: :647–55. https://doi.org/10.1108/GM-07-2020-0236. |
[30] | Quinn EK , Harper A , Rydz E , et al. Men and women at work in Canada, – Labour & Industry: A Journal of the Social and Economic Relations of Work.(2020) ;30: :401–12. https://doi.org/10.1080/10301763.2021.1872841. |
[31] | Goverover Y , Kim G , Chen MH , et al. The impact of the COVID-19 pandemic on engagement in activities of daily living in persons with acquired brain injury. Brain Inj. (2022) ;36: (2):183–90. https://doi.org/10.1080/02699052.2022.2043441. |
[32] | Kim GJ , Kim H , Fletcher J , et al. Differential impact of the COVID-19 pandemic on health care utilization disruption for community-dwelling individuals with and without acquired brain injury. Arch Rehabil Res Clin Transl. (2022) ;4: (1):100176. https://doi.org/10.1016/j.arrct.2021.100176. |
[33] | Screening for TBI using the OSU TBI-ID method. In: The Ohio State University, Wexner Medical Center. (2022) . https://wexnermedical.osu.edu/neurological-institute/departments-and-centers/research-centers/ohio-valley-center-for-brain-injury-prevention-and-rehabilitation/for-professionals/screening-for-tbi#::text=Contact&text=TheOhioStateUniversityTraumatic, TB. Accessed 22 Mar 2022. |
[34] | The Ohio State University Traumatic Brain Injury Identification method. In: The Ohio State University, Wexner Medical Center. (2022) https://wexnermedical.osu.edu/-/media/files/wexnermedical/patient-care/healthcare-services/neurological-institute/departments-and-centers/research-centers/ohio-valley/osu-tbi-id-researcher.pdf. Accessed 19 Jan 2022. |
[35] | Bogner J , Corrigan JD . Reliability and predictive validity of the Ohio State University TBI Identification method with prisoners. J Head Trauma Rehabil. (2009) ;24: (4):279–91. https://doi.org/10.1097/HTR.0b013e3181a66356. |
[36] | Corrigan JD , Bogner J . Initial reliability and validity of the Ohio State University TBI Identification method. J Head Trauma Rehabil. (2007) ;22: (6):318–29. https://doi.org/10.1097/01.HTR.0000300227.67748.77. |
[37] | von Steinbüchel N , Wilson L , Gibbons H , et al. Quality of Life after Brain Injury (QOLIBRI): Scale development and metric properties. J Neurotrauma. (2010) ;27: (7):1167–85. https://doi.org/10.1089/neu.2009.1076. |
[38] | von Steinbuechel N , Wilson L , Gibbons H , et al. QOLIBRI Overall Scale: A brief index of health-related quality of life after traumatic brain injury. J Neurol Neurosurg Psychiatry. (2012) ;83: (11):1041–7. http://doi.org/10.1136/jnnp-2012-302361. |
[39] | Canadian Survey on Disability (CSD). In: Statistics Canada. (2018) https://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&Id=321555#a2. Accessed 17 Jan 2022. |
[40] | Impacts of COVID-19 on Canadians: Data collection series. In: Statistics Canada. (2020) . https://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=5323. Accessed 17 Jan 2022. |
[41] | Impacts of the COVID-19 pandemic on postsecondary students (ICPPS). In: Statistics Canada. (2020) https://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=5320. Accessed 17 Jan 2022. |
[42] | Hill R . What sample size is “enough” in internet survey research? Academia ((2012) ;6: :1–10. |
[43] | Memon MA , Ting H , Cheah J-H , et al. Sample size for survey research: Review and recommendations. JASEM. (2020) ;4: (2):i–xx. https://doi.org/10.47263/JASEM.4(2)01. |
[44] | Bradshaw C , Atkinson S , Doody O . Employing a qualitative description approach in health care research. GQNR. (2017) ) http://doi.org/10.1177/2333393617742282. |
[45] | Hsieh H-F , Shannon SE . Three approaches to qualitative content analysis. Qual Health Res. (2005) ;15: (9):1277–88. https://doi.org/10.1177/1049732305276687. |
[46] | Mikolić A , van Klaveren D , Oude Groeniger J , et al. Differences between men and women in treatment and outcome after traumatic brain injury. J Neurotrauma. (2020) ;38: (2):235–51. https://doi.org/10.1089/neu.2020.7228. |
[47] | Coutu MF , Durand MJ , Coté D , et al. How does gender influence sustainable return to work following prolonged work disability? An interpretive description study. J Occup Rehabil. (2021) ;31: (3):552–69. https://doi.org/10.1007/s10926-020-09953-4. |
[48] | Haag HL , Caringal M , Sokoloff S , et al. Being a woman with acquired brain injury: Challenges and implications for practice. Arch Phys Med Rehabil. (2016) ;97: :S64–70. http://doi.org/10.1016/j.apmr.2014.12.018. |
[49] | Graff HJ , Christensen U , Poulsen I , et al. Patient perspectives on navigating the field of traumatic brain injury rehabilitation: A qualitative thematic analysis. Disabil Rehabil. (2018) ;40: (8):926–34. https://doi.org/10.1080/09638288.2017.1280542. |
[50] | Graff HJ , Deleu NW , Christiansen P , et al. Facilitators of and barriers to return to work after mild traumatic brain injury: A thematic analysis. Neuropsychol Rehabil. (2021) ;31: (9):1349–1373. https://doi.org/10.1080/09602011.2020.1778489. |
[51] | Soeker MS , Ganie Z . The experiences and perceptions of employers and caregivers of individuals with mild-moderate traumatic brain injury in returning to work. Work. (2019) ;64: (2):355–70. https://doi.org10.3233/WOR-192997. |
[52] | Poritz JMP , Vos L , Ngan E , et al. Gender differences in employment and economic quality of life following traumatic brain injury. Rehabil Psychol. (2019) ;64: (1):65–71. http://doi.apa.org/getdoi.cfm?doi=10.1037/rep0000234. |
[53] | Hosomi S , Kitamura T , Sobue T , et al. Sex and age differences in isolated traumatic brain injury: A retrospective observational study. BMC Neurol. (2021) ;21: (1):261 https://doi.org/10.1186/s12883-021-02305-6. |
[54] | Paniccia A , Colquhoun H , Kirsh B , et al. Youth and young adults with acquired brain injury transition towards work-related roles: A qualitative study. Disabil Rehabil. (2019) ;41: (11):1331–42. https://doi.org/10.1080/09638288.2018.1425743. |
[55] | Tomas V , Ahmed H , Lindsay S . Unravelling the complexities of workplace disclosure among persons with non-visible disabilities and illnesses: A qualitative meta-ethnography. J Occup Rehabil. (2022) https://doi.org/10.1007/s10926-022-10023-0. |
[56] | Lindsay S , Cagliostro E , Leck J , et al. Disability disclosure and workplace accommodations among youth with disabilities. Disabil Rehabil. (2019) ;41: (16):1914–24. https://doi.org/10.1080/09638288.2018.1451926. |
[57] | Stergiou-Kita M , Grigorovich A , Damianakis T , et al. The big sell: Managing stigma and workplace discrimination following moderate to severe brain injury. Work. (2017) ;57: (2):245–58. https://doi.org/10.3233/WOR-172556. |
[58] | Alon T , Doepke M , Olmstead-Rumsey J , et al. The impact of COVID-19 on gender equality. NBER Working Paper Series. Cambridge; (2020) . |
[59] | Umucu E . Functional limitations and worrying to lose employment among individuals with chronic conditions and disabilities during COVID- A hierarchical logistic regression model. J Vocat Rehabil. (2021) ;54: :25–32. https://doi.org/10.3233/JVR-201114. |
[60] | Jones AM , Koehoorn M , Bültmann U , et al. Impact of anxiety and depression disorders on sustained return to work after work-related musculoskeletal strain or sprain: A gender-stratified cohort study. Scand J Work Environ Health. (2021) ;47: (4):296–305. https://doi.org/10.5271/sjweh.3951.. |




