The grief of loss among breast cancer patients during the COVID-19 pandemic: How can palliative care workers help?
Abstract
BACKGROUND:
Cancer patients suffer from different losses. Studies have focused on examining grief resulting from cancer diagnosis and grief among caregivers of cancer patients and parents who lost their child to cancer. However, there are no studies on the grief resulting from losing a loved one in cancer patients.
OBJECTIVE:
This study examined female breast cancer patients’ grief and aimed to reveal how palliative care can help breast cancer who experience the grief of losing a loved one.
METHODS:
The study applied the qualitative case study design conducted with 10 women with breast cancer; their ages ranged from 47 to 54 years. Data were collected during 18 in-depth interviews by asking semi-open-closed questions.
RESULTS:
Thematic analysis found that losing a partner negatively affected breast cancer patients’ mental health. The grief experience among breast cancer patients has many symptoms: sadness, severe anxiety, sleep disturbance, loneliness, and isolation. Results also indicated many risk factors that increase grief symptoms among breast cancer patients, such as quarantine procedures during the COVID-19 outbreak, extreme emotional attachment to a partner, guilt, self-blame, and social relations. Patients with breast cancer can face grief experienced by coping strategies such as: resorting to God, prayer, patience, and reading the Holy Qur’an. The results also emphasize the importance of integrating palliative care with treatment for breast cancer patients who experience the grief of loss.
CONCLUSION:
The grief of loss among breast cancer patients is a complex experience. These findings have many applied aspects that benefit planning counseling and psychological programs to increase positive coping strategies for those patients with breast cancer suffering from grief of loss disorder and provide psychological services that protect them from risk factors and reduce grief symptoms which reduce the effectiveness of cancer treatments due to the symptoms of traumatic loss of a partner. These findings also emphasize the importance of palliative care for cancer patients with complex distress.
1Introduction and theoretical background
1.1Breast cancer in the Kingdom of Saudi Arabia
The total number of cancer cases in the Kingdom, according to the latest statistics of the Saudi Cancer Registry in 2016, reached 16,859, of which 13,161 were among Saudis, with percentage of 78.1%, of which the males accounted for 44.1%, while the females accounted for 55.9% of them. Breast cancer ranked first 2282 cases, at 17.3% of both females and males and 30.4% of all cancers in women. Then came colorectal cancer, and thyroid cancer, with an infection rate of 27.2 per 1,000 Saudi women [1]. Many studies have shown that physiological and psychological changes happen when cancer patients are directed to chemotherapy or radiotherapy, which affects their mental health [2]. Breast cancer is one of the most common tumors that cause high mortality [3].
A high level of emotional distress was found among patients with cancer [4]. Emotional distress alters the body’s immune function and affects the growth of tumors and malignancies and the survival of cancer patients [5]. There was an increase in female breast cancer incidence after their only children’s death [6]. The results of previous studies [7, 8] found that the partner’s death decreased cellular immunity. Also, previous studies found a relationship between cancer incidence and previous emotional traumatic events, such as the death of a loved one [9], and a relationship between chronic mourning and the incidence of cancerous tumors [10].
1.2COVID-19 and breast cancer
The quarantine procedures during the COVID-19 outbreak have affected human well-being, relationship satisfaction, and economic impact; thus, COVID-19 is considered a significant public health challenge [11]. In the same context, results [12] showed high anxiety, depression, distress, and insomnia rates among breast cancer patients during the COVID-19 pandemic. Also, [13] found that COVID-19-related anxiety can influence decision-making about treatments in cancer patients. Also, [14] showed that social distancing measures, prioritizing health services for COVID-19 patients, and postponing appointments for cancer patients’ reviews led to increased distress levels (59.50%) among cancer patients. Researchers [15] found that the spread of COVID-19 led to a rise in anxiety among cancer patients, especially breast cancer, and anxiety was higher among females than males.
From the above, cancer patients, especially breast cancer patients, suffer from many stresses, which increased during the outbreak of the COVID-19 pandemic and negatively affected the breast cancer patient’s health outcomes and their responses to chemotherapy and other treatments. In this context, [2] found that breast cancer patients were exposed to chronic stresses that caused many psychological adverse health outcomes.
1.3Definition of grief
Regarding grief response, there are many definitions of grief. Grief is related to a family member’s death [16]. Also, [17] defined grief as the loss of something, often associated with a family member’s death. The grief of loss refers to the expressing psychological suffering and high psychological stress that explains the loss of something huge or the separation of a dear person, either by travel or death. Grief may result from the emergence of chronic disease, breaking up a relationship, missing an opportunity or promotion, or any other challenging event in life. These feelings of grief may disrupt social life and affect physical and psychological health.
1.4Grief stages
Individuals may undergo five grief response stages: denial, anger, compromise, depression, and acceptance [17–19]. According to the grief cycle model [15], an individual shows grief response in five stages, as follows:
1. Denial: In the beginning, participants denied what happened and found it impossible to believe the loss of a loved one to them.
2. Anger: When participants start to identify and verify the situation’s truth, the second stage comes, which is the feeling of anger.
3. Bargaining or trying to negotiate: It is not uncommon for survivors who suffer from loss to overcome their suffering by negotiating. Hence, they think the departure of loved ones is more merciful than continuing in life and suffering from illness or a permanent disability.
4. Depression: During all the previous stages, before and after it, they felt great grief, which they feels is a natural thing, and you have to know that it will not last forever, and the feeling that life has stopped and that it will never return to its way before the departure of loved ones, or that she is never able to get through is a familiar feeling also among most - or more - of those who experience this pain.
5. Acceptance: It is the last stage of grief response; at this stage, participants become psychologically qualified to accept what happened and come to terms that enable them to deal with the loss and move forward in their life, and this does not mean that the previous stages have ended, they only calmed down, but they will demand their head from time to time. But then the pain of their loss will become more manageable and subject to more control than initially.
There are differences in the grief stages according to personality type, circumstances surrounding the individual, gender, age, education level, marital status, and other factors that determine the individual’s response to the experience of loss and how to express his grief feelings. The individual’s grief feelings continue for a period, ranging from several weeks and months to several years, and the recovery from grief feelings gradually decreases [15, 20, 21]. Although each person has a particular way of dealing with grief, it passes through specific stages consistent for many people. Researchers [5, 16, 21, 22] have studied the stages we go through in grief, considering the different trauma, circumstances, and people.
1.5Grief among breast cancer patients
Cancer patients experience grief after their diagnosis as a response to threats of losing their ability to work independently, loss of identity, changes in role definition in and outside their family, and fear of death; all of these can lead to increased cancer patients’ conflict and dysfunction; thus, they need support to be able to cope with these feelings of grief and threats [23, 24].
By reviewing the literature about the grief of patients with cancer, the researcher noted a lack of interest in examining the grief resulting from a cancer patient’s loss of important people in their lives (husband, mother, father, and others). A growing number of studies focused on examining grief resulting from cancer, including breast cancer, and studying grief among caregivers of cancer patients and parents who lost their child to cancer [3, 5, 25]. Many quantitative studies have indicated that grief of loss is a complex response that lasts long periods and profoundly affects a person’s physical and psychological well-being [19, 26–30]. Also, grief is associated with depression, suicide attempts, high blood pressure, heart disease, and drug abuse [22, 29, 31, 32]. Previous studies have also indicated that the grief of loss has multiple complex symptoms and reactions that differ from normal grief. Also, studies [9, 18, 27, 33] revealed that grief of loss differs from anxiety and mood disorders.
1.6Palliative care for breast cancer patients
Breast cancer causes many physical manifestations that negatively affect the quality of life and well-being, which increases the need for care that helps them to relieve psychological stress and the deterioration in the quality of their life by providing support to them and their families [15, 24, 34]. Introducing palliative care services for cancer patients from caregivers leads to a tangible improvement in symptom management, quality of life, and treatment planning, especially if this is done early and combined with medical treatment for cancer patients [35]. Thus, palliative care for cancer patients is concerned with relieving the pain and stress caused by cancer and improving the quality of life of patients and their families, along with drug therapy [24, 34–39].
To ensure effective palliative care for breast cancer patients, it is necessary to evaluate and understand the limitations of palliative care workers in terms of knowledge, experience, availability of home care, difficulties in coping with the situation, and effective planning and ongoing care [24].
2Objective of the current study
This study seeks to investigate the impact of grief on breast cancer patient’s mental health, risk factors, and coping strategies to increase the scientific knowledge about the grief of loss among breast cancer patients. The current study tries to answer the following questions:
1. How did grief impact female breast cancer patients’ mental health after losing a partner?
2. What risk factors increase grief symptoms among female breast cancer patients after losing a partner?
3. What strategies do females with breast cancer use to cope with stress relating to experiencing grief?
4. How do palliative care workers help breast cancer patients who experience the grief of loss?
3Materials and methods
3.1Recruitment, sample, and ethical approval
The qualitative study design allows exploration and understanding of an individual’s meaning to a personal or human problem [40]. Thus, the current study applied a qualitative case study design to discover the experiences and meanings of grief loss using the participants’ styles and words, allowing for an in-depth understanding and interpretation of the complex phenomenon of grief loss. The case study design allows an individual to describe his personal experience from his point of view [41].
The researcher chose a purposive sample consisting of 10 surviving women with breast cancer; their ages ranged from 47 to 54 years, and most of them were married and from different educational classes (Table 1) after the researcher obtained verbal consent from them to be a participant in the current study.
Table 1
The demographic characteristics of the participants
| Participants | Age | Educational class | Economic backgrounds | Social structure | Relationships with the dyed one | Coping strategies |
| Participant 1 | 52 | Postgraduate | High-level | Widow | Husband | Resorting to God, prayer |
| Participant 2 | 49 | Graduate | Mid-level | Single | Father | Charity, expressing feelings of grief |
| Participant 3 | 50 | Graduate | Mid-level | Widow | Husband | Supplication, patience |
| Participant 4 | 47 | Graduate | High-level | Single | Mother | Engaged with family and avoided sitting alone |
| Participant 5 | 54 | Postgraduate | High-level | Married | Father | Talking with trusted people and acceptance of feelings and behavior |
| Participant 6 | 51 | Graduate | Mid-level | Widow | Husband | Read the Qur’an, pray, and supplication |
| Participant 7 | 48 | Graduate | High-level | Married | Mother | Accept negative and positive feelings of grief, living with feelings take care of yourself and family |
| Participant 8 | 50 | Graduate | High-level | Married | Mother | Activities to rest, healthy meals, and getting good enough sleep |
| Participant 9 | 46 | Graduate | Mid-level | Married | Father | Writing poetry and story, listening to music, and going out to gardens and green places |
| Participant 10 | 49 | Graduate | Mid-level | Widow | Husband | Meditation exercises and spiritual alertness |
3.2Data collection
Data were collected during 18 in-depth interviews. Due to the COVID-19 pandemic and the inability to meet with the participants in-person, the one-hour discussions were pre-scheduled. All participants were conducted remotely via the Zoom program in audio-only to protect confidentiality. Data were collected using a semi-structured interview to gain insight and explore ideas and perspectives [40–43] via the Zoom program semi open-closed questions were asked. The semi-structured interviews allowed data collection about the thoughts, feelings, and behaviors of the case participating in the study and how the study sample perceived the experience of the grief of loss. The researcher recorded observations, personal thoughts, biases, and compatible ideas during the interviews, affecting the data’s subjectivity. All discussions were digitally recorded with the participant’s approval to allow the data to be reproduced and analyzed qualitatively.
3.3Data analysis
All discussion sessions were transcribed, coded, and analyzed using the thematic analysis method to identify patterns and themes in the collected data. The analysis of thematics included six stages: reading the data to get familiar with it, generating initial symbols in the data, searching for themes in the data, reviewing themes, identifying and naming the themes, then writing the study report [44]. Qualitative analysis and data report using MAXQDA software (version 2020) was used to code themes and validate the application of the codes. Emergent themes were classified, organized into overarching domains, and assembled with representative quotations. Discrepancies were resolved through discussion in constant comparison until inter-rater reliability was reached.
3.4Legitimation and trustworthiness
Researchers can follow seven approaches to address challenges of validity and reliability in qualitative studies [40]. Thus, the researcher used several techniques to increase the legitimation and trustworthiness of the study procedures and the findings of the study: the collection of rich and intensive data for an extended period through in-depth semi-structured interviews, triangulation, and obtaining feedback from the breast cancer patients participating in the study to reduce misinterpretation of their behavior and opinions, looking for contradictory evidence, continuous comparison to compare results across different settings or events explicitly.
4Results
This study used semi-structured in-depth interviews with participants. The data coding process resulted in 38 themes, crystallizing into three axial codings: symptoms of loss, grief, risk factors, and coping with the grief experience (Table 2 and Fig. 1).
Fig. 1
Code-subcodes-segments model for breast cancer grief patients, MAXQDA.
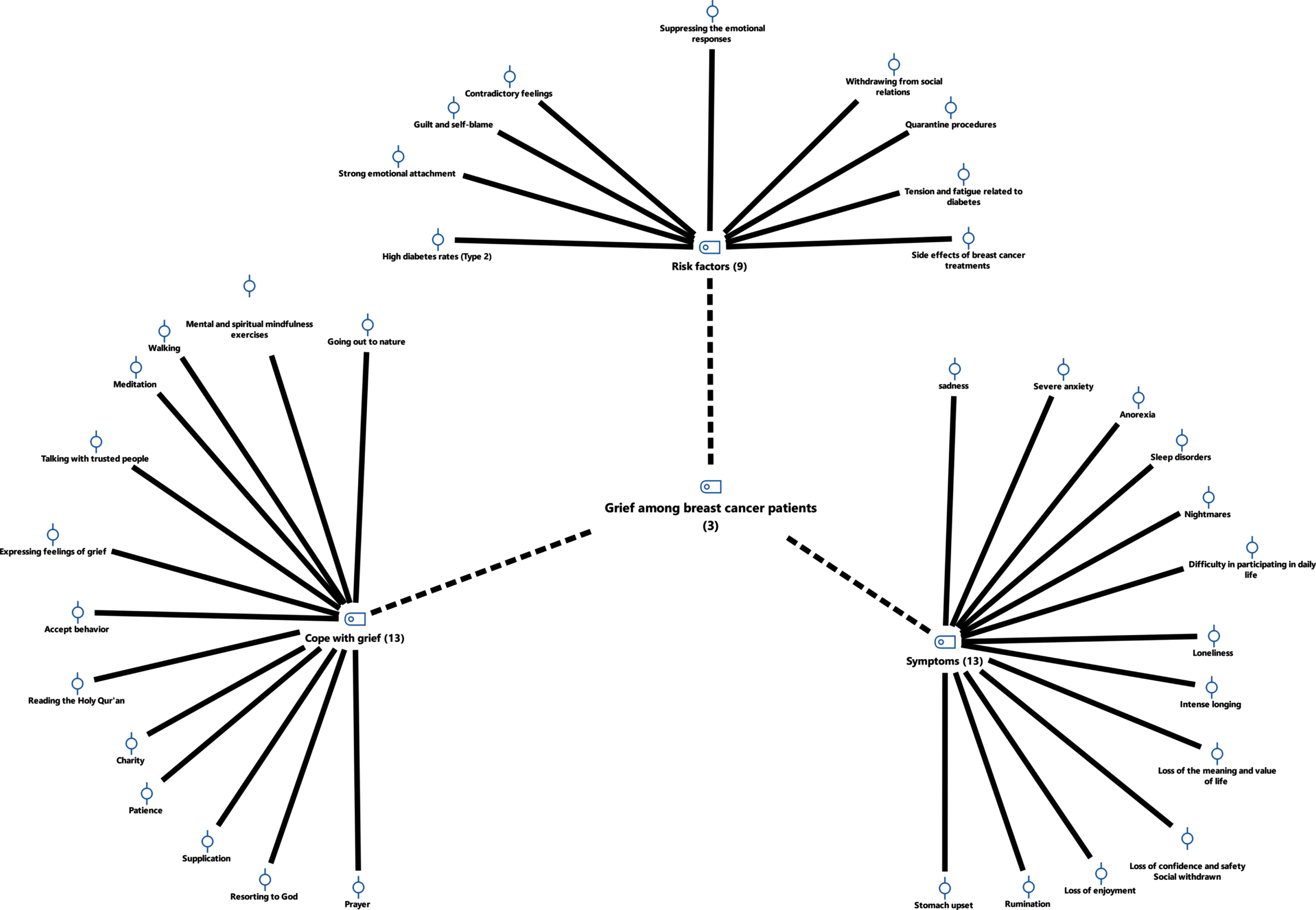
Table 2
Thematic categories and coded themes according to the results of the MAXQDA (2020) software
| Categories | Coded themes |
| Grief symptoms | Sadness |
| Severe anxiety | |
| Anorexia | |
| Nightmares | |
| Loneliness | |
| Sleep disorders | |
| Intense longing | |
| Difficulty in participating in daily life | |
| Loss of enjoyment | |
| Loss of confidence and safety | |
| Social withdrawn | |
| Loss of the meaning and value of life | |
| Rumination | |
| Stomach upset | |
| High diabetes rates (Type 2) | |
| Risk factors | Strong emotional attachment |
| Guilt and self-blame | |
| Contradictory feelings | |
| Suppressing the emotional responses | |
| Withdrawing from social relations | |
| Quarantine procedures | |
| Tension and fatigue related to diabetes | |
| Side effects of breast cancer treatments. | |
| Cope with grief | Resorting to God |
| Prayer | |
| Supplication | |
| Patience | |
| Charity reading the Holy Qur’an | |
| Expressing feelings of grief | |
| Accept behavior | |
| Talking with trusted people | |
| Mental and spiritual mindfulness exercises | |
| Going out to nature | |
| Meditation | |
| Walking |
The results of the thematic analysis of the data collected from the participants of the current study shown in Table 2 found that:
4.1 Breast cancer patients suffer from symptoms of extreme grief, severe anxiety, bouts of intense crying, sleep disturbances, nightmares, loneliness and isolation, difficulty participating in daily activities, loss of enjoyment of life, loss of confidence and safety in others, social withdrawal, rumination, stomach upset, high diabetes.
4.2 Many risk factors increase the female breast cancer patient’s feelings of grief after losing an important person: a strong emotional attachment, guilt, self-blame, contradictory feelings, suppressing emotional responses, withdrawal from social relations, quarantine procedures during COVID-19 outbreak, fatigue related to diabetes, and the side effects of breast cancer treatments.
4.3 The participants of this study used many coping strategies to face the grief of loss: resorting to God, prayer, supplication, patience, charity, reading the Holy Qur’an, expressing feelings of grief, accepting the behavior, talking with trusted people, mental and spiritual mindfulness exercises, going out to nature, meditation, and walking.
4.4 The participants reported that palliative care services are vital to breast cancer patients that help them relieve the symptoms of grief, get rid of the feelings of despair, teach them how to accept the loss of a loved one, and help them cope with life stresses.
5Discussion
Thematic analysis results revealed that the participants suffered from symptoms of extreme grief. Participant 1 said that: “during the past weeks, after the death of my husband and the loss of the only person who was my bond, my health deteriorated very much, and that’s why I decided to go to a psychiatrist to help me reduce the feeling of anxiety, sleeping difficulties and stomach upset, and to tell me a healthy lifestyle that gives hope in my life and to live in confidence and peace with others”. Participant 2 said that: “after losing my father, I suffered from imbalance and loss of identity, loss of the meaning and value of life, loss of support, and the desire to die.”
Psychological trauma is a painful psychological state the individual enters as a result of exposure to a physically and psychologically traumatic event that causes grief and pain and leads to the individual entering a state of severe grief; it may last for several weeks, months, or years [20, 28, 45]. Psychological trauma often occurs in several stages; the first stage begins with denial and loss of control and may reach a loss of consciousness as a hysterical state that self-psychological mechanisms cannot address, and then the second stage is maladaptation. Then, the individual begins to respond and returns to his everyday life. Still, abnormally, as it may appear, he has some symptoms, such as a tendency to isolation, anorexia, sleep disturbance, insomnia, and decreased productivity to reach the third stage: the post-traumatic stage. In that situation, the individual tries to appear normal, and those around him may see that he has recovered from them. Still, the individual suffers internally and feels symptoms similar to depression, prompting the individual to psychotherapy and visit a psychiatric clinic [17, 19, 21].
The feelings and thoughts of individuals in a state of grief are divided into two types [10, 46, 47]:
1. Instrumental grieving: The grieving person focuses on solving problems, controls his thinking, controls his feelings, and tries to reduce them.
2. Intuitive grief: Focuses on an increasingly emotional experience, focuses on sharing emotions, exploring a lost relationship, and thinking about mortality.
There are diagnostic criteria for grief [15]:
1. Grief response persists after the trauma of the loss for at least six months.
2. Exposure to severe trauma to the loss of a loved one.
3. Cognitive impairment is accompanied by non-consensual emotions and behaviors related to the experience of loss for at least a month.
4. Ruminating about the trauma of loss.
5. Avoidant behavior.
6. Physical complaint.
Participants reported that the loss events are followed by disturbed sleep, loss of sense of reality, depression, anger, and severe maladaptive actions. Therefore, the results indicated that a loss experience is considered a traumatic event for patients with breast cancer. These findings are consistent with the results of previous studies such as [5–8, 10].
The results also showed that all participants reported that a strong emotional attachment with a loved one increased their feelings of grief after losing him. Participant (3) said: “she did not imagine that her husband could die and leave her alone one day, that is why, after he died; I felt self-blame.” Participant (4) said: “Gradually, I withdrew from social situations, cut off communication with my family and friends, and preferred to sit alone; I became exhausted and developed sleep disturbances. My mother was the only source of support for me, especially after my father’s death; I am now alone”.
Previous studies showed that the COVID-19 outbreak and its precautionary measures are among the stressors for cancer patients [12, 14, 48].
Participant (3) said: “What increased my suffering after my husband died during the COVID-19 pandemic is the difficulty of obtaining health services and delaying my appointments due to paying attention to COVID-19 patients, and also my fear of leaving the house because I am one of the groups most vulnerable to transmission of infection, all of these created pressures that led to an increase in my rate of diabetes, and increased my feelings of tension and distress”.
Studies found a high cancer incidence among females after losing their children [6] and a relationship between cancer incidence and losing a loved one [23]. Also, the theoretical literature referred that emotional distress changes immune function [5].
Regarding the coping strategies, the results showed that all participants reported the grief experience needs a gradual time until the individual reaches recovery. They used many strategies to overcome this grief. Participant (6) said: “I tried to overcome my grief experience after my husband died with multiple strategies; for example, I read the Qur’an, prayed and supplication.” Participant (4) also said: “I engaged with my family members and avoided sitting alone because loneliness increased my rumination in thinking about him and disrupted my recovery.” Participant (7) added said: “I accepted my negative and positive feelings of grief, such as anger, tension, and exhaustion; I lived with these feelings as normal; my psychiatrist helped me deal with my negative feelings and return them to their correct path, I also took care of myself and my family.” As well as the participant (8) said that: “I set a varied schedule of activities to rest, healthy meals, and get good enough sleep”. Also, Participant (9) said: “I took an interest in writing poetry and story, listening to music, and going out to gardens and green places.” Participant (10) said: “I kept doing meditation exercises and spiritual alertness with my psychiatrist’s help to overcome thinking about feelings of grief and loss”.
Mental health correlated with religiosity and psychological resilience among female breast cancer patients [2]. These findings indicated that it is challenging for a person to overcome the loss of a loved person; it is necessary to overcome this traumatic event to understand what is happening [22, 45, 46, 49, 50]. Dealing with grief and the pain of loss is not manageable; thus, we need several elements and factors to help a person overcome adversity, grief, and pain in the fastest and best possible way [15, 17, 21, 51]. Also, religiosity provides guidelines to help patients devise a course for their lives and cope with life stresses [16, 52, 53].
The results of the current study found that the participants stressed the importance of palliative care to relieve the symptoms of grief of loss. “Participant 2 added, “Cancer patients and their families need urgently psychological help to relieve them of the increasing stress due to the increasing costs of treatment and the fears resulting from cancer. Cancer treatment is not only medicine but also needs the support of institutions, friends, and specialists.” Participant 4 indicated that “after losing my mother, my life changed completely, as she was the only source of care and attention. With her loss, I lost the meaning of life. Cancer is a cursed disease, not only a physical problem but a psychological one that needs professional help provided by qualified people we trust in them who help us overcome the difficulties of life after breast cancer and accept the events and the negativity we are going through; and how we can face and live with it.” Also, Participant 9 said, “I need a specialist to help me get rid of the feelings of despair that dominate me after my husband’s death and teach me how to accept his loss”.
From these findings about the role of palliative care for breast cancer patients, the role of workers concluded in providing palliative care to breast cancer patients who suffer from the grief of loss, as follows:
1. Improving communication and social skills.
2. Psychological and spiritual care.
3. Develop psychological resilience.
4. Help them plan for the future with an optimistic outlook on life.
5. Control of the pathological symptoms resulting from the grief of loss.
6. Helping them return to daily life and integrate into social activities.
7. Lifestyle improvement.
8. Teaching families methods of dealing with stress effectively.
9. Education and psychological education.
10. Reducing anxiety about body image and quality of marital life.
11. Providing psychological support to patients and their families.
6Conclusions
This qualitative study adds further evidence to the literature concerning grief of loss in general and grief in breast cancer patients. Results revealed that losing a loved one negatively affected breast cancer patients’ mental health. The grief experience among breast cancer patients has many symptoms, such as sadness, severe anxiety, crying, sleep disturbance, loneliness, isolation, intense longing, difficulty in participating in daily life, loss of enjoyment, loss of confidence and safety, social withdrawal, loss of meaning and value of life, rumination, stomach upset, higher diabetes rates. Results also indicated many risk factors that increase grief symptoms among breast cancer patients, such as quarantine procedures during the COVID-19 pandemic, emotional attachment with a loved one, guilt, self-blame, suppressing emotional responses, withdrawal from social relations, tension, fatigue related to diabetes, and the side effects of cancer treatments. Patients with breast cancer can face grief experienced by many coping strategies such as: resorting to God, prayer, supplication, patience, charity, reading the Holy Qur’an, expressing feelings of grief, accepting the behavior, talking with trusting people, and mental and spiritual mindfulness exercises, meditation, walking. A depth understanding and assessment of grief loss feelings could inform mental health professionals to help grief individuals, especially breast cancer patients, plan counseling and psychotherapy interventions to promote their mental health.
The results of the current study emphasized the importance of integrating palliative care with pharmacological treatment for breast cancer patients who experience the grief of loss and training caregivers on their role in relieving stress and psychological symptoms for patients and their families.
7Limitations and future directions
Findings from the current study may not be necessarily generalizable to female breast cancer patients with grief or loss experience. In this study, several limitations include self-reporting the data that fits the case study design and examining (10) survivors of the female with breast cancer grief experience and how they dealt with it. The second limitation is selecting the participants in this study, where the selection was made purposeful, and this method fits the qualitative design. The third limitation represents the researcher’s potential bias. The restrictions imposed on generalizing the study results also represent the fourth limitation. Case study design aims to understand the situation, emotional experience, and meaning. Therefore, the case study results can’t be generalized to other cases of patients with cancer. That is why we invite researchers to conduct future studies on other cases and use qualitative research designs such as grounded theory or narrative design among people with chronic diseases and different types of cancer. We also need to conduct a mixed study to reveal the effectiveness of counseling interventions to reduce mental health problems resulting from the experience of grief resulting from losing a partner among cancer patients, as well as the effectiveness of palliative care to alleviate the grief of cancer patients, especially after the loss of a loved one who was the only source of support to them.
8Implications for practice
This study confirms the urgent need for prevention methods to improve the coping strategies among breast cancer patients with grief loss experience. These findings have many applied aspects that benefit planning counseling and psychological programs to increase positive coping strategies for those patients with breast cancer suffering from grief of loss disorder and provide psychological services that protect them from risk factors and reduce grief symptoms which reduce the effectiveness of cancer treatments due to the symptoms of traumatic loss of a partner. These findings also emphasize the importance of palliative care for cancer patients with complex distress.
Ethics statement
All methods were carried out in accordance with relevant guidelines and regulations.
Informed consent
Informed consent was obtained from all subjects.
Conflict of interest
The authors report no conflicts of interest.
Acknowledgments
The authors would like to express their gratitude to King Khalid University, Saudi Arabia, for providing administrative and technical support.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
References
[1] | Saudi Ministry of Health (MOH). Breast cancer. 2020 https://www.moh.gov.sa/en/HealthAwareness/EducationalContent/wh/Breast-Cancer/Pages/default.aspx (accessed online May 2021). |
[2] | Al Eid N , Alqahtani M , Marwa K , et al. Religiosity, Psychological Resilience, and Mental Health Among Breast Cancer Patients in Kingdom of Saudi Arabia. Breast Cancer: Basic and Clinical Research. (2020) ;14: :1–13. |
[3] | Paula NC , Martins JA , Amaral LM , et al. Breast cancer: Is grief a risk factor? Rev Assoc Med Bras. (2018) ;64: (7):595–600. |
[4] | Kubler-Ross E. On Death and Dying. (1969) . Macmillan, New York NY. |
[5] | Li J , Johansen C , Olsen J . Cancer survival in parents who lost a child: a nationwide study in Denmark. Br J Cancer. (2003) ;88: (11):1698–701. |
[6] | Lambe M , Cerrato R , Askling J , et al. Maternal breast cancer risk after the death of a child. Int J Cancer. (2004) ;110: (5):763–6. |
[7] | Bartrop RW , Lazarus L , Luckhurst E , et al. Depressed lymphocyte function after bereavement. Lancet. (1977) ;309: (8016):834–6. |
[8] | Nakaya N. Effect of psychosocial factors on cancer risk and survival. J Epidemiol. (2004) ;24: (1):1–6. |
[9] | Boelen PA , DJ van . Complicated grief and uncomplicated grief are distinguishable constructs. Psychiatry Research. (2008) ;157: (1–3):311–4. |
[10] | Wakefield JC. DSM-5 grief scorecard: Assessment and outcomes of proposals to pathologize grief. World Psychiatry. (2013) . |
[11] | Alqahtani MM , Arnout B , Fadhel F , Sufyan N . Risk perceptions of COVID-19 and its impact on precautionary behavior: A qualitative study. Patient education and counseling. (2021) . https://europepmc.org/article/pmc/pmc7882911 |
[12] | Juanjuan L , Santa-Maria CA , Hongfang F , et al. Patient-reported Outcomes of Patients with Breast Cancer During the COVID-19 Outbreak in the Epicenter of China: A Cross-sectional Survey Study. Clin Breast Cancer. (2020) ;20: (5):e651–e662. |
[13] | Vanni G , Materazzo M , Pellicciaro M , et al. Breast Cancer and COVID- The Effect of Fear on Patients’ Decision-making Process. Vivo. (2020) ;34: (3 Suppl):1651–9. |
[14] | Mendonça AB , Pereira ER , Magnago C , et al. Distress and Spiritual Well-Being in Brazilian Patients Initiating Chemotherapy during the COVID-19 Pandemic-A Cross-Sectional Study. Int J Environ Res Public Health. (2021) ;18: (24):13200. |
[15] | Shear MK , Simon N , Wall M , et al. Complicated grief and related bereavement issues for DSM-5. Depression and Anxiety. (2011) ;28: (2):103–17. |
[16] | Behere PB , Das A , Yadav R , et al. Religion and mental health. Indian J Psychiatry. (2013) ;55: :187–94. |
[17] | Parkes CM. Bereavement. Studies of grief in adult life 3rd (Ed). Penguin publishers. (1998) . |
[18] | Dillen L , Fontaine JR , Verhofstadt-Denève L . Are normal and complicated grief different constructs? A confirmatory factor analytic test. Clinical Psychology & Psychotherapy. (2008) ;15: (6):386–95. |
[19] | Shear MK , Frank EPR , Houck CF , et al. Treatment of complicated grief. JAMA: the journal of the American Medical Association. (2005) ;293: (21):2601–8. |
[20] | Middleton W , Burnett P , Raphael B , et al. The bereavement response: a cluster analysis. The British Journal of Psychiatry. (1996) ;169: (2):167–71. |
[21] | Raphael B , Minkov C . Abnormal grief. Current Opinion in Psychiatry. (1999) ;12: (1):99. |
[22] | Boelen PA , Prigerson H . The influence of symptoms of prolonged grief disorder, depression, and anxiety on quality of life among bereaved adults. European Archives of Psychiatry and Clinical Neuroscience. (2007) ;257: (8):444–52. |
[23] | Boelen PA , J de Keijser MA , van den Hout , et al. treatment of complicated grief: A comparison between cognitive-behavioral therapy and supportive counseling. Journal of Consulting and Clinical Psychology. (2007) ;75: (2):277. |
[24] | Cherny NI , Paluch-Shimon S , Berner-Wygoda Y . Palliative care: needs of advanced breast cancer patients. Breast Cancer (Dove Med Press). (2018) ;10: :231–43. |
[25] | Pakseresht M , Rassouli M , Rejeh N , et al. Explore the bereavement needs of families of children with cancer from the perspective of health caregivers: A qualitative study. Front Psychol. (2021) ;12: :1–9. |
[26] | de Groot MH , de Keijser J , Neeleman J . Grief Shortly After Suicide And Natural Death: A Comparative Study Among Spouses and First-Degree Relatives. Suicide and Life-Threatening Behavior. (2006) ;36: (4):418–31. |
[27] | Lichtenthal WG , Cruess DG , Prigerson HG . A case for establishing complicated grief as a distinct mental disorder in DSM-V. Clinical Psychology Review. (2004) ;24: (6):637–62. |
[28] | Miyabayashi S , Yasuda J . Effects of loss from suicide, accidents, acute illness and chronic illness on bereaved spouses and parents in Japan: Their general health, depressive mood, and grief reaction. Psychiatry and Clinical Neurosciences. (2007) ;61: (5):502–8. |
[29] | Stroebe H , Stroebe W . Health outcomes of bereavement. The Lancet. (2007) ;370(9603):1960–73. |
[30] | Zhang B , El-Jawahri A , Prigerson HG . Update on Bereavement Research: Evidence-Based Guidelines for the Diagnosis and Treatment of Complicated Bereavement. Journal of Palliative Medicine. (2006) ;9: (5):1188–203. |
[31] | Agerbom E. Midlife suicide risk, partner’s psychiatric illness, spouse and child bereavement by suicide or other modes of death: a gender-specific study. Journal of Epidemiology and Community Health. (2005) ;59: (5):407–12. |
[32] | Latham AE , Prigerson HG . Suicidality and Bereavement: Complicated Grief as Psychiatric Disorder Presenting Greatest Risk for Suicidality. Suicide and Life-Threatening Behavior. (2004) ;34: (4):350–62. |
[33] | Horowitz MJ , Bonanno GA , Holen A . Pathological grief: diagnosis and explanation. Psychosomatic Medicine. (1993) ;55: (3):260–73. |
[34] | Bakitas M , Lyons KD , Hegel MT , et al. Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: the Project ENABLE II randomized controlled trial. JAMA. (2009) ;302: (7):741–9. |
[35] | Greer JA , Jackson VA , Meier DE , Temel JS . Early integration of palliative care services with standard oncology care for patients with advanced cancer. CA Cancer J Clin. (2013) ;63: (5):349–63. |
[36] | Algeo N , Kathleen B , Deirdre C . Breast Cancer Survivorship and Employment in Ireland: Legislative Systems and the Return to Work of Women with Breast Cancer’. WORK: A Journal of Prevention, Assessment & Rehabilitation. (2022) ;71: (4):927–39. |
[37] | Wess M. Bringing Hope and Healing to Grieving Patients with Cancer. Journal of Osteopathic Medicine. (2007) ;107: (S7):E41–E47. |
[38] | Arnout BA. Application of Structural Equation Modeling to Develop a Conceptual Model for Entrepreneurship for Psychological Service Workers During the COVID-19 Pandemic. WORK: A Journal of Prevention, Assessment & Rehabilitation. (2021) ;69: (4):1127–41. |
[39] | Wellisch DK , Cohen MM . The special case of complicated grief in women at high risk for breast cancer. Palliat Supportive Care. (2010) ;8: (01):7–15. |
[40] | Creswell JW , Miller DL . Determining validity in qualitative inquiry. Theory into Practice. (2000) ;39: :124–30. |
[41] | Arnout BI. Scientific research is a modern vision (quantitative, qualitative, mixed) Between practice and professionalism. Scholars Press, Germany. 2020. |
[42] | Starks H , Brown S . Choose your method: A comparison of phenomenology, discourse analysis, and grounded theory. Qualitative Health Research. (2007) ;17: (10):1372–80. |
[43] | Creswell JW , Creswell JD . Research design: Qualitative, quantitative, and mixed methods approach (5th ed.). Los Angeles, CA: Sage Publications. (2018) . |
[44] | Braun V , Clarke V . Using thematic analysis in psychology. Qualitative Research in Psychology. (2006) ;3: (2):77–101. |
[45] | Onrust SA , Cuijpers P . Mood and anxiety disorders in widowhood: A systematic review. Aging & Mental Health. (2006) ;10: (4):327–34. |
[46] | Kubler-Ross E. On Death and Dying. 1969. Macmillan, New York NY. (1969) . |
[47] | Doka K. Disenfranchised Grief. In DokaK. J. (Ed.), Living with Grief: Loss in Later Life (pp. 159-168). (2002) , Washington, D.C.: The Hospice Foundation of America. |
[48] | Sigorski D , Sobczuk P , Osmola M , et al. Impact of COVID-19 on anxiety levels among patients with cancer actively treated with systemic therapy. ESMO Open. (2020) ;5: (5):e000970. |
[49] | Tacón AM. Mindfulness, death anxiety, and grief in a patient with metastatic cancer. Clin Case Rep Rev. (2018) ;4: . DOI: 10.15761/CCRR.1000403 |
[50] | Arnout B. Predicting psychological service providers’ empowerment in the light of the COVID-19 pandemic outbreak: A structural equation modelling analysis. Counseling and Psychotherapy Research 14 June. (2020) ;20: (3):406–4018. |
[51] | Arnout B , Al-Dabbagh Z , Al Eid N , et al. The Effects of Corona Virus (COVID-19) Outbreak on the individuals’ Mental Health and on the Decision-Makers: A Comparative Epidemiological Study. International Journal of Medical Research & Health Sciences. (2020) ;9: (3):26–47. |
[52] | Arnout B , Al-Qadimi F . A structural Equation Modeling Analysis of Marital Bullying Scale. Journal of Public Affairs. (2019) ;20: (3):1–8. 10.1002/pa.2045. |
[53] | Arnout B. The Role of Positive Psychology interventions to Reduce Psychological Problems Associated With COVID-19 Pandemic: Prevention and Therapy Approach. Journal of Education Sohage University. 202;4: :7–26. |




