Text neck: An adverse postural phenomenon
Abstract
BACKGROUND:
The excessive use of hand-held mobile devices (HHMD) leads to a postural phenomenon known as text neck.
OBJECTIVE:
The aim of this paper is to discuss the anatomical, biomechanical and muscle activation changes within the cervical and thoracic regions associated with the sustained, forward, flexed neck posture, observed with excessive usage of hand-held mobile devices. Additionally, this paper examines the relationship of gender, as well as the effects of carrying backpack loads by youth, on this forward, flexed neck posture.
METHODS:
Multiple aspects of the text neck position that occur when an individual uses a HHMD are described.
RESULTS:
Prolonged use of hand-held mobile devices results in adverse anatomical and biomechanical changes in the cervical and thoracic spine, muscular imbalances, and postural compensations, all of which contribute to muscular overuse and fatigue resulting in pain.
CONCLUSIONS:
Physical therapists must educate their patients about proper posture while using hand-held mobile devices. Proper posture includes: holding the device close to eye level, using the device while standing or sitting and holding the device with a line of sight perpendicular to the surface of the device, using a larger screen, and texting with both hands. Also, because children are using hand held mobile devices at younger ages, parents and teachers must be educated about the dangers of prolonged use of hand-held devices.
1Introduction
With the growth in popularity of hand-held mobile devices (HHMD) such as smartphones, the incidence of use by adults, adolescents, and children is increasing daily. The average adult reports using a smartphone for 5.1 hours per day [1]. There are a wide variety of musculoskeletal complaints associated with the use of HHMD, including but not limited to neck, shoulder, back, finger, and thumb pain. The most prevalent of these complaints is neck pain, however, which is a component of an emerging phenomenon referred to as text neck [2]. This condition is a relatively new musculoskeletal condition that is intertwined with the increasing prevalence of HHMD usage, as prolonged neck flexion postures and frequency/duration of HHMD use are major risk factors for the development of text neck [3, 4]. It is important for clinicians to be aware of this condition, as it is a growing issue for not only adults but children as well. HHMD use is prevalent in both adults and children of all ages, but because the frequent use of HHMD is relatively new the effects of long-term use in children have not been not well-studied. It is likely that children growing up with smartphones may experience adverse postural and musculoskeletal changes at a young age, possibly causing issues throughout their lives. In addition to cell phone usage, backpack loads carried by children, adolescents, and young adults has been associated with increased complaints of musculoskeletal problems, and the combination of frequent HHMD use and heavy backpack loads has the potential to cause major postural issues, especially in the pediatric population. The purpose of this paper is to discuss the anatomical changes associated with the maintenance of a sustained forward flexed posture, to examine the differences in these changes between genders, to examine posture and muscle activation associated with HHMD use, and to investigate the relationship between text neck and the effect of backpack loading on children and adolescents.
2Prevalence of use
In the United States, 72%of adults (including 92%of adults age 18–34 years old) report owning a smartphone [5]. Across all users, there is a substantial amount of time spent using these devices. While the average adult reports using a smartphone for 5.1 hours per day, the numbers are similar for other age ranges as well. In the United States, university students age 19–22 years old reported using a HHMD for over 8.5 hours per day on average [6]. Likewise, adolescents and young adults had a high total number of reported hours per day spent using HHMD as well. In a census conducted by Common Sense Media, teenagers age 13–18 years old reported that of an average of more than 6.5 hours per day of screen time, 46%of this time was on a smartphone or other HHMD [7]. Similarly, “tweens” between 8 and 12 years old reported an average of more than 4.5 hours per day spent in front of screens, 41%of which was on a smartphone or other HHMD [7]. While adults may have the highest reported rates of HHMD use, children and teenagers are increasingly affected and influenced by HHMD use. Although the majority of studies on anatomical changes resulting from HHMD use have been performed in adult populations, this information is undoubtedly applicable to younger individuals as well. As technology advances, children and adolescents spend greater amounts of time using mobile devices, increasing the likelihood that these same anatomical changes will develop in these populations. If proper posture and decreased duration of HHMD use can be promoted at an earlier age when children start using these devices, there will be a lower chance of early spinal degeneration, cervical instability, muscular imbalance, proprioceptive changes, and disc herniation associated with text neck.
3Anatomical changes
One of the most commonly seen anatomical changes in the cervical spine is forward head posture, and this condition is often coupled with neck pain. Commonly, forward head posture has been linked to occupational or lifestyle habits which cause an anterior deviation of the neck from neutral, most frequently involving looking forward or down. For example, prolonged computer use, backpack carriage, HHMD use, and even mouth breathing have all been associated with forward head posture [8, 9]. When keeping one’s focus on an object held below the line of sight (such as a smartphone or other HHMD), the anterior deviation of the head and neck causes a forward head posture and decreased cervical lordosis, forming the posture commonly referred to as text neck.
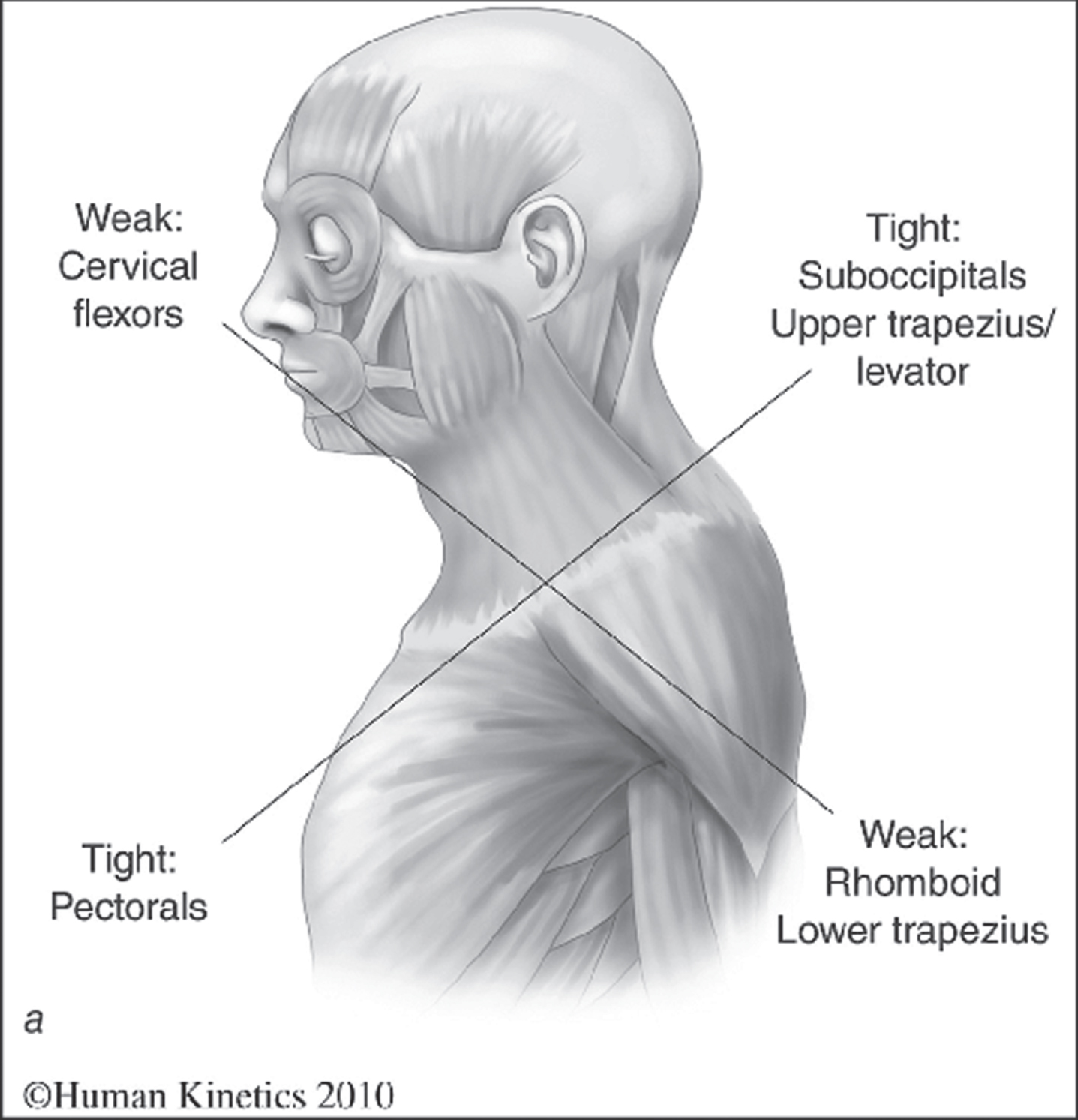
Forward head posture is characterized by lower cervical flexion and upper cervical extension. Since the head and neck migrates ventrally in this posture, this abnormal cervical flexion and extension occurs in order to maintain the eyes at horizontal. Excessive upper cervical extension results in decreased space in the atlanto-occipital and atlantoaxial joints, and a resultant increase in compressive forces placed posteriorly. This posterior compression shortens the suboccipital muscles, compresses the facet joints, slackens posterior ligamentous structures, and can lead to dysfunctions such as irritation and/or compression of the greater occipital nerve or vertebral artery [10]. Observationally, forward head posture is recognized when the head is positioned anterior to the line of gravity, which normally passes through the external auditory meatus, the bodies of the cervical vertebrae and acromion, and anterior to the thoracic spine [11]. This posture also involves a decrease in cervical lordosis, as well as altered thoracic kyphosis and changes in scapular positioning including protraction and downward rotation, in part due to weakness of the rhomboids and middle trapezius and tightness of the pectoralis minor [1, 10]. A secondary condition commonly seen in patients with forward head posture is known as Upper Crossed Syndrome, resulting from ligamentous and muscular imbalance in the neck and upper extremities [12]. This syndrome, shown in Fig. 1, is primarily characterized by tight musculature in the posterior cervical and anterior thoracic regions, particularly in the upper trapezius, levator scapulae, and pectoral muscles, as well as overstretched and weak musculature in the anterior cervical and posterior thoracic regions, particularly in the deep cervical flexors and scapular retractors [12, 13]. Other changes related to forward head posture include increased ligamentous stress applied to the posterior longitudinal ligament, ligamentum flavum, supraspinous ligament, and interspinous ligament due to positional changes, decreased muscular efficiency, muscle fatigue, and compression of the facet joints, all of which may lead to pain and further dysfunction [1, 10].
Fig. 1
Janda’s Upper Crossed Syndrome.
When the head and neck are held in a flexed posture for a prolonged period, such as with forward head posture, creep can occur in the posterior ligaments of the spine after as little as 10 minutes [14]. The occurrence of creep in these structures results in an increased cervical flexion range of motion, which can both cause a negative effect on the length-tension relationship of the posterior cervical musculature as well as decrease the stability provided by the posterior ligaments. These changes may result in the need for additional erector spinae activation to provide spinal stability, counteracting the creep of the passive structures. This muscular overactivation can potentially lead to muscular fatigue and spasm, and possibly pain [14]. If the cervical erector spinae are fatigued, they will be unable to perform efficiently and may demonstrate decreased resistance to forward flexion. A combination of ligamentous incompetence and inefficient cervical erector spinae activation can cause instability in the spine, which may result in abnormal movements between vertebral segments leading to disc herniation. The muscular imbalance, ligamentous changes, and resulting compensations further promote bad posture. These adverse postural changes may be preventable, however, especially if correct posture is promoted starting at a younger age.
The text neck posture assumed while operating a HHMD is similar to that of forward head posture, but instead of upper cervical extension the upper cervical region is held in a flexed position. This is because the compensation of extending the upper cervical spine to maintain the eyes at horizontal to see the environment is not necessary when using a HHMD, as the eyes are facing downward fixed on the device. This upper cervical flexion results in distraction forces posteriorly as opposed to the compression seen in forward head posture. The posterior elements of the occiput, the atlas, and the axis all become further apart, which can lengthen the suboccipital muscles, unweight the facet joints, and lengthen the posterior ligaments. The alar and transverse ligaments, responsible for providing atlanto-occipital and atlantoaxial stability, respectively, may become overstretched as well. Over time, one concern is that this text neck posture may result in upper cervical instability due to incompetence of these ligaments. If instability occurs, the greater occipital nerve, vertebral artery, and spinal cord all may be placed at risk. Similarly, Lee et al. [15] found that when texting, subjects flexed their cervical spine an average of 37 to 47 degrees. When the neck is held in a neutral position, the head has been shown to weigh approximately 10–12 lbs. The more flexed the neck is, however, the more weight is placed on the cervical vertebrae, intervertebral discs, and facet joints, which can lead to degeneration and herniation. When the head flexes to 15 degrees, the load on the spine increases to 27 lbs, and at 30 degrees of flexion the head weighs 40 lbs. At 45 degrees of neck flexion, the load of the head increases to 49 lbs, and further increases to 60 lbs when the neck is in 60 degrees of flexion [2, 16]. Maintaining a hyper-flexed head and neck position while repetitively using a HHMD can result in excessive loading of spinal structures and produce neck pain, a characteristic of the text neck posture [2].
The increased cervical flexion seen while using a HHMD may cause degeneration of cervical vertebrae as well as decrease cervical lordosis angles [17]. Although there is no set “normal” for cervical lordotic angles, it has been suggested that 20 to 35 degrees is the typical range [17]. A curvature less than 20 to 35 degrees appears as a flattened cervical spine, which disrupts the normal function of the neck musculature and can cause degeneration and disc herniation [17]. Typically, a HHMD is used below eye level or on a person’s lap which puts the neck into excessive flexion, decreasing normal cervical lordosis and creating this flattened cervical alignment. Frequent assumption of this posture while using a HHMD produces a significant and repetitive strain on the musculoskeletal system similar to that of forward head posture: increased activation of the cervical erector spinae and suboccipital muscles, levator scapulae, and semispinalis. This increased sustained activation can lead to increased spinal loading, poor posture, muscular fatigue and overall increased risk of musculoskeletal dysfunction [18, 19]. Additionally, increased muscle activation due to the text neck posture may lead to the formation of trigger points in the upper trapezius and suboccipital muscles, producing tension headaches, neck pain, temporomandibular joint pain, and decreased cervical and upper thoracic ranges of motion [20].
In addition to musculoskeletal changes and symptoms, prolonged time in forward head posture has been associated with proprioceptive changes within the spine. In a study by Lee et al. [21], subjects with forward head posture had significantly higher error rates than those without forward head posture when asked to perform an activity involving head position sense. The researchers’ conclusions supported previous research that forward head posture may cause changes in length-tension relationships as well as decreased competence of the muscle spindles, leading to impaired joint position sense in the cervical spine [21]. In the long term, sustained forward head posture can lead to plastic changes within the central nervous system, resulting in sensorimotor integration deficiencies that may cause further dysfunction [19]. Due to the similarities between the two, it would be reasonable to expect to find similar proprioceptive deficits in individuals with text neck.
4Gender differences
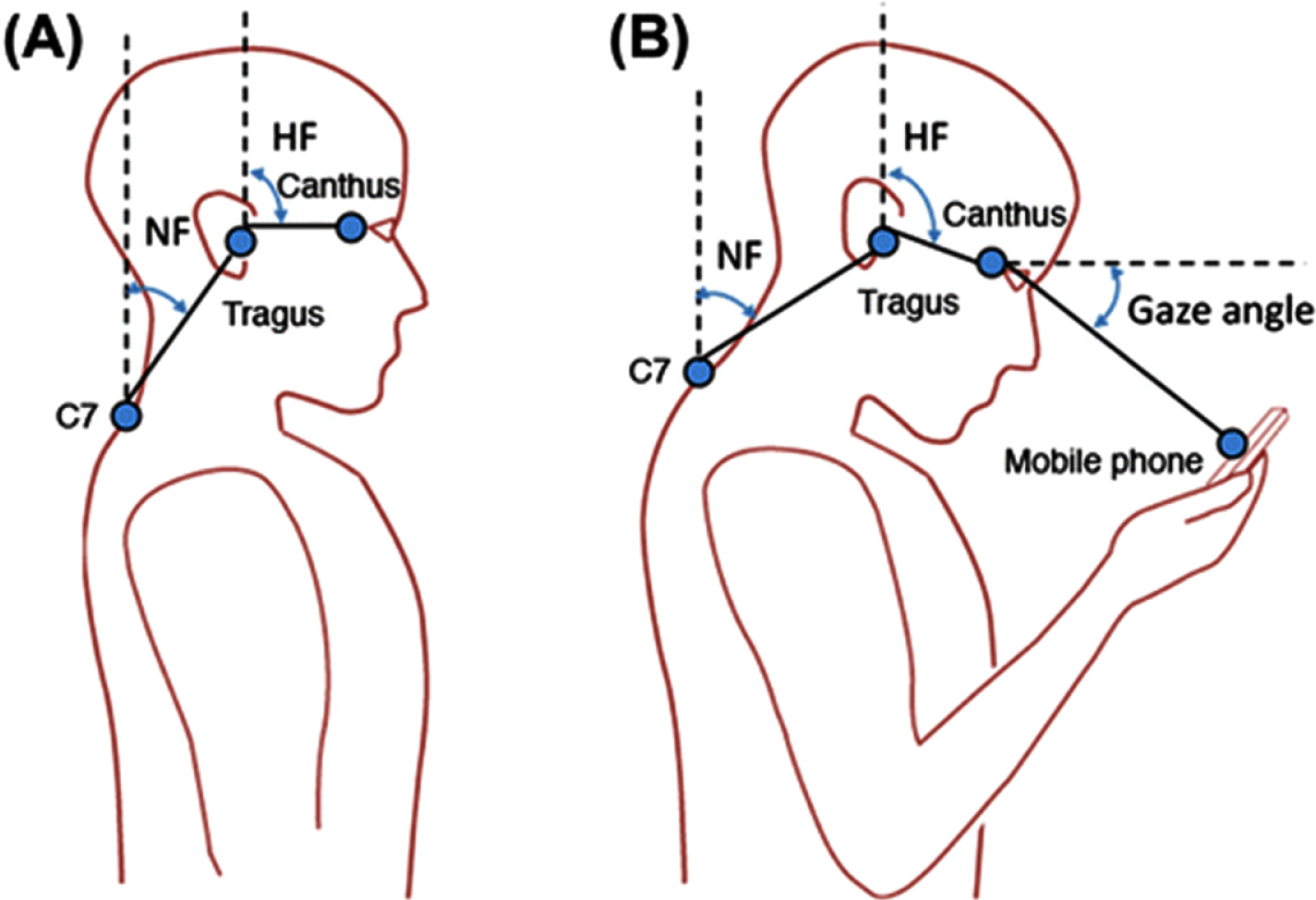
Though many of the adverse anatomical and postural effects associated with text neck are seen in both males and females, there are some slight differences associated with gender. In both males and females, head and neck flexion angles are significantly increased when standing and looking at a HHMD compared to standing without a mobile device [22]. Males, however, have been shown to demonstrate dramatically greater angles than females in two measures, the head flexion angle and the neck flexion angle. The head flexion angle is a measurement of the angle formed between vertical and an invisible line running from the tragus of the ear to the canthus, while the neck flexion angle is a measurement of the angle formed between vertical and an invisible line running from the tragus to the spinous process of the seventh cervical vertebra (see Fig. 2) [23]. Together, higher numbers on these two measures indicate a greater amount of total cervical flexion, and therefore a greater load applied to the cervical spine. In a recent study, on average, the head flexion angle of males increased by 23.54° and the neck flexion angles increased by 14.50° when using a HHMD [22]. Likewise, for both measures males demonstrated significantly larger neck and head flexion angles than females. This suggests that men may regularly text with a greater amount of cervical flexion than females, putting them at a higher risk for developing complications resulting from the text neck posture. Another study by Gold et al. [24] showed that both males and females text with a flexed neck, as well as maintain a non-neutral wrist in their typing hand. In this study, a flexed neck was described as when the ear was observed to be anterior to the acromion, and a non-neutral wrist was described as the appearance of being in either flexion, extension, radial deviation, or ulnar deviation. Another gender difference revealed in this study was that males displayed increased shoulder protraction while females displayed increased elbow flexion when texting on a HHMD [24].
Fig. 2
Visual depiction of the head flexion angle (HF) and neck flexion angle (NF) both in neutral head posture and during HHMD use.
Not only can gender play a role in postural differences seen in those with text neck, but it can also affect the pain and musculoskeletal sequelae resulting from this posture as well. In one study, it was shown that women perceive more overall musculoskeletal pain in the cervical spine and upper extremities than men [5]. Because women tend to perceive and report more musculoskeletal neck and upper extremity pain, it may be important to incorporate additional pain management techniques with this population. Understanding the differences between genders when using a HHMD is important when treating patients with text neck; both men and women text with increased cervical flexion, putting both at risk for neck pain unless their posture is addressed. Therefore, postural correction activities may be critical to both treatment and prevention of text neck.
5Cervical posture while texting
Because HHMD use is increasingly prevalent in adolescents and young adults, Ogrenci et al. [17] studied the association between cervical lordosis angles and duration of daily HHMD use in subjects between the ages of 25 to 42. There is no set “normal” angle of cervical lordosis, although experts agree that less than 20 degrees is associated with increased neck pain, and 30 degrees is a healthier angle that may decrease the risk of symptom development [17]. In the study, subjects with less than 12.5 degrees of cervical lordosis were considered “risky”, meaning they were at a higher risk for developing neck pain due to a flattened cervical spine. These subjects were asked to report their average duration of smartphone use as well as their overall history of use. From the data collected, the researchers concluded that there is an association between cervical lordosis angle and time of HHMD usage. Those using a HHMD at an average of 2 hours/day for 10 years are at a high risk for developing decreased cervical lordosis, thereby greatly increasing their risk for future neck pathologies [17]. As previously mentioned, the average adult currently uses hand-held devices for just over 5 hours per day. Today, children as young as two or three years old can often be seen using these devices. Assuming these children adopt the same HHMD postures and habits as adults, it is reasonable to expect that the development of text neck will be rapidly on the rise in younger populations.
Head and neck flexion angles have also been studied in various postures and with performance of assorted tasks. One study found that the neck flexion angle tends to increase more significantly when using a HHMD in a sitting versus a standing position. On average, the neck flexion angle while sitting is 10-14%greater than when standing [15]. The placement of the device also appears to play a factor in changes in head and neck flexion angles. Using devices placed on a person’s lap, for example, leads to increased head and neck flexion angles [25]. While maintaining a seated position, the best position for device use is placed on a table and angled upward towards the person’s head, or mounted or held just at or below eye level to avoid the need for increased upper and lower cervical flexion.
Ning et al. [26] studied the differences in neck flexion angle and cervical erector spinae muscle activation while changing three different variables: the type of HHMD (phone versus tablet), location of use (either on a table at elbow height or held in hand), and task (reading, typing, or gaming). The results of the study showed three noteworthy outcomes. First, they found that using a mobile phone increased neck flexion angles more so than when a larger tablet was used. This suggests that looking at a smaller screen could increase the neck flexion angle necessary to use the device, in turn increasing symptoms and development of text neck. Second, they found that using a smart phone placed on a table at elbow height resulted in increased neck flexion angles and increased cervical extensor activity. This highlights the fact that placing a device below eye level, such as in the lap, will increase the need for cervical flexion and increase the risk for text neck. Lastly, the typing task on a HHMD resulted in a greater increase in cervical extensor activation than either gaming or reading [26]. This result implies that the difficulty of the task, with texting requiring the greatest fine motor activity, may be correlated with increased muscle activation, thus increasing muscle strain and leading to the development of text neck. Similarly, Xie et al. [27] have shown that the cervical spine is affected differently when texting with one versus both hands. When performing a bilateral texting task, cervical flexion increased greater than when texting with one hand only, but texting with only one hand was associated with more asymmetrical cervical spine postures, including an increase in cervical rotation and side-bending [27]. Both of these abnormal postures can lead to further pain and musculoskeletal dysfunction, highlighting the importance of maintaining a neutral cervical posture when using a HHMD to avoid text neck.
6Thoracic posture while texting
Differences in posture observed while using a HHMD are not limited to the cervical spine, as the kinematics of the entire spine, including the thoracic region, are also affected. In both the cervical and thoracic spine, texting on a HHMD results in a more static and flexed posture compared to a typing task on a computer [27]. In a study by Lau et al. [28], the craniovertebral angle (CVA) and the upper thoracic angle in subjects with and without neck pain were measured. The CVA is a measurement of the degree of forward head posture, and is defined as the angle formed by the intersection of a horizontal line drawn through the spinous process of the seventh cervical vertebra and a line running from the same spinous process to the tragus of the ear. Smaller CVA values are indicative of an increased degree and severity of forward head posture. The upper thoracic angle is a measurement of the degree of thoracic kyphosis, and is measured between a horizontal line drawn through the spinous process of the seventh thoracic vertebra and a line connecting the spinous processes of the seventh cervical and seventh thoracic vertebrae. Lau et al. [28] found that subjects with neck pain displayed a smaller CVA and a larger upper thoracic angle, demonstrating a higher degree of forward head posture and thoracic kyphosis compared to asymptomatic subjects. Likewise, the change in the thoracic angle predicted neck pain more accurately than changes in CVA. As the upper thoracic angle and therefore degree of thoracic kyphosis increased, there was a simultaneous increase in perceived neck pain [28]. These findings indicate that the anatomical and postural changes associated with HHMD use are not limited to just the cervical spine, and that musculoskeletal changes taking place in the thoracic spine (such as thoracic hyperkyphosis and bilateral shoulder protraction) may contribute to pain and the development of other symptoms commonly seen with text neck [29]. It is extremely important for clinicians to recognize that text neck can cause changes to the thoracic region as well in order to properly evaluate and treat these patients.
7Muscle activation while texting
Electromyography (EMG) studies are beneficial in order to study the effect of different postures and activities on the activation of certain muscles, and multiple studies have examined differences in muscle activation specifically in the neck. Both the sternocleidomastoid (SCM) and the middle trapezius muscles demonstrate increased activity when the neck is in a flexed position, with greater SCM activity seen when the neck is fully flexed [30, 31]. These findings indicate that the typical posture seen when using a HHMD, characterized by a flexed neck and rounded shoulders, promotes higher activation of both the SCM and middle trapezius, which may lead to fatigue, pain, and further poor posture associated with text neck.
In patients with forward head and rounded shoulders, the position of the head also effects the kinematics and muscle activity of the shoulder. When individuals in this posture raise their arms overhead, both the serratus anterior and upper trapezius muscles demonstrate increased activation compared to a neutral posture [32]. When cued to correct their posture or when manually corrected by a therapist, these muscles demonstrated decreased EMG activity to perform the same overhead reaching task [32]. Therefore, having a more neutral head posture is related to better movement patterns during tasks involving the shoulder such as overhead reaching tasks, and strengthening periscapular muscles while decreasing overuse in other muscles around the neck and upper extremities can assist in decreasing pain neck and shoulder pain. Adopting a corrected, neutral cervical and thoracic posture can both improve the kinematics of the shoulder and decrease the probability of developing text neck, as well as the associated negative musculoskeletal consequences.
When comparing muscle activation during unilateral texting, bilateral texting, and computer typing, Xie et al. [33] found increased activation of the cervical erector spinae and upper trapezius during all three tasks in individuals with neck or shoulder pain. This suggests that overuse of these superficial muscles during these three tasks may lead to fatigue, and eventually cause chronic neck and shoulder pain. Those with neck or shoulder pain also reported higher Rate of Perceived Exertion (RPE) scores as well as more discomfort than asymptomatic subjects during all three tasks.
To avoid overuse of superficial muscles, it is important to activate the deep cervical muscles to promote correct neck posture and reduce muscular fatigue [34]. Patients with chronic neck pain often have an imbalance between superficial and deep muscles, which in turn further promotes forward head posture. In a study by Kim and Kwag [34], patients with neck pain were given an exercise program focusing on activation of the deep cervical flexors, including the longus colli and longus capitus muscles. Neck Disability Index (NDI) scores, pain, and cervical spine and shoulder postures were assessed at baseline, and then again after both 4 and 8 weeks. The results of this study showed significant improvements in NDI scores, pain, and posture measurements following the deep cervical flexor intervention compared to general strengthening exercises [34]. Additional research has shown that use of isometric contractions of the deep cervical muscles while simultaneously stretching the anterior shoulder muscles, including the pectoral muscles, results in decreased pain and increased cervical range of motion [1].
8Text neck and backpack load
Backpack loads are an especially pertinent risk factor for changes in the cervical and thoracic spine, especially those associated with an increase in forward head posture. While carrying a loaded backpack, the added posterior weight leads to postural changes necessary to accommodate the extra load. The most significant postural changes include an increase in forward trunk lean, usually accompanied by an increase in forward head posture. Combining these changes with the cognitive and visual demands of using a HHMD, the resulting cervical neck position may have deleterious effects over time. Many studies have looked at the effect of different backpack weights on posture, and have come to the consensus that individuals should carry no more than 10%of their body weight (BW) in their backpacks. In adolescents, carrying even 5–10%of their BW was found to cause negative postural compensations throughout the body, including increased forward head posture, rounded shoulders, forward trunk lean, and increased lumbar lordosis [35–38]. In a study by Kistner et al. [36], researchers set out to compare the changes in CVA, forward trunk lean (FTL), pelvic tilt angle (TILT), and pain in schoolchildren before and immediately after donning a backpack, as well as after walking for 6 minutes with various backpack weights. They found that immediately after adding a backpack weighing 10%, 15%, and 20%of the child’s body weight, there were postural compensations leading to changes in CVA, FTL, and TILT. These changes intensified in all three conditions after the children walked for 6 minutes, but this effect was particularly noticeable in the groups carrying 15%and 20%BW. The changes in CVA, FTL, and TILT angles were demonstrated by an increase in forward head, forward trunk lean, and an increase in lumbar lordosis [36]. Also, with an increase in backpack loads there was a coinciding increase in pain levels (rated using the Visual Analog Scale) in the neck, mid-back, and shoulder regions. This study showed that even a small increase in weight in a backpack causes postural compensations that can lead to the development of musculoskeletal disorders. The researchers concluded that it would be beneficial to reduce backpack weight as much as possible, with a maximum of 10%BW, in order to reduce the prevalence of musculoskeletal disorders in children and adolescents, such as chronic forward head posture [36].
Chansirinukor et al. [39] studied the effects on the cervical spine and shoulders after carrying a backpack at the individual students’ “normal” weight (ranging from 6.4%to 13.2%BW) versus at 15%of the students’ BW, as well as from carrying a backpack over only one shoulder and following a 5 minute walk, compared to standing with no backpack. They compared four angles in this study: the degree of forward head posture (measured by CVA), the measurement of rounded shoulders (measured by sagittal shoulder posture), the tilt of the head (measured by the anterior head alignment), and the angle of the upper cervical spine (measured by the craniohorizontal angle, the angle formed by the intersection of a horizontal line through the tragus and a line running from the tragus to the canthus). In all conditions of the study, the authors noted a significant decrease in CVA indicating an increase in forward head posture, and this change was most pronounced when wearing a backpack at 15%BW [39].
These studies highlight the importance of lighter backpacks as well as early intervention when it comes to postural education, as children and adolescents are highly susceptible to postural changes resulting from both increased backpack load as well as daily HHMD use starting at an early age. These early postural changes have the potential to cause musculoskeletal imbalances and degeneration starting in childhood or adolescence, many of which may persist throughout life.
9Discussion
Text neck has become a widespread modern-day epidemic, affecting people of all age groups and especially younger populations, as they are exposed to HHMD use for multiple hours a day starting at a much younger age. Additionally, children and adolescents are carrying heavy backpack loads on a daily basis. The postural compensations resulting from the combination of HHMD use and carrying loaded backpacks can ultimately lead to pain and disability, and the development of various musculoskeletal pathologies later in life.
Many studies have been performed looking at the effects of using a HHMD in various settings. The bottom line of these studies suggests that maintaining proper posture may be the key component in slowing the text neck epidemic. To both treat and prevent this posture and the associated musculoskeletal symptoms, postural education is vital for all HHMD users, regardless of age or gender. Maintaining a sustained, flexed neck posture while using these devices for hours at a time is the primary contributor to structural changes resulting in pain and dysfunction. Therefore, it is imperative that individuals using a HHMD be educated on proper body mechanics and usage. When using a HHMD it is important to maintain a neutral cervical spine, which can be accomplished by keeping the HHMD either at or just below eye level. Similarly, either standing up or sitting while holding the device with a line of sight perpendicular to the surface of the device, may promote a more neutral cervical spine. Larger screens may be beneficial, because a larger picture may decrease the need for cervical hyper-flexion to see the device. If a screen is too large, however, this may increase the overall weight of the HHMD, leading to an increased tendency to place the device in one’s lap, promoting cervical hyper-flexion.
Holding the HHMD at eye level may be accomplished by positioning it on a desk or other surface, or by holding the device up manually. While visual comfort may improve when the HHMD is held at eye level, an individual may experience fatigue in the shoulders and arms, thus requiring consideration for upper body posture in both sitting or standing, so that the arms may be supported in a way that enables an appropriate viewing position while minimizing fatigue and subsequent postural compensations.
While typing on a HHMD, it is more beneficial for both hands to be used instead of one hand to prevent asymmetrical neck postures. Furthermore, individuals should be encouraged to take frequent rest breaks from using a HHMD and to also re-assess their posture during these breaks. Early education and intervention for children and adolescents is essential if they regularly use a HHMD, to prevent pathological musculoskeletal changes from occurring at an early age. Text neck is an altogether preventable condition that must be brought into the spotlight for everyday HHMD users.
10Limitations and future research
This report has described multiple aspects of the text neck position that results when an individual uses a HHMD. The amount of high quality research on HHMD use is limited, especially in children, as these devices are relatively new to everyday consumer use. There are many more issues to be investigated regarding the effects of short term and long-term HHMD use on pain, cervical, thoracic, scapula and jaw posture and strength, cervical position sense, vision, gait, and more. Future research should examine these items during sitting, standing, and movement in both children and adults. Well designed, high quality laboratory, epidemiological and longitudinal studies are needed to strengthen the body of evidence.
11Conclusion
This paper highlights the multitude of adverse biomechanical, kinematic, and electromyographic implications of the cervical and thoracic postures observed when using a HHMD. The resulting text neck posture may have long-term subjective and postural consequences in all populations, highlighting the importance of early intervention when it comes to postural education, especially in younger populations. These early postural changes have the potential to cause musculoskeletal imbalances and spinal degeneration starting in childhood or adolescence that may persist throughout adulthood and it is vital that education on preventing and treating these changes is directed towards children, parents and teachers alike. Therefore, education should be focused on preventing forward head posture, excessive backpack loads, and common postural compensations associated with frequent HHMD use.
Conflict of interest
The authors declare no conflict of interest.
References
[1] | Kong YS , Kim YM , Shim JM . The effect of modified cervical exercise on smartphone users with forward head posture. J Phys Ther Sci. (2017) ;29: (2):328–31. |
[2] | Cuéllar JM , Lanman TH . “Text neck”: an epidemic of the modern era of cell phones? Spine J. (2017) ;17: (6):901–2. |
[3] | Berolo S , Wells RP , Amick BC 3rd. Musculoskeletal symptoms among mobile hand-held device users and their relationship to device use: A preliminary study in a Canadian university population. Appl Ergon. (2011) ;42: (2):371–8. |
[4] | Xie Y , Szeto G , Dai J . Prevalence and risk factors associated with musculoskeletal complaints among users of mobile handheld devices: A systematic review. Appl Ergon. (2017) ;59: (Pt A):132–42. |
[5] | Poushter J . Smartphone ownership and internet usage continues to climb in emerging economies [Internet]. Pew Research Center; 2016 [cited 2019 Aug 26].Available from: https://www.pewresearch.org/global/2016/02/22/smartphone-ownership-and-internet-usage-continues-to-climb-in-emerging-economies/. |
[6] | Roberts J , Yaya L , Manolis C . The invisible addiction: cell-phone activities and addiction among male and female college students. J Behav Addict. (2014) ;3: (4):254–65. |
[7] | Common Sense. The Common Sense Census: Media use by tweens and teens [Internet]. Common Sense; 2015 [cited 2019 Aug 26]. Available from: https://www.commonsensemedia.org/sites/default/files/uploads/research/census_researchreport.pdf. |
[8] | Gustafsson E , Thomée S , Grimby-Ekman A , Hagberg M . Texting on mobile phones and musculoskeletal disorders in young adults: A five-year cohort study. Appl Ergon. (2017) ;58: :208–14. |
[9] | Singla D , Veqar Z . Association between forward head, rounded shoulders, and increased thoracic kyphosis: a review of the literature. J Chiropr Med. (2017) ;16: (3):220–9. |
[10] | Haughie LJ , Fiebert IM , Roach KE . Relationship of forward head posture and cervical backward bending to neck pain. J Man Manip Ther. (1995) ;3: (3):91–7. |
[11] | Kendall FP , McCreary EK , Provance PG , Rodgers M , Romani W . Muscles: testing and function with posture and pain. 5th ed. Philadelphia: Lippincott Williams & Wilkins; (2005) . pp. 560. |
[12] | Bae WS , Lee HO , Shin JW , Lee KC . The effect of middle and lower trapezius strength exercises and levator scapulae and upper trapezius stretching exercises in upper crossed syndrome. J Phys Ther Sci. (2016) ;28: (5):1636–9. |
[13] | Page P . Shoulder muscle imbalance and subacromial impingement syndrome in overhead athletes. Int J Sports Phys Ther. (2011) ;6: (1):51–8.Figure 1, Janda’s Upper Crossed Syndrome. Reprinted, with permission, from Page et al, 2010, Assessment and Treatment of Muscle Imbalanace: The Janda Approach (Champaign, IL; Human Kinetics); pp. 52. |
[14] | Mousavi-Khatir R , Talebian S , Maroufi N , Olyaei GR . Effect of static neck flexion in cervical flexion-relaxation phenomenon in healthy males and females. J Bodyw Mov Ther. (2016) ;20: (2):235–42. |
[15] | Lee S , Kang H , Shin G . Head flexion angle while using a smartphone. Ergonomics. (2014) ;58: (2):220–6. |
[16] | Hansraj KK . Assessment of stresses in the cervical spine caused by posture and position of the head. Surg Technol Int. (2014) ;25: :277–9. |
[17] | Öğrenci A , Koban O , Yaman O , Dalbayrak S , Yılmaz M . The effect of technological devices on cervical lordosis. Open Access Maced J Med Sci.. (2018) ;6: (3):467–71. |
[18] | Kim SY , Koo SJ . Effect of duration of smartphone use on muscle fatigue and pain caused by forward head posture in adults. J Phys Ther Sci. (2016) ;28: (6):1669–72. |
[19] | Abu El Kasem ST , Abdel Raoof NA , Kattabie OM , Moustafa IM . Effect of forward head posture on sensorimotor integration. Int J Physiotherapy. (2017) ;4: (2):118–25. |
[20] | Kim EK , Kim JS . Correlation between rounded shoulder posture, neck disability indices, and degree of forward head posture. J Phys Ther Sci. (2016) ;28: (10):2929–32. |
[21] | Lee M-Y , Lee H-Y , Yong M-S . Characteristics of cervical position sense in subjects with forward head posture. J Phys Ther Sci. (2014) ;26: (11):1741–3. |
[22] | Guan X , Fan G , Chen Z , Zeng Y , Zhang H , Hu A , Gu G , Wu X , Gu X , He S . Gender difference in mobile phone use and the impact of digital device exposure on neck posture. Ergonomics. (2016) ;59: (11):1453–61. |
[23] | Guan X , Fan G , Chen Z , Zeng Y , Zhang H , Hu A , Gu G , Wu X , Gu X , He S . Gender difference in mobile phone use and the impact of digital device exposure on neck posture. Ergonomics. (2016) ;59: (11):1453–61. Figure 1, Schematic presentations of lateral measurements. A: Habitual standing posture. B: Mobile phone use posture. HF: Head flexion angle. NF: Neck flexion. C7: C7 spinous process. pp. 1454. |
[24] | Gold J , Driban J , Thomas N , Chakravarty T , Channell V , Komaroff E . Postures, typing strategies, and gender differences in mobile device usage: An observational study. Appl Ergon. (2012) ;43: (2):408–12. |
[25] | Young JG , Trudeau M , Odell D , Marinelli K , Dennerlein JT . Touch-screen tablet user configurations and case-supported tilt affect head and neck flexion angles. Work. (2012) ;41: (1):81–91. |
[26] | Ning X , Huang Y , Hu B , Nimbarte AD . Neck kinematics and muscle activity during mobile device operations. Int J Ind Ergon. (2015) ;48: :10–5. |
[27] | Xie YF , Szeto G , Madeleine P , Tsang S . Spinal kinematics during smartphone texting –A comparison between young adults with and without chronic neck-shoulder pain. Appl Ergon. (2018) ;68: :160–8. |
[28] | Lau KT , Cheung KY , Chan KB , Chan MH , Lo KY , Chiu TW . Relationships between sagittal postures of thoracic and cervical spine, presence of neck pain, neck pain severity and disability. Man Ther. (2010) ;15: (5):457–62. |
[29] | Morris C , Bonnefin D , Darville C . The Torsional Upper Crossed Syndrome: A multi-planar update to Janda’s model, with a case series introduction of the mid-pectoral fascial lesion as an associated etiological factor. J Bodyw Mov Ther. (2015) ;19: (4):681–9. |
[30] | Cheng CH , Chien A , Hsu EL , Chen CC , Cheng HK . Investigation of the differential contributions of superficial and deep muscles on cervical spinal loads with changing head postures. Plos One. (2016) ;11: (3):e0150608. |
[31] | Cheon S , Park S . Changes in neck and upper trunk muscle activities according to the angle of movement of the neck in subjects with forward head posture. J Phys Ther Sci. (2017) ;29: (2):191–3. |
[32] | Kwon JW , Son SM , Lee NK . Changes in upper-extremity muscle activities due to head position in subjects with a forward head posture and rounded shoulders. J Phys Ther Sci. (2015) ;27: (6):1739–42. |
[33] | Xie Y , Szeto GP , Dai J , Madeleine P . A comparison of muscle activity in using touchscreen smartphone among young people with and without chronic neck–shoulder pain. Ergonomics. (2016) ;59: (1):61–72. |
[34] | Kim JY , Kwag KI . Clinical effects of deep cervical flexor muscle activation in patients with chronic neck pain. J Phys Ther Sci. (2016) ;28: (1):269–73. |
[35] | Cheung C , Shum S , Tang S , Yau P , Chiu TT . The correlation between craniovertebral angle, backpack weights, and disability due to neck pain in adolescents. J Back Musculoskelet Rehabil. (2010) ;23: (3):129–36. |
[36] | Kistner F , Fiebert I , Roach K , Moore J . Postural compensations and subjective complaints due to backpack loads and wear time in schoolchildren. Pediatr Phys Ther. Spring. (2013) ;25: (1):15–24. |
[37] | Mo SW , Xu DQ , Li JX , Liu M . Effect of backpack load on the head, cervical spine and shoulder postures in children during gait termination. Ergonomics. (2013) ;56: (12):1908–16. |
[38] | Ramprasad M , Alias J , Raghuveer AK . Effect of backpack weight on postural angles in preadolescent children. Indian Pediatr. (2010) ;47: (7):575–80. |
[39] | Chansirinukor W , Wilson D , Grimmer K , Dansie B . Effects of backpacks on students: Measurement of cervical and shoulder posture. Aust J Physiother. (2001) ;47: (2):110–6. |




