Disparate healthcare access and telehealth-based hybrid consultations during the COVID-19 pandemic
Abstract
BACKGROUND:
The coronavirus disease-2019 pandemic led to rapid expansion of telehealth services. This was speculated to improve healthcare access among underserved populations, including individuals unable to take time off work or arrange transportation.
OBJECTIVE:
We completed a quality improvement project to evaluate the feasibility of hybrid consultations that combined televisits and abbreviated in-person visits for neuromuscular referrals.
METHODS:
Using a censoring date of August 5, 2021, we reviewed all outpatient neuromuscular consultations from August 5, 2020 to February 5, 2021. For both hybrid and traditional in-person consultations, we reviewed no-show rates, completion rates of ordered diagnostic workup, and billing codes. For hybrid consultations only, we also reviewed intervals between initial televisit and subsequent examination and rates of video-enhanced versus audio-only televisits.
RESULTS:
During the study period, we completed 153 hybrid and 59 in-person new-patient consultations (no-show rates 9% and 27% respectively.) For hybrid consultations, 77% and 73% of laboratory and imaging studies were completed respectively, compared to 89% and 91% for in-person consultations. For hybrid visits, average RVUs (a marker for reimbursement) per consultation depended on whether audio-only televisits were billed as telephone calls or E/M visits per insurance payer rules, while video-enhanced televisits were uniformly billed as E/M visits. This resulted in average RVUs between 2.09 and 2.26, compared to 2.30 for in-person consultations.
CONCLUSIONS:
Telehealth-based hybrid neuromuscular consultations are feasible with minor caveats. However, the future of telehealth may be restricted by decreasing reimbursement rates particularly for audio-only televisits, limiting its potential to improve healthcare access.
1Introduction
The coronavirus disease-2019 (COVID-19) pandemic led to the rapid expansion of telehealth services, a shift aided by revisions to the Centers for Medicare and Medicaid Services (CMS) 1135 waiver structure in March 2020 that drastically increased reimbursement rates for televisits [1]. There was early speculation that this expansion could improve access to subspecialty care, especially for patients in rural areas [2, 3]. It was also predicted that telehealth may reduce disparities in healthcare access both during and past the pandemic [4]. These predictions had high relevance among workers who have difficulty taking time off to attend clinic appointments, especially those in remote areas who must also budget transportation time to the nearest healthcare facility with subspecialty expertise.
Although telehealth services may be appropriate for a subset of neurology outpatient patient encounters, the lack of an in-person neurologic examination poses specific challenges. One patient-experience-based survey study found neuromuscular televisits were rated most poorly among neurological diagnosis categories [5] which may reflect the importance of the confrontational muscle strength testing specific to neuromuscular medicine encounters. During the pandemic, teleneurology experts have described systems to address this need, by describing strategies to evaluate motor strength on video [6, 7], the use of functional scales such as the Amyotrophic Lateral Sclerosis Functional Rating Scale (ALSFRS) and Myasthenia Gravis-Activities of Daily Living (MG-ADL) to evaluate disease progression [8], new disease-specific scales, [9] and comprehensive disease-specific guidance for completing televisits [10]. A recent landmark article detailed the real-world experience of one center where new neuromuscular medicine telehealth consultations were conducted completely via telehealth [11]. Despite these important strategies, none obviate clinical information garnered by confrontational muscle strength testing that requires a healthcare provider to test a patient’s strength via direct physical contact, possible only in an in-person evaluation.
To leverage the use of telehealth to reduce risk of COVID-19 transmission without sacrificing in-person examinations, we trialed a hybrid consultation model in August 2020. We targeted referrals to neuromuscular medicine given the importance of confrontational strength testing associated with new patients seen for this subspecialty. We sought to characterize the logistical and financial outcomes of these consultations as compared to traditional in-person consultations. If successful, we hoped this hybrid model may be adaptable to other specialties both during and following the pandemic.
2Methods
For context, on March 10, 2020, a state of emergency was declared in Massachusetts, leading us to discontinue routine outpatient neuromuscular consultations on March 16. The number of daily new COVID-19 cases peaked on May 1 [12]. Although we had subsequently reintroduced in-person appointments, we prioritized established patients and urgent referrals until August 2020, when we formally reintroduced new neuromuscular consultations.
In our telehealth-based hybrid consultation model, patients are scheduled initially for a televisit. At the conclusion of the televisit, based on their clinical judgment, the physician triages the patient to an abbreviated in-person appointment scheduled for half the duration of a traditional in-person new appointment, electrodiagnostic (EDx) study, or neither. Physicians were provided the option to obtain self-scheduling privileges in our electronic health record system, such that they may book the subsequent appointment with the patient during the televisit. To facilitate earlier EDx appointments after the initial televisit, a subset of weekly EDx slots was reserved for hybrid consultations for each physician. With the introduction of hybrid consultations, we continued to maintain traditional in-person consultations. Newly referred patients were scheduled to either model based on patient preference and next-available appointment slots, irrespective of consult question and without physician input.
Coinciding with the first hybrid consultation visit on August 5, 2020, we initiated a quality improvement project to monitor show rates, billing codes, and rates of ordered and completed laboratory and imaging studies for both hybrid and traditional in-person consultations. For hybrid consultations only, we also monitored the time intervals between initial televisit and subsequent neuromuscular examination conducted during an in-person visit or EDx visit, as well as rates of video-enhanced versus audio-only televisits. This project was undertaken as a quality improvement initiative. As it satisfied 19 criteria set by the Institutional Review Board classifying this work as quality improvement, it did not require formal supervision by the board, as per institutional policies.
3Results
From August 5 to February 5, 2021, we conducted 153 hybrid consultations (no-show rate for initial visit was 9%) and 59 in-person consultations (no-show rate was 27%) (Fig. 1). For the 153 patients who had initial televisits for hybrid consultation, 85 were triaged to EDx study (72 showed; no-show or cancellation rate was 15%), 33 to abbreviated in-person visit (21 showed; no-show or cancellation rate was 36%) and 35 to neither, resulting in a combined no-show rate (defined as no-show to any appointment) of 24%. For the 59 patients seen in in-person consultations, 34 were recommended to have EDx studies among which 28 were completed, for a combined no-show rate of 35%. Show rates and rates of diagnostic study completion are summarized in Table 1. For hybrid consultations, 47% of patients who attended only one in-person EDx study would have attended two in-person appointments in a traditional in-person consultation model (one initial visit and one EDx study), while 23% were deemed not to need an in-person appointment at all. Diagnoses and symptoms evaluated were similar among patient seen via hybrid or in-person consultations (Supplementary Table 1).
Fig. 1
Show rates for (a) hybrid and (b) traditional in-person consultations. Combined no-show rates are 24% and 35% respectively. EDx: electrodiagnostic study.
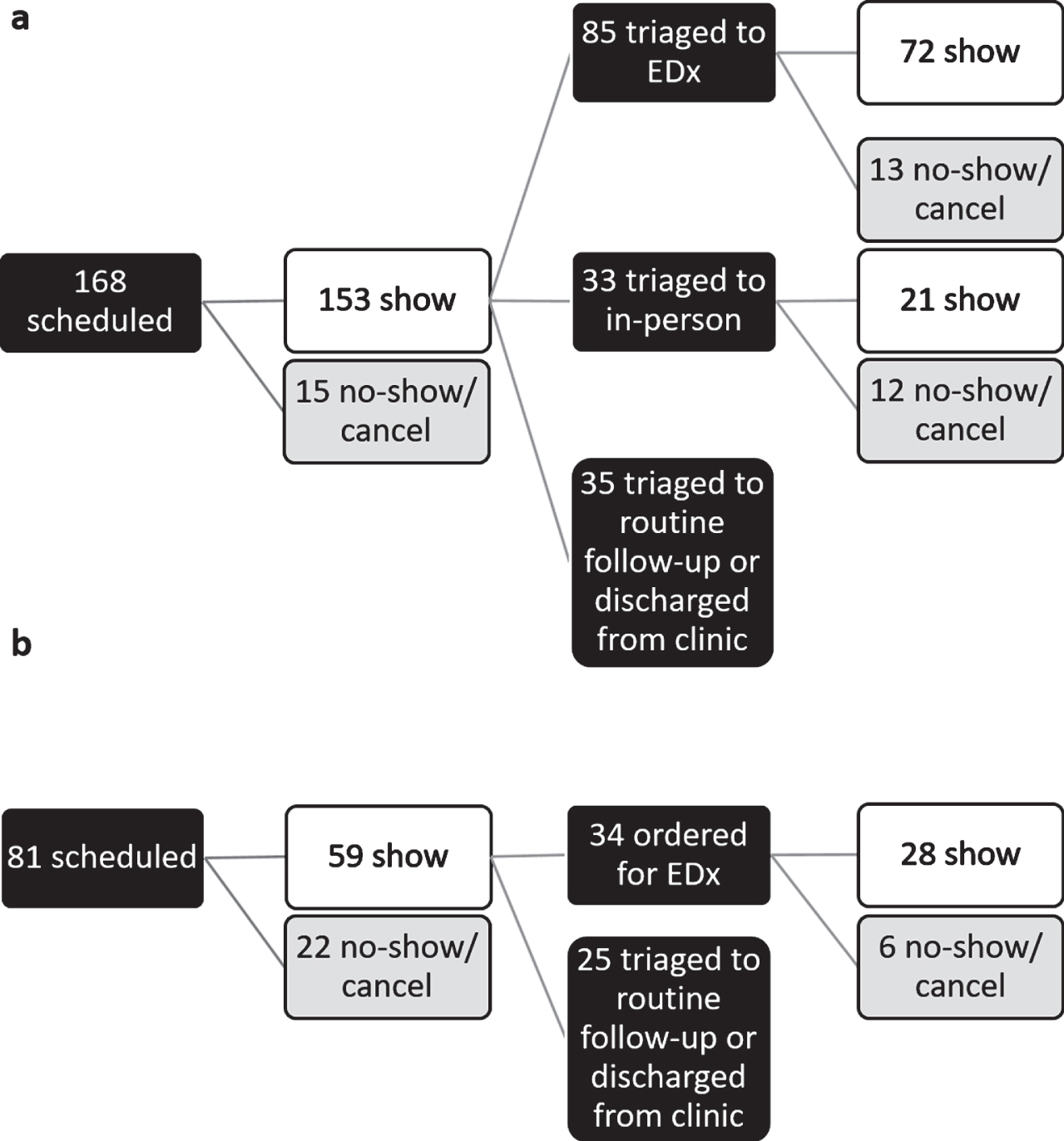
Table 1
Comparison of hybrid and in-person consultations from August 5, 2020 to February 5, 2021 in terms of show rates and rates of completion of ordered diagnostic tests. EDx: electrodiagnostic study
| Hybrid consultations | In-person consultations | |
| Scheduled visits | 168 | 81 |
| Completed visits | 153 | 59 |
| No-show rate to initial televisit | 9% (initial televisit) | 27% |
| Combined no-show rate | 24% (no-show to initial televisit or subsequent in-person visit or subsequent EDx study visit) | 35% (no-show to initial in-person visit or subsequent EDx study visit) |
| Ordered laboratory studies | 57 | 27 |
| Completed laboratory studies within 1 month | 44 | 24 |
| Completion rate of ordered laboratory studies within 1 month | 77% | 89% |
| Ordered imaging studies | 26 | 11 |
| Completed imaging studies within 3 months | 19 | 10 |
| Completion rate of ordered imaging studies within 3 months | 73% | 91% |
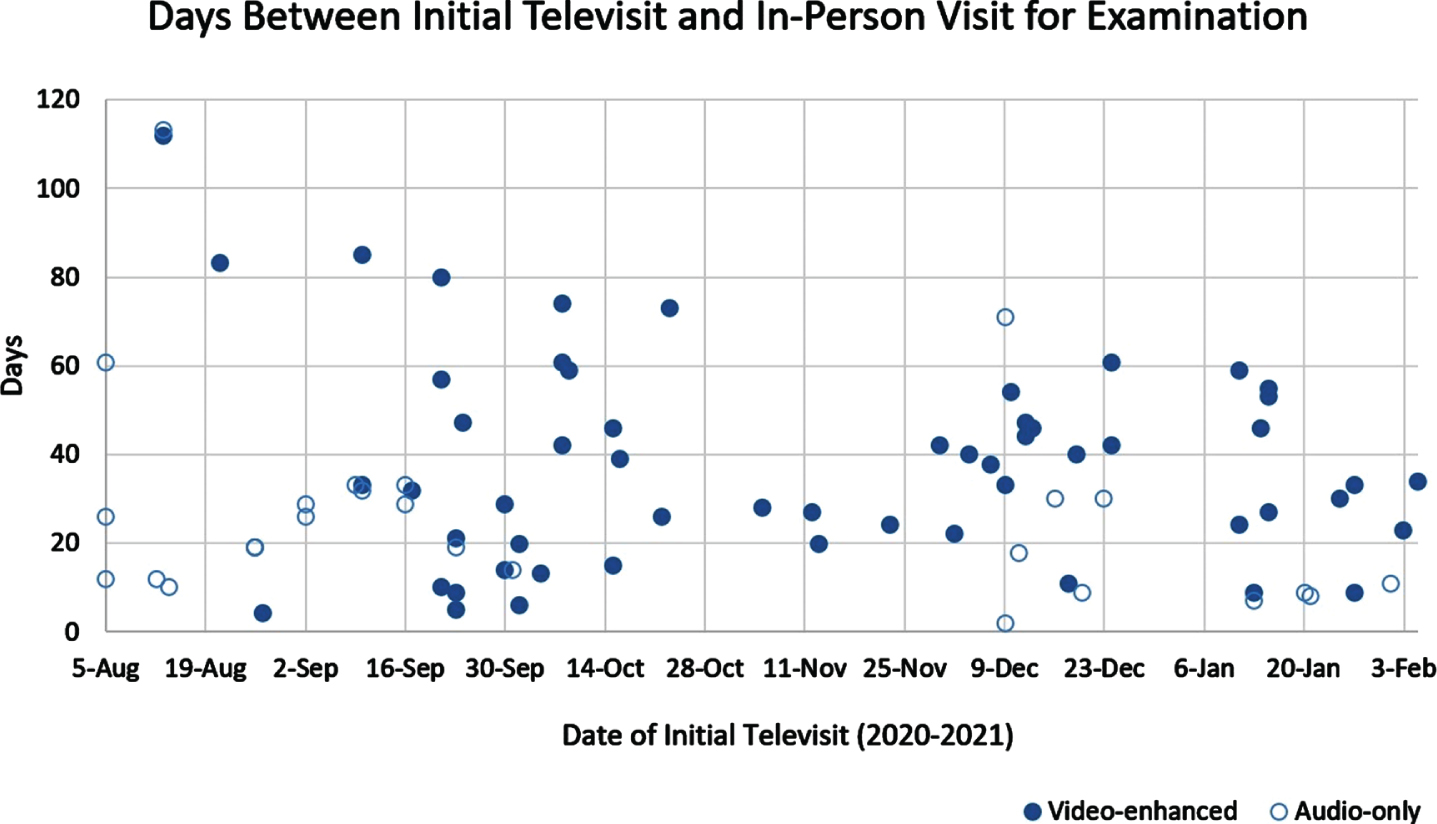
For hybrid consultations, the median and average days between the initial televisit and first examination (in EDx or abbreviated follow-up visit) were 30 and 34 respectively, with an overall decreasing trend over the study period (Fig. 2). This was achieved by more accurate projections of the necessary number of reserved EDx slots per week based on historical data accumulated over the initial weeks of introducing the model. For in-person consultations, the median and average days between initial visit and subsequent EDx (if ordered) were 36 and 47 respectively. For hybrid consultations, the rates of video-enhanced televisits (as opposed to audio-only televisits) increased over time, from 25% in the first 30 days of the study period to 77% in the final 30 days (Fig. 1). This was achieved by augmenting technical support for our telehealth platform over the initial months, as well as the growing experience with telehealth among our physicians.
Fig. 2
Hybrid consultations characterized by days between initial televisit and subsequent in-person visit or electrodiagnostic study. Decreased rates of follow-up for initial televisits in November are likely due to the second surge of coronavirus disease-2019 cases in our state by December 2020.
During this time period, there were no known COVID-19 transmissions between patients and staff, and physicians would have been notified if patients had positive testing in our health network within 14 days of contact.
The average RVUs generated per hybrid consultation depended on whether audio-only televisits were billed as telephone calls or E/M visits per insurance payer rules, while video-enhanced televisits were billed uniformly as E/M visits. This resulted in an average RVU per consultation between 2.17 and 2.40. In comparison, the average RVUs generated per in-person consultation was 2.53.
4Discussion
Our study showed that a telehealth-based hybrid consultation model is feasible for neuromuscular referrals. A large subset of patients attended fewer in-person visits while still having at least one neurological examination to ensure clinical accuracy. This finding is especially meaningful for individuals in rural areas or those of low socioeconomic status, who must both take time off of work to attend appointments while budgeting time for transportation. Alongside overall reduced show rates with hybrid consultations, our findings suggest that hybrid consultations may improve healthcare access without sacrificing clinical accuracy.
One caveat to hybrid consultations is lower rates of completed diagnostic studies. Past the study period, our institution has developed workflows allowing clinicians to send laboratory requisition forms to community laboratories and consolidating diagnostic studies ordered by multiple clinicians. Our radiology electronic platform was also integrated with the main electronic health record system to improve ease of scheduling neuroimaging studies. Similarly, we were also able to implement small workflow changes to reduce the time interval between the initial televisit and subsequent examination, and to increase the proportion of televisits conducted via video instead of telephone. These minor nuances to hybrid consultations and televisits were relatively easy to address, with clearly favorable cost-benefit analyses.
There have been other examples of successful hybrid consultation models, for example for multidisciplinary clinics in which patients are seen by multiple providers over several hours. In this scenario, it is especially important to reduce face-to-face time and conserve personal protective equipment use, with only a subset of providers needed to evaluate the patient in-person while others may rely on these providers’ examination to conduct telehealth visits [13]. Another important application for a hybrid model is the management of patients who need frequent follow-up appointments but may also benefit from occasional in-person visits to maintain rapport or trust. For example, in a New York City-based clinic for patients with drug use, patients were given telephones to conduct televisits and provided the option for in-person visits as needed for further support [14]. Our quality improvement project adds to the literature describing a hybrid model in which an initial televisit is used both for history-taking and triaging, followed by modified in-person appointments.
In terms of billing, RVUs per new hybrid consultation were comparable to traditional in-person consultations if audio-only televisits were eligible for billing as E/M visits, but markedly reduced if they were billed as telephone visits due to insurance payer rules. As such, telehealth-based hybrid consultations may become financially unsustainable, especially as insurance payers have signaled further reduction of reimbursements past the pandemic. Experts who advocate for the use of telehealth to reduce healthcare disparities argue that policies regarding reimbursement must be made at the national rather than state level, to promote equity among health systems [15].
Importantly, even if hybrid consultations are proven logistically and clinically feasible for certain settings, the dimension of both patient and provider satisfaction should be taken into account, representing an area of future study. Increasingly robust studies have emerged on satisfaction towards telehealth in neurology, finding that a majority of patients are satisfied with televisits but a lower proportion wish to continue engaging in the future. These findings may suggest that patients may tolerate televisits out of necessity during the pandemic, but would prefer in-person appointments if given a choice in the future [17]. Qualitatively, patients appreciated the reduction of commute time and associated costs, which has relevance to American workers, particularly among those in rural areas far from subspecialty care centers. Meanwhile, a recent systematic review of satisfaction of physicians across different specialties and practice settings suggest acceptable rates of satisfaction among providers [18]. Future works may investigate patient and provider perceptions specifically for telehealth-based hybrid consultations.
In terms of limitations, our study is a single-center quality improvement-based project at a safety-net hospital, which has specific challenges not generalizable to all institutions. As well, even though we chose a final censoring date six months after the period in question to ensure that the majority of follow-up visits were captured, it is possible some visits may have taken place past the censoring date.
5Conclusion
Telehealth-based neuromuscular hybrid consultations are feasible logistically, with the potential to improve healthcare access. Similar models may be adaptable for outpatient subspecialty clinics at other institutions. However, telehealth is facing decreasing reimbursement rates for both audio-only and video-enhanced visits, which may limit its future use. The COVID-19 pandemic has already augmented pre-existing healthcare disparities, disproportionately affecting those of lower socioeconomic status [16]. In order for televisits to remain an option for patients who can access care from their homes or workplace, it is essential that future decisions regarding telehealth made at the governmental regulatory level be made with close attention on equity.
6Ethical approval
This project was undertaken as a quality improvement initiative. As it satisfied 19 criteria set by the Institutional Review Board classifying this work as quality improvement, it did not require formal supervision by the board, as per institutional policies.
Informed consent
Not applicable.
Conflict of interest
The authors declare that they have no conflict of interest.
Acknowledgments
None to report.
Funding
The authors report no funding.
Supplementary material
[1] The supplementary material is available in the electronic version of this article: https://dx.doi.org/10.3233/WOR-211463.
References
[1] | Steinbach R , Prell T , Gaur N , Stubendorff B , Roediger A , Ilse B , et al. Triage of Amyotrophic Lateral Sclerosis Patients during the COVID-19 Pandemic: An Application of the D50 Model. Journal of Clinical Medicine. (2020) ;9: (9). |
[2] | McGinley MP , Ontaneda D , Wang Z , Weber M , Shook S , Stanton M , et al. Teleneurology as a Solution for Outpatient Care During the COVID-19 Pandemic. Telemedicine Journal and E-health. (2020) ;26: (12):1537–9. |
[3] | Haulman A , Geronimo A , Chahwala A , Simmons Z . The Use of Telehealth to Enhance Care in ALS and other Neuromuscular Disorders. Muscle Nerve. (2020) ;61: (6):682–91. |
[4] | Chirra M , Marsili L , Wattley L , Sokol LL , Keeling E , Maule S , et al. Telemedicine in Neurological Disorders: Opportunities and Challenges. Telemedicine Journal and E-health. (2019) ;25: (7):541–50. |
[5] | McKenna MC , Al-Hinai M , Bradley D , Doran E , Hunt I , Hutchinson S , et al. Patients’ Experiences of Remote Neurology Consultations during the COVID-19 Pandemic. European Neurology. (2020) :1–4. |
[6] | Saporta MA , Granit V , Lewis R , Benatar M . Yes, we can: Neuromuscular examination by telemedicine. Muscle Nerve. (2020) ;62: (6):E83–e5. |
[7] | Al Hussona M , Maher M , Chan D , Micieli JA , Jain JD , Khosravani H , et al. The Virtual Neurologic Exam: Instructional Videos and Guidance for the COVID-19 Era. The Canadian Journal of Neurological Sciences. (2020) ;47: (5):598–603. |
[8] | Garibaldi M , Siciliano G , Antonini G . Telemedicine for neuromuscular disorders during the COVID-19 outbreak. J Neurol. (2020) :1–4. |
[9] | Menon D , Alnajjar S , Barnett C , Vijayan J , Katzberg H , Fathi D , et al. Telephone consultation for myasthenia gravis care during the COVID-19 pandemic: Assessment of a novel virtual myasthenia gravis index. Muscle Nerve. (2021) ;63: (6):831–6. |
[10] | Guidon AC , Muppidi S , Nowak RJ , Guptill JT , Hehir MK , Ruzhansky K , et al. Telemedicine visits in myasthenia gravis: expert guidance and the myasthenia gravis core exam (MG-CE). Muscle Nerve. (2021) . |
[11] | Khan S , Kramer A , McIver J , Cady L , Trivedi JR. New patient access via telehealth in neuromuscular medicine during COVID-19. Work. (2021) ;69: (3):715–9. |
[12] | Gentile L , Mazzeo A , Russo M , Arimatea I , Vita G , Toscano A . Long-term treatment with subcutaneous immunoglobulin in patients with chronic inflammatory demyelinating polyradiculoneuropathy: a follow-up period up to 7 years. Scientific Reports. (2020) ;10: (1):7910. |
[13] | List R , Compton M , Soper M , Bruschwein H , Gettle L , Bailey M , et al. Preserving Multidisciplinary Care Model and Patient Safety During Reopening of Ambulatory Cystic Fibrosis Clinic for Nonurgent Care: A Hybrid Telehealth Model. Telemedicine Journal and E-health. (2021) ;27: (2):193–9. |
[14] | Dunham K , Giardina M , Kolod B , McBratney E , Medina Blanco P , Riazi F , et al. Transitioning Clinical Care for People Who Use Drugs to Telemedicine: Lessons Learned One Year into the COVID-19 Pandemic. Telemedicine Journal and E-health. (2021) ;27: (8):929–33. |
[15] | Gaziel-Yablowitz M , Bates DW , Levine DM . Telehealth in US hospitals: State-level reimbursement policies no longer influence adoption rates. International Journal of Medical Informatics. (2021) ;153: :104540. |
[16] | Tirupathi R , Muradova V , Shekhar R , Salim SA , Al-Tawfiq JA , Palabindala V . COVID-19 disparity among racial and ethnic minorities in the US: A cross sectional analysis. Travel Medicine and Infectious Disease. (2020) ;38: :101904. |
[17] | Olszewski C , Thomson S , Strauss L , et al. Patient Experiences With Ambulatory Telehealth in Neurology: Results of a Mixed-Methods Study. Neurol Clin Pract. (2021) ;11: (6):484–496. |
[18] | Hoff T , Lee DR . Physician Satisfaction With Telehealth: A Systematic Review and Agenda for Future Research. Qual Manag Health Care. (2022) ;10: :1097. |




