Radiographers’ musculoskeletal health in Western Switzerland: WRMSDs symptoms prevalence and risk factors
Abstract
BACKGROUND:
Work-related musculoskeletal disorders (WRMSDs) are a significant occupational health concern in radiographers.
OBJECTIVE:
This study aimed to describe radiographers’ WRMSDs symptoms prevalence and severity, exploring associations with occupational risk factors.
METHODS:
A cross-sectional study was conducted to explore WRMSDs symptoms and occupational risk factors in radiographers of Western Switzerland using an online survey, based on the Nordic Musculoskeletal Questionnaire (NMQ). Descriptive statistics were conducted to analyze the collected data, and associative statistics to identify the risk factors related to symptoms.
RESULTS:
Participants (n = 359) presented a high prevalence of WRMSDs symptoms in the last 12 months (94.7%), with a related absenteeism rate of 15.6%. In the last 7 days, symptoms prevalence was 67.7%. The most affected anatomical regions, over both time periods, were the neck (73.0%, 36.8%) and low back (67.4%, 35.7%). Associative statistics underlined risk factors affecting significantly radiographers’ health (OR >2) were the “awkward postures” (OR = 2.86; 95% CI 1.78–4.58) and “feeling anxiety/stress at work” both for low back (OR = 2.38; 95% CI 1.39–4.08), and being a woman for the neck (OR = 2.64; 95% CI 1.51–4.61).
CONCLUSIONS:
There is a high WRMSDs symptoms prevalence in Western Switzerland radiographers. Radiographers’ work demands namely for awkward postures increases the odds for WRMSDs symptoms presence, affecting predominantly neck, upper and lower back. Our data suggest that further research is needed to implement adapted prevention to this specific context.
1Introduction
Work-related musculoskeletal disorders (WRMSDs) are a significant occupational health concern threating workers’ health and resulting from an imbalance between work demands and workers characteristics and capacities [1].
Radiographers are amongst health professionals presenting a high prevalence of WRMSDs symptoms [2–4]. However, prevalence, and symptoms are slightly dependent on the type of studies and imaging modalities that are assessed [3–6]. Previous studies dedicated to diagnostic radiographers showed a prevalence ranging from 67% [3] to 93% [2] of WRMSDs with back, neck and upper limbs, as the most affected anatomical regions [3, 7]. In other imaging specialties such as sonography, radiographers showed to be particularly exposed to several risk factors with a prevalence of WRMSDs over 90% [4]. The neck, shoulder, and wrist/hand are the most affected anatomical areas [8, 9], notably due to specific wrist and body movements during the ultrasound scanning [9]. WRMSDs are also present amongst therapeutic radiographers, with main complaints on low back, neck, and shoulders [5, 8, 10].
The prevalence and symptoms associated to WRMSDs shows that radiographers are exposed to occupational risk factors [2, 11–14], namely awkward postures adopted during patient positioning and equipment handling, notably in conventional radiography, mammography and radiotherapy [5, 7, 15, 16]. The use of force is another ergonomic risk factor observed in main radiographers’ activities during the manipulation of X-ray tubes, mobile radiography and ultrasound probes [4, 16, 17], but also during patient handling as well. Indeed, the manipulation of obese, elderly and passive patients can promote or aggravated muscular disorders due to the lack of patient participation [18, 19]. The static work, repetitive movements and tasks over long periods were observed and revealed to be problematic [2, 4, 14, 15, 17]. The organizational and psychological factors also seem to be important contributors of WRMSDs in radiographers [5, 16, 18] due to the increased workload, growing complexity of medical imaging examinations and intensification of interdisciplinary interactions. The mental and psychosocial burden associated to the activities can cause systemic stress reactions, which can contribute to increase the risk of WRMSDs [12, 16, 20].
Radiographers tend to postpone the treatment of their injuries having as main consequences the absenteeism, early retirements, loss of performance and productivity, which leads also to a financial and social burden [21, 22]. For this reason, radiographer’s work must be analyzed to implement preventive measures allowing the improvement of work conditions and occupational health in order to reduce WRMSDs consequences [23]. However, current studies focused on radiographers’ activity are still scarce in Swiss context and the existing literature focuses only diagnostic radiographers and/or sonographers, making it difficult to have an overview of the musculoskeletal health in the three radiography fields (diagnostic and interventional radiography, nuclear medicine, and radiotherapy). To prevent accurately WRMSDs symptoms in radiographers, further investigation is necessary specially in Switzerland to have a comprehensive understanding of radiographers in Swiss context and activities, in all imaging fields.
The aim of this study was to characterize WRMSDs symptoms of radiographers working in the three fields available in Western Switzerland, by identifying the prevalence and severity of WRMSDs symptoms. Investigation of associations between WRMSDs symptoms and occupational risk factors and participants characteristics were also carried out.
This study gives a contribution to the radiographers working in medical imaging departments namely in (i) increasing awareness of healthcare stakeholders and policy makers about musculoskeletal health status of radiographers of Western Switzerland; (ii) as well as in identifying the risk factors related to WRMSDs symptoms; (iii) to facilitate a better cooperation between all actors involved in this field to help in the future the creation of a better department and equipment design; (iv) and to elaborate occupational health prevention programs to reduce WRMSDs symptoms and prevalence.
2Materials and methods
2.1Study context
A cross-sectional study was conducted between September 7th and October 31st, 2020, to assess radiographers’ WRMSDs symptoms prevalence, severity, and occupational risks factors in Western Switzerland. The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Vaud Swiss Ethics Committee (protocol code 2020-011774 on 05/08/2020).
2.2Data collection and participants
A survey was designed in French to characterize radiographers’ WRMSDs symptoms by identifying the prevalence, severity, and associated occupational risk factors. The survey was tested with a group of 12 radiographers (4 radiographers per imaging field) ensuring tool consistency, before being distributed to all Western Swiss radiographers.
Swiss Western radiographers were estimated at 1’952 in 2020 [24, 25]. The inclusion criteria of this study were: being a radiographer of Western Switzerland currently working in clinical practice and being actively employed during the last 12-months.
An invitation containing the survey’s link was emailed to the chief-radiographers’ members of “Collège des Chefs TRM” (CCTRM) and to the clinical practice partners of the “Haute Ecole de Santé de Vaud” (HESAV), asking them to transfer it to all their collaborators. Other recruitment methods were used, namely social network communications channels (e.g., LinkedIn) and the radiographers’ Swiss professional association (ASTRM). Reminder emails and posts on social network were used within this period to encourage radiographers to complete the survey.
The survey was distributed using the LimeSurvey software (version 3.20.1) and it was composed by an enclosure letter used as a consent form and other 6 sections requiring: A. Individual factors; B. Professional background factors; C. Self-reported WRMSDs and symptoms severity; D. Ergonomic and physical factors; E. Organizational and psychosocial factors; F. Remarks and comments.
Informed consent was obtained from all subjects involved in the study. The data was confidential and only accessible to authorized persons within the research project’s scope.
Respondents were characterized through 17 questions (section A) namely: gender, date of birth, weight, height, general health, sports activity, tobacco, alcohol, and energy drinks consummation, use of pain medication, medical consultations, rehabilitation treatments, present diseases/health problems and self-reported MSDs. Thirteen questions enquired about the work characteristics (section B), specifically: years of practice, professional function, years working in the current institution, type of institution, work percentage, shift type, imaging modalities practiced, working days per imaging modality, due to its possible impact on WRMSDs development [2, 7, 12, 26].
In this study, the “self-reported WRMSDs symptoms section” (section C) was assessed based on a French version of Nordic Musculoskeletal Questionnaire (NMQ) already validated in French [27]. The NMQ is a standardizer questionnaire, worldwide applied, especially in the healthcare sector to detect and analyze musculoskeletal symptoms [28]. The NMQ allows the self-report of WRMSDs symptoms for nine anatomical regions: neck, upper back, low back, shoulder(s), elbow, wrist(s)/hand(s), hip(s)/thigh(s), knee(s), or ankle(s)/feet within the last 12 months and the last 7 days [29, 30]. The symptoms severity was assessed through work absence and its length in the last 12 month and new questions about pain intensity using Numeric Pain Rating Scale (NPRS) and pain intensity in the last 7 days were added based on a Portuguese version of NMQ [31–33]. Fourteen additional questions were also employed to identify the most affected body regions by imaging modality performed in clinical practice.
The ergonomic risk factors (section D) were assessed by one question of 5 statements covering awkward posture adopted, use of force, prolonged static position and repetitive movements. The physical risk factors were assessed through 7 statements (section D), including radiological equipment, physical environment, service layout, workspace, radiological accessories, IT equipment, and furniture. Both questions were rated with a 4-point Likert scale, one for frequency (ergonomic factors), and the other for adequacy (physical factors). Data management was carried out to assign numbers to anchor terms.
The organizational/psychosocial dimension (section E) covered different dimensions: work pace, time allocated to complete the tasks, requirement of full attention, autonomy, quality of interactions with the hierarchy, colleagues, and other healthcare workers, satisfaction at work, and anxiety/stress.
2.3Study variables and data analysis
According to the nature of variables, descriptive and associative statistics were used to perform data analysis. For statistical analysis, responses were grouped in “Never/Sometimes”, “Often/Always” or “Totally/Mostly inadequate”, “Mostly/Totally adequate” and “Don’t know/Not applicable” according to the item assessed. New variables were created from individual characteristics raw data as “age” from the “date of birth”, “Body Mass Index (BMI)” from “height” and “weight” variables. Radiographers’ functions allowed the definition of radiographers’ practice as “radiographers” or “radiographers and other function(s)”. Other categories were grouped (e.g., frequency of shifts was grouped into two categories: “Never/Sometimes” and “Often/All the time” and general health status in “Very good/Good” and “Very bad/Bad/Moderate”) to meet the needs of statistical analysis. Statements were rated by a 4-points Likert scale indicating the agreement with the statement, and anchor terms were labelled with numbers and regrouped in two categories (“Totally/Mostly disagree” and “Mostly/Totally agree”) for data analysis.
Descriptive statistics were mainly used to describe participants’ characteristics (e.g., age, gender, years of experience), prevalence and severity of WRMSDs (WRMSDs rates, work absence, work absence length, pain intensity and frequency). Quantitative variables were presented with mean, and standard deviation (SD) (e.g., age, year of experience) while qualitative variables were analyzed with modal value, median and contingency tables (e.g., gender, general health status, smoker status). In this study, the 4-point Likert scales were considered as ordinal data [34]. Univariate statistical test, namely, chi-square test and exact Fisher test were used to explore associations of WRMSDs symptoms (for both time periods separately) with participants characteristics and risk factors’ variables. The results with a level of significance above 0.05 were considered as significantly associated. Odd ratios (OR) were used to measure the association between the risk factors and the most common symptoms compared to a reference group, and the 95% confidence intervals (CI) were respectively reported. Stata, version 16.0 (StataCorp LP, College Station, TX, USA) and Microsoft® Excel (version. 16.43) were used for data management and data analysis.
3Results
3.1Response rate and participants’ characteristics
This study did not intend to be representative of Swiss radiographers due to the voluntary basis of the survey. 437 radiographers from Western Switzerland answered the questionnaire but 78 did not meet the inclusion criteria (currently working in clinical practice and actively employed during the last 12-months) being excluded from the analysis. A total of 359 questionnaires were analyzed.
The participants were predominantly women (64.3%). The mean age was 40±11 years ranging from 22 to 65 years old. Out of 359 participants, 76.6% did not smoke and 64.1% practiced regularly physical activities. The majority (85.0%) of the participants perceived their general health status as “good” or “very good”, having a low (30.6%) consummation of medication in the last 7 days; 20.9% consulted a doctor more than 4 times a year and 12.0% underwent rehabilitation treatment during this study. Out of 339, 110 respondents had diseases or health disorders, with 68.5% reporting health problems impacting negatively their musculoskeletal system.
The mean professional experience was 15±12 years, with at least 11±10 years spent in the current institution. The participants worked mainly in full time (52.1%), with 98.3% working often during the day, 20.1% during nightshifts and 9.5% being on-call. The majority (68.3%) of radiographers did not have any other role than standard clinical practice, while 31.7% had “other activities” as chef, or imaging modality manager, researcher or radiation protection expert.
The highest proportion (73.8%) of radiographers worked in diagnostic and interventional radiology, 16.4% worked in radiotherapy and 9.8% in nuclear medicine. The diagnostic radiographers practiced at least 4 (out of 6) imaging modalities, while nuclear medicine radiographers worked in 3 (out of 3) and therapeutic radiographers in 2 (out of 3). In diagnostic, most radiographers were working in conventional radiology (n = 242), followed by Computed Tomography (CT) (n = 192), Magnetic Resonance Imaging (MRI) (n = 152), ultrasound (n = 99), interventional radiology (n = 96) and mammography (n = 95). In nuclear medicine (NM), radiographers equally worked at Single Photon Emission Computed Tomography (SPECT) and Positron Emission Tomography (PET) (n = 34), while a smallest number worked in laboratories (n = 24). Most therapeutic radiographers were applying therapy and/or performing CT/MRI simulation (respectively, n = 55 and n = 41), while a minority worked as dosimetrist (n = 23). Other activities (e.g., management, research, training, expertise) were practiced by a high proportion of nuclear medicine radiographers (51.4%), in contrast to therapeutic (25.4%) and diagnostic (18.9%) radiographers.
Almost all participants were working in the public sector (74.9%), almost equally distributed in university (n = 127) and non-university (n = 142) institutions; 25.1% worked in private or semi-private institutions (n = 90). In public institutions, radiographers provided frequently care to outpatients and inpatients almost equally (respectively 94.1% and 85.5%), in contrast with the private institutions (respectively, 97.8% and 31.1%).
3.2Prevalence and severity of WRMSDs symptoms
Based on the total of participants (n = 359), 94.7% presented WRMSDs symptoms in the last 12 months, and 67.7% in the last 7 days (Fig. 1). The main affected anatomical areas identified by radiographers in last 12 months were neck (73.0%), low back (67.4%), shoulders (55.7%) and upper back (44.9%) (Fig. 1).
Fig. 1
WRMSDs symptoms prevalence in radiographers during the last 12 months, last 7 days and work absence in last 12 months.
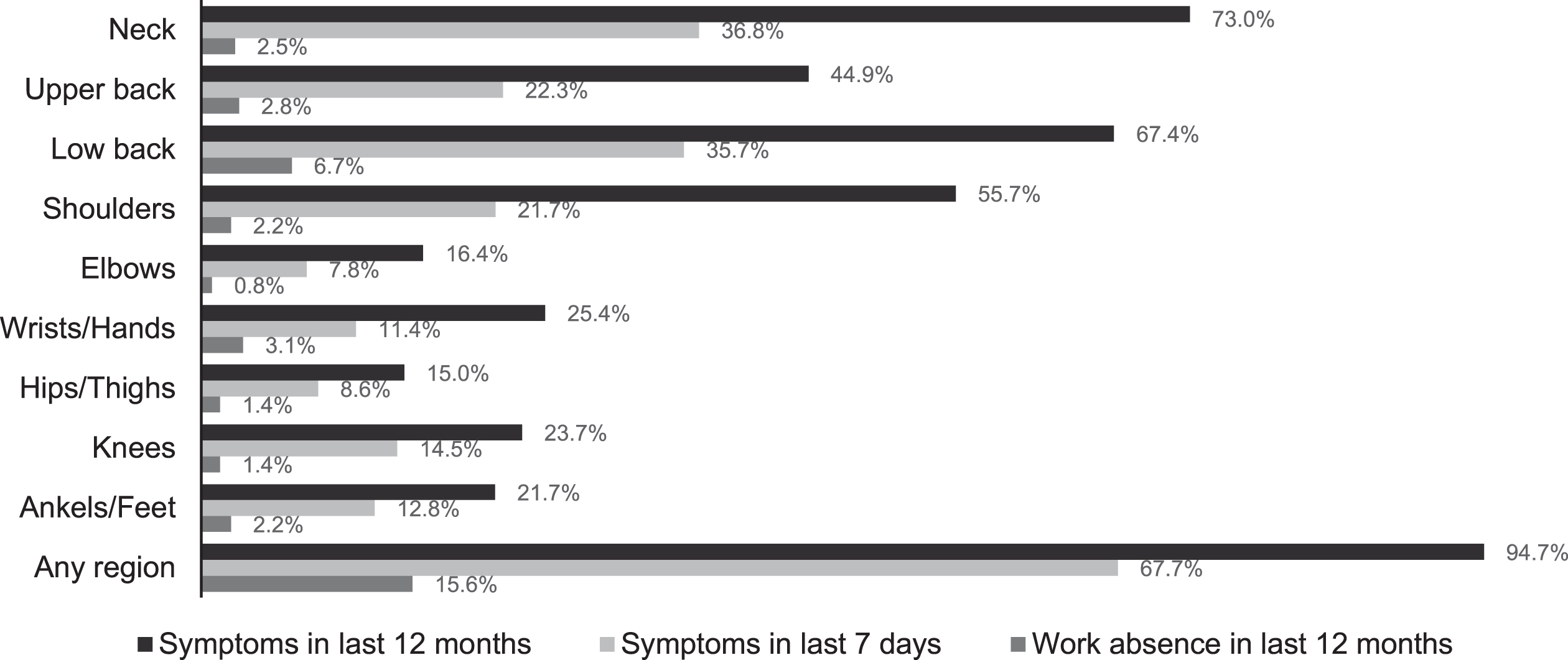
In last 7 days, the regions predominantly reported as painful were neck (36.8%), low back (35.7%), upper back (22.3%) and shoulders (21.7%) (Fig. 1). Amongst diagnostic radiographers, the most affected regions were neck, lower and upper back, while for MN and RT radiographers reported neck, low back and shoulders.
The assessment of the severity of the symptoms revealed that 15.6% (56/359) had a work absence in the last 12 months mainly due to pain in the low back region (6.7%), wrists/hands (2.8%) and upper back (2.8%) (Fig. 1). However, the anatomical regions with the longer absences were related to the elbows (202±154 days), shoulders (97±129 days) and neck (85±118 days). According to radiological field, the work absences were more frequent in nuclear medicine (Nuclear Medicine = 28.6%; Radiotherapy = 20.3%; Diagnostic = 12.8%) but were longer in diagnostic field (for any anatomical region).
The analysis of musculoskeletal symptoms, in terms of pain intensity in last 7 days, revealed that 49.9% of the total participants (179/359) suffer from moderate or severe pain intensity (corresponding to a pain ranging from 4 to 7 on the NPRS). Among symptomatic radiographers, the majority (from 50.0% to 80.0% depending on the anatomical regions and radiological field) had a peak of pain intensity from moderate to severe in the last 7 days. The pain intensity (median) was slightly higher for shoulders, wrists/hands, and low back.
Concerning the pain frequency in the previous 7 days, 40.9% of participants felt the symptoms in any anatomical region “often/every day” in the last 7 days. Among symptomatic radiographers, this number reached 76.1% of radiographers depending the on anatomical region. The anatomical regions most affected by the high frequency of pain were feet (76.1%), hands/wrists (65.9%), elbows (64.3%), hips/thighs (61.3%) and shoulders (51.3%) compared to other anatomical regions where the pain was “rarely/sometimes present”.
3.3Associations between WRMSDs symptoms and risk factors
Lower back was reported as the most affected anatomical region by the 68.8% of the radiographers that self-associated WRMSDs symptoms with imaging modalities/activities, except for laboratory activities where shoulders and wrists/hands were highlighted, and dosimetry and “other activities”, both mainly affecting the neck. The statistical tests showed that there was no significant differences between radiological fields in terms of WRMSDs symptoms (p > 0.05 for all anatomical regions in the last 12 months and 7 days). Since no association could be statistically demonstrated, data were analyzed for radiographers as a group for the two most affected anatomical regions in the last 12 months and 7 days, namely neck and low back. Only risk factors presenting a high probability (OR > 2) were described below. Other significant results are presented in Tables 1–4.
Table 1
WRMSDs symptoms in the neck significantly associated with risk factors (last 12 months)
| Risk factors | Categories | OR | 95% CI | P-value global test |
| Awkward postures | Never/Sometimes | 1.00 | ||
| Often/Always | 2.15 | 1.33–3.49 | 0.001 | |
| Physical environment | Totally/Mostly adequate | 1.00 | ||
| Totally/Mostly inadequate | 1.91 | 1.13–3.25 | 0.015 | |
| Workspace | Totally/Mostly adequate | 1.00 | ||
| Totally/Mostly inadequate | 1.82 | 0.99–3.34 | 0.050 | |
| Furniture | Totally/Mostly adequate | 1.00 | ||
| Totally/Mostly inadequate | 1.89 | 1.11–3.23 | 0.018 | |
| Autonomy in professional activity | Totally/Mostly agree | 1.00 | ||
| Totally/Mostly disagree | 1.87 | 1.03–3.39 | 0.035 | |
| Gender | Men | 1.00 | ||
| Women | 1.90 | 1.17–3.08 | 0.008 | |
| Diseases or health disorders | No | 1.00 | ||
| Yes | 2.22 | 1.26–3.92 | 0.005 |
Table 2
WRMSDs symptoms in the low back significantly associated with risk factors (last 12 months)
| Risk factors | Categories | OR | 95% CI | P-value global test |
| Awkward postures | Never/Sometimes | 1.00 | ||
| Often/Always | 2.86 | 1.78–4.58 | >0.001 | |
| Physical force | Never/Sometimes | 1.00 | ||
| Often/Always | 2.18 | 1.30–3.65 | 0.002 | |
| Radiological equipment | Totally/Mostly adequate | 1.00 | ||
| Totally/Mostly inadequate | 1.93 | 1.01–3.69 | 0.042 | |
| Not feeling anxiety/stress | Totally/Mostly agree | 1.00 | ||
| Totally/Mostly disagree | 1.80 | 1.11–2.91 | 0.016 | |
| Gender | Men | 1.00 | ||
| Women | 1.60 | 1.01–2.53 | 0.043 |
Table 3
WRMSDs symptoms in the neck significantly associated with risk factors (last 7 days)
| Risk factors | Categories | OR | 95% CI | P-value global test |
| Awkward postures | Never/Sometimes | 1.00 | ||
| Often/Always | 2.01 | 1.21–3.34 | 0.006 | |
| Physical force | Never/Sometimes | 1.00 | ||
| Often/Always | 2.03 | 1.09–3.77 | 0.023 | |
| Long/numerous reaches | Never/Sometimes | 1.00 | ||
| Often/Always | 1.84 | 1.10–3.05 | 0.018 | |
| Enough time to complete the volume of work | Totally/Mostly agree | 1.00 | ||
| Totally/Mostly disagree | 1.64 | 1.01–2.68 | 0.048 | |
| Not feeling anxiety/stress | Totally/Mostly agree | 1.00 | ||
| Totally/Mostly disagree | 2.00 | 1.20–3.34 | 0.007 | |
| Gender | Men | 1.00 | ||
| Women | 2.64 | 1.51–4.61 | >0.001 | |
| Diseases or health disorders | No | 1.00 | ||
| Yes | 1.80 | 1.07–3.02 | 0.025 |
Table 4
WRMSDs symptoms in the low-back significantly associated with risk factors (last 7 days)
| Risk factors | Categories | OR | 95% CI | P-value global test |
| Not feeling anxiety/stress | Totally/Mostly agree | 1.00 | ||
| Totally/Mostly disagree | 2.38 | 1.39–4.08 | 0.001 | |
| Gender | Men | 1.00 | ||
| Women | 1.96 | 1.12–3.41 | 0.016 | |
| Diseases or health disorders | No | 1.00 | ||
| Yes | 2.39 | 1.35–4.25 | 0.002 |
3.3.1WRMSDs symptoms in the last 12 months and risk factors
The chances of developing WRMSDs symptoms in the neck in the last 12 months were significantly high (OR >2) for radiographers working frequently in awkward postures during their occupational activities (OR = 2.15; 95% CI 1.33–3.49) and having previous health issues (OR = 2.22; 95% CI 1.26–3.92) (Table 1). Radiographers adopting frequently awkward postures and exerting frequently physical force to perform their activities had a higher probability (OR >2) of having symptoms in low back (respectively OR = 2.86; 95% CI 1.78–4.58 and OR = 2.18; 95% CI 1.30–3.65) (Table 2).
3.3.2WRMSDS symptoms in the last 7 days and risk factors
The effects of assuming awkward postures were considered significantly important for the neck (OR = 2.01; 95% CI 1.21–3.34), as well as exerting force frequently (OR = 2.03; 95% CI 1.09–3.77) or being a woman (OR = 2.64; 95% CI 1.51–4.61) (Table 3). The chance of having WRMSDs symptoms in low back was doubled for radiographers “feeling anxiety/stress at work” (OR = 2.38; 95% CI 1.39–4.08) and presenting previous health issues (OR = 2.39; 95% CI 1.35–4.25) (Table 4).
4Discussion
The findings of this study reveal that radiographers from Western Switzerland presented a set of musculoskeletal symptoms that they felt as related to work and workplace conditions/organization. A high prevalence of WRMSDs symptoms was observed in the last 12 months, affecting several anatomical regions: neck, low back, upper back, and shoulders. Similar results were also observed in other studies carried out internationally on radiographers and nurses with a prevalence of symptoms ranging from 67.0 to 98.3% [35–37]. Some differences, however, emerged regarding the affected anatomical regions, which may be explained by the specificities of each radiographer work context, such as occupational tasks demands and available resources, patient characteristics, radiological equipment manipulation, and work environment. Studies on 7-days prevalence of WRMSDs symptoms were missing concerning radiographers but it can be noted that the same anatomical regions remain affected during the last 12 months and 7 days (neck, low back, upper back, and shoulders). The consistency of symptoms over time suggests that modalities and/or tasks continuously performed by the radiographers stressed the same anatomical regions.
Musculoskeletal disorders affect radiographers’ general health but frequently also their professional practice, having as potential consequences loss of productivity, absenteeism, early retirement or in some cases the end of their career [38]. Since the WRMSDs symptoms presence and high pain severity induced a higher rate of absenteeism [13, 22, 36], it was expected that radiographers with these conditions would have also a high absenteeism, as observed (15.6%). Furthermore, pain intensity and frequency noted in this study were also indicators of WRMSDs severity since the length of absenteeism is typically proportional to the pain severity [36]. Results should be considered in the risk management and prevention strategies of WRMSDs to reduce the frequency and length of work absences. The impact of WRMSDs is not limited to the concerned radiographers since the loss of productivity and absenteeism impact all imaging department by increasing the workload and work pace to other radiographers to keep the department’s performance, which can create tensions and stress in the remaining team and, consequently an increased risk of new injuries [38].
In this study, almost 70% of participants self-associated musculoskeletal symptoms with imaging modalities practiced, being low back pain the most common symptom. An interesting exception was NM laboratory activity which was affecting mostly wrists/hands, suggesting that the manipulation of small and heavy equipment is demanding for this anatomical region. Since wrists/hands symptoms were not prevalent in this study, it may be important to take in account this observation into future prevention strategies: i) reduction of WRMSDS symptoms in general or ii) reduction of WRMSDs in a specific activity/imaging modality. Further research is needed for a better understanding since in Western Switzerland, radiographers can practice in more than one imaging modality.
Associative analyses highlighted some of ergonomic, physical, organizational/psychosocial risk factors, and radiographer gender as the main factors increasing the risk of WRMSDs in neck and low back, which is consistent with the multifactorial nature of these occupational health disorders [19, 22]. In this study, the risk of neck and low back injuries was increased by 2 ergonomic factors such as working in awkward postures and physical force demands. These factors have previously been identified as common sources of WRMSDs in radiographers [3, 16] since they need to handle the patient, the equipment, and respective accessories as part of their daily tasks. Inadequate physical environment, radiological equipment and furniture were also found as sources of neck and low back pain in last 12 months, which was expected since absence of adequate ergonomic conditions affects workers’ safety and health [39]. Besides ergonomic and physical risk factors, organizational/psychosocial factors were recognized as contributing and/or aggravating WRMSDs symptoms in healthcare workers, also in medical imaging departments [6, 18, 35, 40, 41]. Freimann et al. [42] identified work pace, low justice and respect in the workplace, influence on work organization, role conflicts and somatic stress as symptoms affecting WRMSDs occurrence in nurses, as Augner and Kaiser [18] did for depressive symptoms in radiographers. These earlier studies are in line with the present work, regarding the time allocated to complete the tasks, and mental health issues as anxiety/stress. The psychological load may be related to working on their own for most radiographers’ occupational activities (e.g., under patients’ pressure) and facing organizational constraints of workflow. High workload may be responsible for WRMSDs symptoms, dissatisfaction, and resentment of staff negatively impacting on patient safety [38]. This study results also evidenced a relation between radiographers’ WRMSDs symptoms in neck and low back with their individual characteristics, namely gender. Higher odds for women associations with WRMSDs symptoms shows the need of integrating this factor in the risk assessment, to have a successful prevention program [21, 37].
This work provides knowledge of Western Swiss radiographers that can be used by imaging departments, occupational health departments, health policies, and medical equipment designers to improve working conditions and to prevent workers’ healthcare risks. Indeed, the findings gave a WRMSDs symptoms baseline in terms of prevalence and severity, as well as the main risk factors. Occupational health prevention programs are especially important, since radiographers’ health outcomes are expected also to influence patient safety [43, 44]. Interventions could be initiated based on the study’s findings to address WRMSDs health problems and associated economic costs.
Nevertheless, further studies are needed to acquire a more comprehensive evaluation of the associations between the symptoms and specific tasks performed by radiographers, by imaging modality, similarly to other studies [32, 45]. To ensure a successful intervention based on the research results, all stakeholders must be included, mainly radiographers, since they are work experts in their professional activity, having an important role to play in solutions development and implementation success [44, 46], as well as the industry, designers and managers. An ergonomic approach could be used to improve working conditions since all risk factors dimensions need to be considered, mainly those that are conducting to the most prevalent symptoms.
One of the limitations of this study is related to the fact that the survey was disseminated only in French and only in Western Switzerland and it cannot be generalized to all Switzerland. The voluntary basis of the survey may have induced a non-response bias, which cannot be excluded since non-response analysis could not be performed due to lack of data. The survey was running during a pandemic period which could impact the response rate despite several reminders.
5Conclusions and recommendations
Radiographers work-related musculoskeletal disorders symptoms revealed to be an occupational health issue in Western Switzerland. The high prevalence of WRMSDs symptoms in the last 12 months (94.7%) and last 7 days (67.7%) affects predominantly neck, lower and upper back and shoulders. In terms of severity, there is a high absenteeism rate (15.6%), which may be related to the high pain intensity and frequency observed amongst participant radiographers. Working in awkward postures and exerting force frequently revealed to be the main risk factors significantly (p < 0.05) affecting neck and low back within the last 12 months, and neck and shoulders in the last 7 days (OR >2).
Radiographers stress and anxiety at work and being a woman radiographer were also risk factors for WRMSDs symptoms presence (OR >2).
Since WRMSDs symptoms affect healthcare workers’ general health, the quality of care and patient safety can suffer impacts, being important to make all stakeholders aware of this problem. These results contribute to understanding the relationships between work demands and radiographers health that allow emphasizing the need of improving work conditions, providing a safe environment, and reducing the risk of occupational injuries. Furthermore, considering the multifactorial nature of WRMSDs, prevention programs are needed to reduce or eliminate occupational risk factors, decreasing the prevalence of WRMSDs symptoms amongst radiographers. Further studies are required to attain a better understanding of the issues and to complete the findings for Swiss radiographers.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgments
We wish to acknowledge and thank Mr. Patrick Vorlet, President of the Western Swiss Section of Radiographers’ Professional Association (SR-ASTRM) and Mr. Frédéric Zoni, media coordinator and member of the editorial board of the same association, for their help in divulging the survey. Many thanks to all the members of CCTRM, chief radiographers who shared the survey with their collaborators, as well as to all radiographers who agreed to participate in this study.
Funding
The present publication was funded by Fundação Ciência e Tecnologia, with IP national support through CHRC (UIDP/04923/2020).
References
[1] | Luttmann A , Jäger M , Griefahn B , Caffier G , Liebers F . La Prévention des troubles musculo-squelettiques sur le lieu de travail. Genève: Organisation Modial de la Santé; (2004) [cited 2020 Fev 4]. Available online: https://apps.who.int/iris/handle/10665/42802. |
[2] | Daniel SV , Umar MS , Ahmad NM , Joseph ZD . Work-related musculoskeletal disorders: Revalence among clinical radiographers in teaching hospitals in North-Western Nigeria. J Radiogr Radiat Sci. (2018) [cited 2020 May 2];32: (1):57–63. Available from: https://www.researchgate.net/publication/325345157_Work-Related_Musculoskeletal_Disorders_Prevalence_Among_Clinical_Radiographers_in_Teaching_Hospitals_in_North-Western_Nigeria |
[3] | Lorusso A , Bruno S , L’Abbate N . Musculoskeletal complaints among Italian X-ray technologists. Ind Health. (2007) [cited 2020 Nov 17];45: (5):705–8. Available from: https://doi.org/10.2486/indhealth.45.705 |
[4] | Tinetti CJ , Thoirs K . Prevalence, risks, underlying mechanisms, preventative guidelines, and interventions of sonographer work-related injuries: A literature review. Sonography. (2019) [cited 2020 Dec 17];6: (4):164–77. Available from: https://doi.org/10.1002/sono.12187 |
[5] | Griffin H . Work-related musculoskeletal disorders in radiation therapists: An exploration of self-reported symptoms. Master thesis, Ohio State University, Ohio State, (2018) . |
[6] | Pompeii LA , Lipscomb HJ , Dement JM . Surveillance of musculoskeletal injuries and disorders in a diverse cohort of workers at a tertiary care medical center. Am J Ind Med. (2008) [cited 2020 Dec 17];51: (5):344–56. Available from: https://doi.org/10.1002/ajim.20572 |
[7] | Kumar S , Moro L , Narayan Y . Morbidity among X-ray technologists. Int J Ind Ergon. (2004) [cited 2020 Fev 20];33: (1):29–40. Available from: https://doi.org/10.1016/j.ergon.2003.06.002 |
[8] | Evans K , Roll S , Baker J . Work-Related musculoskeletal disorders (WRMSD) among registered diagnostic medical sonographers and vascular technologists. Journal of Diagnostic Medical Sonography. (2009) [cited 2020 Fev 20];25: (6):287–99. Available from: https://doi.org/10.1177/8756479309351748 |
[9] | Ransom E . The causes of musculoskeletal injury amongst sonographers in the UK. Society of Radiographers. (2002) [cited 2020 Fev 20]. Available online: https://www.soundergonomics.com/pdf/SCOR-MSI_Book.pdf |
[10] | Hanania AN , Cook A , Threadgill MP , Conway SH , Ludwig M . Prevalence of musculoskeletal work-related injuries among radiation therapists [Abstract]. Radiologic Technology. (2020) [cited 2020 Fev 20];91: (5). https://doi.org/10.1016/S0360-3016(19)30510-3 |
[11] | Alhasan M , Abdelrahman M , Alewaidat H , Almhdawi K , Nazzal M . Work-related stress, musculoskeletal disorder complaints, and stress symptoms among radiographers in the northern part of jordan. J Med Imaging Radiat Sci. (2014) [cited 2020 Mar 20];45: (3):291–8. Available from: https://doi.org/10.1016/j.jmir.2014.04.002 |
[12] | Hulls PM , Money A , Agius RM , de Vocht F . Work-related ill-health in Radiographers. Occup Med. (2018) [cited 2020 Fev 15];68: (6):354–9. Available from: https://doi.org/10.1093/occmed/kqy076 |
[13] | Maumet S , De Gaudemaris R , Caroly S , Balducci F . Facteurs associés à la prévalence des troubles musculo-squelettiques en milieu hospitalier. Arch Mal Prof Enviro. (2005) [cited 2019 Dec 21];66: (3):236–43. Available from: https://doi.org/10.1016/S1775-8785(05)79088-3 |
[14] | Siegal DS , Levine D , Siewert B , Lagrotteria D , Affeln D , Dennerlein J , Boiselle PM . Repetitive stress symptoms among radiology technologists: Prevalence and major causative factors. J Am Coll Radiol. (2010) [cited 2019 5 Dec];7: (12):956–60. Available from: https://doi.org/10.1016/j.jacr.2010.05.024 |
[15] | Costa S , Oliveira E , Reis C , Viegas S , Serranheira F . Mammography equipment design: Impact on radiographers’ practice. Insights into Imaging. (2014) [cited 2019 5 Dec];5: (6):723–30. Available from: https://doi.org/10.1007/s13244-014-0360-2 |
[16] | Kumar S , Moro L , Narayan Y . Perceived physical stress at work and musculoskeletal discomfort in X-ray technologists. Ergonomics. (2004) [cited 2020 Jan 22];47: (2):189–201. Available from: https://doi.org/10.1080/00140130310001617958 |
[17] | Fisher TF . Radiologic and sonography professionals’ ergonomics: An occupational therapy intervention for preventing work injuries. Journal of Diagnostic Medical Sonography. (2015) [cited 2020 Jan 22];31: (3):137–47. https://doi.org/10.1177/8756479315580020 |
[18] | Augner C , Kaiser G . Predictors of musculoskeletal symptoms in radiology technologists in Austria, Europe. Work. (2019) [cited 2020 Nov 17];64: (4):853–8. Available from: https://doi.org/10.3233/WOR-193047 |
[19] | European Occupational Safety and Health Administration. Discussion paper musculoskeletal disorders in the healthcare. (2020) [cited 2020 Oct 2]. Available online: https://osha.europa.eu/en/publications/musculoskeletal-disorders-healthcare-sector/view |
[20] | Verrier W , Harvey J . An investigation into work related stressors on diagnostic radiographers in a local district hospital. Radiography. (2010) [cited 2020May12];16: (2):115–24. Available from: https://doi.org/10.1016/j.radi.2009.09.005 |
[21] | Delalande-Danet V , Desarmenien A , Incorvaïa A-M , Letheux C , Leviel C , Viossat M . Les Troubles Musculo-Squelettiques. Paris, France; (2015) [cited 2020 Mar 14]. Available online: https://www.presanse.fr/wp-content/uploads/2019/02/GUIDE-TMS-23-06-2015-Version-de-consultation.pdf |
[22] | European Occupational Safety and Health Administration. Work-Related Musculoskeletal Disorders: Prevalence, Costs and Demographics in the European Union. (2019) [cited 2020 Apr 20]. Available online: https://healthy-workplaces.eu/en/tools-and-publications/publications/work-related-musculoskeletal-disorders-prevalence-costs-and |
[23] | Sousa Uva A , Serranheira F . Saúde do trabalhador: Ergonomia e segurança do paciente. In Sousa P, Mende W, (Eds.), Segurança do Paciente: Criando organizações de saúde seguras (Rio de Jan). Fiocruz. (2014) [cited 2020 Apr 20]. Available online: https://doi.org/10.7476/9788575415948.0008 |
[24] | Swiss conference of cantonal health directors, Swiss national health work organization. Besoins en effectifs dans les professions de la aanté - Rapport national 2016. Bern, Switzerland; (2016) [cited 2020 May 8]. Available online: https://www.gdk-cds.ch/fileadmin/docs/public/gdk/themen/gesundheitsberufe/nichtun._gesundheitsberufe/versorgungsbericht/versorgungsbericht_2016-fr-v1.8-web.pdf |
[25] | Lehmann P , Meystre NR , Mamboury N . Analyse dumarché du travail des techniciens en radiologie médicale en Suisse en 2011: Sur mandat de l’association suisse des techniciens en radiologie médicale ASTRM. Lausanne, Switzerland; (2012) [cited 2020 Jun 20]. Available online: https://www.astrm.ch/files/Dokumente/Verband/Projekte/rapport_econcept.pdf |
[26] | Eslick GD , Raj VV . Occupational stress amongst radiographers: Does working in private or public practice make a difference? Radiography. (2002) [cited 2020 Feb 8];8: (1):47–53. Available from: https://doi.org/10.1053/radi.2001.0356 |
[27] | Descatha A , Roquelaure Y , Aublet-Cuvelier A , Ha C , Touranchet A , Leclerc A . Validité du questionnaire de type “Nordique” dans la surveillance des pathologies d’hypersollicitation du membre supérieur. Documents pour leMédecin du Travail, 2007, pp. 509–17. Inserm-00232629 |
[28] | López-Aragón L , López-Liria R , Callejón-Ferre Á-J , Gómez-Galán M . Applications of the standardized nordic questionnaire: A Review. Sustainability. (2017) cited 2020 Feb 8];9: (1514):1–42. Available from: https://doi.org/10.3390/su9091514 |
[29] | Kuorinka I , Jonsson B , Kilbom A , Vinterberg H , Biering-Sørensen F , Andersson G , Jørgensen K . Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon. (1987) [cited 2019 Dec 11];18: (3):233–7. Available from: https://doi.org/10.1016/0003-6870(87)90010-x |
[30] | Forcier L , Lapointe C , Beaugrand S , Lortie M , Kuorinka I , Buckle P . Questionnaire Sur La Santé Musculo-Squelettique Des Travailleurs Issu Du Questionnaire Nordique. Institut de recherche Robert-Sauvé en santé et en sécurité du travail; (2001) [cited 2020 Fev 22]. Available online: http://www.irsst.qc.ca/media/documents/pubirsst/rg1-270.pdf?i=0&redirected=1 |
[31] | Mesquita CC , Ribeiro JC , Moreira P . Portuguese version of the standardized Nordic musculoskeletal questionnaire: Cross cultural and reliability. J Public Health. (2010) [cited 2019 Dec 18];18: :461–6. Available from: https://doi.org/10.1007/s10389-010-0331-0 |
[32] | Serranheira F , Cotrim T , Rodrigues V , Nunes C , Sousa-Uva A . Lesões musculoesqueléticas ligadas ao trabalho em enfermeiros portugueses: «ossos do ofício» ou doenças relacionadas com o trabalho? Rev Port Saude Publica. (2012) [cited 2020] |
[33] | Nawrocka A , Mynarski W , Powerska-Didkowska A , Grabara M , Garbaciak W . Musculoskeletal pain among Polish music school students. Med Probl Perform Art. (2014) [cited 2020 Jun 3];29: (2):64–9. Available from: https://doi.org/10.21091/mppa.2014.2015 |
[34] | Sullivan GM , Artino AR Jr . Analyzing and interpreting data from likert-type scales. J Grad Med Educ. (2020) ; [cited 2020 Jul 11];5: (4):541–2. Available from: https://doi.org/10.4300/JGME-5-4-18 |
[35] | Boocock MG , Trevelyan F , Ashby L , Ang A , Diep N , Teo S , Lamm Felicity. The influence of psychosocial and patient handling factors on the musculoskeletal health of nurses. In: Bagnara S, Tartaglia R, Albolino S, Alexander T, Fujita Y, editors. Proceedings of the 20th Congress of the International Ergonomics Association (IEA 2018). Cham: Springer International Publishing; (2018) [cited 2019 Dec 14]. pp. 596–603. Available from: https://doi.org/10.1007/978-3-319-96083-8_78 |
[36] | Magnago TSB , Lima ACS , Prochnow A , da Silva Ceron MD , Tavares JP , Souza Urbanetto J . Intensidade da dor musculoesquelética e a (in)capacidade para o trabalho na enfermagem. Rev Lat Am Enfermagem. (2012) [cited 2020 Sep 17];20: (6):1125–33. Available from: https://doi.org/10.1590/S0104-11692012000600015 |
[37] | Ribeiro T , Serranheira F , Loureiro H . Work related musculoskeletal disorders in primary health care nurses. Appl Nurs Res. (2017) [cited 2020 Nov 17];33: :72–7. Available from: https://doi.org/10.1016/j.apnr.2016.09.003 |
[38] | Pallotta OJ , Roberts A . Musculoskeletal pain and injury in sonographers, causes and solutions. Sonography. (2017) [cited 2020 Nov 17];4: (1):5–12. Available from: https://doi.org/10.1002/sono.12093 |
[39] | World Health Organization. Healthy Workplaces: A Model for Action for Employers, Workers, Policy-Makers and Practitioners. (2010) [cited 2020 Oct 17]. Available online: https://apps.who.int/iris/bitstream/handle/10665/44307/9789241599313_eng.pdf?sequence=1&isAllowed=y |
[40] | Bos E , Krol B , van der Star L , Groothoff J . Risk factors and musculoskeletal complaints in non-specialized nurses, IC nurses, operation room nurses, and X-ray technologists. Int Arch Occup Environ Health. (2007) [cited 2020 Nov 19];80: (3):198–206. Available from: https://doi.org/10.1007/s00420-006-0121-8 |
[41] | Oakman J , Macdonald W , Wells Y . Developing a comprehensive approach to risk management of musculoskeletal disorders in non-nursing health care sector employees. Appl Ergon. (2014) [cited 2020 Dec 15];45: (6):1634–40. Available from: https://doi.org/10.1016/j.apergo.2014.05.016 |
[42] | Freimann T , Pääsuke M , Merisalu E . Work-related psychosocial factors and mental health problems associated with musculoskeletal pain in nurses: A cross-sectional study. Pain Res Manag. (2016) [cited 2020 Dec 3];2016: :9361016. Available from: https://doi.org/10.1155/2016/9361016 |
[43] | Sikorski J . Connecting worker safety to patient safety: A new imperative for health-care leaders. Ivey Business J. (2009) [cited 2020 May 19]. Available online: https://iveybusinessjournal.com/publication/connecting-worker-safety-to-patient-safety-a-new-imperative-for-health-care-leaders/ |
[44] | Carayon P , Alvarado CJ , Schoofs Hundt A . Work design and patient safety. Theor Issues Ergon Sci. (2007) [cited 20201 Jan 5];8: (5):395–428. Available from: https://doi.org/10.1080/14639220701193157 |
[45] | Ribeiro L , Bodião I , Lesyuk O , Abrantes AF , Almeida RPP , Pinheiro JP . Work-place related ergonomic conditions as prognostic factors for work-related musculoskeletal disorders (WRMD) in radiographers [Poster]. Pap Present EPOSTM - Electron Present Online Syst. (2016) [cited 2019 Dec 21]. Available from: https://doi.org/10.1594/ecr2016/B-1006 |
[46] | Burgess-Limerick R . Participatory ergonomics: Evidence and implementation lessons. Appl Ergon. (2018) [cited 2020 Dec10];68: :289–93. Available from: https://doi.org/10.1016/j.apergo.2017.12.009 |




