A systematic review of work-related interventions for breast cancer survivors: Potential contribution of occupational therapists
Abstract
BACKGROUND:
A high number of breast cancer survivors need to resume work. Therefore, interventions aimed at effective work-related transitions are important.
OBJECTIVE:
A systematic review to determine what occupational therapy interventions are effective in work-related transitions of breast cancer survivors.
METHODS:
Multiple databases were searched for studies on work-related interventions within the scope of occupational therapy. Studies were included if 70% or more study participants were working age (> 18 years) breast cancer survivors, and work-related transition outcome measures were used.
RESULTS:
The search yielded 2 872 articles, of which 12 met the inclusion criteria. When classified according to the International Classification of Function Framework, quantitative sources focussed on Body Structures and Functions component and Multicomponents (consists of the Body Structures and Functions Component and the Activities Component) showed positive effects on improving the work-related transitions of BC survivors, however, the effects were statistically insignificant and the strength of evidence was moderate. Participants in a qualitative source reported that after they underwent a physical exercise programme their work performance improved. A Multicomponents intervention study showed statistically significant improvements on self-reported work-related outcomes of BC survivors. Low evidence was found for implementing a vocational rehabilitation case management programme targeting the Activities component, which showed positive effects in reducing the sick leave days of BC survivors, but the effects were statistically insignificant. No evidence was found for programmes focussed on restoring the Participation component.
CONCLUSION:
The evidence included in this systematic review were insufficient to recommend occupational therapy interventions that are effective (showing statistically significant improvements) for work-related transitions of BC cancer survivors.
1Introduction
The largest proportion of the population of cancer survivors worldwide are breast cancer survivors, with a five-year survival rate of between 70% and 90% [1]. Improved treatment regimens and screening for breast cancer have globally led to an increased survival rate, and breast cancer is beginning to be recognised as a chronic disease [2]. A high number of breast cancer survivors need to resume work as most women diagnosed with breast cancer are of pre-retirement age [3, 4]. Therefore, interventions aimed at effective work-related transitions are increasingly important.
The diagnosis and treatment of breast cancer can have emotional, physical, psychological, social, and existential consequences, including fear of recurrence, cognitive impairments, lymphoedema, limited range of motion and strength in upper limbs, and chronic pain [5–8]. Breast cancer survivors need to cope with anxiety, fatigue, diminished work and social participation, and reduced quality of life [8]. As a result of these challenges, breast cancer survivors experience limitations in work performance and participation [9]. Work-related transitions such as the period required to resume work, work absenteeism, and employment status are concerns of breast cancer survivors [7, 10]. Many breast cancer survivors who do return to professional activity report difficulties in coping with symptoms at work, lack of self-confidence, feeling less capable to perform their jobs, as well as declining career prospects [11].
A systematic review which included 23 articles was conducted by Tamminga, De Boer, Verbeek, and Frings-Dresen [12] and published in 2010. The study aim was to review literature on the content of interventions focusing on the resumption of work, employment, or work retention of cancer survivors. The study suggests that employers, managers, and co-workers have a limited grasp of the psychosocial and physical barriers that cancer survivors face. This leads to poor communication, little managerial proficiency, and insufficient support for work-related transitions [13]. The inadequate organisational understanding underscores the need for advice on how to manage cancer survivors in the workplace [14, 15]. Breast cancer survivors also experience a lack of work schedule flexibility and support by health care workers to assist them with the transition back into the work environment [16].
A conceptual practice model for occupational therapy to facilitate the return-to-work of breast cancer survivors, shows that interventions should be person-centred, involve a multidisciplinary team, be based on The International Classification of Functioning, Disability and Health Framework (ICF), and use evidence-based practice [14]. The main goal of occupational therapy is to assist people to maintain and/or restore their daily activity participation in life domains such as selfcare, leisure, and productivity, which includes work [17]. This goal is in line with the globally recognised ICF Framework, which ultimately underscores the importance of participation in activities of daily living for health and wellbeing [18]. Occupational therapy provided as part of a multidisciplinary rehabilitation programme can have a remarkable impact on the quality of life of breast cancer survivors [17], because of its focus on activity participation in meaningful life roles such as the worker role [20].
Occupational therapy could have a positive effect on facilitating the resumption or maintenance of work by breast cancer survivors, but is not yet widely available [21]. More evidence is required to confirm the effectiveness of occupational therapy interventions for work-related transitions of breast cancer survivors. Should occupational therapy interventions in this context prove effective, the accessibility of these services must be considered.
A systematic review published in 2011 by Désiron, De Rijk, Van Hoof, and Donceel [22] comprising of six studies on occupational therapy and return-to-work, recommend including occupational therapy in multidisciplinary rehabilitation when targeting return-to-work. The recommendation was based on improved results achieved when rehabilitation focuses on functionality and participation using occupational therapy [22].
The aim of this systematic review is to determine what occupational therapy interventions are effective in work-related transitions of breast cancer survivors. A systematic review was decided on, since to our knowledge, no such review has been done in this field of research.
2Methods
2.1Protocol and registration
The Preferred Reporting Items for Systematic Review and Meta-analysis Protocol (PRISMA-P) guidelines were followed in designing this systematic review [23, 24]. Upon completing the protocol, it was registered with the International Prospective Register of Systematic Reviews (PROSPERO), no. CRD42020207410.
2.2Eligibility criteria
2.2.1Types of studies
Qualitative and quantitative primary research studies published in English and discussing work-related interventions for breast cancer survivors within the scope of occupational therapy were included in this review. Although randomised controlled trial (RCT) design studies are preferred for determining the effectiveness of interventions, and more highly regarded in systematic reviews than other designs, this design may not be the most appropriate design for work interventions [25, 26]. Therefore, the researchers also included other study designs. Qualitative research was also included as it provides contextual information which is indispensable [27]. Studies published from the inception of databases until the search date were included, as well as grey literature.
2.2.2Type of participants
Studies were included if 70% or more of the study participants were working age (> 18 years) breast cancer survivors.
2.2.3Types of interventions
Work-related interventions within the scope of occupational therapy (even if not offered by an occupational therapist) were included, such as vocational education and rehabilitation. No limits were placed on the setting of service rendering. Sources focussing on the effect of medical and pharmacological interventions, such as surgical interventions, radiation or chemotherapy, on the work-related transitions of breast cancer survivors were excluded.
2.2.4Types of outcome measures
Work-related transition outcome measures, e.g. a) employment status, b) return-to-work, c) absenteeism, d) time spent on work disability or sick leave, e) work performance (e.g. productivity), and f) work motivation and satisfaction.
2.3Information sources and search strategy
A search strategy was designed with the assistance of an expert librarian. The search was conducted during July and August 2020. EBSCOhost, Cochrane Library, Web of Science, PubMed (Medline), Scopus, OTseeker, and grey literature (National ETD Portal, NDLTD, OATD, OpenDOAR, Sabinet) were searched for articles (title and abstract) by the primary researcher (LS). Search terms in the following areas were used: work-related transitions, occupational therapy interventions, vocational rehabilitation, and breast cancer. Search strings were formulated and adapted per database and included: exploded MeSH terms, Boolean operators, synonyms, lay and medical terminology, and truncation. Refer to Supplementary File 1 for the PubMed database search string. Pearling was used to find articles that may have been overseen in the database searches.
2.4Selection process
Search results were uploaded into an Excel spreadsheet, which included the search date, database name, years covered, search terms, any restrictions or limitations, and number of hits. The articles returned from the search were imported into the Mendeley Reference Management Application and duplicate articles were identified and removed. LS screened the title and abstract using the eligibility criteria to identify and select the articles to be included in the full-text review stage.
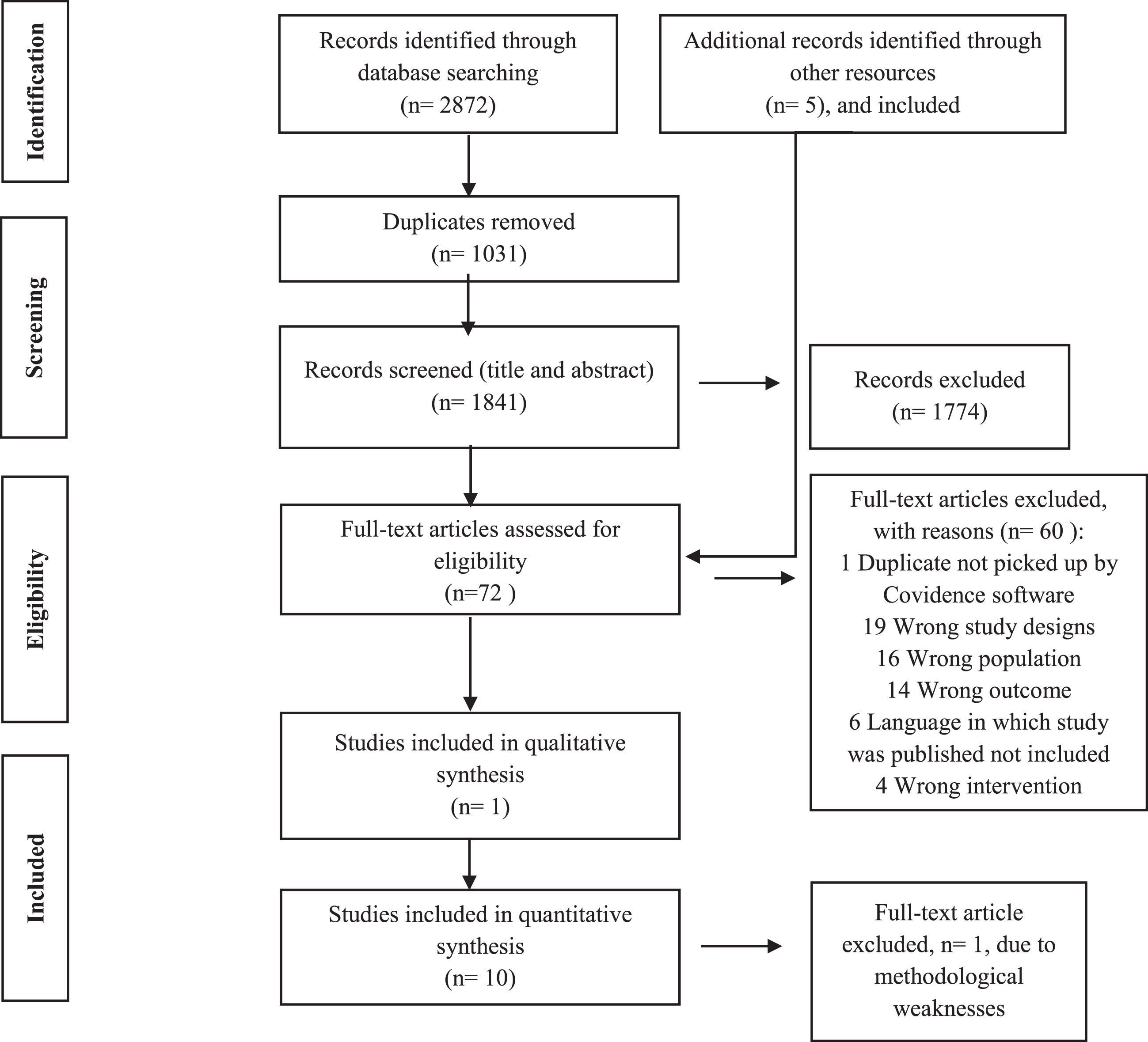
The full text articles were uploaded to the online Covidence Systematic Review Management Program (http://www.covidence.org), and screened by LS and a second reviewer (MH). Disagreements were resolved through discussion with a third reviewer (LvN). The search and selection process, as well as reasons for exclusion at full-text selection stage are indicated in the PRISMA Flow Diagram (Fig. 1).
Fig. 1
PRISMA Flow Diagram.
2.5Data extraction and assessment of methodological quality of studies included
LS extracted and captured data from included studies on two customised forms (Study Characteristics Table and Study Findings Table), adapted from a Standardised Evidence Table (Supplementary File 2). LvN cross-checked 50% of the extracted data to ensure accuracy. LS contacted study authors via email to clarify existing data and to request additional data.
The methodological quality of the included quantitative studies was assessed using three processes, according to the Guidelines for Conducting Systematic Reviews [28], compiled by the American Occupational Therapy Association (AOTA). This included a risk of bias assessment, level of evidence assessment, and strength of evidence assessment. The risk of bias assessment was done by LS and MH, drawing upon: A Revised Tool for Assessing Risk of Bias in Randomised Controlled Trials (RCT) and Non-RCT [29] as well as the Quality Assessment Tool for Pre-Post studies with No Control Group [30] (Supplementary File 3). The risk of bias in the individual studies was reported as low, moderate, or high in the Study Characteristics Table. The level of evidence was assessed by LS, using the OCEBM Levels of Evidence [31] (Table 1). The strength of evidence was assessed by LS, using the guidelines of the U.S. Preventive Services Task Force [32] (Table 2).
Table 1
Levels of evidence (OCEBM Levels of Evidence Working Group)
| Level | Type of evidence |
| 1A | Systematic review of homogeneous RCTs (similar population, intervention, etc.) with or without meta-analysis. |
| 1B | Well-designed individual RCT (not a pilot or feasibility study with a small sample size). |
| IIA | Systematic review of cohort studies. |
| IIB | Individual prospective cohort study, low quality RCT (e.g., < 80% follow-up or low number of participants; pilot and feasibility studies); ecological studies; and two-group, non-randomized studies. |
| IIIA | Systematic review of case-control studies. |
| IIIB | Individual retrospective case-control study, one-group, non-randomised pre-post-test study; cohort studies. |
| IV | Case series. |
| V | Expert opinion without explicit critical appraisal. |
Note. RCT –Randomised Controlled Trial. From OCEBM Levels of Evidence Working Group. (2011). The Oxford Levels of Evidence Oxford Centre for Evidence-Based Medicine.
Table 2
Strength of evidence
| Strength | Description |
| Strong | •Two or more Level 1A/B studies. |
| •The available evidence usually includes consistent results from well-designed, well-conducted studies. | |
| Moderate | •At least Level 1A or Level 1B high-quality study or multiple moderate quality studies (Level 2A/B, Level 3A/B). |
| •The available evidence is sufficient to determine the effects on health outcomes, but confidence in the estimate is constrained by factors such as: | |
| –The number, size, or quality of individual studies. | |
| –Inconsistency of findings across individual studies. | |
| •As more information (other research findings) becomes available, the magnitude or direction of the observed effect could change, and this change may be large enough to alter the conclusion related to the usefulness of the intervention. | |
| Low | •Small number of low-level studies and flaws in the studies. |
| •The available evidence is insufficient to assess effects on health and other outcomes of relevance to occupational therapy. Evidence is insufficient because of: | |
| –The limited number or size of studies; | |
| –Important flaws in study design or methods; | |
| –Inconsistency of findings across individual studies; or | |
| –Lack of information on important health outcomes. | |
| •More information may allow estimation of effects on health and other outcomes of relevance to occupational therapy. |
Note. The strength of evidence is based on the guidelines of the U.S. Preventive Services Task Force.
The methodological quality of the one and only qualitative research study included in the review, was appraised by LS, MH, and LvN, using The JBI Critical Appraisal Checklist [33] (Supplementary File 4).
2.6Data synthesis
The OCEBM Levels of Evidence were used to organise the data in the Study Findings Table. The components of the International Classification of Function, Disability and Health Framework (ICF/ICIDH) were used to organise the Study Characteristics Table. Initially we planned to synthesise and thematically report the study findings based on the type of intervention, but due to the multicomponent intervention programmes applied in the studies, this was not possible. Instead, the studies were collated by making use of the ICF Framework. Thus, the research studies’ findings were synthesised and discussed under the components of: Body Structures and Functions, Multicomponents (Body Structures and Functions, and Activities), Activities, and Participation. Given the heterogeneity of the participants (with regard to medical treatment received), interventions, and outcome measures of the studies, statistically collating data in the form of a meta-analysis was not appropriate for this review.
The strength of evidence, as proposed by the U.S. Preventive Services Task Force [32], for implementing a specific intervention programme focused on Body Structures and Functions, Multicomponents (Body Structures and Functions, and Activities), Activities, and Participation, was respectively discussed to indicate what occupational therapy interventions are effective in work-related transitions for breast cancer survivors (Table 2).
3Results
3.1Study selection and quality appraisal
The literature search yielded a total of 2 872 titles (EBSCOhost: 497; Cochrane Library: 1; Medline: 490; Scopus: 925; Web of Science: 788; OTseeker: 13; and various grey literature: 158) for screening. Of these titles, 1 031 duplicates were identified and removed by using Mendeley and Covidence Data Management Programs. The title and abstract of the remaining 1 841 articles were screened by LS using the eligibility criteria. 1 774 articles were removed as ineligible. LS retrieved the full text of the remaining articles. Pearling of the included full-text articles was done by LS, and five additional articles were included. LS and MH screened 72 full-text articles. 60 articles were excluded for the reasons as indicated in the PRISMA Flow Diagram (Fig. 1).
Of the 12 included articles, three studies were level I evidence studies (three RCTs) [34–36], five studies were level II evidence (one non-RCT, one prospective cohort study and three pilot RCTs) [37–41], two were level III evidence (one pre-and-post-test study and one longitudinal prospective study using a one-group design) [42, 43], and one was a qualitative study [44]. One level V study [45] was excluded after the methodological appraisal of the article, due to the methodological weaknesses present.
The risk of bias assessments are depicted in the tables in Supplementary File 4. Altogether six RCT and non-RCT studies had a moderate risk of bias [34–36, 38, 39, 41]. One RCT [40] had a low risk of bias, and a prospective cohort study published 40 years ago, [37] had a moderate risk of bias. A pre-and-post-test study [43] had a low risk of bias, and one longitudinal prospective study using a one group design had a moderate risk of bias [42]. The qualitative study [44] included in the review met the methodological criteria of the JBI Critical Appraisal Checklist, and was therefore included in the review.
3.2Characteristics of included studies
All 11 studies were conducted in high income countries: four in the Netherlands, three in Sweden, two in the United States of America, two in the United Kingdom, and one in Canada. The articles were published between 1977 and 2018.
Of the 11 studies, nine were conducted in a clinical setting of which seven were in hospital [34, 35, 37, 38, 40, 42, 43] and two at a wellness/medical centre [41, 44]. One study was run at a holiday resort [36]. One study [39] did not clearly indicate the intervention setting. The RCT by Maguire, Brooke, Tait, Thomas, and Sellwood [34] also included a home visit. Two intervention studies [39, 41] recommended a home programme.
Participants included in the studies were working age women diagnosed with primary breast cancer. The sample sizes of the studies ranged from 10–863 participants. Most of the studies included participants who had undergone a mastectomy [34, 35, 37, 38, 40, 42]. Two studies were conducted with participants who were being treated with chemotherapy [43, 44]. Ibrahim, Muanza, Smirnow, Sateren, Fournier, Kavan et al. [41] specifically included young breast cancer survivors (aged between 18 and 45 years) scheduled for post-operative radiation therapy. The Björneklett study [36] included breast cancer survivors that had undergone surgical intervention and/or were undergoing chemotherapy. The study by Rogers, Hopkins-Price, Vicari, Pamenter, Courneya, Markwell et al. [39], included breast cancer survivors on hormonal therapy and who were expected to remain on hormonal therapy for the duration of the study.
Interventions were provided by various health care providers, solely or as part of a multidisciplinary team. These included a specialist/oncology nurse [34, 35, 37, 38]; oncologist [35, 36, 38]; social worker [36, 37, 42]; physical therapist [37, 42, 43]; psychologist [35, 39]; volunteer worker [37, 42]; physical trainer [35]; dietician [35]; vocational rehabilitation case manager [40]; masseuse [36]; personal trainer in qigong and mental visualisation [36]; exercise specialist [39]; exercise physiologist [41]; and oncological occupational physician [43].
The majority of the studies included in the review [34, 35, 37–39, 41, 42], did not have work-related outcomes as their primary objective. Self-reported resumption of work and/or sick leave were used as additional outcome measures in these studies whose primary outcome measures were mainly focused on the component of Body Structures and Functions, such as range of motion, muscle strength, and pain. Self-reported work or resumption of work [29, 36] and/or sick leave days [36, 40] were used by the remaining studies as primary outcome measures. Alongside resumption of work, the Leensen study [43] used work-related self-report questionnaires (Return-to-Work Self-Efficacy Scale, rating importance of work using the Visual Analogue Scale, Work Ability Index, and Work Limitations Questionnaire). The qualitative study by Groeneveld [44] included work and work performance as a topic of discussion in the semi-structured interviews after participants completed an intervention programme.
Only four [35, 36, 40, 42] of the 11 studies included in the review were designed and implemented based on theoretical foundations, for example the Rogers study made use of the cognitive theory [39]. In the absence of a theoretical foundation for an intervention, it is difficult to draw a connection between the intervention components and the outcome benefits thereof [46]. A systematic review of reviews on return-to-work and breast cancer by Cocchiara, Sciarra, D’Egidio, Sestili, Mancino, Backhaus et al. in 2018 [13], also highlighted the absence of theoretical foundations for interventions, as a common limitation among intervention studies.
3.3Interventions
The ICF Framework is recommended by the World Health Organisation (WHO) to be used within health sectors globally [18]. This framework takes into account global concerns of disability and function. The ICF Framework was used to discuss the study findings according to the component the intervention programme focused on, namely Body Structures and Functions, Activities, and Participation. The components are defined in the practice manual for using the ICF Framework, as drafted by the WHO [47], as follows: a) Body Structures and Functions combined are anatomical parts of the body (e.g. limbs) and their components are considered as body structures (e.g. muscle strength) and physiological body functions (e.g. lymphatic system); b) An activity is the execution of a task or action by a person, which differs from participation in that the effect of the context is irrelevant or absent. For the purposes of this review activity is therefore understood as simulated work tasks in a clinical setting; c) Participation is the involvement in a real-life situation in a social environment. For the purposes of this review participation is understood as therapeutic intervention within the workplace, thus workplace-based interventions.
3.4Body structures and functions component
The intervention programmes used in five studies aimed at improving Body Structures and Functions [34, 37, 41, 42, 44]. The same intervention programme was implemented in the Sachs study [37] and Winick study [42], which share noteworthy similarities with that in the Maguire study [34]. The intervention programme implemented in the Maguire study, which was a RCT, comprised of individualised counselling sessions consisting of: physical exercises to restore upper limb function; assisting the breast cancer survivor to adapt to breast loss; providing information on prostheses; and a home visit after discharge to follow-up on adherence to the exercise programme. The specialised nurse who implemented the programme encouraged women to talk to their partners about how they had been affected by the diagnosis and surgery, and she motivated women to return to work and to socialise again. The intervention programme used in the Sachs and Winick studies did not provide information on prostheses, but additionally the intervention programme discussed wound care. In the Maguire study a higher percentage of the participants in the intervention group (76%) returned to work at either 12 or 18 months compared to the control group (54%). In the longitudinal prospective study using a one-group design by Winick, 74% of the employed participants returned to full-time employment at three months post-mastectomy. In the Maguire and Winick studies the intervention programmes achieved positive effects in the return-to-work of the participants, but in both studies the statistical significance of the observed changes were not reported.
An individual based exercise programme was implemented in the pilot RCT by Ibrahim et al. [41], which mainly focused on limiting upper limb dysfunction and pain by including upper body strength training, endurance, and stretching in the treatment programme. Participants were encouraged to perform the programme two to three times per week over a 12-week period. Ten minutes of cardiovascular warm-up and cool-down were also part of each training session. Of the cohort, 86% of participants returned to work 12–18 months post-radiation. No differentiation was made in the results between the intervention and control group; therefore, no comparison between the groups was made which limits interpreting the effect of the intervention programme on work-related outcomes.
The qualitative study [44], with a phenomenological approach, explored cancer survivors’ experiences with return-to-work and work performance, a physical exercise programme after treatment, and the perceived relationship between exercise and work. The participants were recruited after completing a group-based exercise programme consisting of interval and resistance training of moderate intensity. A cycle ergometer was used for interval training, and resistance training was done through weightlifting targeting large muscle groups. Of the ten participants, eight returned to work within six months after the treatment. Participants voiced that increasing energy levels through physical exercise, likely contributed to their ability to resume work. Additionally, some participants reported that the physical exercise improved their work performance, and a supportive work environment encouraged them to continue with physical exercise.
Moderate evidence was found for studies that implemented intervention programmes aimed at improving Body Structures and Functions to achieve effective work-related transitions. Of the five studies focused on improving Body Structures and Functions, none of the study findings concluded that the following led to statistically significant improvements in work-related outcome measures: physical exercise (individual or group based) targeting general physical fitness and/or focusing on the upper body of breast cancer survivors undergoing or after undergoing surgery and/or adjuvant therapy, as well as information provided by healthcare providers and shared by breast cancer survivors. Nonetheless, the findings of the review indicated that intervention programmes focused on improving the component Body Structures and Functions can achieve positive effects by reducing sick leave days, and improving return-to-work rates.
3.5Multicomponents - Body structures and functions, and activities
Five studies’ [35, 36, 38, 39, 43] intervention programmes included a coping skills element in addition to physical exercise and providing information.
The Berglund study (1994) implemented a group therapy programme (“Starting Again Program”) mainly targeting physical training, information, and coping skills training [35]. The physical training sessions also included relaxation training (muscle relaxation and positive images) alongside breast cancer specific information sessions. Cancer education was given by the oncologist, the concept of crisis and the emotional reaction to different phases of crisis were covered by the psychologist, and health and diet were discussed by the dietician. This programme also included life skills coping sessions, addressing activity limitations. These sessions included role playing of return-to-work, anxiety management, and dealing with problem situations. The same intervention programme design (“Starting Again Program”) was used by the study conducted by Berglund, Bolund, Gustavsson and Sjödén (1993) [38]. In both studies, the results for all three areas on which the intervention programme focused –physical training, information, and coping skills training –indicated improvements. Additionally, both studies indicated improvements in work resumption and sick leave days of the intervention group compared to the control group at all intervals of post intervention measurements (three months [38]; six and 12 months (1993) [35]), but the improvements were not statistically significant.
The Björneklett study [36], which was an RCT, implemented a one-week group therapy programme focussing on informative-educational sessions on cancer; physical exercise; relaxation training; mental visualisation; non-verbal communication; and social activities. This programme was provided by a multidisciplinary team. At two, six, and 12 months post-treatment the differences between the intervention and control group in terms of sick leave days were statistically insignificant.
A multidisciplinary physical activity behaviour change intervention programme, based on the social cognitive theory, to gradually increase participants’ walking time to 150 minutes per week, was carried out in the Rogers study [39]. This intervention programme also included discussion group sessions on social support, exercise role models, and coping skills. The results did not indicate a statistically significant difference in sick leave days between the intervention group and control group following the 12-week intervention programme.
In the Leensen study [43], a multidisciplinary rehabilitation programme was implemented combining counselling on work-related issues with a supervised moderate to vigorous exercise programme. A physiotherapist provided the intervention programme, which ran twice weekly for one hour over a 12-week period. The sessions consisted of interval training on a cycle ergometer and resistance training of large muscle groups. Besides the exercise programme, participants underwent one to three individual counselling sessions with an oncological occupational physician. The counselling sessions focused on discussing a transitional return-to-work programme considering the breast cancer survivor’s work demands, work ability, medical situation, and perceived work ability. Six months after the programme was implemented 59 % of the participants returned to work; at 12 months the percentage improved to 86 %; and at 18 months the percentage was 83%. Compelling results were found by using secondary self-reported work-related outcome measures focusing on the importance of work, work ability, return-to-work self-efficacy, and quality of life, which all showed statistically significant improvements at six, 12, and 18 months. The study did not include a control group; therefore, these improvements could also be ascribed to factors other than those associated with the intervention programme.
The findings of the studies [35, 36, 38, 39, 43] of interventions aimed at improving Multicomponents were moderate evidence for indicating that this type of treatment programme did not statistically reduce the sick leave days [35, 36, 38, 39] and/or improve the resumption of work [38, 43] of the breast cancer survivors. Low strength of evidence was found for achieving statistically significant improvements in the self-reported work-related outcome measures of breast cancer survivors by implementing a Multicomponents treatment programme, as this was only found in one study [43].
3.6Activities component
Two studies [40, 45] focused on improving the Activities component to achieve effective work-related transitions for breast cancer survivors. One level V study [45] was excluded following the methodological quality assessment, as the level of evidence was low and the risk of bias of this study was high.
The feasibility study by Hubbard, Gray, Ayansina, Evans, and Kyle [40] that incorporated a RCT, provided vocational rehabilitation case management services to breast cancer survivors. The intervention adopted a biopsychosocial model and a multidisciplinary approach using case management to assess participants’ individual needs to provide support and services accordingly by referring participants to –amongst others –physiotherapy, occupational therapy, an occupational health nurse, and an occupational health doctor. The case manager also contacted the participants’ employers to discuss work-related issues such as a return-to-work plan and to recommend changes in work demands and hours. This was done to decrease the breast cancer survivors’ period of absenteeism and increase their work performance upon return-to-work. The control group received the standard post-operative care with no formal employment support. After the first six months post-operation, the intervention group reported substantially (53 days) less sick leave compared to the control group, but this was not statistically significant. At the 12-month follow-up the intervention group only reported a mere two days fewer sick leave days compared to the control group, which was statistically insignificant. Low evidence was found for studies aimed at improving the Activities component of breast cancer survivors to achieve effective work-related transitions, which indicated no statistically significant improvements in sick leave days.
3.7Participation component
Participation is defined by the ICF Framework as the involvement in a real-life situation in a social environment. For the purposes of this review participation is understood as therapeutic intervention within the workplace. None of the intervention studies in the review aimed directly at restoring the breast cancer survivors’ participation in work within the work context. Therefore, no evidence was found for the Participation component.
4Discussion
The body, level, and strength of evidence included in this systematic review were insufficient to recommend interventions within the scope of occupational therapy that are effective (showing statistically significant improvements) for work-related transitions of breast cancer survivors. None of the studies included had an occupational therapy practitioner as the health care provider.
The study findings of the articles were grouped, synthesised, and discussed using the ICF Framework. The reason for using ICF Framework is that work-related interventions for breast cancer survivors should ideally be based on this framework, as found by a conceptual-practice model for occupational therapy [14].
For most of the studies [34, 35, 37–39, 41, 42] in this review, work-related outcomes were secondary study outcomes. This finding corresponds to that of the systematic review done by Cocchiara, Sciarra, D’Egidio, Sestili, Mancino, Backhaus, et al. [13] in 2018. Our systematic review highlights that most of the intervention studies included in the review focused on the treatment of Body Structures and Functions or Multicomponents in a clinical setting.
Five studies’ intervention programmes aimed at improving the Body Structures and Functions Component, by focusing on upper body range of motion and strength, physical fitness and endurance, and breast cancer education. The one qualitative study found that a group based physical exercise programme consisting of interval and resistance training of moderate intensity, resulted in improved energy levels, which likely contributed to the participants’ ability to resume work. Additionally, some participants reported that physical exercise improved their work performance. Moderate evidence was found for intervention programmes aimed at improving the Body Structures and Functions component to achieve effective work-related transitions, and indicated no statistically significant improvements in the sick leave days and period until resumption of work of breast cancer survivors. This finding agrees with the systematic review conducted in 2017 by De Boer, Taskila, Tamminga, Feuerstein, Frings-Dresen, and Verbeek [48], that found low evidence indicating that physical training was not more effective than usual care in improving the resumption of work of cancer survivors. Nonetheless, the findings of four of the five studies [34, 37, 42, 44] in this review indicated that positive effects –reducing sick leave days and improving period required to return to work –could be achieved.
Five studies consisted of Multicomponents intervention programmes focussed on improving the Activities component alongside Body Structures and Functions. Treatment components aimed at reducing activity limitations comprised of counselling on work-related issues and coping skills training (role playing of return-to-work, identifying and managing anxiety and problem situations, relaxation training, mental visualisation, and non-verbal communication). Moderate evidence was found to support the effectiveness of Multicomponents intervention programmes. The evidence showed that breast cancer survivors’ sick leave days and period until resumption of work, could not be statistically significantly improved by intervention programmes targeting Multicomponents. Two studies showed that positive effects in the sick leave days (27) and period until resumption of work [43] of breast cancer survivors, could be achieved with a Multicomponents intervention programme. A systematic review of reviews on return-to-work and breast cancer found that multidisciplinary interventions addressing Multicomponents of function through physical exercise, counselling, and education could support work outcomes of breast cancer survivors [13].
The Leensen study [43] in which a Multicomponents intervention programme was implemented, found statistically significant improvements in the self-reported measures of breast cancer survivors on the importance of work, work ability, and return-to-work self-efficacy, at six, 12 and 18 months after treatment. This was a level III evidence (no comparison group) study with a low risk of bias. Therefore, the statistically significant improvements reported, may not be exclusively attributed to the intervention itself as no comparison group was included. The strength of evidence for this finding is considered as low, as only one study in the review utilised and reported on these treatment outcomes. Evidence suggests that breast cancer survivors’ perception of their work demands and workplace, plays a pivotal role in their recovery and resumption of work [49, 50].
The study conducted by Hubbard, Gray, Ayansina, Evans, and Kyle [40] on vocational rehabilitation case management aimed at improving the Activities component, concluded that the study was underpowered to indicate statistically significant differences between the intervention and control group, as the recruitment target could not be met. Nonetheless, the intervention group’s 53 fewer sick leave days compared to the control group after the first six months post-surgery, amounted to a substantial difference which was clinically significant. Furthermore, a decrease in the period of absenteeism and an increase in the work performance upon return to work of breast cancer survivors were achieved by addressing work-related issues. This underlines the potential positive effect of an intervention programme that adopts a biopsychosocial model with a multidisciplinary treatment approach using case management. Only one level II study with a low risk of bias aimed at improving the Activities component by implementing a vocational rehabilitation case management programme was included in the review. Thus, low evidence was found for achieving positive effects in work-related transitions (reducing sick leave days) of breast cancer survivors when implementing an intervention programme aimed at improving the Activities component.
No studies targeting the Participation component could be found. This finding is consistent with evidence on return-to-work interventions for cancer survivors [46, 51]. A scoping review done by Bilodeau, Tremblay, and Durand [52] on return-to-work interventions for breast cancer survivors, underscored the absence of involving the work environment in the interventions offered to breast cancer survivors for work-related transitions. In the study conducted by Chow, Ting, and Su [53] the findings underlined that of all factors influencing the resumption of work among breast cancer survivors, environmental factors are the most modifiable. These factors include a supportive environment of friends, family, and health care professionals, as well as a supportive workplace environment (appropriate job demands and working hours as well as support from the employer and colleagues). This highlights a gap in the current research: even though addressing environmental factors has great potential to achieve effective work-related transitions for breast cancer survivors [52], these are not adequately explored in primary intervention research studies. Researchers face marked challenges in the workplace setting with regard to the involvement of employers and the renewal rate of staff [25], which could possibly account for the limited research on the Participation component.
Evidence has shown that the worker role itself could be rehabilitative as work provides a sense of normality, identity, contact with social support structures [9, 11], and work-related activities itself could be inherently rehabilitative in maintaining and/or improving functional performance [15]. A study conducted by Mahar and colleagues [55] showed that with continuous employment, the reported levels of anxiety, depression, somatization, and general distress of female cancer survivors could be reduced, as well as their quality of life improved, when compared to women who were not working. Workplace based interventions could reduce the duration of work disability [56].
4.1Recommendations for future research
The body, level, and strength of evidence that met the inclusion criteria of this review were limited and partially outdated. This finding corresponds to that of a literature review on return-to-work among breast cancer survivors that was done by Sun, Shigaki, and Armer [57] in 2017.
Future researchers should aim to reduce and/or mitigate detection bias, as blinding of the outcome assessment was not done in six of the RCT and the one non-RCT. More high-quality research is needed on the effectiveness of an intervention programme focused on improving the Activities component and Participation component of breast cancer survivors for effective work-related transitions. Future research is needed to determine the effectiveness of intervention programmes implemented in the work context, i.e. workplace based interventions (e.g. work visits that could include work accommodations, ergonomic set-up of workstations, liaison with the employer and breast cancer survivor to compile a return-to-work plan).
The effectiveness of using telehealth workplace based interventions to improve the work-related transitions of breast cancer survivors, should also be investigated. Research should explore the effect the worker role itself, fulfilled in the work or home context with flexible working hours, could have on the work-related transitions of breast cancer survivors whilst they are undergoing adjuvant treatment and/or after completing surgical intervention.
More high-quality research in the field of occupational therapy work-related interventions for breast cancer survivors should be done. Désiron, Crutzen, Godderis, Van Hoof, and De Rijk [58] compiled a four-step return-to-work occupational therapy intervention mapping programme for breast cancer survivors. This programme was developed using intervention theory, but the effectiveness thereof should be established in future research.
A web-based decision and support tool, WISE (Work ability Improvement through Symptom management and Ergonomic education), has been developed as a breast cancer survivor-centred intervention. This tool aims to assist breast cancer survivors with symptom management, to point out ergonomic problems and risks in the workplace, and to perform workplace accommodations [59]. The effectiveness of this intervention tool for work-related transitions of breast cancer survivors, still needs to be determined in future research.
Several studies made use of the FACT-G and/or FACT-B self-reported questionnaires. Findings of these studies were discussed only referring to quality of life outcome measures, and no commentary was made on the work-related items of these outcome measures. Future researchers should specifically comment on these items, as the intervention programmes used in these studies could prove to be of value in this field of research and practice. Evidence has highlighted that only a few intervention studies primarily focus on assessing work-related outcome measures and most studies only consider the overall quality of life of the breast cancer survivors [13, 60].
Future researchers should consider using work-related outcomes measures –the Worker Ability Index [61], Self-efficacy Scale [62], and Work Limitations Questionnaire [63] –that have sound psychometric properties in addition to self-reported sick leave days and the period until resumption of work. By using these outcomes measures the breast cancer survivors’ perception of their work demands and workplace can be assessed, which plays a pivotal role in their recovery and resumption of work [49, 50].
4.2Recommendations for practice
Work-related transition interventions should be offered to breast cancer survivors throughout the cancer care continuum, thus from the time of diagnosis onwards, to achieve work retention and resumption [52, 60]. Early contact (within three months) with the breast cancer survivor and the employer can significantly reduce the period of work disability [27]. This approach would specifically be suited for breast cancer survivors who indicate that work is a priority and important life role [64].
Practitioners need to consider implementing treatment programmes focused on Body Structures and Functions as well as Activities, i.e. Multicomponents intervention programmes. This is recommended because findings of three of the studies [38, 39, 41] showed that improvements in the component of Body Structures and Functions alone do not necessarily translate into reducing the activity limitations and participation restrictions of breast cancer survivors.
Multicomponents intervention programmes should comprise of: exercise programmes (improving upper body strength and flexibility; general physical fitness and endurance); breast cancer education; and coping skills training (stress management, time management, work-related counselling sessions, relaxation training, and return-to-work role play etc.). Positive effects in reducing the sick leave days and reduced periods until resumption of work of breast cancer survivors, can be achieved by a Multicomponents intervention programme. However, moderate strength of evidence for this type of intervention programme was found. Providing a Multicomponents intervention programme to breast cancer survivors can also significantly improve their self-reported work outcomes (importance of work, work ability, and return-to-work self-efficacy), as was found by one study. This specific Multicomponents programme comprised of counselling on work-related issues and a supervised moderate to vigorous exercise programme.
In the first six-months post-operation, practitioners can consider providing a vocational rehabilitation case management programme which adopts a biopsychosocial model and multidisciplinary intervention approach. The programme needs to include employer contact to discuss work-related issues (e.g. work adjustments such as changes in working hours, work demands, or work role) in order to achieve positive effects in reducing the sick leave days of breast cancer survivors. The strength of evidence for this type of programme was low. Evidence has shown that providing cancer-related support to breast cancer survivors in the work-context can have positive effects on their return-to-work during or following treatment [65–67].
Occupational therapy should be included as part of a multidisciplinary rehabilitation programme [7]. The occupational therapy programme needs to also focus on the Participation component. This can be achieved by using work-related activities in the work context which are inherently rehabilitative [27], and it would enable breast cancer survivors to participate in a meaningful life role, namely the worker role [20]. This can have a remarkable impact on the quality of life of breast cancer survivors [7].
4.3Strengths and limitations of the review
This systematic review has several strengths. Firstly, a comprehensive search strategy was used to include qualitative and quantitative primary research to alleviate the impact of reporting bias on the results [68]. Pearling of the articles included in the review was done to search for additional articles that could have been missed during the search and/or selection phases of this review. To limit introducing study availability bias, an expert librarian assisted in getting access to articles that met the eligibility criteria. At the full-text screening phase, selection bias was mitigated by using a second reviewer. Secondly, research studies included were rated according to the level of evidence and risk of bias, which increased the rigour of this systematic review. Thirdly, the review reflects a spectrum of work-related interventions within the scope of occupational therapy. By synthesising the available body of evidence in this field, practitioners and researchers will be able to identify and consider relevant evidence from individual studies to be used in practice and future research. Finally, to our knowledge this is the first review of what occupational therapy interventions are effective in work-related transitions of breast cancer survivors.
The review also has various limitations. Firstly, selection bias might have been introduced at the title and abstract screening phase of the review which was completed by only one reviewer. Secondly, the heterogeneity of the search results did not allow for a meta-analysis to be done; this was in line with several systematic review studies in the field of work-related interventions that were also unable to conduct a meta-analysis [13, 22, 69, 70]. Thirdly, work-related intervention research studies on cancer survivors that did not specifically state that breast cancer survivors were more than 70% of the participants included, were excluded from this review. Therefore, relevant studies could potentially have been excluded. Fourthly, this review was exposed to language bias, as six studies that were not published in English were excluded. These studies could have potentially made valuable contributions to this field of research. Finally, relevant stakeholders such as breast cancer survivors, researchers, and health care practitioners as well as employers of breast cancer survivors, were not consulted prior to drawing up the protocol and when conducting the systematic review. This may have limited the comprehensiveness of the planned search terms and identifying the most up to date research. Furthermore, knowledge translation could be less effective as relevant stakeholders were not involved in the analysis and narrative synthesis of the research findings.
5Conclusion
The body, level, and strength of evidence that met the inclusion criteria of this systematic review were insufficient to recommend interventions within the scope of occupational therapy that are effective (showed statistically significant improvements) in reducing the sick leave days and the period required to resume work, for breast cancer survivors. The study found moderate evidence for intervention studies aimed at improving Body Structures and Functions and Multicomponents, which showed that these treatment programmes can bring about positive effects in reducing the sick leave days and period required until resumption of work of breast cancer survivors. A Multicomponents treatment programme can achieve statistically significant changes in the self-reported work outcomes (importance of work, work ability, and return-to-work self-efficacy) of breast cancer survivors, but the evidence for this was low. Improving Body Structures and Functions does not necessarily translate into reducing activity limitations and participation restrictions for work-related transitions aimed at this group, as the study findings in this review underscored. Future research on interventions for effective work-related transitions of breast cancer survivors should also focus on the Participation component.
Author contributions
Luna Stehle: Conceptualised the systematic review, analysed and interpretated the data as well as wrote up the study findings in article format; Critically appraised and applied the amendments suggested by co-authors; Approved the final draft of the article for publishing; Agreed to be accountable for all aspects of the article.
Munira Hoosain: Substantial contribution to the conceptualisation of the systematic review as well as the analysis and the interpretation of the data of the review; Revised and critically appraised the content of the article; Approved the final draft of the article for publishing; Agreed to be accountable for all aspects of the article.
Lana van Niekerk: Contributed to the analysis and interpretation of the data used in the systematic review as well as the conceptualisation of the reporting of the study findings in an article format; Revised and critically appraised the content of the article; Approved the final draft of the article for publishing; Agreed to be accountable for all aspects of the article.
Availability of data
All data generated or analysed during this study are included in this published article.
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethics approval and consent to participate
The researchers had no conflict of interest in the chosen study. This study made use of research articles as research units and no studies were done with human participants or animals. Therefore, no ethical approval or consent of participants were required.
Funding
No funding was received for conducting this study.
Supplementary material
[1] The supplementary material is available in the electronic version of this article: https://dx.doi.org/10.3233/WOR-210053.
References
[1] | Global Cancer Facts & Figures 4th Edition. American Cancer Society. Atlanta: American Cancer Society; 2018. |
[2] | Meade E , Dowling M . Early breast cancer: Diagnosis, treatment and survivorship. Br J Nurs. (2012) ;21: :4–9. |
[3] | Hoffman B . Cancer Survivors at Work: A Generation of Progress. CA Cancer J Clin. (2005) ;55: :271–80. |
[4] | Short PF , Vasey JJ , Tunceli K . Employment pathways in a large cohort of adult cancer survivors. Cancer. (2005) ;103: :1292–301. |
[5] | Hayes SC , Johansson K , Stout NL , Prosnitz R , Armer JM , Gabram S , et al. Upper-body morbidity after breast cancer: Incidence and evidence for evaluation, prevention, and management within a prospective surveillance model of care. Cancer. (2012) ;118: :2237–49. |
[6] | Rietman JS , Dijkstra PU , Hoekstra HJ , Eisma WH , Szabot BG , Groothoff JW , et al. Late morbidity after treatment of breast cancer in relation to daily activities and quality of life: A systematic review. Eur J Surg Oncol. (2003) ;29: :229–38. |
[7] | Loh SY , Musa AN . Methods to improve rehabilitation of patients following breast cancer surgery: A review of systematic reviews. Breast Cancer Targets Ther. (2015) ;7: :81–98. |
[8] | Pyszel A , Malyszezak K , Pyszel K , Andrzejak R , Szuba A . Disability, psychological distress and quality of life in breast cancer survivors with arm lymphedema. Lymphology. (2006) ;39: :185–92. |
[9] | Lyons KD , Svensborn IA , Kornblith AB , Hegel MT . A Content Analysis of Functional Recovery Strategies of Breast Cancer Survivors. OTJR. (2015) ;35: :73–80. |
[10] | Bradley CJ , Bednarek HL , Neumark D . Breast cancer and women’s labor supply. Health Serv Res. (2002) ;37: :1309–28. |
[11] | Wells M , Williams B , Firnigl D , Lang H , Coyle J , Kroll T , et al. Supporting “work-related goals” rather than “return to work” after cancer? A systematic review and meta-synthesis of 25 qualitative studies. Psychooncology.. (2013) ;22: :1208–19. |
[12] | Tamminga SJ , De Boer AGEM , Verbeek JHAM , Frings-Dresen MHW . Return-to-work interventions integrated into cancer care: A systematic review. Occup Environ Med. (2010) ;67: :639–48. |
[13] | Cocchiara RA , Sciarra I , D’Egidio V , Sestili C , Mancino M , Backhaus I , et al. Returning to work after breast cancer: A systematic review of reviews. Work. (2018) ;61: :463–76. |
[14] | Désiron HAM , Donceel P , De Rijk A , Van Hoof E . A conceptual-practice model for occupational therapy to facilitate return to work in breast cancer patients. J Occup Rehabil. (2013) ;23: :516–26. |
[15] | Clur L , Barnard A , Joubert YT . Work adjustment of cancer survivors: An organisational support framework. SA J Ind Psychol. (2017) ;43: :1–11. |
[16] | Banning M . Employment and breast cancer: a meta-ethnography. Eur J Cancer Care (Engl). England. (2011) ;20: :708–19. |
[17] | Pergolotti M , Williams GR , Campbell C , Munoz LA , Muss HB . Occupational Therapy for Adults With Cancer: Why It Matters. Oncologist. (2016) ;21: :314–9. |
[18] | Stucki G . International classification of functioning, disability, and health (ICF): A promising framework and classification for rehabilitation medicine. Am J Phys Med Rehabil. (2005) ;84: :733–40. |
[19] | Hwang EJ , Lokietz NC , Lozano RL , Parke MA . Functional deficits and quality of life among cancer survivors: Implications for occupational therapy in cancer survivorship care. Am J Occup Ther. 2015;69. |
[20] | Keesing S , Rosenwax L , McNamara B . Identifying the contribution of occupational therapy in meeting the needs of women survivors of breast cancer. Br J Occup Ther. (2018) ;81: :402–12. |
[21] | Désiron HAM , Donceel P , Godderis L , Van Hoof E , De Rijk A , Godderis L , et al. What is the value of occupational therapy in return to work for breast cancer patients? A qualitative inquiry among experts. Eur J Cancer Care (Engl). (2015) ;24: :267–80. |
[22] | Désiron HAM , De Rijk A , Van Hoof E , Donceel P . Occupational therapy and return to work: A systematic literature review. BMC Public Health. 2011;11. |
[23] | Liberati A , Altman DG , Tetzlaff J , Mulrow C , Gøtzsche PC , Ioannidis JPA , et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009;6. |
[24] | Shamseer L , Moher D , Clarke M , Ghersi D , Liberati A , Petticrew M , et al. Preferred reporting items for systematic review and meta-analysis protocols (prisma-p) 2015: Elaboration and explanation. BMJ [Internet]. (2015) ;349: :1–25. Available from: http://dx.doi.org/doi:10.1136/bmj.g7647. |
[25] | Oakman J , Neupane S , Proper KI , Kinsman N , Nygård CH . Workplace interventions to improve work ability: A systematic review and meta-analysis of their effectiveness. Scand J Work Environ Heal. (2018) ;44: :134–46. |
[26] | Hariton E , Locascio JJ . Randomised controlled trials—the gold standard for effectiveness. HHS Public Access. (2018) ;125: :1–4. |
[27] | Franche RL , Cullen K , Clarke J , Irvin E , Sinclair S , Frank J , et al. Workplace-based return-to-work interventions: A systematic review of the quantitative literature. J Occup Rehabil. (2005) ;15: :607–31. |
[28] | American Occupational Therapy Association. Guidelines for Systematic Reviews [Internet]. 2020 [cited 2020 May 16]. Available from: https://ajot.submit2aota.org/journals/ajot/forms/systematic_reviews.pdf |
[29] | Higgins JP , Sterne JA , Savovic J , Page MJ , Hróbjartsson A , Boutron I , et al. A revised tool for assessing risk of bias in randomized trials. Cochrane Database Syst Rev. (2016) ;10: :29–31. |
[30] | Quality assessment tool for before-after (pre-post) studies with no control group. [Internet]. Natl. Hear. Lung, Blood Institute. Washington DC: National Institutes of Health; 2014 [cited 2020 May 19]. Available from: http://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/before-after. |
[31] | Polk C . Guidelines for Systematic Reviews in Environmental Management [Internet]. aota.org. 2020. pp. 80.Available from: http://www.environmentalevidence.org/wp-content/uploads/2014/06/Review-guidelines-version-4.2-final.pdf. |
[32] | Grade Definitions | United States Preventive Services Taskforce [Internet]. [cited 2020 May 18]. Available from: https://www.uspreventiveservicestaskforce.org/uspstf/grade-definitions. |
[33] | The Joanna Briggs Institute. Checklist for Qualitative Research [Internet]. Joanna Briggs Inst. 2020 [cited 2020 Jun 15]. p. 6. Available from: https://joannabriggs.org/sites/default/files/2020-08/Checklist_for_Qualitative_Research.pdf. |
[34] | Maguire P , Brooke M , Tait A , Thomas C , Sellwood R . The effect of counselling on counselling on physical disability and social recovery after mastectomy. Clin Oncol. (1983) ;9: :319–24. |
[35] | Berglund G , Bolund C , Gustaffson U-L , Sjödén PO . A randomised study of a rehabilitation program for cancer patients: The “Starting Again” group. Psychooncology (1994) ;3: :190–120. |
[36] | Björneklett HG , Rosenblad A , Lindemalm C , Ojutkangas ML , Letocha H , Strang P , et al. A randomized controlled trial of support group intervention after breast cancer treatment: Results on sick leave, health care utilization and health economy. Acta Oncol (Madr). (2013) ;52: :38–47. |
[37] | Sachs S , Davis J , Reynolds S , Spagnola M , Hall P , Bloch A . Postmastectomy Rehabilitation in a Community Hospital. J Fam Pract. (1980) ;11: :395–401. |
[38] | Berglund G , Bolund C , Gustavsson UL , Sjödén PO . Starting again-a comparison study of a group rehabilitation program for cancer patients. Acta Oncol (Madr). (1993) ;32: :15–21. |
[39] | Rogers LQ , Hopkins-Price P , Vicari S , Pamenter R , Courneya KS , Markwell S , et al. A randomized trial to increase physical activity in breast cancer survivors. Med Sci Sports Exerc. (2009) ;41: :935–46. |
[40] | Hubbard G , Gray NM , Ayansina D , Evans JMM , Kyle RG . Case management vocational rehabilitation for women with breast cancer after surgery: a feasibility study incorporating a pilot randomised controlled trial. Trials. (2013) ;14: :175. |
[41] | Ibrahim M , Muanza T , Smirnow N , Sateren W , Fournier B , Kavan P , et al. Time course of upper limb function and return-to-work post-radiotherapy in young adults with breast cancer: a pilot randomized control trial on effects of targeted exercise program. J Cancer Surviv. United States. (2017) ;11: :791–9. |
[42] | Winick L , Robbins GF . The Post-Mastectomy Rehabilitation Group programStructure, procedure, and population demography. Cancer. United States. (1977) ;39: :478–86. |
[43] | Leensen MCJ , Groeneveld IF , van der Heide I , Rejda T , van Veldhoven PLJ , van Berkel S , et al. Return to work of cancer patients after a multidisciplinary intervention including occupational counselling and physical exercise in cancer patients: a prospective study in the Netherlands. BMJ Open. 2017;7. |
[44] | Groeneveld IF , De Boer AGEM , Frings-Dresen MHW . Physical exercise and return to work: cancer survivors’ experiences. J Cancer Surviv. United States. (2013) ;7: :237–46. |
[45] | Désiron HAM . Occupational therapy and return to work for breast cancer survivors. WFOT Bull [Internet]. Abingdon, Oxfordshire, <Blank>: Taylor & Francis Ltd; 2(2010) ;61: : 45–51. Available from: http://search.ebscohost.com/login.aspx?direct=true&db=cin20&AN=105010799&site=ehost-live&scope=site |
[46] | Caron M , Durand MJ , Tremblay D . Interventions to support the return-to-work process after cancer: A literature review. Sante Publique (Paris). (2017) ;29: :655–64. |
[47] | WHO | International Classification of Functioning, Disability and Health (ICF) [Internet]. [cited 2020 Apr 9].Available from: https://www.who.int/classifications/icf/en/ |
[48] | De Boer AGEM , Taskila TK , Tamminga SJ , Feuerstein M , Frings-Dresen MHW , Verbeek JH . Interventions to enhance return-to-work for cancer patients. Cochrane Database Syst Rev. 2015;2017. |
[49] | Bijker R , Duijts SFA , Smith SN , de Wildt-Liesveld R , Anema JR , Regeer BJ . Functional Impairments and Work-Related Outcomes in Breast Cancer Survivors: A Systematic Review. J Occup Rehabil. (2018) ;28: :429–51. |
[50] | Barnes AJ , Robert N , Bradley CJ . Job attributes, job satisfaction and the return to health after breast cancer diagnosis and treatment. Psychooncology. (2014) ;23: :158–64. |
[51] | De Boer AGEM , Taskila TK , Tamminga SJ , Feuerstein M , Frings-Dresen MHW , Verbeek JH . Interventions to enhance return-to-work for cancer patients. Cochrane database Syst Rev. (2017) ;2017: :CD007569. |
[52] | Bilodeau K , Tremblay D , Durand MJ . Exploration of return-to-work interventions for breast cancer patients: a scoping review. Support Care Cancer. Supportive Care in Cancer. (2017) ;25: :1993–2007. |
[53] | Chow S , Ting A , Su T . Development of Conceptual Framework to Understand Factors Associated with Return to Work among Cancer Survivors: A Systematic Review. Iran J Public Health. (2014) ;43: :391–4. |
[54] | Sun W , Chen K , Terhaar A , Wiegmann DA , Heidrich SM , Tevaarwerk AJ , et al. Work-related barriers, facilitators, and strategies of breast cancer survivors working during curative treatment. Work. (2016) ;55: :783–95. |
[55] | Mahar KK , BrintzenhofeSzoc K , Shields JJ . The impact of changes in employment status on psychosocial well-being: a study of breast cancer survivors. J Psychosoc Oncol. United States. (2008) ;26: :1–17. |
[56] | Pomaki G , Franche RL , Murray E , Khushrushahi N , Lampinen TM . Workplace-based work disability prevention interventions for workers with common mental health conditions: A review of the literature. J Occup Rehabil. (2012) ;22: :182–95. |
[57] | Sun Y , Shigaki CL , Armer JM . Return to work among breast cancer survivors: A literature review. Support Care Cancer [Internet]. Supportive Care in Cancer; (2017) ;25: :709–18. Available from: http://dx.doi.org/10.1007/s00520-016-3446-1 |
[58] | Désiron HAM , Crutzen R , Godderis L , Van Hoof E , de Rijk A . Bridging Health Care and the Workplace: Formulation of a Return-to-Work Intervention for Breast Cancer Patients Using an Intervention Mapping Approach. J Occup Rehabil. Springer New York LLC. (2016) ;26: :350–65. |
[59] | Sesto M , Wachowiak R , Tevaarwerk A , Faatin M , Heidrich S , Wiegmann D . Improving employment outcomes of breast cancer survivors: Development of a web-based educational and decision support tool. Proc Hum Factors Ergon Soc. 2011. |
[60] | Hunter EG , Gibson RW , Arbesman M , D’Amico M . Systematic review of occupational therapy and adult cancer rehabilitation: Part 1. Impact of physical activity and symptom management interventions.AmJ Occup Ther. 2017;71. |
[61] | Adel M , Akbar R , Ehsan G . Validity and reliability of work ability index (WAI) questionnaire among Iranian workers; a study in petrochemical and car manufacturing industries. J Occup Health. (2019) ;61: :165–74. |
[62] | Lagerveld SE , Blonk RWB , Brenninkmeijer V , Schaufeli WB . Return to work among employees with mental health problems: Development and validation of a self-efficacy questionnaire. Work Stress. (2010) ;24: :359–75. |
[63] | Arumugam V , MacDermid JC . The work limitations questionnaire (WLQ-25). J Physiother. (2013) ;59: :276. |
[64] | Stergiou-Kita M , Grigorovich A , Tseung V , Milosevic E , Hebert D , Phan S , et al. Qualitative meta-synthesis of survivors’ work experiences and the development of strategies to facilitate return to work. J CANCER Surviv. (2014) ;8: :657–70. |
[65] | Taskila T , Martikainen R , Hietanen P , Lindbohm ML . Comparative study of work ability between cancer survivors and their referents. Eur J Cancer. (2007) ;43: :914–20. |
[66] | Torp S , Gudbergsson SB , Dahl AA , Fossa SD , Flotten T . Social support at work and work changes among cancer survivors in Norway. Scand J Public Health. (2011) ;39: :33–42. |
[67] | Torp S , Nielsen RA , Gudbergsson SB , Dahl AA . Worksite adjustments and work ability among employed cancer survivors. Support CARE CANCER. (2012) ;20: :2149–56. |
[68] | Whiting P , Rutjes A , Reitsma J , Bossuyt P , Kleijnen J . The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol. (2003) ;25: :1919–27. |
[69] | Cullen KL , Irvin E , Collie A , Clay F , Gensby U , Jennings PA et al. Effectiveness of Workplace Interventions in Return-to-Work for Musculoskeletal, Pain-Related and Mental Health Conditions: An Update of the Evidence and Messages for Practitioners. J. Occup. Rehabil. Springer New York LLC; (2018) . |
[70] | D’Egidio V , Sestili C , Mancino M , Sciarra I , Cocchiara R , Backhaus I , et al. Counseling interventions delivered in women with breast cancer to improve health-related quality of life: a systematic review. Qual Life Res. (2017) ;26: :2573–92. |




