The influences of corporate policies for COVID-19 on work stress and anxiety among healthcare employees
Abstract
BACKGROUND:
During the coronavirus disease (COVID-19) pandemic, if it is considered that educated manpower is the most valuable resource of countries, it can be thought that various policies should be developed both at the macro- and micro-levels to minimize the loss of healthcare employees.
OBJECTIVE:
This study aims to determine the effects of the corporate policies for COVID-19 on the work stress and anxiety of healthcare employees.
METHOD:
The sample of the study consists of 136 of 265 healthcare employees in Sakarya Provincial Health Directorate Emergency Health Services in Turkey. The average age of the participants was 34.43 years, and the average duration of professional experience was 12.12 years. Approximately 61% of the participants are male and 51% have a bachelor’s degree or higher level. A questionnaire form was used in the study as the data collection tool consisting of socio-demographic characteristics, institutional policies on COVID-19, work stress, and the Status Anxiety Scale. Process Macro Model 4, descriptive statistics and correlation analysis were used for the data analysis.
RESULTS:
According to the results of the study, the corporate policies for COVID-19 perception of participants were above average (3.30±0.82) while work stress (2.99±0.88) and anxiety (2.65±0.56) were below average. The corporate policies for COVID-19 perception of participants reduced their work stress (β= – 0.430) and anxiety (β= – 0.361). Additionally, anxiety played a mediating role in the effect of the corporate policies for COVID-19 perception on work stress, and it further raised the impact of corporate policies for COVID-19 perception on the work stress reduction (β= – 0.169).
CONCLUSIONS:
During the COVID-19 pandemic, health managers should determine and control the anxiety and stress levels of the health employees on their staff and take a number of steps to reduce their anxiety and stress.
1Introduction
Coronavirus disease (COVID-19) has spread all over the world, mostly due to human-to-human transmission, resulting in 538,321,874 cases and 6,320,599 deaths as of June 22, 2022 [1]. Previous studies revealed that the COVID-19 pandemic has resulted in fatigue, physical, and/or psychological disorders, anxiety, exhaustion, depression, and stress as well as respiratory and digestive issues in employees working in the healthcare industry [2– 5]. In addition, because healthcare employees are at the forefront of fighting the pandemic, it increases their risk of contracting the disease, thus putting their health and other lives at risk [3, 6]. Further, the pandemic has caused healthcare employees around the world to contract COVID-19 and even lose their lives [7– 11]. The Ministry of Health of the Republic of Turkey stated that more than 120,000 healthcare employees in Turkey have been infected and 216 of them died, as of December 10, 2020 [12]. According to the first-year evaluation report of the Turkish Medical Association, 337 healthcare workers died due to illnesses related to COVID-19, as of January 8, 2021 [13].
Multiple reasons exist for healthcare employees’ exposure to COVID-19, e.g., not taking appropriate personal-protection measures, being exposed to infected patients, having fewer rest periods, not having enough personal protective equipment, not enough training, and the inability to access sufficient information about the pandemic [14]. As such, COVID-19, which can be considered an occupational disease and/or creating potential for accidents, poses a risk to healthcare employees and makes it necessary for institutions to take measures to prevent adverse situations related to the disease [15– 17]. The developed policies are only useful when applied appropriately, however. Applications created in Turkey reveal that healthcare employees have access to protective equipment; however, the results of the study conducted by the Turkish Thoracic Society show otherwise. According to the study, about 60% of 295 healthcare employees reported that healthcare employees were given COVID-19 training in their institutions and that 11.5% were offered psychological support. According to the results of the study, 60% of participants had no problems with the provision of masks such as N95/FFP2/FFP3; the rate of employees who stated that they did not have any problems in terms of visors, glasses, aprons, and overalls was 56%, 56%, 66%, and 45% respectively [18].
Stress is the body’s response to dealing with a threat [19, 20]. Work stress can be defined as the harmful physical and emotional responses that occur when the requirements of the job do not match the capabilities, resources, or needs of the worker. Job stress can lead to poor health and even injuries [21]. Work stress can also affect employee health due to heavy workloads, caring for severe and terminally ill people, lack of physical opportunities in healthcare services, and difficult working conditions [22]. Further, many stress factors can affect employee health, especially for those who are treating patients diagnosed with COVID-19. These factors include the need to take strict biosecurity measures, the risk of disease transmission, facing multiple medical and personal demands, and stigmatization [23].
People will typically experience anxiety when they do not know what to do or cannot do anything when they are in danger; anxiety also occurs when these people feel inadequate in a threatening environment [24, 25]. Healthcare employees commonly experience this anxiety during infectious disease outbreaks [26]. During the H7N9 (avian flu) outbreak, for example, doctors and nurses who were forced to provide services to patients suffering from this disease were found to be prone to developing severe symptoms of anxiety and stress [27]. Similarly, anxiety and stress disorders have been commonly found among medical personnel during the COVID-19 outbreak [28– 30].
Ambulance services are provided by the Emergency Medical Services Unit in Turkey. Employees of the unit perform the first intervention for individuals with severe COVID-19 in accordance with their duties. The Emergency Medical Services Unit also provides transportation between the home and treatment centers for COVID-19 positive patients. This can increase anxiety and stress levels of healthcare employees. As a result of these discussions, the study aims to determine the impact of the policies developed by institutions against the COVID-19 pandemic in relation to work stress and anxiety of healthcare employees.
2Materials and methods
2.1Sampling and data collection time
Provincial health directorates are established under the Ministry of Health and are present in every province throughout the country. In addition, district healthcare directorates are also established in each district under the provincial healthcare directorates. The healthcare directorates’ duty is to ensure that healthcare facilities throughout the province or district they serve are not interrupted and take all necessary precautions regarding healthcare.
Two hundred sixty-five healthcare employees working in the Sakarya Provincial Health Directorate Emergency Health Services in Turkey constituted the population of this study. The sample of the study consists of employees working in the service who agreed to participate in the study. It is aimed to reach all employees regardless of any criteria.
The field research of this study was conducted between May 29 and July 1, 2020. The data were collected using the online survey method via Google Forms, thus ensuring participant confidentiality. The questionnaire prepared via Google Forms was sent to participants via e-mail to their corporate e-mail addresses. In the first part of the prepared questionnaire, participants were informed about the study. Then, they were asked to mark the question about whether they would participate in the research.
2.2Instruments
To measure the research hypotheses, a four-part questionnaire was used.
Part 1. Sociodemographic characteristics: This section contains questions about the gender, age, level of education, profession, whether healthcare employees have children, their duration of work in the institution, whether they were employees who caught COVID-19 in the institution and unit, and whether appropriate preventive measures had been taken to prevent COVID-19.
Part 2. The COVID-19 experiences of healthcare employees: The scale, developed by Maunder et al. [31], consists of 18 expressions and three subdimensions, i.e., education, protection, and support, work stress, perceived stigma, and interpersonal avoidance. This study uses the education, prevention and support, and work stress subdimensions.
The dimensions of education, protection, and support consists of nine expressions. The scale measures the adequacy of the training, protection, and support opportunities that institutions offered to their employees (for example, “I have received the necessary training to deal with situations I encounter”; “I am provided with the protective equipment and procedures I need”; “My institution provides emotional support for those who need help [for example, consulting is offered]”). For this reason, in our study, this dimension is called “Institutional policies on COVID-19.” The Cronbach’s alpha coefficient of the subscale is 0.89.
Part 3. Work stress: The scale, as developed by Maunder et al. [31], consists of five expressions and aims to measure the employees’ perceived work stress (e.g., “feeling more stressed at work,” “having to do work that I don’t normally do,” “having to work overtime,” etc.). The Cronbach’s alpha coefficient of the subscale is 0.76.
The scale expressions were designed as a five-point Likert scale, namely, 1 = absolutely disagree to 5 = absolutely agree. The Turkish adaptation of the scale was carried out by the authors.
Part 4. Status Anxiety Scale (SAS): The participants’ instant anxiety levels were measured using a scale developed by Spielberger, Gorsuch, and Lushene [32], adapted into Turkish by Öner and Le Compte [33]. The scale consists of 20 expressions (e.g., “I feel very nervous at the moment”; “I am not in any mood at the moment”; “I feel my nerves are very tense,” etc.) and a single subdimension. The scale expressions were scored between 1 and 4 (1 = none to 4 = completely). There are 10 reversed expressions for the SAS, which were reversely encoded before the analysis.
Because the Turkish literature does not include scales that measure whether healthcare employees are offered sufficient opportunities related to protection and information by their institutions concerning COVID-19, the institutional policy scale was used in the study. The work stress scale was included to determine the employees’ stress levels. Since these two scales are not Turkish, they were first translated from English into Turkish and then examined by academicians who are experts in their field. The scales were then translated from Turkish back into English by professional translators and compared with their first form. The scales’ final form was seen to be similar to the first form. After completion of the questionnaire’s final form, the scales were applied.
2.3Analysis of the data
Descriptive statistical methods, reliability and validity analyses, correlation analysis, and Hayes Process Macro Model 4 were used to analyze the data and test mediation with SPSS Indirect Macros Model 4, as recommended by Preacher and Hayes [34]. This was considered the most straightforward bootstrapping method to acquire confidence intervals for indirect effects [35]. Mediation was proved if the indirect effect was significant and the confidence interval did not include zero [36]. In other words, zero should not be between the values of the lower level of confidence interval (LLCI) or upper level of confidence interval (ULCI) values. The data were analyzed according to a 95% confidence interval (p = 0.05).
2.4Validity and reliability analysis
The results of the validity and reliability analysis of the scales used in this study are shown in Table 1. The item correlations and Cronbach’s alpha coefficient were used to determine the reliability of the scales. The correlation coefficient of the items making up the scale was found to be a minimum of 0.50 according to the dimensions; further, the Cronbach’s alpha coefficients ranged from 0.825 to 0.946. Accordingly, it can be said that the scales’ reliability levels are high.
Table 1
Validity and reliability analysis
| Kaiser-Meyer-Olkin measure of sampling adequacy | 0.899 | ||
| Bartlett’s test of sphericity | Approx. chi-square | 3407.826 | |
| df | 528.000 | ||
| Sig. | 0.000 | ||
| Variable | Anxiety | Institutional policies on COVID-19 | Job stress |
| Total varience | 40.732 | 11.093 | 7.437 |
| Eigenvalues | 11.740 | 3.197 | 2.144 |
| Cronbach’s alpha | 0.946 | 0.912 | 0.825 |
| Anxiety 5 | 0.867 | ||
| Anxiety 10 | 0.843 | ||
| Anxiety 15 | 0.798 | ||
| Anxiety 16 | 0.781 | ||
| Anxiety 20 | 0.776 | ||
| Anxiety 9 | 0.707 | ||
| Anxiety 14 | 0.705 | ||
| Anxiety 3 | 0.685 | ||
| Anxiety 12 | 0.677 | ||
| Anxiety 1 | 0.674 | ||
| Anxiety 13 | 0.673 | ||
| Anxiety 2 | 0.659 | ||
| Anxiety 8 | 0.650 | ||
| Anxiety 7 | 0.649 | ||
| Anxiety 17 | 0.642 | ||
| Anxiety 19 | 0.591 | ||
| Anxiety 11 | 0.507 | ||
| Anxiety 4 | 0.432 | ||
| Anxiety 6 | 0.432 | ||
| Institutional policies on COVID-19 9 | 0.827 | ||
| Institutional policies on COVID-19 8 | 0.798 | ||
| Institutional policies on COVID-19 6 | 0.787 | ||
| Institutional policies on COVID-19 2 | 0.772 | ||
| Institutional policies on COVID-19 3 | 0.727 | ||
| Institutional policies on COVID-19 7 | 0.719 | ||
| Institutional policies on COVID-19 1 | 0.664 | ||
| Institutional policies on COVID-19 5 | 0.626 | ||
| Institutional policies on COVID-19 4 | 0.529 | ||
| Job stress 4 | 0.841 | ||
| Job stress 3 | 0.710 | ||
| Job stress 5 | 0.691 | ||
| Job stress 2 | 0.688 | ||
| Job stress 1 | 0.436 | ||
The Kaiser-Meyer-Olkin sample sufficiency (KMO) of the scale is 0.90. The test for sphericity was found to be significant. As shown in Table 1, as a result of the exploratory factor analysis, the scales were divided into three dimensions. The first dimension measures anxiety; the second dimension measures the employees’ perceptions of the institutional policies for COVID-19; and the third dimension measures work stress. The eighteenth expression (“I feel confused due to excitement”) in the anxiety dimension, consisting of 20 expressions, was removed because it showed incompatibility in terms of the distribution. The variances explained by the scale sizes are 40.73%, 11.09%, and 7.44% respectively. The factor loads of the scale expressions range from 0.43 to 0.87. Accordingly, it can be said that the scales are valid and reliable.
3Results
The study sample consists of 136 (51%) healthcare employees who agreed to participate in the study and completed the questionnaire.
The average age of the participants was 34.43 years old (±8.33); the average duration of professional experience was 12.12 years (±7.18). Of the participants, 53 were women; 83 were men. Also, 69 participants had graduated with a bachelor’s degree or higher level. Ninety-one participants had children. One hundred participants were emergency medical technicians; 36 were doctors, nurses, or other medical personnel. The unit, where 51 of the participants worked, had employees who had caught COVID-19.
Table 2 shows the average scores for the variables and correlation analysis. As can be seen from the table, the participants’ institutional policies for COVID-19 were above average (3.30±0.82); work stress (2.99±0.88); and anxiety (2.65±0.56) were below average.
Table 2
Average scores for the variables and correlation analysis
| Mean | S.D. | 1 | 2 | 3 | |
| 1. Institutional policies | 3.30 | 0.82 | 1 | ||
| on COVID-19 | 3.30 | 0.82 | 1 | ||
| 2. Job stress | 2.99 | 0.88 | -.562** | 1 | |
| 3. Anxiety | 2.65 | 0.56 | -.525** | .513** | 1 |
According to the results of the correlation analysis, there is a negative correlation between the participants’ perception of the institutional policies related to their anxieties about COVID-19 (r = – 0.56) and work stress (r = – 0.53). Accordingly, the participants’ training related to the institutional policies on COVID-19, their protection, and the feeling of support reduces the level of work stress and anxiety. However, there is a positive relationship between work stress and the anxiety of the emergency department employees (r = 0.51). The analysis results are shown in Figure 1 and are presented in detail in Table 3.
Fig.1
Model 1.
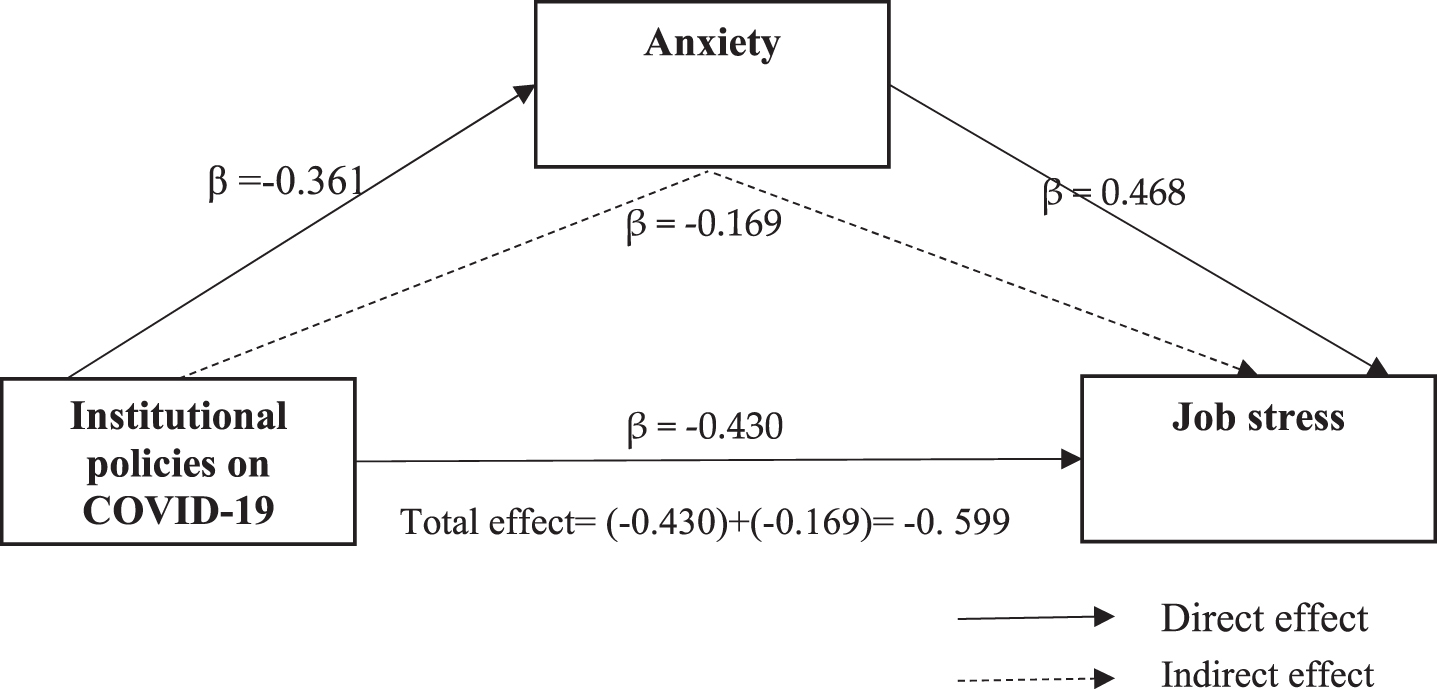
Table 3
Model 1 direct and indirect effects
| Variables | Direct | Indirect | Total | 95% CI | t | P |
| effect | effect | effect | ||||
| Institutional policies | -0.430 | -0.169 | -0.599 | [-0.461 – -0.261] | -7.145 | 0.000 |
| on COVID-19 | ||||||
| Anxiety | 0.468 | [0.222 – 0.714] | 3.763 | 0.002 |
The dependent variable is job stress; CI, confidence interval.
According to the analysis results, the institutional policy perception of the emergency healthcare service employees concerning reducing work stress was β= – 0.430; it was β= – 0.361 for anxiety. In contrast, anxiety increases work stress (β= 0.468). According to another finding, for COVID-19, anxiety plays a mediating role in the impact of the institutional policy perception on work stress; it further increases the impact of the employees’ institutional policy perception on work stress reduction (β= – 0.169). Anxiety alone increases work stress. However, increasing the institutional policy practices such as training, protection, and support for employees reduces anxiety levels. Anxiety increases work stress; however, institutional policies play a role in reducing this stress.
4Discussion
This study was conducted to determine the effect of COVID-19 institutional policies in emergency medical services on work stress and anxiety of healthcare employees. According to the results of this study, COVID-19 institutional policies, e.g., training, providing protective equipment to employees, and supporting the employees, reduces status anxiety of employees and their level of work stress. The results are similar to those reported in the literature. Letshaba and Chinomona [37], for example, conducted a study in the SME sector and concluded that organizational policies and employees’ work stress and anxiety are related, which supports the results of this study. Maunder et al. [31] noted that educating, supporting, and protecting employees during a pandemic reduces their psychological stress and risk of post-traumatic stress. Another study revealed that the social support perceived by healthcare employees during the COVID-19 pandemic also helped to reduce anxiety levels [38]. Furthermore, healthcare employees working in ambulance services should approach all cases with protective equipment because they maybe not be able to properly distinguish between confirmed and suspected cases. Furthermore, healthcare employees need to be supported in relation to mental difficulties they may experience as well as provided with personal protective equipment and to maintain their physical well-being [39]. This is why increasing the well-being and emotional endurance of healthcare employees is one of the main components of maintaining proper healthcare during the COVID-19 pandemic [40]. For this reason, protective equipment provided to healthcare employees will help to protect them against risks of transmission as well as providing psychological relief.
When the results in the literature and the results obtained from this study were evaluated, it can be said that the policies developed and followed by the institutions have a major impact on employees’ stress and anxiety levels. Given the above information, it can be seen that policies such as training at the macro- and micro-levels, the supply of personal protective equipment, and the physical and spiritual support of healthcare employees are necessary during the COVID-19 pandemic. It is thought that the levels of anxiety and stress of healthcare employees may decrease with the implementation of such policies.
According to another result obtained from this study, employee anxiety increased levels of work stress. This result corresponds to research findings [41– 45]. The research in the literature shows that the fear and anxiety experienced in a pandemic has a negative effect on health and well-being [46, 47]. When healthcare employees, as with other people in society, have incomplete or incorrect information about COVID-19, it increases their anxiety levels [38, 48]. In addition to the increased level of anxiety in their public life, when healthcare employees are in direct contact with infected people, it can further increase their overall anxiety levels. Healthcare employees’ anxieties about death of their colleagues, patients, and family members, as a result of COVID-19, can also cause stress [49]. On the other hand, healthcare employees contracting COVID-19 while doing their job, facing life risks, loneliness, physical fatigue, and being separated from their families can be the basis of critical physical and mental health problems [50, 51]. These conditions can reveal the anxiety and fear of healthcare employees [52]. In light of all this information, the anxieties that healthcare employees feel in public and professional life increase work stress. Because of this, healthcare institutions should provide training to healthcare employees in order to strengthen their psychological resilience, which plays an important role in protecting the employee’s health and in controlling the pandemic [28, 50].
Considering the results of this study, it seems that stress and anxiety levels of healthcare employees are still moderate. It is believed that an important reason for this is that most healthcare employees have access to protective equipment. Healthcare employees may feel more confident because they can provide necessary health services via utilizing protective equipment, which can help to reduce their anxiety and stress.
4.1Limitations
The study has important limitations. The first is that the study’s questionnaire application was conducted online. The online survey method has several advantages as well as disadvantages compared with the face-to-face survey method. The main disadvantages are that it is difficult for the person filling out the questionnaire to reach a researcher who can be consulted when something happens that they do not understand and does not allow the researcher to observe the person filling out the questionnaire. The second limitation of the study is related to the population in which it was conducted. Since the study was conducted in 112 emergency medical services units, participants consisted mainly of emergency medical technicians. The number of doctors, nurses, and other healthcare employees remained lower. The last limitation of the study is that the generalizability rate is low because the study was conducted in a single provincial center.
5Conclusion
According to the study’s results, healthcare managers should determine and control the anxiety and stress levels of healthcare employees on their staff. The policies developed and followed by the institutions, thus, will have an impact on these employees. The results of the study show that the political practices (i.e., aimed at enforcing the institutional measures taken against COVID-19) can be useful when it comes to reducing employees’ stress and anxiety levels. Accordingly, it is important that healthcare managers pay attention to the training of healthcare employees in regard to COVID-19 in addition to providing support and providing them with personal protective equipment.
Given the fact that trained manpower is the most valuable resource across countries universally, in order to minimize the loss of healthcare employees in the pandemic, various policies must be developed at the macro- and micro-levels. It is important to investigate how these developed policies affect healthcare employees.
Ethical approval
Before the field research was conducted, the necessary permissions and approvals were obtained from the Sakarya University Ethics Committee (19/05/2020 and E.4578), the Sakarya Provincial Health Directorate (dated 27/05/2020 and numbered E.688), and the Scientific Research Studies Commission of the Ministry of Health (2020-05-05T23_44_21). Also, the study has been conducted according to the principles of the Declaration of Helsinki.
Informed consent
All participants provided informed consent prior to enrollment.
Conflict of interest
The authors declare that there are no conflicts of interest.
Acknowledgments
The authors have no acknowledgments.
Funding
The authors report no funding.
References
[1] | WHO Coronavirus (COVID-19) Dashboard. Available at: https://covid19.who.int/ Accessed at: 22/06/2022. |
[2] | Türktemiz H , Ünal Ö , Aydın DB . Assessment of healthcare professionals’ perceptions and attitudes towards the COVID-19 pandemic in Turkey. Work. (Preprint), (2021) ;1–8. 10.3233/WOR-205305 |
[3] | WHO Coronavirus Disease (COVID-19) Outbreak: Rights, Roles And Responsibilities Of Health Workers, Including Key Considerations For Occupational Safety And Health. (2020) . https://www.who.int/docs/default-source/coronaviruse/who-rights-roles-respon-hw-COVID-19.pdf?sfvrsn=bcabd401_0 Accessed at: 27/09/2020. |
[4] | Lai J , Ma S , Wang Y , Cai Z , Hu J , Wei N ,... Tan H . Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open. (2020) ;3: (3):e203976–e203976. 10.1001/jamanetworkopen.2020.3976. |
[5] | Mayor S . COVID- impact on cancer workforce and delivery of care. The Lancet Oncology. (2020) ;21: (5):633. https://doi.org/10.1016/S1470-2045(20)30240-0 |
[6] | Bielicki JA , Duval X , Gobat N , Goossens H , Koopmans M , Tacconelli E , van der Werf S . Monitoring approaches for health-care workers during the COVID-19 pandemic. The Lancet Infectious Diseases. (2020) ;20: (10):e261–e267. 10.1016/S1473-3099(20)30458-8 |
[7] | Remuzzi A , Remuzzi G . COVID-19 and Italy: what next? The Lancet. (2020) ;395: :1225–8. https://doi.org/10.1016/S0140-6736(20)30627-9. |
[8] | Iversen K , Bundgaard H , Hasselbalch RB , Kristensen JH , Nielsen PB , Pries-Heje M , Knudsen AD , Christensen CE , Fogh K , Norsk JB , Andersen O , Fischer TK , Jensen CAJ , Larsen M , Torp-Pedersen C , Rungby J , Ditlev SB , Hageman I , Møgelvang R , Hother CE , Gybel-Brask M , Sørensen E , Harritshøj L , Folke F , Sten C , Benfield T , Nielsen SD , Ullum H . Risk of COVID-19 in health-care workers in Denmark: an observational cohort study. The Lancet Infectious Diseases. (2020) ;20: (12):1401–8. 10.1016/S1473-3099(20)30589-2. |
[9] | CDC. Characteristics of Health Care Personnel with COVID-19 — United States. MMWR Morb Mortal Wkly Rep. (2020) ;69: :477–481. http://+dx.doi.org/10.15585/mmwr.mm6915e6external icon |
[10] | International Council of Nurses (ICN). International Council of Nurses calls for data on healthcare worker infection rates and deaths, (2020) [17.08.2020]. Available from: https://www.icn.ch/sites/default/files/inline-files/PR_20_Infections%20and%20deaths%20from%20COVID-19%20among%20nurses.pdf. Accessed at: 27/09/2020. |
[11] | The World Medical Association. A call for urgent action to protect health professionals and carers, https://www.wma.net/wp-content/uploads/2020/04/A-call-for-urgent-action-to-protect-health-professionals-and-carers.pdf. Accessed at: 19/10/2021. |
[12] | https://www.medimagazin.com.tr/medilife//tr-saglik-bakani-rakamlari-acikladi-covId-19-salginina-yakalanan-saglik-calisani-sayisi-120-bini-gecti-10-686-92796.html Accessed at: 19/10/2021. |
[13] | Turkish Medical Association (Türk Tabipler Birliği), Covid-19 Pandemic 1st Year Evaluation Report, https://www.ttb.org.tr/kutuphane/1_yil_rapor.pdf Accessed at: 19/10/2021. |
[14] | Qiang F . Shanghai International Forum for Infection Control and Prevention. Rational, scientific, and standardized protection: the core of infection prevention and control of COVID-19 in medical institutions [in Chinese]. (2020) . Available at: https://mweixin.qq.com/s/G5Nwdd9kW9yVD-hTdwsKtg Accessed at: 29/09/2020. |
[15] | Bauchner H , Easley TJ . On behalf of the entire editorial and publishing staff of JAMA and the JAMA Network. Health Care Heroes of the COVID-19 Pandemic. JAMA. (2020) ;323: (20):2021. 10.1001/jama.2020.6197. |
[16] | Istanbul Medical Chamber (IMC), Sağlık çalışanlarının COVID-19 virüsüne maruz kalımına ilişkin risk değerlendirmesi https://www.istabiorg.tr/site_icerik//korona/COVID19_riskdegerlendirme.pdf Accessed at: 23/03/2022. |
[17] | Turkish Medical Association (TMA) Sağlık çalışanında Covid-19 tanısı iş kazası veya meslek hastalığıdır. https://www.ttb.org.tr/haber_goster.php?Guid=92238894-726a-11ea-b12d-d839943d748d Accessed at: 23/03/2022. |
[18] | Turkish Thoracic Society (Türk Toraks Derneği). (2020) . https://www.toraks.org.tr/site/news/5863 Accessed at: 27/09/2020. |
[19] | Selye H . The stress of life. NewYork: McGraw-Hill Book Company. (1956) . |
[20] | Selye H . Stress without distress. In: Serban G. (eds) Psychopathology of Human Adaptation. Springer, Boston, MA. (1976) . |
[21] | National Institute for Occupational Safety and Health (NIOSH 1999), Stress at Work (DHHS Publication No. 99-101), Cincinnati, OH: Author. https://www.cdc.gov/niosh/docs/99-101/pdfs/99-101.pdf?id=10.26616/NIOSHPUB99101. |
[22] | Esen M . The Relationship Between Job Stress, Burnout And Organizational Commitment: A Research On Health Employees (İş stresi, mesleki tükenmişlik ve örgütsel bağlılık ilişkisi: sağlık çalışanları üzerine bir araştırma). International Journal of Economic & Social Research. (2019) ;15: (1):1–13. |
[23] | National Center for Post-Traumatic Stress Disorder PTSD, (2020). Managing Healthcare Workers’ Stress Associated with the COVID-19 Virus Outbreak. https://www.ptsd.va.gov/COVID/COVID19ManagingStressHCW032020.pdf Accessed at: 27/09/2020. |
[24] | Blair L , Huzur Uyku Bozukluğu , Olumsuz Düşünce , Kaygı ve Stresle Baş Etme Yolları, çev. Ceren Aral. (Akılçelen Kitaplar, Ankara). (2014) . |
[25] | Karataş Z , Arslan D , Karataş ME . Examining Teachers’ Trait, State Cursive Handwriting Anxiety. Educational Sciences: Theory & Practice. (2014) ;14: (1):241–8. |
[26] | Peng EYC , Lee MB , Tsai ST , Yang CC , Morisky DE , Tsai LT ,... & Lyu SY . Population-based post-crisis psychological distress: an example from the SARS outbreak in Taiwan. Journal of the Formosan Medical Association. (2010) ;109: (7):524–32. |
[27] | Tang L , Pan L , Yuan L , Zha L . Prevalence and related factors of post-traumatic stress disorder among medical staff members exposed to H7N9 patients. International Journal of Nursing Sciences. (2017) ;4: (1):63–7. 10.1016/j.ijnss.2016.12.002. |
[28] | Huang JZ , Han MF , Luo TD , Ren AK , Zhou XP . Mental health survey of 230 medical staff in a tertiary infectious disease hospital for COVID-19. Zhonghua lao dong wei sheng zhi ye bing za zhi=Zhonghua laodong weisheng zhiyebing zazhi=Chinese. Journal of Industrial Hygiene and Occupational Diseases. (2020) ;38: (3):192–5. 10.3760/cma.j.cn121094-20200219-00063. |
[29] | Arca M , Dönmezdil S , Durmaz ED . The Effect of the COVID-19 Pandemic on Anxiety, Depression, and Musculoskeletal System Complaints in Healthcare Workers. Work. (2021) ;69: (1):47–54. 10.3233/WOR-205014. |
[30] | Potas N , Koçtürk N , Toygar SA . Anxiety Effects on Quality of Life During the COVID-19 Outbreak: A Parallel-serial Mediation Model Among Nurses in Turkey. Work. (2021) ;69: (1):37–45. 10.3233/WOR-205050. |
[31] | Maunder RG , Lancee WJ , Balderson KE , Bennett JP , Borgundvaag B , Evans S ,... Hall LM . Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerging Infectious Diseases. (2006) ;12: (12):1924–32. |
[32] | Spielberger CD , Gorsuch RL , Lushene RE . STAI manual for the State-Trait Inventory. Palo Alto. (1970) . |
[33] | Öner N , LeCompte WA . State-trait anxiety inventory handbook. Istanbul: Boğaziçi University Press. (1985) . |
[34] | Preacher KJ , Hayes AF . SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers. (2004) ;36: (4):717–31. |
[35] | Williams J , MacKinnon DP . Resampling and distribution of the product methods for testing indirect effects in complex models. Structural Equation Modeling: A Multidisciplinary Journal. (2008) ;15: (1):23–51. |
[36] | Qian J , Wang B , Han Z , Song B . Ethical leadership, leader-member exchange and feedback seeking: a double-moderated mediation model of emotional intelligence and work-unit structure. Frontiers in Psychology. (2017) ;8: :1174. |
[37] | Letshaba RK , Chinomona E . Organisational politics and job stress among SMEs employees. Journal of Contemporary Management. (2019) ;16: (2):459–80. |
[38] | Xiao H , Zhang Y , Kong D , Li S , Yang N . The effects of social support on sleep quality of medical staff treating patients with coronavirus disease (COVID-19) in January and February in China. Medical Science Monitor: International Medical Journal of Experimental and Clinical Research. (2020) ;26: :e923549-1. 10.12659/MSM.923549. |
[39] | The Psychiatric Association of Turkey (PAT), A Guide For Physicians And Healthcare Working With Covid-19 Fears And Anxiety (Hekimler ve Sağlık Çalışanları İçin COVID-19 Korku ve Kaygısıyla Baş Etme Rehberi), https://www.psikiyatri.org.tr/uploadFiles/213202011418-saglikcalisanibrosur.pdf Accessed at:19/10/2021. |
[40] | National Center for Post-Traumatic Stress Disorder (PTSD), Managing Healthcare Workers’ Stress Associated with the COVID-19 Virus Outbreak. https://www.ptsd.va.gov/COVID/COVID19ManagingStressHCW032020.pdf Accessed at: 19/10/2021. |
[41] | Dogru-Huzmeli E , Cam Y , Urfali S , Gokcek O , Bezgin S , Urfali B , Uysal H . Burnout and anxiety level of healthcare professionals during the COVID-19 pandemic in Turkey. Work. (2021) ;70: (1):21–9. 10.3233/WOR-210028. |
[42] | Şentürk E , Sağaltıcı E , Geniş B , Günday Toker Ö . Predictors of depression, anxiety and stress among remote workers during the COVID-19 pandemic. Work. (2021) ;70: (1):41–51. 10.3233/WOR-210082. |
[43] | Cebeci SP , Durmaz H . Determination of Depression, Anxiety and Stress Levels among Nurses Caring for Corona Virus Patients (Corona Virüslü Hastalara Bakım Veren Hemşirelerde Depresyon, Anksiyete ve Stres Düzeyinin Belirlenmesi). Journal of Ankara Health Sciences. (2021) ;10: (1):46–56. |
[44] | Aloğlu N , Gecdi T . Investigation of the Emotions of Health Personnel During the Pandemic Process in Terms of Some Variables (Sağlik Personelinin Pandemi Sürecinde Duygu Durumlarinin Bazi Değişkenler Açisindan İncelenmesi). Gevher Nesibe Journal of Medical & Health Sciences. (2021) ;6: (12):29–39. |
[45] | Spoorthy MS , Pratapa SK , Mahant S . Mental health problems faced by healthcare workers due to the Covıd-19 pandemic–A review. Asian Journal of Psychiatry. (2020) ;51: :102119. https://doi.org/10.1016/j.aj2020.102119 |
[46] | Pappas G , Kiriaze IJ , Giannakis P , Falagas ME . Psychosocial Consequences of Infectious Diseases. Clinical Microbiology and Infection. (2009) ;15: (8):743–7. https://doi.org/10.1111/j.14690691.2009.02947.x |
[47] | Ropeik D . The Consequences of Fear. EMBO Reports. (2004) ;5: (Suppl 1):S56–S60. https://doi.org/10.1038/sj.embor.7400228 |
[48] | Schwartz J , King CC , Yen MY . Protecting Healthcare Workers During The Coronavirus Disease (COVID-19) Outbreak: Lessons From Taiwan’s Severe Acute Respiratory Syndrome Response. Clinical Infectious Diseases. (2020) ;71: (15):858–60. https://doi.org/10.1093/cid/ciaa255 |
[49] | Cai H , Tu B , Ma J , Chen L , Fu L , Jiang Y , Zhuang Q . Psychological Impact and Coping Strategies of Frontline Medical Staff in Hunan Between January and March During the Outbreak of Coronavirus Disease (COVID-19) in Hubei, China. Medical Science Monitor: International Medical Journal of Experimental and Clinical Research. (2020) ;26: :e924171. 10.12659/MSM.924171 |
[50] | Kang L , Li Y , Hu S , Chen M , Yang C , Yang BX ,... Chen J . The mental health of medical workers in Wuhan, China dealing with the novel coronavirus. The Lancet Psychiatry. (2020) ;7: (3):e14. 10.1016/S2215-0366(20)30047-X |
[51] | Turkish Public Health Association (HASUDER), Health of Healthcare Workers in Combating Covid-19 Disease (Covid-19 Hastalığı İle Mücadelede Sağlık Çalışanlarının Sağlığı). https://korona.hasuder.org.tr/Covid-19-hastaligi-ile-mucadelede-saglik-calisanlarinin-sagligi/ Accessed at: 19/10/2021. |
[52] | Turkish Medical Association (TMA), Preliminary report of the Risk Assessment survey on Exposure of TMA Health Workers to the COVID-19 Virus has been announced (TTB Sağlık Çalışanlarının COVID-19 Virüsüne Maruz Kalımına İlişkin Risk Değerlendirmesi anketinin ön raporu açıklandı). https://www.ttb.org.tr/haber_goster.php?Guid=1af85302-6da7-11ea-a219-c213173be5c8 Accessed at: 19/10/2021. |




