Development and validation of a method to screen for co-morbid depression by non-behavioral health practitioners treating musculoskeletal pain
Abstract
BACKGROUND:
Although diagnosis and treatment of depressive illness is outside the scope of practice for non-behavioral health practitioners such as occupational therapists, physical therapists, kinesiotherapists, and chiropractors, it frequently is comorbid with painful musculoskeletal disorders such as low back pain and it negatively affects outcomes, including return to work. As psychologically-informed practice becomes more widely implemented without the immediate availability of behavioral health practitioners, safe and effective methods to screen for and appropriately triage depressive illness by nonbehavioral health practitioners are necessary.
OBJECTIVES:
To demonstrate the efficacy and validity of a method employed by non-behavioral health practitioners to screen for and appropriately triage musculoskeletal pain patients who also are experiencing depressive illness.
METHODS:
As part of a previously-published psychometric research study conducted in a community-based musculoskeletal pain rehabilitation program, a method was developed for nonbehavioral health practitioners to screen for and appropriately triage patients for co-morbid depressive illness, thus providing the current opportunity to examine the effects of depressive illness on work outcomes. The first step in the two-step process involves a 22-item questionnaire, providing scores used in the second step to triage for outside consultation with behavioral health practitioners. This paper describes the screening method and its application in an observational study of the impact of depressive illness on work outcomes.
RESULTS:
Among 156 consecutive patients who were presenting with musculoskeletal pain disorders to an outpatient rehabilitation program, 22.3% also were identified to have co-morbid clinical depression. The screening process allowed all patients to continue in the rehabilitation program. Those who were already receiving behavioral health care were encouraged to inform care providers of their participation in the program. Those who were not receiving behavioral health care were successfully triaged to care outside of the clinic. Depressive illness was found to affect success in the program, confirming the validity of the screening process for outpatient rehabilitation program participants experiencing chronic pain.
CONCLUSIONS:
A simple and effective depression screening process that triages patients without interruption of musculoskeletal treatment can be employed by nonbehavioral health practitioners. Because return to work outcomes were found to be negatively affected by depressive illness, this approach has the potential to improve overall program efficacy.
1Introduction
For decades, among all the causes of work disability, low back pain has been one of the most prevalent and costly health problems encountered by industrialized societies and is now the leading cause of disability throughout the world [1]. The most recent estimated global point-prevalence of 11.9% is likely to increase, which will increase economic costs as workforces age [2]. Against this backdrop, methods to successfully understand and treat musculoskeletal pain in general and low back pain in particular have gradually improved [3], leading to the availability of effective clinical practice guidelines (CPG) in many developed countries [4, 5]. Preventing transition from acute pain to chronic pain is a central feature of all CPGs for physical therapists [6], such that chronic musculoskeletal pain is now seen as the natural consequence of acute treatment failure.
For chronic disabling pain of all sorts, a broad consensus has been reached that occupational rehabilitation is most effectively provided on an interdisciplinary basis [7] using a biopsychosocial (BPS) model [8]. The need for the BPS model for chronic pain is partly driven by the comorbid nature of chronic pain with depression [9], a key risk factor for treatment failure [10] especially when return to work is a measured outcome [11]. Depression is co-morbid in about 50% of people who have a chronic painful condition lasting six months or longer [12]. Even without chronic pain, 6.9% of U.S. adults experienced at least one major depressive episode in the past year and 13.2% experience at least one major depressive episode in their lifetime [13]. Depression and other emotional problems (21.0%) are second only to back and neck disorders (30.3%) as causes of work disability [14]. In rehabilitation programs, depressive symptoms have moderate to large effects on pain ratings and significant negative effects on functional status, leading to consistently detrimental outcomes [15]. With back pain rehabilitation patients especially, depression poses several treatment problems [16], including diminishing program compliance [17] and spinal surgery failure [18]. The comorbidity of depression with chronic musculoskeletal pain requires integrated care, which is optimally provided in the biopsychosocial model.
The need to address the comorbidity of musculoskeletal pain and depression with the biopsychosocial model poses challenges to non-behavior health (NBH) practitioners because access to behavioral health colleagues is not readily available. Although physical therapists and other NBH practitioners have been encouraged to include psychosocial perspectives in the treatment of low back pain [19] and recent physical therapy training encourages a biopsychosocial approach [20], “the assessment and management of all of these factors cannot be integrated into everyday practice” [19]. Indeed, the 2019 edition of the National Physical Therapy Examination Review & Study Guide does not address depression screening and management [21]. The observation that “there is a small subset of patients receiving PIP for musculoskeletal pain that should have mental health provider involvement” [20] appears to underestimate the prevalence of depression among patients referred for physical therapy. For example, in a study of 232 patients presenting to physical therapists with low back pain, 40% of the patients had symptoms of depression and 24% scored in the moderate to extremely severe depression range [22]. In this study, the physical therapists’ ability to identify depression was only slightly better than chance. The difficulties faced by physical therapists to address the comorbidity of depression and musculoskeletal pain are likely to be faced by all nonbehavioral health practitioners providing services to patients with musculoskeletal pain. This suggests the potential need for a method that nonbehavioral health practitioners can use to systematically screen for and address depression.
The purpose of this paper is to describe and test the validity of a method that was developed for NBH professionals to screen for depression among patients who present with a range of painful musculoskeletal disorders. This method grew out of a recently-published research project [23] that required NBH practitioners to screen patient volunteers for depressive symptoms as an exclusion criterion because the study focused on psychometric characteristics of measures that would be contaminated by their depressive illness. If the method is valid, participants screened positive for depressive illness will score higher on self-reported pain and lower on self-reported physical ability at baseline, and will experience worse return to work transition outcomes after treatment.
2Methods
2.1Sampling and procedures
The current paper is the byproduct of an observational study conducted with a convenience sample of English-speaking and Spanish-speaking adult participants recruited on admission at three “stand-alone” outpatient physical therapy centers in Southern California. The sponsoring research foundation’s Institutional Review Board approved the experimental protocol and monitored the research activities. All candidates for enrollment provided written informed consent prior to participation. Following completion of the consent procedures, 157 participants age 19 years to 69 (mean, SD = 44.8, 12.5) years with duration of presenting musculoskeletal pain disorder from acute to 47 (mean, SD = 2.4, 4.5) years completed baseline testing. Participants presented with soft-tissue spine impairment (41%), upper extremity impairment (35%), lower extremity impairment (24%). Between baseline testing and the 30-day follow-up testing, all participants continued in the active outpatient physical therapy program for musculoskeletal conditions consisting of rehabilitative exercises, manual therapies, and adjunctive modalities using a measurement-driven approach along with a home exercise program. Typically, each participant participated in eight therapy sessions over the 30-days.
2.2Data acquisition
Data were retained from all consented participants, including those whose data subsequently were excluded from the psychometric research study. At the conclusion of the study, telephone interviews were undertaken with all consented participants to determine work status. Because the participants who were excluded had continued to participate as usual in physical therapy and had given consent for participation, they were included in the telephone follow-up.
2.3Measures
Baseline testing was conducted with three instruments, the Older Adult Health and Mood Questionnaire [24] (OAHMQ), the Multidimensional Task Ability Profile (MTAP) [25], and a 10 cm visual analogue pain scale (VAS) [26]. The OAHMQ was recorded with paper and pen, while the MTAP and the VAS pain scale were recorded using a computer kiosk.
2.3.1Older Adult Health and Mood Questionnaire (OAHMQ)
With two scales to address both dysphoric mood and the cognitive and behavioral and physiologic indicators of depression, the OAHMQ (Table 1) includes 22 self-descriptive items to be used as a screening instrument for depression among older adults participating in outpatient rehabilitation. The OAHMQ was developed at the Clinical Gerontology Service at Rancho Los Amigos National Rehabilitation Center (Downey, CA, USA), an outpatient interdisciplinary rehabilitation setting in which psychological factors such as depression are assumed to affect participation and outcomes. The OAHMQ was developed as a brief multifocal depression screen that would offer better utility in a biopsychosocial program than unifocal screeners including the Beck Depression Inventory [27], Zung Depression Scale [28], Geriatric Depression Scale [29], Hamilton Depression Rating Scale [30], and the Centers for Epidemiological Studies Questionnaire [31]. The critique of these instruments that provides the rationale for OAHMQ development is described elsewhere [24].
Table 1
Older Adult Health and Mood Questionnaire
| 1 | My daily life is not interesting. | T or F |
| 2 | It is hard for me to get started on my daily chores and activities. | T or F |
| 3 | I have been more unhappy than usual for at least a month. | T or F |
| 4 | I have been sleeping poorly for at least the last month. | T or F |
| 5 | I gained little pleasure from anything. | T or F |
| 6 | I feel listless, tired, or fatigued a lot of the time. | T or F |
| 7 | I have felt sad, down in the dumps, or blue much of the time during the last month. | T or F |
| 8 | My memory or thinking is not as good as usual. | T or F |
| 9 | I have been more easily irritated or frustrated lately. | T or F |
| 10 | I feel worse in the morning than in the afternoon. | T or F |
| 11 | I have cried or felt like crying more than twice during the last month. | T or F |
| 12 | I am definitely slowed down compared to my usual way of feeling. | T or F |
| 13 | The things that used to make me happy don’t do so anymore. | T or F |
| 14 | My appetite or digestion of food is worse than ever. | T or F |
| 15 | I frequently feel like I don’t care about anything anymore. | T or F |
| 16 | Life is really not worth living most of the time. | T or F |
| 17 | My outlook is more gloomy than usual. | T or F |
| 18 | I have stopped several of my usual activities. | T or F |
| 19 | I cry or feel saddened more easily than a few months ago. | T or F |
| 20 | I feel pretty hopeless about improving my life. | T or F |
| 21 | I seem to have lost the ability to have any fun. | T or F |
| 22 | I have regrets about the past that I think about often. | T or F |
Note: This embodies two sub-scales. The odd-numbered items reflect mood-related aspects of depression, while the even-numbered items reflect the cognitive, behavioral, and physiologic aspects of depression. A Spanish-language version is also available.
All OAHMQ “True” items are scored as 1, with a total score summed across the instrument. A total score of 4 or higher is optimal for identifying clinically significant depressive symptoms, while a score of 11 or higher indicates a probable major depressive episode. When screening for any depressive disorder given a score of 11 or above, sensitivity was 0.93 and the specificity was 0.87. The odd-numbered items reflect mood-related aspects of depression, while the even-numbered items reflect the cognitive, behavioral, and physiologic aspects of depression. A Spanish-language version has good psychometric properties.
In consultation with the OAHMQ lead developer based on review of the sensitivity/specificity cut-off scores for this instrument, the research project set a score of 9/22 to indicate a level of depressive symptoms that would exclude the participant’s data. Although this is below the score of 11/22 that the original OAHMQ study [24] indicated had a high likelihood of a major depressive disorder, 9/22 was considered to be sufficiently elevated to require closer review and possible study exclusion followed by appropriate triage.
2.3.2Multidimensional Task Ability Profile (MTAP)
A 50-item computer-administered and scored patient-reported outcome measure consisting of drawings with text captions depicting a wide range of physical work tasks and activities of daily living (Fig. 1) with difficulty levels and a rating scale that have been calibrated using the item response theory rating scale method of Rasch analysis [32].
Fig. 1
Sample MTAP items: Panel “A” Carry a full laundry basket up one flight of stairs; Panel “B” Get into an automobile driver’s seat; Panel “C” Use an electric sander to smooth a table top; Panel “D” Write a shopping list with a pencil.
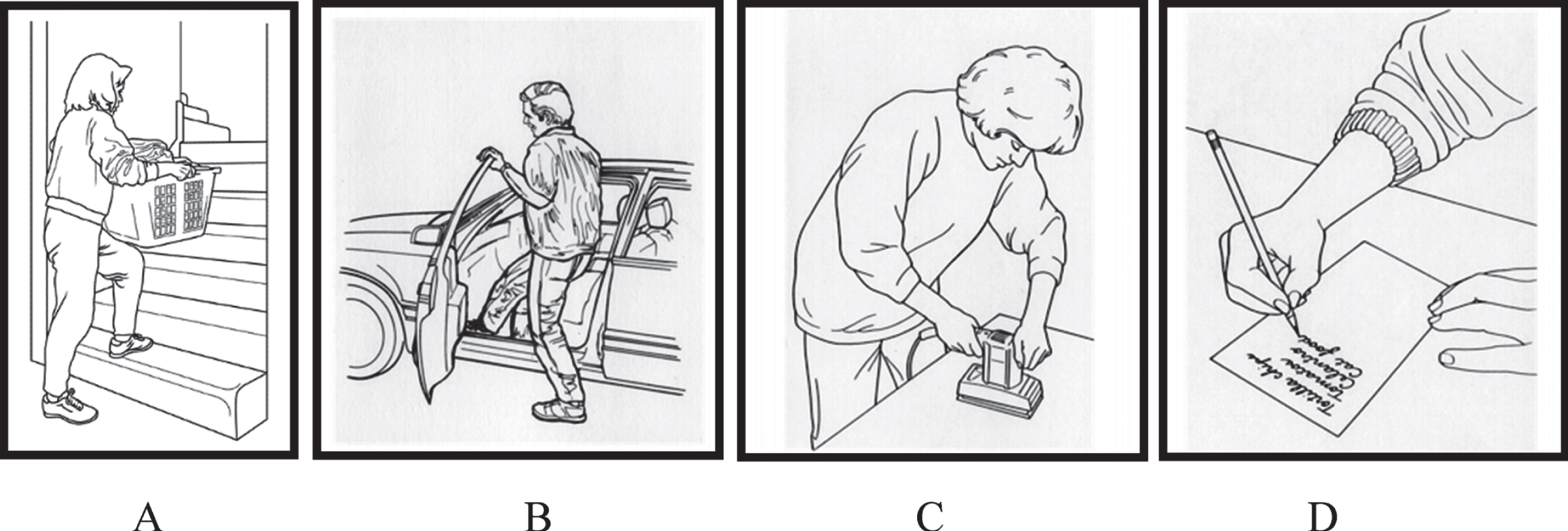
For each item, the MTAP uses a five-level ordinal rating scale (Able, Slightly Restricted, Restricted, Very Restricted, Unable). Items are presented one at a time, starting with items that have the least physical demand. Missed items are not allowed with the computer interface. The mean time to complete the MTAP is approximately 6 minutes to 8 minutes. Once the participant completes the test, the computer automatically scores the responses with this score-weighting rubric: Able = 4, Slightly Restricted = 3, Restricted = 2, Very Restricted = 1, Unable = 0. Weighted item scores are summed over the instrument to calculate a global score ranging from 0 to 200, with higher scores indicating more ability.
2.3.310 cm visual analog pain scale (VAS)
After computer administration of the MTAP, the VAS also was computer-administered to the participant. Presented on the screen of the computer kiosk as a 10 cm horizontal scale anchored at zero = “No Pain”, to 10 = “Worst Imaginable Pain”, the mark along the scale is taken as the participant’s self-rating of nociceptive experience.
2.4Depression screening and triage process
In the original psychometric research study, to avoid contaminating the inter-test comparisons of the patient self-report measures, volunteer patients were screened by a physical therapist and/or a chiropractor for clinical depression, following the flowchart model in Fig. 2.
Fig. 2
Two-step non-behavioral health (NBH) depression screening and triage.
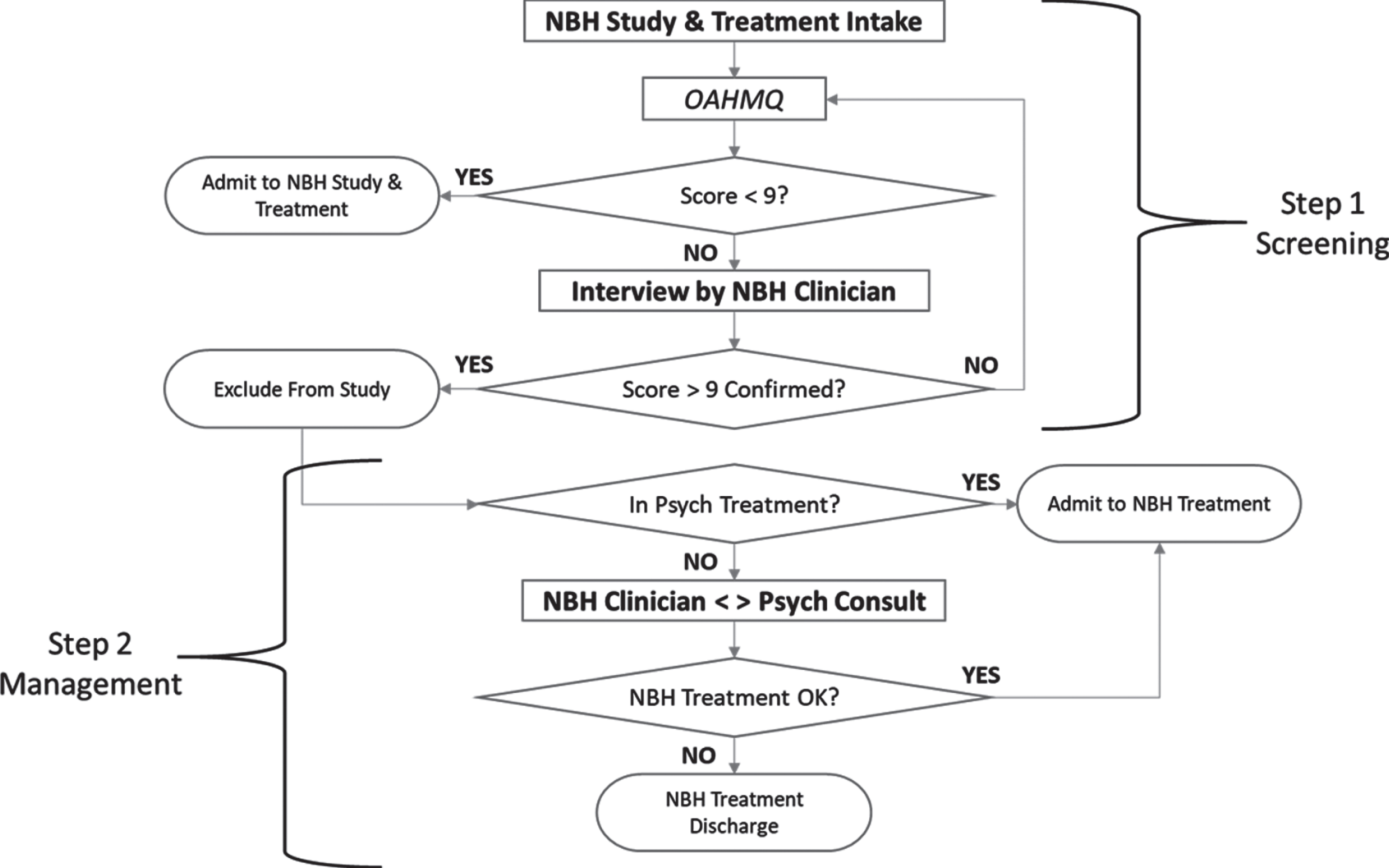
2.4.1Step 1 –Non-behavioral health practitioner screening
The depression screening process begins on admission. After informed consent is provided by the patient, the screening instrument is administered. In this study, a score on the OAHMQ of 9/22 or above is the trigger for review. If the score is 8/22 or lower, the patient is admitted to the study and the treatment program. If the score is 9/22 or higher, the NBH practitioner (a physical therapist and/or chiropractor) interviews the participant to confirm understanding of the items and allows a response to be changed if the participant desires.
2.4.2Step 2 –Behavioral health practitioner consultation and triage
If the confirmed score on the OAHMQ is 9/22 or above, the NBH practitioner enquires about whether or not the participant is receiving psychotherapy and/or medication to treat depression. If the participant was not receiving medication or treatment, the study’s principal investigator (an NBH chiropractor) consulted with an “on-call” psychologist as an off-site consultant to identify the need for a telephone interview with the participant by an “on call” psychiatrist participating as an off-site consultant to determine if the participant could continue in physical therapy or required treatment hiatus to receive immediate behavioral health intervention. The primary concern was suicidality, but other serious mental disorders were also under consideration. Note that this consultation and, if necessary a follow-up telephone interview can be undertaken with any licensed behavioral health practitioner. In the current study, the psychologist was licensed in another state that allowed behavioral health consultation but not direct patient intervention; the psychiatrist was licensed in the state in which the patients resided. Whenever it is possible that intervention with a patient may be required by a behavioral health practitioner, it is necessary for the practitioner to be licensed in the state or province in which the patient resides.
Using the OAHMQ score of 9/22 as the trigger for this two-step process, 35 of the 156 participants (22.3%) were identified as experiencing depressive illness. Twenty-eight (28) were receiving treatment and/or medications for depression which was presumed to be adequate and not requiring additional intervention other than recommending that these participants inform their behavioral health provider that they were participating in physical therapy. The remaining seven (7) participants were interviewed via telephone to confirm the need for psychological treatment and/or suicidality that would preclude ongoing participation in physical therapy. Of these, five participants were found to not require immediate intervention, while two participants were directed to immediate psychiatric treatment. None of the participants were found in the consultation between the NBH practitioner and the behavioral health practitioner to require hiatus from physical therapy. For all 35 of the participants who were identified in the two-step process to be experiencing depressive illness, other than increasing the sensitivity of the treatment staff to potential issues with poor motivation and catastrophizing behavior, the information was not formally integrated into the physical therapy plan of care.
2.5Post-study telephone interview
One month after conclusion of the study, participants received a telephone interview by study personnel to assess work status through two questions: 1) “Were you working when you first started the study?” 2) “Are you working now?” Depending on when the participant concluded study participation, these data were collected 1–9 months (mean±SD: 155±80 days; range: 32–260 days) after visit 3.
3Data management and analysis
After auditing and arithmetic manipulation in Excel, the data were exported to SPSS version 25 (Armonk, NY), which was used to perform statistical analyses, including basic descriptive analyses and analyses to examine validity as described below. Descriptive statistics for continuous data were summarized with mean, standard deviation values, while categorical data were summarized with frequency counts and percentages. Statistical significance was set at α= 0.05.
4Results
Of the 157 participants who were initially consented and completed the OAHMQ, 156 completed the baseline test battery, including 92 native English speakers and 64 native Spanish speakers. After completion of the treatment program, 137 participants (88%) responded to the telephone interview follow-up and provided information about work status, only one of whom was unable to provide information about pre-treatment work status.
4.1Demographic comparisons
A series of one-way analyses of variance comparing participants who were identified as experiencing depressive illness with non-depressed participants found no differences on demographic characteristics for age, the duration of disability, or body mass index (all p > 0.05). Chi-square analyses also found no differences on gender, native language, and whether or not the person was working at baseline or at follow-up (all p > 0.05).
4.2Depressed versus nondepressed participants
To examine the comorbidity of musculoskeletal pain and depression in this sample, a series of one-way analyses of variance were conducted, with groupwise results presented in Table 2.
Table 2
Baseline test battery scores of depressed versus nondepressed participants
| Variable | Depressed? | N | Mean | SD | Min | Max |
| OAHMQ (0–22) | Yes | 35 | 13.97 | 3.19 | 9 | 22 |
| No | 122 | 4.12 | 4.01 | 0 | 19 | |
| Total | 157 | 6.32 | 5.62 | 0 | 22 | |
| VAS (0–10) | Yes | 34 | 5.22 | 2.57 | 0.0 | 10.0 |
| No | 122 | 4.27 | 2.37 | 0.0 | 9.5 | |
| Total | 156 | 4.48 | 2.44 | 0.0 | 10.0 | |
| MTAP (0–200) | Yes | 34 | 103.18 | 35.57 | 33 | 170 |
| No | 122 | 133.61 | 46.40 | 15 | 200 | |
| Total | 156 | 126.97 | 45.92 | 15 | 200 |
Key: OAHMQ: Older Adult Health and Mood Questionnaire - higher score equals worse mental status. VAS: Pain intensity assessed on a 10 cm visual analog scale - higher score equals worse pain; MTAP: Multidimensional Task Ability Profile - higher score equals better physical function.
These analyses found the expected difference on the OAHMQ score (F1,155 = 178.54, p < 0.001), along with significant differences for scores on the VAS score (F1,154 = 4.11, p = 0.044), and the MTAP score (F1,154 = 12.54, p = 0.001). Depressed participants had higher VAS scores and lower MTAP scores.
4.3Work status
Of the 136 participants for whom both pre-treatment and post-treatment work status data were collected, 60 were working prior to treatment and 67 were working at follow-up. A chi-square analysis revealed no categorical trends in terms of gender or native language at either time (both p > 0.05).
To examine the effect of depressive symptoms on work status outcomes, grouping the comparison of outcomes in terms of the clinical value was undertaken using the ordinal ranking rubric described in Table 3.
Table 3
Return to work outcome rubric
| Rank order | Transition | Value |
| 1 | Not Working to Working | Positive |
| 2 | Working to Working | Neutral |
| Not Working to Not Working | ||
| 3 | Working to Not Working | Negative |
This method of ranking clinical value is based on the transition from not working to working having the highest value of clinical significance, the transition from working to not working having the lowest value, and the remaining two transition groups demonstrating no change. The ranked value of these transition groups was used as a factor to examine comparisons among the groups in terms of scores on the OAHMQ, MTAP, and VAS. The data describing the scores for the three ranked groups are presented in Table 4.
Table 4
Pre-treatment prediction of transition to/from working vs not-working
| Factor | Transition | N | Mean | SD | 95% CI | |
| Lower | Upper | |||||
| OAHMQ Total (0–22) | Positive | 33 | 3.97 | 5.09 | 2.16 | 5.77 |
| Neutral | 61 | 6.85 | 5.62 | 5.41 | 8.29 | |
| Negative | 42 | 6.74 | 6.16 | 4.82 | 8.66 | |
| Total | 136 | 6.12 | 5.76 | 5.14 | 7.09 | |
| VAS (0–10) | Positive | 33 | 3.970 | 2.45 | 3.10 | 4.84 |
| Neutral | 60 | 4.117 | 2.38 | 3.50 | 4.73 | |
| Negative | 42 | 5.083 | 2.45 | 4.32 | 5.85 | |
| Total | 135 | 4.381 | 2.45 | 3.97 | 4.80 | |
| MTAP (0–200) | Positive | 33 | 144.94 | 42.13 | 130.00 | 159.88 |
| Neutral | 60 | 129.13 | 46.01 | 117.25 | 141.02 | |
| Negative | 42 | 111.14 | 49.59 | 95.69 | 126.60 | |
| Total | 135 | 127.40 | 47.63 | 119.29 | 135.51 | |
Key: SD = standard deviation; CI = confidence interval; OAMHQ = Older Adult Health and Mood Questionnaire; VAS = visual analog scale pain intensity; MTAP = Multidimensional Task Ability Profile.
A series of one-way analyses of variance comparing outcome transitions across the three baseline measures found that the VAS pain scale score did not significantly predict work outcome (F2,132 = 2.612, p = 0.077), but that there were significant differences among the work outcome groups with regard to both the OAHMQ score (F2,133 = 3.128, p = 0.047) and the MTAP score (F2,132 = 5.007, p = 0.008). A post-hoc analysis based on Fisher’s least significant difference test is depicted in Table 5.
Table 5
Post hoc analysis (LSD) of outcome transition based on pre-treatment scores
| Baseline measure | Outcome transition | Mean difference | p | |
| OAHMQ Total (0–22) | Positive | Neutral | –2.88* | 0.020 |
| Negative | –2.77* | 0.038 | ||
| Neutral | Positive | 2.88* | 0.020 | |
| Negative | 0.11 | 0.920 | ||
| Negative | Positive | 2.77* | 0.038 | |
| Neutral | –0.11 | 0.920 | ||
| MTAP (0–200) | Positive | Neutral | 15.81 | 0.117 |
| Negative | 33.80* | 0.002 | ||
| Neutral | Positive | 15.81 | 0.117 | |
| Negative | 17.99 | 0.055 | ||
| Negative | Positive | 33.80* | 0.002 | |
| Neutral | –17.99 | 0.055 | ||
Key: *Significant at the < .05 level (2-tailed). OAMHQ = Older Adult Health and Mood Questionnaire; VAS = visual analog scale pain intensity; MTAP = Multidimensional Task Ability Profile.
Participants who transitioned over the course of treatment from either negative to positive or from neutral to positive had significantly lower OAHMQ total scores, consistent with depressive symptoms being inversely related to successful return to work transition. Participants who transitioned from negative to positive over the course of treatment demonstrated significantly higher MTAP scores, but relationship between MTAP score and transition from neutral to either positive or negative was not found.
5Discussion
5.1Hypotheses confirmation
A method for nonbehavioral health practitioners to screen for comorbid depression among patients presenting with musculoskeletal pain is described and tested in terms of its concurrent validity and predictive validity. The hypothesized concurrent relationships between depression identified by the screening method and both self-reported pain and functional ability at intake are found, as are the predictive relationships between depression identified at the initiation of musculoskeletal treatment and eventual return to work transition.
5.2Screening for depression
Depression is beyond the scope of practice for NBH practitioners although the prevalence of depression is much higher for people with chronic musculoskeletal pain. Depression is associated with lower levels of treatment efficacy including delay in return to work and duration of disability [33], as well as both reduced work participation and reduced work functioning [34], all of which are important outcomes for treatment of musculoskeletal pain. The use of a screening method to identify musculoskeletal pain patients who are experiencing comorbid depression can be used in value-based payment programs to compensate for the poorer outcomes likely to be found when treating people with depression.
This study presents a two-step method described in Figure 2 that was developed for NBH practitioners to address depression in outpatient musculoskeletal pain rehabilitation. This method is based on the Older Adult Health and Mood Questionnaire (OAHMQ), a 22-item depression screening instrument with two subscales that tap complimentary components of depressive illness. The OAMHQ was developed for use by NBH professionals to screen for depressive symptoms in a physical medicine and rehabilitation setting and is available in both English and Spanish. The use of a score of 9/22 as the trigger for the nonbehavioral health practitioner to seek behavioral health consultation is borne out by the current research. Across the three community-based musculoskeletal pain rehabilitation clinics in which the two-step process was implemented, 22.3% of the patients had comorbid depression. This is similar to the 24.5% for moderate or worse depression among outpatients with low back pain identified by the Depression Anxiety Stress Scales-21 [35] in similar outpatient settings in Australia [22].
The current study found that none of the 35 participants who scored 9/22 or above on the OAHMQ were not in need of care for depressive illness. This indicates that using the score of 9/22 as the cut-point is too high; a lower score would provide better balance between sensitivity and specificity, to identify more participants with depression as well as a few “false positives”. In the original research on development of the OAHMQ [24], 23% of the participants had scores of three or less, while 37% had scores of 4 through 10, which the test developers proposed to indicate a depressive disorder that was not major, and 40% had scores above 10. Of this latter group, 76% of the participants were found to have a major depressive disorder. In the current study, 60% of the participants had scores of 4 or greater. In future studies with this instrument, a score of 7/22 or 8/22 should be used to screen for significant depressive symptoms in Step 1 of the process.
Using the 9/22 score in the process described in Fig. 2, there were no differences in terms of gender, native language, or work status at the start of the program or after treatment concluded. The expected group-wise differences were found for both the VAS pain scale score and the score for the Multidimensional Task Ability Profile (MTAP). The cross-sectional nature of this study does not support causality, but the biopsychosocial model presumes interaction among the variables of pain, depression, and self-perceived physical function [36]. Providing to nonbehavioral health practitioners the tools to screen for depression allows the sole practitioner to become a potential entry point for the patient into an interdisciplinary biopsychosocial program.
5.3Efficacy of the OAMHQ in screening
The OAMHQ subscales to measure dysphoric mood and cognitive-behavioral-physiologic symptoms of depression were useful during Step 2 of this process. The primary advantage of the OAMHQ is the availability of the two subscales, with dysphoria modestly predominant for participants in this study who were identified as experiencing depressive illness. The opportunity to focus nonbehavioral health interventions on the even-numbered items that reflect symptoms that are reasonably considered amenable to intervention within the scope of NBH practice seems to be important. For example, OAMHQ symptoms involving motivation (item 2 and item 20), insomnia (item 4), fatigue (item 6), appetite and digestion (item 14), and inactivity (item 18) are not only “psychiatric”, but can reasonably be addressed by physical therapists, occupational therapists, and chiropractic professionals.
Although dysphoric mood is often the predominant symptom, depression also impacts cognition, social behavior, and physiology. Screening measures for depressive illness that are sensitive to these components should be used whenever possible. As the biopsychosocial model continues to evolve, methods that recognize the interplay among the three major components of the model must be developed.
5.4Work outcomes
In addition to describing a method for physical therapists to screen for depression in physical therapy practice, this study examined the impact of depression on work outcomes through the use of a rubric that ranked work transition pre-post treatment. This rubric is the simplest approach to ordinal ranking both program intake and exit; it provides unequivocal data that are easy to collect. Using this approach, the VAS pain scale was found to not be predictive of outcome, but the OAHMQ total score, as well as the MTAP score were associated with successful work transitions. Pain patients with depression can become more activated through physical therapy, with an increased likelihood of successful return to work outcomes.
5.5Practical applications
Depression is a major cause of disability and lost work productivity and can interfere with physical therapy. While the biopsychosocial approach to musculoskeletal pain rehabilitation is widely endorsed, barriers to implementation exist for individual practitioners who do not have direct access to behavioral health colleagues. This study has demonstrated the feasibility of a routine depression screening process for patients with musculoskeletal pain disorders in outpatient practices. Screening can help nonbehavioral health practitioners participate in interdisciplinary biopsychosocial management by referral to behavioral health services. In addition, as value-based insurance reimbursement proliferates, the proper weighting of difficulty in treating musculoskeletal pain patients with comorbid depression is necessary.
5.6Limitations
This study used a convenience sample of patients at three “stand-alone” outpatient physical therapy clinics in Southern California that were not affiliated with a hospital, rehabilitation center, or surgical practice. Thus, natural selection has probably biased these results. However, the range of chronicity of the musculoskeletal conditions treated in these three practices is sufficiently broad that the findings are likely to be pertinent in most other community-based physical therapy settings.
As noted above, the cut-point of 9/22 is valid and useful, but likely to be too high in that there were no “false positive” patients identified without depression. This argues for a lower cut-point coupled with a robust screening program that identifies patients who have elevated scores but are not in need of treatment for depression. A false positive rate of 5% to 10% is reasonable to consider.
5.7Future research
Research should be undertaken with the OAMHQ (and other instruments so utilized) to determine an optimal score that balances sensitivity and specificity. While treating dysphoric mood is important, other aspects of depression such as physical activation and social participation should be assessed by nonbehavioral health practitioners.
6Conclusion
Depressive illness on intake to treatment for musculoskeletal pain is concordant with lower self-perceived physical ability prior to treatment and predicts lower return to work outcome. Nonbehavioral health practitioners can screen for depression and consult with behavioral health colleagues to properly address patients with elevated scores. Physical therapists and other non-behavioral health practitioners who participate in value-based payment programs can identify those patients with comorbid depression who are thereby likely to be more difficult and experience poorer outcomes, thus providing more appropriate levels of reimbursement based on adjusted outcome expectations.
Conflict of interest
Leonard Matheson and Joe Verna benefit financially from MTAP sales and subscriptions. John Mayer received compensation for contributing to this project.
Ethical statement
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5). Informed consent was obtained from all patients for being included in the study.
Funding
This study was funded by the Vert Mooney Research Foundation, a 501c(3) charitable organization that developed and currently owns the Multidimensional Task Ability Profile. Leonard Matheson, John Mayer, and Joe Verna are board members of the Vert Mooney Research Foundation. The OAHMQ is available in both English and Spanish without cost to healthcare practitioners from the current study’s authors.
Acknowledgments
The authors thank the staff of Spine & Sport Inc. for assistance with coordination and data collection for this study.
References
[1] | Buchbinder R , et al. Placing the global burden of low back pain in context. Best Practice & Research Clinical Rheumatology. (2013) ;27: (5):575–89. |
[2] | Hoy D , et al. A systematic review of the global prevalence of low back pain. Arthritis & Rheumatism.. (2012) ;64: (6):2028–37. |
[3] | Deyo RA , et al. Report of the NIH Task Force on research standards for chronic low back pain. Physical Therapy. (2015) ;95: (2):e1–e18. |
[4] | Koes BW , et al. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. European Spine Journal. (2010) ;19: (12):2075–94. |
[5] | Hanney WJ , et al. The Influence of Physical Therapy Guideline Adherence on Healthcare Utilization and Costs among Patients with Low Back Pain: A Systematic Review of the Literature. PLoS One. (2016) ;11: (6):e0156799. |
[6] | Childs JD ,et al. Implications of early and guideline adherent physical therapy for low back pain on utilization and costs. BMC Health Services Research. (2015) ;15: (1):150. |
[7] | Hoefsmit N , Houkes I , Nijhuis FJ . Intervention characteristics that facilitate return to work after sickness absence: a systematic literature review. Journal of Occupational Rehabilitation. (2012) ;22: (4):462–77. |
[8] | Gatchel RJ ,et al. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychological Bulletin. (2007) ;133: (4):581. |
[9] | Gatchel RJ . Comorbidity of chronic pain and mental health disorders: the biopsychosocial perspective. American Psychologist. (2004) ;59: (8):795. |
[10] | Pincus T ,et al. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine. (2002) ;27: (5):E109–20. |
[11] | Baldwin M ,et al. Self-reported severity measures as predictors of return-to-work outcomes in occupational back pain. Journal of Occupational Rehabilitation.. (2007) ;17: (4):683–700. |
[12] | Bair MJ ,et al. Depression and pain comorbidity: a literature review. Archives of Internal Medicine.. (2003) ;163: (20):2433–45. |
[13] | Author, National-Level Comparisons of Mental Health Estimates from the National Survey on Drug Use and Health and Other Data Sources - NSDUH Methodological Report. 2018, Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration: Research Triangle Park, North Carolina. p. 110. |
[14] | Theis KA ,et al. Prevalence and causes of work disability among working-age US adults, –NHIS. Disability and Health Journal. (2018) ;11: (J1):108–15. |
[15] | Rayner L ,et al. Depression in patients with chronic pain attending a specialised pain treatment centre: prevalence and impact on health care costs. Pain. (2016) ;157: (7):1472. |
[16] | Pinheiro MB ,et al. Symptoms of depression as a prognostic factor for low back pain: a systematic review. The Spine Journal. (2016) ;16: (1):105–16. |
[17] | DiMatteo MR . Social support and patient adherence to medical treatment: a meta-analysis. Health Psychology. (2004) ;23: (2):207. |
[18] | Dunn LK ,et al. Influence of catastrophizing, anxiety, and depression on in-hospital opioid consumption, pain, and quality of recovery after adult spine surgery. Journal of Neurosurgery: Spine. (2018) ;28: (1):119–26. |
[19] | Foster NE , Delitto A . Embedding psychosocial perspectives within clinical management of low back pain: integration of psychosocially informed management principles into physical therapist practice—challenges and opportunities. Physical Therapy. (2011) ;91: (5):790–803. |
[20] | Keefe FJ , Main CJ , George SZ . Advancing psychologically informed practice for patients with persistent musculoskeletal pain: promise, pitfalls, and solutions. Physical Therapy. (2018) ;98: (5):398–407. |
[21] | O’Sullivan S ,et al. National Physical Therapy Examination Review & Study Guide 2019. 2019, Evanston. IL: Therapy Ed Ltd. |
[22] | Haggman S , Maher CG , Refshauge KM . Screening for symptoms of depression by physical therapists managing low back pain. Physical Therapy. (2004) ;84: (12):1157–66. |
[23] | Verna JL ,et al. Validity of the Multidimensional Task Ability Profile. Journal of Occupational Rehabilitation. (2019) ;29: :822–31. |
[24] | Kemp B , Adams B . The Older Adult Health and Mood Questionnaire: a measure of geriatric depressive disorder. Journal of Geriatric Psychiatry and Neurology. (1995) ;8: (3):162–7. |
[25] | Matheson L . Multidimensional Task Ability Profile Professional Manual. 2011, St. Charles, MO: EpicRehab, LLC. |
[26] | Moses MJ ,et al. Comparison of patient reported outcome measurement information system with neck disability index and visual analog scale in patients with neck pain. Spine. (2019) ;44: (3):E162–7. |
[27] | Beck A , Steer R , Brown G . Beck Depression Inventory II. (1995) , San Antonio: PsychCorp. |
[28] | Zung-William W . Depression Status Inventory. Journal of Clinical Psychology. (1972) ;28: (4):539–43. |
[29] | Yesavage JA ,et al. Development and validation of a geriatric depression screening scale: a preliminary report. Journal of Psychiatric Research. (1982) ;17: (1):37–49. |
[30] | Hamilton M . The Hamilton rating scale for depression, in Assessment of Depression. (1986) , Springer. p. 143–52. |
[31] | Lewinsohn PM ,et al. Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychology and Aging. (1997) ;12: (2):277. |
[32] | Andrich D . Rasch Models of Measurement. Quantitative Applications in the Social Sciences. (1988) , Newbury Park: Sage. |
[33] | Vlasveld M ,et al. Predicting return to work in workers with all-cause sickness absence greater than 4 weeks: a prospective cohort study. Journal of Occupational Rehabilitation. (2012) ;22: (1):118–26. |
[34] | Lagerveld S ,et al. Factors associated with work participation and work functioning in depressed workers: a systematic review. Journal of Occupational Rehabilitation. (2010) ;20: (3):275–92. |
[35] | Henry JD , Crawford JR . The short-form version of the Depression Anxiety Stress Scales (DASS-21): Construct validity and normative data in a large non-clinical sample. British Journal of Clinical Psychology. (2005) ;44: (2):227–39. |
[36] | Robinson R ,et al. Improvement in postoperative and nonoperative spinal patients on a self-report measure of disability: the Spinal Function Sort (SFS). Journal of Occupational Rehabilitation. (2003) ;13: (2):107–13. |




