Factors influencing ergonomists’ use of observation-based risk-assessment tools
Abstract
BACKGROUND:
Several observation-based risk-assessment tools have been developed in recent decades. Studies reporting their use often focus only on the user, the ergonomist. The influence of context and the attributes of the tools may also affect the use but are factors that are seldom considered.
OBJECTIVE:
The aim of the present study was to explore the process of risk-assessment assignments and to identify factors influencing the use of research-based observation-based risk-assessment tools among Swedish ergonomists, with a background as reg. physiotherapists, employed in Occupational Health Services (OHS).
METHODS:
A web-based questionnaire (n = 70) was combined with semi-structured interviews (n = 12).
RESULTS:
There was limited use of several observation-based risk-assessment tools. Furthermore, the results showed that ergonomics risk-assessment assignments are most commonly initiated reactively and that interventions were seldom evaluated. Factors that influence use are related both to the ergonomist and to the attributes of the tools as well as to contextual factors assigned to authorities, and internal organisations both within occupational health service companies and client companies.
CONCLUSION:
There was a lack of systematic approaches in ergonomics risks assessment and low use and knowledge of risk-assessment tools. This indicates that there is a need to support OHS companies in implementing systematic tools in their practice.
1Introduction
The last few decades of ergonomics research concerning physical exposures and work-related musculoskeletal disorders (WRMSDs) has resulted in the development of a large number of different risk-assessment tools, e.g. self-administered questionnaires, interview protocols, observation-based risk-assessment tools (OBRATs) and direct (technical) measurement tools [1, 2]. The rationale behind this research and development is to increase the precision of risk assessments to be able to more effectively apply risk reducing measures with regards to WRMSDs.
When assessing physical exposures, OBRATs are often considered a feasible choice for practitioners, since they are relatively time-efficient, flexible and usually less costly than direct measurements [2, 3] and more reliable than self reports. Use of systematic risk-assessment tools, e.g. OBRATs, can be helpful in selecting what exposures to target in the work environment but can also be supportive in evaluating effects of ergonomic interventions. Although there are large similarities among some OBRATs, the coverage of different dimensions of physical exposures varies to some extent; therefore, a combination of several OBRATs may be necessary to make a comprehensive risk assessment of a work place [1]. Moreover, the design and structure vary across OBRATs, and usability aspects, such as applicability in various work settings, time consumption and the complexity of the tool also seem to influence usage [4].
In Sweden, ergonomists (usually with a professional background as reg. physiotherapists) within the occupational health services (OHS) [5] conduct risk assessments of physical exposures; however, the frequency and scope of such assignments vary among ergonomists. A study by Laring et al. [6] indicates that the organization of the OHS company where the ergonomist is employed, for example in-house OHS (incorporated in the client company/industry, municipality or county council) or external OHS (consultant with several client companies), influences the professional role of the ergonomist. This in turn may effect what assignments OHS ergonomists become involved in, reactive assignments (e.g. secondary or tertiary interventions such as individual rehabilitation measures), or proactive assignments (e.g. systematic risk-assessment). Little is known about the underlying reasons regarding when ergonomic assingments are initiated, and knowledge is scarce concerning to what extent OBRATs with a research base are being used within the OHS. Studies indicate that in practice ergonomists frequently rely mainly on their own empirical experience and often use less structured interviews and direct observation [6–8], a practice that has been associated with poor reliability [9]. Further, a recent Swedish study revealed that organizational support for using research-based methods is often lacking within the OHS [10].
In summary, although risk assessment of physical factors is of importance for identifying potentially harmful work tasks and for prioritizing and designing work place interventions, knowledge is lacking, concerning both what tools are being used and how these assignments are conducted.
The aim of this study was therefore, to explore the process of risk-assessment assignments and to identify factors influencing the use of research-based observation-based risk-assessment tools among Swedish OHS ergonomists.
2Methods
2.1Study design
This cross-sectional study has a mixed-method design. Data was collected using both a questionnaire and interviews. The questionnaire was used to investigate the use of OBRATs in a broader perspective and the interviews were used to provide a deeper understanding concerning the process of risk assessment assignments. The analysis and the interpretation of the mixed data was also inspired by Logan's and Graham's [11, 12] framework, the Ottawa Modell of Research Use (OMRU). The rationale to use this framework was that it can be used to study the use of research-based knowledge in practice and assist to identify factors of importance to understand the knowledge translation [11–13].
2.2Questionnaire
A web-based questionnaire was used to quantify the use of research-based OBRATs. The questionnaire targeted Swedish OHS-employed ergonomists (RPTs), members of the Ergonomics Section of the Swedish Association of Physiotherapists. Information about the survey was sent out by the Ergonomics Section of the Swedish Association of Physiotherapists in a periodical e-newsletter addressed to all of their 598 members. Only members that opened the newsletter received information about the survey. Two reminders were sent. Of the 251 ergonomists who opened the newsletter, 107 (43%) completed the questionnaire. After applying the inclusion criteria (conduction of risk assessments >1 year), the study group consisted of 70 (28%) ergonomists. They provided service to various client companies in the private and the public sectors.
The questionnaire included questions about the ergonomists’ backgrounds (Table 1) and their use of OBRATs as well as attributes they considered important in them. Seventeen OBRATs were included based on the criteria that the tool should be available in Swedish or English and publicly available in Sweden. The OBRATs included originated primarily from Takala et al. [1] and were supplemented with five tools suggested by the research group and a reference group of ergonomists (Appendix 1). For each OBRAT, the ergonomists were asked if they had used the tool or not, or if they were unfamiliar with the tool. Depending on their answer, a set of subsequent dichotomous (yes/no) questions followed (Table 4). The ergonomists were asked how they had gained knowledge of these tools (e.g. through colleagues, education, professional sector-specific networks or via internet searches). They were also given the opportunity to provide free-text answers concerning the reasons for use and names of other OBRATs that they had used. Another 15 questions concerned important attributes of OBRATs in general (Fig. 1) using a five-point ordinal scale ranging from 1 (Not important at all) to 5 (Very important).
Fig.1
Rating of important attributes of OBRATs in general. Results from the web-based survey. The respective proportions of respondents that gave a rating from 1 (Not important at all) to 5 (Very important) are indicated (see key).
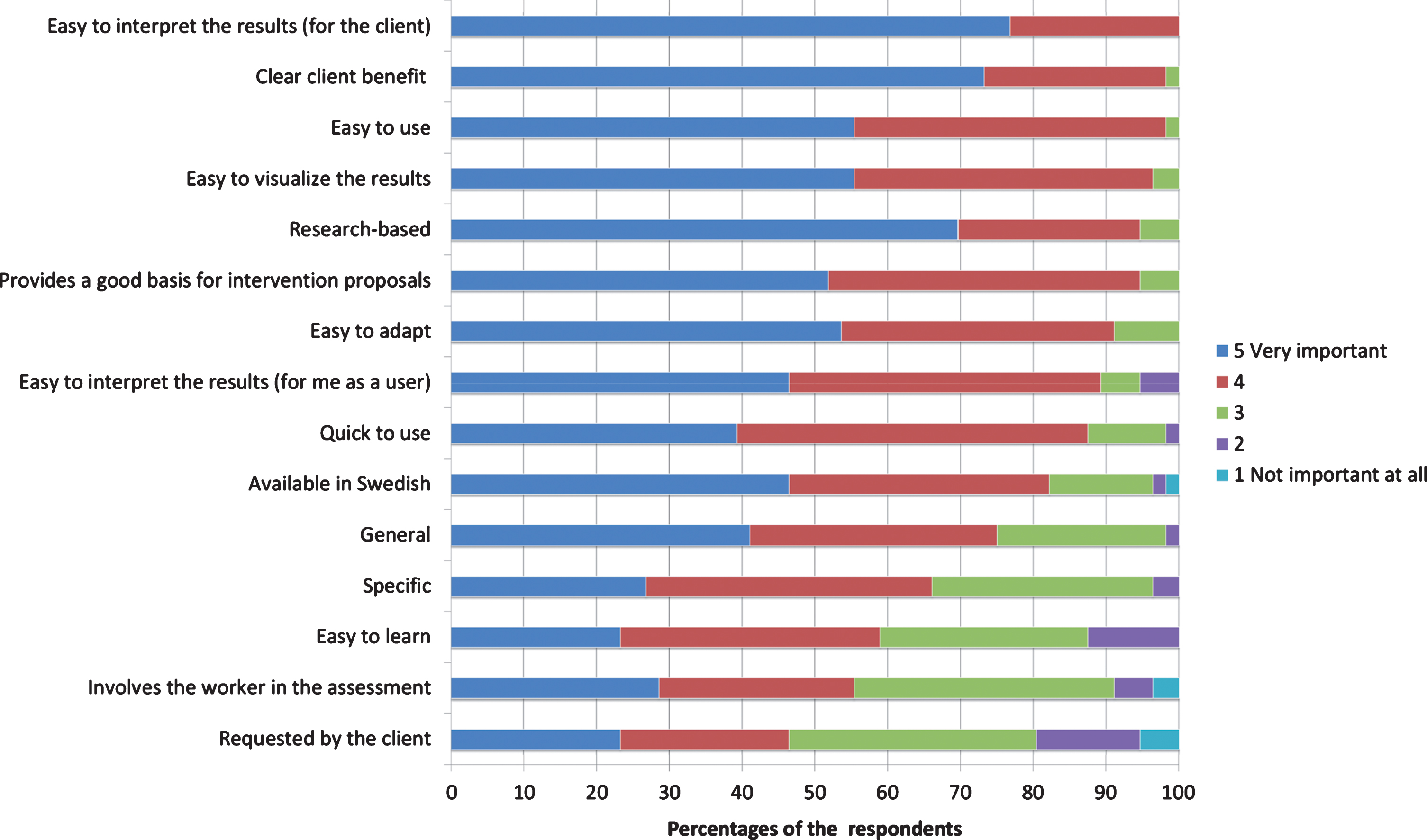
Table 1
Basic characteristics of the respondents in the web-based survey and the interviews
| Web-based survey | Interview | |
| N | 70 | 12 |
| Age, mean (min– max) | 50 (26–67) | 50 (36–65) |
| Women, n (%) | 57 (81) | 9 (75) |
| Men, n (%) | 13 (19) | 3 (25) |
| Years of work experience in ergonomics, mean (min– max) | 14 (2–38) | 15 (4–25) |
| Additional education in ergonomics* (n, %) | 55 (79) | 12 (100) |
*All ergonomist were RPT (Registered physiotherapists) with university level education.
2.2.1Questionnaire analysis
Data from the questionnaire were analysed by using SPSS statistics, version 25. The rating of important attributes of OBRATs in general are presented as descriptive statistics. To investigate potential differences in the frequency of performing risk assessments, fisher’s exact test was used. To explore differences in the use of the 17 different OBRATs, data was analysed using Mann-Whitneys U-test. The analyses were considered statistically significant when p < 0.05.
2.3Interviews
For the interviews, twelve OHS ergonomists (all RPTs) were recruited (Table 1) and gave their informed consent. Inclusion criteria were: ongoing employment as an OHS ergonomist and experience of risk assessments. Five of the ergonomists were recruited from a parallel research project [14, 15]. Contacts were taken with other OHS companies by the first author and an additional seven ergonomists were recruited to the study.
Three of the ergonomists were employed as ‘in-house ergonomists’ within a global industrial manufacturing company but worked at different production plants. Nine of the ergonomists were employed in external OHS companies situated in seven different regions in the southern and central parts of Sweden. The external OHS companies provided services to a wide variety of client companies in different work sectors, which meant that the number of clients differed across the external ergonomists. Six ergonomists described that they visited at least one client company regularly (>1/month) and can therefore be described as ‘partially in-house’. Unlike the in-house ergonomists, all external ergonomists had dual work roles, that is, they treated patients in addition to conducting work environment-related assignments.
Semi-structured interviews lasting 45 to 60 minutes were conducted. Nine of the interviews were conducted by the first author and three interviews were conducted by the second author. The interview guide used was developed through workshops within the research group and had been piloted on two ergonomists (RPTs), which resulted in slight modifications. The ergonomists were each asked to describe a risk-assessment assignment they had been involved in, how the assignment was initiated, what methods were used and how feedback and evaluations were given.
2.3.1Interview analysis
Qualitative directed content analysis was applied [16]. To understand the ergonomists’ current practice regarding risk assessment, the analysis was based on three predetermined main categories; the process of an ergonomic risk-assessment assignment: the initiation of assignments, the assessment of physical exposures, and feedback and evaluation of assignments. Meaning units were identified in the transcribed interviews. These were clustered into sub-categories and finally connected to the three main categories [17]. The analysis was performed by the first author and communicatively validated [17] through presentation of results in workshops with a reference group of ergonomists.
3Results
The results present the process of risk-assessment assignments and explore the questions about how assignments are initiated, how Swedish OHS ergonomists assess physical exposures, and how feedback and evaluation of assignments is provided.
3.1Initiation of assignments
Table 2 gives an overview of the ergonomist risk-assessment process with examples from the interviews analysis.
Table 2
Results from interviews n = 12. Main-categories, sub-categories and examples
| Main categories | Sub-categories | Examples from interviews |
| Initiation of assignments | Reactive | Reported WMSD |
| Rehabilitation | ||
| Injunctions of authority | ||
| Proactive | Periodical screening | |
| Periodical risk assessment | ||
| Assessment of physical exposures | No specific method | Direct observations |
| Interviews | ||
| Photo | ||
| Expertise | ||
| OBRATs | SWEA-AFS | |
| KIM | ||
| VIDAR | ||
| NIOSH-LE | ||
| Own-developed tools | ||
| Direct measurement tools | Dynamometer | |
| Feedback and evaluation of assignments | Feedback | Written reports |
| Evaluation | Effects of assignments seldom evaluated | |
| In-house/partially in-house greater opportunity to follow up assignments |
The ergonomists reported that assignments often were initiated reactively after occurrence of WMSDs (Table 2). Initiative was taken either by the client company, which contacted the ergonomist because one or more employees had reported WMSDs, or from the ergonomist, who contacted the client company when one or more employees in the client company underwent clinical treatment. Both ways to initiate the assignment resulted in the ergonomist visiting the client company, observing the employee/s at work and assessing physical exposures.
She came to me for physiotherapy treatment and later I visited her workplace and I performed an ergonomics risk assessment ... It emerged that job rotation would be beneficial for all parties, not just for her ... (Ergonomist 4, external).
Another example of a reactive initiation of assignments was when an injunction had been issued by SWEA towards the employer due to lack of fulfilment of the employer’s legal health and safety obligations. It was described that the awareness among client-company managers with regards to responsibilities concerning OHSM was sometimes limited:
I would say that inspections by the inspectors from SWEA are our best initiators for assignments, because when they have inspected a workplace and issued an injunction, then they [the managers] understand [their responsibility]. (Ergonomist 2, external).
It emerged that proactive initiatives for ergonomic assignments were related to the maturity of the client companies’ OHSM. In some cases, it was clear that ergonomic assignments were important because they were integrated in the company's OHSM. A precondition seemed to be the relation between the OHS ergonomist and the client, for example the opportunity to be on site within client companies, to know the company. Mainly two types of proactive assignments were described. Periodical screenings at the client company, where the ergonomist visited different departments at the workplace and interviewed employees in a general screening designed to identify potential adverse physical exposures. Another proactive initiative was when the ergonomist was responsible for the periodical risk assessment of physical exposures within a client company.
The client company manages the overall risk assessment; my part [risk assessment of physical exposures] is included in the overall risk assessment [of the work environment]. (Ergonomist 5, external).
Another, but less frequently mentioned example of a proactive initiation was when the client company contacted the ergonomist during the planning or design of new work tasks or workplaces:
A new work task was to be added, which involved scanning of goods. Then they [client] wanted to know if that could lead to physical risks, and, if so, they wanted an impact analysis and proposals for preventive measures. As an ergonomist, I thought it was fantastic to get involved before the work task was introduced (Ergonomist 9, external).
3.2Assessment of physical exposures and use of observation-based risk-assessment tools
A majority of the respondents in the questionnaire (70%), conducted risk assessments at least once a month (Table 3). The interviews revealed that the practice of identifying and assessing physical exposures were mainly based on the ergonomist’s own experience and expertise. A screening through direct observations without any specific method or tool, interviewing employees and taking still images or video footage of work tasks was often the practice to assess risk.
Table 3
Education level, frequency of performing risk assessments and the use of OBRATs
| Additional education in ergonomics | ||
| Yes | No | |
| Frequency of conducting risk assessments, n (%) | ||
| At least once a year | 1 (2) | 0 (0) |
| At least once every 6 months | 4 (7) | 2 (13) |
| At least once every 3 months | 12 (22) | 2 (13) |
| At least once a month | 22 (40) | 5 (33) |
| At least once a week | 16 (29) | 6 (40) |
| Number of different OBRATs used, median (min– max) | 4 (1–11) | 2 (1–5) |
... often when you visit a workplace you base your observation on your knowledge as an ergonomist ... That [work operation] does not look good because they work too far away from the body, too high, for too long a time or too repetitively and so on. And for that assessment I do not use any specific methods ... I actually don’t. (Ergonomist 1, external)
The survey explored the ergonomists’ knowledge about different OBRATs (Table 4). The results show the most commonly used OBRAT was the “Physical Ergonomics: Provisions of the Swedish Work Environment Authority” (SWEA-AFS) [18, 19], which was used by all ergonomists. Other commonly used OBRATs were, in descending order, “Key Item Method – Pulling, Pushing” (KIM I) [20] (51%), “Key Item Method – Lifting, Holding, Carrying” (KIM II) [20] (36%), “Quick Exposure Check” (QEC) [21] (27%) and “VIDAR” (an acronym for the Swedish expression Video och Datorbaserad ARbetsanalys (Video- and computer-based work analysis) [22] (27%) (Table 4). A majority of the ergonomists reported that important attributes that affected the use of SWEA-AFS [18, 19], KIM I [20], KIM II [20] and QEC [21] were that the tools were both easy to use and easy to communicate to the client company. About half of the ergonomists (40–53%) also reported that they were quick to use. However, the attributes of OBRATs with the highest proportion of ergonomists’ rating those attributes as very important were 1) easy to interpret for the client (77%), 2) have a clear client benefit (73%), and 3) be research-based (70%) (Fig. 1). Other important attributes were that the tool should: 4) be easy to use, 5) produce results that are easy to visualize, 6) be easy to adapt to different lines of businesses/work tasks, 7) provide a good basis for intervention proposals, and 8) produce results that are easy for the user to interpret. All but one attribute, ‘the tool being requested by the client’, were given a score of ≥4 by a majority of the ergonomists.
Table 4
The five most frequently (>25%) used observational risk-assessment tools (OBRATs) among Swedish ergonomists. Results based on the survey questions: ‘Have you used the observational tool in question?’ and ‘Why do you use the method?’ respectively. Number of respondents and percentages (%)
| SWEA-AFS | KIM I | KIM II | QEC | VIDAR | |
| Have you used this tool? | |||||
| Yes | 70 (100) | 36 (51) | 25 (36) | 19 (27) | 19 (27) |
| No | 0 (0) | 16 (23) | 28 (40) | 23 (33) | 44 (63) |
| Not familiar with the tool | 0 (0) | 18 (26) | 17 (24) | 28 (40) | 7 (10) |
| If yes, why do you use this tool? | |||||
| Easy to use | 53 (76) | 26 (72) | 15 (60) | 10 (53) | 4 (21) |
| Easy to communicate to the client | 45 (64) | 21 (58) | 16 (64) | 10 (53) | 7 (37) |
| Quick | 35 (50) | 15 (42) | 10 (40) | 10 (53) | 0 (0) |
| Most suitable for my assignments | 15 (21) | 12 (33) | 11 (44) | 5 (26) | 8 (42) |
| Easy to interpret the results | 18 (26) | 16 (44) | 11 (44) | 9 (47) | 6 (32) |
| No technical equipment is required | 36 (51) | 10 (28) | 6 (24) | 6 (32) | 0 (0) |
| Easy to adapt | 31 (44) | 11 (31) | 8 (32) | 6 (32) | 4 (21) |
| The method that I know best | 44 (63) | 6 (17) | 5 (20) | 4 (21) | 3 (16) |
SWEA-AFS: Physical Ergonomics: Provisions of the Swedish Work Environment Authority [14, 15], KIM I: (Key Item Method – Pulling, Pushing [16]. KIM II: Key Item Method – Lifting, Holding, Carrying [16]. QEC: Quick Exposure Check [17]. VIDAR: Video- och databaserad arbetsanalys [a video- and computer-based method for ergonomic assessment] [18].
Education was the most frequently reported way of having gained knowledge of a tool (64%). Seventy-nine percent of the respondents in the questionnaire reported having additional education within ergonomics. The nature of the education reported varied from shorter courses (8 weeks) with specific focus at risk assessment and risk assessment methods, to university level master programs (1–2 years) in ergonomics. The number of OBRATs used was significantly higher among ergonomists with additional ergonomics education (Mann-WhitneyU-test, p = 0.004) (Table 3). Other ways of gaining knowledge of tools were through colleagues (20%), through internet searches (9%), and through sector networks (6%). There was no correlation between the ergonomists work experience and the number and the number of different OBRATs used. (Mann-Whitney U-test, p = 0.805)
The use of internationally well-known OBRATs was distributed as follow: NIOSH-Lifting Equation [23] (23%), RULA [24] (23%), REBA [25] (17%), the Strain Index [26] (11%), ACGIH-HAL [27] (4%), OWAS [28] (4%) and OCRA [29] (3%). Lack of knowledge/skill (including familiarity) was reported as the main reason for not using a tool. Other reasons were attributes related to the tool, such as being too complicated, too time-consuming or unnecessary. A further reason not to use OBRATs more extensively was expressed by one interviewee, who argued that the use of OBRATs led to less flexibility:
I feel the need for flexibility, to be able to discuss with the client ... If I use specific tools, I tend to lose some of the dynamics in work [assessments] because the tools are not adaptable enough. (Ergonomist 1, external)
Subsequently, the results from the questionnaire regarding the use of OBRATs were confirmed by the interviewees. The ergonomists had knowledge of a number of different OBRATs but mainly used the SWEA-AFS [18, 19] (Table 4). However, the three in-house ergonomists worked, in contrast to the external ergonomists, solely with work environment-related assignments, and not as clinical physiotherapists treating patients. They used several risk-assessment tools, combining different OBRATs, direct measurements, interviews and footage/photos. The in-house ergonomists’ organization supported the use of a set of tools/OBRATs via a company policy.
I primarily use the company's custom-developed risk-assessment tool, but in the logistics [department] we use other tools; KIM, a tool for small lot delivery system [Small Lot Delivery], and the Ergonomics Thermometer. These are all standardized ergonomics tools that we use ... . (Ergonomist 11, in-house)
3.3Feedback and evaluation
Risk assessments were often summarised in a report and sent to the client company. In this process, OBRATs were sometimes used as references by the ergonomists when communicating physical exposures and risk factors for WMSDs to representatives within the client company.
... so I use it [SWEA-AFS] and I write a report based on it. (Ergonomist 6, in-house)
Potential effects of risk reducing measures were most often not evaluated. The external ergonomists reported that a barrier to re-visiting and evaluating completed assignments was an economic factor, the inability to bill the client company for this service. Ergonomists working in-house or partially in-house expressed greater opportunities to follow-up and evaluate risk reducing measures. However, some of these assignments were described as more informal ‘follow-up checks’ and not systematic evaluations including before-and-after measurements.
Since I visit [the client] regularly, follow-up checks can occur at any time... Sometimes, you do not even think about booking a specific time for follow-ups, it just happens naturally. (Ergonomist 7, external)
Systematic evaluation was reported only by in-house ergonomists. They evaluated any possible changes in exposure after interventions by using the same tools that were used for the initial assessments.
Have we removed the red areas? And if we used KIM, we use KIM again and we can analyse current risk factors. (Ergonomist 10, in-house)
4Discussion
The results display that ergonomics risk-assessment assignments were most commonly initiated reactively, after the identification of WMSDs. The use of systematic risk-assessment tools, such as the observation-based NIOSH lifting equation [23], RULA [24] and OWAS [28], was low among Swedish OHS ergonomists. Evaluation is important to ensure the quality in services provided by the OHS, and the finding that assignments were seldom evaluated is suggested to be associated with the low usage of systematic tools.
Furthermore, except for the in-house ergonomists, organisational support for working in a systematic way and for using research-based tools was lacking. Overall, the results indicate deficiencies within the OHS companies in ensuring that research-based tools are implemented and used, findings that are in concordance with Bramberg et al. [10]. They investigated the attitudes and knowledge regarding evidence-based practice among Swedish OHS practitioners and managers, and concluded that the OHS organisations did not use evidence-based practice as an organizational strategy [10]. Hence, there is a need to support the OHS in implementing research-based tools as a part of organisational quality improvements.
The overall results of the present study suggest a gap in knowledge translation [30] (OBRATs are insufficiently implemented within the OHS ergonomists’ practice). To identify areas of importance for an implementation intervention to increase the use of OBRATs among OHS ergonomists the results from the current study was analyzed using the OMRU [11, 12]. The OMRU framework provides direction for planning and guiding of activities supporting knowledge translation [11–13]. The first part of OMRU involves the assessment of barriers and support in three different areas: the innovation, the potential adopters (users) and the practice environment (Fig. 2). By adapting the OMRU model to fit the context of the present study, the results can be fitted into the three fundamental areas of the OMRU, hence facilitating the identification of factors that influence the use of OBRATs.
Fig.2
An adapted version of “The Ottawa Model of Research Use” (OMRU). The figure shows the results in the present study fitted into the three fundamental elements (dashed frame); the innovation (OBRATs), potential adopters (OHS ergonomists) and practice environment (context of OHS ergonomists).
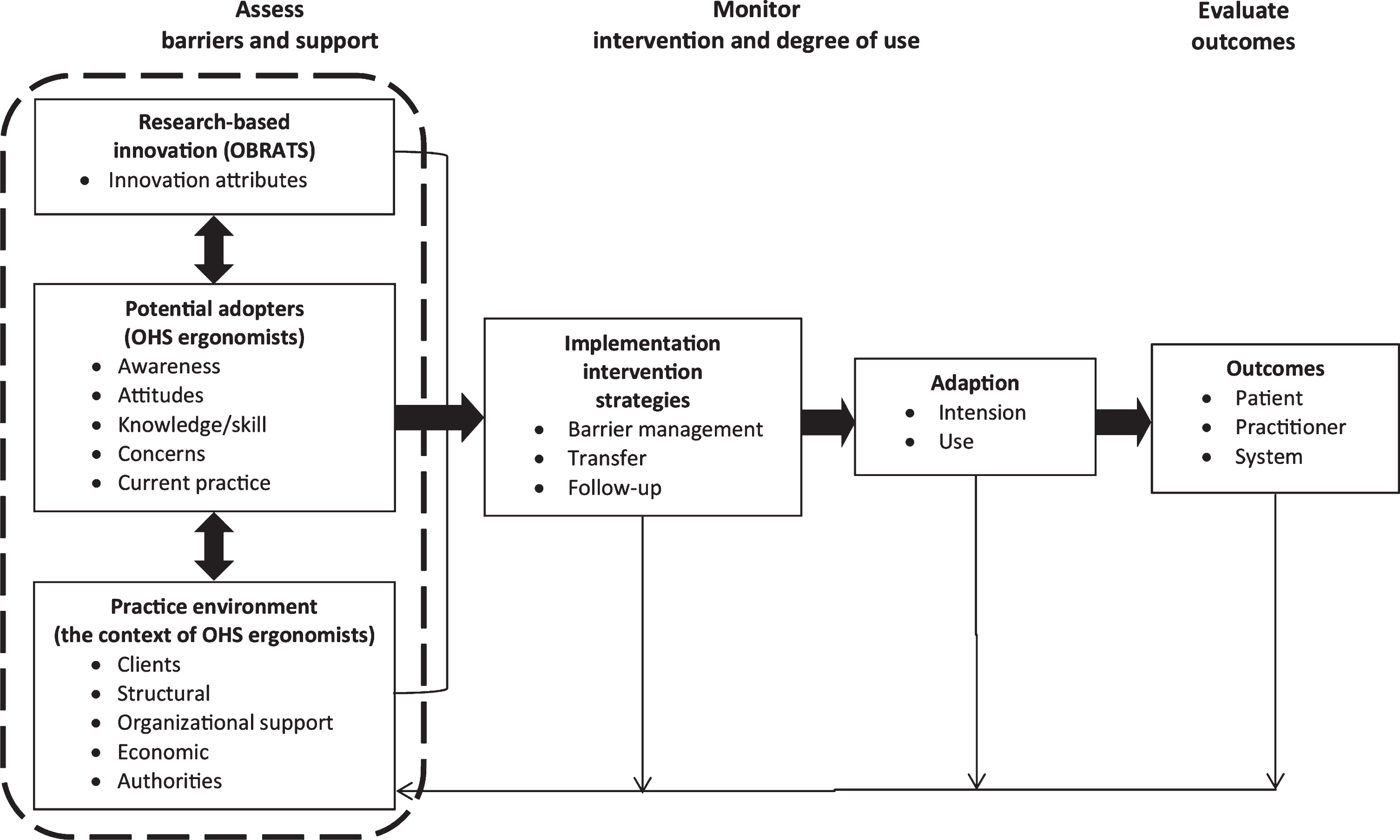
4.1Research-based innovation; The observation-based risk-assessment tools
In the OMRU framework, the innovation can be represented by various knowledge tools [12], which in this study is represented by the OBRATs. Table 5 presents ergonomists’ perception of what attributes in OBRATs motivate use. In accordance with Diego-Mas, Poveda-Bautista, and Garzon-Leal [4], the results indicate that OBRATs should facilitate decision making regarding risk reducing measures (here: provide an appropriate basis for intervention proposals) and be applicable to different types of jobs. However, issues related to training (e.g. ease of learning or requirements of training) seem to be of less importance. In contrast to the findings of Diego-Mas, Poveda-Bautista, and Garzon-Leal [4], an OBRAT’s being quick to use was identified as a factor of importance in the present study. This finding is concordant with Buckle and Li [31] and Rose et al. [32] and was proportionally high among those OBRATs that had proportionally high usage (Table 4). However, being quick to use seems, in agreement with Rose et al. [32], to be less important than being easy to use. The proportionally high rating of the tool’s being research-based might be unexpected, since the scientific basis of the three tools with the highest proportion of use (SWEA-AFS [18, 19] KIM I [20] and KIM II [20]) is somewhat unclear, and studies evaluating their ability to predict increased risk of WMSDs are lacking [33, 34]. However, the fact that these tools are promoted by a governmental body (i.e. SWEA) may give the impression that they are scientifically valid and reliable.
Table 5
Preferred attributes of OBRATs among different users and from different studies
| Practitioners’ needs, Mas-Diego et al. [4] | Practitioners’ needs, Buckle and Li, [30] | Experts’ needs, Buckle and Li, [30] | Ergonomists’ needs, The present study |
| Facilitates decision regarding measures Properly addresses the relevant risks of the job Is applicable to different types of jobs | Quick to apply Easy to learn Clear User friendly Required limited paperwork Does not require collection of unnecessary data Has check boxes Specific | Seen as standard tool, backed by regulatory bodies Valid Reliable High face validity Equal balance across risk factors Comprehensive Can generalize results across plants, etc. | Easy to interpret results (client) Clear client benefit Easy to use Easy to visualize results Scientifically based Provides good basis for intervention proposals Easy to adapt Easy to interpret results (the assessor) Quick to use Available in Swedish General Specific Easy to learn Involves the worker in the assessment |
4.2Potential adopters: The OHS ergonomists
Potential adopters are those who may use the innovation [12]. In this study potential adopters are represented by the OHS ergonomists. The results show that education or training was an important factor that prompted the ergonomists to use different OBRATs, which is in agreement with findings from Arezes, Miguel, and Colim [35]. In the present study, there was a spread in education level among the respondents, ranging from shorter eight-week courses focused only on risk assessment to full university level master programs in ergonomics. The results showed that the number of different OBRATs used by ergonomists was significantly higher among those with an additional education in ergonomics (Table 3). However, the frequency of risk assessment assignments was similar among the groups (Table 3) which indicates the value of additional education. Even if the ergonomists knew of the existence of a number of different OBRATs, they stated that they lacked the skills to use many of them. This may contribute to less informative and less accurate risk assessments since different OBRATs focus on different dimensions of physical exposures, and a combination of several tools may be necessary for more comprehensive risk assessments [1]. For the eight tools with the lowest proportion of users, about half of the ergonomists stated that they were not familiar with these tools. This group included the OWAS [28], OCRA [29] and the Strain Index [26]. Interestingly, these tools were among the most commonly used OBRATs among Spanish-speaking ergonomics practitioners [4], and the Strain Index was used by about 40% of ergonomists in the U.S. [36].
It is possible that the dual work role which is common for Swedish OHS externally employed ergonomists, that is, acting as both a clinical physiotherapist treating patients and as an ergonomist conducting work environment-related assignments, may hinder the ergonomists’ ability to specialize and develop in-depth knowledge and skills concerning risk-assessment procedures and different OBRATs.
4.3Practice environment; the context of the OHS ergonomists
In the OMRU framework, the practice environment is comprised by structural factors: e.g. policies, decision-making structure, rules, workload and current practice [12]. Identified factors related to the OHS ergonomists’ context include structural factors at several levels, all of which affect the use of OBRATs:
1) At a policy level, factors such as availability and promotion from regulatory bodies seemed to highly influence the use of different OBRATs. This is reflected in both results from the interviews and the questionarie. For example, the use of the NIOSH-LE [23] (23%), RULA [24] (23%), and the Strain Index [26] (11%) was lower in the present study compared to other surveys among certified ergonomists in the U.S. [36] and Canada [37] and among Spanish-speaking ergonomics practitioners [4]. These four OBRATs are contrary to SWEA-AFS [18, 19], KIM I [20] and KIM II [20] (Table 4) not promoted by a regulatory body in Sweden which likely affect their use.
The extensive use of SWEA-AFS [18, 19] confirms the results from earlier surveys in Sweden [38]. SWEA-AFS, KIM I and KIM II were all available from the SWEA website, and promotion from a regulatory body (in this case SWEA) is a likely contributor to high usage [31]. The interviews revealed that the SWEA-AFS [19], which is a provision issued by a regulatory body (SWEA) and is based on the Swedish Work Environment Act, could be used as an incentive for risk reducing measures, which indicates that support from regulatory bodies is a determinant for the use of OBRATs. However, both SWEA-AFS [18, 19] and VIDAR [22] (which is based on SWEA-AFS), are not systematic risk-assessment tools with quantifiable indexing; they can be considered screening tools instead.
2) At an organizational level, factors within both OHS companies and the client companies also seem to affect the use of OBRATs. Factors that can be assigned to the organizations of OHS companies are organizational support and routines for working with standardized tools. Structural factors at client companies involve the development of their internal OHSM. Interviewees described that the awareness among managers (at client companies) concerning responsibilities for OHSM varied considerably, and previous research support that small and medium-sized companies (especially) have difficulty fulfilling the requirements for their OHSM [39]. Schmidt et al. [40] describe that a well-developed OHSM at the client company is a key factor in using the OHS company effectively, promoting specialization and a more systematic approach [6], including the use of OBRATs.
Contextual factors that can be assigned both to the OHS companies and their clients are related to their relationship. A close relationship (e.g. in-house, partially in-house, opportunity to client company/sector specialization) and closeness to the client, with regular visits and long-term collaboration, seem to influence whether OHS services are used proactively or reactively. The interviews indicate a predominance of reactive assignments, which may explain the low use of OBRATs, as risk assessment can be regarded as predominantly a proactive action.
The relationship may be impacted by the contracts between OHS and clients. In Sweden, contracts between a company and an OHS provider are seldom preceded by a needs assessment and are often short term in character (1–3 years), which narrows the possibilities of establishing long-lasting relationships and results in external OHS companies’ often becoming passive recipients of assignments instead of working proactively together with the client company [41]. These preconditions may contribute to client companies’ mainly contacting the contracted OHS company after identification of WMSD problems (e.g. for rehabilitation), which also is described by Whysall, Haslam, and Haslam [7], and may hamper the use of the OHS company for preventive/proactive assignments. A contributing factor to this approach may be that client companies are unfamiliar with the ergonomist’s competence concerning proactive work [42], which is reported among engineers and design professionals [43]. However, there is not always a clear distinction between proactive and reactive, and the interview results indicate that it is possible for ergonomists to make use of a reactive assignment to initiate proactive work which involves risk assessment resulting in risk reducing measures targeting entire work groups.
4.4Methodological considerations
Concerning the sample, the gender distribution of the questionnaire respondents (81% women) and the interviewees (75% women) is close to that of Swedish ergonomists in general (79% women), members of the Ergonomics Section within the Swedish Association of Physiotherapists, as was communicated in an e-mail to the authors.
The response rate of the questionnaire was 28%, and caution should be observed when generalizing these results to all Swedish OHS ergonomists. It is possible that the ergonomists that responded to the questionnaire have a special interest in risk assessments compared to those that did not. If so, the use of OBRATs may be even lower than reported in this study. However, 70% of the responders conducted risk assessment >1 month, we consider their answers regarding the use of OBRATs are representative among Swedish OHS ergonomists. Questions about seventeen OBRATs were included in the questionnaire. It seems to have covered the most commonly used OBRATs in this population, because only two additional OBRATs were reported, the Ergonomics Thermometer [44] and ‘SARA’ [45], both used by fewer than 3% of the ergonomists. Education or training was an important factor that stimulated the use of OBRATs. The questionnaire provided some opportunity for the respondents to elucidate what kind of additional education within ergonomics they had participated in, however more specific information concerning the content of the education is lacking. Hence, how to successfully design courses that facilitates the implementation of OBRATs needs to be further explored in future research.
Only twelve interviewees were included in this study. However, they represented both in-house and external OHS ergonomists with clients in several different sectors. The differences in their experience, (range from 4 to 25 years (mean 15 years) and the different organizational context covered different perspectives and experiences. Thus, we consider that the findings strengthen the ability to draw conclusions about the Swedish OHS ergonomists practice regarding risk assessment.
5Conclusions
By exploring the use of observational risk-assessment tools and the process surrounding risk-assessment assignments among Swedish OHS ergonomists, we found a lack of a systematic approach. Research-based risk-assessments tools were not used to a great extent. A conclusion that can be drawn is that there is a need for implementations strategies within the OHS community to increase the use of systematic risk-assessment methods. In Sweden, the OHS represents the most commonly contracted work-environment expertise, and hence the results in the present study can add value also for other professional groups in the OHS, as well as for the OHS community as a whole.
By applying an implementation framework, several factors were identified that can be targeted in an implementation intervention, for example, easily accessible educational interventions, increased availability of OBRATs via e.g. links from webpages belonging to work environmental authorities.
Conflict of interest
None to report.
Funding
This study was supported by AFA Insurance (Grant 090168) and the Swedish Research Council for Health, Working Life and Welfare (Grant 2010-1563).
Appendices
Appendix 1.
The table below presents the 17 observation-based risk-assessment tools included in the web-based survey. The selections of tools were mainly based on Takala et al. [1]. After suggestions from the research group and ergonomists, a further five tools were added to the list. The tools added were: the provisions on physical ergonomics from Swedish Work Environment Authority (SWEA-AFS), ALBA, WEST, KIM I and KIM II.
| Observation-based risk-assessment tool | Reference |
| Physical Ergonomics: Provisions of the Swedish Work Environment Authority. (SWEA-AFS) | Swedish Work Environment Authority (SWEA). Provision 1998 : 01. Belastningsergonomi.(Physical Ergonomics). Stockholm, Swedish Work Environment Authority; 1998. Swedish. Swedish Work Environment Authority (SWEA). Provision 2012 : 2. Belastningsergonomi.(Physical Ergonomics). Stockholm, Swedish Work Environment Authority; 1998. Swedish. |
| Key Item Method – Pulling, Pushing (KIM I) | Steinberg U, New Tools in Germany: Development and Appliance of the First two KIM (“Lifting, Holding and Carrying” and “Pulling and Pushing”) and Practical Use of These Methods. Work 2012;41 : 3990–3996. |
| Key Item Method – Lifting, Holding, Carrying (KIM II) | Steinberg U, New Tools in Germany: Development and Appliance of the First two KIM (“Lifting, Holding and Carrying” and “Pulling and Pushing”) and Practical Use of These Methods. Work 2012;41 : 3990–3996. |
| Quick Exposure Check (QEC) | David G, Woods V, Li G, Buckle P. The Development of the Quick Exposure Check (QEC) for Assessing Exposure to Risk Factors for Work-Related Musculoskeletal Disorders. Appl. Ergon. 2008;39 (1):57–69. |
| Video- och databaserad arbetsanalys (VIDAR) [a video- and computer-based method for ergonomic assessment] | Kadefors R, Forsman M. Ergonomic Evaluation of Complex Work: A Participative Approach Employing Video-Computer Interaction, Exemplified in a Study of Order Picking. Int. J. Ind. Ergon. 2000; 25 (4):435–445. |
| The NIOSH lifting equation (NIOSH– LE) | Waters T, Putz-Anderson V, Garg A, Fine L. Revised NIOSH equation for the design and evaluation of manual lifting tasks. Ergonomics. 1993;36 (7):749–776. |
| Rapid upper-limb assessment (RULA) | McAtamney L, Corlett E N. RULA: A Survey Method for the Investigation of Work-Related Upper Limb Disorders. Appl. Ergon. 1993; 24 (2):91–99. |
| ALBA program | Eklund J, Liew M, Odenrick P. ALBA; Antropometri, Lyftrekommendationer, Biomekanik och Arbetsobservation. [Anthropometry, Recommendations for manual lifting, Biomechanics and Observation of work]. Linköping; Avdelning för Industriell arbetsvetenskap. 2013. Swedish. Available from: https://www.kth.se/polopoly_fs/1.170759!/Menu/general/column-content/attachment/ALBAKompendium.pdf |
| Plan för identifiering av belastningsfaktorer (PLIBEL) [a plan for the identification of ergonomic hazards] | Kemmlert K. A Method Assigned for the Identification of Ergonomic Hazards—PLIBEL. Appl. Ergon. 1995; 26 (3):199–211. |
| Rapid entire body assessment (REBA) | Hignett S, McAtamney L. Rapid Entire Body Assessment (REBA). Appl. Ergon. 2000; 31 (2):201–205. |
| The strain Index (SI) | Moore J S, Garg A. The Strain Index: a Proposed Method to Analyze Jobs for Risk of Distal Upper Extremity Disorders. Am. Ind. Hyg. Assoc. J. 1995; 56 (5):443–58. |
| The American Conference of Governmental Industrial Hygienists threshold limit value for hand activity level (ACGIH HAL) | Armstrong T. The ACGIH TLV for Hand Activity Level. In: Marras WS and Karwowski W, editors. Fundamentals and assessment tools for occupational ergonomics. Boca Raton: Taylor &Francis Group. 2006;1–14. |
| Ovako working posture assessment system (OWAS) | Karhu O, Kansi P, Kuorinka I. Correcting Working Postures In Industry- Practical Method for Analysis. Appl. Ergon. 1977; 8 (4):199–201. |
| Occupational Repetitive Actions (OCRA) | Occhipinti E. OCRA: A Concise Index for the Assessment of Exposure to Repetitive Movements of the Upper Limbs. Ergonomics 1998; 41 (9):1290–1311. |
| Manual Handling Assessment Charts (MAC) | Monnington S C, Pinder AD, Quarrie C. Development of an Inspection Tool for Manual Handling Risk Assessment. Sheffield (United Kingdom): Health &Safety Laboratory. 2002. Available from: http://www.hse.gov.uk/research/hsl_pdf/2002/hsl02-30.pdf |
| Postural loading on the upper-body assessment (LUBA) | Kee D, Karwowski W. LUBA: An Assessment Technique for Postural Loading on the Upper Body Based on Joint Motion Discomfort and Maximum Holding Time. Appl. Ergon. 2001; 32 (4):357–366. |
| Work Environment Screening Tool (WEST) | Karling M, Brohammer G. Work Environment Screening Tool. Mölndal: Institutet för verkstadsteknisk forskning (IVF); 2002. Swedish. |
Acknowledgments
The authors wish to thank Jennie Mattes and Marcus Ternblad for their work with the collection of questionnaire data. Annika Vänje is greatly acknowledged for advice regarding qualitative analysis, and Linda Rose in the recruitment of interviewees.
References
[1] | Takala EP , Pehkonen I , Forsman M , Hansson GA , Mathiassen SE , Neumann WP , et al. Systematic evaluation of observational methods assessing biomechanical exposures at work. Scandinavian Journal of Work Environment & Health. (2010) ;36: (1):3–24. |
[2] | David G . Ergonomic methods for assessing exposure to risk factors for work-related musculoskeletal disorders. Occupational Medicine. (2005) ;55: :190–9. |
[3] | Chiasson M-È , Imbeau D , Major J , Aubry K , Delisle A . Influence of musculoskeletal pain on workers’ ergonomic risk-factor assessments. Applied Ergonomics. (2015) ;49: :1–7. |
[4] | Diego-Mas J-A , Poveda-Bautista R , Garzon-Leal D-C . Influences on the use of observational methods by practitioners when identifying risk factors in physical work. Ergonomics. (2015) ;58: (10):1660–70. |
[5] | Axelsdotter Hök Å, S. Tegle Svensk Företagshälsovård: Litteratur- och faktaöversikt. ((2009) ).Tegle Jansson och Partners AB; 2009. Swedish. |
[6] | Laring J , Neumann P , Nagdee T , Wells R , Theberge N . Human facors tool use among Swedish ergonomists. Association of Canadian Ergonomists 38th Annual Conference October 14-17; (2007) . |
[7] | Whysall ZJ , Haslam RA , Haslam C . Processes, Barriers, and Outcomes Described by Ergonomics Consultants in Preventing Work-Related Musculoskeletal Disorders. Applied Ergonomics. (2004) ;35: (4):343–51. |
[8] | Wells RP , Neumann WP , Nagdee T , Theberge N . Solution Building Versus Problem Convincing: Ergonomists Report on Conducting Workplace Assessments. IIE Transactions on Occupational Ergonomics and Human Factors. (2013) ;1: (1):50–65. |
[9] | Eliasson K , Palm P , Nyman T , Forsman M . Inter- and intra- observer reliability of risk assessment of repetitive work without an explicit method. Applied Ergonomics. (2017) ;62: :1–8. |
[10] | Bramberg EB , Nyman T , Kwak L , Alipour A , Bergstrom G , Elinder LS , et al. Development of evidence-based practice in occupational health services in Sweden: a 3-year follow-up of attitudes, barriers and facilitators. International archives of occupational and environmental health. (2017) ;90: (4):335–48. |
[11] | Logan J , Graham ID . Toward a Comprehensive Interdisciplinary Model of Health Care Research Use. Science Communication. (1998) ;20: (2):227–46. |
[12] | Logan J , Graham ID . The ottawa model of research use. In: Rycroft-Malone J , Bucknall T , editors. Models and frameworks for implementing evidence-based practice: linking evidence to action: John Wiley & Sons; (2011) . |
[13] | Graham K , Logan J . Using the Ottawa Model of Research Use to implement a skin care program. Journal of nursing care quality. (2004) ;19: (1):18–24. |
[14] | Lind C , Rose L. Shifting to proactive risk management: Risk communication using the RAMP tool. Agronomy Research. (2016) ;14: (2):513–24. |
[15] | Lind CM . Pushing and pulling: an assessment tool for occupational health and safety practitioners. International journal of occupational safety and ergonomics. (2018) ;24: (1):14–26. |
[16] | Hsieh HF , Shannon SE . Three approaches to qualitative content analysis. Qualitative Health Research. (2005) ;15: (9). |
[17] | Graneheim UH , Lundman B . Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. (2004) ;24: (2):105–12. |
[18] | Swedish Work Environment Authority (SWEA). Provision 1998:01. Belastningsergonomi.(Physical Ergonomics). Stockholm, Swedish Work Environment Authority; (1998) . Swedish. |
[19] | Swedish Work Environment Authority (SWEA). Provision 2012:2. Belastningsergonomi.(Physical Ergonomics). Stockholm, Swedish Work Environment Authority; (1998) . Swedish. |
[20] | Steinberg U . New Tools in Germany: Development and Appliance of the First two KIM (“Lifting, Holding and Carrying” and “Pulling and Pushing”) and Practical Use of These Methods. Work (2012) ;41: :3990–3996. |
[21] | David G , Woods V , Li G , Buckle P . The development of the Quick Exposure Check (QEC) for assessing exposure to risk factors for work-related musculoskeletal disorders. Appl Ergon. (2008) ;39: (1):57–69. |
[22] | Kadefors R , Forsman M . Ergonomic evaluation of complex work: a participative approach employing video–computer interaction, exemplified in a study of order picking. International Journal of Industrial Ergonomics. (2000) ;25: (4):435–45. |
[23] | Waters T , Putz-Anderson V , Garg A , Fine L . Revised NIOSH equation for the design and evaluation of manual lifting tasks. Ergonomics. (1993) ;36: (7):749–76. |
[24] | McAtamney L , Corlett EN . RULA: A Survey Method for the Investigation of Work-Related Upper Limb Disorders. Applied Ergonomics. (1993) ;24: (2):91–9. |
[25] | Hignett S , McAtamney L . Rapid Entire Body Assessment (REBA). Applied Ergonomics. (2000) ; 31: (2):201–205. |
[26] | Moore JS , Garg A . The Strain Index: a proposed method to analyze jobs for risk of distal upper extremity disorders. Am Ind Hyg Assoc J. (1995) ;56: (5):443–58. |
[27] | Armstrong T . The ACGIH TLV for Hand Activity Level. In: Marras WS and Karwowski W , editors. Fundamentals and assessment tools for occupational ergonomics. Boca Raton: Taylor & Francis Group. (2006) ;1–14. |
[28] | Karhu O , Kansi P , Kuorinka I . Correcting working postures in industry: a practical method for analysis. Applied ergonomics. (1977) ;8: (4):199–201. |
[29] | Occhipinti E . OCRA: A concise index for the assessment of exposure to repetitive movements of the upper limbs. Ergonomics. (1998) ;41: (9):1290–311. |
[30] | Graham ID , Logan J , Harrison MB , Straus SE , Tetroe J , Caswell W , et al. Lost in knowledge translation: time for a map? Journal of continuing education in the health professions. (2006) ;26: (1):13–24. |
[31] | Buckle P , Li G . User needs in exposure assessment for musculoskeletal risk assessment. Proceedings of the First International Cyberspace Conference on Ergonomics. (1996) . |
[32] | Rose L , Lind C , Franzon H , Nord-Nilsson L , Clausén A . Development, implementation and dissemination of ramp: Risk management assessment tool for manual handling proactively. 43rd Annual Nordic Ergonomics Society Conference (NES) (2011) . |
[33] | Berlin C , Örtengren R , Lämkull D , Hanson L . Corporate-internal vs. national standard – A comparison study of two ergonomics evaluation procedures used in automotive manufacturing. International Journal of Industrial Ergonomics. (2009) ;39: (6):940–6. |
[34] | Verbeek J , Kuijer PP . Does KIM what she promises to do? Work. (2012) ; 43: (2):249–50. |
[35] | Arezes PM , Miguel AS , Colim AS . Manual materials handling: Knowledge and practices among Portuguese Health and Safety practitioners. Work. (2011) ;39: (4):385–95. |
[36] | Dempsey PG , McGorry RW , Maynard WS . A survey of tools and methods used by certified professional ergonomists. Applied Ergonomics. (2005) ;36: (4):489–503. |
[37] | Pascual SA , Naqvi S . An Investigation of Ergonomics Analysis Tools Used in Industry in the Identification of Work-Related Musculoskeletal Disorders. International Journal of Occupational Safety & Ergonomics. (2008) ;14: (2):237–45. |
[38] | Andersson I-M . Arbetsmiljöfrågans väg: samverkan mellan kundföretag och företagshälsovård. Stockholm: Arbetslivsinstitutet; (2007) . Swedish. |
[39] | Hasle P , Limborg HJ . A review of the literature on preventive occupational health and safety activities in small enterprises. Ind Health. (2006) ;44: (1):6–12. |
[40] | Schmidt L , Sjöström J , Antonsson A-B . How can occupational health services in Sweden contribute to work ability? Work. (2012) ;41: :2998–3001. |
[41] | Paulsson SÅ , Parmsund M , Hök ÅA , Eriksson T , Nyman T , Schmidt L , et al. Stimulerar avtal mellan arbetsgivare och företagshälsovård till samarbete för hälsosamma arbetsplatser? -En genomlysning av avtal och avtalsprocess. Uppsala: Arbets- och miljömedicin, (2014) . Rapport; 2014:5. Swedish. |
[42] | Eliasson K , Lind C , Nyman T . Facilitators for the implementation of ergonomic interventions. Proceedings of the 47th International the Nordic Ergonomics Society Conference; (2015) . |
[43] | Berlin C , Neumann WP , Theberge N , Örtengren R . ‘Power base’ tactics for workplace change – an interview study with industrial engineers and ergonomists. Ergonomics. (2016) :1–15. |
[44] | Bjurvald M , Nilsson B . Ergonomi på rätt sätt -så här gör du. Stockholm: Prevent; (2007) . Swedish. |
[45] | Lundahl C . WERA - ny modell för riskbedömning vid Scania CV AB. Luleå: Luleå tekniska universitet; (2010) . Swedish. |




