An exploratory study of dialectical behaviour therapy for emotional dysregulation and challenging behaviours after acquired brain injury
Abstract
BACKGROUND:
Challenging behaviours and emotional dysregulation are common sequelae of acquired brain injury (ABI), but treatment remain underdeveloped. Dialectical behaviour therapy is an evidence-based therapy for emotional dysregulation.
OBJECTIVE:
To explore the feasibility and preliminary efficacy of dialectical behaviour therapy for ABI.
METHODS:
An exploratory longitudinal study that compared thirty adults with brain injury presenting persistent emotion dysregulation or challenging behaviours. Control group received a personalized multidisciplinary program only (n = 13). The dialectical behaviour therapy group received five months of emotion regulation skills learning as an add-on (n = 17). Preliminary efficacy was measured on Difficulties in Emotion Regulation Scale-16 and Quality of Life after Brain Injury total score and emotion subscore.
RESULTS:
Fourteen participants completed the dialectical behaviour therapy. This study provided preliminary evidence for the feasibility and acceptability of dialectical behaviour therapy. Repeated measures revealed improvement on the Difficulties in Emotion Regulation Scale-16 (–7.6 [–17.3; 1.7]; Pr = 0.95) and on the Quality Of Life emotion subscore (13.5 [–3.8; 30.9]; Pr = 0.94).
CONCLUSION:
This study raises important questions regarding the type of patients who can benefit from this intervention, necessary adaptations of dialectical behaviour therapy and the way it can help post-traumatic growth and identity reconstruction after ABI.
1Introduction
Acquired brain injury (ABI) often leads to physical, neurocognitive and/or psychological impairments. Challenging behaviours (Howlett et al., 2022; Sabaz et al., 2014; Wiart et al., 2016) and difficulty regulating emotions (Cantor et al., 2014a; Draper et al., 2007; Neumann et al., 2017; Ownsworth & Gracey, 2017) are common sequelae of ABI and especially traumatic brain injury (TBI) (Stéfan & Mathé, 2016). These sequelae cause suffering to the patients, family members’ distress and poor family functioning (Ponsford & Schönberger, 2010) but their management remains to this day challenging for rehabilitation teams. In the face of behavioural, emotional and cognitive disturbances, cognitive behavioural therapy (CBT) appear well suited and are recommended for challenging behaviours (Wiart et al., 2016). Among those, third-wave CBTs seem particularly relevant because they give a central place to emotions. Core to third-wave CBTs are mindfulness, non-judgmental awareness and acceptance strategies that enable changes. The aim is to improve quality of life by making life more meaningful and worth living, rather than reducing symptoms (Ashworth et al., 2017; Thoma et al., 2015). Patients are guided to build a meaningful life by increasing their awareness of their personal values and by encouraging concrete and effective actions (Ownsworth & Gracey, 2017) towards their goals. This is possible thanks to acceptance of life situation (for example that life after ABI is no longer the same as before) and acceptance of the pain that goes with it. Recent researches advocate for the development of third-wave CBT for acquired brain injury (Ashworth et al., 2017) and provides preliminary evidence of efficacy for Acceptance and Commitment Therapy (Sander et al., 2021), for Mindfulness-Based Cognitive Therapy (Bédard et al., 2014) and for Compassion Focused Therapy (Ashworth et al., 2015). Third-wave CBTs suggest that behavioural disorders can be viewed as the result of too strong, too reactive and/or insufficiently regulated emotions, a mechanism called emotional dysregulation. Dialectical Behaviour Therapy (DBT) is a third-wave CBT developed by Marsha Linehan (Linehan, 1993; Lynch et al., 2007), targeting emotional regulation through the acquisition of emotional regulation skills. DBT was initially developed for borderline personality disorder (Linehan et al., 1993), but its use is expanding in other conditions where emotion dysregulation is also a central mechanism (Lynch et al., 2007; Neacsiu et al., 2014), with over 1000 papers describing it use referenced in PubMed. Surprisingly, although classical DBT has gathered strong evidence in other conditions and the rationale for its use in ABI has been advocated (Ownsworth & Gracey, 2017), it has never been tested in ABI.
The aim of this exploratory study was to explore the feasibility of DBT (regarding attrition, attendance and satisfaction) in persons presenting persistent emotional dysregulation or challenging behaviours following ABI. Secondary aims were: 1/ to monitor DBT adaptations needed because of the cognitive difficulties experienced after ABI (in order to develop an ABI-friendly DBT program that could be replicable); 2/ to evaluate the preliminary potential effectiveness of DBT on emotional dysregulation, quality of life and emotion-related quality of life (in order to provide rationale and to calculate the number of participants to be included for a future larger scale trial).
2Methods
2.1Study design
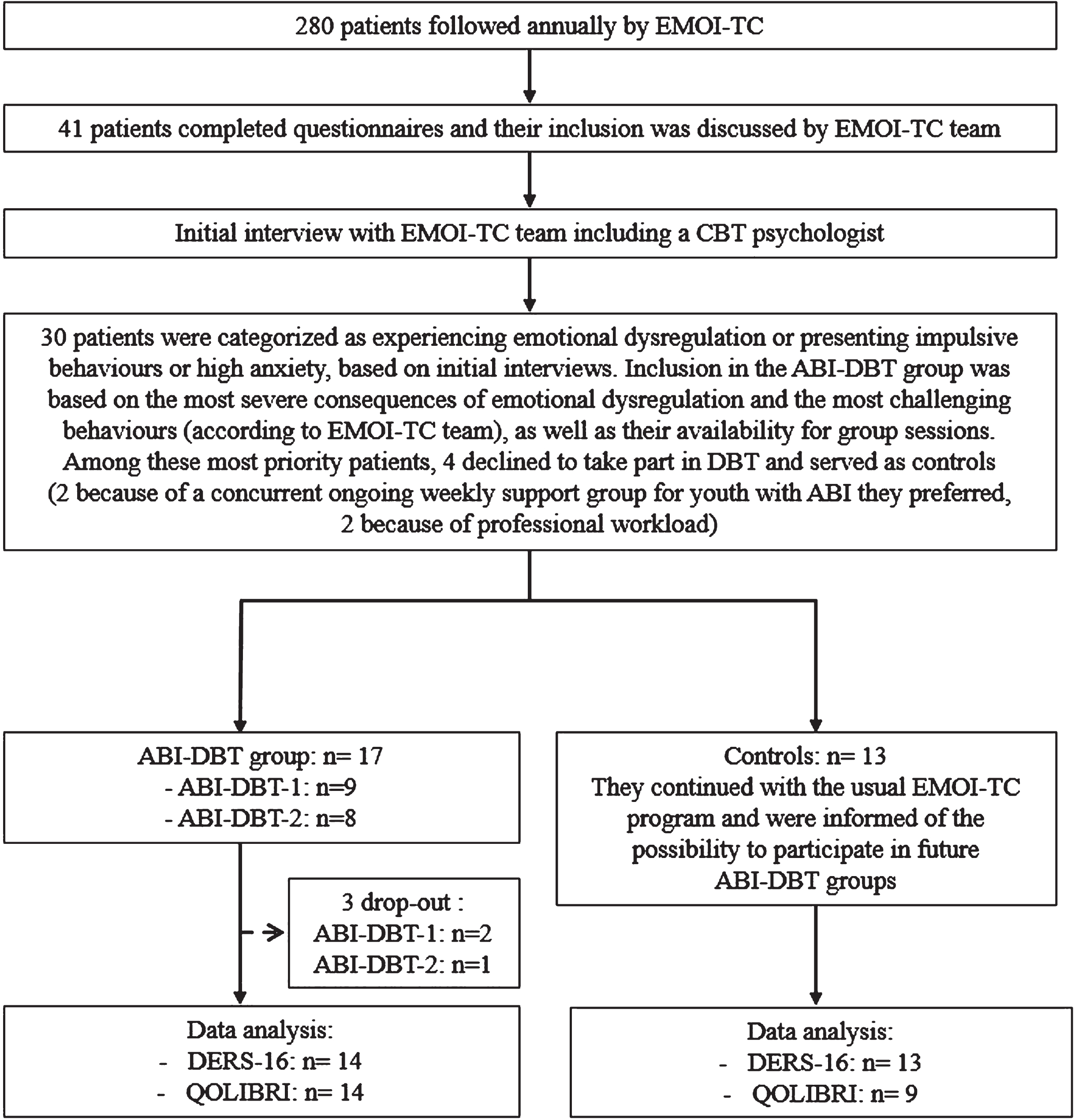
This was a longitudinal study of persons with chronic ABI attending the EMOI-TC service (a personalized multidisciplinary program). It compared the outcomes of control participants (n = 13) receiving EMOI-TC program only to the outcomes of participants receiving the ABI-DBT program (n = 17, divided into two groups) as an add-on to EMOI-TC program (see Table 1 for a description). The first group (ABI-DBT-1 group, n = 9) ran from November 2019 to June 2020 with a three-month break due to COVID-19 containment and the second group (ABI-DBT-2 group, n = 8) ran from January to June 2021. Inclusion flow chart is presented in Fig. 1.
Table 1
Description of the multidisciplinary personalized program EMOI-TC and ABI-DBT program proposed as an add-on to EMOI-TC program
| Multidisciplinary personalizedprogram EMOI-TC | ABI-DBT programcontent | ABI-DBT program groupsession structure | ABI-DBT program homeassignments |
| – Neuropsychological rehabilitation focusing on daily living goals – Construction of the professional/work plan – Psychological support not focused on emotion regulation skills – Social support – Regular visits with physiatrists and psychiatrists specializing in brain injury rehabilitation – Education of the group on the consequences of ABI – Psychological support for patients’ families | – 21 weekly group skills training (2 h 30) – Individual psychotherapy (1 to 4/month) a (1 h) – Intersession access to phone coaching – Weekly homework assignments – Diary card to be filled in every day | – 5 minutes of mindfulness – Homework review(1 h 10) – 15 to 30 minutes break – Presentation of new skills and homework assignments (1 h) | – Weekly homework assignments to practice skills in daily life – Diary card to be filled in every day – YouTube videos reviewing skillsb – Mindfulness practice at homeb |
aABI-DBT-1 group: As this first intervention group had to stop during COVID-19 containment, this group also received 1 to 6 individual skills coaching sessions by telephone during the group’s break. bNote that the ABI-DBT-1 group received YouTube reviews and YouTube mindfulness sessions only after the beginning of the containment, whereas the ABI-DBT-2 group received the YouTube reviews systematically from the beginning of the group.
Fig. 1
Study flowchart.
The study was approved by the Ethics Committee of the Medicine Faculty of Strasbourg University on July 27, 2021 (approval number: CE-2021-101). All participants were informed of the aim, the modalities of the study and of participants’ selection for ABI-DBT. Participants gave written informed consent to use their data.
2.2Participants
For all participants, the inclusion criteria were (a) persistent cognitive and/or behavioural impairments following ABI, (b) sustained at least 18 months prior to pre-intervention assessment, (c) aged 18–65 years, (d) participating in the multidisciplinary personalized EMOI-TC program, (e) presenting with either clear emotional dysregulation or high anxiety or challenging behaviours, perceived as needing emotional regulation skills by the EMOI-TC team, even in the absence of pathological self-rated emotion dysregulation scores.
For all participants, the exclusion criteria were (a) progressive or non-stabilized brain injuries (e.g. brain cancer), (b) being non fluent in French.
It should be noted that due to the high prevalence of comorbidities, especially in participants with TBI, participants with associated developmental disorders, personality disorders and mental disorders (e.g. depression) were not excluded, in order to stay as close as possible to the “real life” participants attending ABI services.
2.3DBT intervention
Usually, full-model DBT includes 4 modes: weekly two hour and fifteen minutes long group skills training, weekly one-hour individual psychotherapy, intersession access to phone coaching to help generalize skills, weekly consultation team meetings for DBT providers (readers can refer to Linehan (1993; 2015) and Rizvi & Roman (2019) for detailed descriptions), but DBT can also be used with only group or only individual session modalities (Linehan, 2017). We used a 21-weeks protocol, initially thought to comprise a group modality only. Therefore, the ABI-DBT-1 group had DBT delivered in group sessions only (with occasionally individual DBT psychotherapy sessions). Feedback after ABI-DBT-1 group (see results) led us to propose the full-model DBT for ABI-DBT-2 group (seeTable 1).
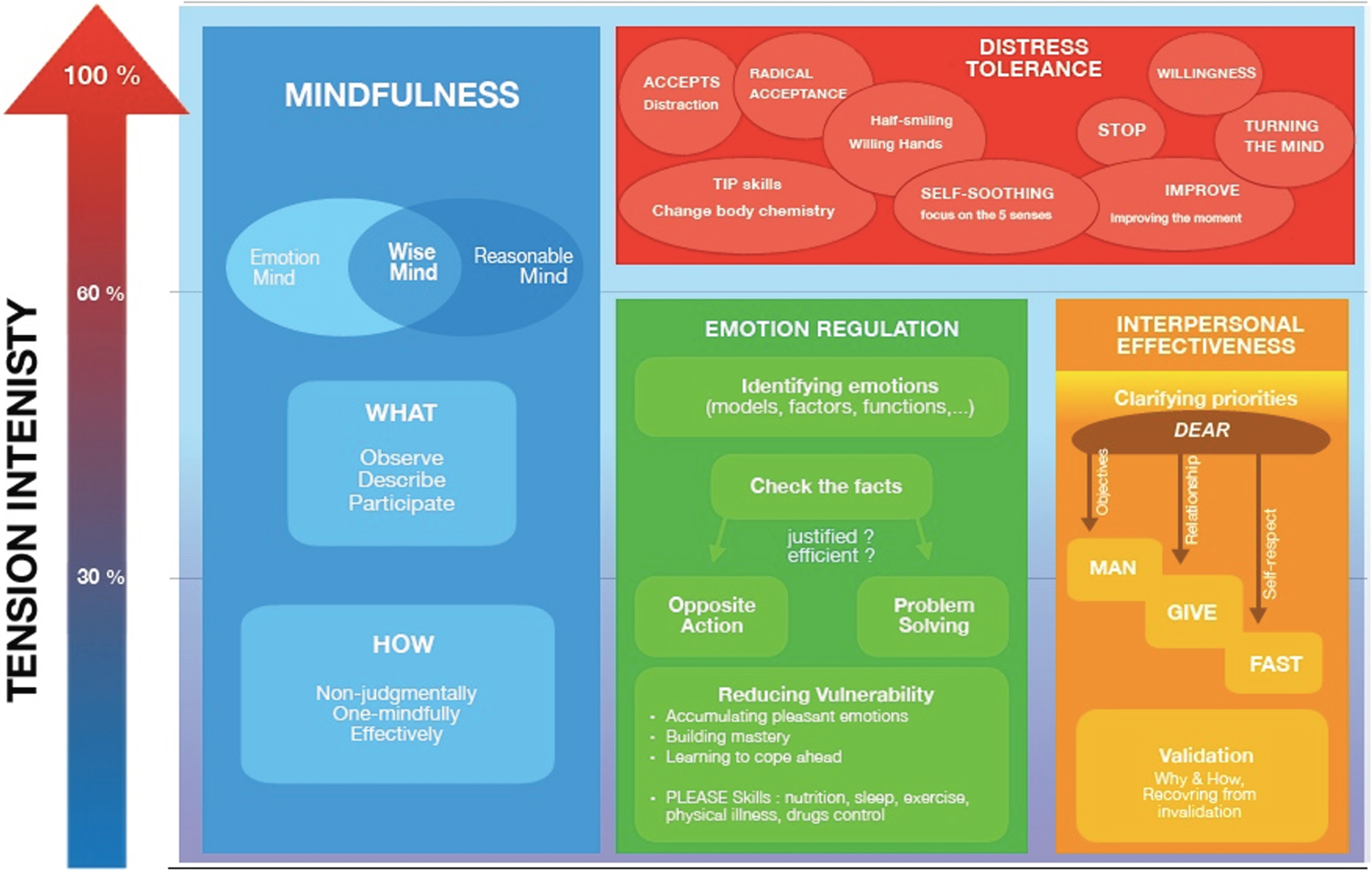
Group skills training covers 4 modules of skills allowing emotion and behaviour regulation: mindfulness, emotion regulation, distress tolerance and interpersonal effectiveness (see Table 2 and Fig. 2 for detailed descriptions). Implementation of DBT was based on DBT manuals (Linehan, 2015; 2017) and we used the Weiner and Bemmouna French version of patients handouts, simplified for patients with autism spectrum disorder (Linehan, 2015; Weiner & Bemmouna, 2019).
Table 2
Brief description of the 4 Dialectical Behaviour Therapy skills modules
| MODULES | DESCRIPTION |
| Mindfulness: The prerequisite skills before learning and using any other skills | It is focusing attention on the present moment, “here and now”, in order to observe what is happening inside and outside of oneself and describe non judgmentally emotions, thoughts and urges to act, during whichever activities the person is engaging in |
| Emotion regulation: To regulate acute or chronic arousal by improving emotional control and learning to modulate emotions | These skills include understanding emotions and their functions, experiencing and labelling emotions, checking if the emotion corresponds to facts, checking if the behaviour/urge to act is in accordance with one’s value, reducing vulnerability to difficult emotions, increasing positive experiences |
| Distress tolerance To use when emotional distress is high, in order not to make things worse (e.g.: by an outburst, aggressive behaviours ...) | These skills include crisis survival skills to tolerate painful life events without engaging in impulsive actions and acceptance skills to radically accept painful situations that are unlikely to change. The aim is not just to be “under control” but to allow emotion level to drop sufficiently in order to have access to the other skills, especially “emotional regulation skills” that are the core of DBT |
| Interpersonal effectiveness: To regulate communication and social interactions | These skills comprise effective communication strategies (e.g.: asking for something assertively or refusing requests, maintaining self-respect in interpersonal situations), strategies for building relationships with others and for supporting valued relationships, even in case of high emotional arousal |
Fig. 2
The use of the 4 DBT modules and their component skills depending on emotional intensity. (Enzo Lachaux, based on (M. M. Linehan, 1993)). Acronyms meaning: DEAR MAN = Describe the current situation; Express your feelings and opinions about the situation; Assert yourself by asking for what you want or saying “No” clearly; Reinforce (reward) the person; Mindful keep your focus on your goals; Appear confident, effective, and competent; Negotiate be willing to give to get. GIVE = (be) Gentle, (act) Interested, Validate, (use an) Easy manner. FAST = (be) Fair, don’t over-Apology, Stick to your Values, be Truthful. ACCEPTS = Activities, Contributions, Comparisons, Emotions, Pushing away, Thoughts, Sensations. TIPP = tip the Temperature, Intense Exercise, Paced breathing, Progressive muscle relaxation. STOP = Stop, Take a step back, Observe, Proceed mindfully. IMROVE = Imagery, Meaning, Prayer, Relaxation, One thing in the moment, Vacation, Encouragement.
Individual therapy focuses on decreasing challenging behaviours, by identifying the variables that influence behaviours. Patients monitor their emotions and challenging behaviours on a diary card every day. This diary card is used in individual sessions to work on one problematic situation of the week using a behavioural chain analysis, which involves: 1) identifying the problematic behaviour, prompting event, vulnerability factors, links in the chain (emotions, thoughts, physical sensations, urges to act, actions) and the consequences of the problematic behaviour (Landes, 2019; Rizvi, 2019; Rizvi & Ritschel, 2014); 2) seeking for most effective solutions (including use of DBT skills) to replace that problematic behaviour by a functionally more appropriate behaviour (a step called “solution analysis” (see supplementary figure 1 for an example of behavioural chain analysis and solution analysis)).
2.4Therapists
Three therapists were involved in each group. They received weekly DBT supervision at the University Hospital of Strasbourg by a CBT and DBT specialist. They relied on the French version of the DBT Skills Training Manual (Linehan, 2017) and were engaged in weekly DBT team consultation at the University Hospital of Strasbourg with DBT specialists, to discuss difficulties and increase adherence to the DBT model.
2.5Outcome measures
2.5.1Feasibility
The feasibility of ABI-DBT was assessed by: a) attrition and attendance rate in ABI-DBT group sessions; b) a satisfaction questionnaire; c) a focus group discussion on the usefulness, difficulties and strengths of ABI-DBT with the participants and the therapists after the two ABI-DBT groups; d) number of DBT skills recalled by ABI-DBT-1 group at the end of the program.
Note that the focus group was not recorded and that therapists only took notes of most salient comments, in order to gather preliminary feedback from patients. The intend was not to conduct a qualitative data analysis following the focus group, which is planned in future research.
2.5.2Preliminary efficacy
Preliminary efficacy was assessed using two scales:
1. The Difficulties in Emotion Regulation Scale-16 (DERS-16) (Bjureberg et al., 2016), the short version of DERS-36 (Gratz & Roemer, 2004), validated in French (Dan-Glauser & Scherer, 2013), is a 16-items scale that assesses emotion regulation difficulties according to 5 factors: lack of emotional clarity, difficulties in engaging in goal-directed behaviours, difficulties in impulse control, limited access to effective emotion regulation strategies, non-acceptance of emotional responses. Items are rated on a five-point Likert scale (1 = “almost never”, to 5 = “almost always”). The DERS-16 can range from 16 to 80, with higher scores reflecting greater levels of emotion dysregulation. The DERS-16 has been found to demonstrate high magnitude correlation with the original DERS-36, excellent internal consistency, good test-retest reliability and convergent and discriminant validity (Bjureberg et al., 2016). DERS-36 have been used previously with patients with ABI (Cantor et al., 2014b; Johnson et al., 2018; Neumann et al., 2017, 2024; Shields et al., 2016; Tsaousides et al., 2017). To our knowledge, no studies have used DERS-16 in ABI so far, but on-going research (Kuppelin et al., In prep) suggests it might be a useful scale in ABI, although its psychometrics properties in this population are unknown. The great advantage of this scale is that its short form is less challenging for patients with cognitive problems and fatigue issues.
2. The Quality of Life after Brain Injury (QOLIBRI) questionnaire (von Steinbüchel et al., 2010), is a 37-items scale that assesses quality of life across 6 factors: cognition, self, daily life and autonomy, social relationships, emotions and physical problems. Items are rated on a five-point Likert scale (for “satisfaction” items: 1 = ’not at all satisfied’ to 5 = ’very satisfied’; for “bothered items” scores are reverse: 1 = ‘very bothered’ and 5 = ‘not at all bothered’). The QOLIBRI scores are reported on a scale from 0 to 100, where 0 is the worst possible quality of life and 100 is the best possible quality of life. The QOLIBRI has been found to demonstrate favourable psychometric properties with acceptable to good internal consistency and test-retest reliability, both in the total sample and in different language groups (von Steinbüchel et al., 2010). The QOLIBRI is the first instrument specifically developed to assess health-related quality of life (QOLIBRI – Online Home of QOLIBRI, n.d.) and has been used in different types of ABI (Heiberg et al., 2018; Mak et al., 2016; Wong et al., 2014). The quality of life total score and the emotion-related quality of life score were used as outcomes.
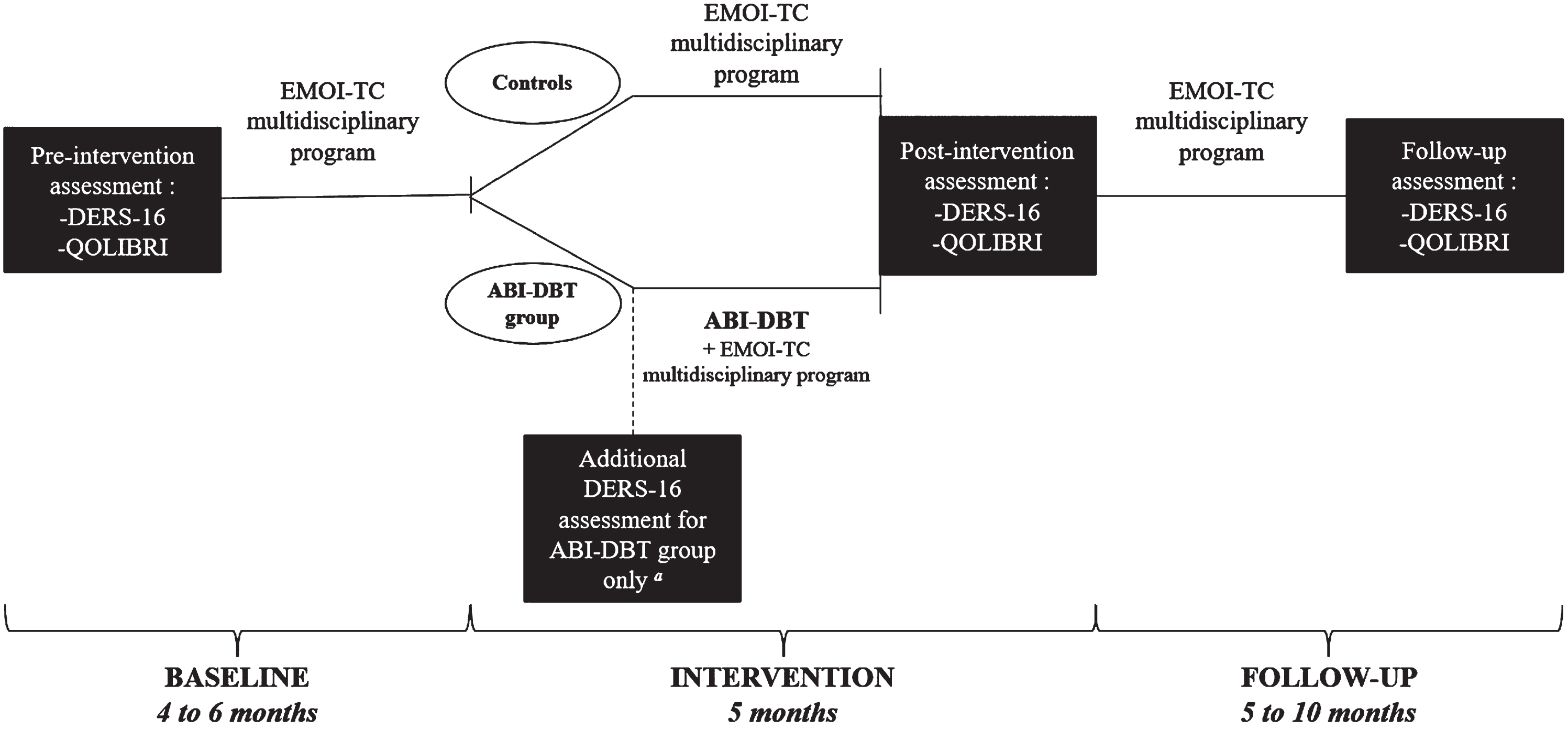
All participants were assessed 4 to 6 months before the intervention (pre-intervention assessment), then entered a 5 months period of either ABI-DBT and EMOI-TC program or EMOI-TC program alone, after which they were assessed again (post-intervention assessment). A small sample of participants who had continued EMOI-TC program (N = 14) were assessed again, 5 to 10 months after the intervention (follow-up assessment) (see Fig. 3 for the assessment design).
Fig. 3
Assessment design. aBecause there is little data on the ability of persons with ABI to self-assess their emotion regulation, we checked ABI-DBT participants’ stability on DERS-16 immediately before the start of the ABI-DBT program. Because the ABI-DBT group had higher DERS-16 scores than controls pre-intervention, DERS stability was crucial to avoid that decrease in DERS-16 scores after intervention would be considered a simple of regression to the mean.
2.6Statistical analysis
Statistical analysis used R v.4.2.2 and JAGS. Continuous outcomes were described using median (quartiles). Qualitative outcomes were described using counts and percentages. Inferential analysis was made under Bayesian paradigm. It relies on a subjectivist definition of probability, where it measures the degree of credibility of a hypothesis. Analysis of the differences for stability used a linear regression. A score was calculated despite missing data if it didn’t exceed twenty percent of the questions. A patient was included in analysis if s/he had at least one valid measure before and after intervention (see Table 3).
Table 3
Number of patients included in analysis by groups and by questionnaires
| N | ABI-DBT group median (q1; q3) | N | Controls median (q1; q3) | ||
| DERS-16 total score | Baseline | 16 | 56 (49; 63) | 13 | 40 (27; 62) |
| Stabilitya | 15 | 52 (41; 60) | – | – | |
| Post-intervention | 14 | 41 (27; 49) | 13 | 35 (22; 42) | |
| Follow-up | 11 | 37 (29; 42) | 9 | 37 (27; 48) | |
| QOLIBRI total score | Baseline | 14 | 51 (43; 56) | 9 | 57 (47; 64) |
| Post-intervention | 14 | 62 (49; 73) | 9 | 62 (56; 74) | |
| Follow-up | 11 | 61 (55; 77) | 7 | 57 (54; 67) | |
| QOLIBRI emotion subscore | Baseline | 14 | 50 (28; 59) | 9 | 50 (40; 80) |
| Post-intervention | 14 | 62 (50; 80) | 9 | 75 (55; 90) | |
| Follow-up | 11 | 70 (62; 75) | 7 | 65 (45; 80) |
aBecause there is little data on the ability of persons with ABI to self-assess their emotion regulation, we checked ABI-DBT participants’ stability on DERS-16 immediately before the start of the ABI-DBT program. Because the ABI-DBT group had higher DERS-16 scores than controls pre-intervention, DERS stability was crucial to avoid that decrease in DERS-16 scores after intervention would be considered a simple of regression to the mean.
The model used for the analysis of repeated continuous outcomes was a mixed beta regression model with a logit link. The variable was transformed from [min;max] to]0;1[using the Smithson & Verkuilen transformation to follow a beta distribution. Then its mean was modeled through a regression based on time, treated as a continuous variable, group and a random effect for subject. The a priori used were minimally informative. From the a posteriori distribution of the parameters, differences were reverse transformed on the original scale. Group differences are ABI-DBT minus controls. Time differences are calculated for a 10 months period. A posteriori distributions are presented this way: median [95% credibility interval] and a posteriori probabilities are calculated comparing the differences with 0. For the initial difference, probabilities towards one translate worse scores in the ABI-DBT group, whereas for the difference in evolution it translates better score improvement in the ABI-DBT group. It must not be confused with a p-value. The models used 3 chains, 155 000 iterations per chain, 5 000 iterations burnt and a thinning of 5. Convergence was assessed graphically and through a R-hat<1.05.
3Results
3.1Participants
Characteristics of the participants are presented in Table 4.
Table 4
Participants’ characteristics
| ABI-DBT group | Controls | |
| N = 17 | N = 13 | |
| Age, median (q1a; q3a), in years | 43 (27; 58) | 31 (21; 60) |
| Sex-ratio (M/F) | 1.1 (9/8) | 5.5 (11/2) |
| Time since ABI in months, median (q1; q3) | 39 (21; 298) | 37 (19; 360) |
| Type of ABI, count (%) | ||
| Stroke | 4 (23%) | 1 (8%) |
| Mild TBIb | 1 (6%) | 3 (23%) |
| Moderate TBIb | 2 (12%) | 0 (0%) |
| Severe TBIb | 6 (35%) | 3 (23%) |
| Other | 4 (23%) | 6 (46%) |
| Educational levelc, count (%) | ||
| 2 | 5 (29%) | 4 (31%) |
| 3 | 1 (6%) | 2 (15%) |
| 4 | 5 (29%) | 4 (31%) |
| 5 | 4 (23%) | 2 (15%) |
| 6 | 1 (6%) | 1 (8%) |
| 8 | 1 (6%) | 0 (0%) |
This table includes the characteristics of the 3 patients who dropout before the end of the study. TBI severity was based on Glasgow Coma Scale initial score, but using the U.S. Department of Veteran Affairs that restricts the diagnosis of mild TBI to injuries with no signs of brain injury on clinical neuroimaging (Howlett et al., 2022). aq1 = first quartile; q3 = third quartile. bTBI = traumatic brain injury. cLevels of study are taken from the nomenclature defined by the French Ministry of Education and the Ministry of Higher Education and Research; for example, level 4 corresponds to the baccalaureate; level 7 to a Master’s degree.
3.2Feasibility and acceptability
3.2.1Attrition and attendance rate
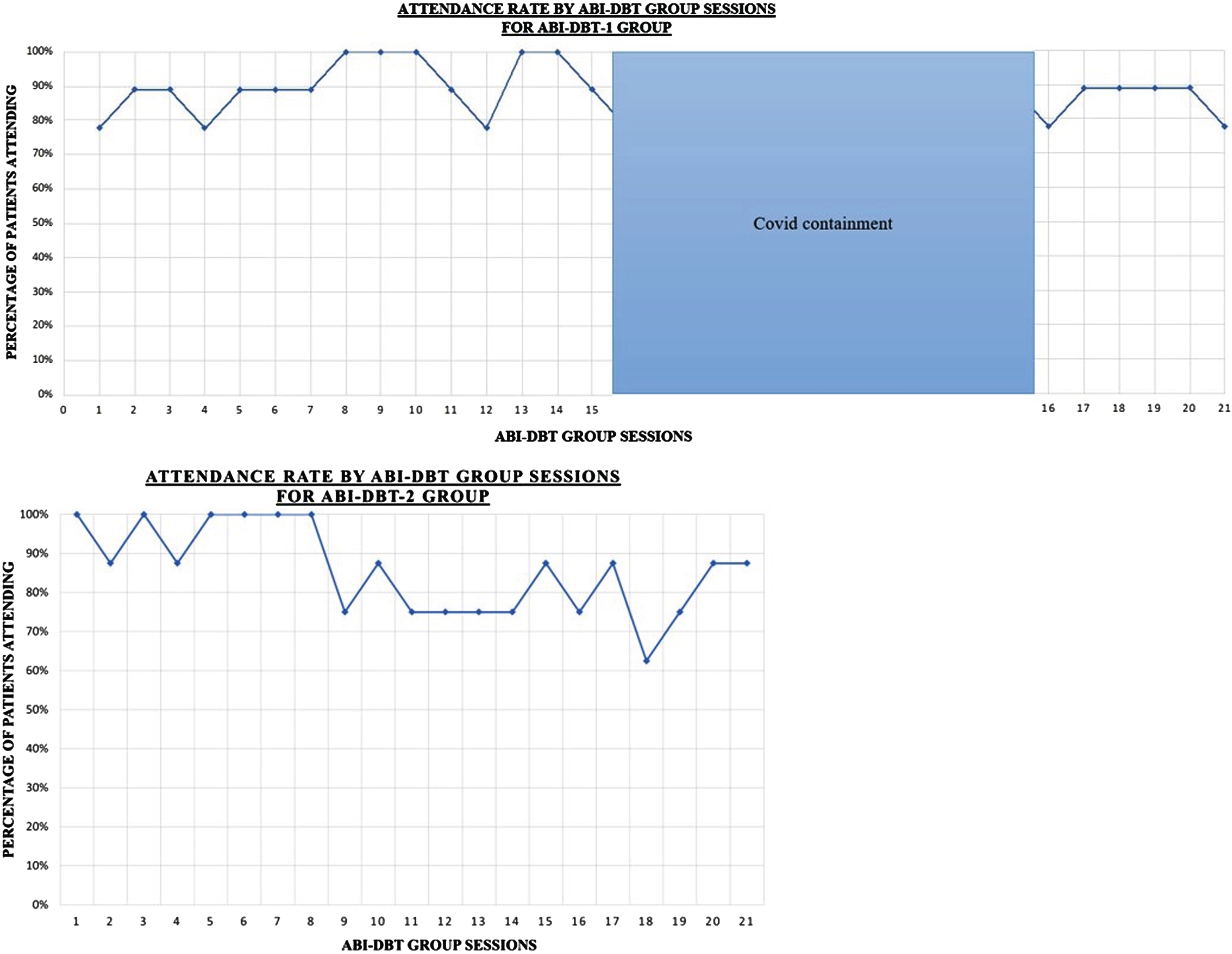
Three participants (18%) out of seventeen dropped out in ABI-DBT group. They had the following characteristics: (1) lack of awareness of the emotional difficulties (participant enrolled mainly because of the high distress of his wife) and severe medical condition (face dog bite with multiple surgery needed during COVID-19 containment) that made coming to the session difficult (ABI-DBT-1); (2) escalating challenging behaviours after COVID-19 containment and unwillingness to continue the program wearing a mask (mandatory post containment) (ABI-DBT-1); (3) busy timetable (working full time, with 2 small children), associated with cognitive fatigue that worsened during the intensive DBT program (ABI-DBT-2).The results showed excellent participation in the group sessions with a median attendance rate of 89% (see Fig. 4). For each participant, missing a session was occasional, with all participants attending most sessions. Note that DBT includes a guideline about missing sessions: participants who miss 4 weeks of scheduled skills training session in a row have dropped out. This attendance rate demonstrates high adherence to the therapy and is particularly interesting for people with ABI for whom fatigue and cognitive impairments can affect their ability to participate.
Fig. 4
Attendance rate for ABI-DBT-1 group and ABI-DBT-2 group.
3.2.2Satisfaction level
The results show good satisfaction (see supplementary figure 2). For ABI-DBT-1 group, satisfaction improved after the first focus group discussion with participants’ feedback and program adaptations.
3.2.3Main participants’ feedback on their experience of ABI-DBT program
Number of DBT skills recalled at the end of the program for ABI-DBT-1: Participants in the ABI-DBT-1 group were able to list a median number of 7 out of 22 skills, which triggered adaptation in DBT program to compensate for memory problems, following CBT recommendations for ABI (Ownsworth & Gracey, 2017). Ten- to fifteen-minute YouTube videos (YouTube channel “GREMO HUS”) were sent to participants after each ABI-DBT group sessions (always the same day during the week), encouraging participants to watch them as many times as needed to improve memorization of DBT skills. Video comprised an explanation of the skill (similar to the English “DBT-RU” YouTube channel), followed by a role play of an emotionally challenging daily life situation, played without and with the use of DBT skills (Durpoix et al., 2021) which allowed to enter into a DBT-language and attitude. After each ABI-DBT group session, participants were reminded of the skill to practice and of home assignments (i.e.-see Table 1) through emails and a WhatsApp group.
Skills: In DBT, skills are often presented as acronyms (see Fig. 2) and those that had non-French meaning were considered challenging to learn (e.g. DEAR MAN). Repetitive revisions seemed required and specifically for those complicated-to-memorize skills.
Participant’s feedback revealed massive resistance to the radical acceptance skill, which is thought to be a major active ingredient for change following DBT (Sayrs & Linehan, 2019). Radical acceptance is the complete and total acceptance of reality as it is, meaning stopping fighting against the reality and accepting it in your mind, heart and body. Although radical acceptance is a skill to use primarily in usual daily life situations that cannot be changed, but that trigger high emotional reactivity (e.g.: partner leaving again dirty socks on the coach), participants viewed most of their daily life problems as related to their ABI and therefore were not willing to “radically accept” the situation, believing this would mean resignation.
Format: Group format was appreciated for not feeling lonely anymore, consistent with extensive literature that encourages group format for ABI interventions (Ownsworth & Gracey, 2017). In the ABI-DBT-2 group, all patients gave the same feedback: that it was essential to learn DBT skills through three modalities (ABI-DBT group sessions, individual therapy sessions and revisions via YouTube videos) together. These adaptations (i.e. systematic use of all 3 modalities) were introduced after the ABI-DBT-1 group feedback and difficulties to recall skills at the end of the program (see above). Participants reported that using these three modalities throughout the program helped them not to drop out and to sustain motivation over the months. Videos especially helped participants to manage the many information given during ABI-DBT group sessions which challenged participants’ cognitive abilities.
3.2.4Feedback of therapists participating in the trial during ABI-DBT-1
Therapists were enthusiastic and felt that DBT allowed evidence-based coaching on how to manage behavioural problems, which contrasted with usually subjective, experience-acquired, advice they usually provided for persons and families living with the consequences of an ABI. Emotion identification was found very difficult for most participants, many needing emotion lists and important stepwise feedback to identify the emotion to regulate. It underlines the importance of the emotional regulation module, in which identifying emotions is the first skill to be learned. Low mental flexibility was a major challenge towards engaging participants in new skills, which led to the introduction of two supplemental skills, including “flexible mind” from an adapted DBT to treat older adults with depression and personality disorder (Lynch & Cheavens, 2007). Emotion regulation skills deficit and flexibility deficit are the focus of this intervention.
Fidelity to DBT model was considered very challenging in a context of program adaptation to a new population and no previous use of DBT outside the initial training. For example, DBT is based on a hierarchy of targets for intervention, where participant’s personal goals and quality of life should be the focus only after life threatening behaviour (hierarchy target 1) and therapy interfering behaviours (hierarchy target 2) have been eliminated. As such, until the participant does not fully participate in all proposed DBT-related tools (i.e. coming to sessions, filling diary card, preparing home assignments, watching YouTube in case of difficulty to memorize the skill ...), therapists should not work with the participant on other goals. This approach was difficult for EMOI-TC therapists in the ABI-DBT-1 group. Failing to follow this hierarchy has the risk of concluding that DBT is not effective, while in fact DBT has not been properly used. To manage this hierarchy, effective psycho-education about this DBT model is essential, both for patients and for therapists to keep it in focus. In fact, this hierarchy is extremely useful and logical, and could even benefit in other interventions. In ABI-DBT-2 group, hierarchy was better respected and simplifications were implemented.
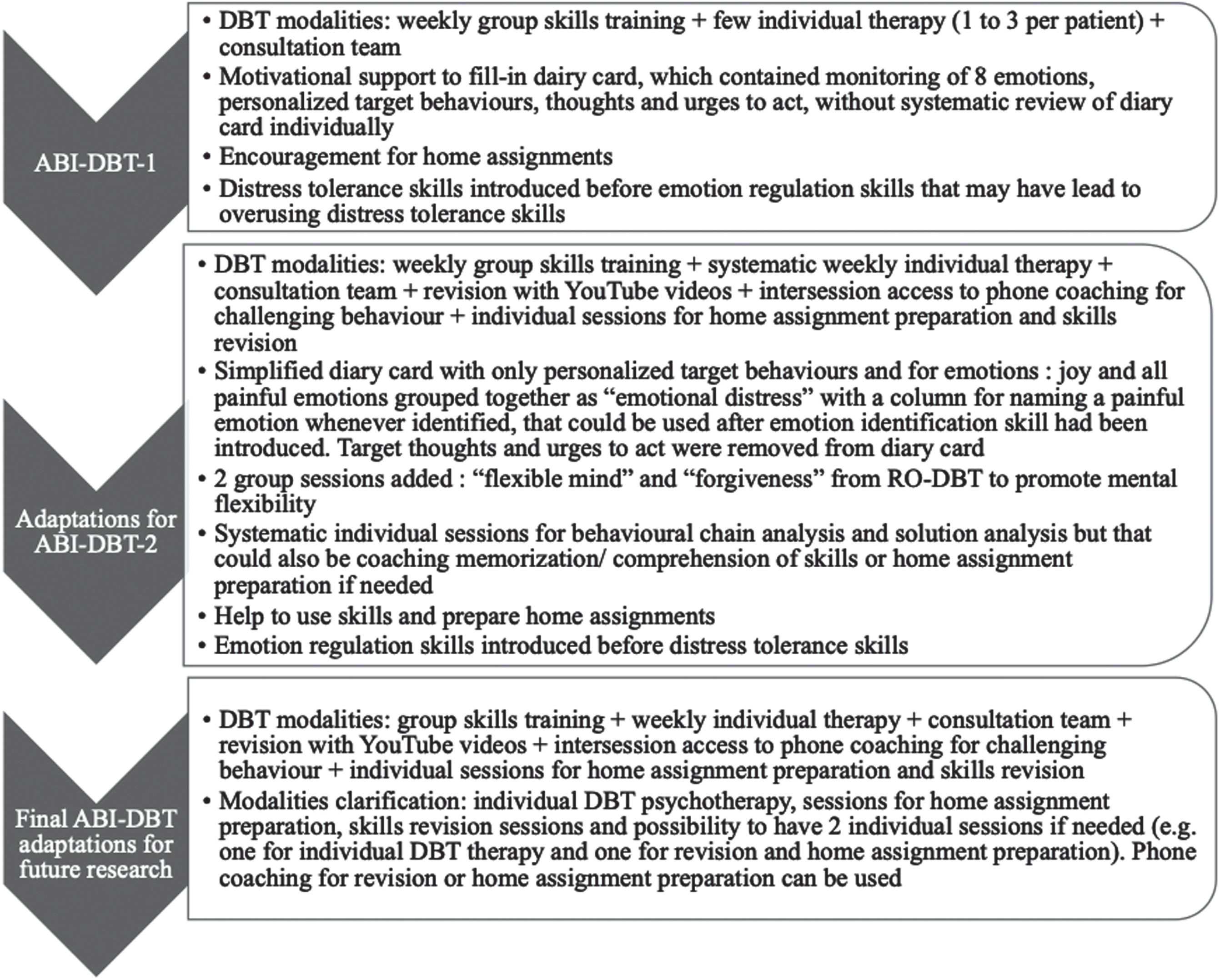
Behavioural chain analysis, used to work on controlling variables of challenging behaviours, was considered a powerful tool but underused by therapists in ABI-DBT-1 because of (1) lack of time (participants needed time during individual sessions to fully understand the skill they had to complete the home assignment which often took the whole hour), (2) participants’ memory problems not enabling participants to remember the chain succession of thoughts and emotions, (3) difficulty to adopt a DBT attitude for participants and therapists used to other models of participant-therapist interactions. Behavioural chain analysis was more systematized for ABI-DBT-2. These different adaptations can be found in Fig. 5.
Fig. 5
ABI-DBT adaptations during program and for future research.
The therapists subjective view (based on commitment to home assignments, diary card and skill practice between sessions) was that the following criteria may be a negative predictor of intervention utility/effectiveness: (1) participants in acute stage waiting for spontaneous improvement; (2) participants included because of family burden but not experiencing themselves distress; (3) participants with low insight and introspective possibility due to cognitive consequences of ABI but also pre-injury functioning; (4) participants not having enough time to commit and practice (e.g.: participants working full time and with young children).
3.3Preliminary efficacy
Emotional dysregulation was associated with poorer quality of life in baseline (Spearman’s correlation coefficient between DERS-16 and QOLIBRI total scores = –0.72 [–0.88; –0.41]). The first repeated measure for the DERS-16 stability, in the ABI-DBT group, represented a mean difference of –2.2 [–4.5; 4.7], but with extremes values ranging from –35 to +18 (see Fig. 6).
Fig. 6
Box plot of DERS-16 total score by assessment times. Dots correspond to score of outliers i.e. scores smaller than the lower quartile plus 1.5 times the IQR, or greater than the upper quartile plus 1.5 times the IQR.
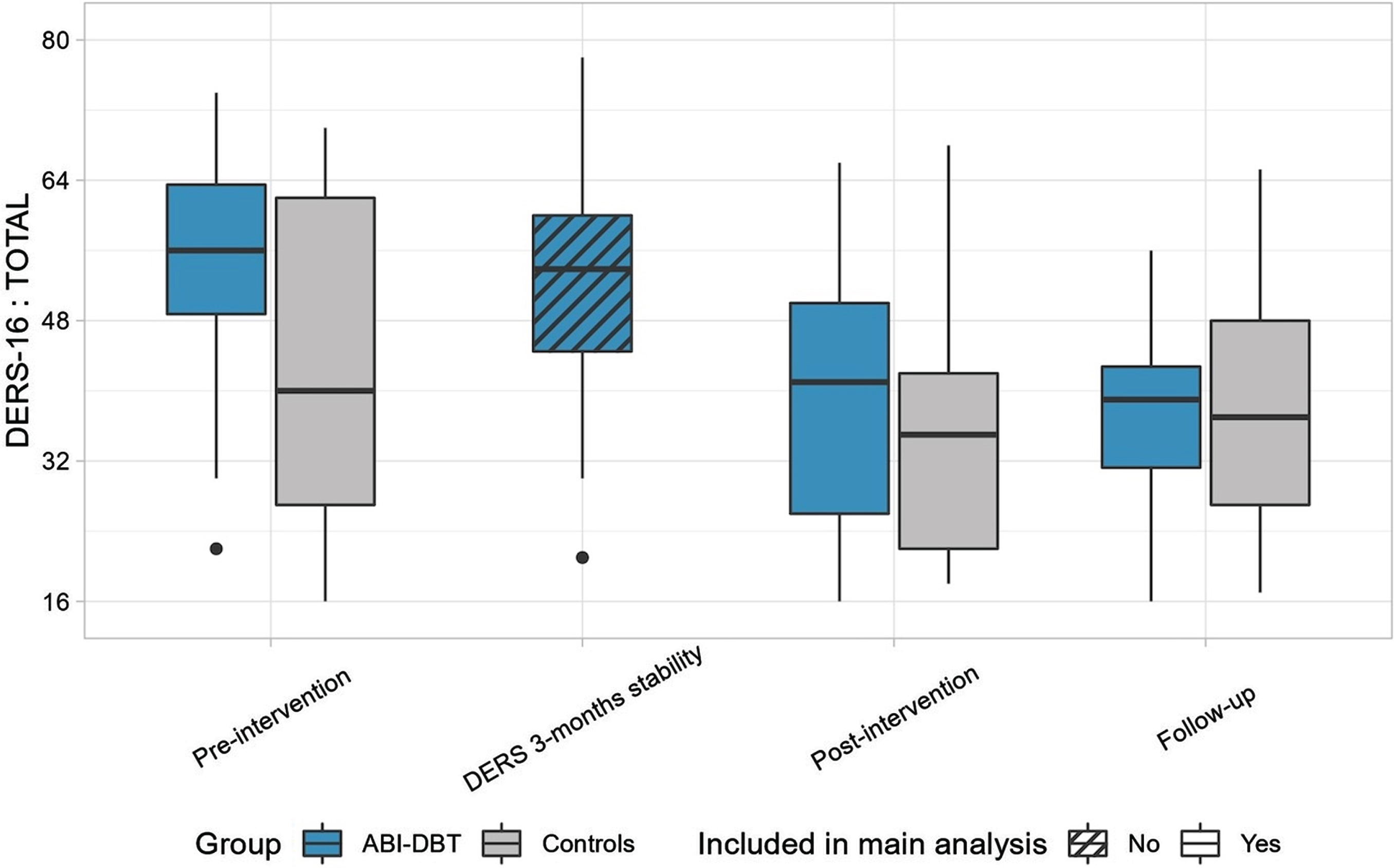
Consistent with our eligibility criteria prioritizing the most dysregulated participants for the ABI-DBT program (inclusions flowchart -see Fig. 1) and the non-randomized nature of the study, the ABI-DBT group had higher emotion dysregulation scores than the controls. There was a mean difference of 10.4 [–4.3; 24.5] (Pr = 0.92) on the DERS-16 questionnaire, prior to the intervention. Score change was better in the ABI-DBT group than in controls (–12.6 [–19.4; –5.6] vs –4.5 [–10.9; 1.8]) for a difference of –7.6 [–17.3; 1.7] (Pr = 0.95) (see Fig. 6 and Table 5).
Table 5
Bayesians statistics of the evolution of DERS-16 and QOLIBRI questionnaires
| DERS-16 Total (N = 27) | Prd | QOLIBRI Total (N = 23) | Prd | QOLIBRI Emotion (N = 23) | Prd | |
| Initial differencea,b | 10.4 [–4.3; 24.5] | 0.92 | –3.5 [–18.7; 12.4] | 0.67 | –15.5 [35.1; 5.4] | 0.93 |
| Evolution in controlsa,c | –4.5 [–10.9; 1.8] | – | 3.8 [–5.5; 13.2] | – | 1.7 [–10.0; 14.2] | – |
| Evolution in ABI-DBT groupa,c | –12.6 [–19.4; –5.6] | – | 9.2 [1.0; 17.3] | – | 15.5 [3.7; 27.1] | – |
| Difference of evolutiona,b | –7.6 [–17.3; 1.7] | 0.95 | 5.2 [–6.7; 17.8] | 0.80 | 13.5 [–3.8; 30.9] | 0.94 |
aAll results are medians [95% credibility interval] on the a posteriori mean differences distributions from the original scale. bGroups differences are always ABI-DBT group minus controls. cDifferences in time are calculated for a ten months period. dFor initial difference, a probability towards one shows worse scores in the ABI-DBT group; for difference of evolution it shows better improvement in the ABI-DBT group.
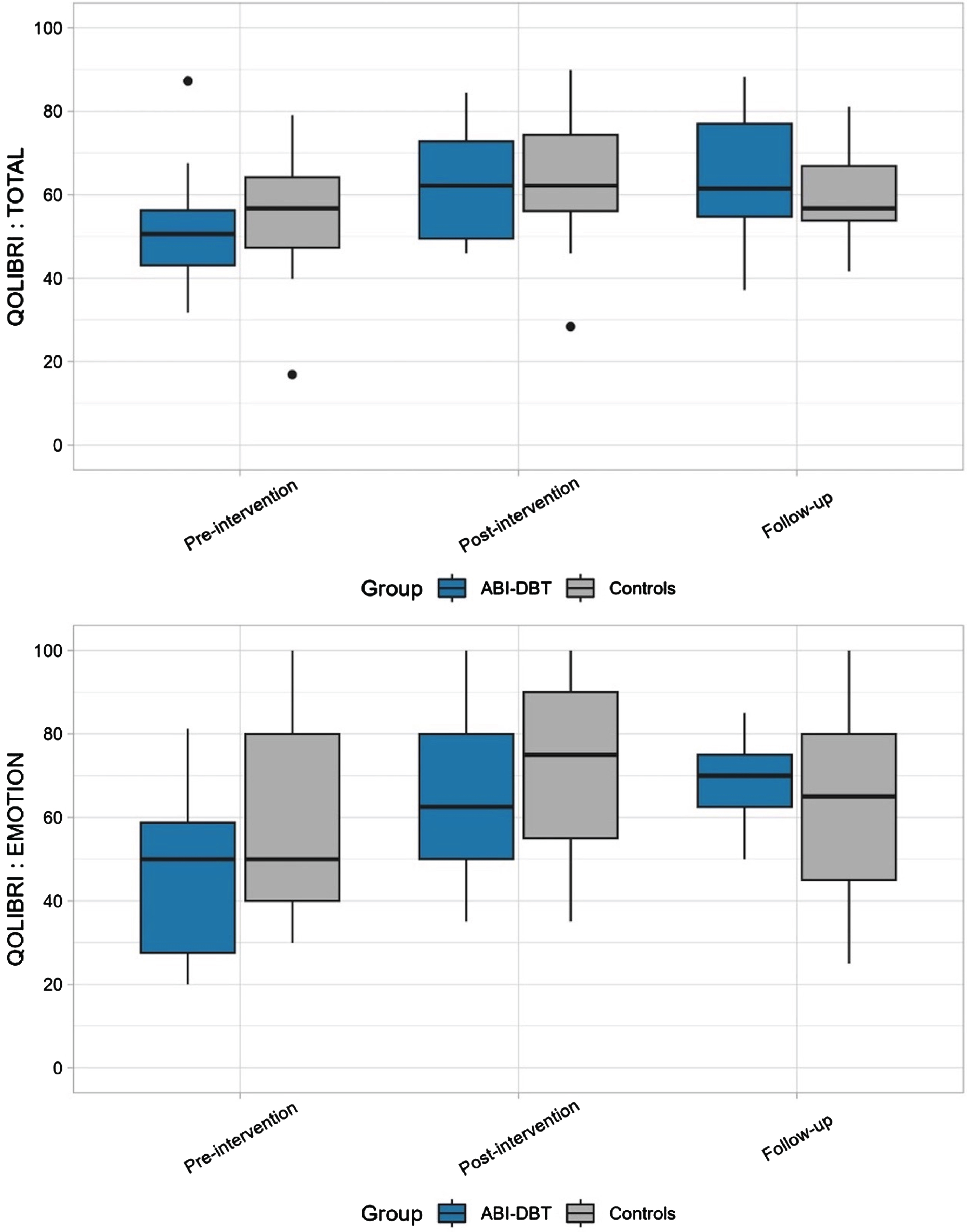
On the total QOLIBRI score, there was an initial mean difference of –3.5 [–18.7; 12.4] (Pr = 0.67). Score change was also slightly better in the ABI-DBT group (9.2 [1.0; 17.3] vs 3.8 [–5.5; 13.2]) for a difference of 5.2 [–6.7; 17.8] (Pr = 0.80). These differences were more pronounced on the emotion subscale of the QOLIBRI. The mean difference pre-intervention was –15.5 [35.1; 5.4] (Pr = 0.93). Score change was better in the ABI-DBT group (15.5 [3.7; 27.1] vs 1.7 [–10.0; 14.2]) for a difference of 13.5 [–3.8; 30.9] (Pr = 0.94) (see Fig. 7 and Table 5).
Fig. 7
Box plot of QOLIBRI total score and QOLIBRI emotions subscore by assessment times. Dots correspond to score of outliers i.e. scores smaller than the lower quartile plus 1.5 times the IQR, or greater than the upper quartile plus 1.5 times the IQR.
4Discussion
This exploratory study provides preliminary evidence for the feasibility and acceptability of DBT after ABI based on excellent participation, low attrition rate and good satisfaction of both participants and therapists. Administering DBT in group sessions only was not sufficient to learn skills so individual sessions and revisions on YouTube had to be introduced after participants’ and therapists’ feedback. Regarding outcome measures, satisfying stability was shown on the DERS-16 prior to the intervention, but with a high intra-individual variability for some patients (suggesting that this questionnaire may not be reliable for all patients with ABI). Both the DERS-16 and the QOLIBRI emotion subscore were sensitive to change, although there was an inter-individual variability in the response to treatment. The non-randomized nature of the study induced not comparable groups in terms of severity of emotional regulation, but also in terms of sex ratio (in controls women were less represented). Therefore, we cannot conclude on the effectiveness of DBT but we can only suggest its preliminary potential efficacy. In a context of need for interventions targeting challenging behaviours and emotional dysregulation after ABI, this exploratory study showed encouraging results to use DBT to treat emotional dysregulation in people with ABI (Ashworth et al., 2017; Ownsworth & Gracey, 2017). Although originally it was intended to be an exploratory study to a randomized controlled trial (RCT), this study brought severalquestions.
What is emotional dysregulation in the context of ABI? How is it related to impulsivity, behavioural executive syndrome or simply anxiety experienced in relation to the changes after ABI/ adjustments? Emotional dysregulation has mainly been explored as part of post-traumatic stress disorder (PTSD) after TBI (Weis et al., 2022). It is thought to be a transdiagnostic feature of many psychiatric conditions (Neacsiu et al., 2014) including those often encountered by persons with ABI (depression, anxiety disorders ...). Better conceptualization of emotional dysregulation in ABI could lead to a better understanding of the emotional and behavioural problems patients and their families experience.
DBT skills like STOP and TIPP (see Fig. 2) are particularly useful components for ABI-related impulsivity, but implementation of DBT in ABI must be based on the extensive DBT literature outside ABI that showed that overreliance on distress tolerance skills (such as STOP and TIPP) negatively impacts intervention outcome (Dunkley, 2018), because it does not tackle the root of the behaviour i.e. emotional regulation.
Is there an entity such as emotional dysregulation related to ABI or is it just a comorbidity? An obvious question is: are there specific brain areas implicated that can predict emotional dysregulation? For us, this last question is secondary as far as interventions are concerned. Brain injuries, irrespective of their localization, provide room for emotional dysregulation, even in the absence of lesions in areas or connectivity of emotion-related brain pathways: (a) fatigue is known to massively influence emotion regulation and persons with ABI experiencing chronic, accelerated, severe cognitive fatigue are much more likely to experience emotion dysregulation as a result; (b) ABI induces a series of life stressors due to changes in family and societal roles, with insecurity triggering emotional dysregulation, (c) experiencing repeated cognitive dysfunction and failures in daily life activities through the day may overwhelm emotion regulation capacities; (d) Patients with ABI (and TBI especially) often have psychiatric comorbidities responsible for emotional dysregulation (Alway et al., 2016).
Who can benefit most from DBT? Which format should be used? In case of low or moderate cognitive impairments, adaptations like repetitions and spaced retrieval of key learning (Ownsworth & Gracey, 2017), external aids (like YouTube videos) to compensate for learning and memory problems seem essential. In case of severe cognitive impairments, Skills System®, based on DBT, has been used by Brown et al. (Brown et al., 2013) for persons with intellectual impairments. It is a different and massively simplified program compared to standard DBT, with fewer emotion regulation skills and using pictograms. This may be the best format for persons with severe cognitive impairments after ABI. Outside the classical third wave CBTs trials, other studies explore how emotional regulation can enhanced by increasing emotional self-awareness. However past studies did not focus on specific emotional regulation skills (Neumann et al., 2017), while our study specifically trained evidence-based skills from DBT. Neumann et al. found that improving emotional awareness and labeling can partially help people to better control some unpleasant emotions but their intervention was not sufficient on its own for lasting effect. They concluded that this type of intervention should be considered as a precursor or supplement to intervention that explicitly teach patients how to regulate emotions.
The duration of DBT can vary according to the types of dysregulation, patients and their cognitive impairments. Future research on DBT must ensure that intervention and follow-up is long enough, as previous emotion regulation approaches failed to show benefits (Cantor et al., 2014c). For all DBT formats, anosognosia seams a major challenge. Finally, neuropsychological and speech language rehabilitation may be extremely useful during ABI-DBT, to help patients to structure their thoughts and decrease digressions (the preparation of home assignment can actually become an excellent rehabilitation tool to learn how to synthetize thoughts and to communicate effectively). This is particularly important in order to ensure the effectiveness of group sessions (limited time available per participant) but also individual session (to keep focused on chain analysis). Future research could better define the timings and modalities of cognitive rehabilitation in relation to emotional regulation skills learning.
What is DBT useful for? And how can emotional dysregulation be evaluated? DBT’s target is emotional dysregulation causing challenging behaviours that make people’s life unbearable. The aim is to build “a life worth living”. The aim of ABI-DBT intervention is perhaps not so much to lower emotional levels but to help persons living with an ABI to choose their behaviour in accordance with their life goals (even in the presence of unchanged high emotional levels). Among emotion regulation skills, this implies values identification, planning activities in accordance to one’s values and personal goals. In this context of learning how to deal differently with internal experiences in order to build a fulfilling life, one idea is to explore if DBT could be a tool for post-traumatic growth (defined as “positive change that the individual experiences as a result of the struggle with a traumatic event” (Calhoun & Tedeschi, 1999), p.11) (Baseotto et al., 2020; Tedeschi & Calhoun, 2004) and identity reconstruction (Levack et al., 2014), i.e. targeting something wider than quality of life. Further, DBT may impact not only the participants but their families: future research could evaluate changes in family functioning, burden, and following a DBT program for the family member.
4.1Limitations
This study was exploratory and set in a care-as-usual service for ABI (EMOI-TC). The advantage is that it was a setting that shows the feasibility of implementing DBT in usual services, but it induced a number of limits that should be emphasize when interpreting our results. Participants were not randomized, ABI-DBT group had higher emotional dysregulation. Controls were therefore not matched and it cannot be assumed that the less severe controls would have shown gains or even found utility in the ABI-DBT program. The fact that ABI-DBT group rated their DERS-16 twice before intervention and controls once only, may have influenced score. It is however unlikely, as participants are used to rate these questionnaires, including DERS-16, as part of their usual EMOI-TC program, neurological and psychiatric follow-up, expertise assessments.
Because inclusion was based on EMOI-TC perception of “need for emotion regulation skills”, the sample is heterogenous. Not all participants had a clear emotion dysregulation on DERS-16. However, based on EMOI-TC knowledge of the patients’ clinical presentation and history, and consequences of their challenging behaviours, all patients corresponded to an emotion dysregulation such as described by Beauchaine (“a pattern of emotional experience and/or expression that interferes with appropriate goal-directed behaviour” and “emotions experienced either too intensely or too enduringly to be adaptive” (Beauchaine, 2015)), rather than simply emotional burden (impulsivity, anxiety ...) related to ABI.
Although satisfaction and feedback were assessed also anonymously in a written form, focus group discussion may have constrained some participants’ negative views. A formalized qualitative methodology was not used: focus group were not audio-recorded and transcribed but main ideas brought by the participants and therapists were written down by a therapist, which may have induced biases. Future studies should include a clear qualitative methodological model and individual interviews to better analyze participants feedback and to better explore the benefits of DBT outside emotional regulation.
Fidelity to the DBT model, especially in individual sessions was not assessed and was probably insufficient in ABI-DBT-1 group: this is a major flaw of the study. Adaptations made for ABI-DBT-2 group were useful: therapists’ fidelity to DBT model as well as patients’ adherence to therapy and benefits seemed improved, although no fidelity checklist has been used, which is another flaw. In future research, the DBT adherence checklist will be used (Harned et al., 2023). Future research should stay closer to the DBT model: behavioural chain analysis, self-monitoring diary card and target hierarchy are active ingredients that cannot be neglected even if their application with ABI is challenging. Treatment fidelity is essential to any trial and to DBT it is even more essential as the therapy has strong evidence to rely on. Therapists working with ABI are not familiar with DBT and a prolonged use of DBT is needed before engaging them in an RCT. Conversely, experienced DBT therapists are not familiar with the cognitive challenges of participants with ABI, as DBT is mainly used in psychiatry, with persons presenting borderline personality disorder.
For future research, an adapted version of DBT (using the present study ABI-DBT-2 format), containing the same skills as original DBT and based on Neacsiu et al. and Weiner for 16-weeks duration (Neacsiu et al., 2014; Weiner, 2019) could be used. The following modalities should be further explored for persons living with ABI: the 4 modes of DBT: (1) weekly group skills training (2) weekly individual psychotherapy, (3) intersession access to phone coaching, (4) weekly consultation team for DBT providers, in adjunction with 2 modalities explored specifically for ABI in this exploratory study: (5) sessions planned specifically for skills revisions and home assignment preparation in an individual session format or by phone (6) sending YouTube videos presenting DBT skills and illustrating them with examples to repeat skills in memory. The latter seem to promote skills retention, adherence to home assignments and therefore ecological use of skills and participation in the group modality. It may contribute to better generalization and automatization to daily life. However, such an intervention will be intensive. So, indications for such an intensive program must be well reasoned to target persons with high behavioural and emotional burden.
5Conclusion
In conclusion, using DBT group modality alone does not seem feasible for patients with cognitive impairments after ABI but the full-model DBT seems a promising tool. Other outcome measures than quality of life, however, should also be searched for, to better capture the changes due to DBT in persons and families experiencing the consequences ofan ABI.
Acknowledgments
We are grateful to Luisa Weiner and Sébastien Weibel for supervising DBT implementation; to Enzo Lachaux and Doha Bemmouna for providing an adapted version of the French DBT manual with patients’ handouts and Fig. 2 in this manuscript; and to Claire Di Santi, the EMOI-TC team and all participants for their implication in this study.
Conflict of interest
The authors declare no conflict of interest.
Ethics statement
The study was approved by the Ethics Committee of the Medicine Faculty of Strasbourg University on July 27, 2021 (approval number: CE-2021-101). The study was conducted in accordance with the Declaration of Helsinki.
Informed consent
Participants were informed of the aim, the modalities of the study and of participants selection for ABI-DBT. All participants provided written informed consent to use their data.
Funding
The authors report no funding.
Supplementary material
[1] The supplementary figures is available in the electronic version of this article: https://dx.doi.org/10.3233/NRE-230383
References
1 | Alway, Y. , Gould, K. R. , Johnston, L. , McKenzie, D. , & Ponsford, J. ((2016) ). A prospective examination of Axis I psychiatric disorders in the first 5 years following moderate to severe traumatic brain injury. Psychological Medicine, 46: (6), 1331–1341. https://doi.org/10.1017/S0033291715002986 |
2 | Ashworth, F. , Clarke, A. , Jones, L. , Jennings, C. , & Longworth, C. ((2015) ). An exploration of compassion focused therapy following acquired brain injury. Psychology and Psychotherapy: Theory, Research and Practice, 88: (2), 143–162. https://doi.org/10.1111/papt.12037 |
3 | Ashworth, F. , Evans, J. J. , & McLeod, H. ((2017) ). Third wave cognitive and behavioural therapies: Compassion Focused Therapy, Acceptance and Commitment Therapy and Positive Psychotherapy. In Neuropsychological rehabilitation: The international handbook (pp. 327–339). Routledge/Taylor & Francis Group. |
4 | Baseotto, M. C. , Morris, P. G. , Gillespie, D. C. , & Trevethan, C. T. ((2020) ). Post-traumatic growth and value-directed living after acquired brain injury. Neuropsychological Rehabilitation, 1–20. https://doi.org/10.1080/09602011.2020.1798254 |
5 | Beauchaine, T. P. ((2015) ). Future Directions in Emotion Dysregulation and Youth Psychopathology. Journal of Clinical Child and Adolescent Psychology: The Official Journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division, 44: (5), 875–896. https://doi.org/10.1080/15374416.2015.1038827 |
6 | Bédard, M. , Felteau, M. , Marshall, S. , Cullen, N. , Gibbons, C. , Dubois, S. , Maxwell, H. , Mazmanian, D. , Weaver, B. , Rees, L. , Gainer, R. , Klein, R. , & Moustgaard, A. ((2014) ). Mindfulness-based cognitive therapy reduces symptoms of depression in people with a traumatic brain injury: Results from a randomized controlled trial. The Journal of Head Trauma Rehabilitation, 29: (4), E13–E22. https://doi.org/10.1097/HTR.0b013e3182a615a0 |
7 | Bjureberg, J. , Ljótsson, B. , Tull, M. T. , Hedman, E. , Sahlin, H. , Lundh, L.-G. , Bjärehed, J. , DiLillo, D. , Messman-Moore, T. , Gumpert, C. H. , & Gratz, K. L. ((2016) ). Development and Validation of a Brief Version of the Difficulties in Emotion Regulation Scale: The DERS-16. Journal of Psychopathology and Behavioral Assessment, 38: (2), Article 2. https://doi.org/10.1007/s10862-015-9514-x |
8 | Brown, J. F. , Brown, M. Z. , & Dibiasio, P. ((2013) ). Treating Individuals With Intellectual Disabilities and Challenging Behaviors With Adapted Dialectical Behavior Therapy. Journal of Mental Health Research in Intellectual Disabilities, 6: (4), 280–303. https://doi.org/10.1080/19315864.2012.700684 |
9 | Calhoun, L. G. , & Tedeschi, R. G. ((1999) ), Facilitating Posttraumatic Growth: A Clinician’s Guide. Routledge. https://doi.org/10.4324/9781410602268 |
10 | Cantor, J., Ashman, T., Dams-O’Connor, K., Dijkers, M. P., Gordon, W., Spielman, L., Tsaousides, T., Allen, H., Nguyen, M., & Oswald, J. ((2014) a). Evaluation of the Short-Term Executive Plus Intervention for Executive Dysfunction After Traumatic Brain Injury: A Randomized Controlled Trial With Minimization. Archives of Physical Medicine and Rehabilitation, 95: (1), 1-9.e3. https://doi.org/10.1016/j.apmr.2013.08.005 |
11 | Cantor, J., Ashman, T., Dams-O’Connor, K., Dijkers, M. P., Gordon, W., Spielman, L., Tsaousides, T., Allen, H., Nguyen, M., & Oswald, J. ((2014) b). Evaluation of the Short-Term Executive Plus Intervention for Executive Dysfunction After Traumatic Brain Injury: A Randomized Controlled Trial With Minimization. Archives of Physical Medicine and Rehabilitation, 95: (1), Article 1. https://doi.org/10.1016/j.apmr.2013.08.005 |
12 | Cantor, J., Ashman, T., Dams-O’Connor, K., Dijkers, M. P., Gordon, W., Spielman, L., Tsaousides, T., Allen, H., Nguyen, M., & Oswald, J. ((2014) c). Evaluation of the short-term executive plus intervention for executive dysfunction after traumatic brain injury: A randomized controlled trial with minimization. Archives of Physical Medicine and Rehabilitation, 95: (1), 1-9.e3. https://doi.org/10.1016/j.apmr.2013.08.005 |
13 | Dan-Glauser, E. S. , & Scherer, K. R. ((2013) ). The Difficulties in Emotion Regulation Scale (DERS): Factor Structure and Consistency of a French Translation. Swiss Journal of Psychology, 72: (1), Article 1. https://doi.org/10.1024/1421-0185/a000093 |
14 | Draper, K. , Ponsford, J. , & Schönberger, M. ((2007) ). Psychosocial and Emotional Outcomes Years Following Traumatic Brain Injury. Journal of Head Trauma Rehabilitation, 22: (5), 278–287. https://doi.org/10.1097/01.HTR.0000290972.63753.a7 |
15 | Dunkley, C. ((2018) ). Conceptual and Practical Issues in the Application of Emotion Regulation in Dialectical Behaviour Therapy. In Swales M. A. (Ed.), The Oxford Handbook of Dialectical Behaviour Therapy (p. 0). Oxford University Press. https://doi.org/10.1093/oxfordhb/9780198758723.013.31 |
16 | Durpoix, A. , Weiner, L. , Bemmouna, D. , Lachaux, E. , Krasny-Pacini, A. , & Weibel, S. ((2021) ). Psychoéducation et régulation émotionnelle en temps de confinement. Annales Médico-Psychologiques, Revue Psychiatrique. https://doi.org/10.1016/j.am2021.10.016 |
17 | Gratz, K. L. , & Roemer, L. ((2004) ). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 26: (1), 41–54. https://doi.org/10.1023/B:JOBA.0000007455.08539.94 |
18 | Harned, M. S. , Schmidt, S. C. , Korslund, K. E. , & Gallop, R. J. ((2023) ). Development and Evaluation of a Pragmatic Measure of Adherence to Dialectical Behavior Therapy: The DBT Adherence Checklist for Individual Therapy. Administration and Policy in Mental Health and Mental Health Services Research, 50: (5), 734–749. https://doi.org/10.1007/s10488-023-01274-x |
19 | Heiberg, G. , Pedersen, S. G. , Friborg, O. , Nielsen, J. F. , Holm, H. S. , Steinbüchel von, N. , Arntzen, C. , & Anke, A. ((2018) ). Can the health related quality of life measure QOLIBRI- overall scale (OS) be of use after stroke? A validation study. BMC Neurology, 18: (1), 98. https://doi.org/10.1186/s12883-018-1101-9 |
20 | Howlett, J. R. , Nelson, L. D. , & Stein, M. B. ((2022) ). Mental Health Consequences of Traumatic Brain Injury. Biological Psychiatry, 91: (5), 413–420. https://doi.org/10.1016/j.biopsych.2021.09.024 |
21 | Johnson, R. A. , Albright, D. L. , Marzolf, J. R. , Bibbo, J. L. , Yaglom, H. D. , Crowder, S. M. , Carlisle, G. K. , Willard, A. , Russell, C. L. , Grindler, K. , Osterlind, S. , Wassman, M. , & Harms, N. ((2018) ). Effects of therapeutic horseback riding on post-traumatic stress disorder in military veterans. Military Medical Research, 5: (1), 3. https://doi.org/10.1186/s40779-018-0149-6 |
22 | Kuppelin, M., Goetsch, T., Bemmouna, D., Lagzouli, A., Weiner, L., & Krasny-Pacini, A. (In prep). Emotion dysregulation in adults with acquired brain injury: Comparison to nonclinical controls and borderline personality disorder using the DERS-16 scale. Manuscript in Preparation. |
23 | Landes, S. J. ((2019) ). Conducting effective behavioural and solution analyses. In. The Oxford handbook of dialectical behaviour therapy (pp. 259–282). Oxford University Press. |
24 | Levack, W. M. , Boland, P. , Taylor, W. J. , Siegert, R. J. , Kayes, N. M. , Fadyl, J. K. , & McPherson, K. M. ((2014) ). Establishing a person-centred framework of self-identity after traumatic brain injury: A grounded theory study to inform measure development, 4: (5), e004630. https://doi.org/10.1136/bmjopen-2013-004630 |
25 | Linehan, M. ((2015) ). DBT skills training handouts and worksheets (Second edition). The Guilford Press. |
26 | Linehan, M. M. ((1993) ). Cognitive-behavioral treatment of borderline personality disorder (pp. xvii, 558). Guilford Press. |
27 | Linehan, M. M. ((2015) ). DBT® skills training manual, 2nd ed (pp. xxiv, 504). Guilford Press. |
28 | Linehan, M. M. ((2017) ). Manuel d’entraînement aux compétences TCD (2e éd., traduit par Prada P., Nicastro R., Perroud N.). Médecine et hygiène. |
29 | Linehan, M. M. , Heard, H. L. , & Armstrong, H. E. ((1993) ). Naturalistic follow-up of a behavioral treatment for chronically parasuicidal borderline patients. Archives of General Psychiatry, 50: , 971–974. https://doi.org/10.1001/archpsyc.1993.01820240055007 |
30 | Lynch, T. R. , & Cheavens, J. ((2007) ). Dialectical Behavior Therapy for Depression with Comorbid Personality Disorder: An Extension of Standard Dialectical Behavior Therapy with a Special Emphasis on the Treatment of Older Adults. In Dimeff L. A., Koerner K., & Linehan M. M. (Eds.), Dialectical Behavior Therapy in Clinical Practice: Applications across Disorders and Settings (1st edition). Guilford Press. |
31 | Lynch, T. R. , Trost, W. T. , Salsman, N. , & Linehan, M. M. ((2007) ). Dialectical Behavior Therapy for Borderline Personality Disorder. Annual Review of Clinical Psychology, 3: (1), 181–205. https://doi.org/10.1146/annurev.clinpsy.2.022305.095229 |
32 | Mak, M. , Moulaert, V. R. M. , Pijls, R. W. , & Verbunt, J. A. ((2016) ). Measuring outcome after cardiac arrest: Construct validity of Cerebral Performance Category. Resuscitation, 100: , 6–10. https://doi.org/10.1016/j.resuscitation.2015.12.005 |
33 | Neacsiu, A. D. , Eberle, J. W. , Kramer, R. , Wiesmann, T. , & Linehan, M. M. ((2014) ). Dialectical behavior therapy skills for transdiagnostic emotion dysregulation: A pilot randomized controlled trial. Behaviour Research and Therapy, 59: , 40–51. https://doi.org/10.1016/j.brat.2014.05.005 |
34 | Neumann, D. , Hammond, F. M. , Sander, A. M. , Bogner, J. , Bushnik, T. , Finn, J. A. , Chung, J. S. , Klyce, D. W. , Sevigny, M. , & Ketchum, J. M. ((2024) ). A Longitudinal Investigation of Alexithymia as a Predictor of Empathy, Emotional Functioning, Resilience, and Life Satisfaction Two Years after Brain Injury. Archives of Physical Medicine and Rehabilitation, S0003-9993(24)00950-X. https://doi.org/10.1016/j.apmr.2024.04.008 |
35 | Neumann, D. , Malec, J. F. , & Hammond, F. M. ((2017) ). Reductions in Alexithymia and Emotion Dysregulation After Training Emotional Self-Awareness Following Traumatic Brain Injury: A Phase I Trial. Journal of Head Trauma Rehabilitation, 32: (5), 286–295. https://doi.org/10.1097/HTR.0000000000000277 |
36 | Ownsworth, T. , & Gracey, F. ((2017) ). Cognitive behavioural therapy for people with brain injury. In Neuropsychological rehabilitation: The international handbook (pp. 313–326). Routledge/Taylor & Francis Group. |
37 | Ponsford, J. , & Schönberger, M. ((2010) ). Family functioning and emotional state two and five years after traumatic brain injury. Journal of the International Neuropsychological Society: JINS, 16: (2), 306–317. https://doi.org/10.1017/S1355617709991342 |
38 | QOLIBRI – Online home of QOLIBRI. (n.d.). Retrieved December 20, 2023, from https://qolibrinet.com/ |
39 | Rizvi, S. L. ((2019) ). The Basics of the Chain Analysis. In Chain Analysis in Dialectical Behavior Therapy (Guilford Publications). |
40 | Rizvi, S. L. , & Ritschel, L. A. ((2014) ). Mastering the Art of Chain Analysis in Dialectical Behavior Therapy. Cognitive and Behavioral Practice, 21: (3), 335–349. https://doi.org/10.1016/j.cbpra.2013.09.002 |
41 | Rizvi, S. L. , & Roman, K. M. ((2019) ). Generalization modalities: Taking the treatment out of the consulting room—Using telephone, text, and email. In. The Oxford handbook of dialectical behaviour therapy (pp. 201–215). Oxford University Press. |
42 | Sabaz, M. , Simpson, G. K. , Walker, A. J. , Rogers, J. M. , Gillis, I. , & Strettles, B. ((2014) ). Prevalence, comorbidities, and correlates of challenging behavior among community-dwelling adults with severe traumatic brain injury: A multicenter study. The Journal of Head Trauma Rehabilitation, 29: (2), E19–E30. https://doi.org/10.1097/HTR.0b013e31828dc590 |
43 | Sander, A. M. , Clark, A. N. , Arciniegas, D. B. , Tran, K. , Leon-Novelo, L. , Ngan, E. , Bogaards, J. , Sherer, M. , & Walser, R. ((2021) ). A randomized controlled trial of acceptance and commitment therapy for psychological distress among persons with traumatic brain injury. Neuropsychological Rehabilitation, 31: (7), 1105–1129. https://doi.org/10.1080/09602011.2020.1762670 |
44 | Sayrs, J. H. R. , & Linehan, M. M. ((2019) ). Modifying CBT to meet the challenge of treating emotion dysregulation. Utilizing Dialectics. In. The Oxford handbook of dialectical behaviour therapy (pp. 107–118). Oxford University Press. |
45 | Shields, C. , Ownsworth, T. , O’Donovan, A. , & Fleming, J. ((2016) ). A transdiagnostic investigation of emotional distress after traumatic brain injury. Neuropsychological Rehabilitation, 26: (3), 410–445. https://doi.org/10.1080/09602011.2015.1037772 |
46 | Stéfan, A. , & Mathé, J.-F. ((2016) ). What are the disruptive symptoms of behavioral disorders after traumatic brain injury? A systematic review leading to recommendations for good practices. Annals of Physical and Rehabilitation Medicine, 59: (1), 5–17. https://doi.org/10.1016/j.rehab.2015.11.002 |
47 | Tedeschi, R. G. , & Calhoun, L. G. ((2004) ). TARGET ARTICLE: “Posttraumatic Growth: Conceptual Foundations and Empirical Evidence.”. Psychological Inquiry, 15: (1), 1–18. https://doi.org/10.1207/s15327965pli1501_01 |
48 | Thoma, N. , Pilecki, B. , & McKay, D. ((2015) ). Contemporary Cognitive Behavior Therapy: A Review of Theory, History, and Evidence. Psychodynamic Psychiatry, 43: (3), 423–461. https://doi.org/10.1521/pdps.2015.43.3.423 |
49 | Tsaousides, T. , Spielman, L. , Kajankova, M. , Guetta, G. , Gordon, W. , & Dams-O’Connor, K. ((2017) ). Improving Emotion Regulation Following Web-Based Group Intervention for Individuals With Traumatic Brain Injury. The Journal of Head Trauma Rehabilitation, 32: (5), 354–365. https://doi.org/10.1097/HTR.0000000000000345 |
50 | von Steinbüchel, N. , Wilson, L. , Gibbons, H. , Hawthorne, G. , Höfer, S. , Schmidt, S. , Bullinger, M. , Maas, A. , Neugebauer, E. , Powell, J. , von Wild, K. , Zitnay, G. , Bakx, W. , Christensen, A.-L. , Koskinen, S. , Sarajuuri, J. , Formisano, R. , Sasse, N. , Truelle, J.-L. , & QOLIBRI Task Force. ((2010) ). Quality of Life after Brain Injury (QOLIBRI): Scale development and metric properties. Journal of Neurotrauma, 27: (7), Article 7. https://doi.org/10.1089/neu.2009.1076 |
51 | Weiner, L. ((2019) ). Évaluation de la faisabilité et de l’efficacité d’un groupe de thérapie comportementale dialectique (TCD) transnosographique: Le groupe de régulation EMOtionnelle (GREMO). French Journal of Psychiatry, 1: , S24–S25. https://doi.org/10.1016/j.fjpsy.2019.10.208 |
52 | Weiner, L. , & Bemmouna, D. ((2019) ). Manuel et fiches de travail Groupe de Régulation Emotionnelle TCD. |
53 | Weis, C. N. , Webb, E. K. , deRoon-Cassini, T. A. , & Larson, C. L. ((2022) ). Emotion Dysregulation Following Trauma: Shared Neurocircuitry of Traumatic Brain Injury and Trauma-Related Psychiatric Disorders. Biological Psychiatry, 91: (5), 470–477. https://doi.org/10.1016/j.biopsych.2021.07.023 |
54 | Wiart, L. , Luauté, J. , Stefan, A. , Plantier, D. , & Hamonet, J. ((2016) ). Non pharmacological treatments for psychological and behavioural disorders following traumatic brain injury (TBI). A systematic literature review and expert opinion leading to recommendations. Annals of Physical and Rehabilitation Medicine, 59: (1), 31–41. https://doi.org/10.1016/j.rehab.2015.12.001 |
55 | Wong, G. K. C. , Lam, S. W. , Ngai, K. , Wong, A. , Mok, V. , & Poon, W. S. ((2014) ). Quality of Life after Brain Injury (QOLIBRI) Overall Scale for patients after aneurysmal subarachnoid hemorrhage. Journal of Clinical Neuroscience, 21: (6), 954–956. https://doi.org/10.1016/j.jocn.2013.09.010 |




