Combining HD-tDCS with music stimulation for patients with prolonged disorders of consciousness: Study protocol for an RCT trial
Abstract
BACKGROUND:
Patients with prolonged disorders of consciousness (pDOC) pose significant challenges to healthcare workers due to their severe motor impairments and limited interaction with the environment. Non-invasive brain stimulation such as high-definition transcranial direct current stimulation (HD-tDCS) and music stimulation show promise in awakening this population.
OBJECTIVE:
In this study, we present a protocol aiming at investigating the efficacy of combined HD-tDCS and music stimulation in awakening patients with pDOC through a single-blind, randomized controlled trial.
METHODS:
Ninety patients with pDOC will be randomly divided into three groups: active HD-tDCS with music stimulation, active HD-tDCS, and sham HD-tDCS. All participants will receive 20 treatment sessions over a period of 10 days and the Coma Recovery Scale-Revised, Glasgow Outcome Scale and electroencephalogram will be used as assessment measures to evaluate their level of consciousness throughout the study. Adverse events and complications will be recorded during treatment. Within-group pre-post comparisons and between-group efficacy comparisons will be conducted to identify the most effective intervention approach. Statistical analysis will be performed using SPSS software with a significance level set at P < 0.05.
CONCLUSION:
The pursuit of awakening therapy for patients with pDOC remains a clinical research challenge. This study protocol is designed with the aim of introducing an innovative non-pharmacological approach which combined HD-tDCS and music stimulation to facilitate the reinstatement of consciousness in patients with pDOC.
1Introduction
Disorders of consciousness (DOC) pose significant challenges in providing targeted therapeutic interventions and implementing effective rehabilitation strategies (Eapen et al., 2017). Patients with DOC often have severe motor impairments and limited communication abilities, making the management of their condition particularly difficult (Lin et al., 2015). Prolonged disorders of consciousness (pDOC) refer to impaired consciousness lasting for more than 28 days (Li et al., 2023). Current treatment options for pDOC are limited (Giacino et al., 2018), and there is a need for effective interventions that can improve arousal without relying on active patient participation (Thibaut et al., 2019).
High-definition transcranial direct current stimulation (HD-tDCS) offers an effective non-invasive therapeutic option for patients with pDOC (Chen et al., 2022; Han et al., 2022a). By modulating the cerebral cortex’s membrane potential through the application of direct current, HD-tDCS can influence subthreshold neuronal activity and modulates neural functional connectivity (Zhang et al., 2020). Studies have demonstrated that HD-tDCS, particularly when applied to the prefrontal cortex, can enhance neural network activity and increase functional connectivity in patients with pDOC (Guo et al., 2019). Additionally, repetitive HD-tDCS of the left dorsolateral prefrontal cortex has shown promise in increasing Electroencephalogram (EEG) slow wave power and improving arousal in patients with Minimally Conscious State (MCS) (Wu et al., 2019).
Music stimulation, as a sound stimulus with personal meaning and emotional potency, has shown potential for improving mood and increasing arousal in patients with pDOC (Castro et al., 2015). The unique properties of music, such as its psychological engagement and rhythmic entrainment, make it a compelling candidate for facilitating cognitive and motor recovery in individuals with pDOC (Zuo et al., 2021). Music stimulation has been found to increase neurological activity and activate the reward system, thereby modulating cognitive-emotional responses (Kotchoubey et al., 2015). It has also been shown to enhance the functional activity of brain networks related to internal self-referential awareness and external awareness, positively impacting the patient’s state of consciousness (Carriere et al., 2020).
Accumulating evidence indicates that music has a complementary role in enhancing the therapeutic impact of HD-tDCS, specifically in areas such as working memory, pseudo neglect, and response inhibition, resulting in improved cognitive outcomes (Picazio et al., 2015; Mansouri et al., 2017; Chow et al., 2021). Despite the increasing amount of research on HD-tDCS and music-based interventions, their combined use in the treatment of pDOC has not been thoroughly investigated.
EEG serves as a valuable tool for assessing the effects of HD-tDCS and music stimulation on patients with pDOC. For instance, following HD-tDCS administration, changes can be observed in spectral power, functional connectivity, and event-related potentials by analyzing EEG signals (Cavinato et al., 2019). Musical stimulation has also been shown to increase the amplitude of the EEG mismatch negativity (MMN) wave in patients with pDOC (Hu et al., 2021). EEG enables the examination of neurophysiological changes induced by therapeutic interventions, providing objective measures and insights into their mechanisms of action (Modolo et al., 2020).
This study protocol aims to explore the effects and mechanisms of a combined intervention involving HD-tDCS and music for patients with pDOC. Coma Recovery Scale-Revised (CRS-R) (Fan et al., 2022), Glasgow Outcome Scale (GOS) (Sun et al., 2023), and EEG (He et al., 2018) are selected as outcome measures to comprehensively evaluate changes in the consciousness state of patients with pDOC before and after treatment. The findings of this study can provide valuable insights into the development of innovative rehabilitation strategies for this challenging population.
2Materials and methods
2.1Design
This is a prospective, single-blind, randomized controlled study. The study protocol was approved by the local Ethic Committee (20220920002-FS01) and registered on https://www.chictr.org.cn (ChiCTR2300071688).
2.2Participants
Participants will be recruited from patients who suffer from pDOC admitted in the inpatient department of local rehabilitation center. After reviewing the medical records for potential subjects, the project leader will engage in communication with the patient’s family members to obtain their informed consent. Demographic and clinical information will be obtained from patient’s medical record. Patients or the public were not involved in the design, or conduct, or reporting, or dissemination plans of our research.
2.3Inclusion and exclusion criteria
The inclusion criteria are as follows: (1) Diagnosis of Vegetative State/Unresponsive Wakefulness Syndrome (VS/UWS) or MCS based on the score obtained from CRS-R (Giacino et al., 2002; Estraneo et al., 2015; Zhang et al., 2019); (2) Age between 18 and 75 years; (3) Onset of the DOC for a minimum duration of 28 days; (4) Absence of hearing impairment, with mid-latency auditory evoked potentials within normal range or slightly delayed, and the presence of primary somatosensory cortical potentials (N20) observed through somatosensory evoked potentials elicited by median nerve stimulation (Ribeiro et al., 2014); (5) No history of tDCS treatment three months prior the study.
The exclusion criteria are as follows: (1) Presence of pacemakers, aneurysm clips, neurostimulators, or metal brain implants, in accordance with safety standards for transcranial electrical stimulation in humans (Thair et al., 2017); (2) Neuroimaging evidence of focal lesions in the left dorsolateral prefrontal cortex (DLPFC); (3) Presence of severe medical conditions that may influence clinical diagnosis and EEG assessments, such as severe cardiopulmonary, renal, or liver diseases (Hirsch, 2011); (4) History of epilepsy, psychiatric disorders, or neurodegenerative diseases.
2.4Sample size
Sample size estimation was conducted using G*Power software. The effect size value was calculated based on previous similar studies (Han et al., 2022b), with f = 0.47, α= 0.05, and power (1-β) = 0.95. Considering a potential participant attrition rate of 20%, the total sample size was determined to be 90 cases. This sample size calculation ensures that the study will have sufficient statistical power to produce reliable and robust results.
2.5Randomization and blinding
In this study, a block randomization method will be used, and patients will be divided into the VS/UWS category and the MCS category according to the classification of pDOC. Then, utilizing the random sequence generated by the “plan” function in SPSS 21.0 (IBM Corp., Armonk, NY, USA), participants in each category will be randomly allocated to three groups: Group I, receiving active HD-tDCS combined with music stimulation; Group II, receiving active HD-tDCS; and Group III, receiving sham HD-tDCS in a 1:1:1 ratio to ensure balanced distribution of two categories.
The randomization process will be performed by an independent statistician who is not involved in the experiment. The random allocation sequence will be concealed from the participants, their caregivers, nursing staff, treating clinicians, evaluators, and statisticians. The sham stimulation mode of HD-tDCS devices ensures that subjects are blinded to the treatment they are receiving.
2.6Intervention
2.6.1HD-tDCS
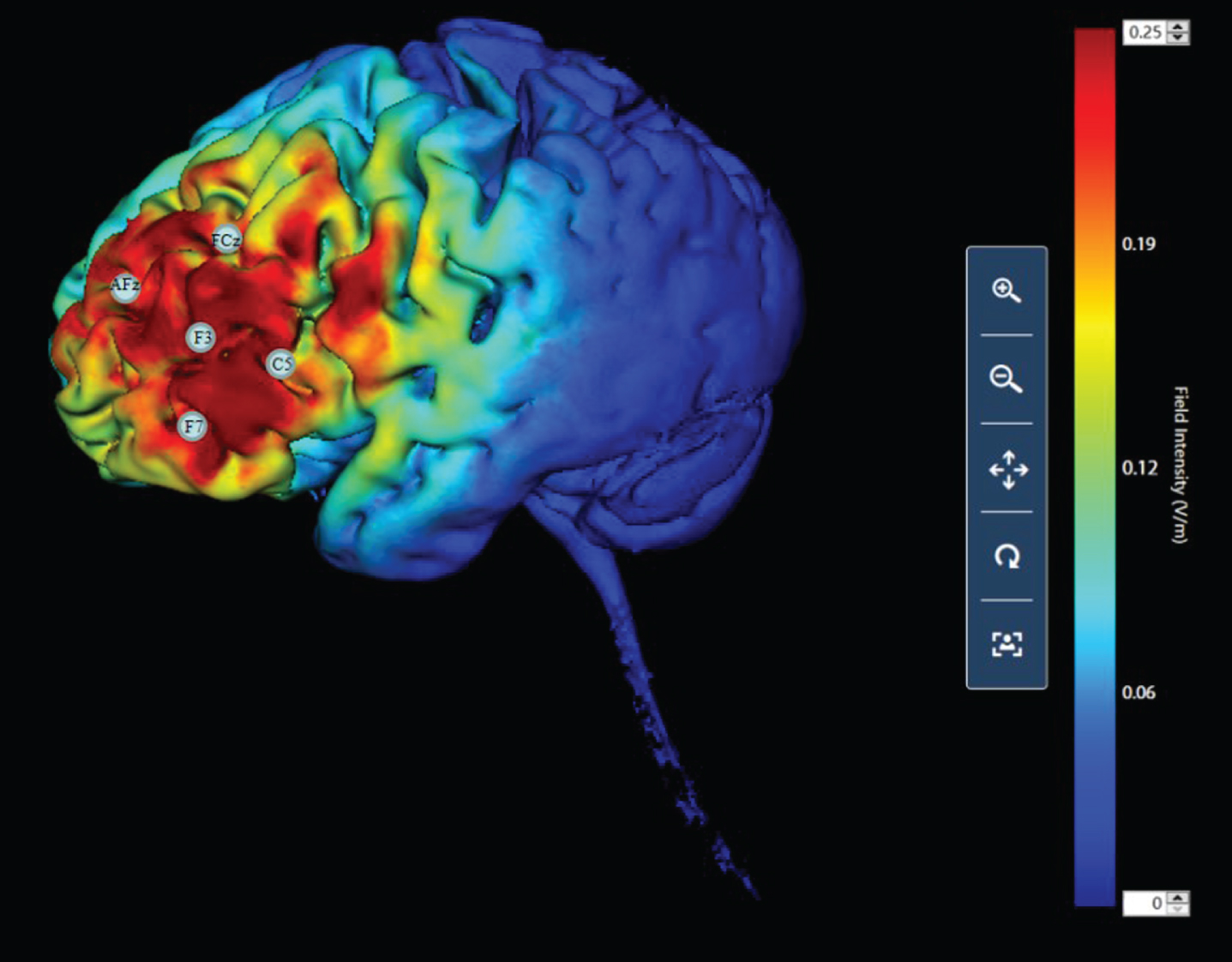
In this study, HD-tDCS will be administered using a 4×1 high-definition constant current stimulator manufactured by Soterix. Five high-definition electrodes will be used to deliver direct current to the brain. These electrodes include one central anode electrode and four cathode electrodes placed around the target brain region. According to International 10–20 system, the anode will be positioned over the left dorsolateral prefrontal cortex (DLPFC) area (F3), and the four cathode electrodes will be placed approximately 3.5 cm away from the F3 location, approximately at AFz, FCz, F7, and C5 positions (Fig. 1) (Han et al., 2022a).
Fig. 1
HD-tDCS montage. F3 denotes the anodal electrode, while AFz, FCz, F7, and C5 denote cathodal electrodes. The selected montage induces an electric field distribution within the cortical gray matter.
During the active HD-tDCS stimulation phase, the current will gradually increase from 0 mA to 2 mA over a period of 30 seconds, remain constant for 20 minutes, and then decrease back to 0 mA over 30 seconds. While during the sham HD-tDCS stimulation phase, the current will increase gradually to 2 mA over a 30-second window and then drop backdown to 0 mA within 30 seconds. The current will be maintained at this level for 20 minutes during the sham stimulation phase until the stimulation period ends (Han et al., 2022b).
2.6.2Music stimulation
The selection of music stimuli is informed by previous research (Binzer et al., 2016), opting for familiar music that has demonstrated therapeutic efficacy in patients with DOC. The following music compositions have been selected: (1) “Spring Festival Overture” composed by Chinese composer Huanzhi Li (Hu et al., 2021), (2) “The Sun Rises as Usual” by Japanese composer Joe Hisaishi; (3) “Summer” by Japanese composer Joe Hisaishi; (4) “Four Seasons in Beijing-Colorful Butterflies Dance Summer” by Chinese composer Zhenzhen He; (5) “New Ambush on All Sides” by Chinese composer Cong Zhao; (6) “Summer in Satoyama” by Japanese composer Masaaki Kishibe. These six pieces of music are well-known to the Chinese audience and are instrumental compositions with rich emotional connotations. Previous studies have demonstrated their awakening effects in patients with DOC (Hu et al., 2021; Zhang et al., 2021).
A playlist will be created with the selected music compositions. The order of the music will be randomized to eliminate sequence effects, managed by a music player. After each piece of music ends, the next one will be played immediately, and fade-in and fade-out techniques will be used to ensure smooth transitions between music tracks. The group receiving music stimulation will listen to the music twice a day, with each session lasting 20 minutes without interruptions. The volume will be controlled between 40–70 dB. Noise-canceling headphones will be used to eliminate environmental noise interference and enhance the effect of familiar music stimuli for the patients (Lizette et al., 2021).
2.6.3Conventional treatments
Participants in all three groups will receive standard treatments, including medical treatment (medication, nutritional support and prevention of complications) and rehabilitation therapy (physiotherapy, occupational therapy and speech therapy).
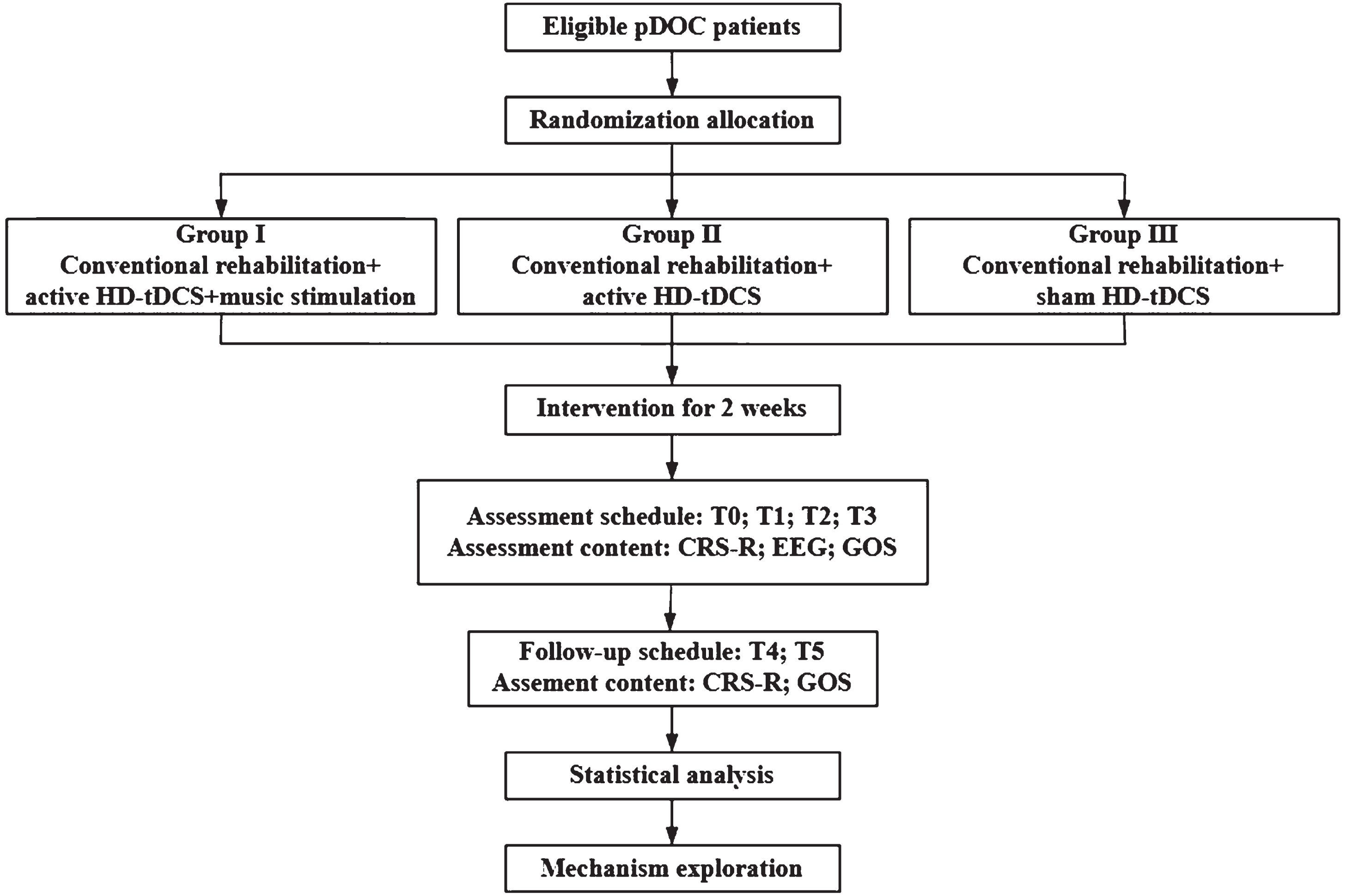
2.7Procedure
Participants in each group will undergo 20 treatment sessions, each lasting 20 minutes (Han et al., 2022b). There will be two sessions per day over a period of two weeks, with a two-day interval between each week. The initial session will be conducted in a dedicated room equipped with EEG. Participants will be positioned in a supine posture and fitted with a standardized EEG cap with 64 electrodes by treating clinicians. Five HD-tDCS electrodes are attached to EEG cap and noise-canceling headphones will be placed on participants. After first EEG is taken, all participants will receive the initial session. In group I, both HD-tDCS and music stimulation will be administrated simultaneously to patients for 20 mins while in group II, only HD-tDCS will be administrated. As for participants in group III, they will receive sham HD-tDCS for 20 mins. Subsequent sessions will then take place in the participant’s bedside. EEG recording will be conducted before and immediately after the initial and the final sessions for all participants. The study procedure is shown in Fig. 2.
Fig. 2
Study design. This schematic illustrates the study design, encompassing the chronological sequence of events, participant logistics, and the timing of assessments at various time points including baseline, pre- and post-intervention, post-test, and follow-up. T0: before the first session; T1: after the first session; T2: after ten sessions; T3: after twenty sessions; T4: one week after the end of the twenty sessions; T5: three months after the end of the twenty sessions. Abbreviations: prolonged disorders of consciousness (pDOC); Coma Recovery Scale-Revised (CRS-R); high-definition transcranial direct current stimulation (HD-tDCS); Glasgow Outcome Scale (GOS); Electroencephalogram (EEG).
2.8Outcome measures
2.8.1Primary outcome
CRS-R will be utilized to assess patient’s level of consciousness (Zhang et al., 2019). This scale encompasses six subcategories: auditory, visual, motor, verbal, communication, and arousal, with a scoring range of 0 to 23. Scores are assigned based on patient’s behavioral responses to specific sensory stimuli. This scale enables differentiation between patients in VS/UWS, patients in MCS, and those who have emerged from MCS. Higher scores indicate a lesser degree of consciousness impairment.
2.8.2Secondary outcomes
GOS will be employed to assess patient outcomes. This scale encompasses five levels, ranging from 1 to 5. Level 1 represents death, level 2 indicates a vegetative state or a prolonged coma with the possibility of sucking, eye opening, and partial localized movements (McMillan et al., 2016). Level 3 represents severe disability, where the patient is conscious but experiences cognitive or physical impairments requiring 24-hour care. Level 4 represents moderate disability, where the patient is capable of self-care but exhibits mild hemiparesis, swallowing difficulties, or similar symptoms. Level 5 represents a good recovery, where the patient can engage in social and occupational activities (McMillan et al., 2013).
EEG recordings will be performed using a 64-channel EEG recorder for data acquisition, recording, and preprocessing. The study will primarily capture amplitude and power values of five slow wave frequency bands (Wu et al., 2019), latency and amplitude of mismatch negative waves. The selected frequency bands of interest are delta (1–4 Hz), theta (4–8 Hz), alpha (8–12 Hz), beta1 (12–18 Hz), and beta2 (18–30 Hz) (Han et al., 2022a). EEG data will be collected for each patient, with scalp electrodes placed according to the International 10–20 system (Acharya & Acharya, 2019). A reference electrode will be positioned above the right mastoid, and a ground electrode above the left earlobe. Skin impedance will be maintained below 5kΩ, and recordings will be sampled at a rate of 1000 Hz, with each EEG session lasting approximately 12 minutes.
Offline analysis will be conducted using BrainVision Analyzer 2.1. High-pass and low-pass band-pass filtering will be applied using a 0.1–30 Hz range. Independent Component Analysis (ICA) utilizing classic sphericalization and infomax algorithms will be employed to remove artifacts such as eye blinks (Urigüen & Garcia-Zapirain, 2015). Fast Fourier Transform (FFT) will be used to generate spectra or amplitudes as a function of frequency for each electrode. Furthermore, brain power within different frequency bands will be estimated, obtaining absolute power in the five frequency bands for all electrodes. Relative power will then be calculated based on absolute power to measure the post-effects of HD-tDCS combined with music stimulation across the five frequency bands.
Additionally, patient’s MMN will be measured by providing auditory stimulation during EEG data acquisition using the Oddball paradigm (Hu et al., 2021). Regular high-probability low-tone stimuli will be presented to the patient via headphones with an occurrence rate of 85% and intensity of 60 dB. Deviant high-tone stimuli (deviation stimuli) will be randomly introduced among the regular low-tone stimuli, occurring at a rate of 15% and intensity of 80 dB. The deviant stimuli will be presented 40 times in total. Waveform elicited by standard and deviant stimuli will be recorded separately and subtracted to obtain the first prominent negative wave, which represents the MMN. The presence or absence of MMN and its latency will be observed.
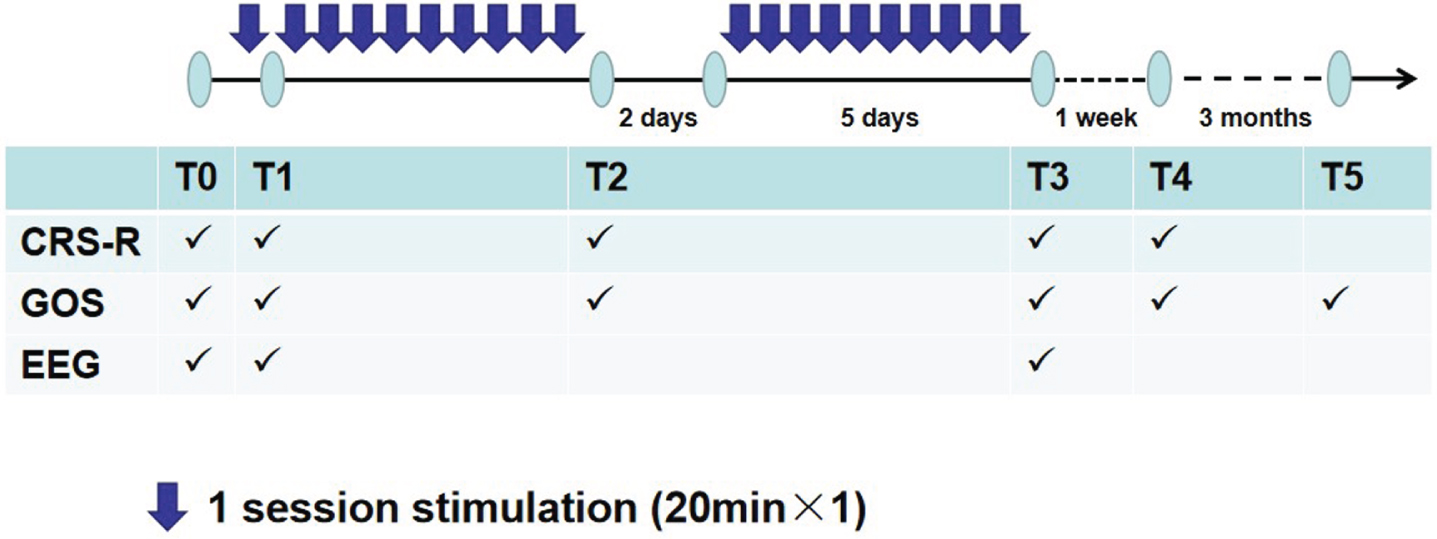
2.9Data collection and management
Behavioral assessments, including GOS and CRS-R, will be conducted before and after the first treatment session, immediately after the ten treatment sessions, after the final session, and one week following the final session. EEG examinations will be performed prior and post the first and final sessions (Fig. 3). Additionally, three months after the final session, a follow-up evaluation using the GOS will be conducted to assess patient’s outcomes. Adverse reactions and events occurring during the treatment process will be recorded and evaluated.
Fig. 3
Outline of the experimental design. T0: before the first session; T1: after the first session; T2: after ten sessions; T3: after twenty sessions; T4: one week after the twenty sessions; T5: three months after the end of the twenty sessions.
2.10Statistics methods
Statistical analysis will be performed using SPSS 21.0 software. The CRS-R score, relative power, and MMN latency will be presented as mean±standard deviation (x±s) for continuous variables, and comparisons among groups will be conducted using t-tests or Mann-Whitney U tests. The GOS score will be compared using Pearson’s chi-square test or Fisher’s exact test. Paired sample t-tests will be used for within-group comparisons before and after treatment. A one-way analysis of variance (ANOVA) followed by post hoc Tukey’s test will be used for continuous variables among the three groups. Similarly, the Wilcoxon signed-rank test will be applied for ordinal data within-group comparisons before and after treatment, and the Kruskal-Wallis rank-sum test will be used to compare ordinal data among the three groups. Statistical significance will be set at P < 0.05.
3Discussion
The objective of this study is to investigate the combined application of HD-tDCS and music stimulation as a novel therapeutic approach to improve the consciousness level of patients with pDOC. Previous research has demonstrated that both HD-tDCS and music stimulation are effective forms of non-invasive brain stimulation (Hu et al., 2021; Zhang et al., 2021; Han et al., 2022a; Yuan et al., 2022). Our study aims to investigate whether the combined application can further enhance the treatment efficacy. We hypothesize that patients in the active HD-tDCS group will show improvements in behavioral and electrophysiological assessments, while those receiving the combined intervention of HD-tDCS and music stimulation are expected to exhibit even more notable improvements, which are observable after the first and final treatment sessions, as indicated by EEG analysis. Additionally, we expect that these improvements persist in one-week and three-month follow-up.
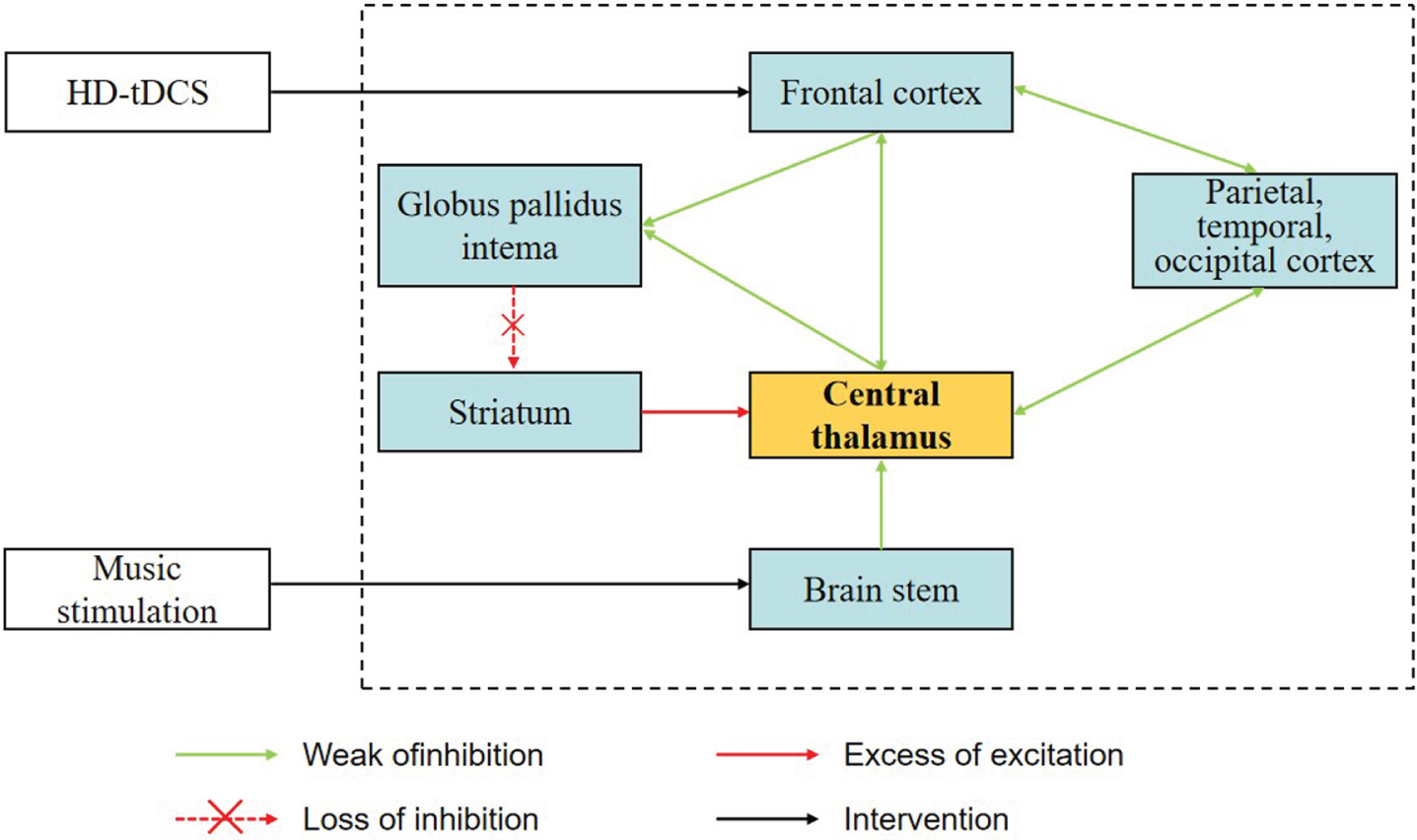
The underlying mechanisms of our experimental design revolve around the concurrent modulation of the central thalamus achieved through the synergistic influence of HD-tDCS and music stimulation (Fig. 4). HD-tDCS, when applied to the prefrontal cortex, directly modulates thalamic activity, potentially influencing consciousness regulation (Thibaut et al., 2015). It may also facilitate the re-establishment of inhibitory control of the globus pallidus over the central thalamus when it is applied to the prefrontal cortex to impact the activity of the striatum (Fridman et al., 2014; Fridman & Schiff, 2014). Music stimulation, on the other hand, targets the central thalamus through an alternative route via the brainstem reticular activating system (Xiao et al., 2023). This complementary mechanism further contributes to the intricate central-peripheral combined stimulation paradigm. The enhancement of central thalamic function, through the orchestrated impact of these distinct modalities, emerges as a pivotal pathway for the elevation of consciousness states (Van der Werf et al., 2002; Fins & Bernat, 2018).
Fig. 4
Mesocircuit fronto-parietal model. This mesocircuit model potentially explains the mechanisms of HD-tDCS and music stimulation, which have demonstrated promising results in the recovery of consciousness among patients with prolonged disorders of consciousness (pDOC). The black dotted box shows the neural mechanisms of impaired consciousness. After brain injury, a reduction in central thalamic neurons leads to diminished outputs in the corticothalamic and thalamo-striatal pathways (green lines). Consequently, the inhibitory effect of the striatum on the pallidum interna weakens (dashed red line), allowing the pallidum interna neurons to exhibit tonic firing and exert active inhibition (red line) on their synaptic targets, including the relay neurons in the already significantly impaired central thalamus(Fridman et al., 2014; Fridman and Schiff, 2014). This sequence of events may contribute to the consciousness disorders. Adapted from Giacino and colleagues(Fins and Bernat, 2018).
Addressing the challenges associated with devising this protocol and providing relevant solutions is of great importance. In the initial planning phase of the study protocol, the EEG cap and HD-tDCS cap applied to participant’s head were two independent equipment that needed to be swapped in between EEG measurement and HD-tDCS treatment in the first and last treatment sessions. The conductive gel applied on the electrodes of two caps introduced a risk of EEG signal channel concatenation during the swapping process. A novel electrostimulation electronode used for HD-tDCS treatment was designed and it can be attached to the EEG cap. This advancement allows for the use of a single EEG cap, eliminating the need for cap swapping and associated signal interference risks.
Furthermore, the severe interaction impairment of patients with pDOC poses difficulty in accurately quantifying therapeutic effects as they have limited respond to behavioral assessment. Therefore, electrophysiological method was introduced in our study and a 64-channel EEG system was used to measure neurophysiological responses. Additionally, the measurement of EEG activity relies patients to maintain still and minimize body movements, especially head and ocular movements. However, individuals with consciousness disorders lack the ability to actively collaborate with experimental protocols. Especially for those with MCS, they exhibit restlessness and agitation which may interference the EEG recording. To address this, semiautomatic ICA techniques are employed to effectively eliminate EEG artifacts and enhance signal quality.
This study possesses several strengths. It represents the first investigation into the effects of combined HD-tDCS and music stimulation on consciousness levels in patients with pDOC, thus offering innovative insights. In addition, the research team consulted experts from multiple disciplines, including music therapist, neuroscientist, and EEG analyst, ensuring a comprehensive analysis of the study. Furthermore, HD-tDCS is utilized in our study. Compared to conventional tDCS techniques, it provides improved targeting precision and deeper penetration, allowing in a more focused therapeutic effect.
Previous studies, such as the one conducted by Hu et al., have demonstrated the enhancement of the MMN component in the electroencephalogram and improvement in the CRS-R scores of patients with pDOC due to music-only stimulation (Hu et al., 2021). Additionally, Wang et al.’s study showed that a 14-day HD-tDCS intervention over the precuneus anode significantly improved CRS-R scores and MMN amplitudes in DOC patients (Wang et al., 2020). While substantial research has been conducted on HD-tDCS intervention, the precise impact of this intervention, with a specific focus on the DLPFC, on the MMN component in patients with pDOC remains unexplored. Our study aims to simultaneously address this research gap and investigate the potential combined effects of combining HD-tDCS intervention, specifically targeting the DLPFC, with music stimulation on both the CRS-R scores and MMN in patients with pDOC. While recognizing that the inclusion of a music-only stimulation group could have enhanced the comprehensiveness of our study, we made the decision to forego this option due to anticipated challenges associated with expanding the sample size, potential pressures on research personnel, and time constraints. It is important to acknowledge that this decision represents a limitation in our current research design. Future research endeavors may consider the inclusion of a music-only stimulation group to further explore the distinct contributions of each intervention method.
4Conclusion
The pursuit of awakening therapy for patients with pDOC remains a clinical research challenge. This study protocol is designed with the aim of introducing an innovative non-pharmacological approach which combined HD-tDCS and music stimulation to facilitate the reinstatement of consciousness in patients with pDOC. The results of this research will make a valuable contribution to advancing evidence-based therapeutic approaches. This protocol is also anticipated to offer valuable insights for the design and implementation of future multi-center randomized controlled trials.
Acknowledgments
We would like to express our sincere gratitude to Ms. Zhihui Hu for her professional language editing and proofreading assistance throughout the preparation of this manuscript.
Conflict of interest
The authors declare no competing interests.
Funding
This study was supported by Shenzhen Science and Technology Innovation Program (No. JCYJ20220530151018039), the Sanming Project of Medicine in Shenzhen (No. SZSM202111010), Shenzhen Science and Technology Innovation Program (No. JCYJ20210324103409023), and a project supported by Hainan Province Clinical Medical Center (No. 0202067).
Ethics statement
This study was registered at the Chinese Clinical Trial Registry (ID: ChiCTR2300071688). The research protocol was approved by the Ethical Committee of Shenzhen Second People’s Hospital, China (ID: 20220920002-FS01) and designed following the principles of the Declaration of Helsinki. Informed consent will be obtained from all study participants.
References
1 | Acharya, J. N. , Acharya, V. J. ((2019) ). Overview of EEG Montages and Principles of Localization. Journal of Clinical Neurophysiology: Official Publication of the American Electroencephalographic Society, 36: , 325–329. |
2 | Binzer, I. , Schmidt, H. U. , Timmermann, T. , Jochheim, M. , Bender, A. ((2016) ). Immediate responses to individual dialogic music therapy in patients in low awareness states. Brain Injury, 30: , 919–925. |
3 | Carriere, M. , Larroque, S. K. , Martial, C. , Bahri, M. A. , Aubinet, C. , Perrin, F. , Laureys, S. , Heine, L. ((2020) ). An echo of consciousness: Brain function during preferred music. Brain Connect, 10: , 385–395. |
4 | Castro, M. , Tillmann, B. , Luauté, J. , Corneyllie, A. , Dailler, F. , André-Obadia, N. , Perrin, F. ((2015) ). Boosting cognition with music in patients With disorders of consciousness. Neurorehabilitation and Neural Repair, 29: , 734–742. |
5 | Cavinato, M. , Genna, C. , Formaggio, E. , Gregorio, C. , Storti, S. F. , Manganotti, P. , Casanova, E. , Piperno, R. , Piccione, F. ((2019) ). Behavioural and electrophysiological effects of tDCS to prefrontal cortex in patients with disorders of consciousness. Clinical Neurophysiology: Official Journal of the International Federation of Clinical Neurophysiology, 130: , 231–238. |
6 | Chen, C. , Han, J. , Zheng, S. , Zhang, X. , Sun, H. , Zhou, T. , Hu, S. , Yan, X. , Wang, C. , Wang, K. , Hu, Y. (2022). Dynamic changes of brain activity in different responsive groups of patients with prolonged disorders of consciousness. Brain Sciences, 13. |
7 | Chow, R. , Noly-Gandon, A. , Moussard, A. , Ryan, J. D. , Alain, C. ((2021) ). Effects of transcranial direct current stimulation combined with listening to preferred music on memory in older adults. Scientific Reports, 11: , 12638. |
8 | Eapen, B. C. , Georgekutty, J. , Subbarao, B. , Bavishi, S. , Cifu, D. X. ((2017) ). Disorders of consciousness. Physical Medicine and Rehabilitation Clinics of North America, 28: , 245–258. |
9 | Estraneo, A. , Moretta, P. , De Tanti, A. , Gatta, G. , Giacino, J. T. , Trojano, L. , Italian Crs, R. M. V. G. ((2015) ). An Italian multicentre validation study of the coma recovery scale-revised. Eur J Phys Rehabil Med, 51: , 627–634. |
10 | Fan, J. , Zhong, Y. , Wang, H. , Aierken, N. , He, R. ((2022) ). Repetitive transcranial magnetic stimulation improves consciousness in some patients with disorders of consciousness. Clin Rehabil, 36: , 916–925. |
11 | Fins, J. J. , Bernat, J. L. ((2018) ). Ethical, palliative, and policy considerations in disorders of consciousness. Archives of Physical Medicine and Rehabilitation, 99: , 1927–1931. |
12 | Fridman, E. A. , Beattie, B. J. , Broft, A. , Laureys, S. , Schiff, N. D. ((2014) ). Regional cerebral metabolic patterns demonstrate the role of anterior forebrain mesocircuit dysfunction in the severely injured brain. Proceedings of the National Academy of Sciences of the United States of America, 111: , 6473–6478. |
13 | Fridman, E. A. , Schiff, N. D. ((2014) ). Neuromodulation of the conscious state following severe brain injuries. Current Opinion in Neurobiology, 29: , 172–177. |
14 | Giacino, J. T. , Ashwal, S. , Childs, N. , Cranford, R. , Jennett, B. , Katz, D. I. , Kelly, J. P. , Rosenberg, J. H. , Whyte, J. , Zafonte, R. D. , Zasler, N. D. ((2002) ). The minimally conscious state: definition and diagnostic criteria. Neurology, 58: , 349–353. |
15 | Giacino, J. T. , Katz, D. I. , Schiff, N. D. , Whyte, J. , Ashman, E. J. , Ashwal, S. , Barbano, R. , Hammond, F. M. , Laureys, S. , Ling, G. S. F. , Nakase-Richardson, R. , Seel, R. T. , Yablon, S. , Getchius, T. S. D. , Gronseth, G. S. , Armstrong, M. J. ((2018) ). Practice guideline update recommendations summary: Disorders of consciousness: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology; the American Congress of Rehabilitation Medicine; and the National Institute on Disability, Independent Living, and Rehabilitation Research. Neurology, 91: , 450–460. |
16 | Guo, Y. , Bai, Y. , Xia, X. , Li, J. , Wang, X. , Dai, Y. , Dang, Y. , He, J. , Liu, C. , Zhang, H. ((2019) ). Effects of long-lasting high-definition transcranial direct current stimulation in chronic disorders of consciousness: A pilot study. Frontiers in Neuroscience, 13: , 412. |
17 | Han, J. , Chen, C. , Zheng, S. , Yan, X. , Wang, C. , Wang, K. , Hu, Y. ((2022) a). . High-definition transcranial direct current stimulation of the dorsolateral prefrontal cortex modulates the electroencephalography rhythmic activity of parietal occipital lobe in patients with chronic disorders of consciousness. Frontiers in Human Neuroscience, 16: , 889023. |
18 | Han, J. , Chen, C. , Zheng, S. , Zhou, T. , Hu, S. , Yan, X. , Wang, C. , Wang, K. , Hu, Y. (2022b). Functional connectivity increases in response to high-definition transcranial direct current stimulation in patients with chronic disorder of consciousness. Brain Sciences, 12. |
19 | He, F. , Wu, M. , Meng, F. , Hu, Y. , Gao, J. , Chen, Z. , Bao, W. , Liu, K. , Luo, B. , Pan, G. ((2018) ). Effects of Hz Repetitive Transcranial Magnetic Stimulation on Disorders of Consciousness: A Resting-State Electroencephalography Study. Neural Plasticity, 2018: , 5036184. |
20 | Hirsch, L. J. ((2011) ). Classification of EEG patterns in patients with impaired consciousness. Epilepsia, 52: (Suppl 8), 21–24. |
21 | Hu, Y. , Yu, F. , Wang, C. , Yan, X. , Wang, K. ((2021) ). Can Music Influence Patients With Disorders of Consciousness? An Event-Related Potential Study. Frontiers in Neuroscience, 15: , 596636. |
22 | Kotchoubey, B. , Pavlov, Y. G. , Kleber, B. ((2015) ). Music in Research and Rehabilitation of Disorders of Consciousness: Psychological and Neurophysiological Foundations. Frontiers in Psychology, 6: , 1763. |
23 | Li, H. , Zhang, X. , Sun, X. , Dong, L. , Lu, H. , Yue, S. , Zhang, H. ((2023) ). Functional networks in prolonged disorders of consciousness. Frontiers in Neuroscience, 17: , 1113695. |
24 | Lin, C. M. , Lin, M. C. , Huang, S. J. , Chang, C. K. , Chao, D. P. , Lui, T. N. , Ma, H. I. , Liu, M. Y. , Chung, W. Y. , Shih, Y. H. , Tsai, S. H. , Chiou, H. Y. , Lin, M. R. , Jen, S. L. , Wei, L. , Wu, C. C. , Lin, E. Y. , Liao, K. H. , Chiang, Y. H. , Chiu, W. T. , Lin, J. W. ((2015) ). A prospective randomized study of brain tissue oxygen pressure-guided management in moderate and severe traumatic brain injury patients. BioMed Research International, 2015: , 529580. |
25 | Lizette, H. , Alexandra, C. , Florent, G. , Jacques, L. , Mathieu, L. , Fabien, P. (2021). Virtually spatialized sounds enhance auditory processing in healthy participants and patients with a disorder of consciousness. Scientific Reports, 11. |
26 | Mansouri, F. A. , Acevedo, N. , Illipparampil, R. , Fehring, D. J. , Fitzgerald, P. B. , Jaberzadeh, S. ((2017) ). Interactive effects of music and prefrontal cortex stimulation in modulating response inhibition. Scientific Reports, 7: , 18096. |
27 | McMillan, T. , Wilson, L. , Ponsford, J. , Levin, H. , Teasdale, G. , Bond, M. ((2016) ). The Glasgow Outcome Scale - 40 years of application and refinement. Nature reviews. Neurology, 12: , 477–485. |
28 | McMillan, T. M. , Weir, C. J. , Ireland, A. , Stewart, E. ((2013) ). The Glasgow Outcome at Discharge Scale: an inpatient assessment of disability after brain injury. Journal of Neurotrauma, 30: , 970–974. |
29 | Modolo, J. , Hassan, M. , Wendling, F. , Benquet, P. ((2020) ). Decoding the circuitry of consciousness: From local microcircuits to brain-scale networks. Network Neuroscience (Cambridge, Mass.), 4: , 315–337. |
30 | Picazio, S. , Granata, C. , Caltagirone, C. , Petrosini, L. , Oliveri, M. ((2015) ). Shaping pseudoneglect with transcranial cerebellar direct current stimulation and music listening. Frontiers in Human Neuroscience, 9: , 158. |
31 | Ribeiro, A.S. , Ramos, A. , Bermejo, E. , Casero, M. , Corrales, J. M. , Grantham, S. ((2014) ). Effects of different musical stimuli in vital signs and facial expressions in patients with cerebral damage: a pilot study. The Journal of Neuroscience Nursing: Journal of the American Association of Neuroscience Nurses, 46: , 117–124. |
32 | Sun, W. , Liu, G. , Dong, X. , Yang, Y. , Yu, G. , Sun, X. , Feng, Z. , Ma, C. ((2023) ). Transcranial direct current stimulation improves some neurophysiological parameters but not clinical outcomes after severe traumatic brain injury. Journal of Integrative Neuroscience, 22: , 15. |
33 | Thair, H. , Holloway, A. L. , Newport, R. , Smith, A. D. ((2017) ). Transcranial direct current stimulation (tDCS): A beginner’s guide for design and implementation. Frontiers in Neuroscience, 11: , 641. |
34 | Thibaut, A. , Di Perri, C. , Chatelle, C. , Bruno, M. A. , Bahri, M. A. , Wannez, S. , Piarulli, A. , Bernard, C. , Martial, C. , Heine, L. , Hustinx, R. , Laureys, S. ((2015) ). Clinical Response to tDCS Depends on Residual Brain Metabolism and Grey Matter Integrity in Patients with Minimally Conscious State. Brain Stimulation, 8: , 1116–1123. |
35 | Thibaut, A. , Schiff, N. , Giacino, J. , Laureys, S. , Gosseries, O. ((2019) ). Therapeutic interventions in patients with prolonged disorders of consciousness. The Lancet. Neurology, 18: , 600–614. |
36 | Urigüen, J. A. , Garcia-Zapirain, B. ((2015) ). EEG artifact removal-state-of-the-art and guidelines. Journal of Neural Engineering, 12: , 031001. |
37 | Van der Werf, Y. D. , Witter, M. P. , Groenewegen, H. J. ((2002) ). The intralaminar and midline nuclei of the thalamus. Anatomical and functional evidence for participation in processes of arousal and awareness. Brain research. Brain Research Reviews, 39: , 107–140. |
38 | Wang, X. Y. , Guo, Y. K. , Zhang, Y. G. , Li, J. J. , Gao, Z. Q. , Li, Y. X. , Zhou, T. L. , Zhang, H. , He, J. H. , Cong, F. Y. ((2020) ). Combined Behavioral and Mismatch Negativity Evidence for the Effects of Long-Lasting High-Definition tDCS in Disorders of Consciousness: A Pilot Study. Frontiers in Neuroscience14. |
39 | Wu, M. , Yu, Y. , Luo, L. , Wu, Y. , Gao, J. , Ye, X. , Luo, B. ((2019) ). Efficiency of Repetitive Transcranial Direct Current Stimulation of the Dorsolateral Prefrontal Cortex in Disorders of Consciousness: A Randomized Sham-Controlled Study. Neural Plasticity, 2019: , 7089543. |
40 | Xiao, X. , Chen, W. , Zhang, X. ((2023) ). The effect and mechanisms of music therapy on the autonomic nervous system and brain networks of patients of minimal conscious states: a randomized controlled trial. Frontiers in Neuroscience, 17: , 1182181. |
41 | Yuan, P. , Jingpu, Z. , Xiao, L. , Juntao, D. , Shunxi, Z. , Jin, Z. , Huihua, L. , Xiuyuan, Z. , Xin, W. , Yue, L. , Tiebin, Y. ((2022) ). Efficacy of Transcranial Direct Current Stimulation Over Dorsolateral Prefrontal Cortex in Patients With Minimally Conscious State& #. Frontiers in Neurology13. |
42 | Zhang, R. , Zhang, L. , Guo, Y. , Shi, L. , Gao, J. , Wang, X. , Hu, Y. ((2020) ). Effects of High-Definition Transcranial Direct-Current Stimulation on Resting-State Functional Connectivity in Patients with Disorders of Consciousness. Frontiers in Human Neuroscience, 14: , 560586. |
43 | Zhang, X. Y. , Li, J. J. , Lu, H. T. , Teng, W. J. , Liu, S. H. ((2021) ). Positive effects of music therapist’s selected auditory stimulation on the autonomic nervous system of patients with disorder of consciousness: a randomized controlled trial. Neural Regeneration Research, 16: , 1266–1272. |
44 | Zhang, Y. , Wang, J. , Schnakers, C. , He, M. , Luo, H. , Cheng, L. , Wang, F. , Nie, Y. , Huang, W. , Hu, X. , Laureys, S. , Di, H. ((2019) ). Validation of the Chinese version of the Coma Recovery Scale-Revised (CRS-R. Brain Injury, 33: , 529–533. |
45 | Zuo, J. , Tao, Y. , Liu, M. , Feng, L. , Yang, Y. , Liao, L. ((2021) ). The effect of family-centered sensory and affective stimulation on comatose patients with traumatic brain injury: A systematic review and meta-analysis. Int J Nurs Stud, 115: , 103846. |




