Follow-up visits after a concussion in the pediatric population: An integrative review
Abstract
BACKGROUND:
Concussions are a significant health issue for children and youth. After a concussion diagnosis, follow-up visits with a health care provider are important for reassessment, continued management, and further education.
OBJECTIVE:
This review aimed to synthesize and analyse the current state of the literature on follow-up visits of children with a concussive injury and examine the factors associated with follow-up visits.
METHODS:
An integrative review was conducted based on Whittemore and Knafl’s framework. Databases searched included PubMed, MEDLINE, CINAHL, PsycINFO, and Google Scholar.
RESULTS:
Twenty-four articles were reviewed. We identified follow-up visit rates, timing to a first follow-up visit, and factors associated with follow-up visits as common themes. Follow-up visit rates ranged widely, from 13.2 to 99.5%, but time to the first follow-up visit was only reported in eight studies. Three types of factors were associated with attending a follow-up visit: injury-related factors, individual factors, and health service factors.
CONCLUSION:
Concussed children and youth have varying rates of follow-up care after an initial concussion diagnosis, with little known about the timing of this visit. Diverse factors are associated with the first follow-up visit. Further research on follow-up visits after a concussion in this population is warranted.
1Background
Concussions are a significant health issue for children and youth, with the potential for long-term consequences including depression and learning difficulties (Thomas et al., 2018). Recent statistics indicate that between 1.1 and 1.9 million concussions occur annually in children aged less than 18 years in the United States (Bryan et al., 2016). However, this number is likely an underestimation, as research suggests that concussions are underreported by those who are injured, leading not only to inaccurate estimations of annual incidence rates but also to a subsequent lack of care for those individuals (Langer et al., 2020; Seabury et al., 2018). Underreporting can delay the recovery of all concussed individuals and increase the likelihood of poor health outcomes, especially for children and youth who are not yet physically or developmentally mature (Levin &Diaz-Arrastia, 2015). However, even when concussions are reported and diagnosed, there may be a lack of appropriate follow-up.
Follow-up visits after a concussion are necessary for providing education on symptom management and oversight of return to school and activities. Furthermore, follow-up visits are also important to assess the need for more specialized care (Velikonja et al., 2017). Current guidelines outline that a follow-up visit should occur at any point within four weeks of an initial diagnosis (Velikonja et al., 2017). Although most children and youth follow a decreasing symptom trend and recover from concussion during this period (Macartney et al., 2018), some clinicians and researchers have suggested that the timing of follow-up visits be standardized as a way of managing concussion cases (Polinder et al., 2018). To help guide post-concussion care, several guidelines exist for clinicians to follow the management of pediatric concussion. In Canada, post-concussion care guidelines have been produced by organizations such as Parachute and the Ontario Neurotrauma Foundation. Parachute (2017), Canada’s national injury prevention organization, has produced the Canadian Guideline on Concussion in Sport, a guideline to ensure that athletes of all ages with a suspected concussion receive timely and appropriate care. However, this guideline is tailored specifically to sports-related injury and the athletes who participate in these activities; roughly 50% of pediatric concussions are non-sport related (Suskauer et al., 2019).
Post-concussion care requires appropriate service involvement from health care professionals that is dependent upon an individual’s recovery pattern after a concussion. For example, concussed individuals may only require education about symptom management from a primary care provider, while others with more persistent symptoms will require multidisciplinary care. The Standards for Post-Concussion Care from the Ontario Neurotrauma Foundation apply to all cases of concussion, irrespective of age, injury mechanism, or geographic residence (Velikonja et al., 2017). In general, these guidelines specify that diagnosis and management of a concussion should be conducted by a physician or a nurse practitioner (Velikonja et al., 2017). The overall management of pediatric concussion involves decisions around both return to school and return to play, underscoring the importance of follow-up with a primary care provider (Choe &Barlow, 2018; Polinder et al., 2018). After an initial rest period, a gradual return to activity and school is recommended for children and youth (Levin &Diaz-Arrastia, 2015; Velikonja et al., 2017). Upon completion of either or both gradual returns, a final clearance from a physician or a nurse practitioner is required (Parachute, 2017; Velikonja et al., 2017). Despite this simple requirement after an initial diagnosis of concussion, follow-up visits are often not completed in accordance with concussion guidelines. Therefore, it is of relevance to identify the evidence around follow-up visits after a concussion in the pediatric population.
There has been rising interest in research on follow-up visits after a concussion diagnosis in children and youth (Ramsay, 2021). A recent scoping review (Lundine et al., 2022) described factors contributing to follow-up care after pediatric acquired brain injury. Lundine et al. (2022) reviewed the literature on which factors contribute to the initiation or receipt of medical or rehabilitative services. However, the review also included studies that focused on brain injuries related to brain cancer and tuberculosis-associated meningitis. Although the review included a heterogeneous sample, the findings provided some evidence of the factors impacting brain injured patients’ choices or ability to seek follow-up care. Despite the growing body of literature, no study has yet synthesized the rate of follow-up visits after an initial concussion diagnosis in children andyouth.
1.2Objective
This integrative review aims to synthesize and analyse the current state of the literature on follow-up visits of children with a concussive injury and examine the factors associated with the occurrence of such visits within this population. The general research questions that guided this review were: (1) What is the rate of follow-up visits among concussed children and youth? (2) What is the length of time to the first follow-up visit? (3) What factors are associated with children and youth attending a first follow-up visit subsequent to an initial diagnosis of concussion? By answering these questions, new insights may be provided to improve the management of pediatric concussions and address factors impairing follow-up, which in turn can improve health outcomes of concussed children and youth.
2Methods
In this review, follow-up visits, in accordance with current guidelines, are defined as visits with a health care provider in the first four weeks after an initial diagnosis of concussion (Velikonja et al., 2017). A concussion is a type of traumatic brain injury (TBI) induced by direct or indirect biomechanical forces resulting in an alteration in brain function (McCrory et al., 2017). As a result, it is common in the literature for the term concussion to be interchanged with the term mild traumatic brain injury (mTBI), therefore both were used in this review to identify follow-up visits after injuries. Furthermore, many head injury studies include the full spectrum of TBIs, therefore any studies that identified mTBIs or concussions were also included. The pediatric population is defined as anyone who is 19 years of age or younger.
2.1Design
We conducted an integrative review using Knafl and Whittemore’s (2005) framework. An integrative review was chosen because of its ability to combine and synthesize findings from different types of research studies (Pearson et al., 2014). Integrative reviews can contain a wide range of purposes, which when combined with diverse methods, can lead to an in-depth understanding of a health care issue (Knafl &Whittemore, 2005). In applying Knafl and Whittemore’s (2005) five steps of identifying the purpose of the review, searching the relevant literature, evaluating and extracting data, analyzing or synthesizing the data, and presenting findings, we sought to explore and summarize the literature relevant to our three research questions.
2.2Search methods
An ordered and consistent search of the literature was conducted in August of 2022 to identify studies focused on follow-up visits of concussed children and youth. The primary patient population of interest was the concussed pediatric population. While follow-up visits are the focus of this review, the topics reviewed were part of a larger search regarding the spectrum of concussive disorders, follow-up or aftercare, and health outcomes. The databases searched included PubMed, MEDLINE, Cumulative Index of Nursing and Allied Health Literature (CINAHL), PsycINFO, and Google Scholar.
The search strategy was designed broadly by SR and VSD, so as to identify as many eligible studies for this review as possible. The inclusion criteria for this review were a) full-text empirical articles with an abstract, b) published in English and in the past 10 years, c) studies with a sample or a sub-sample of the pediatric population, and d) studies reporting on a follow-up visit after a concussion or mTBI (self-report, diagnosis, or International Classification of Disease code). Protocol studies, dissertations, and case reports were excluded. We also excluded studies focusing solely on describing after-care of concussion that did not report any relevant findings that answered either research question.
Subject headings/descriptors and keywords were identified to capture key concepts as MeSH headings and included brain concussion, brain injuries, traumatic, traumatic brain injury, head injuries, brain injuries, post-concussion syndrome, postconcussion syndrome, aftercare, follow-up, posttreatment follow-up, patient care, secondary care, retreatment, management, and health outcomes. Terms were adjusted according to the vocabulary used in each database. The searches for concussion, follow-up, and health outcomes were then combined using the AND Boolean operator. Keywords were searched within titles, abstracts, and keywords of articles. All research literature describing follow-up, management, or aftercare of the concussion spectrum of disorders in the pediatric population were considered for this review. Table 1 outlines an example of a detailed search strategy (CINAHL). Reference lists of included articles were also hand-searched with the same limiters to identify additional relevant studies.
Table 1
Search strategy for CINAHL and number of records identified (August 2022)
| Source | Search Strategy | n |
| CINAHL | 1. (MH “Brain Concussion+”) OR (MH “Postconcussion Syndrome”) OR (MH “Brain Injuries+”) | n = 515 |
| 2. (MH “Management”) OR (MH “Patient Care+”) OR (MM “After Care+”) | ||
| 3. (MH “Child+”) OR (MH “Adolescence+”) | ||
| 4. 1 AND 2 AND 3 | ||
| 5. Limit 4 to full text | ||
| 6. Limit 5 to English |
Fig. 1
PRISMA diagram: Follow-up visits after a concussion in the pediatric population.
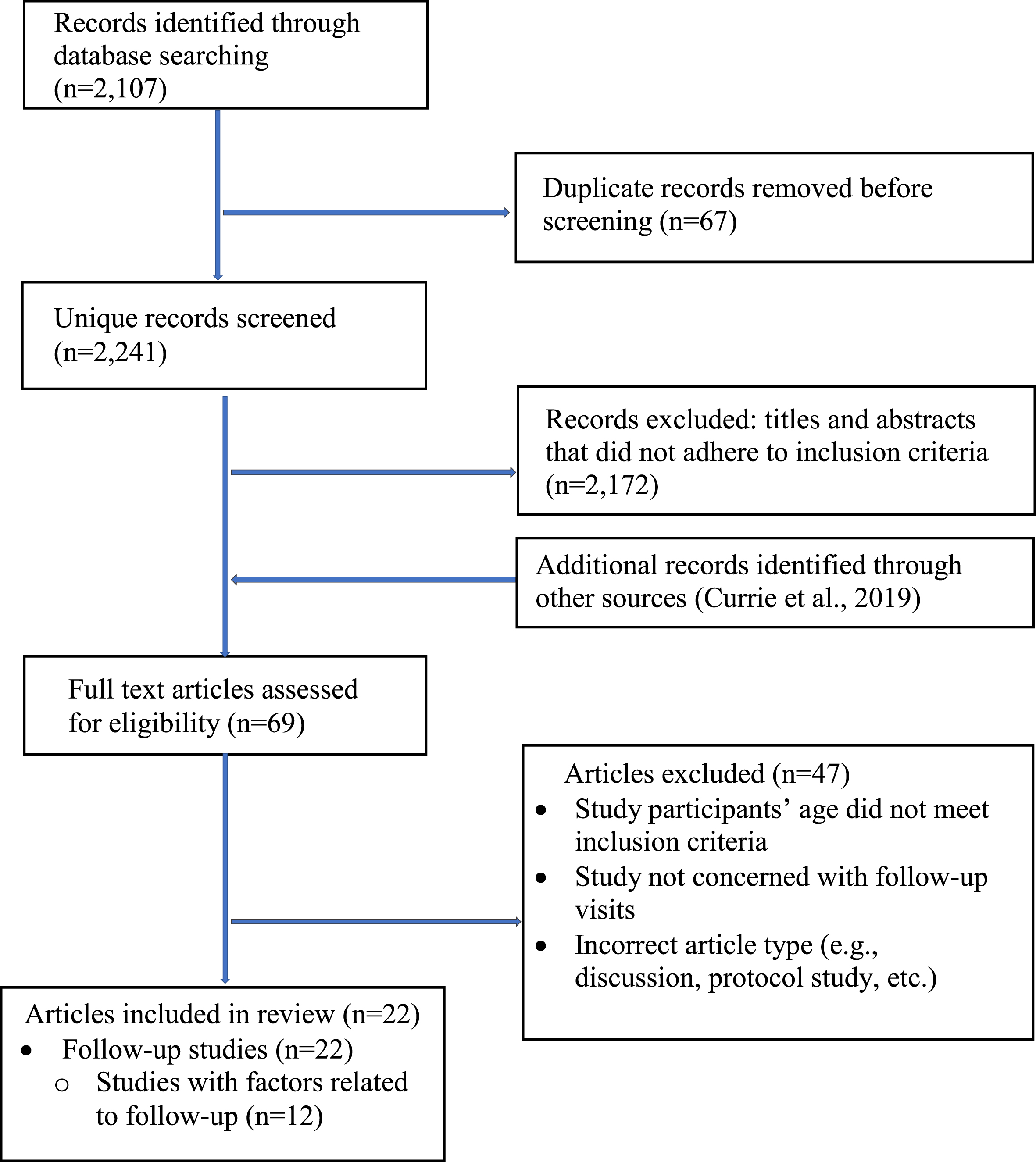
2.3Search outcomes
The integrative review process contains several stages in the selection of articles (Fig. 1). The search yielded a total of 2,308 studies from the five databases, of which 67 duplicates were removed. The titles and abstracts of 2,241 studies were screened against the inclusion and exclusion criteria to identify those that required full-text screening. Full-text review of 69 articles followed to identify those to include in the final synthesis. An additional article was identified through scanning references. Twenty-two articles pertained to follow-up after concussion in the pediatric population and were included in this review. Forty-seven articles were excluded for the following reasons: age or study type (e.g., discussion, protocol study) did not meet inclusion criteria, or the study did not focus on follow-up visits. The primary author (SR) carried out the search and managed the screening and initial selection of articles. The second author (VSD) reviewed selected articles to ensure search criteria were met.
2.4Data extraction and synthesis
Relevant data from the 22 included articles were extracted and entered into a data matrix. The extracted data identified the study authors, year, and country; methods (sample, design); follow-up rates; timing to a first follow-up visit; and factors associated with attendance of a follow-up visit. These are reported in Table 2 alphabetically by author. Data from each study were reviewed by SR and VSD to ensure the research questions were answered. There were some articles that did not investigate follow-up as a primary outcome, but presented sufficient data that the follow-up rate could be calculated. For example, in the study by Kania et al. (2016) 12 of the 45 patients were lost to follow-up, leaving 33 patients in the study, resulting in an adjusted follow-up visit rate of 73.3% as calculated by the first and second authors. Thus, all studies in this review include a follow-up rate. Critical appraisal of each study was completed using various Joanna Briggs Institute (JBI) Critical Appraisal Checklists (2020a, 2020b, 2020c) to identify the study’s strengths and weaknesses. Our appraisal of study quality is reported in text throughout the section on findings.
Table 2
Description of studies and study findings
| Authors (year) country | Sample | Data source injury type | Follow-up rates | Time to first follow-up visit | Factors associated with follow-up visits |
| Choe et al., (2016) | N = 151 (retrospective) | Clinical data | •88 of 151 (58.3%) retrospective patients attended a follow-up visit. | •Retrospective: 88 participants seen within 6 months. | •N/A |
| United States | N = 403 (prospective) Age: 0 to 25 years | TBI | •Prospective: Mean follow-up time = 8.1 months; median follow-up time = 1.2 months. | ||
| Corwin et al., (2020) | N = 159 (immediate diagnosis) | Clinical data Concussion | •72.9% of all patients attended a follow-up visit. | •Delayed concussion diagnosis = median of 3 days after initial visit. | •Symptoms present at initial visit was significantly more in immediate diagnosis group, while at follow- up total symptoms were significantly higher in delayed diagnosis group |
| United States | N = 85 (delayed diagnosis) Age: 6 to 18 years | ∘ 58.5% of immediate diagnosis patients attended a follow-up visit. | •Immediate concussion diagnosis = median of 4 days after initial visit. | ||
| Currie et al., (2019) | N = 183 Age: 8 to 18 years | Survey-based | •77.6% by 30 days | •N/A | •Females had increased odds of attending follow-up visits compared with males. |
| United States | Concussion | •54.4% attended follow-up within 7 days of ED discharge. | •Insurance type not associated with a follow-up visit. | ||
| Falk (2013) | N = 149 | Clinical data | •92% within 5 weeks post-discharge. | •N/A | •N/A |
| Sweden | Age: 1 day to 16 years | Concussion | |||
| Feyissa et al., (2015) | N = 198 | Clinical data | •79.8% within 60 days. | •Mean follow-up time = 6.5 days (intervention group) and 6.58 days (control group). | •The intervention of co-management between primary care providers and specialists significantly improved the likelihood of follow-up. |
| United States | Age: 7 to 18 years | Concussion | |||
| Fridman et al., (2018) | N = 126,654 | Population-based | •Overall follow-up rate of 21.2%. | •The median time to the first follow-up visit was 8 days. | •N/A |
| Canada | Age: 5 to 18 years | Concussion | |||
| Grubenhoff et al., (2015) | N = 179 | Survey-based | •45% had primary care follow-up in the month following concussion. | •N/A | •The total number of follow up visits was not significantly different for participants with and without persistent symptoms. |
| United States | Age: 8 to 18 years | Concussion | |||
| Haarbaueer-Krupa et al., (2018) | N = 39 | Survey-based | •26% attended an outpatient rehabilitation visit after discharge from the hospital. | •N/A | •Children hospitalized for 5 days or more were nearly six times more likely to follow-up with rehabilitation services than children hospitalized 4 days or less. |
| United States | Age: 6 to 9 years | TBI | |||
| Hwang et al., (2014) | N = 150 | •Physician follow-up of 58% by 2 weeks. | •N/A | •Private insurance was significantly more common in patients who completed 2-week follow-up with a physician. | |
| United States | Age: 8 to 17 years | Survey-based Concussion | •Physician follow-up of 64% by 4 weeks. | ||
| Jimenez et al., (2016) | N = 9,361 | Population-based | •A total of 2,706 outpatient rehabilitation follow-up visits (28.9%) upon discharge from acute settings | N/A | •Patients received more outpatient rehabilitation if they received inpatient rehabilitation. |
| United States | Age: 0 to 20 years | TBI | . | •There was no difference in follow-up for rehabilitation among the age groups. | |
| Kania et al., (2016) | N = 45 | Clinical data | •73.3% of patients included in the study followed-up. | •Mean time to first follow-up = 30 days after injury. | •N/A |
| United States | Age: 5 to 17 years | mTBI | |||
| Keenan et al., (2013) | N = 545 (TBI) | Population-based | •80.0% of participants had some type of outpatient follow-up. | •N/A | •Regardless of injury severity that children with a TBI did not have an increased risk of visiting a pediatrician compared to healthy controls. |
| United States | N = 2,310 (healthy comparisons) Age: 2 to 14 years | TBI | |||
| Macartney et al., (2018) | N = 136 | Clinical data | •68% of patients completed a follow-up assessment. | •N/A | •N/A |
| Canada | Age: 13 to 17 years | Concussion | |||
| McDonald et al., (2021) | N = 2,454 | Clinical data | •84.1% of potentially concussed individuals followed-up with a health care provider after being assessed over the phone. | N/A | •N/A |
| United States | Age: 0 to 17 years | Concussion | |||
| Purcell et al., (2016) | N = 198 | Clinical data | •99.5% of patients were seen at a sports medicine clinic for follow-up by a physician. | •The mean time to presentation at a sports medicine clinic after initial evaluation for patients aged 8 to 12 years was 5.7 days and 6.4 days for those 13 to 17 years of age. | •N/A |
| Canada | Age: 8 to 17 years | Concussion | |||
| Rao et al., (2018) | N = 27,447 (2014) | Survey-based | •86.8% of 12 to 17-year-olds not receiving follow-up from an HCP at the time of the survey (only 13.2% of youth received follow-up). | •N/A | •A higher proportion of hospitalized individuals (64.6%) compared to not hospitalized individuals (21.9%) reported being followed-up by a health professional. |
| Canada | Age:12 to 17 years | TBI | |||
| Register-Mihalik et al., (2015) United States | N = 245 Age: 10 to 18 years | Survey-based Concussion | •55.1% of participants attended a concussion clinic after initial assessment in an ED. | •50% of participants took a mean of 4.9 days to be seen at clinic after ED. | •N/A |
| Snedden et al., (2019) United States | N = 160 Age: 8 to 18 years | Survey-based Concussion | •78.1% of children attended a follow-up visit within 30 days of injury. | •The median number of days to a follow-up visit was 5 days for children with academic support and 7 days for children with no academic support. | •N/A |
| Spaw et al., (2018) | N = 352 | Clinical data | •80.1% of patients had a follow-up visit after injury; 52.8% were fully adherent to follow-up instructions. | •N/A | •Injury severity was not associated with follow-up. |
| United States | Age: 2 to 18 years | TBI | •Cause of injury not associated with follow-up within 4 weeks of injury. | ||
| •Age was associated with adherence to follow-up with the oldest age group significantly less likely to attend all follow-up in comparison to young children. | |||||
| •Sex was not a factor for adherence to follow-up, as males were similar to females. | |||||
| •Children who had private insurance were 3.5 times more likely to attend all follow-up visits compared to those on Medicaid/Medicare. | |||||
| •Patients who had follow-up with more than one specialty had an odds of 5.8 of attending at least one follow-up visit within 4 weeks of injury compared to those that saw physical medicine. | |||||
| Tarimala et al. (2018) | N = 12, 512 | Population-based | •51.2% of children had a follow-up visit after being seen initially in an emergency department. | •N/A | •Children 10 years or older had approximately double the likelihood of having follow-up care. |
| United States | Age: 0 to 18 years | Concussion | •A significant difference between sexes, as males had 1.27 greater odds of receiving follow-up care compared with females. | ||
| •Children living in an urban area had a higher rate of attendance for follow-up visits than those living in rural areas. | |||||
| Wendling-Keim et al., (2017) | N = 267 | Survey-based | •30 ambulatory patients and 41 hospitalized patients had follow-up at outpatient clinic or pediatrician (26.6%). | •N/A | •N/A |
| Germany | Age: 1 month to 16 years | Concussion | |||
| Zuckerbraun et al., (2014) | N = 354 | Survey-based | •Follow-up visit rates were 31% at 2 weeks and 32% at 4 weeks. | •N/A | •No differences in reported follow-up rates for gender. |
| United States | Age: 6 to 14 years | Concussion | •After implementation of the tool, follow-up rates increased to 55% at 2 weeks and 61% at 4 weeks. | •Patients with private commercial insurance reported significantly higher follow-up than those who had medical insurance from social assistance programs. |
3Results
3.1Study characteristics
Of the 22 full-text articles included in this review, 16 were conducted in the United States, four in Canada, one in Germany, and one in Sweden. Participants in the studies ranged in age from infancy to 25 years, but all studies included children and youth. Five studies included the full spectrum of TBI severity, but it was noted that mTBI and concussions were included. Of note, 12 studies included children less than 7 years old as part of their study sample. Half of the studies (n = 11) were published in the past 5 years.
All 22 reviewed articles used quantitative methods, but with varying sources of data. Nine were survey-based studies, nine drew on clinical data, and four studies used population-based data. Sample sizes ranged from 39 in one of the survey-based studies (Haarbauer-Krupa et al., 2018) to 126,654 in the largest population-based data study (Fridman et al., 2018).
Three main findings emerged, aligned with the research questions. These were: follow-up rates, the timing to a first follow-up visit, and factors associated with attending a follow-up visit. The findings on follow-up rates are grouped according to the data source used to allow for a more focussed review and comparison of findings, strengths, and limitations. As few studies investigated time to first follow-up visit, all study findings are reported together. The findings on factors associated with attending follow-up visits after an initial concussion diagnosis are grouped and discussed by injury-related factors, individual factors, and health service factors.
3.2Follow-up rates
This section reports findings by data source, but also groups and discusses study findings by follow-up rate (i.e.,< 50% and ≥50%).
Nine studies analyzed survey data and reported on the rates of follow-up visits after a concussion. Four studies had rates of follow-up visits ≥50% (Currie et al., 2019; Hwang et al., 2014; Register-Mihalik et al., 2015; Snedden et al., 2019), and five studies had rates below 50% (Grubenhoff et al., 2015; Haarbauer-Krupa et al., 2018; Rao et al., 2018; Wendling-Keim et al., 2017; Zuckerbraun et al., 2014). Still, there was a wide range of follow-up visit rates within each group. Snedden and colleagues (2019) reported the highest follow-up rate of survey-based studies, as 78.1% of children attended a follow-up visit by 30 days. In contrast, a sub-analysis of a Canadian wide survey reported the lowest percentage of follow-up visits of any study, with only 13.2% of youth (ages 12 to 17 years) being followed-up (Rao et al.,2018).
Among the nine studies that used clinical data all follow-up rates were greater than 50%, ranging from 58% to almost 100% (Choe et al., 2016; Falk, 2013; Kania et al., 2016; Macartney et al., 2018; McDonald et al., 2021; Spaw et al., 2018; Feyissa et al., 2015; Purcell et al., 2016). The study with the highest follow-up rate in this review (99.5%) was a retrospective chart review conducted at a sports medicine clinic in Ontario, Canada (Purcell et al.,2016).
Four population-based data studies were reviewed. Although all used administrative data, the study methods varied by sample size, time frame for measuring a follow-up visit, severity of brain injury and in their findings. Similar to the survey-based data, follow-up visit rates were evenly split above (Keenan et al., 2013; Tarimala et al., 2019) and below 50% (Fridman et al., 2018; Jiminez et al., 2016). The lowest follow-up visit rate (21.2%) was reported by Fridman et al. (2018) compared with the highest follow-up visit rate of 80% by Keenan et al. (2013).
3.3Time to a first follow-up visit
While timing of a visit is an important marker of care, this specific measure is often neglected when authors investigate or report on follow-up visits. Only eight of the 22 articles explicitly reported the time to first follow-up visit. In these studies, time was measured in days (Corwin et al., 2020; Feyissa et al., 2015; Fridman et al., 2018; Kania et al., 2016; Purcell et al., 2016; Register-Mihalik et al., 2015; Snedden et al., 2019) or months (Choe et al., 2016). The study with the shortest time to follow-up reported a median of 4 days for diagnosed patients to visit a concussion clinic after an initial encounter (Corwin et al., 2020). The longest time to a follow-up visit reported a mean follow-up time of 8.1 months (median 1.2 months) (Choe et al., 2016).
3.4Factors associated with a follow-up visit
Twelve of the 22 studies reported on at least one factor associated with a follow-up visit, with most reporting more than one factor. Three types of factors emerged: injury-related, individual, and health service factors.
Eight studies found an association between injury-related factors, such as hospitalization or injury severity, symptomology, and injury mechanism, and a follow-up visit. Three of the five studies that investigated hospitalization or injury severity found that these factors were associated with higher attendance rates at follow-up visits (Haarbauer-Krupa et al., 2018; Jiminez et al., 2016; Rao et al., 2018). Similarly, two of the three studies that investigated the relationship between symptoms and attending a follow-up visit found that children with more total and more persistent symptoms were more likely to have attended a follow-up visit compared to children who had early symptom resolution (Corwin et al., 2020; Currie et al., 2019). In contrast, three studies failed to find an association between injury-related factors and a follow-up visit (Grubenhoff et al., 2015; Keenan et al., 2013; Spaw et al., 2018). Only one study investigated injury mechanism and found no differences regarding attendance of at least one follow-up visit within 4 weeks of an initial injury (Spaw et al., 2018).
Seven studies investigated an association between the individual characteristics of age, sex, urban or rural residence, and insurance and a follow-up visit. Two studies identified significant age-related differences for having follow-up visits (Spaw et al., 2018; Tarimala et al., 2019), although another study found no age-related differences in attending a rehabilitation follow-up visit (Jiminez et al., 2016). Four studies investigated sex or gender as a factor associated with follow-up after a concussion in the pediatric population. Two studies found sex- or gender-related differences in follow-up visits but the results were mixed. Currie et al. (2019) identified females as having a greater likelihood of follow-up visits compared to the study by (Tarimala et al., 2019) that found a greater likelihood for males. The two other studies failed to find such a relationship (Spaw et al., 2018; Zuckerbraun et al., 2014). Geographic residence was also found associated with follow-up, with children 18 years and younger living in rural areas having a significantly lower odds of a follow-up visit compared to those living in urban areas (Tarimala et al., 2019). Lastly, three studies found that insurance type was associated with follow-up rates (Spaw et al., 2018; Hwang et al., 2014; Zuckerbraun et al., 2014), while another study found that insurance type did not predict children’s attendance to a follow-up visit (Currie et al., 2019).
Individuals with a concussion may receive care from a variety of health care providers with different disciplinary backgrounds and specialty education. Health service factors were investigated in three studies and included the type of health care provider and the provider’s specialty. In the population-based study by Jiminez et al. (2016), the most important predictor of a rehabilitation follow-up visit was consultation with a rehabilitation physician during initial hospitalization. Spaw and colleagues (2018) found that children who received a follow-up visit with more than one specialist compared to children who only visited a physiatrist were almost six times more likely to attend at least one follow-up visit by 4 weeks after injury. A quasi-experimental study that implemented co-management of patient care between pediatric primary care providers and subspecialists, found that co-management (versus regular primary physician care) significantly improved the likelihood of follow-up for pediatric patients with a concussion (Feyissa et al., 2015).
4Discussion
This integrative review aimed to identify and synthesize the evidence on follow-up visits for the pediatric population with a concussive injury. Follow-up visits are important for reassessment and management of pediatric concussions. The overall management of pediatric concussion involves decisions around both return to school and return to play underscoring the importance of follow-up with a health care provider (Velikonja et al., 2017). Despite the importance of follow-up visits in the concussed pediatric population, there is a lack of relevant reviews on the literature.
Our review suggests that children and youth are not consistently followed-up after an initial concussion diagnosis. Follow-up visit rates differed greatly amongst studies (13 to 99.5%), but differences in study designs (i.e., survey, clinical, or population-based), methods for identifying concussion cases, study samples, and reporting of results preclude comparison across many of the studies. Very few (8) of the 22 studies in this review measured the time to first follow-up visit; thus, we were unable to fully answer the second research question. However, among those eight studies (4 days to 8.1 months), six met the standard for timing of a first follow-up visit (28 days) after initial diagnosis documented by the Ontario Neurotrauma Foundation (Velikonja et al., 2017). In regards to research question 3, injury-related (hospitalization, persistent symptoms), individual (age, sex/gender, geographic residence, insurance type), and health service (multidisciplinary, specialist) factors were all found to be associated with follow-up visits in children and youth after an initial concussion diagnosis, but the evidence was mixed. Overall, our findings have shown that this area of research is still emerging—given the increasing number of studies in the last 10 years, especially in the past 5 years, but with particular limitations in regards to time to first follow-up and factors that influence the occurrence follow-up visits.
Understanding follow-up rates and timing of first follow-up visits are crucial for improving care and management of pediatric concussions. Recent research conducted in Australia demonstrated the importance of timing of care following a concussion in the pediatric population (Cassimatis et al., 2021). This study found that individuals who sought care beyond 28 days after an injury had significantly longer recovery times compared to those who sought care within 28 days of an injury. Therefore, care is not only pivotal to children and youth during the acute phase of concussion (i.e., within 72 hours of an injury), but also during the sub-acute phase (i.e.,> 72 hours of an injury) and continuously throughout the recovery process.
In their review, Lundine et al. (2022) found multiple factors associated with follow-up care in children with brain injury, concluding that socioeconomic variables (e.g., transportation issues, insurance, time off work) served as challenges to attending follow-up care. Our findings support this stance but differ in that we also identified injury-related factors and health service factors that are associated with the occurrence of a follow-up visit after an initial diagnosis. Two studies in our review reported that follow-up visits were more likely when multiple health care professionals were involved (Feyissa et al., 2015; Spaw et al., 2018), suggesting that a multidisciplinary approach may be more effective than a traditional single provider approach when providing follow-up care. This finding is supported by clinical research, as Ellis et al. (2017) recommended from their chart review that management of pediatric concussion patients requires the contributions of several team members with specialized expertise in various brain injury-related sub-disciplines. Follow-up care of this nature may be in the form of co-management of a patient to a multidisciplinary clinic but will ultimately depend on an individual’s injury and recoverypattern.
Based on the findings of this review, we support the following recommendations for clinical practice and policy. First, follow-up care should be timely and uninterrupted after an initial concussion diagnosis (Velikonja et al., 2017). This requires that there are effective and efficient referral processes and the triaging of referrals in place. An example of a timely process was described in the study by Register-Mihalik et al. (2015), where patients (aged 10-18 years) took an average of 4.9 days to visit a sports medicine clinic after an initial assessment in the ED. Second, follow-up care should be provided based on the recovery pattern of the concussed child or youth. For example, initial symptom burden has been shown to be a predictor of prolonged concussion recovery in children and youth (Cassimatis et al., 2021). However, one of the studies in our review found that children and youth with more initial symptoms and an immediate diagnosis, but less follow-up symptoms, were less likely to attend a follow-up visit than those with fewer initial symptoms and a delayed diagnosis, but more follow-up symptoms (Corwin et al., 2020), suggesting those with dissipating symptoms may be less likely to seek follow-up. Third, it is important that follow-up care be multidisciplinary and led by a physician or nurse practitioner to oversee symptom management (Velikonja et al., 2017). To ensure that follow-up care is provided to children and youth with a concussion, health care organizations should adopt standardized guidelines set out by internationally recognized organizations. An example of a guideline is the Standards for Post-concussion Care developed by the Ontario Neurotrauma Foundation, which is intended to improve health care service processes and coordination during the concussion recovery period (Velikonja et al., 2017). While these guidelines broadly cover a wide range of ages, guidelines need to be tailored to the pediatric population to address their specific needs. These recommendations, when bundled and applied together, have the potential to improve follow-up care processes and the coordination of care duringrecovery.
In light of our review findings, we recommend the following for future research. First, future research should aim at investigating follow-up and follow-up timing as primary outcomes. The studies in this review on the follow-up of pediatric concussion did not all investigate follow-up as a primary outcome and not all studies included the timing of the first follow-up visit after diagnosis. Second, more useful findings might be obtained if the study focussed on a specific injury type or included sub-analyses of the various degrees of injury, rather than including all TBI severities as found in some of the studies in this review. Third, there should be more investigation of factors that influence follow-up visits of concussed children and youth. Although injury-related factors have received substantial attention amongst researchers, policymakers, and health care professionals, individual and health service factors may play a more prominent role in follow-up visits than is currently understood. As such, further research focussing on individual and health care service factors that may impact follow-up visits is strongly recommended. Finally, there is a need for high quality studies that use diverse methodologies such as qualitative and mixed methods, as all the articles we were able to identify for this review used only quantitative study designs.
4.1Limitations
There were some limitations to the current review. For example, as the search was limited to full-text articles published in English and the use of specific search terms, it is possible that relevant studies were not identified or included. Further, studies published prior to 2010 may have been excluded due to the date restriction placed during literature searches. Limitations to the above studies were identified. The studies used varying time frames when measuring the occurrence of a follow-up visit, and few measured the time to first follow-up visit. There were also differences in study designs, study samples, methods for identifying concussion cases (e.g., self-report vs. International Classification of Disease code), injury severity, and reporting of results that precluded comparison across many of the studies and limit the generalizability of findings. However, it is noteworthy that this is the first review of its kind. Despite a recent scoping review on factors contributing to follow-up care after acquired brain injury in the pediatric population (Lundine et al., 2022), our review adds important findings because of the focus on pediatric concussion, plus the emphasis on the rates of follow-up visits and the timing of the first follow-up visits. Also, we followed a thorough framework for integrative reviews that guided our review.
5Conclusion
Follow-up visits are an important component of post-concussion care for the pediatric population. In this integrative review we reviewed and synthesized the current evidence on follow-up visit rates among concussed children and youth, the timing of the first follow-up visit after an initial diagnosis, and factors associated with attending a follow-up visit. Overall, our findings indicate that children and youth are not consistently followed-up after an initial concussion diagnosis; however, little can be concluded regarding time to first follow-up and factors that influence the occurrence follow-up visits. Our review indicates that research into the follow-up care of children and youth with concussion is a new and emerging field of study with limitations to the current research. Nonetheless, our findings are an important starting point to begin addressing this significant injury and its associated care.
Conflict of interest
The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
Acknowledgments
The authors have no acknowledgements.
Funding
Scott Ramsay received support for the third and fourth years of his doctoral program from the University of British Columbia, the Canadian Nurses Foundation, Indspire, and the Registered Nurses Foundation of British Columbia.
Ethical Approval
Not applicable, as no human subjects were engaged in this study.
References
1 | Bryan, M. A. , Rowhani-Rahbar A. , Comstock, R. D. , & Rivara, F. ((2016) ) Sports-and recreation- related concussions in US youth. Pediatrics, 138: (1), 1–8. https://doi.org/10.1542/peds.2015-4635 |
2 | Cassimatis, M. , Orr, R. , Fyffe, A. , & Browne, G. ((2021) ) Early injury evaluation following concussion is associated with improved recovery time in children and adolescents. Journal of Science and Medicine in Sport, 24: , 1235–1239. https://doi.org/10.1016/j.jsams.2021.06.012 |
3 | Choe, M. , & Barlow, K. M. ((2018) ) Pediatric traumatic brain injury and concussion. CONTINUUM, 24: (1, Child Neurology), 300–311. https://doi.org/10.1212/CON.0000000000000569 |
4 | Choe, M. C. , Valino, H. , Fischer, J. , Zeiger, M. , Breault, J. , McArthur, D. L. , Leung, M. , Madikians, A. , Yudovin, S. , Lerner, J. T. , & Giza, C. C. ((2016) ) Targeting the epidemic: Interventions and follow-up are necessary in the pediatric traumatic brain injury clinic. Journal of Child Neurology, 31: (1), 109–115. https://doi.org/10.1177/0883073815572685 |
5 | Corwin, D. J. , Arbogast, K. B. , Haber, R. A. , Pettijohn, K. W. , Zonfrillo, M. R. , Grady, M. F. , & Master, C. L. ((2020) ) Characteristics and outcomes for delayed diagnosis of concussion in pediatric patients presenting to the emergency department. The Journal of Emergency Medicine, 59: (6), 795–804. https://doi.org/10.1016/j.jemermed.2020.09.017 |
6 | Currie, D. , Snedden, T. , Pierpoint, L. , Comstock, R. D. , & Grubenhoff, J. A. ((2019) ) Factors influencing primary care follow-up after pediatric mild traumatic brain injury. Journal of Head Trauma Rehabilitation, 34: (4), E11–804. https://doi.org/10.1097/HTR.0000000000000461 |
7 | Ellis, M. J. , Ritchie, L. J. , McDonald, P. J. , Cordingley, D. , Reimer, K. , Nijjar, S. , Koltek, M. , Hosain, S. , Johnston, J. , Mansouri, B. , Sawyer, S. , Silver, N. , Girardin, R. , Larkins, S. , Vis, S. , Selci, E. , Davidson, M. , Gregoire, S. , Sam, A. , & Russell, K. ((2017) ) Multidisciplinary management of pediatric sports-related concussion. The Canadian Journal of Neurological Sciences, 44: , 24–34. https://doi.org/10.1017/cjn.2016.312 |
8 | Falk, A. C. ((2013) ) A nurse-led paediatric head injury follow-up service. Scandinavian Journal of Caring Sciences, 27: (1), 51–56. https://doi.org/10.1111/j.1471-6712.2012.00999.x |
9 | Feyissa, E. A. , Cornell, E. , Chandhok, L. , Wang, D. , Ionita, C. , Schwab, J. , & Rubin, K. ((2015) ) Impact of co-management atthe primary-subspecialty care interface on follow-up and referralpatterns for patients with concussion. Clinical Pediatrics, 54: (10), 969–975. https://doi.org/10.1177/0009922814566929 |
10 | Fridman, L. , Scolnik, M. , Macpherson, A. , Rothman, L. , Guttmann, A. , Grool, A. M. , Rodriguez Duque, D. , & Zemek, R. L. ((2018) ) Annual trends in follow-up visits for pediatric concussion in eemergency departments and physicians’ offices. Journal of Pediatrics, 192: , 184–188. https://doi.org/10.1016/j.jpeds.2017.09.018 |
11 | Grubenhoff, J. A. , Deakyne, S. J. , Comstock, R. D. , Kirkwood, M. W. , & Bajaj, L. ((2015) ) Outpatient follow-up and return to school after emergency department evaluation among children with persistent post-concussion symptoms. Brain Injury, 29: (10), 1186–1191. https://doi.org/10.3109/02699052.2015.1035325 |
12 | Haarbauer-Krupa, J. , Lundine, J. P. , Depompei, R. , & King, T. Z. ((2018) ) Rehabilitation and school services following traumatic brain injury in young children. NeuroRehabilitation, 42: (3), 259–267. https://doi.org/10.3233/NRE-172410 |
13 | Hwang, V. , Trickey, A. W. , Lormel, C. , Bradford, A. N. , Griffen, M. M. , Lawrence, C. P. , Struek, C. , Stacey, E. , & Howell, J. M. ((2014) ) Are pediatric concussion patients compliant with discharge instructions? Journal of Trauma and Acute Care Surgery, 77: (1), 117–122. https://doi.org/10.1097/TA.0000000000000275 |
14 | Jimenez, N. , Symons, R. G. , Wang, J. , Ebel, B. H. , Vavilala, M. S. , Buchwald, D. , Temkin, N. , Jaffe, K. M. , & Rivara, F. P. ((2016) ) Outpatient rehabilitation for medicaid-insured children hospitalized with traumatic brain injury. Pediatrics, 137: (6), 1–9. https://doi.org/10.1542/peds.2015-3500 |
15 | Joanna Briggs Institute. (2020a). Checklist for analytical cross sectional studies.https://jbi.global/critical-appraisal-tools/checklist-for-analytical-cross-sectional-studies |
16 | Joanna Briggs Institute. (2020b). Checklist for prevalence studies.https://jbi.global/critical-appraisal-tools/checklist-for-prevalence-studies |
17 | Joanna Briggs Institute. (2020c). Checklist for quasi-experimental studies. https://jbi.global/critical-appraisal-tools/checklist- for-quasi-experimental-studies |
18 | Kania, K. , Shaikh, K. A. , White, I. K. , & Ackerman, L. L. ((2016) ) Follow-up issues in children with mild traumatic brain injuries. Journal of Neurosurgery: Pediatrics, 18: (2), 224–230. https://doi.org/10.3171/2016.1.PEDS15511 |
19 | Keenan, H. T. , Murphy, N. A. , Staheli, R. , & Savitz, L. A. ((2013) ) Healthcare utilization in the first year after pediatric traumatic brain injury in an insured population. The Journal of head trauma rehabilitation, 28: (6), 426–432. https://doi.org/10.1097/HTR.0b013e31825935b8 |
20 | Knafl, R. , & Whittemore, K. K. ((2005) ) The integrative review: updated methodology. Journal of Advanced Nursing, 52: (5), 546–53. https://doi.org/10.1111/j.1365-2648.2005.03621.x |
21 | Langer, L. , Levy, C. , & Bayley, M. ((2020) ) Increasing incidence of concussion: True epidemic or better recognition? Journal of Head Trauma Rehabilitation, 35: (1), E60–E66. https://doi.org/10.1097/HTR.0000000000000503 |
22 | Levin, H. S. , & Diaz-Arrastia, R. R. ((2015) ) Diagnosis, prognosis, and clinical management of mild traumatic brain injury. The Lancet Neurology, 14: (5), 506–517. https://doi.org/10.1016/S1474-4422(15)00002-2 |
23 | Lundine, J. P. , Ciccia, A. H. , Koterba, C. , & Guernon, A. ((2022) ) Factors that influence follow-up care for families of children with acquired brain injury: A scoping review. Brain Injury, 36: (4), 469–478. https://doi.org/10.1080/02699052.2022.2051741 |
24 | Macartney, G. , Simoncic, V. , Goulet, K. , & Aglipay, M. ((2018) ) Concussion symptom prevalence, severity and trajectory: Implications for nursing practic. Journal of Pediatric Nursing, 40: , 58–62. https://doi.org/10.1016/j.pedn.2018.03.006 |
25 | McCrory, P. , Meeuwisse, W. , Dvorak, J. , Aubry, M. , Bailes, J. , Broglio, S. , & Vos, P. E. ((2017) ) Consensus statement on concussion in sport—the 5th international conference on concussion in sport held in Berlin, October. British Journal of Sports Medicine, 51: , 838–847. https://doi.org/10.1136/bjsports-2017-097699 |
26 | McDonald, C. C. , Pfeiffer, M. R. , Robinson, R. L. , Arbogast, K. B. , & Master, C. L. ((2020) ) Telephone triage in pediatric head injury: follow-up patterns and subsequent diagnosis of concussion. Clinical Nursing Research, 30: (2), 104–109. https://doi.org/10.1177/1054773820924572 |
27 | Parachute. (2017). Canadian guideline on concussion in sport. Retreived from https://parachute.ca/en/professionalresource/concussion-collection/canadian-guideline-onconcussion-in-sport/ |
28 | Pearson, A. , White, H. , Bath-Hextall, F. , Apostolo, J. , Salmond, S. , & Kirkpatrick, P. (2014). The Joanna Briggs Institute reviewers' manual 2014: Methodology for JBI mixed methods systematic reviews, vol. 1. The Joanna Briggs Institute,5–34. |
29 | Polinder, S. , Cnossen, M. C. , Real, R. G. L. , Covic, A. , Gorbunova, A. , Voormolen, D. C. , Master, C. L. , Haagsma, J. A. , Diaz-Arrastia, R. , & Von Steinbuechel, N. ((2018) ) A multidimensional approach to post-concussion symptoms in mild traumatic brain injury. Frontiers in Neurology, 9: (1113), 1–14. https://doi.org/10.3389/fneur.2018.01113 |
30 | Purcell, L. , Harvey, J. , & Seabrook, J. A. ((2015) ) Patterns of recovery following sport-related concussion in children and adolescents. Clinical Pediatrics, 55: (5), 452–458. https://doi.org/10.1177/0009922815589915 |
31 | Ramsay, S. ((2021) ) Follow-up care in children and young people diagnosed with a concussion: a commentary. British Journal of Neuroscience Nursing, 17: (6), 226–229. https://doi.org/10.12968/bjnn.2021.17.6.226 |
32 | Rao, D. P. , McFaull, S. , Thompson, W. , & Jayaraman, G. C. ((2018) ) Traumatic brain injury management in Canada: Changing patterns of care. Health Promotion and Chronic Disease Prevention in Canada, 38: (3), 147–150. https://doi.org/10.24095/hpcdp.38.3.05 |
33 | Register-Mihalik, J. K. , De Maio, V. J. , Tibbo-Valeriote, H. L. , & Wooten, J. D. ((2015) ) Characteristics of pediatric and adolescent concussion clinic patients with postconcussion amnesia. Clinical journal of sport medicine, 25: (6), 502–508. https://doi.org/10.1097/JSM.0000000000000161 |
34 | Seabury, S. A. , Gaudette, É. , Goldman, D. P. , Markowitz, A. J. , Brooks, J. , McCrea, M. A. , Okonkwo, D. O. , & Manley, G. T. ((2018) ) Assessment of Follow-up Care After Emergency Department Presentation for Mild Traumatic Brain Injury and Concussion Results From the TRACK-TBI Study. JAMA Network Open, 1: (1), 1–13. https://doi.org/10.1001/jamanetworkopen.2018.0210 |
35 | Snedden, T. R. , Pierpoint, L. A. , Currie, D. W. , Comstock, R. D. , & Grubenhoff, J. A. ((2019) ) Post-concussion Academic Support in Children Who Attend a Primary Care Provider Follow-up Visit after Presenting to the Emergency Department. Journal of Pediatrics, 209: , 168–175. https://doi.org/10.1016/j.jpeds.2019.01.041 |
36 | Spaw, A. J. , Lundine, J. P. , Johnson, S. A. , Peng, J. , Wheeler, K. K. , Shi, J. , Yang, G. , Haley, K. J. , Groner, J. I. , & Xiang, H. ((2018) ) Follow-Up Care Adherence after Hospital Discharge in Children with Traumatic Brain Injury. Journal of Head Trauma Rehabilitation, 33: (3), E1–E10. https://doi.org/10.1097/HTR.0000000000000314 |
37 | Suskauer, S. J. , Yeates, K. O. , Sariento, K. , Benzel, E. C. , Breiding, M. J. , Broomand, C. , & Lumba-Brown, A. ((2019) ) Strengthening the evidence base: Recommendations for future research identified through the development of CDC’s pediatric mild TBI guideline. Journal of Head Trauma Rehabilitation, 34: (4), 215–223. https://doi.org/10.1097/HTR.0000000000000455 |
38 | Tarimala, A. , Singichetti, B. , Yi, H. , Huang, L. , Doerschuk, R. , Tiso, M. , & Yang, J. ((2019) ) Initial emergency department visit and follow-up care for concussions among children with medicaid. Journal of Pediatrics, 206: , 178–183. https://doi.org/10.1016/j.jpeds.2018.10.021 |
39 | Thomas, D. J. , Coxe, K. , Li, H. , Pommering, T. L. , Young, J. A. , Smith, G. A. , & Yang, J. ((2018) ) Length of recovery from sports-related concussions in pediatric patients treated at concussion clinics. Clinical Journal of Sport Medicine, 28: , 56–63. https://doi.org/10.1097/JSM.0000000000000413 |
40 | Velikonja, D. O. , Baldisera, T. , Bauman, S. , Davis, S. , Di Salle, C. , Freedman, M. , Ouchterlony, D. , Quon, D. , Reed, N. , Sims, K. , Wilcock, R. , Zemek, R. , Kagan, C. , Gargaro, J. , Hansen, M. , & Wiseman-Hakes, C. (2017). Standards for Post-concussion Care. Retrieved from http://concussionsontario.org/wp-content/uploads/2017/06/ONF-Standards-for-Post-Concussion-Care-June-8-2017.pdf |
41 | Wendling-Keim, D. S. , König, A. , Dietz, H. G. , & Lehner, M. ((2017) ) Ambulatory or inpatient management of mild TBI in children: a post-concussion analysis. Pediatric Surgery International, 33: (2), 249–261. https://doi.org/10.1007/s00383-016-4021-z |
42 | Zuckerbraun, N. S. , Atabaki, S. , Collins, M. W. , Thomas, D. , & Gioia, G. A. ((2014) ) Use of modified acute concussion evaluation tools in the emergency department. Pediatrics, 133: (4), 635–642. https://doi.org/10.1542/peds.2013-2600 |




