Predictors of caregiver burden in caregivers of individuals with traumatic or non-traumatic brain injury: A scoping review
Abstract
BACKGROUND:
Caregivers of individuals with traumatic (TBI) or non-traumatic (nTBI) brain injuries are at risk of significant caregiver burden. Consequently, it is crucial to examine predictors of caregiver burden to enable early identification and intervention.
OBJECTIVE:
To examine predictors of caregiver burden in caregivers of individuals with TBI/nTBI.
METHODS:
A scoping review was conducted in the bibliographic databases PubMed, EMBASE (Ovid) and APA PsycInfo (EBSCO). Search terms included: ‘acquired brain injur*’, ‘traumatic brain injur*’, ‘brain injur*’, ‘non-traumatic brain injur*’, or ‘stroke*’ combined with ‘burden’, ‘caregiver burden’, ‘perceived burden’, or ‘caregiver strain’. The search was limited to articles written in English and published in academic journals between 2000 and March 2022. EndNote was used to manage the references and identify duplicates.
RESULTS:
Twenty-four studies were included. Care recipient-related predictors of caregiver burden included more severe injuries, functional disabilities (including decreased physical and neuropsychological functioning), and worse mental health. Caregiver-related predictors included more time spent caregiving, worse mental health, and unmet needs. For several predictor variables, evidence was mixed or vague.
CONCLUSION:
The results highlight which caregivers are at risk of caregiver burden and point to several areas of potential intervention to prevent caregiver burden. Future research should explore the relationship between characteristics of the caregiver and caregiver burden, including coping style, problem-solving techniques, and personality, as these have been sparsely investigated and are potentially modifiable through intervention. Further research is needed to elucidate if burden can be prevented by interventions targeting caregivers at risk. Addressing these gaps may clarify the link between caregiver burden and predictor variables and assist in development of interventions that may prevent burden.
1Introduction
Every year, the number of individuals acquiring an injury to the brain, including external trauma and internal sources such as stroke, is substantial (Tagliaferri et al., 2006; Dewan et al., 2018; Feigin et al., 2003). Approximately, 135 million people live with the consequences of stroke or traumatic brain injury (TBI) worldwide (Cieza et al., 2020). There are two main categories of brain injury acquired after birth, including TBI and non-traumatic brain injury (nTBI). TBI is caused by external forces that damage the brain, e.g. falls, motor traffic accidents, sport- or leisure accidents, or assaults, whereas nTBI usually involves an underlying pathology, e.g. a tumor, brain infection, or vascular problems resulting in stroke (Brain Injury Association of America, 2020). Regardless of the cause of the injury, individuals with TBI or nTBI may experience persistent physical, emotional, cognitive, social, and behavioral impairments and disabilities (Arango-Lasprilla et al., 2010; King & Tyerman, 2010; Griffen & Hanks, 2014). The chronic functional impairments that follow from TBI and nTBI can compromise the individual’s ability to live an independent life. Consequently, individuals with TBI or nTBI often rely on family caregivers for emotional support, care, supervision, and practical support in activities of daily living (Kreitzer et al., 2018). Since the onset of TBI and nTBI is sudden and consequently unexpected, the closest family members are not prepared for their new role as caregivers (Kreitzer et al., 2018).
Family caregivers have an important role as they contribute to the sustainability of the health care system by reducing the need for professional caregivers and institutional care (Kokorelias et al., 2020). Many caregivers are capable of adjusting to the caregiving role, and some caregivers emphasize the positive and rewarding aspects of caregiving (Mackenzie & Greenwood, 2012). However, providing the required care and support to an individual who sustained an injury to the brain can be time-consuming and demanding. Consequently, the caregiving role can lead to a substantial burden on the family caregivers (Baker et al., 2017). The term ‘caregiver burden’ has been coined to describe the potential negative consequences of caregiving. The term encompasses the psychological, social, economic, emotional, and physical problems experienced by caregivers because of the caregiving role (Rottmann et al., 2022). Studies have demonstrated high frequencies of burden in family caregivers of individuals with TBI and nTBI. A systematic review of literature within the field of stroke demonstrated that 25–54% of caregivers experienced a significant burden, and levels of burden remained elevated for an indefinite period following injury (Rigby et al., 2009b). Likewise, studies have found that between 40–61% of caregivers of individuals with TBI experienced moderate to high burden (Bayen et al., 2016; Doser & Norup, 2015; Manskow et al., 2015). The high frequencies of caregiver burden emphasize the need for further attention to caregiver issues and stress the importance of gaining knowledge on the topic.
Experiencing burden from providing care to an individual with TBI or nTBI can have adverse consequences for the caregiver. It has been well established that family caregivers often suffer long-term stress (Verhaeghe et al., 2005), lower quality of life, (Norup et al., 2010, 2017; Vogler et al., 2014), low life satisfaction (Bergström et al., 2011), anxiety and depression (Arango-Lasprilla et al., 2010; Norup et al., 2013), and burnout (Kreitzer et al., 2018). In keeping with these findings, a recent study investigating the socioeconomic consequences of TBI showed that relatives of individuals with TBI had increased health care costs following the injury (Norup et al., 2020). Psychological consequences of having a family member sustaining an injury to the brain could likely explain the increased health care costs for the closest relatives. These findings emphasize the potential societal costs of caregivers experiencing high levels of burden. Moreover, the health consequences of providing care to an individual with TBI or nTBI have important implications for the well-being and the outcome of the individual with the injury (Rigby et al., 2009b), since the quality of the care provided is optimized, when the caregiver has good mental and physical health (Norup, 2018). These findings emphasize the importance of early identification of vulnerable caregivers in order to provide them with support, and thus prevent the possible long-term consequences that can follow from experiencing caregiver burden.
There are individual differences regarding how well caregivers cope with a changed life situation (Chronister et al., 2010). Previous research has demonstrated that many factors are related to caregiver outcomes. Evidence suggests that caregiver burden is associated with care recipient-related factors, including the severity of the injury (Bayen et al., 2016; Doser & Norup, 2016; Manskow et al., 2015), level of functional disability (Davis et al., 2009; Roopchand-Martin & Creary-Yan, 2014; Zhu & Jiang, 2018), age (Ilse et al., 2008; Rigby et al., 2009a), and gender (Rigby et al., 2009a). Caregiver-related factors, including the amount of time and effort spent caregiving (Doser & Norup, 2016; Rigby et al., 2009b), unmet needs (Doser & Norup, 2016), gender (Roopchand-Martin & Creary-Yan, 2014), and age (Kruithof et al., 2016; Nabors et al., 2002), have also been associated with caregiver burden. Some studies have also demonstrated an association between caregiver burden and other factors such as availability of social support in the family (Davis et al., 2009; Manskow et al., 2015), and kinship between the care recipient and the caregiver (Tramonti et al., 2015; Doser & Norup, 2016). Nevertheless, findings on predictors of caregiver burden are inconsistent and little systematic information is available on the topic. Previously, research on predictors of caregiver burden has focused on caregivers of individuals with either TBI or nTBI. Despite different etiologies, these injuries have overarching similarities that make their consequences comparable. Consequently, a scoping review integrating current evidence regarding predictors of caregiver burden in caregivers of individuals with TBI or nTBI will provide an overview of the current knowledge and is therefore needed. Knowledge about specific predictors of caregiver burden is important, as it will enable identification of caregivers at risk of experiencing high caregiver burden. It is of the utmost importance to identify vulnerable caregivers as early as possible to be able to support them and provide appropriate interventions aiming at reducing potential risk factors and improving their well-being (Rottmann et al., 2022). By identifying caregivers at risk early on, the potential negative consequences of caregiving can possibly be prevented. Therefore, the aim of this scoping review was to examine predictors of caregiver burden in caregivers of individuals with TBI or nTBI in order to provide an overview of the available evidence and thus obtain more comprehensive and systematic information on the topic.
2Methods
A review protocol was developed based on Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR) Checklist (Tricco et al., 2018).
2.1Eligibility criteria
Studies were included if they: (1) investigated predictors of caregiver burden in caregivers of adult (≥15) individuals with TBI or nTBI. Caregivers were defined as the primary, informal caregivers of the individual with the injury. This definition excluded formal caregivers such as nurses or health care professionals at rehabilitation facilities; (2) had a quantitative study design, including longitudinal and cross-sectional studies; and (3) were conducted in Europe, the United States of America, or Australia. This inclusion criterion was added to prevent cultural biases from interfering with the generalizability of the results, as there are large differences in welfare and health care policies across countries worldwide due to both structural and cultural factors (Johnsen & Grønbæk, 2022). Literature reviews and studies investigating the effect of an intervention targeting caregiver burden were excluded.
2.2Information sources and search strategy
The main search for literature was conducted in the bibliographic databases PubMed, EMBASE (Ovid) and APA PsycInfo (EBSCO). Search terms in the database APA PsycInfo (EBSCO) included: ‘acquired brain injur*’, ‘traumatic brain injur*’, ‘brain injur*’, ‘non-traumatic brain injur*’, or ‘stroke’ combined with ‘burden’, ‘caregiver burden’, ‘perceived burden’ or ‘caregiver strain’. In the databases PubMed and EMBASE (Ovid), the term ‘burden’ was not included. The search was limited to articles written in English and published in academic journals between 2000 and March 2022. EndNote was used to manage the references and identify duplicates.
2.3Selection of sources of evidence
The first and second authors independently screened titles and abstracts for assessment in relation to the eligibility criteria. This process was conducted using Covidence Systematic Review Software (2021). Divergences were resolved through discussion. The first author read full-text articles and listed reasons for exclusion of the ineligible studies in accordance with the PRISMA-ScR Checklist (Tricco et al., 2018).
2.4Data items and data charting process
Data from eligible studies were charted using a charting table (Table 1) developed for the present study. The charting table captured relevant information on study characteristics, participant characteristics, outcome measures, and key findings. In the charting table, studies were categorized according to study design (longitudinal or cross-sectional) to encompass the differing designs. Two authors charted data from the included studies. Disagreements were resolved through discussion.
Table 1
Study characteristics and key findings
| First author, year, country | Caregiver demographics | Care recipient demographics | Time since injury/ time of follow-up | Etiology and severity of injury | Outcome measures (burden /predictors) | Key findings of relevance to this review |
| Cross sectional studies | ||||||
| Achilike (2020) USA | 88 caregivers Average age 54.3±13.7 69% female 31% male | Average age 63.9±15.2 53% female 47% male | <6 months (63%) ≥6 months (38%) | Stroke, type of stroke NA | ZBIB Predictors: PHQ-9B, BIB | Higher burden was associated with care recipient functional disability and caregiver depressive symptoms. No association between caregiver gender and burden |
| Arnould (2015) France | 68 caregivers Average age NA Sex ratio NA | Average age 35.6±13.7 83.8% female 16.2% male | 3–120 months Mean = 38.85± 29.47 | Severe TBI | ZBIB Predictors: AIB, SPRSB | Higher burden was associated with care recipient apathy, including lack of initiative and emotional blunting and lower psychosocial functioning in the care recipient. Care recipient age, education level, and time since injury did not correlate significantly with burden |
| Bayen (2013) France | 66 caregivers Average age NA Sex ratio NA | Average age 38.1±17.9 21% female 79% male | 1 year | Severe TBI | ZBIaB Predictors: DEXB, GCSC, GOSA, GOS-EA, ISSC, SF-36B | Higher burden was associated with care recipient global disability and executive dysfunction. Care recipient age, injury severity, and professional status did not correlate significantly with caregiver burden |
| Bergström (2011) Sweden | 81 caregivers Average age NA Median age = 66, range 19–84 70% female 30% male | Average age NA Median age = 71, range 32–93 33% female 67% male | 1 year | Stroke, 86% Ischemic 14% Hemorrhagic | CBB Predictors:LiSat-9A,B, SISA | Higher burden was associated with care recipient lower life satisfaction and caregivers’ low life satisfaction, and combined life satisfaction of the two |
| Davis (2009) USA | 114 caregivers Average age 45.7±12.3 85.8% female 24.2% male | Average age NA Sex ratio NA | 1–2 years Mean = 12.71 months±2.82 months | Moderate to severe TBI | PBS of MCASB Predictors: DRSB, WOCQB, MSPSSB, BSIB | Higher burden was predicted by care recipient disability, caregivers’ use of the escape-avoidance coping style, and lower perceived social support |
| Doser (2016) Denmark | 44 caregivers Average age 53.2±12.3 75% female 25% male | Average age 42.9±20.1 31.8% female 68.2% male | 3–6 years Mean = 64.6 months±15.9 months | Severe TBI (75%) and nTBI (25%) | CBB Predictors: GOATC, FNQB | Higher burden was associated with spousal caregivers, more severe injuries, more time spent caregiving, and more unmet needs |
| Jaracz (2012) Poland | 150 caregivers Average age 53.5±13.8 83% female 17% male | Average age 64.0±12.6 47% female 53% male | 6 months post discharge | Stroke, type of stroke NA | CBB Predictors: HADSB, PSSB, SOCB, SSSC, GDSNNA, BINA | Higher burden was associated with lower sense of coherence, higher emotional distress, lower care recipient’s functional status, and more time spent caregiving. Care recipient age and social support did not directly influence caregiver burden |
| Machamer (2002) USA | 180 caregivers Average age 45±12,8 77% female 23% male | Average age 35±16 Sex ratio NA | 6 months | Moderate to severe TBI | ZBIB Predictors: CES-DB, FSEA,B, GCSC, WAISC, | Higher burden was associated with injury severity, worse neuropsychological functioning, increased dependency, behavioral changes, caregiver depression, more time spend assisting the care recipient in ADL, and giving up own activities. No significant association between burden and relation to the care recipient, caregiver age, gender, number of years the care recipient and caregiver had known each other, current living situation, and frequency of contact |
| Manskow (2015) Norway | 92 caregivers Average age NA 75 % female 25% male | Average age 38.7±18.2 13% female 87% male | 1 year | Severe TBI | CBB Predictors: GCSC, GOS-EA, ISSaC, LCFSC, ISSC | Higher burden was associated with caregivers’ perceived loneliness, more severe care recipient disability, marital status (married), and low frequency of meeting friends. No significant relation between burden and severity- and type of injury, care recipient age/gender, and caregiver age/gender |
| Nabors (2002) USA | 45 caregivers Average age 51±12.69 91% female 9% male | Average age 36 26.7% female 73.3% male | Mean = 29.79 months (2.5 years) | TBI | HI-FIB, FNQB, FADB Predictors: HI-FIB, FNQB, FADB, NONB | Higher burden was associated with more unmet needs met and higher importance of needs. Younger caregiver age and lower education level was related to cognitive burden, and care recipient post injury employment, and social support was related to affective/behavioral caregiver burden |
| Oosterveer (2014) The Netherlands | 179 caregivers Average age NA Sex ratio NA | Average age 68.8 years in the non-strain group 70.1 in the high-strain group 38.5% female 61.5% male | 6 weeks after discharge | Stroke, 93% Ischemic 7% Hemorrhagic | CSIB Predictors: BIC, BBSC, MRSC, FSSA, HADSA, LiSat-9A, FAIA | Higher burden was associated with care recipient anxiety and low life satisfaction. Burden was unrelated to care recipient gender and age at stroke onset, type of stroke, and the absence of stairs in the care recipient’s house |
| Rigby (2009) England | 298 caregivers Average age NA Sex ratio NA | Average age 73 41.3% female 58.7% male | 1 year | Stroke, 77.4% Ischemic, 13.5% transient ischemic attack, 9% Hemorrhagic | RSSA, BCOSA Predictors: BIC, OHSC, MRSNA, MFISNA, GDSC, SF-36A | Higher burden was associated with older care recipient age, male gender, ischemic stroke, urinary incontinence, impaired clock drawing, poor mental health, functional handicap, and functional disability |
| Tramonti (2015) Italy | 30 caregivers Average age 63.2±13.2 (female caregivers) 55.9±12.1 (male caregivers) 66.6% female 33.3% male | Average age 60.9±17.8 46.7% female 53.3% male | Mean = 3 months (range 1–8 months) | Severe TBI | CBIB Predictors: FACES IIIB, MSPSSB, SEIQoLB | Higher time-dependent burden was associated with spousal caregivers compared to adult children, while adult children scored higher on emotional burden compared to spouses. Social support did not correlate significantly with burden |
| Wu (2019) The Netherlands | 60 caregivers Average age 59.18±10.45 67% female 33% male | Average age 65.87±13.23 Sex ratio NA | 6 months | Stroke, 73% Ischemic | ZBIB Predictors: DAS-7B, CCIC, D-KEFSC, FIMC, NIHSSC | Higher burden was predicted by poor relationship consensus. Burden was unrelated to relationship cohesion and satisfaction, care recipient age, gender, comorbidity, cognitive fluency, and the gender and self-reported health of the caregiver |
| Longitudinal studies | ||||||
| Bayen (2016) France | 39 caregivers at baseline, 98 caregivers at 1-year assessment Average age NA 81% female 19% male | Average age at 4-year follow-up 37.2±13.3 20% female 80% male | 1 and 4 years | Severe TBI | ZBIaB Predictors: GOS-EA, BIC, DEXA, NRS-rC, HADSA | Higher burden was associated with poorer GOS-E scores, more NRS-r disorders, drug/alcohol abuse, involvement in litigation, and no-coresidency status. Burden was unrelated to care recipient gender and educational level |
| Blake (2003) England | 116 caregivers at both assessments Average age 66.4±10.8 72% female 28% male | Average age 68.6±10.5 28% female 72% male | 3 and 6 months | Stroke, type of stroke NA | CSIB Predictors: GHQ-12B, EADLB, PANASB | Higher burden was associated with care recipient functional disability, low mental health, and caregiver negative affectivity and low mood. No significant differences on burden level between male and female spouses |
| Ilse (2008) Belgium | 90 caregivers were assessed at all three points Average age NA 67% female 33% male | Average age 67.3±11.2 Sex ratio NA | 2, 4 and 6 months | Stroke, type of stroke NA | CSIB Predictors: RMAC, BIC, NEADLC, MRSC, HADSA, NIHSSC, SIPC | Higher burden at 2-months was associated with care recipient disability, dependence in ADL, younger care recipient age and incontinence. Higher burden at 4-months was related to younger care recipient age and dependency in ADL. Burden at 6-months was related to dependency in ADL and disability |
| Jaracz (2015) Poland | 150 caregivers at 6-months follow-up 88 caregivers at 5-years follow-up Average age at baseline 53.6% ±12.1 83% female 17% male | Average age at baseline 61.1±12.2 43.2% female 56.8% male | 6 months and 5 years | Stroke, type of stroke NA | CBB Predictors: BINA, GDSNA, HADSB, SOCB, PSSB | Higher burden was associated with caregivers’ low sense of coherence and more caregiving time 6-months post stroke, and with caregiver anxiety 5-years post stroke. Burden was unrelated to care recipient age, gender, depression, and caregiver age, gender, relation to the care recipient, and social support |
| Kruithof (2016) The Netherlands | 172 caregivers at baseline assessment, 183 caregivers at 1-year follow-up Average age 62.5±10.9 at baseline 78.7% female 21.3% male | Average age 64.1±11 at baseline Sex ratio NA | 2 months and 1 year | Stroke, 95.1% Ischemic | CSIB Predictors: HADSA,B, UPCCB, GSESB, SSLI-12B, NIHSSC, BINA, MoCaNA | Higher burden was associated with younger caregiver age, less relationship satisfaction, high self-efficacy, anxiety, and care recipient’ stroke severity and depression 2-months post stroke. 1-year post stroke, predictors of burden were level of burden 2-months post stroke, care recipients lower cognitive functioning and symptoms of anxiety |
| Manskow (2017) Norway | 119 caregivers at 1-year follow-up 80 caregivers at 2-year follow-up Average age NA 77.3% female 22.7% male | Average age 39.4±19.19 Sex ratio NA | 1 and 2 years | TBI | CBB Predictors: AISC, GCSC, GOS-EA | Higher burden was predicted by loneliness from 1–2 years post injury. Burden was not significantly related to caregiver gender, care recipient age, and level of functioning |
| Marsh (2002) New Zealand | 52 caregivers at both assessments Average age 43±9 88% female 12% male | Average age 28±11 19% female 81% male | 6 months and 1 year | Severe TBI | CQ (designed for the study)B Predictors: BDIB, TAIB, SASB, HIBRSB | Higher burden scores were explained by more physical changes, behavioral problems, and less social contact 6 months post injury. Higher burden was explained by cognitive changes at 1-year post injury, behavioral changes, and less social contact |
| Pont (2018) The Netherlands | 129 caregivers. 72 caregivers at both time points Average age NA Median age = 59 68.2% female 31.8% male | Average age NA Median age = 61 38% female 62% male | 6 and 12 months | Stroke, 78.6% Ischemic | CSIB | Higher burden at any time point correlated with living together with the care recipient and stroke etiology |
| Pucciarelli (2018) Italy | 244 caregivers at baseline, 133 completed all assessments Average age at baseline 53±13 65% female 35% male | Average age at baseline 71±12 50% female 50% male | 3, 6, 9 and 12 months | Stroke, 79% Ischemic | CBIB Predictors: HADSNA, BINA, CCINA | Higher burden was predicted by caregiver male gender, not cohabiting and care recipient lower physical functioning. No significant associations between burden and care recipient age, gender, care recipient comorbid conditions, and caregiver age and educational level |
| Tooth (2005) Australia | 71 caregivers at baseline, 57 at 12 months’ follow-up Average age 60.4±14.9 72% female 28% male | Average age 68.5±12.8 39% female 61% male | 6 and 12 months after discharge from hospital | Stroke, 92% Ischemic 8% Hemorrhagic | CSIB and CBIB Predictors: FIMA,B, SF-36A,B | Higher burden was associated with poorer care recipient mental health, caregivers having other caregiving roles, caregiver employment, more personal supports, higher perceived quality of social support, and care recipient receiving outpatient therapy and community service. Improved motor function resulted in decreased burden from 6–12 months |
Source of outcome: ACare recipient report, BCaregiver report, CClinician report. Abbreviations: Abbreviated Injury Severity scale (AIS), Activities of Daily Living (ADL), Apathy Inventory (AI), Bakas Caregiver Outcome Scale (BCOS), Barthel Index (BI), Beck Depression Inventory (BDI), Berg Balance Scale (BBS), Berlin Perceived Social Support Scale (PSS), Brief Symptom Inventory (BSI), Caregiver Burden Inventory (CBI), Caregiver Burden scale (CB), Caregiver Strain Index (CSI), Caregiver Questionnaire (CQ), Center for Epidemiologic Studies-Depression scale (CES-D), Charlson Comorbidity Index (CCI), Delis-Kaplan Executive Function System (D-KEFS), Disability Rating Scale (DRS), DysExecutive Questionnaire (DEX), Frenchay Activities Index (FAI), Family Adaptivity and Cohesion Evaluation Scales III (FACES III), Family Assessment Device (FAD), Family Needs Questionnaire (FNQ), Functional Independence Measure (FIM), Fatigue Severity Scale (FSS), Functional Status Examination (FSE), Galveston Orientation and Amnesia Test (GOAT), General Health Questionnaire-12 (GHQ-12), General Self-Efficacy Scale (GSES), Geriatric Depression Scale (GDS), Glasgow Coma Scale (GCS), Glasgow Outcome Scale (GOS), Glasgow Outcome Scale-Extended (GOS-E), Global Deterioration Scale (GlDS), Head Injury Behavior Rating Scale (HIBRS), Head Injury Family Interview (HI-FI), Hospital Anxiety and Depression Scale (HADS), Injury Severity Scale (ISSa), Injury Severity Score (ISS), International Classification of Functioning (ICF), Life Satisfaction Questionnaire (LiSat-9), Modified Caregiver Appraisal Scale (MCAS), Modified Fatigue Impact Scale (FIS), Modified Rankin Scale (MRS), Montreal Cognitive Assessment (MoCa), Multidimensional Scale of Perceived Social Support (MSPSS), National Institute of Health Stroke Scale (NIHSS), Non-traumatic brain injury (nTBI), Nottingham Extended Activities of Daily Living (NEADL), Neurobehavioral Rating Scale-revised (NRS-r), Non-Support Scale (NON), Not applicable (NA), Oxford Handicap Scale (OHS), Patient Health Questionnaire-9 (PHQ-9), Perceived Burden Subscale (PBS), Positive and Negative Affectivity Schedule (PANAS), Relatives Stress Scale (RSS), Rancho Levels of Cognitive Functioning (LCFS), Rivermead Motor Assessment (RMA), Scandinavian Stroke Scale (SSS), Schedule for the Evaluation of Individual Quality of Life (SEIQoL), Sense of Coherence Scale (SOC), Sickness Impact Profile (SIP), Social Adjustment Scale (SAS), Social Support List-Interaction (SSLI-12), Stroke Impact Scale (SIS), Sydney Psychosocial Reintegration Scale (SPRS), Trait Anxiety Inventory (TAI), Traumatic brain injury (TBI), Utrecht Proactive Coping Competence Scale (UPCC), Ways of Coping Questionnaire (WOCQ), Wechsler Adult Intelligence Scale (WAIS), Zarit Burden Interview Scale (ZBI), Zarit Burden Inventory (ZBIa).
2.5Synthesis of results
The predictors of caregiver burden identified in the eligible studies were summarized according to whether they were related to: 1) the care recipient; 2) the caregiver; or 3) other factors. A narrative synthesis of the results of the studies were undertaken, and the results are presented in a narrative format.
3Results
3.1Selection of sources of evidence
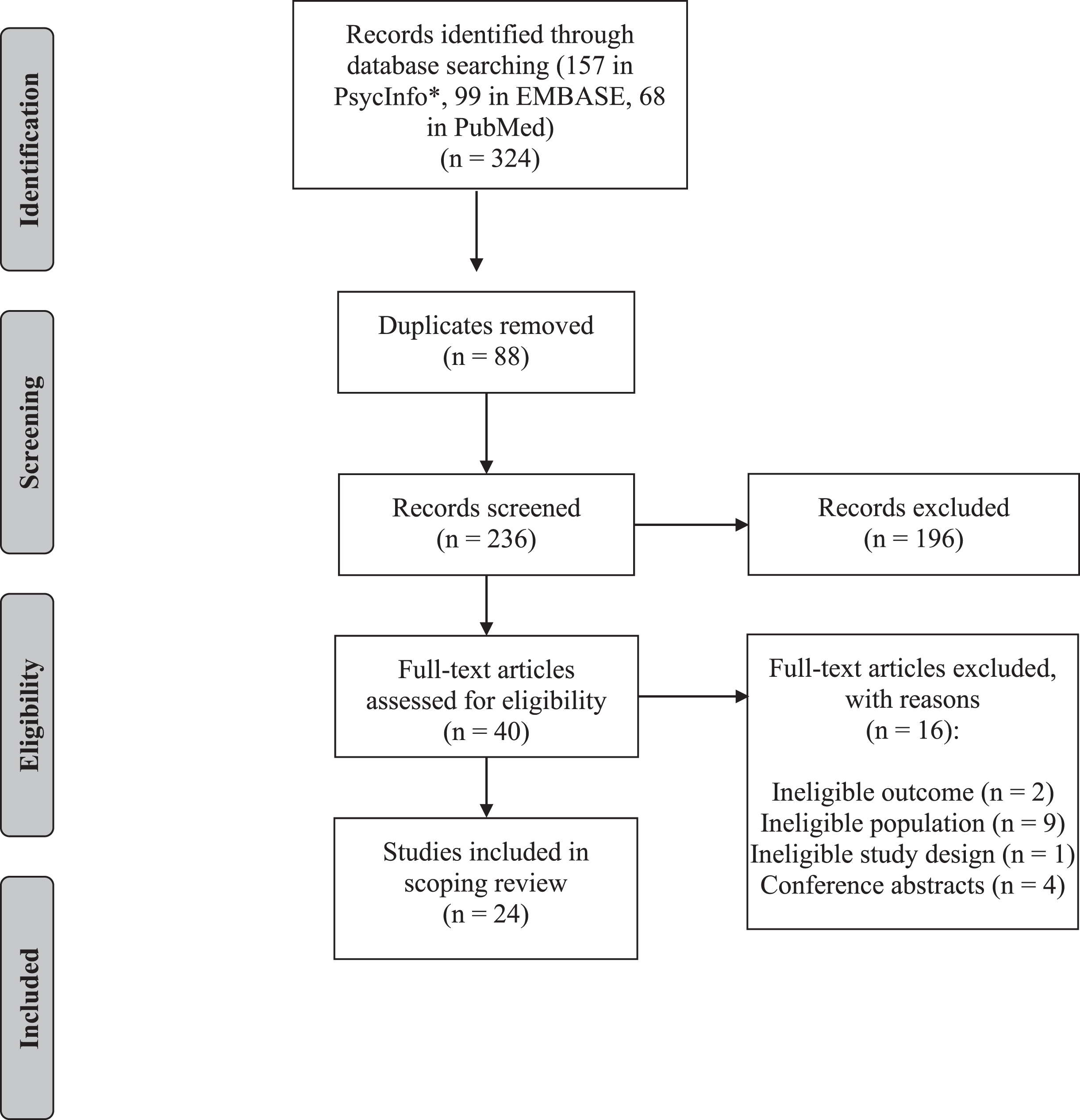
The main search yielded 324 articles. Of these articles, 157 were identified in APA PsycInfo (EBSCO), 99 in EMBASE (Ovid), and 68 in PubMed. After duplicates were removed, 236 articles were screened based on the relevance of their title and abstract. During the screening of titles and abstracts, 196 articles were excluded. The remaining 40 articles were read as full texts. A total of 24 articles met the eligibility criteria and were included in the scoping review. The selection process and the reasons for exclusion of ineligible studies are depicted in Fig. 1.
Fig. 1
PRISMA flowchart.
3.2Characteristics of sources of evidence
Table 1 presents a summary of data on first author, year of publication, country of publication, study design, caregiver demographics, care recipient demographics, time since injury, etiology and severity of injury, outcome measures, and key findings. Included papers were conducted in the United States (n = 4), The Netherlands (n = 4), England (n = 2), France (n = 3), Italy (n = 2), Norway (n = 2), Poland (n = 2), Australia (n = 1), Belgium (n = 1), Denmark (n = 1), New Zealand (n = 1), and Sweden (n = 1). Studies were published between 2002 and 2020. Of the 24 included studies, 14 had a cross-sectional design, while 10 had a longitudinal design (Table 1).
3.3Synthesis of results
3.3.1Care recipient-related predictors of caregiver burden
3.3.1.1 Care recipient demographics. Several studies investigated the association between caregiver burden and sociodemographic variables related to the care recipient, and discrepancies were found. Nine studies (Arnould et al., 2015; Bayen et al., 2013, 2016; Jaracz et al., 2012, 2015; Manskow et al., 2015, 2017; Oosterveer et al., 2014; Pucciarelli et al., 2018) reported no significant association between care recipient age and caregiver burden, and two studies (Ilse et al., 2008; Rigby et al., 2009a) found an association. However, the two studies found conflicting results. Ilse et al. (2008) found that younger care recipient age predicted caregiver burden, whereas Rigby et al. (2009a) found that older care recipient age predicted caregiver burden. In the two studies that reported an association, the main part of the caregivers were spouses (61–66%). The average age of the care recipients in these two studies were higher than in the studies that reported no association, with a mean care recipient age of 67.3 and 73, respectively. The mean age of the care recipients in the studies that did not report an association ranged from 35.6 to 71.
With regards to the relation between care recipient gender and caregiver burden, six studies (Bayen et al., 2013; Jaracz et al., 2015; Manskow et al., 2015, 2017; Oosterveer et al., 2014; Pucciarelli et al., 2018) found no significant relation, while Rigby et al. (2009a) found that caregivers experienced higher caregiver burden when caring for a male care recipient. Furthermore, evidence was mixed with regards to care recipient educational level and professional status (see Table 1).
3.3.1.2 Injury severity. Five studies explored whether injury severity had an impact on caregiver burden. Three of these studies (Doser & Norup, 2016; Kruithof et al., 2016; Machamer et al., 2002) found that more severe injuries led to a higher caregiver burden in caregivers of individuals with either TBI or nTBI. Two studies (Bayen et al., 2013; Manskow et al., 2015) found no association between injury severity and caregiver burden. The two studies that reported no association investigated caregivers of individuals with TBI. The three studies that did report an association investigated caregivers of individuals with stroke (Kruithof et al., 2016), TBI (Machamer et al., 2002), or both TBI and nTBI (Doser & Norup, 2016). All studies used clinician-reported measures of injury severity (see Table 1). Overall, most of the studies reported that more severe injuries were associated with higher caregiver burden.
3.3.1.3 Functional disability. Evidence was rather consistent with respect to the impact of functional disability on caregiver burden. Fifteen studies found that poorer functional outcomes in different aspects of care recipient functioning were related to higher caregiver burden, including impaired physical functioning and impaired neuropsychological functioning. Specifically, studies found that higher caregiver burden was associated with lower levels of global functioning (Bayen et al., 2013, 2016; Blake et al., 2003; Davis et al., 2009; Manskow et al., 2015), dependency in activities of daily living (Achilike et al., 2020; Ilse et al., 2008; Jaracz et al., 2012; Pucciarelli et al., 2018; Rigby et al., 2009a), impaired motor function (Tooth et al., 2005), worse neuropsychological status (Machamer et al., 2002), impaired cognitive functioning (Kruithof et al., 2016; Marsh et al., 2002; Rigby et al., 2009a), behavioral changes (Marsh et al., 2002), cognitive-behavioral disturbances (Bayen et al., 2016), executive dysfunction (Bayen et al., 2013), and symptoms of apathy (Arnould et al., 2015). Additionally, one study (Tooth et al., 2005) demonstrated that when care recipients received outpatient therapy or community services, caregiver burden was higher. By contrast, two studies did not find an association between functional disability and caregiver burden (Jaracz et al., 2015; Manskow et al., 2017).
3.3.1.4 Care recipient mental health. Five studies demonstrated that factors related to the care recipient’s mental health were associated with caregiver burden, including worse overall mental health (Rigby et al., 2009a; Tooth et al., 2005), anxiety (Kruithof et al., 2016; Oosterveer et al., 2014), depression (Kruithof et al., 2016), and low life satisfaction (Bergström et al., 2011; Oosterveer et al., 2014). According to one study (Jaracz et al., 2015), depression in the care recipient was not associated with burden. However, care recipients’ mental health was quite consistently linked with caregiver burden, implying that poor mental health in the care recipient has a negative impact on the caregiver.
3.3.1.5 Substance abuse. As the sole study, Bayen et al. (2016) found an association between care recipients’ drug or alcohol abuse and higher caregiver burden.
3.3.2Caregiver-related predictors of caregiver burden
3.3.2.1 Caregiver demographics. Several studies investigated the association between caregiver burden and sociodemographic variables related to the caregiver. Three studies (Jaracz et al., 2015; Machamer et al., 2002; Pucciarelli et al., 2018) reported no significant correlation between caregiver age and caregiver burden. By contrast, two studies (Kruithof et al., 2016; Nabors et al., 2002) suggested that younger caregivers experienced higher burden. Likewise, evidence was mixed with respect to the relation between caregiver gender and caregiver burden. Six studies (Achilike et al., 2020; Blake et al., 2003; Jaracz et al., 2015; Machamer et al., 2002; Manskow et al., 2015, 2017) found no association, while one study (Pucciarelli et al., 2018) found that male caregivers experienced higher burden in comparison to female caregivers. Furthermore, one study (Manskow et al., 2015) found that caregiver marital status (married) was associated with a higher caregiver burden. Additionally, the results of one study (Pucciarelli et al., 2018) indicated that caregiver burden and caregiver educational level was unrelated, whereas another study (Nabors et al., 2002) found that lower years of education led to higher caregiver burden.
3.3.2.2 Time spent caregiving. Evidence was consistent with respect to the association between time spent on caregiving and caregiver burden. Three studies (Doser & Norup, 2016; Jaracz et al., 2015, 2012) reported that more time spent on caregiving was related to a more substantial caregiver burden. Also, caregivers, who reported giving up their own activities to care for the care recipient, reported higher burden (Machamer et al., 2002). Additionally, one study (Tooth et al., 2005) demonstrated that having other caregiving roles (e.g. caring for children) increased burden.
3.3.2.3 Caregiver mental health. Seven studies demonstrated associations between factors related to caregiver mental health and caregiver burden, including emotional distress (Jaracz et al., 2012), caregiver anxiety (Jaracz et al., 2015; Kruithof et al., 2016), depressive symptoms (Achilike et al., 2020; Machamer et al., 2002), low life satisfaction (Bergström et al., 2011), and low caregiver mood and negative affectivity (Blake et al., 2003). These results indicate that caregivers are at higher risk of burden when they experience problems related to mental health.
3.3.2.4 Unmet needs. Two studies (Doser & Norup, 2016; Nabors et al., 2002) found that caregivers, who reported that their needs were not met, experienced higher caregiver burden.
3.3.2.5 Coping strategies and self-efficacy. One study (Davis et al., 2009) investigated the relationship between different coping strategies and caregiver burden and found that use of the coping strategy escape-avoidance was associated with burden. Additionally, one study (Kruithof et al., 2016) established a relation between high self-efficacy in caregivers and caregiver burden.
3.3.2.6 Sense of coherence. Two studies (Jaracz et al., 2012; Jaracz et al., 2015) found that a higher sense of coherence in the caregiver was related to diminished caregiver burden. Sense of coherence was defined as a perception of having the resources to meet the demands of the environment, and a feeling of structure and predictability of the inner and outer environment (Jaracz et al., 2012).
3.3.3Other predictors of caregiver burden
3.3.3.1 Time since injury. Arnould et al. (2015) investigated the relationship between time since injury and burden without finding an association.
3.3.3.2 Social support. Several studies investigated the association between social support and caregiver burden, and the evidence was mixed. Five studies (Davis et al., 2009; Manskow et al., 2017, 2015; Marsh et al., 2002; Nabors et al., 2002) reported that more social support or lower perceived loneliness in either the caregiver or the care recipient resulted in less experienced burden. In contrast to these findings, Tooth et al. (2005) found that higher perceived quality of social support correlated with higher burden. Three studies (Jaracz et al., 2012, 2015; Tramonti et al., 2015) found no significant relationship between social support and caregiver burden.
3.3.3.3 The care recipient-caregiver relationship. Some studies investigated the association between caregiver burden and factors linked to the care recipient-caregiver relationship. According to Doser & Norup (2016), spouses experienced higher burden compared to parents. Likewise, Tramonti et al. (2015) found that spouses experienced higher levels of time-dependent burden, while adult children experienced higher levels of emotional burden. Two studies (Jaracz et al., 2015; Machamer et al., 2002) reported no significant differences. The results of two studies (Pucciarelli et al., 2018; Bayen et al., 2016) indicated that when the caregiver and the care recipient were not living together, the caregiver experienced higher levels of burden. By contrast, Pont et al. (2018) reported that caregivers living with the care recipient experienced higher levels of burden. Machamer et al. (2002) reported that there were no significant differences in caregiver burden, current living situation, frequency of contact, and the number of years the caregiver and the care recipient with TBI had known each other. Furthermore, one study (Krutihof et al., 2016) found that caregivers who reported less satisfaction with their relationship to the care recipient reported a higher burden. Conversely, Wu et al. (2019) found no association between these variables. However, Wu et al. (2019) found that lower relationship consensus determined a higher caregiver burden. Relationship consensus was characterized by agreement of goals and expectations between the dyad (Wu et al., 2019).
3.3.3.4 Involvement in litigation. Involvement in litigation was a predictor of a higher caregiver burden in the study of Bayen et al. (2016).
4Discussion
4.1Summary of evidence
The aim of the present scoping review was to examine predictors of caregiver burden in caregivers of individuals with TBI or nTBI. Twenty-four studies investigating predictors of caregiver burden were identified and results were synthesized. The main findings were that caregivers were at higher risk of experiencing caregiver burden when the care recipient sustained a more severe injury, experienced more functional disabilities, including decreased physical and neuropsychological functioning, and mental health problems, including worse overall mental health, anxiety, and low life satisfaction. Furthermore, caregivers were at increased risk of experiencing caregiver burden when spending more time on caregiving, reporting more unmet needs, and experiencing mental health problems, including anxiety, depression, low life satisfaction, low caregiver mood and negative affectivity. The results highlight several areas of potential intervention to prevent caregiver burden.
4.2Discussion of main findings
4.2.1Care recipient-related predictors of caregiver burden
4.2.1.1 Injury severity. The comparison of findings on the relation between injury severity and caregiver burden across studies are complicated by differences in injury etiology and consequently differences in outcome measures. Kruithof et al. (2016) longitudinally investigated the impact of stroke severity on caregiver burden in a large sample of 183 caregivers, measured with the National Institutes of Health Stroke Scale (Brott et al., 1989). The authors found that stroke severity predicted caregiver burden 2-months post stroke, but the association was no longer present 1-year post stroke. Machamer et al. (2002) found that caregiver burden was associated with higher scores on the Glasgow Coma Scale (GCS; Teasdale & Jennett, 1974) at 6-months post-TBI in a sample of 180 caregivers. The GCS measures level of consciousness and has proven to be a valid indicator of injury severity. Doser & Norup (2016) found that injury severity was associated with caregiver burden as much as 3–6 years post-injury in a small sample of 44 caregivers of individuals with nTBI or TBI. In the study by Doser & Norup (2016), length of post-traumatic amnesia (PTA) was used as an indicator of injury severity measured by a neuropsychologist using the Galveston Orientation and Amnesia Test (Levin et al., 1979). Two studies (Bayen et al., 2013; Manskow et al., 2015) did, however, not find an association between injury severity and caregiver burden. Bayen et al. (2013) investigated a sample of 66 caregivers of individuals with TBI 1-year post injury. Manskow et al. (2015) investigated a sample of 92 caregivers of individuals with TBI and found no relation between injury severity and caregiver burden. Both studies applied the Injury Severity Scale (Baker et al., 1974), a clinically validated measure of the severity of global body injury that provides an overall score for patients with multiple injuries in six body regions. It is possible that differences in injury etiology or outcome measures account for the differences in findings. Furthermore, measures of injury severity can be directly associated with the levels and types of functional disability that individuals with brain injury experience, which further complicates the interpretation of these findings. Therefore, further research is needed to draw a conclusion with greater certainty, and to elucidate whether the relation between injury severity and caregiver burden is mediated by injury etiology or level of functional disability. However, most evidence indicated that injury severity was associated with a higher caregiver burden, which stresses the importance of providing support for caregivers caring for individuals with more severe injuries.
4.2.1.2 Functional disability. Across the 15 studies that found an association between functional disability and caregiver burden, a vast amount of different measures of functional disability were applied. The most commonly applied measure was the Barthel Index (BI; Mahoney & Barthel, 1965), and six studies used the BI, which is a clinically validated instrument measuring the care recipient’s dependency in activities of daily living, including eating, bathing, dressing, etc. It is one of the most widely applied measures to assess care recipients’ independence in activities of daily living. According to five studies investigating caregivers of individuals with stroke (Achilike et al., 2020; Ilse et al., 2008; Jaracz et al., 2012; Pucciarelli et al., 2018; Rigby et al., 2009a), greater dependence in daily living measured with the BI predicted a higher caregiver burden. Furthermore, three studies (Bayen et al., 2013, 2016; Manskow et al., 2015) found that care recipient functional disability, measured with the Glasgow Outcome Scale-extended (GOS-E; Wilson et al., 1998), predicted caregiver burden in caregivers of individuals with TBI. The GOS-E evaluates global function through a structured interview. Likewise, Davis et al. (2009) found that lower levels of global functioning in individuals with TBI predicted caregiver burden in 114 caregivers, measured with the Disability Rating Scale, an instrument with good psychometric properties (Hall et al., 1985). Furthermore, Tooth et al. (2005) found that improved motor function resulted in decreased caregiver burden from 6–12 months post stroke, measured by a clinically validated instrument, the Functional Independence Measure (FIM) (Hamilton et al., 1994). Several studies investigated functional disability through caregiver-reports (see Table 1). Former research shows that the emotional involvement of the caregiver related to burden can negatively or positively skew the caregiver’s perception of the functioning level of the care recipient (Denckla, 2002; Rosenberg et al., 2005). Thus, caregiver-report measures can cause bias compared to objective clinician-reported measures of functional disability, and results of studies relying on caregiver-report only should therefore be interpreted with caution. Nonetheless, the evidence strongly suggests that global functional disability, including greater dependence in daily living and more severe disabilities and impairments, leads to higher levels of caregiver burden. The studies established an association between functional disability and caregiver burden both in the early stages of injury, as early as 2-months post injury (Ilse et al., 2008), and in the later stages, as much as 4 years after injury (Bayen et al., 2016). As functional disabilities are often associated with a reduction of the care recipient’s independence, a higher level of disabilities can increase the need for support from the caregiver. These results emphasize the importance of rehabilitation of both physical and cognitive functions, as this is not only essential for the individual with the injury but could potentially alleviate caregiver burden. Providing care recipients with more self-management training could increase their independency and consequently alleviate the burden placed on the caregiver.
Seven studies specifically examined the impact of neuropsychological functioning on caregiver burden. These studies used a variety of study designs and outcome measures, but all studies found that when care recipients exhibited problems with neuropsychological functioning, caregiver burden tended to increase, both early on and long-term. Machamer et al. (2002) found that worse neuropsychological status at both 1-month and 6-months post-TBI predicted caregiver burden 6-months post injury in a sample of 180 caregivers. This study investigated neuropsychological status with a comprehensive battery of tests, including the Trail Making Test Parts A and B, the Selective Reminding Test Sum of Recall (SRTSR), and the Performance Intelligence Quotient (PIQ) of the Wechsler Adult Intelligence Scale (WAIS; Wechsler, 1981). Worse scores on all neuropsychological measures 1-month post injury correlated with higher caregiver burden 6-months post injury, while only the PIQ and the Trail Making Test Part A correlated significantly with caregiver burden 6-months post injury. According to Kruithof et al. (2016), lower levels of cognitive functioning predicted caregiver burden 1-year post stroke, measured with the Montreal Cognitive Assessment (MoCa). This instrument assesses the cognitive state in individuals with stroke. Bayen et al. (2013) investigated caregiver burden 1-year after TBI and found that executive dysfunction, including deficits in intentionality, inhibition, executive memory and affect regulation, were specifically related to subjective caregiver burden 1-year post injury. Likewise, Arnould et al. (2015) concluded that symptoms of apathy, including lack of initiative and emotional blunting in the care recipient, was associated with caregiver burden in 68 caregivers of individuals with TBI. Symptoms of apathy were measured with the Apathy Inventory, a clinically validated instrument showing good psychometric properties (Robert et al., 2002). Furthermore, Bayen et al. (2016) found that cognitive behavioral disturbances predicted caregiver burden as much as 4-years post injury, measured with the Neurobehavioral rating scale revised (Vanier et al., 2000). Rigby et al. (2009a) found that worse cognitive status at baseline predicted caregiver burden 1-year post stroke. A major strength of this study was the large sample size of 298 caregivers. However, cognitive status was measured with orientation and clock drawing tests only. Also, the authors examined caregiver burden with the Relatives Stress Scale (RSS; Greene et al., 1982) and the Bakas Caregiving Outcome Scale (BCOS; Bakas & Champion, 1999). The BCOS measures life changes that result from providing care, while the RSS measures the degree of stress and upset in caregivers, and this instrument was originally applied to a population of elderly with dementia. Considering this, the results of this study should be interpreted with caution. According to Marsh et al. (2002), behavioral changes predicted caregiver burden 6-months post injury, while behavioral changes and cognitive changes predicted caregiver burden 1-year post injury. However, this study used a non-validated measure of caregiver burden, the Caregiver Questionnaire, designed specifically for the study. The use of a non-validated measure of caregiver burden poses a problem of validity to the findings, as it can be questioned whether the applied instrument captures the construct ‘caregiver burden’. Also, meaningful comparisons of the predictors are complicated by the diversity of instruments. The studies have used both standard neuropsychological assessment as well as subjective rating scales, which give different perspectives on cognitive function. However, a majority of the studies have used more objective tests such as WAIS, MoCa, and consequently, the evidence consistently implies that worse neuropsychological functioning of the care recipient increases caregiver burden in caregivers of both individuals with TBI and nTBI in both early and later stages of injury. From a clinical point of view, these findings highlight the importance of systematic neuropsychological screening following TBI or nTBI in order to detect persisting problems with neuropsychological functioning. This would enable appropriate referral to specialized cognitive rehabilitation services. Additionally, delivering information- and education interventions to the caregiver aimed at enhancing their understanding of neuropsychological disturbances and care needs could help prepare them for the caregiving role (Revenson et al., 2016). Thus, caregiver burden might be prevented by adequate management of neuropsychological disorders combined with appropriate intervention and support for the caregiver.
4.2.1.3 Care recipient mental health. Five studies established an association between caregiver burden and mental health problems in the care recipient, including worse overall mental health, anxiety, and low life satisfaction. Rigby et al. (2009a) concluded that worse overall mental health measured with the mental health sub-category of the 36-item Short Form Health Survey (SF-36; Ware & Sherbourne, 1992) predicted caregiver burden 1-year post stroke in a large sample of 298 caregivers. Using the same instrument, Tooth et al. (2005) found that poorer care recipient mental health was the strongest predictor of caregiver burden both 6- and 12-months post stroke in a sample of 71 caregivers. Two studies found that low life satisfaction in the care recipient was related to higher burden. Oosterveer et al. (2014) demonstrated that lower life satisfaction predicted caregiver burden 6 weeks after discharge in a larger sample of 179 caregivers of individuals with stroke. Bergström et al. (2011) found that low life satisfaction predicted caregiver burden 1-year post stroke in a sample of 81 caregivers. Oosterveer et al. (2014) measured life satisfaction with the Life Satisfaction Questionnaire-9, while Bergström et al. (2011) applied the Life Satisfaction Checklist-11. Both instruments have been clinically validated and have good psychometric properties (Fugl-Meyer et al., 2002). Furthermore, Oosterveer et al. (2014) found that high levels of anxiety in the care recipient was related to caregiver burden as early as 6 weeks after discharge from hospital in 179 caregivers of individuals with stroke. In this study, anxiety was measured with the Hospital Anxiety and Depression Scale (HADS), a clinically validated questionnaire used for detecting anxiety and depression (Bocéréan & Dupret, 2014). Also using the HADS, a longitudinal study by Kruithof et al. (2016) demonstrated that caregiver burden was associated with care recipient anxiety 1-year post stroke. With regards to the relation between care recipient depression and caregiver burden, evidence was inconsistent. Kruithof et al. (2016) demonstrated that care recipient depression predicted caregiver burden 2-months post stroke, measured with the HADS. However, Jaracz et al. (2015) found no association between caregiver burden and care recipient depression in a sample of 150 caregivers of stroke individuals, measured with the Geriatric Depression Scale (van Marwijk et al., 1995). Thus, evidence is inconsistent with regards to the association between caregiver burden and care recipient depression, and future research should further elucidate this association. Furthermore, none of the five studies investigated caregivers of individuals with TBI. Therefore, more studies investigating the relation between caregiver burden and mental health in individuals with TBI are needed to confirm that these results apply to both caregivers of individuals with TBI and nTBI. Nonetheless, the evidence indicated that factors related to the care recipient’s mental health predicted caregiver burden both early after injury and in the chronic phase, including worse overall mental health, low life satisfaction, and anxiety. This stresses the importance of treating comorbid mental disorders in the individual who sustained the injury, as such disorders are not only distressing for the individual with the injury and a potential barrier to adherence to rehabilitation services, but they also serve as a source of burden for the caregiver.
4.2.2Caregiver-related predictors of caregiver burden
4.2.2.1 Time spent caregiving. Two cross-sectional studies (Doser & Norup, 2016; Jaracz et al., 2012) and one longitudinal study (Jaracz et al., 2015) reported that more hours spent caregiving or supervising the care recipient per day was related to a higher caregiver burden. Doser & Norup (2016) found that more time spent caregiving predicted caregiver burden as much as 3–6 years post-TBI or nTBI in a smaller sample comprising 44 caregivers. Jaracz et al. (2012) established an association between time spent caregiving and caregiver burden 6-months post stroke in a large sample of 150 caregivers. The study of Jaracz et al. (2015) had a longitudinal design and investigated the same cohort as Jaracz et al. (2012) across time points, and their results indicated that the association between more hours spent caregiving and caregiver burden was still evident 5-years post stroke. However, attrition was large in the study, compromising the strength of the results. Furthermore, data on 95 caregivers included in the study by Machamer et al. (2002) indicated that more personal activities given up by the caregiver to care for the care recipient was related to higher levels of burden 6-months post injury. Additionally, one study (Tooth et al., 2005) demonstrated that having other caregiving roles (e.g. caring for children) increased caregiver burden, but only on the ‘time burden’ dimension of the Caregiver Burden Inventory. Thus, evidence strongly suggests that caregivers who spend more hours caregiving and report giving up their own activities to care for the care recipient tend to experience larger caregiver burden in the early phases of rehabilitation continuing several years after the injury. Therefore, potential intervention to prevent caregiver burden could target caregivers spending many hours caregiving. Providing these caregivers with practical support interventions or respite care could reduce the amount of time the caregiver spends on caregiving. Respite care services could include adult daycare or a temporary residential admission (Rottmann et al., 2022).
4.2.2.2 Caregiver mental health. Factors related to the caregiver’s mental health were associated with burden. Jaracz et al. (2012) found that caregiver burden was related to higher emotional distress in a sample of 150 caregivers of individuals with stroke* 1-year post injury. In this study, emotional distress was indicated by the mean of the caregivers’ score* on the HADS, which measures both anxiety and depression. Investigating the same cohort, Jaracz et al. (2015) found that anxiety predicted caregiver burden 5-years post injury, also using the HADS. Likewise, in a longitudinal study, Kruithof et al. (2016) demonstrated that higher anxiety scores on the HADS was associated with a higher burden in 183 caregivers 2-months post stroke. This correlation was, however, not significant 1-year post stroke. Furthermore, Blake et al. (2003) found that low caregiver mood and negative affectivity predicted caregiver burden in 116 caregivers of individuals with stroke. In addition, Machamer et al. (2002) demonstrated that depressive symptoms were related to caregiver burden in a large study comprising 180 caregivers of individuals with TBI, measured by the Center for Epidemiologic Studies-Depression Scale (Weissman et al., 1977). Likewise, Achilike et al. (2020) found that caregiver depressive symptoms were associated with higher caregiver burden in 88 caregivers of individuals with stroke, using the Patient Health Questionnaire-9 (PHQ-9; Kroenke et al., 2001). One study by Bergström et al. (2011) found that low life satisfaction in the caregiver was associated with a higher caregiver burden in 81 caregivers of individuals with stroke. Thus, the evidence strongly suggests that factors related to lower caregiver mental health are associated with higher caregiver burden. However, five (Achilike et al., 2020; Bergström et al., 2011; Blake et al., 2003; Jaracz et al., 2012; Machamer et al., 2002) of the studies that investigated this association had a cross-sectional design, while only two (Jaracz et al., 2015; Kruithof et al., 2016) had a longitudinal design. The cross-sectional study designs prevented any indications about causality. Therefore, the direction of the association between caregiver burden and factors related to caregivers’ mental health can be questioned: did worse mental health lead to high levels of burden, or did high levels of burden lead to worse mental health? More studies investigating predictors of caregiver burden longitudinally could further establish the direction of the identified associations and are highly needed.
4.2.2.3 Unmet needs. Two studies (Doser & Norup, 2016; Nabors et al., 2002) found that unmet needs predicted higher caregiver burden. Nabors et al. (2002) found that percentage of needs met and importance of needs was the strongest predictor of caregiver burden. Both studies applied the Family Needs Questionnaire (Kreutzer et al., 1995), a clinically validated instrument designed to identify the importance of needs in the family following brain injury and assess if the perceived needs are met or unmet. Thus, the association between burden and unmet needs seems evident, although the evidence is limited. However, there are some limitations to consider. The two studies had rather small samples of 44 and 45 caregivers, which warrants caution with respect to generalization of the results. Furthermore, both studies had a cross-sectional design and examined the association between unmet needs and caregiver burden 2-years post injury and 3–6 years post injury, respectively. Thus, these studies only give an indication of the association between unmet needs and caregiver burden in the chronic phase of TBI or nTBI. Therefore, studies investigating the association between unmet needs and caregiver burden in the early phases of rehabilitation are needed. Furthermore, longitudinal studies could elucidate the association between unmet needs and caregiver burden at different time points. Nonetheless, caregivers seem to be at greater risk of experiencing burden when they report more unmet needs. Therefore, health care professionals ought to address caregiver needs throughout the neurorehabilitation process, as persisting unmet needs can potentially result in higher caregiver burden.
4.3Clinical implications
While many caregivers adapt well to their changed life situation and to the caregiving role, some caregivers are at risk of experiencing caregiver burden. The findings indicate that caregivers are at risk of burden if the care recipient sustained a more severe injury, experience problems related to mental health or a high level of physical or neuropsychological disabilities, and if the caregiver spends more time on caregiving, experience mental health problems and report more unmet needs. The results of this review draw attention to the complex interplay of different factors contributing to a higher caregiver burden. This stresses the importance of undertaking a systematic assessment of the individual caregivers’ situation to identify risk factors and ensure that they receive the support they need. Future intervention programs should target caregivers in need of more support and long-lasting help, and identification of risk factors for caregiver burden can guide the choice of intervention. Practical support intervention and respite care could be provided for caregivers spending many hours caregiving and caregivers caring for an individual with a high level of disabilities. Furthermore, caregivers should be provided with sufficient information about the care recipient’s illness and care needs to enhance their knowledge about the consequences of the injury and allow them to reach a greater understanding of the injured individuals situation and needs (Adelman et al., 2014). Psychosocial support interventions could aid in improving the caregiver’s well-being and prevent problems related to mental health (Rottmann et al., 2022). Such interventions could address the caregiver’s problem-solving skills (Kreutzer et al., 2009,), coping strategies (Backhaus et al., 2010), and management of emotions (Kreutzer et al., 2009; Rottmann et al., 2022). Furthermore, caregivers should be encouraged to improve self-care by engaging in activities that promote the caregiver’s own health (Adelman et al., 2014; Revenson et al., 2016).
4.4Study limitations
This scoping review has several limitations. First, the generalizability of the findings of this review is compromised by limiting the inclusion to studies conducted in Europe, the United States of America, or Australia. There are vast differences in developed and developing countries in terms of governmental policies regarding formal long-term care resources, opportunities to outsource caregiving tasks and obtain support from health care professionals. Furthermore, cultural norms on injury, recovery, rehabilitation, and family caregiving vary by global region (Norup et al., 2015). Given the heterogeneity of the caregiver population across the world, it was decided to include studies conducted in populations with more similar and well-developed national health care system structures. However, including caregivers from populations across the whole world would have given an even broader insight into predictors of caregiver burden. Second, the search for literature was limited to the selected databases. Additionally, as only articles in English were considered, the findings are subject to language-of-publication-bias. Furthermore, only published work was included in the scoping review, thus resulting in publication bias. Last, it is acknowledged that a formal appraisal of the quality of the included studies was not undertaken, which remains yet to be completed.
5Conclusion and future directions
The current scoping review synthesized evidence regarding predictors of caregiver burden in caregivers of individuals with TBI or nTBI. Despite the mentioned limitations, the results highlighted that certain caregivers are at increased risk of caregiver burden; namely caregivers of individuals with more severe injuries who experience a higher level of disabilities and problems related to mental health, and caregivers who spend more time on caregiving, experience mental health problems and report more unmet needs. These results highlight which caregivers are at risk and point to several areas, where potential intervention will help prevent caregiver burden. Consequently, the results enable professionals to target the limited resources toward the families most at risk. Through early identification of caregivers at risk, vulnerable caregivers can be provided with appropriate intervention and support, which might prevent caregiver burden and potential long-lasting consequences of providing care. Helping caregivers at risk will benefit the caregiver, the individual with the injury, and society in terms of reduced costs of care.
Future research could 1) Explore the relationship between other characteristics of the caregiver and caregiver burden, such as coping style, problem-solving techniques, personality traits or other personality-related variables such as optimism, self-esteem, and health behaviors, i.e. habits regarding sleep, diet, physical activity, and use of substances; 2) Explore the relationship between family characteristics and caregiver burden, including family functioning, family dynamics and conflicts. Addressing these gaps may assist in the development and implementation of interventions in informal caregiving, as such factors are potentially modifiable through intervention; and 3) Elucidate if burden can be prevented by support programs targeting caregivers at risk. Furthermore, future research would benefit from consistently utilizing clinically validated instruments designed for measuring caregiver burden and predictor variables. Also, more longitudinal studies are needed to increase the understanding of how predictor variables contribute differently at different time points.
Conflict of interest
None to declare.
Acknowledgments
The authors have no acknowledgements.
Funding
The authors report no funding.
References
1 | Achilike, S. , Beauchamp, J. E. S. , Cron, S. G. , Okpala, M. , Payen, S. S. , Baldridge, L. , Okpala, N. , Montiel, T. C. , Varughese, T. , Love, M. , Fagundes, C. , Savitz, S. , & Sharrief, A. ((2020) ) Caregiver burden and associated factors among informal caregivers of stroke survivors, American Association of Neuroscience Nurses 52: (6). |
2 | Adelman, R. D. , Tmanova, L. L. , Delgado, D. , Dion, S. , & Lachs, M. S. ((2014) ) Caregiver burden: A clinical review. JAMA: The Journal of the American Medical Association, 311: (10), 1052–1060. https://doi.org/10.1001/jama.2014.304. |
3 | Arango-Lasprilla, J. C. , Quijano, M. C. , Aponte, M. , Cuervo, M. T. , Nicholls, E. , Rogers, H. L. , & Kreutzer, J. ((2010) ) Family needs in caregivers of individuals with traumatic brain injury from Colombia, South America, Brain Injury 24: (7-8), 1017–1026. DOI: 10.3109/02699052.2010.490516. |
4 | Arnould, A. , Rochat, L. , Azouvi, P. , & Linden, M. V. ((2015) ) Apathetic symptom presentations in patients with severe traumatic brain injury: Assessment, heterogeneity and relationships with psychosocial functioning and caregivers’ burden, Brain Injury 29: (13-14), 1597–1603. DOI: 10.3109/02699052.2015.1075156. |
5 | Backhaus, S. L. , Ibarra, S. L. , Klyce, D. , Trexler, L. E. , & Malec, J. F. ((2010) ) Brain injury coping skills group: A preventative intervention for patients with brain injury and their caregivers, Archives of Physical Medicine and Rehabilitation 91: (6), 840–848. |
6 | Bakas, T. , & Champion, V. ((1999) ) Development and psychometric testing of the Bakas Caregiving outcomes scale, Nursing Research 48: , 250–259. |
7 | Baker, A. , Barker, S. , Sampson, A. , & Martin, C. ((2017) ) Caregiver outcomes and interventions: A systematic scoping review of the traumatic brain injury and spinal cord injury literature, Clinical Rehabilitation 31: (1), 45–60. |
8 | Baker, S. P. , O’Neill, B. , Haddon, W. , & Long, W. B,. ((1974) ) The injury severity score: A method for describing patients with multiple injuries and evaluating emergency care, Journal of Trauma 14: (3), 187–196. |
9 | Bayen, E. , Jourdan, C. , Ghout, I. , Darnoux, E. , Azerad, S. , Vallat-Azouvi, C. , Weiss, J. , Aegerter, P. , Pradat-Diehl, P. , Joël, M. , & Azouvi, P. ((2016) ) Objective and subjective burden of informal caregivers 4 years after a severe traumatic brain injury: Results from the PariS-TBI study, Journal of Head Trauma Rehabilitation 31: (5), 59–67. |
10 | Bayen, E. , Pradat-Diehl, P. , Jourdan, C. , Ghout, I. , Bosserelle, V. , Azerad, S. , Weiss, J. J. , Joël, M. E. , Aegerter, P. , & Azouvi, P. ((2013) ) Predictors of informal care burden 1 year after a severe traumatic brain injury: Results from the PariS-TBI study, The Journal of Head Trauma Rehabilitation 28: (6), 408–418. DOI: 10.1097/HTR.0b013e31825413cf. |
11 | Bergström, A. L. , Eriksson, G. , Koch, L. , & Tham, K. ((2011) ) Combined life satisfaction of persons with stroke and their caregiver: Associations with caregiver burden and the impact of stroke, Health and Quality of Life Outcomes 9: (1). |
12 | Blake, H. , Lincoln, N. B. , & Clarke, D. D. ((2003) ) Caregiver strain in spouses of stroke patients, Clinical Rehabilitation 17: , 312–317. Doi: 10.1191/0269215503cr613oa. |
13 | Bocéréan, C. , & Dupret, E. ((2014) ) A validation study ofthe Hospital Anxiety and Depression Scale (HADS) in a large sampleof French employees, BMC Psychiatry 14: (1), 354–354. DOI: 10.1186/s12888-014-0354-0. |
14 | Brain Injury Association of America. (2020). Brain Injury Overview. Retrieved February 3rd, 2022, from https://www.biausa.org/brain-injury/about-brain-injury/basics/overview. |
15 | Brott, T. , Adams, H. P. Jr , Olinger, C. P. , et al. ((1989) ) Measurements of acute cerebral infarction: A clinical examination scale, Stroke 20: , 864–870. |
16 | Chronister, J. , Chan, F. , Sasson-Gelman, E. J. , & Chiu, C. Y. ((2010) ) The association of stress-coping variables to quality of life among caregivers of individuals with traumatic brain injury, NeuroRehabilitation 27: , 49–62. |
17 | Cieza, A. , Causey, K. , Kamenov, K. , Hanson, S. W. , Chatterji, S. , & Vos, T. ((2020) ) Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: A systematic analysis for the Global Burden of Disease Study 2019, The Lancet (British Edition) 396: (10267), 2006–2017. DOI: 10.1016/S0140-6736(20)32340-0. |
18 | Covidence. (2021). Retrieved from https://www.covidence.org/home. |
19 | Davis, L. C. , Sander, A. M. , Struchen, M. A. , Sherer, M. , Nakase-Richardson, R. , & Malec, J. F. ((2009) ) Medical and psychosocial predictors of caregiver distress and perceived burden following traumatic brain injury, Journal of Head Trauma Rehabilitation 24: (3), 145–154. |
20 | Denckla, M. B. ((2002) ) The behavior rating inventory of executive function: Commentary, Child Neuropsychology 8: (4), 304–306. |
21 | Dewan, M. C. , Rattani, A. , Gupta, S. , Baticulon, R. E. , Hung, Y. C. , Punchak, M. , Agrawal, A. , Adeleye, A. O. , Shrime, M. G. , Rubiano, A. M. , Rosenfeld, J. V. , Park, K. B. (2018). Estimating the global incidence of traumatic brain injury. Journal of Neurosurgery, 1-18. |
22 | Doser, K. , & Norup, A. ((2016) ) Caregiver burden in Danish family members of patients with severe brain injury: The chronic phase, Brain Injury 30: (3), 334–342. DOI: 10.3109/02699052.2015.1114143. |
23 | Feigin, V. L. , Lawes, C. M. , Bennett, D. A. , & Anderson, C. S. ((2003) ) Stroke epidemiology: A review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century, Lancet Neurology 2: (1), 43–53. DOI: 10.1016/S1474-4422(03)00266-7. |
24 | Fugl-Meyer, A. R. , Melin, R. , & Fugl-Meyer, K. S. ((2002) ) Life satisfaction in 18- to 64-year- old Swedes: In relation to gender, age, partner and immigrant status, Journal of Rehabilitation Medicine 34: (5), 239–246. |
25 | Greene, J. G. , Smith, R. , Gardiner, M. , & Timbury, G. C. ((1982) ) Measuring behavioural disturbance of elderly demented patients in the community and its effects on relatives: A factor analytic study, Age Ageing 11: , 121–126. |
26 | Griffen, J. , Hanks, R. (2014). Cognitive and Behavioral Outcomes from Traumatic Brain Injury. In Sherer, M., & Sander, A. M. (Eds.), Handbook on the Neuropsychology of Traumatic Brain Injury, 1st ed., Springer, (20 SP), pp. 25-45. |
27 | Hall, K. M. , Cope, D. N. , & Rappaport, M. ((1985) ) Glasgow outcome scale and disability rating scale: Comparative usefulness in following recovery in traumatic head injury, Archives of Physical Medicine and Rehabilitation 66: , 35–37. |
28 | Hamilton, B. , Laughlin, J. , & Fiedler, R. ((1994) ) Interrater reliability of the 7-level functional independence measure (FIM, Scandinavian Journal of Rehabilitation Medicine 26: , 115–1194. |
29 | Ilse, I. B. , Feys, H. , Wit, L. , Putman, K. , & Weerdt, W. ((2008) ) Stroke caregivers’ strain: Prevalence and determinants in the first six months after stroke, Disability and Rehabilitation 30: (7), 523–530. |
30 | Jaracz, K. , Grabowska-Fudala, B. , & Kozubski, W. ((2012) ) Caregiverburden after stroke: Towards a structural model, Neurologia INeurochirurgia Polska 46: (3), 224–232. |
31 | Jaracz, K. , Grabowska-Fudala, B. , Górrna, k. , Jaracz, J. , Moczko, J. , & Kozubski, W. ((2015) ) Burden in caregivers of long-term stroke survivors: Prevalence and determinants at 6 months and 5 years after stroke, Patient Education and Counseling 98: , 1011–1016. |
32 | Johnsen, A. T. , Grønbæk, M. (2022). Social Inequalities in Health –with a Focus on within-country Differences in the Richer Part of the World. In Pedersen, S. S., Roessler, K. K., Andersen, T. E., Johnsen, A. T., & Pouwer, F. (Eds.), Textbook of Applied Medical Psychology: A Multidisciplinary Approach. University Press of Southern Denmark, pp. 517-566. |
33 | King, N. S. , Tyerman, A. (2010). Neuropsychological presentation and treatment of traumatic brain injury. In Gurd, J., Kischka, U., & Marshall, J., (Eds.), The Handbook of Clinical Neuropsychology, 2nd ed., Ch. 27. Oxford University Press. |
34 | Kokorelias, K. M. , Lu, F. K. T. , Santos, J. R. , Xu, Y. , Leung, R. , & Cameron, J. I. ((2020) ) Caregiving is a full-time job” impacting stroke caregivers’ health and well-being: A qualitative meta-synthesis, Health and Social Care in the Community 28: , 325–340. |
35 | Kreitzer, N. , Kurowski, B. G. , & Bakas, T. ((2018) ) Systematic review of caregiver and dyad interventions after adult traumatic brain injury, Archives of Physical Medicine and Rehabilitation 99: , 2342–2354. |
36 | Kreutzer, J. S. , Marwitz J. , West, D. (1998). Family needs questionnaire, administration and scoring manual. Physical Medicine & Rehabilitation Neuropsychology. |
37 | Kreutzer, J. S. , Stejskal, T. M. , Ketchum, J. M. , Marwitz, J. H. , Taylor, L. A. , & Menzel, J. C. ((2009) ) A preliminary investigation of the brain injury family intervention: Impact on family members, Brain Injury 23: (6), 535–547. |
38 | Kroenke, K. , Spitzer, R. L. , & Williams, J. B. ((2001) ) The PHQ-9: Validity of a brief depression severity measure, Journal of General Intern Medicine 16: (9), 606–613. DOI: 10.1046/j.1525-1497.2001.016009606.x. |
39 | Kruithof, W. , Post, M. W. M. , Mierlo, M. L. , Bos, G. , Ginkel, J. M. , & Visser-Meily, J. M. A. ((2016) ) Caregiver burden and emotional problems in partners of stroke patients at two months and one year post-stroke: Determinants and prediction, Patient Education and Counseling 99: , 1632–1640. |
40 | Levin, H. S. , O’Donnell, V. M. , & Grossman, R. G. ((1979) ) The Galveston Orientation and Amnesia Test: A practical scale to assess cognition after head injury, The Journal of Nervous and Mental Disease 167: , 675–684. |
41 | Machamer, J. , Temkin, N. , & Dikmen, S. ((2002) ) Significant other burden and factors related to it in traumatic brain injury, Journal of Clinical and Experimental Neuropsychology 24: (4), 420–433. |
42 | Mackenzie, A. , & Greenwood, N. ((2012) ) Positive experiences of caregiving in stroke: A systematic review, Disability and Rehabilitation 34: (17), 1413–1422. |
43 | Mahoney, F. I. , & Barthel, D. W. ((1965) ) Functional evaluation: The Barthel index, Maryland State Medical Journal 14: , 61–65. |
44 | Manskow, U. S. , Friborg, O. , Røe, C. , Braine, M. , Damsgard, E. , & Anke, A. ((2017) ) Patterns of change and stability in caregiver burden and life satisfaction from 1 to 2 years after severe traumatic brain injury: A Norwegian longitudinal study, Neuro Rehabilition 40: , 211–222. DOI: 10.3233/NRE-161406. |
45 | Manskow, U. S. , Sigurdardottir, S. , Røe, C. , MD, Andelic, N. , Damsgård, E. , Skandsen, T. , Elmståhl S. , & Anke, A. ((2015) ) Factors affecting caregiver burden 1 year after severe traumatic brain injury: A prospective nationwide multicenter study, Journal of Head Trauma Rehabilitation 30: (6), 411–423. |
46 | Marsh, N. V. , Kersel, D. A. , Havill, J. H. , & Sleigh, J. W. ((2002) ) Caregiver burden during the year following severe traumatic brain injury, Journal of Clinical and Experimental Neuropsychology 24: (4), 434–447. |
47 | Nabors, N. , Seacat J. , & Rosenthal, M. ((2002) ) Predictors of caregiver burden following traumatic brain injury, Brain Injury 16: (12), 1039–1050. |
48 | Norup, A. ((2018) ) Family matters in neurorehabilitation: Why, when, who, and how?, In Revista Iberoamericana de Neuropsicologia, 1: (1), 17–31. |
49 | Norup, A. , Kristensen, K. S. , Poulsen, I. , & Mortensen, E. L. ((2017) ) Evaluating clinically significant changes in health- related quality of life: A sample of relatives of patients with severe traumatic brain injury, Neuropsychological Rehabilitation 27: (2), 196–215. |
50 | Norup, A. , Kruse, M. , Soendergaard, P. L. , Rasmussen, K. W. , & Biering-Sørensen, F. ((2020) ) Socioeconomic conseqences of traumatic brain injury: A danish nationwide register-ased Study, Journal of Neurotrauma 37: (24). |
51 | Norup, A. , Perrin, P. B. , Cuberos-Urbano, G. , Anke, A. , Andelic, M. , Doyle, S. T. , et al. ((2015) ) Family needs after brain injury: A cross cultural study, NeuroRehabilitation 36: (2), 203–214. |
52 | Norup, A. , Siert, L. , & Mortensen, E. L. ((2010) ) Emotional distress and quality of life in relatives of patients with severe brain injury: The first month after injury, Brain Injury 2: (2), 81–88. |
53 | Norup, A. , Siert, L. , & Mortensen, E. L. ((2013) ) Neuropsychological intervention in the acute phase: A pilot study of emotional wellbeing of the relatives of patients with severe brain injury, Journal of Rehabilitation Medicine 45: , 827–834. |
54 | Oosterveer, D. M. , Mishre, R. R. , Oort, A. , Bodde, K. , Aerden, L. A. M. , ((2014) ) Anxiety and low life satisfaction associate with high caregiver strain early after stroke, Journal of Rehabilitation Medicine 46: , 139–143. |
55 | Pont, W. , Groeneveld, I. , Arwert, H. , Meesters, J. , Mishre, R. R. , Vlieland, T. V. , & Grossens, P. ((2018) ) Caregiver burden after stroke: Changes over time?, Disability and Rehabilitation 42: (3), 360–367. DOI: 10.1080/09638288.2018.1499047. |
56 | Pucciarelli, G. , Ausili, D. , Galbussera, A. A. , Rebora, P. , Savini, S. , Simeone, S. , Alvaro, R. , & Vellone, E. ((2018) ) Quality of life, anxiety, depression and burden among stroke caregivers: A longitudinal, observational multicentre study, Journal of Advanced Nursing 74: , 1875–1887. |
57 | Rasmussen, M. A. , Arango-Lasprilla, J. C. , Andelic, N. , Nordenmark, T. H. , & Soberg, H. L. ((2020) ) Mental health and family functioning in patients and their family members after traumatic brain injury: A cross-sectional study, Brain Sciences 10: . DOI: 10.3390/brainsci10100670. |
58 | Revenson, T. A. , Griva, K. , Luszzczynska, A. , Morrison, V. , Panagopolou, E. , Vilchinsky, N. , et al., ((2016) ). Caregiving in the Illness Context. London: Palgrave Macmillan UK. |
59 | Rigby, H. , Gubitz, G. , Eskes, G. , Reidy, Y. , Christian, C. , Grover, V. , Philips, S. , (a). Caring for stroke survivors: Baseline and 1-year determinants of caregiver burden, International Journal of Stroke 4: , 152–158. |
60 | Rigby, H. , Gubitz, G. , Philips, S. , (b). A systematic review of caregiver burden following stroke, International Journal of Stroke 4: , 285–292. |
61 | Robert, P. H. , Clairet, S. , Benoit, M. , Koutaich, J. , Bertogliati, C. , Tible, O. , Caci, H. , Borg, M. , Brocker, P. , & Bedoucha, P. ((2002) ) The Apathy Inventory: Assessment of apathy and awareness in Alzheimer’s disease, Parkinson’s disease and mild cognitive impairment, International Journal of Geriatric Psychiatry 17: (12), 1099–1105. DOI: 10.1002/gps.755. |
62 | Rosenberg, P. B. , Mielke, M. M. , & Lyketsos, C. G. ((2005) ) Caregiver assessment of patients’ depression in Alzheimer disease: Longitudinal analysis in a drug treatment study, American Journal of Geriatric Psychiatry 13: (9), 822–826. |
63 | Roopchandmartin, S. , & Crearyyan, S. ((2014) ) Level of caregiver burden in jamaican stroke caregivers and relationship between selected sociodemographic variables, West Indian Medicine Journal 63: , 605–609. |
64 | Rottmann, N. , Norup, A. , Dieperink, K. B. (2022). Informal Caregiving in Life-threatening or Chronic Illness. In Pedersen, S. S., Roessler, K. K., Andersen, T. E., Johnsen, A. T., & Pouwer, F. (Eds.), Textbook of Applied Medical Psychology: A Multidisciplinary Approach, University Press of Southern Denmark, pp. 517-566. |
65 | Tagliaferri, F. , Compagnone, C. , Korsic, M. , Servadei, F. , & Kraus, J. ((2006) ) A systematic review of brain injury epidemiology in Europe, Acta Neurochirurgica 148: , 255–268. |
66 | Teasdale, G. , & Jennett, B. ((1974) ) Assessment of coma and Impaired Consciousness: A Practical Scale, The Lancet (British Edition) 304: (7872), 81–84. |
67 | Tooth, L. , Mckenna, K. , Barnett, A. , Prescott, C. , & Murphy, S. ((2005) ) Caregiver burden, time spent caring and health status in the first 12 months following stroke, Brain Injury 19: (12), 963–974. DOI: 10.1080/02699050500110785. |
68 | Tramonti, F. , Bonfiglio, L. , Bernardo, C. D. , Ulivi, C. , Virgillito, A. , Rossi, B. , & Carboncini, M. C. ((2015) ) Family functioning in severe brain injuries: Correlations with caregivers’ burden, perceived social support and quality of life, Medicine 20: (8), 933–939. DOI: 10.1080/13548506.2015.1009380. |
69 | Tricco, A. C. , Lillie, E. , Zarin, W. , O’Brien, K. K. , Colquhoun, H. , & Levac, D. ((2018) ) PRISMA Extension for Scoping Reviews (PRISMAScR): Checklist and Explanation, In Annals og Internal Medicine 169: , 467–473. DOI: 10.7326/M18-0850. |
70 | van Marwijk H. W. , Wallace, P. , de Bock, G. H. , Hermans, J. , Kaptein, A. A. , & Mulder, J. D. ((1995) ) Evaluation of the feasibility, reliability and diagnostic value of shortened versions of the geriatric depression scale, British Journal of General Practice 45: , 195–199. |
71 | Vanier, M. , Mazaux, J. M. , Lambert, J. , Dassa, C. , & Levin H. S. ((2000) ) Assessment of neuropsychologic impairments after head injury: Interrater reliability and factorial and criterion validity of the Neurobehavioral Rating Scale-Revised, Archives of Physical Medicine and Rehabilitation 81: (6), 796–806. |
72 | Verhaeghe, S. , Defloor, T. , & Grypdonck, M. ((2005) ) Stress and coping among families of patients with traumatic brain injury: A review of the literature, Journal of Clinical Nursing 14: , 1004–1012. |
73 | Vogler, J. L. , Klein, A. , & Bender, A. ((2014) ) Long-term health-related quality-of-life in patients with acquired brain injury and their caregivers, Brain Injury 28: (11). DOI: 10.3109/02699052.2014.919536. |
74 | Ware, J. E. , & Sherbourne, C. D. ((1992) ) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection, Medical Care 30: , 473–483. |
75 | Wechsler. (1981). WAIS-R manual: Wechsler adult intelligence scale - revised. Psychological corp. |
76 | Weissman, M. M. , Sholomskas, D. , Pottenger, M. , Prusoff, B. A. , Locke, B. Z. , ((1977) ) Assessing depressive symptoms in five psychiatric populations: A validation study, American Journal of Epidemiology 106: , 203–214. |
77 | Wilson, J. T. , Pettigrew, L. E. , & Teasdale, G.M. ((1998) ) Structured interviews for the Glasgow Outcome Scale and the extended Glasgow Outcome Scale: Guidelines for their use, Journal of Neurotrauma 15: (8), 573–585. |
78 | Wu, C. , Skidmore, E. R. , & Rodakowski, J. ((2019) ) Relationship consensus and caregiver burden in adults with cognitive impairments months following stroke, American Academy of Physical Medicine and Rehabilitation 11: , 597–603. |
79 | Zhu, W. , Jiang ((2018) ) A meta-analytic study of predictors for informal caregiver burden in patients with stroke, Journal of Stroke and Cerebrovascular Diseases 27: (12), 3636–3646. |




