Associations between protective resources and family functioning after traumatic brain injury: A cross-sectional study using a structural equation modeling approach
Abstract
BACKGROUND:
A strength-based approach in the rehabilitation after traumatic brain injury (TBI) is recommended for patients and their families. However, further exploration of the complexity of individual and family factors is needed.
OBJECTIVE:
To explore the associations between individual protective resources in patients and family members and the overall family functioning using a strength-based approach.
METHODS:
Secondary analysis of data collected at baseline in a randomized controlled trial. Structural equation modeling with two latent constructs and six observed variables was performed. Outcome measures included the Resilience Scale for Adults, the Mental Component Summary (SF-36), the General Self-Efficacy Scale, and the Family Adaptability and Cohesion Evaluation Scale-IV.
RESULTS:
Hundred and twenty-two participants (60 patients, 62 family members) with a mean age of 43 years were included at a median of 11 months post-injury. The final model demonstrated a strong covariance (coefficient = 0.61) between the latent Protective construct and Family functioning. Model-fit statistics indicated an acceptable fit to the data.
CONCLUSION:
Higher levels of protective resources (resilience, self-efficacy, and mental HRQL) were positively associated with family functioning. These resources should be further assessed in patients and their families, to identify factors that can be strengthened through TBI rehabilitation intervention.
1Introduction
Regardless of the severity of traumatic brain injury (TBI), individuals may experience various physical, cognitive, and emotional problems after injury, which can impact daily life activities and participation, and reduce the quality of life ( Polinder et al., 2018; Rasmussen et al., 2020; Wilson, Stewart, et al., 2017).
From a family system perspective, the impact of TBI concerns all family members and might adversely affect family dynamics (Ergh et al., 2002; Gan et al., 2006). Family systems consist of multiple reciprocal relationships among the members within the system; consequently, if one family member changes it will impose changes in all the other members as well ( Verhaeghe et al., 2005). Studies exploring the effects of TBI on families have demonstrated an increased risk for unhealthy family dynamics, as well as increased levels of emotional distress ( Ennis et al., 2013) and caregiver burden in family members ( Bayen et al., 2016; Rasmussen et al., 2021). However, when the family system is exposed to an unexpected stressor, such as a TBI, the system may also adjust to maintain stability and continue functioning ( Olson, 2011).
Regarding the consequences of TBI on both individuals and families, the focus of studies has shifted from negative outcomes to a more strength-based perspective, which is relevant for understanding the recovery process following TBI ( King et al., 2021). Despite the distress and challenges in the aftermath of TBI, some individuals and families seem to adjust and cope more efficiently than do others ( Ponsford et al., 2003; Verhaeghe et al., 2005). Studies on caregivers of persons with TBI have demonstrated that a significant proportion of families report generally healthy family communication and functioning ( Lehan et al., 2012; Perrin et al., 2013; Ponsford et al., 2003; Rasmussen et al., 2020; Schönberger et al., 2010). Based on these findings, researchers have called for further exploration of factors associated with healthy coping and adjustment (Ponsford et al., 2003; Verhaeghe et al., 2005).
Two psychological constructs pertaining to rehabilitation have received attention in line with the increasing focus on the strength-based approach: resilience and self-efficacy. Resilience refers to factors that facilitate coping and adjustment in response to traumatic and challenging events ( Friborg et al., 2009), and is applicable at both individual and family levels ( Aburn et al., 2016; Godwin et al., 2015). According to Bonanno, resilience is both an individual resource and a modifiable factor ( Bonanno, 2005). Self-efficacy often is considered a quality of resilience; it refers to how people think, feel, and act, to shape and take control over their lives to achieve desirable outcomes ( Schwarzer & Warner, 2012; Seligman & Csikszentmihalyi, 2000).
At the individual level, skills that have been identified to facilitate resilience include personal abilities such as maintaining a positive outlook, having positive emotions, and placing greater value on support from family and friends ( Bonanno, 2004; Friborg et al., 2003). At a family level, resilience is reflected in a family’s ability to establish mutual and shared responses to challenges. Moreover, family resilience is dependent on the level of cohesion, flexibility, and communication skills among family members (Godwin et al., 2015; Olson et al., 2019; Stejskal, 2012).
Previous studies have mainly explored protective factors in either patients or caregivers ( Anderson et al., 2020; Hanks et al., 2016), and few studies have explored resilience from a family perspective by including outcomes for both patients and family members. An exception is a study by Scholten et al. (2020) on dyads of patients and caregivers facing an acquired brain injury or spinal cord injury. The study found that low self-efficacy in the acute phase after an injury is associated with adjustment problems and unhealthy family functioning at six months post-discharge, whereas dyads with high self-efficacy demonstrated more healthy family functioning (Scholten et al., 2020).
In persons with TBI, high resilience has been associated with better functional outcomes and lower levels of emotional distress one year after injury ( Marwitz et al., 2018). Other studies have shown that persons with mild-to-severe TBI who report low levels of resilience are at particular risk of impaired subjective well-being, including psychological distress, symptom burden, and reduced life satisfaction ( Brands et al., 2019; Rapport et al., 2020). Meanwhile, in persons with mild TBI, high self-efficacy is associated with a more active coping style ( Scheenen et al., 2017).
Similar associations have been revealed in studies on resilience in caregivers of persons with TBI and acquired brain injury. Resilient caregivers tend to cope more actively and have better mental health ( Simpson & Jones, 2013; Simpson et al., 2021). Simpson et al. (2021) suggest that resilience and social support mediate the relationship between coping and caregiver burden. Higher levels of resilience are also associated with better mental health-related quality of life in both individuals with TBI and family members (Rasmussen et al., 2020), consistent with the resilience theory. Moreover, TBI patients’ behavioral changes, caregivers’ well-being and the family functioning are strongly influenced by each other ( Norup, 2018; Schönberger et al., 2010).
In a rehabilitation context, the increasing interest in protective factors and the family system’s abilities to adjust and recover following a TBI has led to the development of strength-based family interventions that aim to promote positive outcomes for all family members ( Godwin & Kreutzer, 2013). However, empirical studies are needed to determine the relevance of these protective factors for the TBI population from a positive psychology perspective and to identify core components, in order to develop effective family interventions ( Evans, 2011; Godwin & Kreutzer, 2013; Sullivan et al., 2016). Furthermore, such studies should explore various factors that influence the family functioning ( Walsh, 2003). Given the complex nature of relationships among constructs such as individual and family resilience, multivariate methods are recommended in rehabilitation research ( Dimitrov, 2006).
The objectives of this study, therefore, were to determine the associations between protective factors and family functioning-related factors. Specifically, by applying a structural equation modeling (SEM) approach, we aimed to examine the interactions between protective factors and family functioning, from the perspectives of both patients and their family members. Based on individual resources and the family systems theory, we hypothesized that individual protective factors would be strongly correlated with family functioning in families experiencing the consequences of TBI.
2Methods
2.1Study design
This cross-sectional study involved secondary data analysis of baseline data collected from a randomized controlled trial (RCT) of a family-based intervention for patients and family members affected by TBI (Rasmussen et al., 2021). The RCT was registered in Clinical Trials with the identifier: NCT03000400 and approved by the Norwegian Medical Research Ethic Committee (#2016/1215). Written informed consent was obtained from all participants.
2.2Procedures and participants
Participants were enrolled at the Department of Physical Medicine and Rehabilitation, Oslo University Hospital, Norway, from January 2017 to June 2019. Participants were recruited from a specialized TBI outpatient clinic where they had been referred for follow-up after mild TBI, with a protracted course of recovery, to severe TBI. Eligibility criteria were patients a) aged 16–65 years, b) who were diagnosed with a TBI according to the International Classification of Diseases, 10th Revision (ICD-10) classification system (S06.0–S06.9), c) who had sustained the TBI 6-18 months prior to study inclusion, d) who had a cognitive functioning level corresponding to a Rancho Los Amigos Scale score of 8 ( Hagen et al., 1979), and e) were residing at their homes. Patients who met the selection criteria were identified and screened by their attending physicians. The family members were selected by the patients; the eligibility criteria for the family members were: a) aged 18–65 years, b) actively involved in the patient’s daily life and having regular contact. Patients and family members were excluded in case of: a) inability to speak/read Norwegian, b) a pre-injury learning disability, c) an ICD-10 diagnosis of severe psychiatric or degenerative neurological illness, d) ongoing substance abuse, and e) having other family members in need of professional care.
2.3Data collection and outcome measures
Data were collected using standardized self-reported questionnaires that were filled out by both patients and family members. A short questionnaire was designed in adjunction with the study to collect sociodemographic data. In addition, injury-related variables were obtained from patients’ medical records. To control for bias, the outcome measures were administered by research assistants who were blinded to the study allocation. Baseline data from the intervention and control arms in the RCT were utilized in the current study. The questionnaires were completed during the introductory session for the families in the intervention group and via mail by families in the control group.
Sociodemographic data included age, gender, level of education (dichotomized into low/high, with high representing college/university degree), family member’s relationship to the patient, duration of the relationship, employment status, and the number of people living in the patient’s household.
Injury-related characteristics included cause of injury, time since injury (months), the lowest Glasgow Coma Scale (GCS) score recorded within the first 24 h after injury; scores 3–8, 9–12, and 13–15 indicate severe, moderate and mild injury, respectively ( Teasedale & Benett, 1975), the Abbreviated Injury Scale Head score ( Association for the Advancement of Automotive Medicine, 2008), and intracranial injury on CT/MRI.
Resilience: Resilience was assessed using the Resilience Scale for Adults (RSA) (Friborg et al., 2003). The RSA is a 33-item scale that assesses positive individual factors across five domains: perception of self/future, social competence, family cohesion, social resources, and structured style. Responses are made on a 5-point scale, and the total score ranges from 33 (worst) to 165 (best). The scale has demonstrated good internal consistency, with Cronbach’s alphas ranging from 0.67 to 0.90 for the different domains (Friborg et al., 2003).
General self-efficacy: General self-efficacy was assessed using the General Self-Efficacy Scale (GSE), which assesses the degree to which a person believes in their competence to cope with stressful events and demands ( Schwarzer & Jerusalem, 1995). The GSE consists of 10 items scored on a 4-point scale from 1 (not at all) to 4 (exactly true). The total score ranges from 10 (worst) to 40 (best). The GSE has shown good internal consistency with Cronbach’s alphas ranging from 0.86 to 0.94 ( Luszczynska et al., 2005).
Mental health-related quality of life: This outcome was assessed using the Mental Component Summary (MCS) of the Medical Outcomes 36-item Short Form Health Survey (SF-36), version 2 ( Ware & Gandek, 1994). It comprises the following mental domains: vitality, social functioning, role-emotional functioning, and mental health. The MCS scores are transformed into T-scores based on US normative data with a mean of 50 and a standard deviation (SD) of 10 (Ware & Gandek, 1994). Scores >55 are considered above the average mental HRQL, whereas scores ranging from 45 to 55 indicate normal mental HRQL. Scores 40–45 and <40 indicate somewhat reduced mental HRQL and reduced mental HRQL, respectively ( Wilson, Marsden-Loftus, et al., 2017). The internal consistency was reported to be satisfactory (Cronbach’s alpha = 0.82) in a recent Norwegian study on individuals with moderate-to-severe TBI ( Forslund et al., 2021).
Family functioning: Family functioning was assessed using the Family Adaptability and Evaluation Scale –Fourth Edition (FACES-IV) (Olson, 2011). The FACES is a 42-items scale that assesses the degree of cohesion and flexibility in a family system. The responses are made on a 5-point scale from 1 (strongly disagree) to 5 (strongly agree). The measure consists of two balanced scales (balanced cohesion and flexibility) and four unbalanced scales: two for high and low cohesion (enmeshed and disengaged) and two for high and low flexibility (chaotic and rigid). The Circumplex ratio score is recommended for research purposes, as it indicates whether a family system is balanced or unbalanced in terms of cohesion and flexibility. A ratio score of 1 indicates equal levels of balance/unbalance, whereas higher or lower scores indicate balanced or unbalanced systems, respectively. The Circumplex ratio score was used in the current study. Additionally, the FACES consists of 20 items that measure the level of family communication and family satisfaction, with total percentile scores ranging from 10 (worst) to 99 (best) (Olson, 2011).
2.4Sample size
The sample size was estimated prior to the RCT, and the sample size calculation is described in a previous publication (Rasmussen et al., 2021). In conjunction with the current study, we performed a post-hoc calculation for a SEM approach (https://www.analyticscalculators.com/calculator.aspx?id=89). With an expected effect size of 0.3, β= 0.8, and α= 0.05, we added two latent variables and six observed variables, which estimated a minimum sample size of 90 participants to detect an effect. The sample size (n = 122) meets this requirement and was considered acceptable according to existing recommendations ( Wolf et al., 2013). Considering that this was an explorative study in a rehabilitation context and that the incidence of TBI in Norway is lower compared to other countries ( Andelic et al., 2012), we determined a sample size of 122 to be sufficient for the current study.
2.5Statistical analyses
All statistical analyses were performed using StataCorp LLC (STATA) software (College Station, TX, USA), version 17. Descriptive statistics are presented with means and standard deviations for normally distributed continuous data and with medians and interquartile ranges (IQR) for skewed data. Categorical data are presented as frequencies (n) and percentages (%). Correlations using Pearson’s r were interpreted according to Cohen’s d as small (0.10), medium (0.30), and large (0.50) effect sizes ( Cohen, 1992). To test the model, we used a SEM approach to investigate the covariance between two sets of variables and to examine multiple associations simultaneously. Standardized coefficients were reported. The model comprised two latent variables, namely the strength-based Protective factors and Family functioning. The observed measures for the Protective latent construct included RSA, GSE, and MCS. The constructs for the Family construct were the Circumplex ratio score, the Family Communication Scale, and the Family Satisfaction Scale of the FACES-IV. To assess model fit, we calculated maximum likelihood estimates. We used the root mean squared error of approximation (RMSEA), the comparative fit index (CFI), and the Tucker-Lewis index (TLI). RMSEA value <0.08, standardized root mean squared residual (SPRM)<0.07, and CFI and TLI >0.95 were considered to indicate an acceptable model fit ( Hu & Bentler, 1999).
3Results
A total of 122 participants (60 persons with TBI and 62 family members) were included in the study. Participants’ mean age was 43 years. Most family members (92%) were spouses/partners to the patients, and more than 80% reported having been in the relationship for more than five years. Most of the participants (75%) had a high education. Sociodemographic and injury-related data are presented in Table 1.
Table 1
Sociodemographic and injury-related variables
| Variables | Patients | Family members | All participants |
| (n = 60) | (n = 62) | (n = 122) | |
| Age, mean (standard deviation) | 43.8 (11.2) | 42.6 (11.4) | 43.2 (11.3) |
| Female sex, n (%) | 32 (53.3) | 32 (51.6) | 64 (52.5) |
| Family member’s relationship to the patient | |||
| Spouse/partner | – | 57 (91.9) | |
| Parent | – | 1 (1.6) | |
| Child | – | 4 (6.5) | |
| Number of persons in the household, median (range) | 3 (1–6) | ||
| Duration of relationship to the patient (n = 57) | |||
| <1 year | 3 (5.2) | ||
| 1–5 years | 7 (12.3) | ||
| >5 years | 47 (82.5) | ||
| Level of education | |||
| Low | 16 (26.7) | 15 (24.2) | 31 (25.4) |
| High | 44 (73.3) | 47 (75.8) | 91 (74.6) |
| Injury characteristics | |||
| Time since injury months, median (IQR) | 11.4 (8, 16) | ||
| GCS, median (IQR) | 15 (14, 15) | ||
| Mild | 49 (82.0) | ||
| Moderate | 3 (5.0) | ||
| Severe | 8 (13.3) | ||
| AIS, median (IQR) | 1 (1, 3) | ||
| Intracranial injury CT/MRI, n (%) | 18 (30.0) | ||
| Cause of injury | |||
| Falls | 22 (36.7) | ||
| Traffic accidents | 19 (31.7) | ||
| Struck by object | 14 (23.3) | ||
| Others | 5 (8.3) |
GCS, Glasgow Coma Scale; AIS, Abbreviated Injury Scale; CT/MRI, Computed Tomography; MRI, Magnetic Resonance Imaging.
The injured persons were included in the study at a median of 11 months post-injury, and the main causes of injury were falls and traffic accidents. Most participants (82%) had sustained a mild TBI as classified by the GCS score, and approximately 30% showed evidence of intracranial injury on CT/MRI.
The patients reported significantly lower levels of mental HRQL (p < 0.001), resilience (p = 0.025), and general self-efficacy (p = 0.040) than did their family members, based on the self-reported outcome measures. There were no significant differences in the family functioning-related variables between patients and family members. The mean comparison between patients and family members (as assessed by Cohen’s d) showed a moderate effect size for mental HRQL and small effect sizes for resilience and general self-efficacy.
In the assessment of mental HRQL in patients and family members together, approximately one-third of the participants reported reduced mental HRQL (MCS <40). From a strength-based perspective, 24 participants (20%) demonstrated above-average mental HRQL according to the recommended score interpretation guidelines (MCS >55) (Wilson, Marsden-Loftus, et al., 2017). There are no established cut-off scores for interpreting the total RSA and GSE scores. However, 101 points represented the lowest quartile (25th percentiles) on the RSA and 28 points represented the lowest quartile (25th percentiles) on the GSE for all participants in the current study. Regarding family functioning, the average Circumplex ratio score indicated that the families had balanced family dynamics in terms of cohesion and flexibility levels (Circumplex ratio score >1). Moreover, 75 participants (60%) reported high or very high levels of family communication, and 50 participants (40%) reported high or very high family satisfaction. Table 2 displays the means, SDs, and test statistics of the outcome measures.
Table 2
Means, SDs, and test statistics of outcome measures
| Outcome measure | Patients | Family members | All participants | Test statistics (effect size, Cohen’s d) |
| MCS | 41.8 (9.9) | 47.9 (9.0) | 44.9 (9.9) | p = <0.001, (d = –0.63) |
| RSA | 107.2 (16.6) | 113.9 (16.2) | 110.6 (16.7) | p = 0.025 (d = –0.41) |
| GSE | 30.1 (5.1) | 31.9 (4.5) | 31.0 (4.9) | p = 0.040 (d = –0.38) |
| FACES IV | ||||
| Circumplex ratio | 3.0 (1.0) | 3.1 (1.2) | 3.1 (1.2) | p = 0.590 (d = –0.1) |
| FCS | 66.1 (26.2) | 67.3 (24.2) | 66.7 (25.2) | p = 0.798 (d = –0.05) |
| FSS | 56.0 (28.8) | 55.9 (26.2) | 55.9 (27.4) | p = 0.980 (d = 0.00) |
Abbreviations: MCS, Mental Component Summary; RSA, Resilience Scale for Adults; GSE, General Self-Efficacy scale; FACES IV, Family Adaptability and Cohesion Evaluation Scale, Fourth Edition.
3.1Correlation matrix
Table 3 displays Pearson’s correlation coefficients for all observed variables in the measurement model. All correlations were positive and significant (p < 0.05). Resilience and general self-efficacy were strongly correlated. Resilience was strongly and positively correlated with family functioning-related variables except for family communication (FCS), for which the correlation was medium. All family functioning-related variables were strongly correlated with each other, and family communication and family satisfaction showed the strongest correlation (0.81).
Table 3
Pearson’s correlations for self-reported outcome measures included in the model
| RSA | GSE | MCS | Circumplex | FCS | FSS | |
| RSA | 1.0000 | |||||
| GSE | 0.6114* | 1.0000 | ||||
| MCS | 0.5326* | 0.4710* | 1.0000 | |||
| Circumplex ratio | 0.5191* | 0.2933* | 0.2795ł | 1.0000 | ||
| FCS | 0.4801* | 0.2545ł | 0.2135ł | 0.6400* | 1.0000 | |
| FSS | 0.5364* | 0.3503ł | 0.3142ł | 0.6642* | 0.8172* | 1.0000 |
*P < 0.001, łP < 0.05. RSA, Resilience Scale for Adults; GSE, General Self-Efficacy scale; FCS, Family Communication Scale; FSS, Family Satisfaction Scale.
3.2Structural equation model
The final SEM model is shown in Fig. 1, displaying standardized coefficients and measurement error. All coefficients were significant (p < 0.001; see Table 4). The covariance between the two latent constructs—Protective factors and Family functioning—was 0.61, indicating a large effect size. For the latent Protective construct, resilience loaded most highly (0.93), followed by self-efficacy (0.66) and mental HRQL (0.58). For the Family construct, family satisfaction had the largest standardized correlation coefficient (0.93) followed by family communication (0.87) and overall family functioning (0.73). The final model indicated an acceptable fit to the data based on the following estimates: CFI = 0.97, TLI = 0.97, RMSEA = 0.07, and SPRM = 0.045. Table 4 displays the statistics for the SEM model including standardized coefficients, confidence intervals, p-values, and model-fit parameters.
Fig. 1
Structural equation model with standardized coefficients.
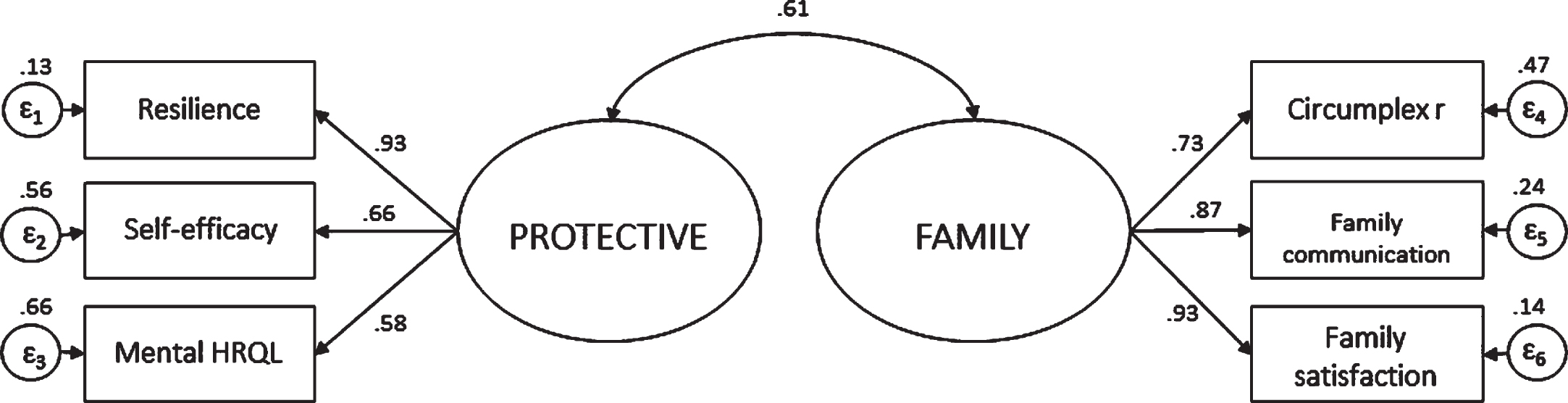
Table 4
Statistics for the structural equation model
| Measurement | Standardized β | 95% CI | p-value | |
| RSA - Protective | 0.93 | 0.83 | 1.03 | <0.001 |
| GSE - Protective | 0.66 | 0.53 | 0.78 | <0.001 |
| MCS - Protective | 0.58 | 0.44 | 0.72 | <0.001 |
| Circumplex ratio - Family | 0.73 | 0.64 | 0.82 | <0.001 |
| FCS – Family | 0.87 | 0.81 | 0.93 | <0.001 |
| FSS – Family | 0.93 | 0.87 | 0.98 | <0.001 |
| Covariance protective – Family | 0.61 | 0.48 | 0.74 | <0.001 |
| Fit statistics for the model | CFI | TLI | SPRM | RMSEA |
| 0.986 | 0.986 | 0.045 | 0.07 | |
RSA, Resilience Scale for Adults; GSE, General Self-Efficacy scale; MCS, Mental Component Summary; FCS, Family Communication Scale; FSS, Family Satisfaction Scale; CFI, Comparative Fit Index; TLI, Tucker-Lewis Index; SPRM, Standardized Root Mean Squared Residual; RMSEA, Root Mean Squared Error of Approximation.
4Discussion
This study aimed to explore the association between protective individual resources and overall family functioning in patients with TBI and their family members at baseline in a RCT of a family-based intervention. The results support our hypothesis that individual protective factors are strongly correlated with family functioning. Higher levels of protective resources—resilience, mental HRQL, and self-efficacy—were significantly and positively associated with family functioning, which were reflected in higher cohesion and flexibility in the family system, and family communication and satisfaction. Our findings support the whole-family approach recommended in TBI rehabilitation, emphasizing the importance of improving both individual and family functioning (Godwin et al., 2015).
The factor loadings for each latent variable were all >0.5, indicating that they defined the respective latent construct according to the suggested methodological recommendations for SEM analyses (Kang & Ahn, 2021). Family satisfaction and family communication had the largest standardized coefficients associated with the latent Family Functioning construct. However, the Circumplex ratio score representing the amount of cohesion and flexibility in the family also showed good convergent validity.
An underlying assumption of the family systems theory is the reciprocity among the members of the system, as well as the system as a whole (Verhaeghe et al., 2005). This study supports this assumption, showing that factors in the individual and family domains are strongly associated with each other. If the family manages to create a shared and collaborative response to TBI-related challenges, they are more likely to maintain a healthy and balanced family functioning (Godwin et al., 2015; Stejskal, 2012). We included both individuals with TBI and their family members, and thus, this study reflects patients’ and family members’ perspectives. This type of approach is necessary for a rehabilitation process, as it may improve all family members’ well-being and yield positive patient outcomes ( Vangel et al., 2011).
As the family perspective becomes increasingly acknowledged in the context of TBI rehabilitation ( Foster et al., 2012), family interventions targeting family functioning have been developed and tested in TBI populations ( Gauvin-Lepage et al., 2015; Lefebvre et al., 2007; Rasmussen et al., 2021; Winter et al., 2016). Although it is necessary to also acknowledge the challenges related to TBI, many of these interventions focus on enhancing the family resources to help families apply their abilities to overcome TBI-related challenges. However, a scoping review of family interventions following acquired brain injury concluded that the evidence of the effectiveness of family interventions is inconsistent, and identifying key components of the interventions has been challenging ( De Goumoëns et al., 2018). This may partly be due to the numerous reciprocal relationships that exist in family systems. Hence, the current study provides more insights into some of the complex relationships among outcomes that may be of interest from a strength-based perspective.
The factor resilience loaded most highly on the Protective construct. Although HRQL is among the most commonly used outcomes for the TBI population ( Polinder et al., 2013), our findings suggest that resilience should be included as an outcome of interest and that validated outcome measures should be implemented for both patients and family members in TBI rehabilitation. A previous study on individuals with TBI using a strength-based approach found a direct positive interaction between healthy family dynamics and mental HRQL ( Cariello et al., 2020). In the present study, the bivariate correlations revealed that among the observed variables linked to the Protective construct, resilience was more strongly correlated to the family functioning-related variables than mental HRQL and self-efficacy. In Rapport et al.’s study on individuals with TBI, screening for resilience levels was found to be important, as strength-based interventions may be more influential on well-being in those with low resilience levels (Rapport et al., 2020). Our findings also support the hypothesis that enhancing resilience in both patients and family members will positively influence the overall family functioning (Godwin & Kreutzer, 2013; Godwin et al., 2015).
A recent systematic review of resilience in family caregivers of persons living with chronic neurological conditions, including TBI, concluded that most studies have explored resilience in connection to negative outcomes such as caregiver burden ( McKenna et al., 2022). The literature on TBI suggests that higher levels of resilience are associated with lower levels of caregiver burden after acquired brain injury and spinal cord injury ( Las Hayas et al., 2015; Simpson & Jones, 2013). Considering that rehabilitation research has emphasized capacities and strengths rather than maladaptive responses (Evans, 2011), the focus on negative outcomes in studies of TBI resilience could be considered somewhat contradictory (McKenna et al., 2022). Sullivan et al. showed in their systematic review that resilience is most often used as a predictor rather than the outcome of interest (Sullivan et al., 2016). The present study is one of the first to demonstrate the association of positive resources in both patients and family members, including resilience, with positive aspects of the Family Functioning construct.
Although it is well known that TBI may negatively affect family functioning in both the short- and long-term (Cariello et al., 2020; Ergh et al., 2002; Gan et al., 2006; Schönberger et al., 2010), several studies have revealed that a significant proportion of families have reported healthy and balanced levels of cohesion, flexibility, and family communication following a TBI (Lehan et al., 2012; Perrin et al., 2013; Ponsford et al., 2003). Similarly, on average, the families in the present study reported balanced levels of cohesion and flexibility and a high level of family communication. Despite reporting a balanced family functioning, we found in a previous study on the same study population that both patients and their family members experience emotional distress, indicating that these individuals are burdened to some extent (Rasmussen et al., 2020). This observation accords with a study by Kreutzer et al., which showed that caregivers reporting healthy family functioning still experienced elevated levels of emotional distress ( Kreutzer et al., 1994). The presence of both negative and positive outcomes highlights the importance of assessing positive outcomes in addition to negative ones because it can help identify resources that can be further strengthened ( Dunst & Trivette, 2009).
Further, Ponsford et al. suggest that having access to a rehabilitation system might alleviate family distress following TBI (Ponsford et al., 2003). This is particularly relevant in the current study, as all individuals with TBI had received follow-up at a specialized TBI outpatient clinic at the time of participant enrollment. Nevertheless, previous studies have noted the importance of examining families that adjust and cope well following a family member’s TBI, as they can provide invaluable information about the factors associated with positive outcomes and growth (Ponsford et al., 2003; Vangel et al., 2011). Based on the results of the current study, families who maintain adequate communication levels and are satisfied with the family functioning may be more likely to have higher levels of individual protective resources. Both family communication and family satisfaction are important outcome measures of family functioning; they enable changes within the cohesion and flexibility dimensions, thereby improving the overall family function ( Olson et al., 2019). Furthermore, they can help identify families at risk of unhealthy family functioning because balanced families tend to have more positive communication than do unbalanced families (Olson et al., 2019). Family satisfaction is associated with lower levels of burden in caregivers of individuals with an acquired brain injury ( Tramonti et al., 2019); it also functions as a buffer against caregiver burden and distress following a TBI ( Coy et al., 2013; Vangel et al., 2011).
According to the family systems theory, individual behavior is the product of both individual and family functioning (Vangel et al., 2011). Our results reflect this notion, showing that individual resources and family function are closely connected, and suggest that identifying both personal and environmental factors is important in the rehabilitation process. Personal resources comprise factors such as social functioning, self-efficacy, and coping style, whereas environmental factors include family and social support (Dunst & Trivette, 2009; Nalder et al., 2019). Social support, in addition to health information, is rated among the most important needs by family members following a TBI ( Norup et al., 2015). Furthermore, social support and resources are predictors of family members’ HRQL and family functioning (Ergh et al., 2002; Sabella & Suchan, 2019). Social functioning and social resources are both embedded in the MCS and the RSA (Friborg et al., 2003; Ware & Gandek, 1994). It is, however, also possible that the families in the current study perceived that some of their needs were met through specialized follow-ups. Receiving information about the injury and available resources in the rehabilitation process can improve patients’ and family members’ sense of control and confidence, which in turn may strengthen protective factors such as resilience and HRQL (Hanks et al., 2016; Neils-Strunjas et al., 2017).
Expanding from an individualistic perspective to the family perspective might improve desirable outcomes in individuals with a TBI. A greater focus on positive outcomes rather than negative outcomes may be beneficial in TBI rehabilitation and the development of family-based interventions. If clinicians succeed in improving resources and competencies for both patients and their family members, it may improve the outcomes for the whole family.
4.1Strengths and limitations
A strength of this study is that protective and family resources were explored from a family perspective based on responses from individuals with TBI and their family members. Further, this study applied a novel approach for understanding factors that are associated with positive family outcomes after TBI.
Some limitations should be taken into account when interpreting the findings. First, multivariate methods, such as SEM, usually require a large sample size. The sample size of 122 in the present study might be considered somewhat small and limiting the significance of the results. However, the model-fit parameters showed an acceptable model fit to the data. Furthermore, multivariate methods have been recommended in rehabilitation research because they can provide unique insights into the complex rehabilitation process ( Peek, 2000). Second, although we included all TBI severities, the majority of the patients had sustained a mild TBI with a protracted course of recovery. Thus, our results may not apply to families facing more severe injuries. Third, there may have been a selection bias, as the families reported a generally healthy family functioning. Troubled families may have been hesitant to participate in an RCT that investigated an eight-week family intervention (Rasmussen et al., 2021). Nevertheless, several researchers have pointed to the importance of studying families that seem to cope well after TBI, as these families may provide invaluable insights into their characteristics (Ponsford et al., 2003; Vangel et al., 2011).
5Conclusion
Based on the model presented in this study, we propose an evaluation of the complex interaction between individual and family functioning in those who have experienced a TBI. Consistent with the family systems theory, the model showed that individual protective resources (resilience, self-efficacy, and mental HRQL) were strongly correlated with the overall family functioning factors (family cohesion, flexibility, communication, and satisfaction), with a large effect size. Resilience loaded most highly on the Protective construct, whereas family satisfaction loaded most highly on the Family Functioning construct. This study supports a change toward a more whole-family and resource-focused approach in TBI rehabilitation.
Acknowledgments
The authors thank Prof. Are Hugo Pripp for his advice and guidance in the statistical analyses. They also thank all patients and their family members for their participation in this study. They acknowledge the physicians at the specialized outpatient clinic who took part in the recruitment of patients and their families.
Conflict of interest
The authors state no potential conflicts of interest.
Funding
The study was supported by the DAM Foundation, Norway, under grant no. 2016/FO77196. The trial funders played no role in the study design, data collection, analysis and interpretation, writing of the manuscript, or decision to submit the article for publication.
Trial registration
The study was registered in the Clinical Trials Registry on December 22, 2016, under the identifier: NCT03000400.
References
1 | Aburn, G. , Gott, M. , & Hoare, K. ((2016) ). What is resilience? An Integrative Review of the empirical literature. Journal of Advanced Nursing, 72: (5), 980–1000. https://doi.org/10.1111/jan.12888 |
2 | Andelic, N. , Anke, A. , Skandsen, T. , Sigurdardottir, S. , Sandhaug, M. , Ader, T. , & Roe, C. ((2012) ). Incidence of hospital-admitted severe traumatic brain injury and in-hospital fatality in norway: A national cohort study. Neuroepidemiology, 38: (4), 259–267. https://doi.org/10.1159/000338032 |
3 | Anderson, M. I. , Daher, M. , & Simpson, G. K. ((2020) ). A predictive model of resilience among family caregivers supporting relatives with traumatic brain injury (TBI): A structural equation modelling approach. Neuropsychological Rehabilitation, 30: (10), 1925–1946. https://doi.org/10.1080/09602011.2019.1620787 |
4 | Association for theAdvancement of Automotive Medicine. (2008). The Abbriviated Injuy Scale (AIS) 2005. Association for the Advancement of Automotive Medicine. Retrieved 01.02.2021 from https://www.aaam.org/abbreviated-injuy-scale-ais/ |
5 | Bayen, E. , Jourdan, C. , Ghout, I. , Darnoux, E. , Azerad, S. , Vallat-Azouvi, C. , Weiss, J. J. , Aegerter, P. , Pradat-Diehl, P. , Joël, M. E. , & Azouvi, P. ((2016) ). Objective and subjective burden of informal caregivers 4 years after a severe traumatic brain injury: Results from the pariS-TBI study. E-E. Journal of Head Trauma Rehabilitation, 31: (5), 67 https://doi.org/10.1097/htr.0000000000000079 |
6 | Bonanno, G. A. ((2004) ). Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events?. American Psychologist, 59: (1), 20–28. https://doi.org/10.1016/j.jsurg.2016.07.008. |
7 | Bonanno, G. A. ((2005) ). Clarifying and Extending the Construct of Adult Resilience. The American psychologist, 60: (3), 265–267. https://doi.org/10.1037/0003-066X.60.3.265b |
8 | Brands, I. M. H. , Verlinden, I. , & Ribbers, G. M. ((2019) ). A study of the influence of cognitive complaints, cognitive performance and symptoms of anxiety and depression on self-efficacy in patients with acquired brain injury. Clinical Rehabilitation, 33: (2), 327–334. https://doi.org/10.1177/0269215518795249 |
9 | Cariello, A. N. , Perrin, P. B. , Rodríguez-Agudelo, Y. , Plaza, S. L. O. , Quijano-Martinez, M. C. , & Arango-Lasprilla, J. C. ((2020) ). A multi-site study of traumatic brain injury in mexico and colombia: Longitudinal mediational and cross-lagged models of family dynamics, coping, and health-related quality of life. International Journal of Environmental Research and Public Health, 17: (17), 1–16.https://doi.org/10.3390/ijerph17176045 |
10 | Cohen, J. ((1992) ). A power primer. Psychological bulletin, 112: (1), 155–159.https://doi.org/10.1037/0033-2909.112.1.155 |
11 | Coy, A. E. M. S. , Perrin, P. B. P. , Stevens, L. F. P. , Hubbard, R. M. S. , Díaz Sosa D. M. B. A. , Espinosa Jove I. G. M. D. , & Arango-Lasprilla, J. C. P. ((2013) ). Moderated mediation path analysis of mexican traumatic brain injury patient social functioning, family functioning, and caregiver mental health. Archives of Physical Medicine and Rehabilitation, 94: (2), 362–368. https://doi.org/10.1016/j.apmr.2012.08.210 |
12 | De Goumoëns V. , Rio, L. M. , Jaques, C. , & Ramelet, A. -S. ((2018) ). Family-oriented interventions for adults with acquired brain injury and their families: A scoping review. JBI Database System Rev Implement Rep, 16: (12), 2330–2367. https://doi.org/10.11124/JBISRIR-2017-003846 |
13 | Dimitrov, D. M. ((2006) ). Comparing groups on latent variables: A structural equation modeling approach. Work, 26: (4), 429–436. |
14 | Dunst, C. J. , & Trivette, C. M. ((2009) ). Capacity-building family-systems intervention practices. Journal of Family Social Work, 12: (2), 119–143.https://doi.org10.1080/10522150802713322 |
15 | Ennis, N. , Rosenbloom, B. N. , Canzian, S. , & Topolovec-Vranic, J. ((2013) ). Depression and anxiety in parent versus spouse caregivers of adult patients with traumatic brain injury: A systematic review. Neuropsychological Rehabilitation, 23: (1), 1–18.https://doi.org/10.1080/09602011.2012.712871 |
16 | Ergh, T. C. , Rapport, L. J. , Coleman, R. D. , & Hanks, R. A. ((2002) ). Predictors of caregiver and family functioning following traumatic brain injury: Social support moderates caregiver distress. Journal of Head Trauma Rehabilitation, 17: (2), 155–174. https://doi.org/10.1097/00001199-200204000-00006 |
17 | Evans, J. J. ((2011) ). Positive Psychology and Brain Injury Rehabilitation. Brain Impairment, 12: (2), 117–127.https://doi.org/10.1375/brim.12.2.117. |
18 | Forslund, M. V. , Perrin, P. B. , Sigurdardottir, S. , Howe, E. I. , van Walsem M. R. , Arango-Lasprilla, J. C. , Lu, J. , Aza, A. , Jerstad, T. , Roe C. , & Andelic, N. ((2021) ). Health-related quality of life trajectories across 10 years after moderate to severe traumatic brain injury in norway. J Clin Med, 10: (1), 157–https://doi.org/10.1016/j.jsurg.2016.07.00810.3390/jcm10010157 |
19 | Foster, A. M. , Armstrong, J. , Buckley, A. , Sherry, J. , Young, T. , Foliaki, S. , James-Hohaia, T. M. , Theadom, A. , & McPherson, K. M. ((2012) ). Encouraging family engagement in the rehabilitation process: A rehabilitation provider’s development of support strategies for family members of people with traumatic brain injury. Disability and Rehabilitation, 34: (22), 1855–1862. https://doi.org/10.3109/09638288.2012.670028 |
20 | Friborg, O. , Hjemdal, O. , Martinussen, M. , & Rosenvinge, J. H. ((2009) ). Empirical support for resilience as more than the counterpart and absence of vulnerability and symptoms of mental disorder. Journal of individual differences, 30: (3), 138–151 https://doi.org/10.1027/1614-0001.30.3.138 |
21 | Friborg, O. , Hjemdal, O. , Rosenvinge, J. H. , & Martinussen, M. ((2003) ). A new rating scale for adult resilience: What are the central protective resources behind healthy adjustment?. Int J Methods Psychiatr Res, 12: (2), 65–76 https://doi.org/10.1002/mpr.143 |
22 | Gan, C. , Campbell, K. A. , Gemeinhardt, M. , & McFadden, G. T. ((2006) ). Predictors of family system functioning after brain injury. Brain Injury, 20: (6), 587–600 https://doi.org/10.1080/02699050600743725 |
23 | Gauvin-Lepage, J. , Lefebvre, H. , & Malo, D. ((2015) ). Family resilience following a physical trauma and efficient support interventions: A critical literature review. The Journal of Rehabilitation, 81: (3), 34–42. |
24 | Godwin, E. E. , & Kreutzer, J. S. ((2013) ). Embracing a new path to emotional recovery: Adopting resilience theory in post-TBI psychotherapy. Brain Injury, 27: (6), 637–639 https://doi.org/10.3109/02699052.2012.750745 |
25 | Godwin, E. E. , Lukow Ii H. R. , & Lichiello, S. ((2015) ). Promoting resilience following traumatic brain injury: Application of an interdisciplinary, evidence-based model for intervention. Fam Relat, 64: (3), 347–362 https://doi.org/10.1111/fare.121228 |
26 | Hagen, C. , Malkmus, D. , Durham, P. Levels of cognitive functioning, Rehabilitation of the Head Injured Adult; Comprehensive Physical Management. http://file.lacounty.gov/SDSInter/dhs/218111RLOCFFamilyGuideEnglish.pdf |
27 | Hanks, R. A. , Rapport, L. J. , Waldron Perrine B. , & Millis, S. R. ((2016) ). Correlates of resilience in the first 5 years after traumatic brain injury. Rehabilitation Psychology, 61: (3), 269–276 https://doi.org/10.1016/j.jsurg.2016.07.00810.1037/rep0000069 |
28 | Hu, L.-T. , & Bentler, P. M. ((1999) ). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural equation modeling, 6: (1), 1–55 https://doi.org/10.1080/10705519909540118 |
29 | King, G. , Nalder, E. , Stacey, L. , & Hartman, L. R. ((2021) ). Investigating the adaptation of caregivers of people with traumatic brain injury: A journey told in evolving research traditions. Disability and Rehabilitation, 43: (21), 3102–3116 https://doi.org/10.1080/09638288.2020.1725158 |
30 | Kreutzer, J. S. , Gervasio, A. H. , & Camplair, P. S. ((1994) ). Primary caregivers’ psychological status and family functioning after traumatic brain injury. Brain Injury, 8: (3), 197–210 https://doi.org/10.3109/02699059409150973 |
31 | Las Hayas C. , López de Arroyabe E. , & Calvete, E. ((2015) ). Resilience in family caregivers of persons with acquired brain injury. Rehabilitation Psychology, 60: (3), 295–302 https://doi.org/10.1037/rep0000040 |
32 | Lefebvre, H. , Pelchat, D. , & Levert, M. -J. ((2007) ). Interdisciplinary family intervention program: A partnership among health professionals, traumatic brain injury patients, and caregiving relatives. Journal of Trauma Nursing, 14: (2), 4900–4113 https://doi.org/10.1097/01.JTN.0000278797.51407.d5 |
33 | Lehan, T. J. , Stevens, L. F. , Arango-Lasprilla, J. C. , Díaz Sosa D. M. , & Espinosa Jove I. G. ((2012) ). Balancing act: The influence of adaptability and cohesion on satisfaction and communication in families facing TBI in Mexico. Neuro Rehabilitation, 30: (1), 75–86 https://doi.org10.3233/NRE-2012-0729 |
34 | Luszczynska, A. , Scholz, U. , & Schwarzer, R. ((2005) ). The general self-efficacy scale: Multicultural validation studies. Journal of Psychology, 139: (5), 439–457 https://doi.org/10.3200/JRLP.139.5.439-457 |
35 | Marwitz, J. H. , Sima, A. P. , Kreutzer, J. S. , Dreer, L. E. , Bergquist, T. F. , Zafonte, R. , Johnson-Greene, D. , & Felix, E. R. ((2018) ). Longitudinal examination of resilience after traumatic brain injury: A traumatic brain injury model systems study. Archives of Physical Medicine and Rehabilitation, 99: (2), 264–271 https://doi.org/10.1016/j.jsurg.2016.07.00810.1016/j.apmr.2017.06.013 |
36 | McKenna, O. , Fakolade, A. , Cardwell, K. , Langlois, N. , Jiang, K. , & Pilutti, L. A. ((2022) ). Towards conceptual convergence: A systematic review of psychological resilience in family caregivers of persons living with chronic neurological conditions. Health Expectations, 25: (1), 4–37 https://doi.org/10.1111/hex.13374 |
37 | Nalder, E. , Hartman, L. , Hunt, A. , & King, G. ((2019) ). Traumatic brain injury resiliency model: A conceptual model to guide rehabilitation research and practice. Disability and Rehabilitation, 41: (22), 2708–2717 https://doi.org/10.1080/09638288.2018.1474495 |
38 | Neils-Strunjas, J. , Paul, D. , Clark, A. N. , Mudar, R. , Duff, M. C. , Waldron-Perrine, B. , & Bechtold, K. T. ((2017) ). Role of resilience in the rehabilitation of adults with acquired brain injury. Brain Injury, 31: (2), 131–139 https://doi.org/10.1080/02699052.2016.1229032 |
39 | Norup, A. ((2018) ). Family matters in neurorehabilitation: Why, when, who, and how?. Revista Iberoamericana de Neuropsicologia, 1: (1), 17–31. |
40 | Norup, A. , Perrin, P. B. , Cuberos-Urbano, G. , Anke, A. , Andelic, N. , Doyle, S. T. , Quijano, M. C. , Caracuel, A. , Sosa, D. M. D. , Jove, I. G. E. , & Arango-Lasprilla, J. C. ((2015) ). Family needs after brain injury: A cross cultural study. NeuroRehabilitation, 36: (2), 203–214 https://doi.org/10.3233/NRE-151208 |
41 | Olson, D. ((2011) ). FACES IV and the Circumplex Model: Validation Study. Journal of Marital and Family Therapy, 37: (1), 64–80 https://doi.org/10.1111/j.1752-0606.2009.00175.x |
42 | Olson, D. H. , Waldvogel, L. , & Schlieff, M. ((2019) ). Circumplex model of marital and family systems: An update. Journal of Family Theory & Review, 11: (2), 199–211 https://doi.org/10.1111/jftr.12331 |
43 | Peek, M. K. ((2000) ). Structural equation modeling and rehabilitationresearch. Am J Phys Med Rehabil, 79: (3), 301–309 https://doi.org/10.1097/00002060-200005000-00014 |
44 | Perrin, P. B. , Stevens, L. F. , Sutter, M. , Hubbard, R. , Díaz Sosa D. M. , Espinosa Jove I. G. , & Arango-Lasprilla, J. C. ((2013) ). Exploring the connections between traumatic brain injury caregiver mental health and family dynamics in Mexico City, Mexico. Pm r, 5: (10), 839–849 https://doi.org/10.1016/j.pmrj.2013.05.018 |
45 | Polinder, S. , Cnossen, M. , Real, R. G. L. , Covic, A. , Gorbunova, A. , Voormolen, D. , Master, C. L. , Haagsma, J. , Diaz-Arrastia, R. , & Von Steinbuechel N. ((2018) ). A multidimensional approach to post-concussion symptoms in mild traumatic brain injury. Frontiers in Neurology, 9: (1113), 1–14 https://doi.org/10.3389/fneur.2018.01113 |
46 | Polinder, S. P. , Haagsma, J. A. P. , Steyerberg, E. W. P. , & van Beeck E. F. P. ((2013) ). Health-related quality of life in persons after traumatic brain injury: A systematic review of the literature. The Lancet (British edition), 381: (S2), S116–S116.https://doi.org/10.1016/S0140-6736(13)61370-7 |
47 | Ponsford, J. , Olver, J. , Ponsford, M. , & Nelms, R. ((2003) ). Long-term adjustment of families following traumatic brain injury where comprehensive rehabilitation has been provided. Brain Injury, 17: (6), 453–468 https://doi.org/10.1080/0269905031000070143 |
48 | Rapport, L. J. , Wong, C. G. , & Hanks, R. A. ((2020) ). Resilience and well-being after traumatic brain injury. Disability and Rehabilitation, 42: (14), 2049–2055 https://doi.org/10.1080/09638288.2018.1552327 |
49 | Rasmussen, M. S. , Andelic, N. , Pripp, A. H. , Nordenmark, T. H. , & Soberg, H. L. ((2021) ). The effectiveness of a family-centred intervention after traumatic brain injury: A pragmatic randomised controlled trial. Clinical Rehabilitation,35: (10), 1428–1441. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8495317/pdf/10.117702692155211010369.pdf |
50 | Rasmussen, M. S. , Arango-Lasprilla, J. C. , Andelic, N. , Nordenmark, T. H. , & Soberg, H. L. ((2020) ). Mental health and family functioning in patients and their family members after traumatic brain injury: A cross-sectional study. Brain Sciences, 10: (10), 1–14 https://doi.org/10.3390/brainsci10100670 |
51 | Scheenen, M. E. , van der Horn H. J. , de Koning M. E. , van der Naalt J. , & Spikman, J. M. ((2017) ). Stability of coping and the role of self-efficacy in the first year following mild traumatic brain injury. Soc Sci Med, 181: (May), 184–190 https://doi.org/10.1016/j.socscimed.2017.03.025 |
52 | Scholten, E. W. M. , Ketelaar, M. , Visser-Meily, J. M. A. , Stolwijk-Swüste, J. , van Nes I. J. W. , Gobets, D. , van Laake - Geelen C. C. M. , Stolwijk, J. , Dijkstra, C. A. , Agterhof, E. , Gobets, D. , Maas, E. M. , van der Werf, H. , de Boer C. E. , Beurskens, M. , van Nes I. , van Diemen T. , Woldendorp, K. H. , Hurkmans, J. , & Post M. W. M. ((2020) ). Self-efficacy predicts personal and family adjustment among persons with spinal cord injury or acquired brain injury and their significant others: A dyadic approach. Archives of Physical Medicine and Rehabilitation, 101: (11), 1937–1945 https://doi.org/10.1016/j.apmr.2020.06.003 |
53 | Schwarzer, R. , & Jerusalem, M. ((1995) ). Generalized self-efficacy scale. Weinman, J., S., & Johnston, M.. Measures in health psychology: A user’s portfolio. Causal and control beliefs, 35: , 37. |
54 | Schwarzer, R. , Warner, L. M. Perceived Self-Efficacy and its Relationship to Resilience. In (pp. 139–150). NewYork, NY: Springer New York. https://doi.org/10.1007/978-1-4614-9634939-310 |
55 | Schönberger, M. , Ponsford, J. , Olver, J. , & Ponsford, M. ((2010) ). A longitudinal study of family functioning after TBI and relatives’ emotional status. Neuropsychological Rehabilitation, 20: (6), 813–829 https://doi.org/10.1080/09602011003620077 |
56 | Seligman, M. E. P. , & Csikszentmihalyi, M. ((2000) ). Positive psychology: An introduction. The American psychologist, 55: (1), 5–14 https://doi.org/10.1037/0003-066X.55.1.5 (Positive Psychology) |
57 | Simpson, G. , & Jones, K. ((2013) ). How important is resilience among family members supporting relatives with traumatic brain injury or spinal cord injury?. Clinical Rehabilitation, 27: (4), 367–377 https://doi.org/10.1177/0269215512457961 |
58 | Simpson, G. K. , Anderson, M. I. , Daher, M. , Jones, K. F. , & Morey, P. ((2021) ). Testing a model of resilience in family members of relatives with traumatic brain injury vs spinal cord injury: Multigroup analysis. Archives of Physical Medicine and Rehabilitation, 102: (12), 2325–2334 https://doi.org/10.1016/j.apmr.2021.06.0168 |
59 | Stejskal, T. M. ((2012) ). Removing barriers to rehabilitation: Theory-based family intervention in community settings after brain injury. NeuroRehabilitation, 31: (1), 75–83 https://doi.org/10.3233/NRE-2012-0776 |
60 | Sullivan, K. A. , Kempe, C. B. , Edmed, S. L. , & Bonanno, G. A. ((2016) ). Resilience and other possible outcomes after mild traumatic brain injury: A systematic review. Neuropsychology Review, 26: (2), 173–185 https://doi.org/10.1007/s11065-016-9317-1 |
61 | Teasedale, G. , & Benett, B. ((1975) ). Assessment of coma: Teasdale, G., and Jennett, D. (), ‘Assessment of coma and impaired consciousness’, Lancet. Injury, 6: (3), 265–265 https://doi.org/10.1016/0020-1383(75)90136-9 |
62 | Tramonti, F. , Bonfiglio, L. , Bongioanni, P. , Belviso, C. , Fanciullacci, C. , Rossi, B. , Chisari, C. , & Carboncini, M. C. ((2019) ). Caregiver burden and family functioning in different neurological diseases. Psychology, Health & Medicine,, 24: (1), 27–34 https://doi.org/10.1080/13548506.2018.1510131 |
63 | Vangel, S. J. , Rapport, L. J. , & Hanks, R. A. ((2011) ). Effects of family and caregiver psychosocial functioning on outcomes in persons with traumatic brain injury. Journal of Head Trauma Rehabilitation, 26: (1), 20–29 https://doi.org/10.1097/HTR.0b013e318204a70d |
64 | Verhaeghe, S. , Defloor, T. , & Grypdonck, M. ((2005) ). Stress and coping among families of patients with traumatic brain injury: A review of the literature. Journal of Clinical Nursing, 14: (8), 1004–1012 https://doi.org/10.1111/j.1365-2702.2005.01126.x |
65 | Walsh, F. ((2003) ). Family resilience: A framework for clinical practice. Family Process, 42: (1), 1–18 https://doi.org/10.1111/j.1545-5300.2003.00001.x |
66 | Ware, J. J. E. , & Gandek, B. ((1994) ). The SF-36 health survey: Development and use in mental health research and the IQOLA project. International Journal of Mental Health, 23: (2), 49–73 https://doi.org/10.1080/00207411.1994.11449283 |
67 | Wilson, L. , Marsden-Loftus, I. , Koskinen, S. , Bakx, W. , Bullinger, M. , Formisano, R. , Maas, A. , Neugebauer, E. , Powell, J. , Sarajuuri, J. , Sasse, N. , von Steinbuechel N. , von Wild K. , & Truelle, J.-L. ((2017) ). Interpreting quality of life after brain injury scores: Cross-walk with the short form-. Journal of Neurotrauma, 34: (1), 59–65 https://doi.org/10.1089/neu.2015.4287 |
68 | Wilson, L. , Stewart, W. , Dams-O’Connor, K. , Diaz-Arrastia, R. , Horton, L. , Menon, D. K. , & Polinder, S. ((2017) ). The chronic and evolving neurological consequences of traumatic brain injury. Lancet Neurology, 16: (10), 813–825 https://doi.org/10.1016/S1474-4422(17)30279-X |
69 | Winter, L. , Moriarty, H. J. , Robinson, K. , Piersol, C. V. , Vause-Earland, T. , Newhart, B. , Iacovone, D. B. , Hodgson, N. , & Gitlin, L. N. ((2016) ). Efficacy and acceptability of a home-based, family-inclusive intervention for veterans with TBI: A randomized controlled trial. Brain Injury, 30: (4), 373–387 https://doi.org/10.3109/02699052.2016.1144080 |
70 | Wolf, E. J. , Harrington, K. M. , Clark, S. L. , & Miller, M. W. ((2013) ). Sample size requirements for structural equation models: An evaluation of power, bias, and solution propriety. Educational and Psychological Measurement, 73: (6), 913–934. |




