Does acupuncture therapy improve language function of patients with aphasia following ischemic stroke? A systematic review and meta-analysis
Abstract
BACKGROUND:
Aphasia is one of the most common complications in patients with ischemic stroke. Studies have shown that acupuncture can improve the symptoms of aphasia patients. However, the effect of acupuncture on language function in patients with ischemic stroke is still controversial.
OBJECTIVE:
This study aimed to critically assess the efficacy and safety of acupuncture for aphasia following ischemic stroke.
METHODS:
PubMed, Embase, Cochrane Central Register of Controlled Trials, Web of Science Core Collection, China National Knowledge Infrastructure, Wanfang Digital Periodicals, and Chinese Science and Technology Periodicals database were searched. All randomized controlled trials (RCTs) that met the criteria were included.
RESULTS:
Meta-analyses showed that mean difference in change of auditory comprehension score (MD = 7.71, 95% CI: 1.83 to 13.59, P = 0.01), spontaneous speech (MD = 2.77, 95% CI: 0.59 to 4.95, P = 0.01), repetition score (MD = 14.48, 95% CI: 11.04 to 17.91, P < 0.00001) and naming score (MD = 14.60, 95% CI: 11.33 to 17.88, P < 0.00001) measured by WAB scale were statistically significant. Subgroup analyses demonstrated that there were statistically significant mean differences in four items of WAB scale in patients with sub-acute stroke, and no statistically significant differences in patients with acute stroke.
CONCLUSION:
The present study suggests that acupuncture may improve the language function of patients with aphasia following ischemic stroke, especially during the sub-acute phase. However, due to insufficient sample sizes and information on the safety, more high-quality RCTs are still needed
1Introduction
Stroke is one of the leading causes of death and disease burden worldwide (Strong, Mathers, & Bonita, 2007). Ischemic stroke is the most common type of stroke (Feigin, Norrving, & Mensah, 2017). Aphasia is one of the most common complications in patients with ischemic stroke. For example, a prospective study showed that the incidence of aphasia was 30% in patients with first-ever ischemic stroke (Engelter et al., 2006). Inatomi et al. found that 15.2% of patients experienced aphasia during the acute phase of ischemic stroke (2008). Wu et al. indicated that the prevalence of aphasia was 16.93% in patients with acute ischemic stroke (2020). Aphasia after stroke may be associated with cardioembolism cognitive impairments, and contributes to poor survival, increased long-term mortality, and high costs (Wu et al., 2020; Ellis, Simpson, Bonilha, Mauldin, & Simpson, 2012; El Hachioui et al., 2014; Laska, Hellblom, Murray, Kahan, & Von Arbin, 2001).
There are many pharmacological and non-pharmacological interventions for aphasia in patients with stroke (Greener, Enderby, & Whurr, 2001; Picano, Quadrini, Pisano, & Marangolo, 2021). However, there was only a Class-I recommendation with a level of evidence A that speech and language therapy (SLT) was effective for aphasia following stroke according to the latest guideline from the American Heart Association/American Stroke Association (Winstein et al., 2016). A 2016 Cochrane systematic review also indicated that SLT was beneficial for improving functional communication in patients with aphasia following stroke (Brady, Kelly, Godwin, Enderby, & Campbell, 2016). However, it remains unsatisfactory after SLT rehabilitation alone (Nouwens et al., 2017). Guidelines for Stroke Prevention and Treatment in China point out that there is no consensus on the optimal frequency, optimal intensity, time distribution or duration of SLT for post-stroke aphasia (2021). A latest review indicated that unconventional treatments as an adjunct to conventional interventions were still needed for aphasia rehabilitation (Picano, Quadrini, Pisano, & Marangolo, 2021).
Acupuncture therapy is an important part of complementary and alternative medicine (Mccubbin, Kempe, & Beck, 2017), which has been used for thousands of years in China. It has been considered as adjunctive therapy for some complications of stroke (such as dysphagia and hemiplegic shoulder pain) in a recent clinical guideline (Winstein et al., 2016). A systematic review has verified the effectiveness and safety of acupuncture in reversing neurological impairments during post-stroke rehabilitation (Yang et al., 2016). A piece of level-B evidence showed that acupuncture might be beneficial for post-stroke aphasia according to a clinical guideline in China (Zhang et al., 2019). A clinical study has suggested the efficacy of acupuncture for aphasia after stroke, which can reduce the degree of aphasia (Wu, Hu, Wen, Li, & Fu, 2016). However, acupuncture was also not mentioned in the latest review investigating the efficacy of new adjunctive approaches for post-stroke aphasia (Picano, Quadrini, Pisano, & Marangolo, 2021). Due to insufficient sample sizes, it is still unclear whether acupuncture therapy can improve the language function of patients with aphasia following ischemic stroke. Also, the safety of acupuncture for aphasia following ischemic stroke has not been assessed. Therefore, this systematic review aimed to critically assess the efficacy and safety of acupuncture for aphasia following ischemic stroke.
2Method
This study was registered in PROSPERO (No. CRD42021230262) and conducted according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) statement.
2.1Criteria for considering studies for this review
2.1.1Types of participants
Patients who suffered from aphasia of any type after ischemic stroke were eligible. Patients were diagnosed with ischemic stroke according to acknow-ledged diagnostic criteria, such as the World Health Organization criteria, computerized tomography, and magnetic resonance imaging (Stroke, 1989; Cheng et al., 2015). Aphasia was defined by recognized diagnostic criteria or tools, such as Western Aphasia Battery (WAB), and Aphasia Battery of Chinese (ABC) (Shewan, & Kertesz, 1980; Gao et al., 1992).
2.1.2Types of interventions
Experimental intervention was acupuncture combined with SLT. Control interventions included SLT alone or combined with sham acupuncture. Two comparisons (acupuncture plus SLT versus SLT, and acupuncture plus SLT versus SLT plus sham acupuncture) were investigated if possible. Type, frequency, or course of acupuncture and SLT was unrestricted.
2.1.3Types of outcome measures
Primary outcome measures included change from baseline in WAB score and Aphasia Quotient (AQ) after treatment. WAB is an internationally recognized scale to test aphasia impairment level (Wallace et al., 2019) and includes seven areas: spontaneous speech, auditory comprehension, repetition, naming, reading and writing, praxis, and construction (Shewan, & Kertesz, 1980; Crary, & Gonzalez Rothi, 1989). AQ is a weighted scoring of four areas in WAB (spontaneous speech, auditory comprehension, repetition, and naming) to assess the severity of the spoken language deficit in aphasia (Crary, & Gonzalez Rothi, 1989). The higher score of any area or AQ indicates the milder language impairment.
Secondary outcome measures included change from baseline in ABC, Clinical Rehabilitation Research Center Aphasia Examination (CRRCAE), Chinese Functional Communication Profile (CFCP), Comprehensive Activities of Daily Living (CADL) after treatment, etc. Adverse reactions were also assessed if possible. ABC is a Chinese-specific scale to evaluate aphasia impairment level in adults (Gao et al., 1992). CRRCAE is also a Chinese-specific scale to quantificationally assess the severity of aphasia (Zhang et al., 2005). CFCP is a stroke-specific scale to evaluate the ability of functional communication in aphasia patients (Wang, & Zhuo, 1992). CADL can be used to assess comprehensive activities of daily living in stroke patients with satisfactory reliability and validity (Hsueh, Wang, Liou, Lin, & Hsieh, 2012).
2.1.4Types of studies
Randomized controlled trials (RCTs) as the gold standard for evaluating efficacy of interventions were included regardless of language, publication date or status. Grey literatures that met the eligible criteria was also included. Quasi-RCTs were excluded to reduce selection bias.
2.2Search methods for identifying studies
PubMed, Embase, Cochrane Central Register of Controlled Trials, Web of Science Core Collection, China National Knowledge Infrastructure, Wanfang Digital Periodicals, and Chinese Science and Technology Periodicals database were searched from inception to April 2021. A detailed search strategy is available in the Appendix. We also checked the reference lists of eligible studies, the WHO International Clinical Trials Registry Platform, Chinese Clinical Trial Registry, and ClinicalTrials.gov to identify any other eligible studies.
2.3Selection of studies
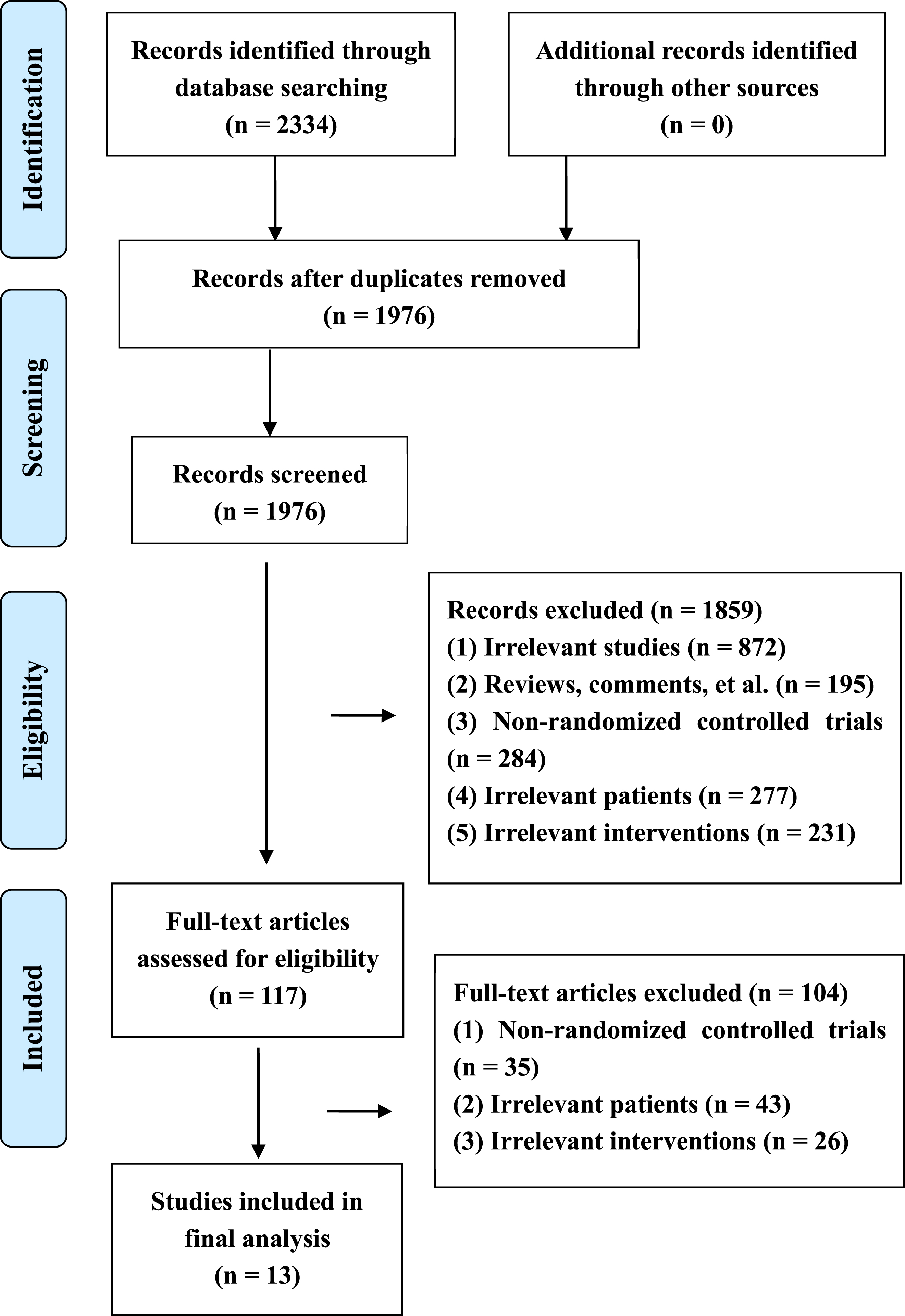
Selection of studies was completed independently by two reviewers (TH, MLZ). Duplicates and irrelevant publications were excluded by checking the title and abstract. Full texts of the remaining studies were checked for inclusion. The disagreement between the two reviewers was solved by a third reviewer (CYQ). The selection process is presented in a PRISMA flowchart (Fig. 1).
Fig. 1
PRISMA flow diagram of study retrieval and selection.
2.4Data extraction and management
Two authors (TH, BFZ) independently extracted information on designs, participants, interventions, outcomes, etc. A third review author (SZD) was involved to solve disagreements. If necessary, authors identified from original studies were asked for additional information.
2.5Assessment of risk of bias in included studies
Risk of bias of included studies was assessed by two review authors (BMS, JBZ) independently using Cochrane’s ‘Risk of bias’ tool (Higgins et al., 2021). This tool includes seven important items on randomization, allocation concealment, blinding, outcome data, outcome reporting, etc. Any item is graded as high, low, or unclear risk of bias according to the relevant information from included studies. Any disagreement was resolved by a third reviewer (SZD).
2.6Statistical analysis
Dichotomous outcomes were described using risk ratios (RR) with 95% confidence intervals (CIs). Mean difference (MD) with CIs was used as effect size for continuous outcomes. Change of continuous variables from baseline after treatment was estimated according to methods from Cochrane handbook and an assumptive correlation coefficient of 0.5 (Higgins et al., 2021; Follmann, Elliott, Suh, & Cutler, 1992). Statistical heterogeneity was assessed by chi-square test and I2 value. We used the meta-analysis with fixed-effects model (P > 0.10 and I2 < 50%) or random-effects model ((P≤0.10 or I2≥50%) to estimate overall effect size. A narrative description was conducted if a meta-analysis was not feasible. The meta-analysis was performed by RevMan 5.3 software. If possible, subgroup analysis was conducted based on acute (first 14 days) and sub-acute phase (from 15 days to 6 months) after ischemic stroke (Godecke et al., 2021; Bath, Lee, & Everton, 2018; Gao et al., 2018). Publication bias was assessed by the funnel plot or Egger’s test for a meta-analysis involving more than ten studies.
3Results
3.1Literature search
We obtained 2334 potentially eligible studies through an extensive search. Three hundred and fifty-eight duplicates were deleted by EndNote software. After checking titles and abstracts, 1859 irrelevant studies were excluded. Then, we read full texts of the remaining studies for inclusion. Finally, thirteen eligible studies (Liu et al., 2006; Luo, Tan, & Huang, 2008; Sun, Ji, Cui, Chen, & Wang, 2010; Luo, Huang, & Zhu, 2010; Mu et al., 2010; Wu et al., 2010; Dong, 2011; Li, Xiao, Wang, Xiong, & Huang, 2013; Zhou, Song, Li, & Li, 2015; Wang, & Li, 2015; Xiong, Zhang, Guo, Fan, & Zhang, 2016; Song et al., 2019; Zhong, 2019) were included for statistical analysis. The screening process is presented in Fig. 1.
3.2Characteristics of included studies
The characteristics of included studies are showed in Table 1. These studies involved 848 patients, and were published from 2006 to 2019. Sample size ranged from 15 to 60 in each group. Three studies included patients with acute stroke, five studies with sub-acute stroke, and others with acute and sub-acute stroke. Nine studies included patients with Broca’s aphasia, one with Broca’s and Basal ganglion aphasia. The remaining studies did not report the type of aphasia. Acupuncture plus SLT in experimental group and SLT alone in control group were used in all of eligible studies. The frequency of acupuncture ranged from 3 to 7 times a week. The course of acupuncture ranged from 20 days to 16 weeks. The reported outcome measures included WAB, AQ, ABC, CFCP, CRRCAE, CADL, and BDAE. Adverse reactions were not reported in any included study.
Table 1
Characteristics of included studies
| Author, year | Number of patients in experimental group | Number of patients in control group | Type of aphasia | Phase (course) of stroke | Experimental interventions | Control interventions | Frequency of acupuncture | Duration of acupuncture | Outcome measures |
| Liu, 2006 | 30 | 28 | Broca, Basal ganglion | Acute (< 14 days) | TA + SLT | SLT | 7 times a week | 30 days | CRRCAE |
| Luo, 2008 | 30 | 30 | Broca | Acute and sub-acute (< 6 months) | TA + SLT | SLT | 6 times a week | 30 days | ABC |
| Sun, 2010 | 30 | 30 | Unclear | Acute and sub-acute (7 to 59 days) | TA + SLT | SLT | 5 times a week | 4 weeks | ABC |
| Luo, 2010 | 30 | 30 | Broca | Acute and sub-acute (< 6 months) | TA + SLT | SLT | 5 times a week | 30 days | ABC |
| Mu, 2010 | 30 | 30 | Broca | Sub-acute (15 to 90 days) | TA + SLT | SLT | 5 times a week | 30 days | WAB,AQ, CADL |
| Wu, 2010 | 15 | 15 | Broca | Sub-acute (1 to 6 months) | TA + SLT | SLT | 7 times a week | 20 days | BDAE, CRRCAE |
| Dong, 2011 | 30 | 30 | Broca | Acute (7 to 10 days) | TA + SLT | SLT | 5 times a week | 30 days | ABC |
| Li, 2013 | 28 | 29 | Broca | Acute (< 14 days) | TA + SLT | SLT | Unclear | 4 weeks | WAB, AQ |
| Zhou, 2015 | 38 | 36 | Unclear | Sub-acute (3 to 6 months) | TA + SLT | SLT | 3 times a week | 4 weeks | ABC, CFCP |
| Wang, 2015 | 20 | 20 | Broca | Acute and sub-acute (1 to 24 days) | TA + SLT | SLT | 6 times a week | 4 weeks | ABC, CFCP |
| Xiong, 2016 | 32 | 32 | Broca | Sub-acute (20 to 54 days) | TA + SLT | SLT | 5 times a week | 5 weeks | WAB,AQ,CFCP |
| Song, 2019 | 35 in each group | 35 | Unclear | Sub-acute | (1)TA + SLT;(2) TA + electroacupuncture + SLT | SLT | 5 times a week | 16 weeks | ABC |
| Zhong, 2019 | 60 | 60 | Broca | Acute and sub-acute (10 to 30 days) | TA + SLT | SLT | Unclear | Unclear | BDAE,CADL |
Abbreviations: TA, traditional acupuncture; SLT, speech and language therapy; WAB, Western Aphasia Battery; AQ, Aphasia Quotient; ABC, Aphasia Battery of Chinese; CFCP, Chinese Functional Communication Profile; CRRCAE, Clinical Rehabilitation Research Center Aphasia Examination; CADL, Comprehensive Activities of Daily Living; BDAE, Boston Diagnostic Aphasia Examination.
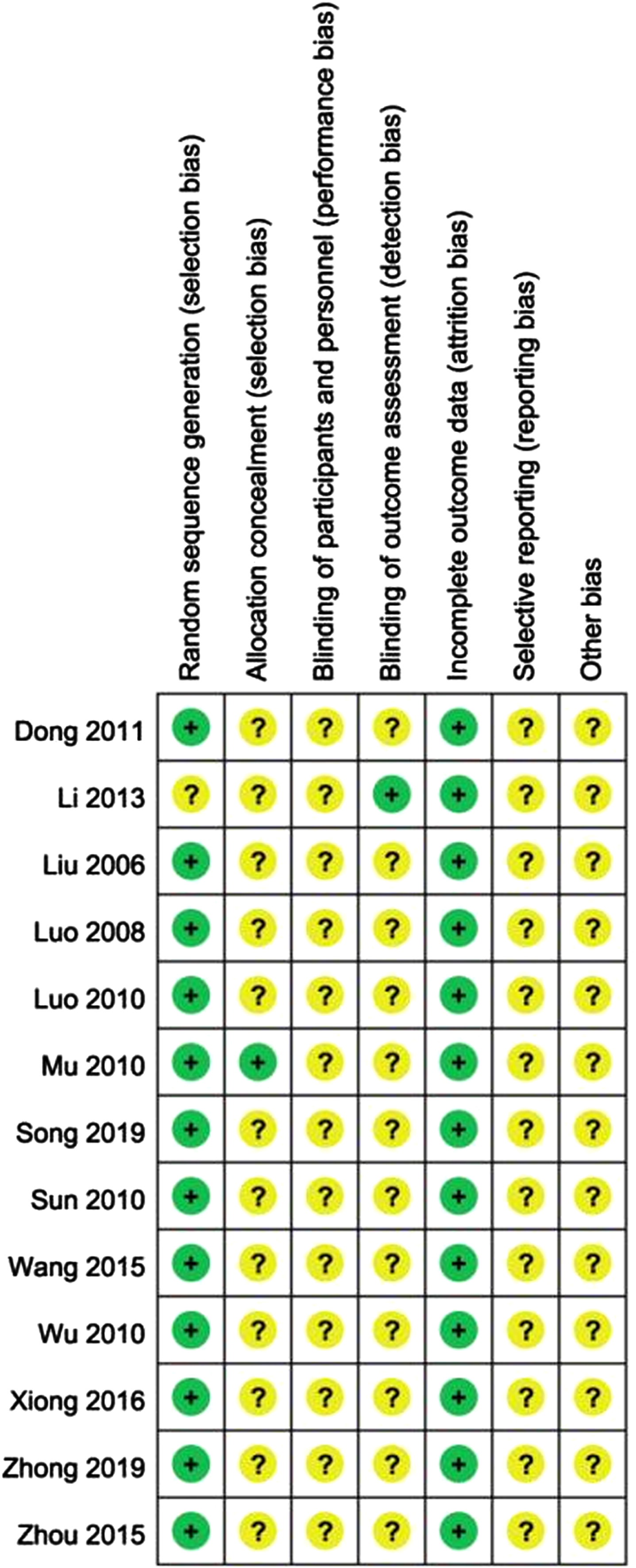
3.3Assessment of risk of bias
The results of assessment of risk of bias are presented in Fig. 2. Twelve studies used random number table to generate random sequence. Only one did not report the method of generating random sequence. Opaque and sealed envelope was used to reduce selection bias in one study. Other studies did not report the method to conceal allocation. Outcome assessor was blinded in one study. Because of insufficient information, risk of bias in blinding item was graded as unclear in other studies. Attrition bias was low, and reporting and other bias were unclear in all of included studies.
Fig. 2
Risk of bias summary.
3.4Primary outcomes
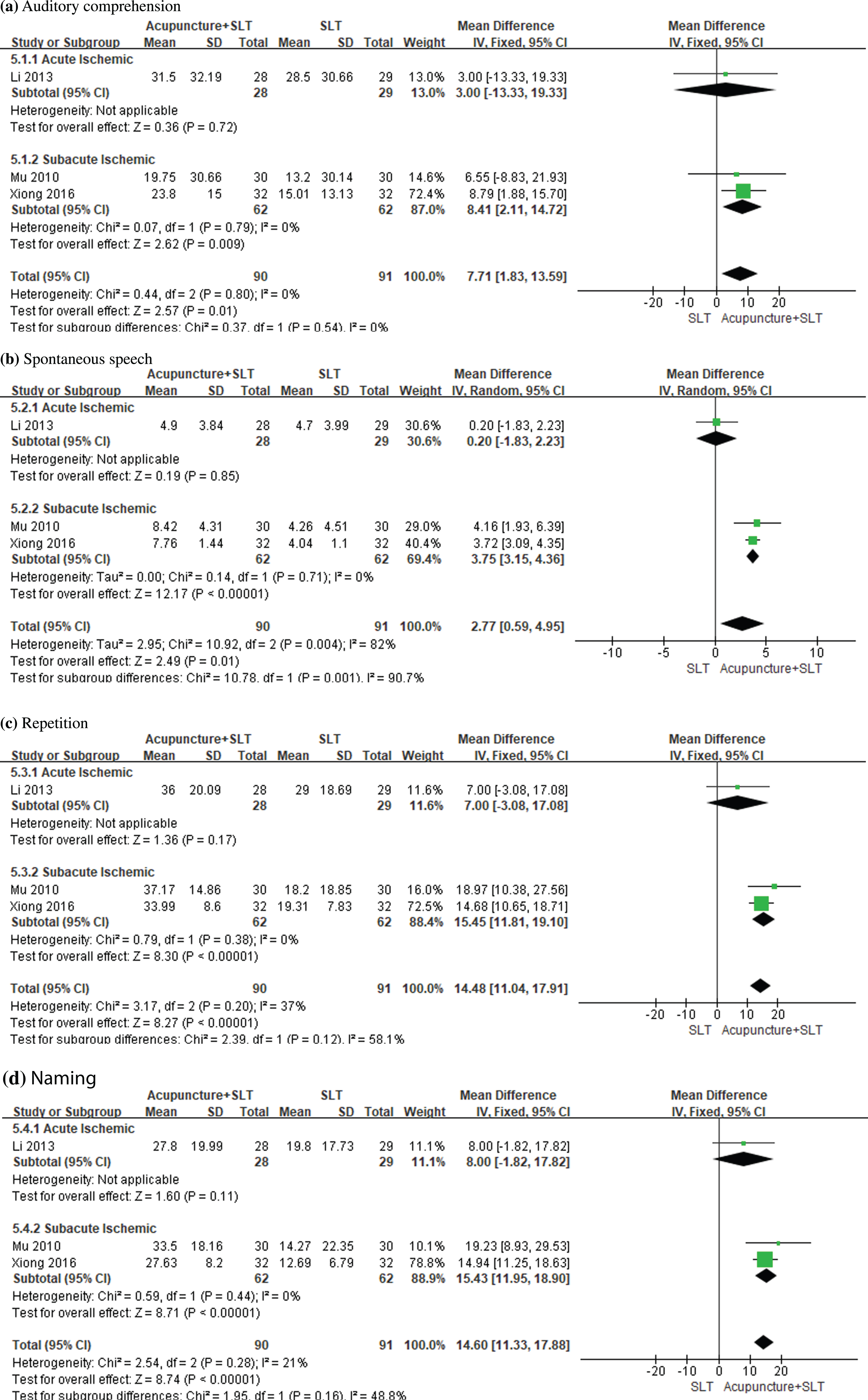
3.4.1Change of any item score in WAB (follow-up minus baseline)
WAB was reported in three eligible studies. The results of meta-analyses are presented in Fig. 3. Meta-analyses showed that mean difference (acupuncture + SLT minus SLT) in change of auditory comprehension score (MD = 7.71, 95% CI: 1.83 to 13.59, P = 0.01), spontaneous speech (MD = 2.77, 95% CI: 0.59 to 4.95, P = 0.01), repetition score (MD = 14.48, 95% CI: 11.04 to 17.91, P < 0.00001) and naming score (MD = 14.60, 95% CI: 11.33 to 17.88, P < 0.00001) were statistically significant. Subgroup analyses demonstrated that there were statistically significant mean differences in the four items in patients with sub-acute stroke, and no statistically significant differences in the four items in patients with acute stroke.
Fig. 3
Forest plots of acupuncture plus SLT versus SLT for WAB score.
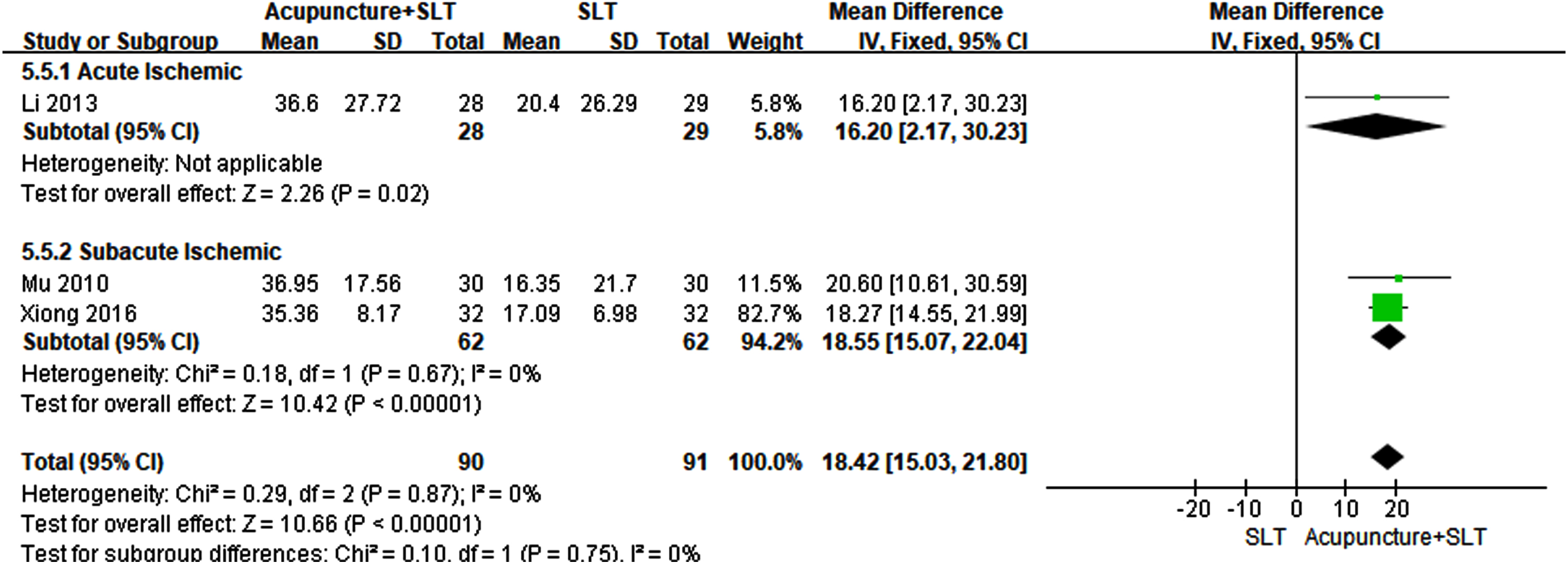
3.4.2Change of AQ (follow-up minus baseline)
Three eligible studies reported AQ value. The meta-analysis indicated that change of AQ in acupuncture plus SLT group was statistically higher than that in SLT group (MD = 18.42, 95% CI: 15.03 to 21.80, P < 0.00001). The statistically significant mean difference was also found in a subgroup analysis based on acute and sub-acute stroke (Fig. 4).
Fig. 4
Forest plots of acupuncture plus SLT versus SLT for AQ score.
3.5Secondary outcomes
3.5.1Change of any item score in ABC (follow-up minus baseline)
ABC was reported in six eligible studies. The results of meta-analyses are presented in Fig. 5. According to meta-analyses, change of auditory comprehension score (MD = 8.49, 95% CI: 1.51 to 15.47, P = 0.02) and repetition score (MD = 10.11, 95% CI: 5.91 to 14.32, P < 0.00001) in acupuncture plus SLT group was significantly higher than that in SLT group. However, no statistically significant mean difference (acupuncture + SLT minus SLT) was found in change of spontaneous speech score (MD = 11.54, 95% CI: –6.33 to 29.42, P = 0.21) and naming score (MD = 4.13, 95% CI: –0.43 to 8.69, P = 0.08).
Fig. 5
Forest plots of acupuncture plus SLT versus SLT for ABC score.
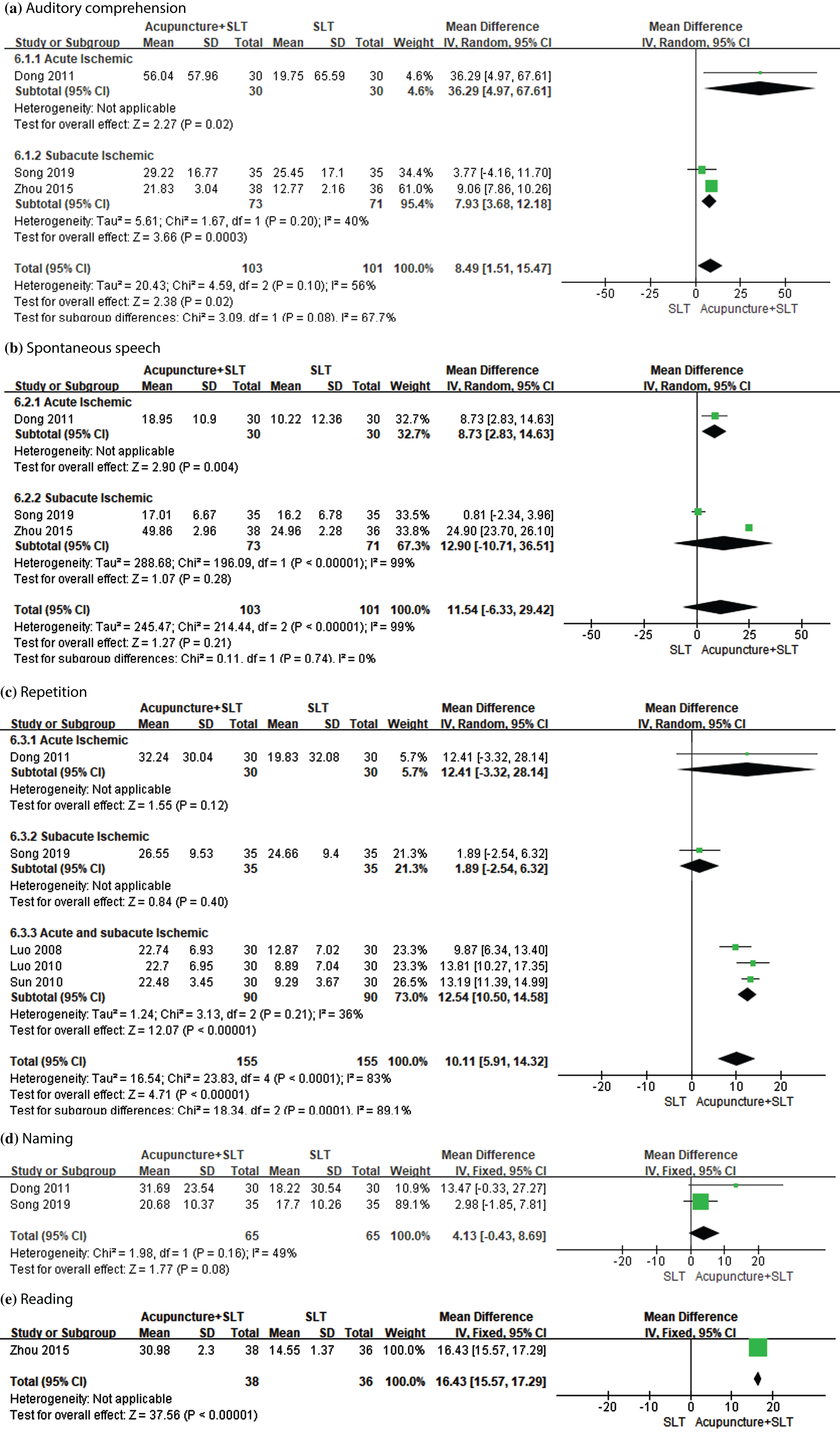
The results of subgroup analyses based on acute and sub-acute stroke found that mean difference (acupuncture + SLT minus SLT) in change of auditory comprehension and spontaneous speech score was statistically significant in patients with acute stroke. Change of auditory comprehension score in acupuncture plus SLT group was significantly higher than that in SLT group in patients with sub-acute stroke. Acupuncture plus SLT could significantly increase repetition score compared with SLT alone in patients with acute and sub-acute stroke.
One trial comparing traditional acupuncture +electroacupuncture + SLT with SLT alone found statistically significant mean difference in change of auditory comprehension score (MD = 49.44, 95% CI: 40.07 to 58.81, P < 0.00001), spontaneous speech (MD = 25.02, 95% CI: 21.60 to 28.44, P < 0.00001), repetition score (MD = 21.79, 95% CI: 17.30 to 26.28, P < 0.00001) and naming score (MD = 29.61, 95% CI: 24.58 to 34.64, P < 0.00001), respectively.
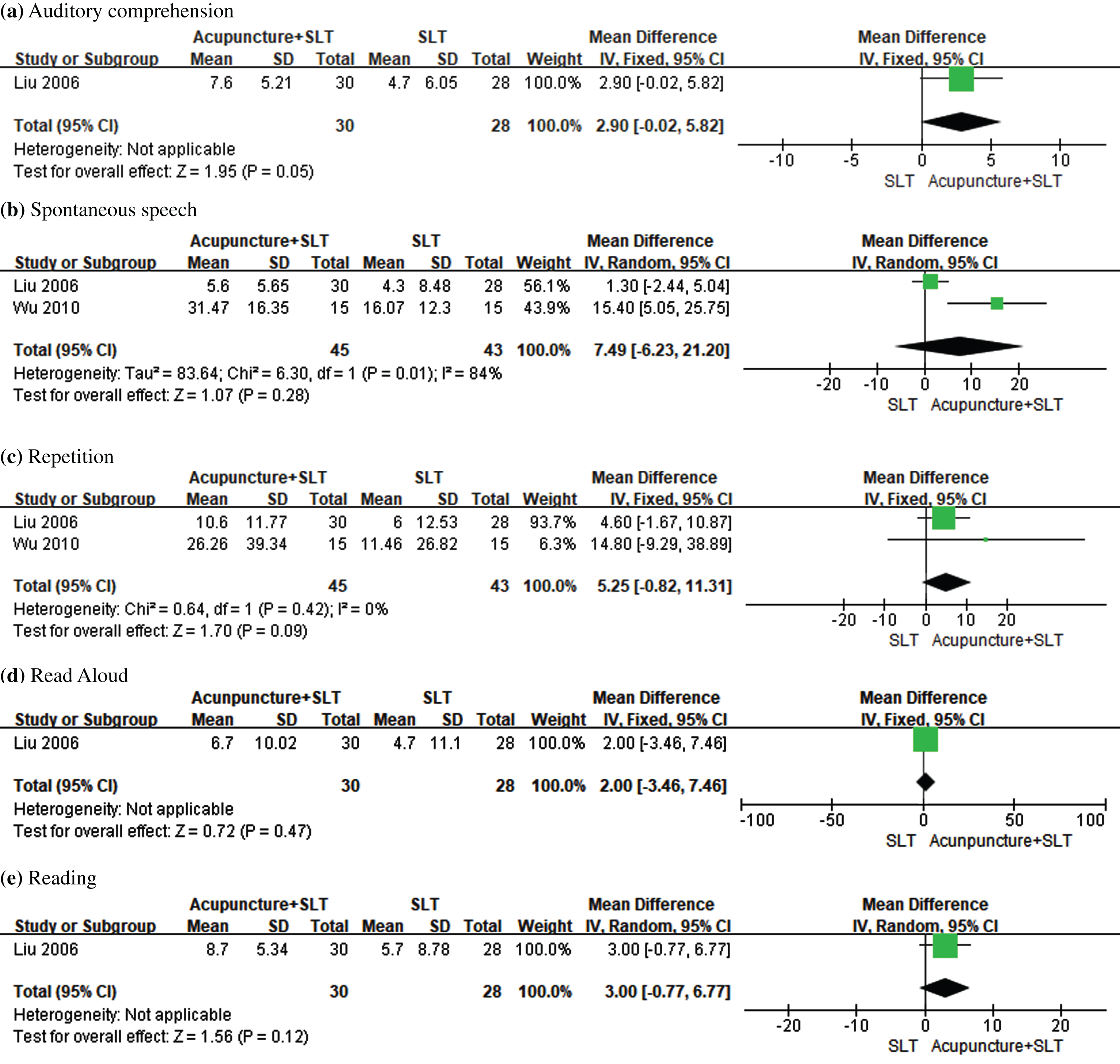
3.5.2Change of any item score in CRRCAE (follow-up minus baseline)
Three trials reported CRRCAE score. In Fig. 6, the results of meta-analyses found no statistically significant difference in change of spontaneous speech score (MD = 7.49, 95% CI: –6.23 to 21.20, P = 0.28) and repetition score (MD = 5.25, 95% CI: –0.82 to 11.31, P = 0.09) between two groups. Subgroup analyses showed that change of spontaneous speech score in acupuncture plus SLT group was significantly higher than that in SLT group in patients with sub-acute stroke. No statistically significant mean difference (acupuncture + SLT minus SLT) in change of other CRRCAE item scores was identified in patients with acute or sub-acute stroke.
Fig. 6
Forest plots of acupuncture plus SLT versus SLT for CRRCAE score.
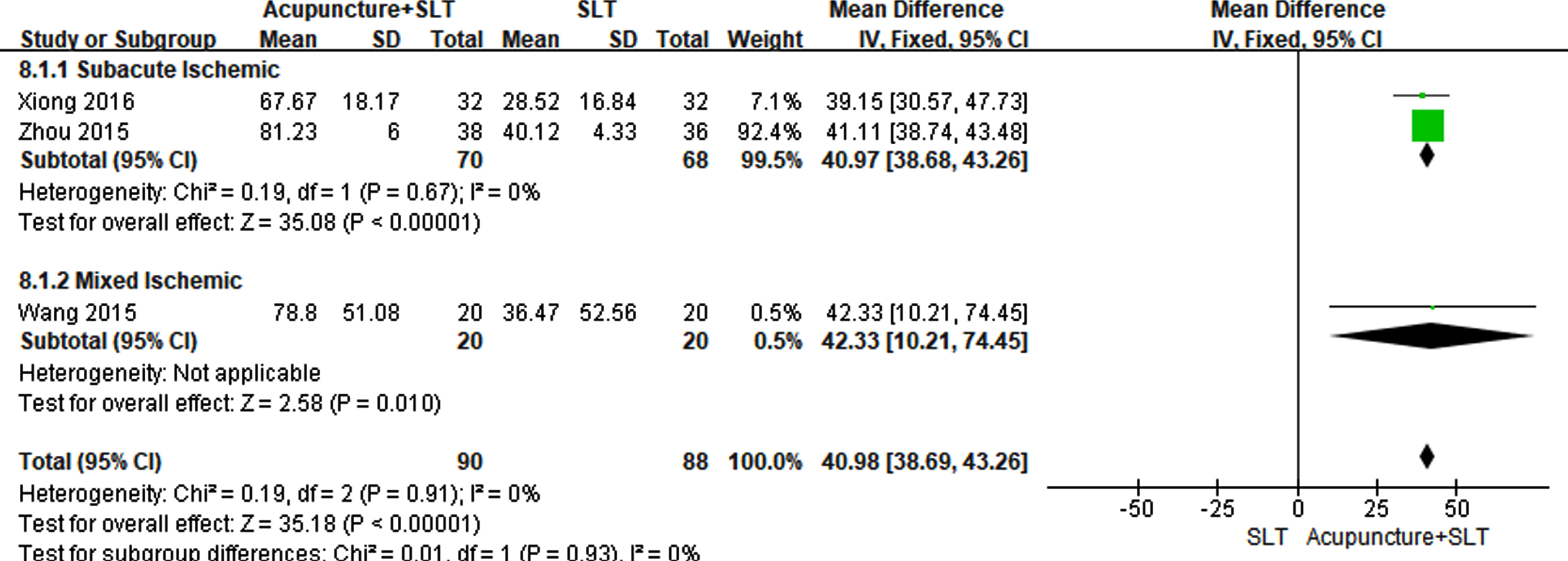
3.5.3Change of CFCP score (follow-up minus baseline)
One meta-analysis showed that change of CFCP score in acupuncture plus SLT group was statistically higher (MD = 40.98, 95% CI: 38.69 to 43.26, P < 0.00001) than that in SLT group in Fig. 7. Subgroup analyses showed that mean difference (acupuncture + SLT minus SLT) in change of CFCP score was statistically significant in two trials involving patients with sub-acute stroke (MD = 40.97, 95% CI: 38.68 to 43.26, P < 0.00001) and one trial involving patients with acute and sub-acute stroke (MD = 42.33, 95% CI: 10.21 to 74.45, P = 0.01), respectively.
Fig. 7
Forest plots of acupuncture plus SLT versus SLT for CFCP score.
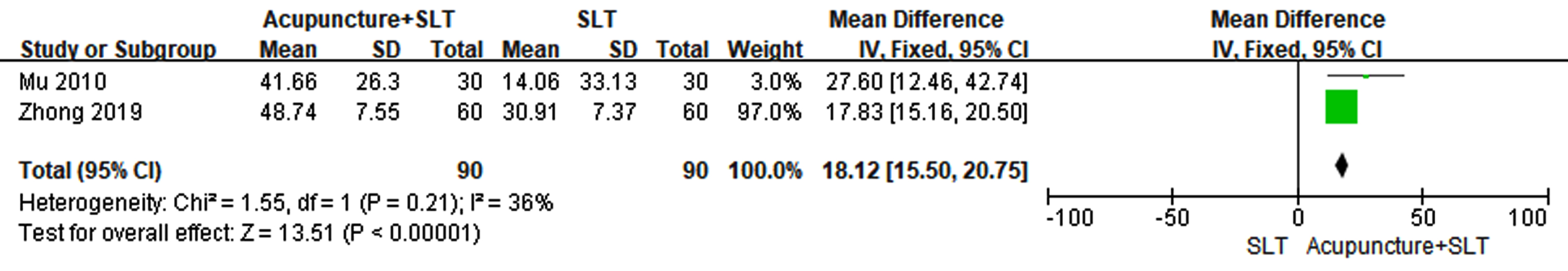
3.5.4Change of CADL score (follow-up minus baseline)
One meta-analysis showed that change of CADL score in acupuncture plus SLT group was significantly higher than that in SLT group (MD = 18.12, 95% CI: 15.50 to 20.75, P < 0.00001) in Fig. 8. Subgroup analyses showed that mean difference (acupuncture + SLT minus SLT) in change of CADL score was statistically significant in one trial involving patients with sub-acute stroke (MD = 27.60, 95% CI: 12.46 to 42.74, P = 0.0004) and one trial involving patients with acute and sub-acute stroke (MD = 17.83, 95% CI: 15.16 to 20.50, P < 0.00001), respectively.
Fig. 8
Forest plots of acupuncture plus SLT versus SLT for CADL score.
3.5.5Adverse reactions
No trials reported adverse reactions.
3.6Publication bias
Publication bias was not assessed by funnel plots because of no meta-analyses involving more than ten studies.
4Discussion
4.1Main findings and comparisons with existing literature
The present study is the first systematic review to critically assess the efficacy and safety of acupuncture for aphasia following ischemic stroke. SLT was recommended for treating aphasia following stroke according to a latest guideline (Winstein et al., 2016). Our meta-analysis showed that acupuncture combined with SLT significantly improved auditory comprehension, spontaneous speech, repetition, and naming items measured by WAB scale compared with SLT alone. No previous systematic reviews conducted the subgroup analysis based on acute and sub-acute ischemic stroke to assess the improvement in language functioning between acupuncture plus SLT and SLT alone (Zhang et al., 2019; Tang, Tang, Yang, Wu, & Shen, 2019). In this study, significant improvements in the above-mentioned four items in WAB scale were also found in patients with sub-acute ischemic stroke. However, there were no significant differences in the above-mentioned four items in WAB scale between acupuncture plus SLT and SLT alone in patients with acute ischemic stroke. AQ can be used to assess the severity of the spoken language deficit in aphasia (Crary, & Gonzalez Rothi, 1989). An increase in AQ score indicates an improvement in language impairment. The results from a meta-analysis involving three studies showed that acupuncture plus SLT could significantly increase AQ score compared with SLT alone in patients with aphasia following ischemic stroke. However, comparisons with existing literature were restricted because no previous systematic reviews on acupuncture for post-stroke aphasia reported AQ score (Zhang et al., 2019; Tang, Tang, Yang, Wu, & Shen, 2019). A recent review found that the optimal timing of SLT for aphasia after stroke was inconclusive (Nouwens et al., 2015). In this study, a subgroup analysis found that AQ score was increased significantly after acupuncture plus SLT treatment compared with SLT alone in patients with both acute and sub-acute stroke. It suggests that acupuncture may have beneficial effects on aphasia after ischemic stroke, especially during the sub-acute phase.
In a previous systematic review, pooled effects were estimated with the standard mean difference due to the heterogeneity of measurement tools (Zhang et al., 2019). In this study, pooled effects were estimated conservatively based on WAB, ABC, and CRRCAE scale, respectively. Heterogeneous results from different measurement tools were identified. For example, no statistically significant difference was found between the two groups in spontaneous speech item in ABC scale. The use of acupuncture for aphasia following ischemic stroke may be restricted in making clinical decisions due to heterogeneous results of the meta-analyses. More high-quality RCTs on this topic are still needed.
Wallace et al. developed the Research Outcome Measurement in Aphasia (ROMA) consensus statement to measure core outcomes for patients with post-stroke aphasia in 2019 (2019). ROMA includes Western Aphasia Battery Revised (WAB-R), General Health Questionnaire (GHQ), and Stroke and Aphasia Quality of Life Scale (SAQOL-39). In the present study, WAB was considered as the primary outcome measure, and only three of thirteen included studies reported WAB score. However, WAB was used as a secondary outcome measure in a previous systematic review (Zhang et al., 2019). GHQ and SAQOL-39 were not reported in systematic reviews on this topic. The heterogeneity of reported outcomes may lead to the difficulty of combining and comparing results from different studies and waste of resources. Therefore, it is recommended to use ROMA in further studies of acupuncture for aphasia following ischemic stroke.
Functional magnetic resonance imaging (fMRI) has been widely used to investigate the mechanisms of language function recovery in patients with post-stroke aphasia (Smits, Visch-Brink, van de Sandt-Koenderman, & van der Lugt, 2012). Time to peak (TTP) is a blood oxygen level-dependent signal measured by fMRI. A study found that the TTP in the left perisylvian area in 3 patients with stroke-induced aphasia was increased significantly compared with normal participants (Bonakdarpour, Parrish, & Thompson, 2007). Another study showed that patients with aphasia following stroke had longer TTP in the left hemisphere naming network than healthy individuals (Bonakdarpour, Beeson, DeMarco, & Rapcsak, 2015). A negative correlation was found between WAB-AQ and TTP in the naming network (Bonakdarpour, Beeson, DeMarco, & Rapcsak, 2015). A regression analysis showed that improvement in AQ was associated with blood oxygen level-dependent activation in the speech area after acupuncture treatment in patients with post-stroke aphasia (Chau, Fai Cheung, Jiang, Au-Yeung, & Li, 2010). A review reported that acupuncture had modulatory effects in multiple brain regions (Bai, & Lao, 2013). A study found that acupuncture might induce some specific patterns of brain activity in healthy participants (Yan et al., 2005). (Li et al. reported that the brain on the lesion side might be activated by acupuncture in patients with aphasia after stroke (2011). Our findings may be explained partly by the above-mentioned evidence.
4.2Limitations
This systematic review has some limitations. Effect size may be overestimated due to the small sample size. The incidence of aphasia was different between men and women after stroke (Wallentin 2018). However, no subgroup analysis based on gender was conducted because of insufficient information. In addition, the subgroup analysis based on the type of aphasia was also not conducted because the type of aphasia was not provided in some included studies.
5Conclusions
The present study suggests that acupuncture may improve the language function of patients with aphasia following ischemic stroke, especially during the sub-acute phase. However, due to insufficient sample sizes and information on the safety, more high-quality RCTs are still needed.
Conflict of interest
The authors declare that they have no competing interests.
Funding
This study was funded by the National Key Research and Development Program of China (No. 2018YFC1706001).
SUPPLEMENTARY MATERIAL
[1] The supplementary material is available in the electronic version of this article: https://dx.doi.org/10.3233/NRE-220007.
References
1 | Bai, L. , & Lao, L. ((2013) ). Neurobiological foundations of acupuncture: the relevance and future prospect based on neuroimaging evidence. Evidence-based Complementary and Alternative Medicine, eCAM, 812568. https://doi.org/10.1155/2013/812568 |
2 | Bath, P. M. , Lee, H. S. , & Everton, L. F. ((2018) ). Swallowing therapy for dysphagia in acute and subacute stroke. The Cochrane Database of Systematic Reviews, 10: (10), CD000323. https://doi.org/10.1002/14651858.CD000323.pub3 |
3 | Bonakdarpour, B. , Parrish, T. B. , & Thompson, C. K. ((2007) ). Hemodynamic response function in patients with strokeinduced aphasia: implications for fMRI data analysis. NeuroImage, 36: (2), 322–331. https://doi.org/10.1016/j.neuroimage.2007.02.035 |
4 | Bonakdarpour, B. , Beeson, P. M. , DeMarco, A. T. , & Rapcsak, S. Z. ((2015) ). Variability in blood oxygen level dependent (BOLD) signal in patients with stroke-induced and primary progressive aphasia. NeuroImage. Clinical, 8: , 87–94. https://doi.org/10.1016/j.nicl.2015.03.014 |
5 | Brady, M. C. , Kelly, H. , Godwin, J. , Enderby, P. , & Campbell, P. ((2016) ). Speech and language therapy for aphasia following stroke. The Cochrane Database of Systematic Reviews, 2016: (6), CD000425. https://doi.org/10.1002/14651858.000425.pub4 |
6 | Chau, A. C. , Fai Cheung, R. T. , Jiang, X. , Au-Yeung, P. K. , & Li, L. S. ((2010) ). An fMRI study showing the effect of acupuncture in chronic stage stroke patients with aphasia. Journal of Acupuncture and Meridian Studies, 3: (1), 53–57. https://doi.org/10.1016/S2005-2901(10)60009-X |
7 | Cheng, D. , Qu, Z. , Huang, J. , Xiao, Y. , Luo, H. , & Wang, J. ((2015) ). Motivational interviewing for improving recovery after stroke. The Cochrane Database of Systematic Reviews, 2015: (6), CD011398. https://doi.org/10.1002/14651858.CD011398.pub2 |
8 | Crary, M. A. , & Gonzalez Rothi, L. J. ((1989) ). Predicting the Western Aphasia Battery Aphasia Quotient. The Journal of Speech and Hearing Disorders, 54: (2), 163–166. https://doi.org/10.1044/jshd.5402.163 |
9 | Dong, B. J. ((2011) ). Study of the combination of scalp acupuncture and body acupuncture in treating acute ischemic stroke patients with Broca aphasia, M. A. Thesis. Beijing: Beijing University of Chinese Medicine. |
10 | El Hachioui, H. , Visch-Brink, E. G. , Lingsma, H. F. , van de Sandt-Koenderman, M. W. , Dippel, D. W. , Koudstaal, P. J. , & Middelkoop, H. A. ((2014) ). Nonlinguistic cognitive impairment in poststroke aphasia: a prospective study. Neurorehabilitation and Neural Repair, 28: (3), 273–281. https://doi.org/10.1177/1545968313508467 |
11 | Ellis, C. , Simpson, A. N. , Bonilha, H. , Mauldin, P. D. , & Simpson, K. N. ((2012) ). The one-year attributable cost of poststroke aphasia. Stroke, 43: (5), 1429–1431. https://doi.org/10.1161/STROKEAHA.111.647339 |
12 | Engelter, S. T. , Gostynski, M. , Papa, S. , Frei, M. , Born, C. , Ajdacic-Gross, V. ,... Lyrer P. A. ((2006) ). Epidemiology of aphasia attributable to first ischemic stroke: incidence, severity, fluency, etiology, and thrombolysis. Stroke, 37: (6), 1379–1384. https://doi.org/10.1161/01.STR.0000221815.64093.8c |
13 | Feigin, V. L. , Norrving, B. , & Mensah, G. A. ((2017) ). Global Burden of Stroke. Circulation Research, 120: (3), 439–448. https://doi.org/10.1161/CIRCRESAHA.116.308413 |
14 | Follmann, D. , Elliott, P. , Suh, I. , & Cutler, J. ((1992) ). Variance imputation for overviews of clinical trials with continuous response. Journal of Clinical Epidemiology, 45: (7), 769–773. https://doi.org/10.1016/0895-4356(92)90054-q |
15 | Gao, S. R. , Chu, Y. F. , Shi, S. Q. , Peng, Y. , Dai, S. D. , Wang, Y. H. ,... Zhao, H. M. ((1992) ). Research on standardization of Chinese aphasia examination. Chinese Mental Health Journal, 6: (3), 125–128 + 143. https://doi:10.3321/j.issn:10006729.1992.03.011. |
16 | Gao, C. Y. , Wu, C. H. , Zhao, J. G. , Cao, X. L. , Xu, B. Y. , Wu, B. S. ,... Zhang, X. J. ((2018) ). Guidelines for the Diagnosis and Treatment of Cerebral Infarction with Integrated Traditional Chinese andWestern Medicine (2017). Chinese Journal of Integrative Medicine, 38: (02), 136–144. https://doi:10.7661/j.cjim.20171221.483. |
17 | Godecke, E. , Armstrong, E. , Rai, T. , Ciccone, N. , Rose, M. L. , Middleton, S. ,... VERSE Collaborative Group ((2021) ). A randomized control trial of intensive aphasia therapy after acute stroke: The Very Early Rehabilitation for SpEech (VERSE) study. International Journal of Stroke, 16: (5), 556–572. https://doi.org/10.1177/1747493020961926 |
18 | Greener, J. , Enderby, P. , & Whurr, R. ((2001) ). Pharmacological treatment for aphasia following stroke. The Cochrane Database of Systematic Reviews, 2001: (4), CD000424. https://doi.org/10.1002/14651858.CD000424 |
19 | Higgins, J. , Thomas, J. , Chandler, J. , Cumpston, M. , Li, T. , Page, M. , & Welch, V. ((2021) ). Cochrane Handbook for Systematic Reviews of Interventions version 6.2. Cochrane. Retrieved July 9, 2021, from www.training.cochrane.org/handbook |
20 | Hsueh, I. P. , Wang, C. H. , Liou, T. H. , Lin, C. H. , & Hsieh, C. L. ((2012) ). Test-retest reliability and validity of the comprehensive activities of daily living measure in patients with stroke. Journal of Rehabilitation Medicine, 44: (8), 637–641. https://doi.org/10.2340/16501977-1004 |
21 | Inatomi, Y. , Yonehara, T. , Omiya, S. , Hashimoto, Y. , Hirano, T. , & Uchino, M. ((2008) ). Aphasia during the acute phase in ischemic stroke. Cerebrovascular Diseases, 25: (4), 316–323. https://doi.org/10.1159/000118376 |
22 | Laska, A. C. , Hellblom, A. , Murray, V. , Kahan, T. , & Von Arbin, M. ((2001) ). Aphasia in acute stroke and relation to outcome. Journal of Internal Medicine, 249: (5), 413–422. https://doi.org/10.1046/j.1365-2796.2001.00812.x |
23 | Li, A. P. , Xiao, W. M. , Wang, Y. M. , Xiong, X. P. , & Huang, X. Q. ((2013) ). A follow-up study of post-stroke aphasia recovery using acupuncture and donepezfil. Journal of New Medicine, 44: (12), 832–835. https://doi:10.3969/g.issn.0253-9802.2013.12.008. |
24 | Li, G , & Yang, E. S. ((2011) ). An fMRI study of acupuncture-induced brain activation of aphasia stroke patients. Complementary Therapies in Medicine, 19: (Suppl 1), S49–S59. https://doi.org/10.1016/j.ctim.2010.11.004 |
25 | Liu, L. A. , Guo, R. Y. , Pang, S. M. , Li, X. Q. , Dai, S. Z. Q , Li, X. Y. ,... Zhang, G. P. ((2006) ). Clinical study of acupuncture combined with language training for treating aphasia in the early stage of stroke. Chinese Archives of Traditional Chinese Medicine, 24: (12), 2256–2259. https://doi:10.13193/j.archtcm.2006.12.98.liula.047. |
26 | Luo, W. P. , Tan, J. L. , & Huang, H. Y. ((2008) ). Clinical observation on treatment of cerebral infarction-induced Broca aphsia by Tiaoshen Fuyin acupuncture therapy combined with language training. Chinese Acupuncture & Moxibustion, 28: (3), 171–175. https://doi:10.13703/j.0255-2930.2008.03.027. |
27 | Luo, W. P. , Huang, H. Y. , & Zhu, J. Y. ((2010) ). Clinical research on Broca Aphasia from ischemic apoplexy treated by acupuncture associated with language training. Chinese Archives of Traditional Chinese Medicine, 28: (11), 2451–2454. https://doi:10.13193/j.archtcm.2010.11.213.luowp.005. |
28 | Mccubbin, T. , Kempe, K. L. , & Beck, A. ((2017) ). Complementary and Alternative Medicine in an Integrated Health Care Delivery System: Users of Chiropractic, Acupuncture, and Massage Services. The Permanente Journal, 21: , 16–172. https://doi.org/10.7812/TPP/16-172 |
29 | Mu, J. , Fu, L. X. , Lu, Y. M. , Ren, Y. L. , He, J. Y. , & Qi, Y. Z. ((2010) ). Clinical observation on the Xingnao Kaiqiao acupuncture plus language rehabilitation training for Motor Aphasia caused by cerebral infarction: a report of 30 cases. Journal of Traditional Chinese Medcine, 51: (5), 428–431. https://doi:10.13288/j.11-2166/r.2010.05.048 |
30 | Nouwens, F. , de Lau, L. M. , Visch-Brink, E. G. , van de Sandt-Koenderman, W. M. , Lingsma, H. F. , Goosen, S. ,... Dippel, D. W. ((2017) ). Efficacy of early cognitive-linguistic treatment for aphasia due to stroke: A randomised controlled trial (Rotterdam Aphasia Therapy Study-3). European Stroke Journal, 2: (2), 126–136. https://doi.org/10.1177/2396987317698327 |
31 | Nouwens, F. , Visch-Brink, E. G. , Van de Sandt-Koenderman, M. M. , Dippel, D. W. , Koudstaal, P. J. , & de Lau, L. M. ((2015) ). Optimal timing of speech and language therapy for aphasia after stroke: more evidence needed. Expert Review of Neurotherapeutics, 15: (8), 885–893. https://doi.org/10.1586/14737175.2015.1058161 |
32 | Picano, C. , Quadrini, A. , Pisano, F. , & Marangolo, P. ((2021) ). Adjunctive Approaches to Aphasia Rehabilitation: A Review on Efficacy and Safety. Brain Sciences, 11: (1), 41. https://doi.org/10.3390/brainsci11010041 |
33 | Shewan, C. M. , & Kertesz, A. ((1980) ). Reliability and validity characteristics of the Western Aphasia Battery (WAB). The Journal of Speech and Hearing Disorders, 45: (3), 308–324. https://doi.org/10.1044/jshd.4503.308 |
34 | Smits, M. , Visch-Brink, E. G. , van de Sandt-Koenderman, M. E. , & van der Lugt, A. ((2012) ). Advanced magnetic resonance neuroimaging of language function recovery after aphasic stroke: a technical review. Archives of Physical Medicine and Rehabilitation, 93: (1 Suppl), S4–S14. https://doi.org/10.1016/j.apmr.2011.02.023 |
35 | Song, Z. Y. , Zheng, H. Y. , Liu, Y. C. , Ma, Z. H. , Yang, Y. J. , Liu, J. ,... Li, H. ((2019) ). Clinical study on treatment of Aphasia after Ischemic Stroke by Electroacupuncture nonverbal eight points in Shenying Jing. Journal of Sichuan of Traditional Chinese Medicine, 37: ((6)), 177–179. |
36 | Stroke Prevention engineering Committee ((2021) ). Guidelines for Stroke Prevention and Treatment in China (2021 edition). Retrieved September 3, 2021, from https://www.nhc.gov.cn/yzygj/s3593/202108/50c4071a86df4bfd9666e9ac2aaac605.shtml |
37 | Stroke—1989. Recommendations on stroke prevention, diagnosis, and therapy. Report of theWHOTask Force on Stroke and other Cerebrovascular Disorders. ((1989) ). Stroke, 20: (10), 1407–1431. https://doi.org/10.1161/01.str.20.10.1407 |
38 | Strong, K. , Mathers, C. , & Bonita, R. ((2007) ). Preventing stroke: saving lives around the world. The Lancet. Neurology, 6: (2), 182–187. https://doi.org/10.1016/S1474-4422(07)70031-5 |
39 | Sun, Q. R. , Ji, X. D. , Cui, Z. P. , Chen, X. J. , & Wang, Y. J. ((2010) ). Observation on the therapeutic effect of scalp acupuncture, plum-blossom needle combined with speech rehabilitation training on aphasia of ischemic apoplexy. World Journal of Acupuncture-Moxibustion, 20: , 13–18. |
40 | Tang, H. Y. , Tang, W. , Yang, F. , Wu, W. W. , & Shen, G. M. ((2019) ). Efficacy of acupuncture in the management of post-apoplectic aphasia: a systematic review and meta-analysis of randomized controlled trials. BMC Complementary and Alternative Medicine, 19: (1), 282. https://doi.org/10.1186/s12906-019-2687-1 |
41 | Wallace, S. J. , Worrall, L. , Rose, T. , Le Dorze, G. , Breitenstein, C. , Hilari, K. ,... Webster, J. ((2019) ). A core outcome set for aphasia treatment research: The ROMA consensus statement. International Journal of Stroke, 14: (2), 180–185. https://doi.org/10.1177/1747493018806200 |
42 | Wallentin, M. ((2018) ). Sex differences in post-stroke aphasia rates are caused by age. A meta-analysis and database query. PloS One, 13: (12), e0209571. https://doi.org/10.1371/journal.pone.0209571 |
43 | Wang, N. , & Li, Y. ((2015) ). Therapeutic observation of cluster needling at anterior oblique line of vertex-temporal plus speech training for Motor Aphasia after cerebral infarction. Shanghai Journal of Acupuncture and Moxibustion, 34: (5), 412–414. https://doi:10.13460/j.issn.1005-0957.2015.05.0412. |
44 | Wang, X. R. , & Zhuo, D. H. ((1992) ). Functional language communication ability test and its application in the detection of aphasia following stroke. Development of functional language communication ability test. Chinese Journal of Rehabilitation Medicine, 7: (6), 248–250. |
45 | Winstein, C. J. , Stein, J. , Arena, R. , Bates, B. , Cherney, L. R. , Cramer, S. C. ,... Council on Quality of Care and Outcomes Research ((2016) ). Guidelines for Adult Stroke Rehabilitation and Recovery: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke, 47: (6), e98–e169. https://doi.org/10.1161/STR.0000000000000098 |
46 | Wu, C. , Qin, Y. , Lin, Z. , Yi, X. , Wei, X. , Ruan, Y. , & He, J. ((2020) ). Prevalence and Impact of Aphasia among Patients Admitted with Acute Ischemic Stroke. Journal of Stroke and Cere brovascular Diseases, 29: (5), 104764. https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.104764 |
47 | Wu, F. , Yang, W. Z. , Zhao, N. , Sheng, Y. X. , Ye, B. Y. , & Liu, X. L. ((2010) ). Influence of Tongli acunpuncture combined with speech function rehabilitation training on speech function in patients with Motor Aphasia after cerebral infarction. Chinese Journal of Integrative Medicine on Cardio-Cerebrovascular Disease, 8: (3), 290–292. |
48 | Wu, Q. , Hu, X. , Wen, X. , Li, F. , & Fu, W. ((2016) ). Clinical study of acupuncture treatment on motor aphasia after stroke. Technology and Health Care, 24: (Suppl 2), S691–S696. https://doi.org/10.3233/THC-161197 |
49 | Xiong, J. , Zhang, M. , Guo, W. L. , Fan, S. H. , & Zhang, Y. L. ((2016) ). Clinical research on Xingnao Kaiqiao acupuncture method combined with language rehabilitation training in patients with cerebral infarction motor aphasia. Acta Chinese Medicine, 31: ((10)), 1609–1613. https://doi:10.16368/j.issn.1674-8999.2016.10.453. |
50 | Yan, B. , Li, K. , Xu, J. , Wang, W. , Li, K. , Liu, H. ,... Tang, X. ((2005) ). Acupoint-specific fMRI patterns in human brain. Neuroscience Letters, 383: ((3)), 236–240. https://doi.org/10.1016/j.neulet.2005.04.021 |
51 | Yang, A. , Wu, H. M. , Tang, J. L. , Xu, L. , Yang, M. , & Liu, G. J. ((2016) ). Acupuncture for stroke rehabilitation. The Cochrane Database of Systematic Reviews, 2016: (8), CD004131. https://doi.org/10.1002/14651858.CD004131.pub3 |
52 | Zhang, B. , Han, Y. , Huang, X. , Liu, Z. , Li, S. , Chang, J. , & Gao, Y. ((2019) ). Acupuncture is effective in improving functional communication in post-stroke aphasia : A systematic review and meta-analysis of randomized controlled trials. Wiener klinische Wochenschrift, 131: (9-10), 221–232. https://doi.org/10.1007/s00508-019-1478-5 |
53 | Zhang, T. , Zhao, J. , Bai, Y. L. , Li, X. P. , Qu, Y. , Wang, B. J. , & Li, B. J. ((2019) ). A clinical guideline for the management of cerebrovascular diseases in China (Excerpt Edition)—Management of Stroke Rehabilitation. Chinese Journal of Stroke, 14: (8), 823–831. https://doi:10.3969/j.issn.1673-5765.2019.08.017. |
54 | Zhang, Q. S. , Ji, S. R. , Li, S. L. , He, Y. , Jia, G. H. , Qin, J. T. ,... Tian, H. ((2005) ). Reliability and Validity of Chinese Rehabilitation Research Center Standard Aphasia Examination. Chinese Journal Rehabilitation Theory and Practice, 11: (9), 703–705. |
55 | Zhong, Y. ((2019) ). Efficacy of scalp acupuncture and tongue acupuncture plus language rehabilitation training on aphemia after cerebral infarction. Clinical Journal of Chinese Medicine, 11: (10), 124–126. https://doi:10.3969/j.issn.1674-7860.2019.10.048. |
56 | Zhou, Y. H. , Song, J. H. , Li, X. X. , & Li, X. Q. ((2015) ). Sichong Point Yinzhong Yinyang acupuncture combined with schuell language training for Aphasia after Ischemic Stroke. Journal of Clinical Acupuncture and Moxibustion, 31: (7), 26–28. |




