Post-traumatic cephalalgia
Abstract
After traumatic brain injury (TBI), a host of symptoms of varying severity and associated functional impairment may occur. One of the most commonly encountered and challenging to treat are the post-traumatic cephalalgias. Post-traumatic cephalalgia (PTC) or headache is often conceptualized as a single entity as currently classified using the ICHD-3. Yet, the terminology applicable to the major primary, non-traumatic, headache disorders such as migraine, tension headache, and cervicogenic headache are often used to specify the specific type of headache the patients experiences seemingly disparate from the unitary definition of post-traumatic headache adopted by ICHD-3. More complex post-traumatic presentations attributable to brain injury as well as other headache conditions are important to consider as well as other causes such as medication overuse headache and medication induced headache. Treatment of any post-traumatic cephalalgia must be optimized by understanding that there may be more than one headache pain generator, that comorbid traumatic problems may contribute to the pain presentation and that pre-existing conditions could impact both symptom complaint, clinical presentation and recovery. Any treatment for PTC must harmonize with ongoing medical and psychosocial aspects of recovery.
1Introduction
After traumatic brain injury (TBI), a host of symptoms of varying severity and associated functional impairment may occur. One of the most commonly encountered and challenging to treat are the post-traumatic cephalalgias which have been found to exist as a chronic problem in a substantial number of individuals with mild, moderate and severe brain injuries based on available studies (Hoffman et al., 2012; Ruet et al., 2019). Post-traumatic cephalalgia (PTC) or headache is often conceptualized as a single entity as currently classified using the ICHD-3. Yet, the terminology applicable to the major primary, non-traumatic, headache disorders such as migraine, tension headache, and cervicogenic headache are often used to specify the specific type of headache the patients experiences seemingly disparate from the unitary definition of post-traumatic headache adopted by ICHD-3. More complex post-traumatic presentations attributable to brain injury as well as other headache conditions are important to consider as well as other causes such as medication overuse headache and medication induced headache. Treatment of any post-traumatic cephalalgia must be optimized by understanding that there may be more than one headache pain generator, that comorbid traumatic problems may contribute to the pain presentation and that pre-existing conditions could impact both symptom complaint, clinical presentation and recovery. Any treatment for PTC must harmonize with ongoing medical and psychosocial aspects of recovery.
2Classification
The most widely used definition of post-traumatic headache has been provided by the International Headache Society (IHS) (3rd edition of the International Headache Society International Classification of Headache Disorders, or ICHD-3). This definition divides post-traumatic headache into acute and persistent subcategories based on symptoms, with the former lasting <3 months and the latter at least 3 months. The ICHD-3 builds on prior definitions of persistent post-traumatic headache by distinguishing those occurring in the context of mild injury to the head versus moderate or severe injury (although the nomenclature is confusing as there is no real distinction made between head or cranial injury and TBI). Section 5 of the classification is the first of the secondary headaches and is represented as follows:
5. Headache attributed to trauma or injury to the head and/or neck
5.1 Acute headache attributed to traumatic injury to the head
5.1.1 Acute headache attributed to moderate or severe traumatic injury to the head
5.1.2 Acute headache attributed to mild traumatic injury to the head
5.2 Persistent headache attributed to traumatic injury to the head
5.2.1 Persistent headache attributed to moderate or severe traumatic injury to the head
5.2.2 Persistent headache attributed to mild traumatic injury to the head
5.3 Acute headache attributed to whiplash1
5.4 Persistent headache attributed to whiplash
5.5 Acute headache attributed to craniotomy Persistent headache attributed to craniotomy
Headache onset must occur within 7 days of injury, return of consciousness or “discontinuation of medication(s) impairing ability to sense or report headache following the injury to the head” (Headache Classification Committee). The 7-day onset criterion has been shown to underestimate incidence of this disorder as PTC may have its onset after one-week post-injury (Hoffman, Lucas, Dikmen, 2011). Although empirical, this criterion embodies an effort to consolidate the highly variable pathophysiologic mechanisms of post-traumatic headache into one definition; although in practice, this goal is often lost and PTC is viewed with “blinders on” as all migrainous in nature. In that context, ICHD-3 relies instead on relatively non-specific features such as onset latency, duration and severity of associated TBI (if applicable) which in and of themselves are not pathognomonic for any specific PTC. Such consolidation generally does not positively contribute to the diagnostic or treatment planning process. Additionally, the classification system ignores details of both known or suspected injury mechanisms (which may give clues as to risk factors for certain types of headaches) as well as physical examination findings both of which provide critical cues on likely headache pathogenesis. ICHD-3 also confuses pathophysiological correlates of the traumatic event, inadequately differentiating between head or cranial trauma, traumatic brain injury and cervical acceleration deceleration injuries as contributors to PTC (Zasler, Etheredge, 2020). Use of appropriate and accurate nomenclature is critical when trying to dissect pain generators responsible for PTC as well as communicating with fellow clinicians, patients and families. It is therefore possible that the current system of classification in the absence of a more complete delineation of headache subtypes and clinician assessment may result in incorrect clinical diagnoses as well as subsequent treatment resulting in more headache chronification as opposed to less. Studies to date have not dissected how much the latter issue is contributory to the high rate of more chronic headache complaints in some studies.
3Epidemiology and risk factors
TBI is a common problem, with at least 1.7 million injuries occurring in the United States annually and 3.2 million people living with TBI-related functional impairment (Lucas, 2015; Zaloshnja et al., 2008). The lifetime post-traumatic headache (PTC) prevalence is 4.7% in men and 2.4% in women (Baandrup and Jensen, 2005). PTC accounts for approximately 4% of all symptomatic headaches (Elahi & Reddy, 2014). PTC is more commonly encountered in patients with mTBI than those recovering from moderate or severe TBI (Couch and Bearrs, 2001), though headaches in the moderate and severe groups are more likely to remain chronic if headache is reported. There remains debate as to why incidence is possibly higher in milder injuries if the common pathoetiology is the brain injury itself (Zasler, Leddy, Etheredge, Martelli, 2019). In one recent study, 45% of adults with mild TBI experienced headaches with a prevalence of continued headaches at 3 months following injury as high as 22% (Cooksley et al., 2018). PTC meeting ICHD-3 criteria for migraine and tension subtypes are the most frequently encountered (Ashina et al., 2019). Historically, tension type has been viewed as more common than migraine (Baandrup and Jensen, 20015; Haas, 1996; Stovner et al., 2009), but prospective studies have shown higher prevalences of migraine (Lucas et al 2012, Lucas et al 2014) as have large studies of military populations (Theeler et al., 2010). How much the frequency of migraine diagnosis in these studies has to do with the true incidence versus a consequence of “blinders on” classification per IHS criteria remains debated as other authors have opined that other types of headaches subtypes are more common including tension type headache as mentioned above (Appenzeller, 1993; Lew, Lin, Fuh, et al., 2006), as well as cervicogenic referred headaches (Packard, 2002; Zasler, Leddy, Etheredge, Martelli, 2019: Zasler, Etheredge, 2020). Trigeminal autonomic cephalgias may occur with any severity of TBI and include cluster headache, hemicranias continua, short-lasting unilateral neuralgiform headache with conjunctival injection and tearing, short-lasting unilateral headache, and paroxysmal hemicranias (Jacob et al., 2008; Matharu et al., 2001; Putzki et al., 2005).
D’Onofrio et al., 2014 found that female gender, poorer socioeconomic status, pre-existing psychiatric disease burden and certain personality factors may negatively influence post-traumatic headache risk and course (Lucas et al., 2012; Vargas et al., 2012).
4Diagnostic considerations
In order to adequately diagnose and treat any PTC, a thorough headache history including both preinjury, injury and postinjury details should be completed (Zasler Martelli, Jordan, 2019).
Fig. 1
Reprinted and modified from Zasler, N.D. (2015). Sports Concussion Headache. Brain Injury. 29(2):207–220 2015. Used with permission.
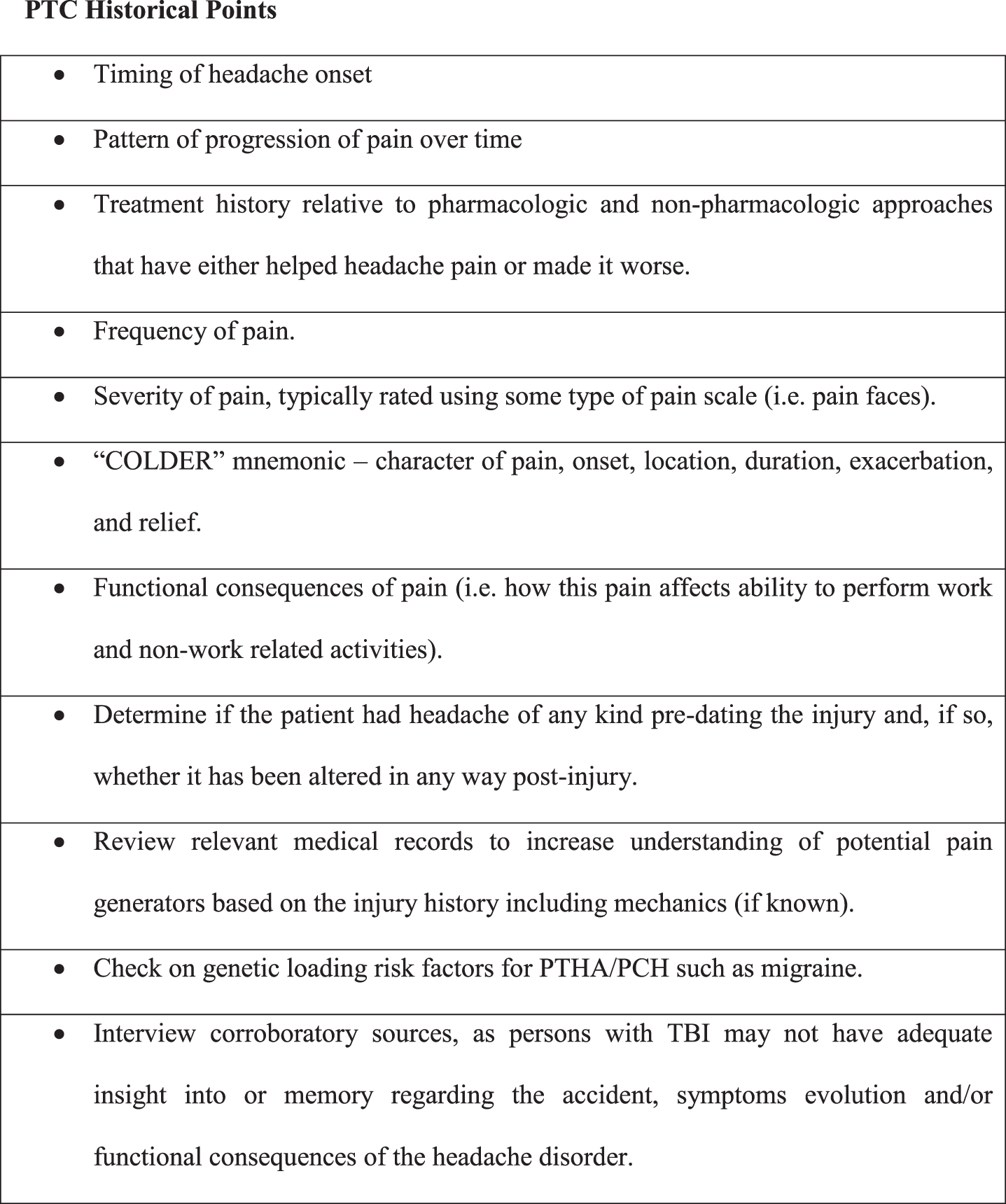
A good history will often guide how the clinician focuses their headache physical examination for the range of possible neurological, both central and peripheral, as well as musculoskeletal abnormalities incited or exacerbated by trauma that may be serving as primary headache pain generators or perpetuating same (Zasler, Etheredge, 2020).
A number of structures and systems require consideration when attempting to diagnose and treat post-traumatic cephalalgias. While it is well established that brain injury can trigger headache profiles aligning closely with non-traumatic primary headache subtypes (i.e. migraine and tension type headache), secondary headache pathology must also be appropriately identified and managed as present. There is still debate about the frequency of headache due to primary brain injury versus extracerebral causes; although, these conditions can be comorbid. Post traumatic pain generators that are not uncommonly responsible for PTC include scalp or facial neuralgias, myofascial referred head pain, temporomandibular disorder related headaches, cervicogenic referred pain (which may be myofascial, neuralgic, discogenic or due to somatic dysfunctions among other causes), syndrome of the trephined, intracranial pressure abnormalties (both low and high), cavernous sinus thrombosis, late extra-axial collections such as expanding subdurals, among others (Katta-Charles, Tessler, Horn, 2021; Zasler, Leddy, Etheredge, Martelli, 2019). Other headaches etiologies not directly related to the trauma must also be considered including psychogenic headache, medication overuse headache, medication induced headache as well as feigned headache. The dura, dural venous system, periosteum and scalp are sensitive to pain, as are the cervical spine and craniocervical junction. Local pain, referred pain and impairment of sensory integration and postural control may contribute to headache symptomatology (Packard et al. 1999; Zafonte & Horn 1999; Hecht 2004). PTC may develop in the context of local impact injury, compression or entrapment of the supratrochlear or supraorbital nerve as well as the occipital nerves (3rd, lesser and greater) with radiating pain extending to parietal, temporal, frontal and periorbital/retroorbital regions, especially in the context of degenerative spine changes, vertebral fracture, or chronically paraspinal muscle spasm (Zaremski et al., 2015; Katta-Charles, Tessler, Horn, 2021; Zasler, Etheredge, 2020).
Traumatic trigeminal nerve injury is uncommon, but when it occurs it may cause facial pain. Trigeminal neuropathy as a source of post-traumatic cephalalgia is rare but would typically occur after major craniofacial trauma. Of trigeminal injuries, the minority are painful (Benoliel et al., 2016). Supraorbital and supratrochlear neuralgias are fairly common following trauma (Pareja, Caminero, 2006). Infraorbital branch injury associated with zygomatic complex fracture featured neuropathic pain only 3.3% of the time at 6 months (Benoliel et al., 2005).
Rare headache profiles triggered by cerebrospinal fluid (CSF) leakage and reduced CSF volume can occur in the setting of leaks involving dural nerve root sleeves, ventral dural tears in the setting of intervertebral disk herniations and CSF-venous fistulas (Kranz et al., 2017) in addition to cribiform plate fracture (Siavoshi et al., 2016). The pain associated with intracranial hypotension may be caused by displacement of pain-sensitive structures or compensatory vasodilation of dural sinuses and meningeal blood vessels. This is typically exacerbated by upright position (Ferrante et al., 2004; Siavoshi et al., 2016). Spontaneous intracranial hypotension-related headache reporting patterns appear to differ on the basis of gender and age, with females and patients under 40 presenting with more acute and severe headache. Males over 40 were more likely to present with a longer course of symptoms and with associated subdural hematomas (Tanaka et al., 2016). Nausea, vomiting, abducens nerve palsy and pain involving the neck or the site of the CSF leak may be observed (Primalani, 2019). MR imaging often reflects pachymeningeal enhancement, development of subdural hygromas, pituitary enlargement and characteristic changes of sag at the brainstem and cerebellum (Mokri, 2014; Samii et al., 1999). CSF leaks which communicate with sinuses can rarely evolve into tension pneumocephalus; in a low-pressure environment there is potential for rapid expansion as late as 4 years post-trauma (Zasler, 1999; Donovan et al., 2008). Separate from traumatic leaks and instances of intracranial hypotension, CSF flow dynamics and metabolism have been pondered as relatively unexplored aspects of post-traumatic headache exacerbation (Kamins and Charles, 2017).
Acute intracranial hemorrhage as well as extra-axial hemorrages may be an early recognized complication of moderate or severe brain injury. Late-expanding hemorrhages can also occur, even if the inciting trauma is mild. Subdural hematoma is most commonly encountered. Delayed-onset subdural hematoma has been reported >40 days post-trauma (Gurer et al., 2016). Epidural hematoma with expansion 5 days to 3 weeks post-trauma have also been described (Illingworth and Shawdon, 1983). Other rare potential complications to be considered include cerebral venous sinus thrombus, cavernous sinus thrombosis, carotid dissection, carotid-cavernous fistulas and hydrocephalus (Katta-Charles, Tessler, Horn, 2021; Zasler, Leddy, Etheredge, Martelli, 2019). Headache due to dysautonomia or (post-craniectomy) syndrome of the trephined may be encountered in cases of more severe brain injury.
Referred pain from cervical whiplash or other local neck/shoulder myofascial injury should be considered as a cause or contributor to PTC, especially when there is proximity to cranial nerve V, VII, IX and X afferents in the neck and potential for convergence projection. The trigeminocervical complex (TCC) relays nociceptive afferent input from the meninges and cervical structures to the head and face.
Fig. 2
Reprinted with permission from Horn, L.J. Siebert, B., Patel, N., Zasler, N.D. (2013). Post traumatic headache. In: Zasler, ND, Katz, DI, Zafonte, RD (eds): Brain Injury Medicine: Principles and Practice, Second Edition, Demos Medical Publishing, page 936.
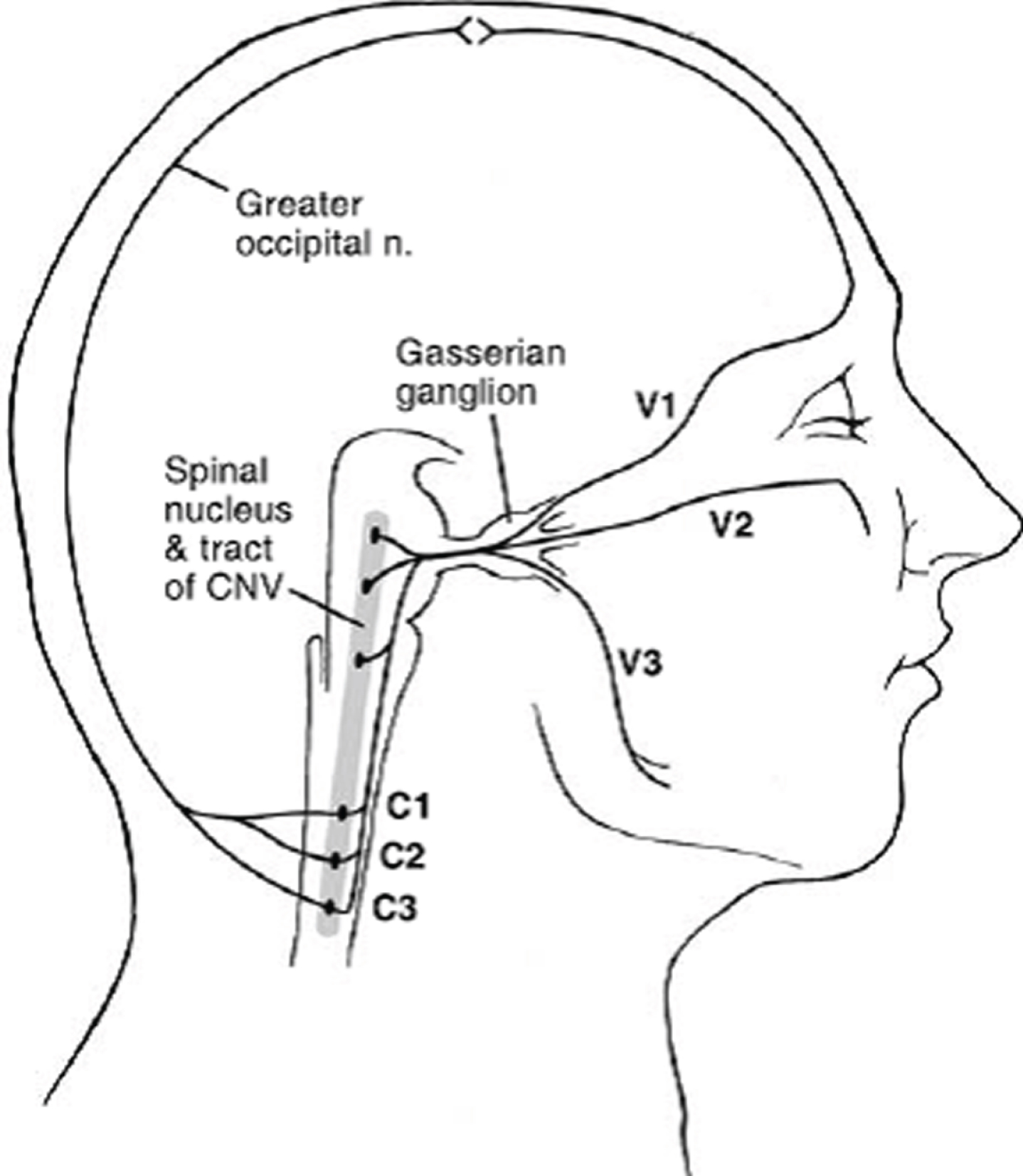
This likely explains why cervicalgia following whiplash must be evaluated and treated to prevent secondary activation of the TCC which may cause aggravation of headache disorders such as migraine (Bartsch, Goadsby, 2003) due to promulgation of trigeminal system hypersensitivity as well as spread and referral of pain. Trauma that may occur with cervical whiplash may also induce migraine headaches through a yet unknown mechanism that may involve the trigeminocervical complex (Watson, Drummond, 2016). Whiplash injuries to the cervical spine also commonly occur with associated autonomic symptoms that may mimic post-TBI symptomatology and confound headache classification. Chronification of pain may then lead to central sensitization of the TCC neurons leading to further aggravation of the headache disorder and typically a worsening of prognosis.
Mechanisms of central sensitization are still being explored, however it appears that abnormal neuronal excitability may lead to altered processing of sensory stimuli causing cortical spreading depression and trigeminal activation. There are numerous pathways in the neuromatrix that when damaged may lead to centrally mediated pain. Central sensitization contributes to both acute allodynia and headache persistence. Sensitization, whether peripheral and/or central, is not just relevant to post-traumatic migraine but may be seen in cervical whiplash injury, traumatic temporomandibular disorder, among other conditions. Repetitive concussions may promote trigeminal sensitivity and microglial proliferation, astrocytosis and neuropeptide release in the trigeminovascular system further exacerbating the underlying headache disorder (Tyburski, Cheng, Assari, et al., 2017; Zasler, Etheredge, 2020).
The role and frequency of involvement of the cervical spine in the differential diagnosis of post-concussive symptoms including PTC although acknowledged for many years by clinicians in the trenches (Packard, 2002) has recently been better studied and acknowledged (Marshal, Vernon, Leddy, et al., 2015; Ellis, Leddy, Willer, 2015; Kennedy, Quinn, Tumilty et al., 2017; Kennedy Quinn, Chapple, et al., 2019). What role subtle anatomical relations between the rectus capitis posterior minor and the dura mater may have in headache persistence remains controversial and poorly studied, albeit an interesting association that warrants further scrutiny (Hack, Koritzer, Robinson, et al., 1995; Fakhran, Qu, Alhilali, 2016). Associated clinical features may include accompanying tinnitus, ear fullness or vertigo. Vertigo may also present as a migrainous phenomenon or as a separately induced peripheral vestibular injury (Akin et al., 2017).
5Pathophysiology
PTC has been shown to be mediated by numerous disruptive structural and metabolic processes; although, the exact correlates with specific subtypes of PTC such as migraine, tension, neuritic, cervicogenic are presently poorly understood It should also be clear that these structural and metabolic alterations do not necessarily occur across all PTC subtypes although there may be common pain processing pathways triggered by any craniocervical afferent nociceptive input. Cellular membrane integrity and pump dysfunction, axonal injury, vascular dysfunction including disruption of the blood brain barrier and flow/metabolism mismatch, mitochondrial dysfunction, altered neurotransmitter and hormone release as well as inflammatory cascades (Selwyn et al., 2013; Yorns et al., 2013; Barlow et al., 2017; Giza and Hovda, 2014; Barkhoudarian et al., 2016). There are pathophysiologic similarities to cortical spreading depression, which have been associated with the occurrence of aura in migraine (Charles and Baca, 2013).
Patients with a history of familial hemiplegic migraine, types 1 and 2, can experience an exaggerated response to minor trauma with responses ranging from severe migraine to hemiplegic attacks to cerebral edema and coma. Whether P/Q type calcium channel or Na+/K+ pump variation or dysfunction could be implicated in PTC is relatively unexplored (Barros et al 2013; Tottene et al., 2005; Kors et al., 2001; Kamins and Charles, 2018).
Piantino et al. (2019) explored a potential connection between TBI, post-traumatic sleep disruption and occurrence of PTC, suggesting that both trauma and sleep disturbance could impair clearance of pathophysiologically significant headache substrates such as CGRP via recently described paravascular/interstitial pathways of CSF flow (Xie et al., 2013).
Whether structurally or functionally based neuroimaging differences correlate with headache and other pain syndromes after mild brain injury is of great importance in understanding the evolution of post-traumatic pain. MRI-based functional connectivity has been explored in the setting of traumatic and non-traumatic cases of migraine (Dumkrieger et al., 2019). Static and dynamic functional connectivity differences have been noted in regions that involve elaboration of pain and were correlated with frequency and intensity of migraine (Van der Horn et al., 2016). Neuroimaging in post-traumatic chronic pain was recently reviewed by Ofoghi et al (2020). Studies of total brain volume, grey matter density by voxel-based morphometry, diffusion tensor-imaging examination of white matter integrity, task-based and resting state fMRI were included. Populations were heterogeneous and all but one of the 19 studies included focused on adults. Morphological differences were noted in the frontal and parietal cortex as well as the spinothalamic tract, with implications for central pain processing and deficits in cognitive control and descending modulation of pain. Schwedt et al (2017) noted structural differences between healthy controls and those with persistent PTC involving the right lateral orbitofrontal lobe, right supramarginal gyrus, and left superior frontal lobe. Ascending pain signals may also be altered given reports of altered spinothalamic tract volumes and white matter differences involving the corpus callosum, spinothalamic tract, periaqueductal gray and fornix-septohippocampal circuit (Ofoghi et al., 2020). Inter-hemispheric connectivity between pain-related regions may be adversely affected by disturbances in callosal white matter integrity. For example, Alhilali and colleagues (2017) analyzed 75 subjects who had PTC with a migrainous versus non-migrainous presentation. At 20 days, the migraine subtype sufferers had lower fractional anisotropy (FA) of the corpus callosum and fornix/septohippocampal circuit than the non-migrainous group of patients. This was also associated with disturbances of visual memory performance, such that reduced callosal FA was not always specific to headache-related signs and symptoms.
Fig. 3
Regions with structural differences when comparing individuals with persistent post-traumatic cephalalgia (PPTC) to those with migraine. When comparing structural measurements of entire brain regions in patients with PPTC to patients with migraine, the right lateral orbital frontal region differed in area, volume, and curvature. The left caudal middle frontal, precuneus, and superior frontal regions and the right supramarginal gyrus region differed in cortical thickness (Schwedt et al., 2017).
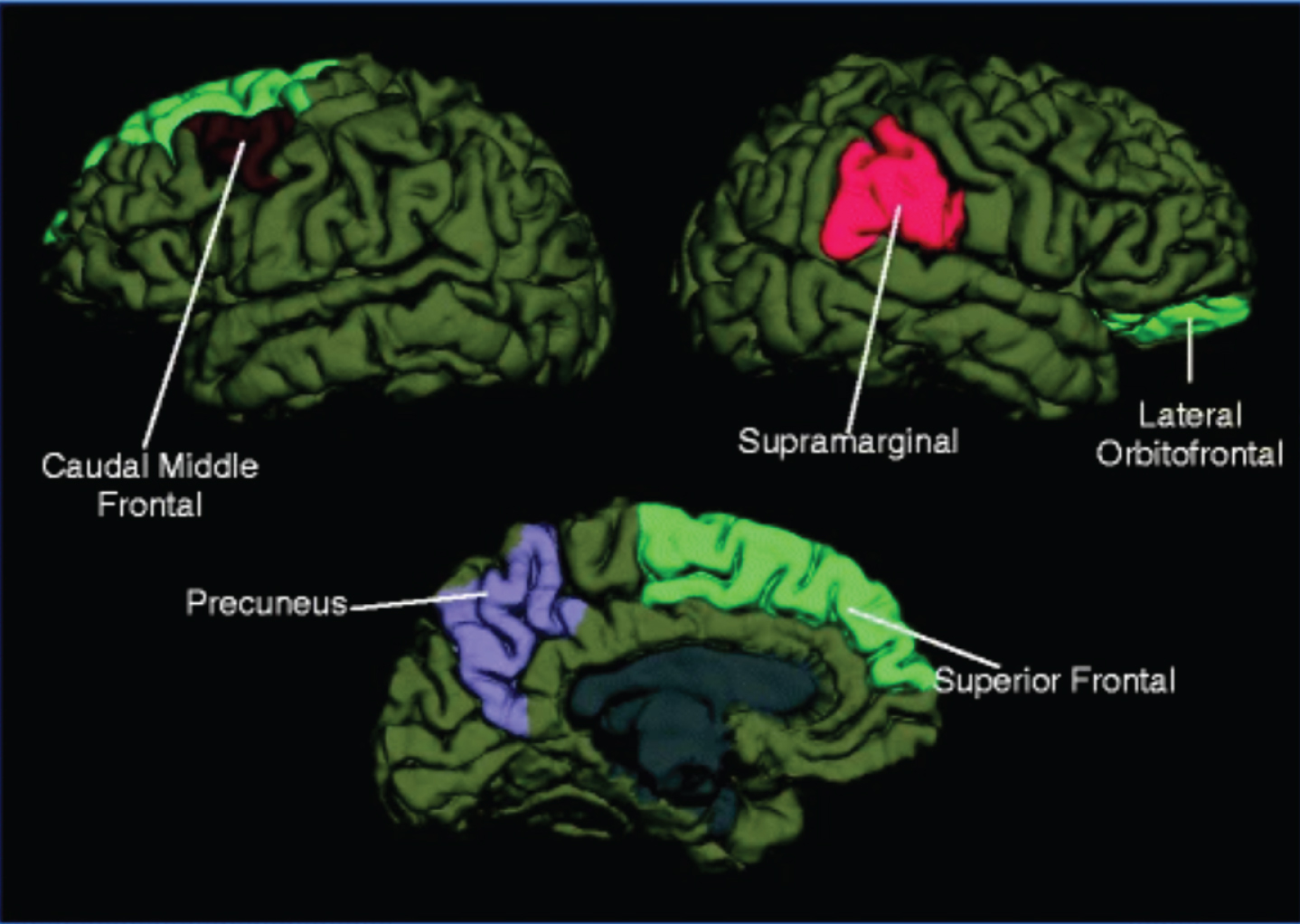
Shannon entropy (SE), a measure of data set complexity, was recently applied to fractional anisotropy to differentiate between both mTBI and non-TBI subjects as well as those with migrainous and non-migrainous PTC (Delic et al., 2016). TBI-induced altered functioning of the descending pain modulation network was also suggested in functional heat pain stimulation tasks.
Care should be taken with how neuroimaging data is used as none of these neuroimaging tests ultimately tap the issue of differentiating pain itself as a first-person subjective experience from nociceptive peripheral and central pain responses and/or mechanisms (Zasler, 2021).
6Clinical course
The majority of individuals who sustain an mTBI can expect a good recovery. The adult sports concussion population has historically demonstrated a recovery time on the order of weeks compared to TBI occurring through other mechanisms, often within 1-3 months (Levin et al., 1987; Ponsford et al., 2000; Rohling et al., 2009). A subset of these individuals will continue to experience chronic PTC. Patients with moderate to severe TBI are subject to poorer prognoses regarding headache, as is the case with other neurological and neuropsychological residuals of more severe TBI. (Walker et al., 2005).
The reality is that we really do not understand the natural history of untreated PTC never mind the natural history of treated PTC. To compound that problem, there is overlap in clinical presentations between a number of the posttraumatic headache subtypes relative to laterality, character of pain, and location of pain that in and of themselves may be clues as to the pain generator, but are not pathognomonic for same. Diagnosis is further complicated by the frequent occurrence of autonomic symptoms such as sonosensitivity and photosensitivity following TBI which may be mislabeled as migrainous phenomena. In “treated” PTC, there remains controversy regarding whether the relatively frequent occurrence of chronification is a reflection of the intractability of the underlying pain generator responsible for the headache or alternatively a consequence of inadequate diagnosis and as a result, inappropriate or incomplete treatment for the actual cause or causes of the persisting headache (Zasler, Martelli, Jordan, 2019).
Prognostic risk factors for poor outcome have historically been discussed within the context of post-concussive symptomatology or late-phase post-traumatic disorder (Dwyer and Katz, 2018). The 5th International Conference of Concussion and Sport noted that relatively more severe symptoms in the first few days after sport-related concussion was a strong predictor of slowed recovery (McCrory et al., 2017). The American Academy of Neurology (AAN) “Guidelines on the evaluation and management of concussion in sports” identified a prior history of concussion as associated with more severe and persistent symptoms. Also identified were “probable” risk factors for prolonged symptoms, including younger age of play, early post-traumatic headache, fatigue, early amnesia, alteration in mental status, and disorientation and “possible” risk factors of dizziness, playing the position of quarterback in American football, and wearing a half-face shield in ice hockey (Giza et al., 2013). Additional research has suggested that pre and post-injury mood disturbance, comorbid personality disorder, and female gender are associated with poorer prognosis after mTBI, including persistent headaches (Greiffenstein and Baker, 2001; Mooney and Speed 2001; Meares et al. 2011; Evered et al., 2003). The greater prevalence of PTC among women may be a function of premorbid disease burden (Lucas et al., 2012) and/or anatomical differences in brain and neck structure. Hoge et al. noted that after adjusting for PTSD and depression, only headache was significantly associated with mild TBI among post-deployment US Army soldiers returning from Iraq (Hoge et al., 2008).
Presentation with a migrainous subtype of PTC is associated with a prolonged course and a greater degree of overall impairment. For example, in a study of 138 male football players by Kontos et al., the group experiencing migraine performed worse on tests of visual memory, verbal memory, reaction time and reported greater symptom burden. They were 7.3 times (95% CI 1.80-29.91) more likely to experience a protracted (>20 day) recovery than those without headache (Kontos et al., 2013).
Genetic risk factors have recently received research attention. Those with a family history of migraine are at significantly higher (2.6 times (OR = 2.60, [CI = 1.35–5.02], p = 0.003) risk of post-traumatic migraine as a sequela of sport-related mTBI (Sufrinko et al., 2017). More than 38 susceptibility loci for migraine were identified in a meta-analysis of 375,000 individuals performed by Gormley et al., though none had a large effect size (Gormley et al., 2016).
A recent systematic review of risk factors for the development of acute and/or persistent PTC after TBI as defined by any version of the ICHD headache criteria yielded only 3 publications meeting criteria, and a lack of strong evidence for any particular risk factor for the development of acute or persistent PTC (Anderson et al., 2020).
7Management
PTC management should include a fully described and carefully monitored behavioral modification plan. Such plans are particularly important in patients with more chronic PTC. A careful return to physical and cognitive exertion, often with time away from work, school and recreation are part of a methodical, symptom-guided return to activity that is now broadly recommended. Brain injury-mediated headache, as present, is an included target of this intervention, but not in isolation. Other interventions for PTC have historically relied less upon a history of trauma per se and more upon the pain profile being encountered, although in some ways this may be counterintuitive, with reliance upon evidence-based protocols for comparable non-traumatic presentations. This reliance is more resource-based than evidence-based given the lack of research supporting headaches syndromes that are specifically post-traumatic. A recent systematic review (Larsen et al., 2019) sought to identify applicable evidence relating specifically to the abortive and preventative treatment of PTC as defined by ICHD criteria; however, such treatment paradigms may inaccurately imply that all PTC is migrainous in all cases which is clearly not the reality of the situation. Unfortunately, no strong evidence from clinical trials is available to direct the treatment of PTC. Some guidelines have been offered for management based on primary headache categories and treatments (Watanabe, Bell, Walker, et al., 2012). It is essential that well-designed clinical studies be conducted to inform clinicians on the management and prevention of PTC.
Abortive therapy and initiation of headache prophylaxis in the days to weeks following trauma remains controversial. In cases of moderate and severe TBI, level of consciousness and ability to report symptoms may preclude the ability to fully assess and treat the patient. In cases of mild TBI, the question of whether to treat acutely arises frequently. The 5th International Consensus on Concussion in Sport acknowledged the symptom burden and functional limitations associated with recovery from mild TBI but emphasized that the scientific basis for prescribing medications was quite limited. Non-medication approaches should be maximized and prioritized. Appropriate efforts to optimize quantity and quality of sleep, stabilize mood and modulate pain are some of the essential components of management regardless of injury severity.
Acute PTC management may involve use of analgesics such as chlorpromazine (Herd et al., 1994), acetaminophen, NSAIDs or caffeine-containing formulations and opiates. A group of 34 patients suffering from PTC (time since trauma 1 day to 3 years) were given IV dihydroergotamine and metoclopramide with 85% achieving “excellent relief” (McBeath, 1994) implying migrainous elements were contributory to the headache presentation.
For prophylaxis, tricyclic antidepressants (TCAs) have been commonly used (Patil et al., 2011; Weiss et al., 1991). Gabapentin, topiramate and valproic acid (Packard, 2000) have also been used in PTC, but have greater side effect considerations. Forty percent of subjects in Packard’s 2000 review of divalproex for chronic daily PTC discontinued medication due to a lack of effect (26%) or side effects (14%). There is some evidence to support mirtazapine for prophylaxis in chronic tension headache (Bendtsen, 2007). Other general prophylactic choices for migraine include beta blockers and calcium channel blockers (Silberstein, 2015; Schiapparelli et al., 2010). Sphenopalatine ganglion block (Sussman et al., 2015) and greater auricular nerve (Elahi & Reddy, 2014) blocks and neuromodulation have been explored with existing successful case reports in the literature.
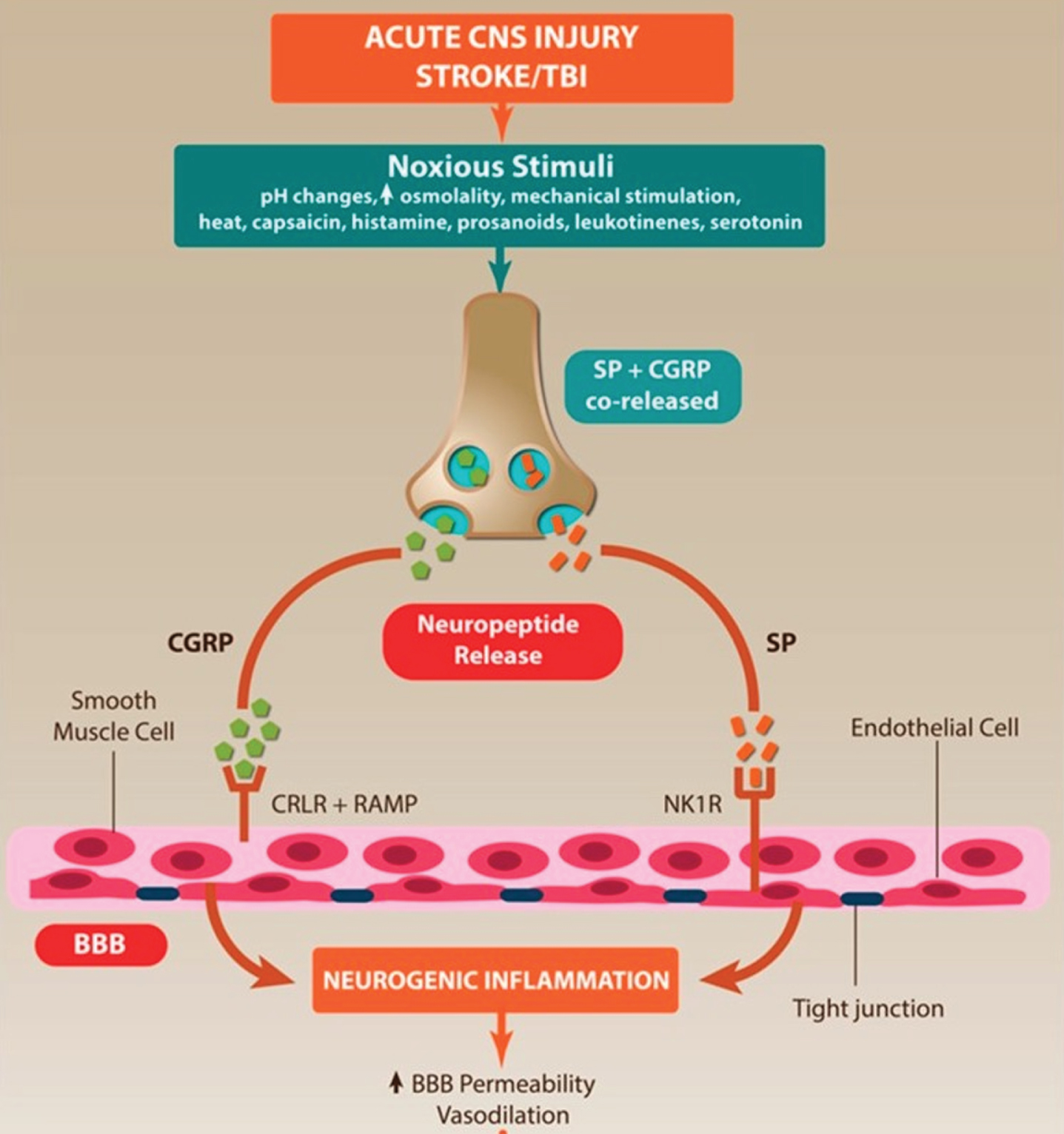
A literature review of interventional treatments for PTC found no randomized placebo-controlled studies, but did conclude that the available prospective and retrospective case analyses, review articles or consensus opinion papers favored physical therapy, neurostimulation and onobotulinum toxin among other interventions. (Conidi, 2016; Yerry, 2015). Occipital nerve blocks have been explored for multiple indications including, historically, greater and lesser occipital neuralgias (Zaremski et al., 2015) and more recently post-concussive headache (tension and migraine) and cervicogenic headache (Gawel et al., 1992; Tobin et al., 2011; Hecht, 2004), including favorably for trigeminal autonomic cephalgias (Leroux and Ducros, 2013). A 2010 review of peripheral nerve blocks and trigger point injections in general headache management concluded that current evidence lacked sufficiently large, rigorous and methodologically comparable studies pertaining to headache management (Ashkenazi et al., 2010). Obviously, the absence of proof does not mean these interventions do not have relevance in treating PTC but further study is obviously needed. Indomethacin was shown to be effective for posttraumatic hemicrania continua and chronic paroxysmal hemicranias (Lay and Newman, 1999; Matharu and Goadsby, 2001). CGRP inhibitors have been increasingly used for primary migraine, and CGRP is suspected to play a role in the neuroinflammatory processes of traumatic headache (Adams et al., 2017; Piantino et al., 2019) and may play a role in both abortive and prophylactic treatment of post-traumatic migraine. Efficacy and recommendations for use of CGRP inhibitors in the context of PTC have yet to established.
Fig. 4
Neurogenic inflammation in acute central nervous system (CNS) injury. Acute CNS injury stimulates the release of neuropeptides, which lead to the development of neurogenic inflammation in the CNS, characterized by vasodilation, increased blood-brain barrier (BBB) permeability and cerebral edema. Arrows indicate sequence of events following acute CNS injury (Sorby-Adams et al., 2017).
Medication overuse may paradoxically exacerbate headache symptoms and prolong recovery times when superimposed upon pre-existing headache pathology. It may also develop when high-risk medications are used to treat concurrent injuries or chronic pains elsewhere in the body. Depending on the timing of clinical evaluation, it may be a presenting feature to diagnose rather than a complication to plan and counsel against. The risk of medication overuse headache increases when use exceeds >10 days per month for ergotamines, opioids and triptans and >15 days per month for simple analgesics. ICHD-3 criteria are as follows:
(1) A headache is occurring on greater than or equal to 15 days per month for a patient with a pre-existing headache disorder;
(2) Regular medication overuse for greater than 3 months of one or more drugs that can be taken for acute and/or symptomatic treatment of a headache; and
(3) Not better accounted for by another ICHD-3 diagnosis.
Whether the pathophysiology of headache exacerbation in non-traumatic headache conditions is comparable to that of traumatic headaches is unknown (Heyer et al., 2014), as are any specific classes or dose thresholds of medications distinct from non-traumatic exacerbators of chronic headache. When headaches are persistent in the setting of trauma or accompanied by specific clinical features, imaging is often considered. Recently published evidence-based guidelines from the American Headache Society (Evans et al., 2020) suggest that for migraine, neuroimaging should not be routinely performed but should be considered when migraine is post-traumatic, atypical, features prolonged, severe or brainstem aura, features confusion or hemiplegia, is side-locked, presents in the context of dynamic frequency/severity/features, or is the patient’s first or worst ever migraine. These recommendations were noted, however, to continue to be based on consensus opinion (Grade C). Obviously, these recommendations do not necessarily apply to other potential suspected PTC etiologies that may require cerebral neuroimaging.
In the last several years, at least 15 clinical trials have been published relating to interventions for PTC including cervicogenic headache. For example, acute treatment of post-traumatic headache with commonly used ED migraine abortives metoclopramide+diphenhydramine was examined by Friedman et al. (2018). Twenty-one patients meeting ICHD criteria for acute post-traumatic headache were administered IV metoclopramide 20 mg+ diphenhydramine 25 mg in the emergency department. Seven experienced recurrent moderate/severe headache within 48 hours, with the remainder reporting mild headache or remission by telephone interview. Five reported continued frequent or constant headache after one week.
Chan et al. (2015) retrospectively examined headache relief among 254 children and adolescents presenting to a tertiary children’s hospital ED with mild TBI and headache. Greater than 50% headache pain reduction (as measured on a 1–10 numeric rating scale) was achieved with several different IV medications, including ketorolac (80%), ketorolac with metoclopramide or prochlorperazine (89%), metoclopramide or prochlorperazine only (93%) or ondansetron only (78%). Thirty-seven percent of subjects had been pre-treated with ibuprofen or acetaminophen. Dubrovsky et al. (2014) studied 28 children (mean 14.6 years) presenting for acute management of postconcussive headache. They were managed with either greater occipital nerve block or peripheral nerve blocks of the lesser occipital nerve and supraorbital nerve. Immediate headache resolution was noted in 71% following the intervention and 93% reported headache relief lasting longer than 24 hours. Of the 82% who completed follow up surveys at an unspecified time, 26% reported that the procedure had cured headache entirely.
An observational study by Erickson et al. (2011) retrospectively reviewed the histories of 100 military personnel (99 male) with ICHD-defined mTBI and chronic headache in terms of combination acute and prophylactic therapies. For acute therapy, 73 used triptans and 33 used other medications including NSAIDs, acetaminophen, opioids, Excedrin, Cafergot and Midrin. 23% used multiple medications. Seventy percent of patients reported “relief” within 2 hours of triptan use, while only 42% of subjects using alternative acute medications did. Prophylactic medications included amitritptyline or nortriptyline 25–50 mg per day (48 subjects), topiramate 100 mg/day (29 subjects), Propranolol LA (18 subjects) and Depakote ER 500 mg daily (5 subjects). Two-thirds of subjects were compliant with prophylaxis over a three month period. Headache frequency was significantly decreased among subjects treated with topiramate (p = 0.02) but not the other prophylactic medications prescribed. In contrast, Kuczynski’s (2013) retrospective study of 44 concussed children and adolescents (mean age 14.1) showed a good response among 68% of those taking amitriptyline, and 75% of those taking melatonin. Five of six taking flunarazine with available response data also had a full response. Treatment response was “unknown” for 4 of 6 taking topiramate. Headaches satisfied criteria for a migrainous subtype in 39% and tension type in only 9%. Indomethacin was “successfully” used for stabbing headache in two subjects, and one subject with suspected occipital neuralgia responded to injections of lidocaine and triamcinolone.
Chronic management was explored further by Seeger et al. in 2015 in a small single center retrospective study of 15 subjects (mean age 15.5) with post-traumatic headache (11 chronic, 4 subacute). Six met criteria for occipital neuralgia and eitght had occipital tenderness. An additional 3 had cervical pain and 6 had migrainous features. Daily headaches were occurring in 13 of 15 patients at the time of treatment performed a median of 5.57 (+/–3.5) months postinjury. Follow up was performed at an equal median of time post-procedure, 5.57 (+/–3.52) months. Nine participants had a “full” (>50%) reduction in headache frequency at follow up, and 1 had a < 50% response. Seven of the ten with response did not have a diagnosis of occipital neuralgia.
Cushman et al. retrospectively analyzed 277 children and adults (median age 23) presenting to an academic sports medicine practice for headache treatment over 1 year and returning for at least one follow up visit. Patients receiving a median dose of 20 mg amitriptyline, 900 mg gabapentin or no medication experienced similar reductions in headache symptom scores.
For chronic post-traumatic headaches, a prospective study of 22 active duty service members and 3 dependents with chronic post-traumatic headache, specifically post-concussive headache, with onset of headache symptoms occurring within 7 days of concussion and persistence of headaches >4 weeks. Subjects were between 1 month and 10 years beyond their inciting trauma at the beginning of retrospective analysis, which lasted 2 years. Prospective interventions included outpatient neurology follow up emphasizing both pharmacotherapy and non-pharmacotherapy options such as oral hydration therapy, sleep hygiene, stress reduction and where possible, down-titration or discontinuation of either abortive or preventative medications used for treatment of headache. Botulinum toxin was used in 2 of 25 patients. After 1 year, there was a 26% decrease in headache frequency, a 56% decrease in headache severity and 60% reported improved quality of life (Baker et al., 2018). Wan et al. (2017) demonstrated comparable short and long-term efficacy in 60 patients using ultrasound guided versus fluoroscopy guided C2-C3 cervical plexus block for the treatment of cervicogenic headache. When greater occipital nerve blocks are effective for pain relief, a subcompartmental procedure technique under fluoroscopy may achieve pain relief for far longer periods (24 weeks) than a traditional greater occipital nerve block (2 weeks) (Lauretti et al., 2015).
Other studies have examined chronic cervicogenic headaches but are not clearly or safely applicable to the post-traumatic population. A 2016 randomized controlled comparison of cervical/thoracic manipulation to mobilization and exercise but excluded participants with a history of whiplash injury in the prior 6 weeks (Dunning et al., 2016). A dual center prospective study reporting a linear dose-response relationship of spinal manipulation with reductions in cervicogenic headache excluded subjects with a history of brain and neck trauma in the prior 5 years (Haas et al., 2018). As noted above, there have been studies addressing treatment of post-traumatic headache with physical interventions that have shown efficacy (Kennedy, Quinn, Tumilty, et al., 2017).
In chronic PTC cases it is critically important to take a biopsychosocial approach to both assessment and management. There is a large literature on the importance of behavioral and psychological interventions in pain management with a more limited number specifically germane to PTC (Zasler, Martelli, et al., 2019). It is also very important for clinicians to recognize and treat central sensitization (Woolf, 2011) in this patient population as it is likely an underdiagnosed consequence of acute and subacute headache pain generators that are suboptimally managed. Treatment of central sensitization remains challenging and debated but treatment protocols have been proposed (Nijs, Malfliet, Ickmans, et al., 2014; Nijs, Goubert, Ickmans, 2016; Zasler, Martelli, Jordan, 2019). A multipronged approach has been shown to have the best results by focusing on specific targets for desensitization including both bottom up and top down strategies such as enteral medications, topical analgesic therapies, metabolic and neurotrophic factors, and neuromodulation all with the goal of decreasing hyperexcitability in the CNS (Nijs, Malfliet, Ickmans, et al., 2014; Zasler, Etheredge, 2019).
8Limitations of existing PTC literature
The vast majority of the extant literature has relied on IHS ICHD classification to drive data regarding headache subtype incidence. The non-specific nature of the current classification of post-traumatic headache and the studies emanating from same, as noted above, provide little, if any, useful information to the clinician regarding the specific headache diagnosis or the implicit treatment options. The PTC literature is also highly variable in study methodologies, criteria for TBI versus head/cranial trauma versus cervical whiplash. The amount of variance across studies in headache subtype incidence as well as persistence of headache suggests that we need to more critically examine how these studies are being conducted. Very few studies have examined historical markers as headache subtype risk factors or physical examination findings and their correlation with headache subtypes. The role of response biases in headache reporting relative to cultural, affective, nocebo, negative expectancies and secondary gain incentives to under-report versus over-report subjective headache symptoms have all been poorly explored (Zasler, Etheredge, 2020).
9Conclusion
The post-traumatic cephalalgias continue to be a complex and frequently encountered challenge. They encompass a wide range of presentations sharing a common etiologic thread but diverse in their clinical priming, pathophysiology and clinical course. Current classification using the ICHD-3 has significant limitations that warrant reassessment of the classification methodology. The importance of an adequate trauma and headache history as well as relevant headache physical examination cannot be overstated in the context of arriving at accurate diagnostic impressions and improving the efficacy of recommended treatments. Readers are referred to more comprehensive treatises on the topic of PTC history and physical examination (Zasler, Etheredge, 2020; Zasler, Haider, et al., 2020; Zasler, Leddy, Etheredge, Martelli, 2019). Traumatic brain injury may be comorbid with cranial/cranial adnexal injury, cervical acceleration deceleration injuries (whiplash), vestibular injury, vascular or meningeal injury, nerve compression, and limb or trunk injury exacerbating deleterious sleep disturbance and medication use patterns. Clinicians should also remember that PTC frequently occurs unrelated to brain injury but due to other post-traumatic pain generators in the head and neck. It may be conceptually useful to apply primary headache category subtypes to traumatic headache presentations, especially given that the evidence basis for medical management is heavily founded upon non-traumatic headache research. Applications are, however, limited by the inherently individualized pathology of head, neck and brain injury.
Novel applications of diagnostic imaging after head/brain injury continue to be explored and could eventually be used to prioritize management options, develop new management tools or inform prognosis. It will be important to further distinguish traumatic structural and functional imaging changes from those that are specific to traumatic headache; likewise, distinguishing traumatic headache-related findings from headache-associated findings should be a priority. Also unclear are the pathophysiologic differences between immediate versus delayed onset of post-traumatic headache within definitional acute criteria, and those with constant versus intermittent frequency or a resolving versus persistent course. A multifactorial diagnostic and treatment approach, cognizant of biopsychosocial factors as well as the unique interplay between central and musculoskeletal pain, sleep, mood, cognition and exertional limitations, continues to be most successful.
Conflict of interest
Dr. Dwyer and Dr. Zasler have no conflicts of interest.
Headache resources
American Headache Society
https://americanheadachesociety.org
American Headache Society Committee for Headache Education (ACHE)
Information for Health Care Professionals: Concussion and Post-Traumatic Headache
https://americanheadachesociety.org/wp-content/uploads/2018/05/Alan_Finkel_-_Concussion_and_PTH.pdf. Copyright © 2019 American Psychiatric Association Publishing. Posttraumatic Headache 487
American Migraine Foundation
https://americanmigrainefoundation.org
https://americanmigrainefoundation.org/understanding-migraine/post-traumaticheadache
Brain Injury Association of America
Brainline
www.brainline.org/contentfinder?keys=headache
International Headache Society
National Headache Foundation
References
[1] | Akin, F. W , Murnane, O. D , Hall, C. D , Riska, K. M. ((2017) ). Vestibular consequences of mild traumatic brain injury and blast exposure: a review. Brain Inj, 31: (9), 1188–1194. doi: 10.1080/02699052.2017.1288928 |
[2] | Alhilali, L. M , Delic, J , Fakhran, S. ((2017) ). Differences in Callosal and Forniceal Diffusion between Patients with and without Postconcussive Migraine. AJNR Am J Neuroradiol, 38: (4), 691–695. doi: 10.3174/ajnr.A5073 |
[3] | Andersen, A. M , Ashina, H , Iljazi, A , Al-Khazali, H. M , Chaudhry, B , Ashina, M ,... & Schytz, H. W. ((2020) ). Risk Factors for the Development of Post-Traumatic Headache Attributed to Traumatic Brain Injury: A Systematic Review. Headache. doi:10.1111/head.13812 |
[4] | Appenzeller, O. , Posttraumatic headaches. In Wolfe’s Headache and Other Head Pain. Sixth edition. EDS: D.J. Dalessio and Silberstein. Oxford University press. New York. (1993) , pages 365–383. |
[5] | Ashina, H , Porreca, F , Anderson, T , Amin, F. M , Ashina, M , Schytz, H. W , Dodick, D. W. ((2019) ). Post-traumatic headache: epidemiology and pathophysiological insights. Nat Rev Neurol, 15: (10), 607–617. doi: 10.1038/s41582-019-0243-8 |
[6] | Ashkenazi, A , Blumenfeld, A , Napchan, U , Narouze, S , Grosberg, B , Nett, R ,... & Interventional Procedures Special Interest Section of the, A. ((2010) ). Peripheral nerve blocks and trigger point injections in headache management - a systematic review and suggestions for future research. Headache, 50: (6)943–952. doi: 10.1111/j.1526-4610.2010.01675.x |
[7] | Baandrup, L , Jensen, R. ((2005) ). Chronic post-traumatic headache–a clinical analysis in relation to the International Headache Classification 2nd Edition. Cephalalgia, 25: (2), 132–138. doi: 10.1111/j.1468-2982.2004.00818.x |
[8] | Baker, V. B , Eliasen, K. M , Hack, N. K. ((2018) ). Lifestyle modifications as therapy for medication refractory post-traumatic headache (PTHA) in the military population of Okinawa. J Headache Pain, 19: (1), 113. doi: 10.1186/s10194-018-0943-2 |
[9] | Barkhoudarian, G , Hovda, D. A , Giza, C. C. ((2016) ). The Molecular Pathophysiology of Concussive Brain Injury - an Update. Phys Med Rehabil Clin N Am, 27: (2), 373–393. doi: 10.1016/j.pmr.2016.01.003 |
[10] | Barlow, K. M , Marcil, L. D , Dewey, D , Carlson, H. L , MacMaster, F. P , Brooks, B. L , Lebel, R. M. ((2017) ). Cerebral Perfusion Changes in Post-Concussion Syndrome: A Prospective Controlled Cohort Study. J Neurotrauma, 34: (5), 996–1004. doi: 10.1089/neu.2016.4634 |
[11] | Barros, J , Damasio, J , Tuna, A , Alves, I , Silveira, I , Pereira-Monteiro, J ,... & Coutinho, P. ((2013) ). Cerebellar ataxia, hemiplegic migraine, and related phenotypes due to a CACNA1A missense mutation: 12-year follow-up of a large Portuguese family. JAMA Neurol, 70: (2), 235–240. doi: 10.1001/jamaneurol.2013.591 |
[12] | Bartsch, T , Goadsby, P.J. ((2003) ). The trigeminocervical complext and migraine: current concepts and synthesis. Cur Pain Headache Rep, 7: , 371–376. doi: 10.1007/s11916-003-0036-y |
[13] | Bendtsen, L , Buchgreitz, L , Ashina, S , Jensen, R. ((2007) ). Combination of low-dose mirtazapine and ibuprofen for prophylaxis of chronic tension-type headache. Eur J Neurol, 14: (2), 187–193. doi: 10.1111/j.1468-1331.2006.01607.x |
[14] | Benoliel, R , Birenboim, R , Regev, E , Eliav, E. ((2005) ). Neurosensory changes in the infraorbital nerve following zygomatic fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 99: (6), 657–665. doi: 10.1016/j.tripleo.2004.10.014 |
[15] | Benoliel, R , Teich, S , Eliav, E. ((2016) ). Painful Traumatic Trigeminal Neuropathy. Oral Maxillofac Surg Clin North Am, 28: (3), 371–380. doi: 10.1016/j.coms.2016.03.002 |
[16] | Chan, S , Kurowski, B , Byczkowski, T , Timm, N. ((2015) ). Intravenous migraine therapy in children with posttraumatic headache in the ED. Am J Emerg Med, 33: (5), 635–639. doi: 10.1016/j.ajem.2015.01.053. |
[17] | Charles, A. C , Baca, S. M. ((2013) ). Cortical spreading depression and migraine. Nat Rev Neurol, 9: (11), 637–644. doi: 10.1038/nrneurol.2013.192 |
[18] | Conidi, F. X. ((2016) ). Interventional Treatment for Post-traumatic Headache. Curr Pain Headache Rep, 20: (6), 40. doi: 10.1007/s11916-016-0570-z |
[19] | Cooksley, R , Maguire, E , Lannin, N. A , Unsworth, C. A , Farquhar, M , Galea, C ,... & Schmidt, J. ((2018) ). Persistent symptoms and activity changes three months after mild traumatic brain injury. Aust Occup Ther J, 65: (3), 168–175. doi: 10.1111/1440-1630.12457 |
[20] | Couch, J. R , Bearss, C. ((2001) ). Chronic daily headache in the posttrauma syndrome: relation to extent of head injury. Headache, 41: (6), 559–564. doi: 10.1046/j.1526-4610.2001.041006559.x |
[21] | Cushman, D. M , Borowski, L , Hansen, C , Hendrick, J , Bushman, T , Teramoto, M. ((2019) ). Gabapentin and Tricyclics in the Treatment of Post-Concussive Headache, a Retrospective Cohort Study. Headache, 59: (3), 371–382. doi: 10.1111/head.13451 |
[22] | D’Onofrio, F , Russo, A , Conte, F , Casucci, G , Tessitore, A , Tedeschi, G. ((2014) ). Post-traumatic headaches: an epidemiological overview. Neurol Sci, 35: (Suppl 1), 203–206. doi: 10.1007/s10072-014-1771-z |
[23] | Delic, J , Alhilali, L. M , Hughes, M. A , Gumus, S , Fakhran, S. ((2016) ). White Matter Injuries in Mild Traumatic Brain Injury and Posttraumatic Migraines: Diffusion Entropy Analysis. Radiology, 279: (3), 859–866. doi: 10.1148/radiol.2015151388 |
[24] | Donovan, D. J , Iskandar, J. I , Dunn, C. J , King, J. A. ((2008) ). Aeromedical evacuation of patients with pneumocephalus: outcomes in 21 cases. Aviat Space Environ Med, 79: (1), 30–35. doi: 10.3357/asem.1893.2008 |
[25] | Dubrovsky, A. S , Friedman, D , Kocilowicz, H. ((2014) ). Pediatric post-traumatic headaches and peripheral nerve blocks of the scalp: a case series and patient satisfaction survey. Headache, 54: (5), 878–887. doi: 10.1111/head.12334 |
[26] | Dumkrieger, G , Chong, C. D , Ross, K , Berisha, V , Schwedt, T. J. ((2019) ). Static and dynamic functional connectivity differences between migraine and persistent post-traumatic headache: A resting-state magnetic resonance imaging study. Cephalalgia,, 39: (11), 1366–1381. doi: 10.1177/0333102419847728 |
[27] | Dunning, J. R , Butts, R , Mourad, F , Young, I , Fernandez-de-Las Penas, C , Hagins, M ,... & Cleland, J. A. ((2016) ). Upper cervical and upper thoracic manipulation versus mobilization and exercise in patients with cervicogenic headache: a multi-center randomized clinical trial. BMC Musculoskelet Disord, 17: , 64–10.1186/s12891-016-0912-3 |
[28] | Dwyer, B , Katz, D. I. ((2018) ). Postconcussion syndrome. Handb Clin Neurol, 158: , 163–178. doi: 10.1016/B978-0-444-63954-7.00017-3 |
[29] | Elahi, F , Reddy, C. ((2014) ). Neuromodulation of the great auricular nerve for persistent post-traumatic headache. Pain Physician, 17: (4), E531–536. |
[30] | Ellis, M.J , Leddy, J.J , Willer, B. ((2015) ). physiological, vestibulo-ocular and cervicogenic post-concussion disorders: An evidence-based classification system with directions for treatment. Brain Injury, 29: (2), 238–248. doi: 10.3109/02699052.2014.965207 |
[31] | Erickson, J. C. ((2011) ). Treatment outcomes of chronic post-traumatic headaches after mild head trauma in US soldiers: an observational study. Headache, 51: (6), 932–944. doi: 10.1111/j.1526-4610.2011.01909.x |
[32] | Evans, R. W , Burch, R. C , Frishberg, B. M , Marmura, M. J , Mechtler, L. L , Silberstein, S. D , Turner, D. P. ((2020) ). Neuroimaging for Migraine: The American Headache Society Systematic Review and Evidence-Based Guideline. Headache, 60: (2), 318–336. doi: 10.1111/head.13720 |
[33] | Evered, L , Ruff, R , Baldo, J , Isomura, A. ((2003) ). Emotional risk factors and postconcussional disorder. Assessment, 10: (4), 420–427. doi: 10.1177/1073191103259539 |
[34] | Ferrante, E , Savino, A , Sances, G , Nappi, G. ((2004) ). Spontaneous intracranial hypotension syndrome: report of twelve cases. Headache, 44: (6), 615–622. doi: 10.1111/j.1526-4610.2004.446012.x |
[35] | Fakhran, S , Qu, C , Alhilali, L.M. ((2016) ). Effect of the suboccipital musculature on symptom severity and recovery after mild traumatic brain injury. AJNR, 37: (8), 1556–1560. DOI: https://doi.org/10.3174/ajnr.A4730 |
[36] | Friedman, B. W , Babbush, K , Irizarry, E , White, D , John Gallagher, E. ((2018) ). An exploratory study of IV metoclopramide+diphenhydramine for acute post-traumatic headache. Am J Emerg Med, 36: (2), 285–289. doi: 10.1016/j.ajem.2017.10.034 |
[37] | Gawel, M. J , Rothbart, P. J. ((1992) ). Occipital nerve block in the management of headache and cervical pain. Cephalalgia, 12: (1), 9–13. doi: 10.1046/j.1468-2982.1992.1201009.x |
[38] | Giza, C. C , Hovda, D. A. ((2014) ). The new neurometabolic cascade of concussion. Neurosurgery, 75: (Suppl 4), S24–33. doi: 10.1227/NEU.0000000000000505 |
[39] | Giza, C. C , Kutcher, J. S , Ashwal, S , Barth, J , Getchius, T. S , Gioia, G. A ,... & Zafonte, R. ((2013) ). Summary of evidence-based guideline update: evaluation and management of concussion in sports: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology, 80: (24), 2250–2257. doi: 10.1212/WNL.0b013e31828d57dd |
[40] | Gormley, P , Anttila, V , Winsvold, B. S , Palta, P , Esko, T , Pers, T. H ,... & Palotie, A. ((2016) ). Meta-analysis of 375,000 individuals identifies 38 susceptibility loci for migraine. Nat Genet, 48: (8), 856–866. doi: 10.1038/ng.3598 |
[41] | Greiffenstein, F. M , Baker, J. W. ((2001) ). Comparison of premorbid and postinjury mmpi-2 profiles in late postconcussion claimants. Clin Neuropsychol, 15: (2), 162–170. doi: 10.1076/clin.15.2.162.1895 |
[42] | Gurer, B , Kertmen, H , Dolgun, H , Sekerci, Z. ((2016) ). Late onset of subdural hematoma after bifrontal contusion. Asian J Neurosurg, 11: (4), 448–10.4103/1793-5482.145115 |
[43] | Haas, D. C. ((1996) ). Chronic post-traumatic headaches classified and compared with natural headaches. Cephalalgia, 16: (7), 486–493. doi: 10.1046/j.1468-2982.1996.1607486.x |
[44] | Haas, M , Bronfort, G , Evans, R , Schulz, C , Vavrek, D , Takaki, L ,... & Neradilek, M. B. ((2018) ). Dose-response and efficacy of spinal manipulation for care of cervicogenic headache: a dual-center randomized controlled trial. Spine J, 18: (10), 1741–1754. doi: 10.1016/j.spinee.2018.02.019 |
[45] | Hack, G. D , Koritzer, R. T , Robinson, W. L , et al. ((1995) ). anatomic relation between the rectus capitis posterior minor muscle and the dura mater. Spine, 20: (23), 2484–2486. doi: 10.1097/00007632-199512000-00003 |
[46] | Headache Classification Committee of the International Headache, S. ((2013) ). The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia, 33: (9), 629–808. doi: 10.1177/0333102413485658 |
[47] | Hecht, J. S. ((2004) ). Occipital nerve blocks in postconcussive headaches: a retrospective review and report of ten patients. J Head Trauma Rehabil, 19: (1), 58–71. doi: 10.1097/00001199-200401000-00006 |
[48] | Herd, A , Ludwig, L. ((1994) ). Relief of posttraumatic headache by intravenous chlorpromazine. J Emerg Med, 12: (6), 849–851. doi: 10.1016/0736-4679(94)90496-0 |
[49] | Heyer, G. L , Idris, S. A. ((2014) ). Does analgesic overuse contribute to chronic post-traumatic headaches in adolescent concussion patients? Pediatr Neurol, 50: (5), 464–468. doi: 10.1016/j.pediatrneurol.2014.01.040 |
[50] | Hoge, C. W , McGurk, D , Thomas, J. L , Cox, A. L , Engel, C. C , Castro, C. A. ((2008) ). Mild traumatic brain injury in U.S. Soldiers returning from Iraq. N Engl J Med, 358: (5), 453–463. doi: 10.1056/NEJMoa072972 |
[51] | Hoffman, J. M , Lucas, S , Dikmen, S , et al. ((2011) ). Natural history of headache after traumatic brian injury. J Neurotrauma, 28: (9), 1719–1725. doi: 10.1089/neu.2011.1914 |
[52] | Horn, L. J , Siebert, B , Patel, N , Zasler, N. D. ((2013) ). Post traumatic headache. In: Zasler, ND, Katz, DI, Zafonte, RD (eds): Brain Injury Medicine: Principles and Practice, Second Edition, Demos Medical Publishing, page 936. |
[53] | Illingworth, R , Shawdon, H. ((1983) ). Conservative management of intracranial extradural haematoma presenting late. J Neurol Neurosurg Psychiatry, 46: (6), 558–560. doi: 10.1136/jnnp.46.6.558 |
[54] | Jacob, S , Saha, A , Rajabally, Y. ((2008) ). Post-traumatic short-lasting unilateral headache with cranial autonomic symptoms (SUNA). Cephalalgia, 28: (9), 991–993. doi: 10.1111/j.1468-2982.2008.01622.x |
[55] | Kamins, J , Charles, A. ((2018) ). Posttraumatic Headache: Basic Mechanisms and Therapeutic Targets. Headache, 58: (6), 811–826. doi: 10.1111/head.13312 |
[56] | Katta-Charles, S , Tessler, J , Horn, L. J. ((2021) ). Post-traumatic headache. IIn: Zasler, ND, Katz, DI, Zafonte, RD (eds): Brain Injury Medicine: Principles and Practice, Third Edition, Demos Medical Publishing. |
[57] | Kennedy, E , Quinn, D , Chapple, C , Tumilty, S. ((2019) ). Can the neck contribute to persistent symptoms post-concussion? a prospective descriptive case series. SPT, 49: (11), 845–856. doi: 10.2519/jospt.2019.8547 |
[58] | Kennedy, E , Quinn, D , Tumilty, S , Chapple, C. ((2017) ). Clinical characteristics and outcomes of treatment of the cervical spine in patients with persistent post-concussion symptoms: A retrospective analysis. Musculoskelet Sci Pract, 29: , 91–98. doi: 10.1016/j.msksp.2017.03.002 |
[59] | Kontos, A. P , Elbin, R. J , Lau, B , Simensky, S , Freund, B , French, J , Collins, M. W. ((2013) ). Posttraumatic migraine as a predictor of recovery and cognitive impairment after sport-related concussion. Am J Sports Med, 41: (7), 1497–1504. doi: 10.1177/0363546513488751 |
[60] | Kors, E. E , Terwindt, G. M , Vermeulen, F. L , Fitzsimons, R. B , Jardine, P. E , Heywood, P ,... & Ferrari, M. D. ((2001) ). Delayed cerebral edema and fatal coma after minor head trauma: role of the CACNA1A calcium channel subunit gene and relationship with familial hemiplegic migraine. Ann Neurol, 49: (6), 753–760. doi: 10.1002/ana.1031 |
[61] | Kranz, P. G , Malinzak, M. D , Amrhein, T. J , Gray, L. ((2017) ). Update on the Diagnosis and Treatment of Spontaneous Intracranial Hypotension. Curr Pain Headache Rep, 21: (8), 37–10.1007/s11916-017-0639-3 |
[62] | Kuczynski, A , Crawford, S , Bodell, L , Dewey, D , Barlow, K. M. ((2013) ). Characteristics of post-traumatic headaches in children following mild traumatic brain injury and their response to treatment: a prospective cohort. Dev Med Child Neurol, 55: (7), 636–641. doi: 10.1111/dmcn.12152 |
[63] | Larsen, E. L , Ashina, H , Iljazi, A , Al-Khazali, H. M , Seem, K , Ashina, M ,... & Schytz, H. W. ((2019) ). Acute and preventive pharmacological treatment of post-traumatic headache: a systematic review. J Headache Pain, 20: (1), 98–10.1186/s10194-019-1051-7 |
[64] | Lauretti, G. R , Correa, S. W , Mattos, A. L. ((2015) ). Efficacy of the Greater Occipital Nerve Block for Cervicogenic Headache: Comparing Classical and Subcompartmental Techniques. Pain Pract, 15: (7), 654–661. doi: 10.1111/papr.12228 |
[65] | Lay, C. L , Newman, L. C. ((1999) ). Posttraumatic hemicrania continua. Headache, 39: (4), 275–279. doi: 10.1046/j.1526-4610.1999.3904275.x |
[66] | Leroux, E , Ducros, A. ((2013) ). Occipital injections for trigemino-autonomic cephalalgias: evidence and uncertainties. Curr Pain Headache Rep, 17: (4), 325–10.1007/s11916-013-0325-z |
[67] | Leung, A , Metzger-Smith, V , He, Y , Cordero, J , Ehlert, B , Song, D ,... & Lee, R. ((2018) ). Left Dorsolateral Prefrontal Cortex rTMS in Alleviating MTBI Related Headaches and Depressive Symptoms. Neuromodulation, 21: (4), 390–401. doi: 10.1111/ner.12615 |
[68] | Leung, A , Shukla, S , Fallah, A , Song, D , Lin, L , Golshan, S ,... & Lee, R. ((2016) ). Repetitive Transcranial Magnetic Stimulation in Managing Mild Traumatic Brain Injury-Related Headaches. Neuromodulation, 19: (2), 133–141. doi: 10.1111/ner.12364 |
[69] | Levin, H. S , Mattis, S , Ruff, R. M , Eisenberg, H. M , Marshall, L. F , Tabaddor, K ,... & Frankowski, R. F. ((1987) ). Neurobehavioral outcome following minor head injury: a three-center study. J Neurosurg, 66: (2), 234–243. doi: 10.3171/jns.1987.66.2.0234 |
[70] | Lew, H.L , Lin, P.H , Fuh, J.L , et al. ((2006) ). Characteristics and Treatment of Headache After Traumatic Brain Injury: A Focused Review. Am J Phys Med Rehabil, 85: (7), 619–627. doi: 10.1097/01.phm.0000223235.09931.c0 |
[71] | Lucas, S. ((2015) ). Characterization and Management of Headache after Mild Traumatic Brain Injury. In F. H. Kobeissy (Ed.), Brain Neurotrauma: Molecular Neuropsychological and Rehabilitation Aspects. Boca Raton (FL). |
[72] | Lucas, S , Hoffman, J. M , Bell, K. R , Dikmen, S. ((2014) ). A prospective study of prevalence and characterization of headache following mild traumatic brain injury. Cephalalgia, 34: (2), 93–102. doi: 10.1177/0333102413499645 |
[73] | Lucas, S , Hoffman, J. M , Bell, K. R , Walker, W , Dikmen, S. ((2012) ). Characterization of headache after traumatic brain injury. Cephalalgia, 32: (8), 600–606. doi: 10.1177/0333102412445224 |
[74] | Marshall, C.M , Vernon, H , Leddy, J.J , et al. ((2015) ). The role of the cervical spine in post-concussion syndrome. Phys Sportsmed, 43: (3), 274–84. doi: 10.1080/00913847.2015.1064301 |
[75] | Matharu, M. J , Goadsby, P. J. ((2001) ). Post-traumatic chronic paroxysmal hemicrania (CPH) with aura. Neurology, 56: (2), 273–275. doi: 10.1212/wnl.56.2.273 |
[76] | McBeath, J. G , Nanda, A. ((1994) ). Use of dihydroergotamine in patients with postconcussion syndrome. Headache, 34: (3), 148–151. doi: 10.1111/j.1526-4610.1994.hed3403148.x |
[77] | McCrory, P , Meeuwisse, W , Dvorak, J , Aubry, M , Bailes, J , Broglio, S ,... & Vos, P. E. ((2017) ). Consensus statement on concussion in sport-the 5(th) international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med, 51: (11), 838–847. doi: 10.1136/bjsports-2017-097699. |
[78] | Meares, S , Shores, E. A , Taylor, A. J , Batchelor, J , Bryant, R. A , Baguley, I. J ,... & Marosszeky, J. E. ((2011) ). The prospective course of postconcussion syndrome: the role of mild traumatic brain injury. Neuropsychology, 25: (4), 454–465. doi: 10.1037/a0022580 |
[79] | Mokri, B. ((2014) ). Spontaneous CSF leaks: low CSF volume syndromes. Neurol Clin, 32: (2), 397–422. doi: 10.1016/j.ncl.2013.11.002 |
[80] | Mooney, G , Speed, J. ((2001) ). The association between mild traumatic brain injury and psychiatric conditions. Brain Inj, 15: (10), 865–877. doi: 10.1080/02699050110065286 |
[81] | Nardone, R , Sebastianelli, L , Versace, V , Brigo, F , Golaszewski, S , Manganotti, P ,... & Trinka, E. ((2020) ). Repetitive transcranial magnetic stimulation in traumatic brain injury: Evidence from animal and human studies. Brain Res Bull, 159: , 44–52. doi: 10.1016/j.brainresbull.2020.03.016 |
[82] | Nijs, J , Goubert, D , Ickmans, K. ((2016) ). recognition and treatment of central sensitization in chronic pain patients: Not limited to specialized care. JOSPT, 46: (12), 1024–1028. doi: 10.2519/jospt.2016.0612 |
[83] | Nijs, J , Malfliet, A , Ickmans, K , et al. ((2014) ). Treatment of central sensitization in patients with “unexplained” chronic pain: an update . Expert Opin Pharmacother, 15: (12), 1671–83. doi: 10.1517/14656566.2014.925446 |
[84] | Ofoghi, Z , Dewey, D , Barlow, K. M. ((2020) ). A Systematic Review of Structural and Functional Imaging Correlates of Headache or Pain after Mild Traumatic Brain Injury. J Neurotrauma, 37: (7), 907–923. doi: 10.1089/neu.2019.6750 |
[85] | Packard, R. C. ((1999) ). Epidemiology and pathogenesis of posttraumatic headache. J Head Trauma Rehabil, 14: (1)9–21. doi: 10.1097/00001199-199902000-00004 |
[86] | Packard, R.C. The relationship of neck injury and post-traumatic headache. ((2002) ). Curr Pain Headache Rep, 6: (4), 301–307. doi: 10.1007/s11916-002-0051-4 |
[87] | Pareja, J. A , Caminero, A. B. ((2006) ). Supraorbital neuralgia. { 302–305. doi: 10.1007/s11916-006-0036-9 |
[88] | Patil, V. K , St Andre, J. R , Crisan, E , Smith, B. M , Evans, C. T , Steiner, M. L , Pape, T. L. ((2011) ). Prevalence and treatment of headaches in veterans with mild traumatic brain injury. Headache, 51: (7), 1112–1121. doi: 10.1111/j.1526-4610.2011.01946.x |
[89] | Piantino, J , Lim, M. M , Newgard, C. D , Iliff, J. ((2019) ). Linking Traumatic Brain Injury, Sleep Disruption and Post-Traumatic Headache: a Potential Role for Glymphatic Pathway Dysfunction. Curr Pain Headache Rep, 23: (9), 62. doi: 10.1007/s11916-019-0799-4 |
[90] | Ponsford, J , Willmott, C , Rothwell, A , Cameron, P , Kelly, A. M , Nelms, R ,... & Ng, K. ((2000) ). Factors influencing outcome following mild traumatic brain injury in adults. J Int Neuropsychol Soc, 6: (5), 568–579. doi: 10.1017/s1355617700655066 |
[91] | Primalani, N. K , Quek, T. J , Low, D. C. Y , Low, S. Y. Y. ((2019) ). Spontaneous Intracranial Hypotension Presenting As Cervicogenic Headache: Case Report and Review of Literature. World Neurosurg, 130: , 550–554. doi: 10.1016/j.wneu.2019.05.107 |
[92] | Prins, M. L , Matsumoto, J. ((2016) ). Metabolic Response of Pediatric Traumatic Brain Injury. J Child Neurol, 31: (1), 28–34. doi: 10.1177/0883073814549244 |
[93] | Putzki, N , Nirkko, A , Diener, H. C. ((2005) ). Trigeminal autonomic cephalalgias: a case of post-traumatic SUNCT syndrome? Cephalalgia, 25: (5), 395–397. doi: 10.1111/j.1468-2982.2004.00860.x |
[94] | Rohling, M. L , Binder, L. M , Demakis, G. J , Larrabee, G. J , Ploetz, D. M , Langhinrichsen-Rohling, J. ((2011) ). A meta-analysis of neuropsychological outcome after mild traumatic brain injury: re-analyses and reconsiderations of Binder et al. (1997), Frencham et al. (2005), and Pertab et al. (2009). Clin Neuropsychol, 25: (4), 608–623. doi: 10.1080/13854046.2011.565076 |
[95] | Ruet, A , Bayen, E , Jourdan, C , Ghout, I , Meaude, L , Lalanne, A ,... & Azouvi, P. ((2019) ). A Detailed Overview of Long-Term Outcomes in Severe Traumatic Brain Injury Eight Years Post-injury. Front Neurol, 10: , 120. doi: 10.3389/fneur.2019.00120 |
[96] | Samii, C , Mobius, E , Weber, W , Heienbrok, H. W , Berlit, P. ((1999) ). Pseudo Chiari type I malformation secondary to cerebrospinal fluid leakage. J Neurol, 246: (3), 162–164. doi: 10.1007/s004150050327 |
[97] | Schiapparelli, P , Allais, G , Castagnoli Gabellari, I , Rolando, S , Terzi, M. G , Benedetto, C. ((2010) ). Non-pharmacological approach to migraine prophylaxis: part II. Suppl, 31: (Suppl 1), S137–139. doi: 10.1007/s10072-010-0307-4 |
[98] | Schwedt, T. J , Chong, C. D , Peplinski, J , Ross, K , Berisha, V. ((2017) ). Persistent post-traumatic headache vs. migraine: an MRI study demonstrating differences in brain structure. J Headache Pain, 18: (1), 87. doi: 10.1186/s10194-017-0796-0 |
[99] | Sedighi, A , Nakhostin Ansari, N , Naghdi, S. ((2017) ). Comparison of acute effects of superficial and deep dry needling into trigger points of suboccipital and upper trapezius muscles in patients with cervicogenic headache. J Bodyw Mov Ther, 21: (4), 810–814. doi: 10.1016/j.jbmt.2017.01.002 |
[100] | Seeger, T. A , Orr, S , Bodell, L , Lockyer, L , Rajapakse, T , Barlow, K. M. ((2015) ). Occipital Nerve Blocks for Pediatric Posttraumatic Headache: A Case Series. J Child Neurol, 30: (9), 1142–1146. doi: 10.1177/0883073814553973 |
[101] | Selwyn, R , Hockenbury, N , Jaiswal, S , Mathur, S , Armstrong, R. C , Byrnes, K. R. ((2013) ). Mild traumatic brain injury results in depressed cerebral glucose uptake: An (18)FDG PET study. J Neurotrauma, 30: (23), 1943–1953. doi: 10.1089/neu.2013.2928 |
[102] | Siavoshi, S , Dougherty, C , Ailani, J , Yadwadkar, K , Berkowitz, F. ((2016) ). An Unusual Case of Post-Traumatic Headache Complicated by Intracranial Hypotension. Brain Sci, 7: (1). doi: 10.3390/brainsci7010003 |
[103] | Silberstein, S. D. ((2015) ). Preventive Migraine Treatment. Continuum (Minneap Minn), 21: (4 Headache), 973–989. doi: 10.1212/CON.0000000000000199 |
[104] | Sorby-Adams, A. J , Marcoionni, A. M , Dempsey, E. R , Woenig, J. A , Turner, R. J. ((2017) ). The Role of Neurogenic Inflammation in Blood-Brain Barrier Disruption and Development of Cerebral Oedema Following Acute Central Nervous System (CNS) Injury. Int J Mol Sci, 18: (8). doi: 10.3390/ijms18081788 |
[105] | Stilling, J , Paxman, E , Mercier, L , Gan, L. S , Wang, M , Amoozegar, F ,... & Debert, C. ((2020) ). Treatment of Persistent Post-Traumatic Headache and Post-Concussion Symptoms Using Repetitive Transcranial Magnetic Stimulation: A Pilot, Double-Blind, Randomized Controlled Trial. J Neurotrauma, 37: (2), 312–323. doi: 10.1089/neu.2019.6692 |
[106] | Stovner, L. J , Schrader, H , Mickeviciene, D , Surkiene, D , Sand, T. ((2009) ). Headache after concussion. Eur J Neurol, 16: (1), 112–120. doi: 10.1111/j.1468-1331.2008.02363.x |
[107] | Sufrinko, A , McAllister-Deitrick, J , Elbin, R. J , Collins, M. W , Kontos, A. P. ((2018) ). Family History of Migraine Associated With Posttraumatic Migraine Symptoms Following Sport-Related Concussion. J Head Trauma Rehabil, 33: (1), 7–14. doi: 10.1097/HTR.0000000000000315 |
[108] | Sullivan, P. G , Geiger, J. D , Mattson, M. P , Scheff, S. W. ((2000) ). Dietary supplement creatine protects against traumatic brain injury. Ann Neurol, 48: (5), 723–729. |
[109] | Sussman, W. I , Mautner, K , Mason, R. A , Bonecutter, K , Shealy, A. K. ((2017) ). Sphenopalatine Ganglion Block for Management of Refractory Chronic Posttraumatic Headaches After a Sport-Related Concussion. Clin J Sport Med, 27: (2), e6–e8–10.1097/JSM.0000000000000325 |
[110] | Tanaka, Y , Tosaka, M , Fujimaki, H , Honda, F , Yoshimoto, Y. ((2016) ). Sex- and Age-Related Differences in the Clinical and Neuroimaging Characteristics of Patients With Spontaneous Intracranial Hypotension: A Records Review. Headache, 56: (8), 1310–1316. doi: 10.1111/head.12887 |
[111] | Theeler, B. J , Flynn, F. G , Erickson, J. C. ((2010) ). Headaches after concussion in US soldiers returning from Iraq or Afghanistan. Headache, 50: (8), 1262–1272. doi: 10.1111/j.1526-4610.2010.01700.x |
[112] | Tottene, A , Pivotto, F , Fellin, T , Cesetti, T , van den Maagdenberg, A. M , Pietrobon, D. ((2005) ). Specific kinetic alterations of human CaV2.1 calcium channels produced by mutation S218L causing familial hemiplegic migraine and delayed cerebral edema and coma after minor head trauma. J Biol Chem, 280: (18), 17678–17686. doi: 10.1074/jbc.M501110200 |
[113] | Tyburski, A.L , Cheng, L , Assari, S , et al. ((2017) ). Frequent mild head injury promotes trigeminal sensitivity concomitant with microglial proliferation, astrocytosis and increased neuropeptide levels in the trigeminal pain system. J Headache Pain, 18: (1), 16. doi: 10.1186/s10194-017-0726-1 |
[114] | van der Horn, H. J , Liemburg, E. J , Scheenen, M. E , de Koning, M. E , Marsman, J. B , Spikman, J. M , van der Naalt, J. ((2016) ). Brain network dysregulation, emotion, and complaints after mild traumatic brain injury. Hum Brain Mapp, 37: (4), 1645–1654. doi: 10.1002/hbm.23126 |
[115] | Vargas, B. B , Dodick, D. W. ((2012) ). Posttraumatic headache. Curr Opin Neurol, 25: (3), 284–289. doi: 10.1097/WCO.0b013e3283535bf5 |
[116] | Walker, W. C , Seel, R. T , Curtiss, G , Warden, D. L. ((2005) ). Headache after moderate and severe traumatic brain injury: a longitudinal analysis. Arch Phys Med Rehabil, 86: (9), 1793–1800. doi: 10.1016/j.apmr.2004.12.042 |
[117] | Wan, Q , Yang, H , Li, X , Lin, C , Ke, S , Wu, S , Ma, C. ((2017) ). Ultrasound-Guided versus Fluoroscopy-GuidedDeepCervical Plexus Block for the Treatment of Cervicogenic Headache. Biomed Res Int, 2017, 4654803. doi:10.1155/2017/4654803 |
[118] | Watanabe, T , Bell, K.R , Walker, W.C , Schomer, K. ((2012) ). Systematic Review of Interventions for Post-Traumatic Headache. PMR, 4: (2), 129–40. doi: 10.1016/j.pmrj.2011.06.003 |
[119] | Watson, D. H , Drummond, P. D. ((2016) ). The role of the trigeminocervical complex in chronic whiplash associated headache: a cross sectional study. Headache, 56: (6), 961–975. doi: 10.1111/head.12805 |
[120] | Weiss, H. D , Stern, B. J , Goldberg, J. ((1991) ). Post-traumatic migraine: chronic migraine precipitated by minor head or neck trauma. Headache, 31: (7), 451–456. doi: 10.1111/j.1526-4610.1991.hed3107451.x |
[121] | Woolf, C.J. ((2010) ). Central sensitization: Implications for the diagnosis and treatment of pain. Pain., 152: (3 Suppl), S2–15. doi: 10.1016/j.pain.2010.09.030 |
[122] | Xie, L , Kang, H , Xu, Q , Chen, M. J , Liao, Y , Thiyagarajan, M ,... & Nedergaard, M. ((2013) ). Sleep drives metabolite clearance from the adult brain. Science, 342: (6156), 373–377. doi: 10.1126/science.1241224 |
[123] | Yerry, J. A , Kuehn, D , Finkel, A. G. ((2015) ). Onabotulinum toxin a for the treatment of headache in service members with a history of mild traumatic brain injury: a cohort study. Headache, 55: (3), 395–406. doi: 10.1111/head.12495 |
[124] | Yorns, W. R Jr , Hardison, H. H. ((2013) ). Mitochondrial dysfunction in migraine. Semin Pediatr Neurol, 20: (3), 188–193. doi: 10.1016/j.spen.2013.09.002 |
[125] | Zafonte, R. D , Horn, L. J. ((1999) ). Clinical assessment of posttraumatic headaches. J Head Trauma Rehabil, 14: (1), 22–33. doi: 10.1097/00001199-199902000-00005 |
[126] | Zaloshnja, E , Miller, T , Langlois, J. A , Selassie, A. W. ((2008) ). Prevalence of long-term disability from traumatic brain injury in the civilian population of the United States, 2005. J Head Trauma Rehabil, 23: (6)394–400. doi: 10.1097/01.HTR.0000341435.52004.ac |
[127] | Zaremski, J. L , Herman, D. C , Clugston, J. R , Hurley, R. W , Ahn, A. H. ((2015) ). Occipital neuralgia as a sequela of sports concussion: a case series and review of the literature. Curr Sports Med Rep, 14: (1), 16–19. doi: 10.1249/JSR.0000000000000121 |
[128] | Zasler, N. D. ((1999) ). Posttraumatic tension pneumocephalus. J Head Trauma Rehabil,, 14: (1), 81–84. doi: 10.1097/00001199-199902000-00009 |
[129] | Zasler, N.D. ((2015) ). Sports Concussion Headache. Brain Injury, 29: (2), 207–220. doi: 10.3109/02699052.2014.965213 |
[130] | Zasler, N.D , Pain management in persons with traumatic brain injury. (2021). In: F. Zollman (3rd Ed.). Management of Traumatic Brain Injury. Demos Medical. New York. |
[131] | Zasler, N. D , Etheredge, S. ((2020) ). Post-concussive headache. In: B Eapen and D Cifu (Eds.). Concussion: Assessment, management and rehabilitation. Elsevier. New York, New York. Pgs. 59-75. |
[132] | Zasler, N , Haider, M.N , Grzibowski, N.R , Leddy, J.J. ((2019) ). Physician medical assessment in a multidisciplinary concussion clinic. JHTR, 34: (6), 409–418. doi: 10.1097/HTR.0000000000000524 |
[133] | Zasler, N.D , Leddy, J.J , Etheredge, S , Martelli, M.F. ((2019) ). Post-traumatic headache. In: J.M. Silver, T.W. McAllister, D. Arciniegas (Eds.): “Textbook of Traumatic Brain Injury”, 3rd Edition. American Psychiatric Publishing, Inc. 471-490. |
[134] | Zasler, N.D , Martelli, M.F , Jordan, B.D. ((2019) ). Civilian post-concussive headache. In: Textbook of Concussion and Traumatic Encephalopathy. Editors JVictoroff, E. Bigler. Cambridge University Press. Cambridge. Pgs. 728-742. |




