Anxiety, depression, and quality of life among subgroups of individuals with acquired brain injury: The role of anxiety sensitivity and experiential avoidance
Abstract
OBJECTIVES:
The objectives of this observational cohort study were to 1) cluster individuals with acquired brain injury (ABI) into subgroups according to their level of anxiety sensitivity (AS) and experiential avoidance (EA), and 2) compare subgroups with respect to anxiety, depression, and quality of life (QoL).
METHODS:
Individuals were recruited from an ABI outpatient clinic in Ontario, Canada and completed comprehensive psychosocial questionnaires. A two-step cluster analysis was performed to identify unique subgroups based on the clustering variables Anxiety Sensitivity Index (ASI) and Acceptance and Action Questionnaire (AAQ) which measure AS and EA, respectively. Clinical outcome measures were compared between clusters using multivariate analysis of variance: Generalized Anxiety Disorder 7 item (anxiety); Patient Health Questionnaire-9 (depression), and EQ-5D overall health item (QoL).
RESULTS:
Among 86 participants included for analysis (mean age 47.1±14.2 years, 54.7% female), three unique clusters were produced. ASI and AAQ were significantly different among all groups (p < 0.001). Cluster 1 (n = 26) had the lowest levels of AS and EA whereas Cluster 3 (n = 24) had the highest levels of AS and EA; Cluster 2 (n = 36) had moderate levels of AS and EA. There was no significant difference between groups in age, gender, time since injury, or Glasgow Coma Scale scores. Cluster 3 had significantly higher anxiety and depression scores than Cluster 1 and 2 (p < 0.001 for all). Further, Cluster 2 had significantly higher anxiety and depression scores than Cluster 1 (p < 0.001 for all). There was no significant difference in EQ-5D scores between Clusters 1 and 2 or Cluster 2 and 3; however, Cluster 3 scored significantly lower on EQ-5D than Cluster 1 (p = 0.032).
CONCLUSIONS:
There exists a subgroup of individuals with ABI that have high levels of AS and EA; this was associated with greater symptoms of anxiety and depression, and poorer QoL. Interventions to address AS and EA may improve mood and QoL in this population.
1Introduction
Acquired brain injury (ABI) consists of both traumatic and non-traumatic aetiologies, with traumatic being more common. In the United States alone, approximately 1.7 million people sustain a traumatic brain injury (TBI) each year (Faul, Xu, Wald, & VG, 2010). Regardless of injury severity, post injury distress is common, with many individuals experiencing both anxiety and depressive symptoms. Within the first year of a TBI, pooled prevalence rates of anxiety and depressive disorders were 21% and 17%, respectively (Scholten et al., 2016). Over the long term, these rates remained high for both anxiety (36%) and depression (43% (Scholten et al., 2016)). Treatment of these mood disorders is vitally important as they can have long-lasting effects on both quality of life (QoL) and subjective cognitive status up to 10 years post injury (Grauwmeijer et al., 2018).
Stress and allostatic load, a concept referring to the long-lasting effects of persistently activated stress reactions, (McEwen, 1998; Silverberg, Panenka, & Iverson, 2018) have been linked to the development of depression post TBI. Overexposure to mediators of neural, endocrine, and immune stress negatively impacts organ systems leading to disease (McEwen, 1998). In a mild-moderate TBI population, Bay et al. (2008) reported that significant risk factors for depression included perceived stress, pain, and involvement in litigation; these factors explained 70% of the variance of depressive symptoms (84% sensitivity and 69% specificity). In other studies, 54% of the variance in depressive symptoms was explained by post-injury stress alone (E. Bay, Hagerty, Williams, Kirsch, & Gillespie, 2002; Esther Bay, Kirsch, & Gillespie, 2004).
To reduce one’s allostatic load and potential for depression, consideration needs to be paid, in part, to coping behaviour which is linked to personality traits. High levels of self-reported depression and anxiety has been predicted by non-productive coping (Spitz, Schonberger, & Ponsford, 2013). Maladaptive personality traits such as anxiety sensitivity (AS) and experiential avoidance (EA) are just two ways an individual may cope behaviourally with stress from or as a result of depression and TBI. The relationship between AS and depression has been studied among several chronic medical populations. AS is the fear of both anxiety and anxiety-related sensations (Reiss & McNally, 1985). AS is considered to be a fairly stable dispositional variable which may contribute to avoidant behaviour, anxiety disorders, and fear of learning (Reiss, Peterson, Gursky, & McNally, 1986). AS has been deconstructed into three dimensions: 1) physical concerns (i.e., fear of physiological responses); 2) cognitive concerns (i.e., fear of cognitive dyscontrol), and 3) social concerns (i.e., fear of publicly observable symptoms of anxiety (Taylor et al., 2007)). Saulnier et al. (2018) have found that AS cognitive concerns are associated with depression, more so than the other dimensions of AS. Individuals who have AS may respond to stressful situations by exhibiting avoidant behaviour. EA is an attempt to avoid unwanted emotions, thoughts, bodily sensations and feelings (Steven C. Hayes, Wilson, Gifford, Follette, & Strosahl, 1996). EA has been associated with rumination, worry, and neuroticism, which are also associated with depression (Spinhoven, Drost, de Rooij, van Hemert, & Penninx, 2016). While EA has been described as a consequence of anxiety-related pathology, it also encompasses a vulnerability to it (Kashdan, Barrios, Forsyth, & Steger, 2006). Silverberg et al. (2018) examined the use of avoidance behaviour among a mild TBI population. Whether the behaviour stemmed from a fear of experiencing post-concussion symptoms or fear of consequences/inability to resume pre-injury activities, the use of such behaviour was found to increase the risk of chronic symptoms, disability, and adverse mental health outcomes (Silverberg et al., 2018).
EA and AS have not been well-studied with respect to QoL in an ABI population. Over the long-term, one study found that approximately 25% of individuals with severe TBI had low health-related QoL (Maillard, De Pretto, Delhumeau, & Walder, 2019). Maillard et al. (2019) found less stable working situations and lower Glasgow Coma Scale (GCS) scores were predictors of long-term low health-related QoL; other risk factors reported in the literature include age, gender, education level pre-injury, comorbidity, length of stay in hospital, pain, depression, anxiety, and functional impairment. The research gap examining the relationship between personality traits and QoL should be addressed. Furthermore, while studies have examined the role of AS and EA on mood, disability, and pain in several clinical populations; (Mehta, Rice, Janzen, Pope, et al., 2016; Mehta, Rice, Janzen, Serrato, et al., 2016) little research has been conducted exploring AS and EA specifically within a ABI population. Therefore, the objectives of this study were to 1) cluster individuals with ABI into subgroups according to their level of AS and EA, and 2) compare subgroups with respect to anxiety, depression, and QoL.
2Methods
This observational cohort study is reported in adherence to the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) guidelines (See https://www.strobe-statement.org/fileadmin/Strobe/uploads/checklists/STROBE_checklist_v4_cohort.pdf).
2.1Participants
Participants were recruited from an ABI outpatient clinic in London, Ontario; no restrictions were placed on sample size and ongoing recruitment continued from 2016 until 2018. Individuals were given a letter of information and referred to the study by their physician at the end of the clinic visit. For individuals who expressed interest, the research assistant reviewed the letter of information in detail and answered questions. Informed consent was obtained from willing participants. Participants were included in the study if they met the following inclusion criteria: 1) diagnosis of an ABI; 2) at least 18 years of age; and 3) able to read and write in English. Individuals were not excluded based on previous neurological or psychiatric history, history of substance use or learning disabilities; however, if a patient could not provide consent they were not included in the study. Since individuals were required to complete self report questionnaires, those who were unable to read and write in English were excluded.
In total, 89 individuals were recruited to the study; all but three individuals completed the study booklets and were included for analysis (N = 86); the three individuals who did not complete the study booklets did not indicate why they no longer wanted to participate in the study. The sample had a mean age of 47.1±14.2 years and was comprised of a slightly greater number of females (54.7%). Individuals had a mean Glasgow Coma Scale score of 13.1±3.4 and were 3.5±4.4 years post injury.
2.2Procedure
Individuals completed the Patient Health Questionnaire-9 (PHQ-9) while still in clinic to ensure the item on suicidality could be reviewed by the research assistant immediately. Individuals were then given a booklet consisting of a comprehensive set of self-report questionnaires, which they were asked to complete on their own. The questionnaires included: Anxiety Sensitivity Index (ASI), Acceptance to Action Questionnaire (AAQ), Generalized Anxiety Disorder 7-item (GAD-7), and EQ-5D. Additional sociodemographic and clinical health information was also collected (e.g., age, gender, Glasgow Coma Scale score, time post injury). Individuals were asked to complete the booklet within the next two weeks and return it using the self-addressed, stamped, return envelope. Those who did not return the booklet received a telephone reminder. Once data was returned to the research site, data was entered into a standardized SPSS file. All procedures were approved by the Western University Health Sciences Ethics Review Board.
2.3Cluster variable measures
2.3.1Anxiety Sensitivity Index
The ASI is a 16-item self report questionnaire, which evaluates AS (Peterson & Reiss, 1992). Anxiety sensitivity is defined as the fear of anxiety-related sensations or behaviours (i.e. fear of fear (Deacon, Abramowitz, Woods, & Tolin, 2003)). Three factors of anxiety-related symptoms are measured: (1) fear of somatic symptoms of anxiety, (2) fear of mental incapacitation, and (3) fear of negative social repercussions of anxiety (Zinbarg, Barlow, & Brown, 1997). Each item is rated on a five-point Likert scale ranging from 0 (very little) to 4 (very much). High ASI scores are associated with the development of panic attacks (Arnau, Broman-Fulks, Green, & Berman, 2009). While not yet studied in the ABI population, the psychometric properties and predictive validity of this measure have been well established in the general population (Peterson & Reiss, 1992; Rodriguez, Bruce, Pagano, Spencer, & Keller, 2004).
2.3.2Acceptance and Action Questionnaire
The AAQ is a nine-item self report questionnaire, which assesses psychological inflexibility (EA (Bond et al., 2011)). Psychological inflexibility is defined as altering one’s physiological sensations, emotions or feelings, even when doing so leads to actions that are inconsistent with one’s values or goals (e.g., avoiding pursing a long term goal due to anxiety (Bond et al., 2011)). Each item is rated on a seven-point scale ranging from 1 (never true) to 7 (always true). High AAQ scores are associated with a wide range of negative behavioural and physical health outcomes, including increased avoidance and immobility, while low scores reflect acceptance (Steven C. Hayes et al., 2004). While it as yet to be studied specifically in ABI, the AAQ is reported as a reliable and valid measure in the general population (Bond et al., 2011).
2.4Outcome measures
2.4.1Generalized Anxiety Disorder 7-item
The GAD-7 is a seven-item self report questionnaire which screens for, and determines, the severity of generalized anxiety disorder (GAD) symptoms (Spitzer, Kroenke, Williams, & Löwe, 2006). Each item is rated on a four-point scale ranging from 0 (not at all) to 3 (nearly every day). Anxiety severity is determined over the last two weeks and total scores range from 0 to 21, with a score of 5, 10, or 15 indicating mild, moderate, or severe anxiety, respectively (Spitzer et al., 2006). The GAD-7 has not been validated in ABI; however, it is established as a valid and reliable measure for assessing GAD symptoms in the general population (Ruiz et al., 2011; Spitzer et al., 2006).
2.4.2Patient Health Questionnaire 9-item
The PHQ-9 is a nine-item self report questionnaire commonly used to assess depression symptoms (Kroenke, Spitzer, & Williams, 2001). Each item is rated on a four-point scale ranging from 0 (not at all) to 3 (nearly every day (Kroenke et al., 2001)). The measure involves recalling depression symptoms over the last two weeks and results in a total score ranging from 0 to 27, with a score of 5, 10, 15, or 20 indicating mild, moderate, moderately severe, or severe depression, respectively (Kroenke et al., 2001). The PHQ9 has demonstrated a high level of clinical utility as a reliable and valid means of screening for, and assessing depression within TBI populations’ (Donders & Pendery, 2017; Fann et al., 2005).
2.4.3EQ-5D
The EQ-5D is a five-item self report questionnaire and visual analogue scale which assesses health status and QoL (The EuroQol Group, 1990). The questionnaire evaluates five dimensions of health status including: (1) mobility, (2) self-care, (3) usual activities, (4) pain/discomfort, and (5) anxiety/depression (The EuroQol Group, 1990). Each dimension has five response levels: no problems, slight problems, moderate problems, severe problems, or unable to/extreme problems (The EuroQol Group, 1990). In addition, a quantitative measure of the respondent’s self rated health is reported on a vertical visual analogue scale from 0 to 100, where 0 is “The worst health you can imagine” and 100 is “The best health you can imagine” (The EuroQol Group, 1990). High scores suggest that a respondent’s subjective health status is good, while low scores suggest they see their health as being poor. In addition to the general population, the psychometric properties of this measure have been established for TBI (Geraerds et al., 2019; The EuroQol Group, 1990).
2.5Data analysis
Descriptive analyses were conducted to present demographic characteristics of the sample population through means with standard deviations and frequencies. A two-step cluster analysis was performed in order to identify groups with common properties based on personality traits. This method was chosen to maximize flexibility in determining the most appropriate number of groups. The hierarchical approach identifies the optimal number of clusters by maximizing differences between groups and minimizing differences within groups, with respect to the clustering variables, ASI (AS) and AAQ (EA (Zhang, 1996)).
After categorizing by cluster membership, differences in demographic characteristics and outcome measures (i.e., GAD-7, PHQ-9, and EQ-5D) were compared using multivariate analysis of variance. Post hoc analyses were conducted with a Bonferroni correction to compare anxiety, depression, and QoL between clusters. Analyses were performed using SPSS version 23.0 (Chicago, IL, USA) and were two-tailed; significance was set at 0.05.
3Results
The two-step cluster analysis sorted participants into three clusters based on levels of AS and EA. The AAQ and ASI were significantly different between the three clusters (p < 0.001). Cluster 1 (n = 26) had the lowest levels of both AS and EA, both falling below the sample means for ASI and AAQ, respectively; these individuals could be characterized as effective and adaptive copers. Cluster 2 (n = 36) had moderate levels of AS and EA; while the cluster’s mean ASI scores were below the overall sample, AAQ scores were approximately the same as the overall sample. This group may be described as those with average coping. Cluster 3 (n = 24) had the highest scores for ASI and AAQ, both scoring above the sample mean. They constitute a subgroup of highly avoidant individuals with high AS. Demographic and clustering variable characteristics are reported in Table 1; there was no significant difference between clusters in age, gender, time since injury, or Glasgow Coma Scale scores.
Table 1
Mean values (standard deviation) of demographic and clinical characteristics of overall sample and subdivided into the three clusters
| Overall | Cluster 1 | Cluster 2 | Cluster 3 | p | |
| (N = 86) | (N = 26) | (N = 36) | (N = 24) | ||
| Mean age (SD) | 47.1 (14.2) | 50.1 (13.5) | 44.6 (14.1) | 47.6 (15.1) | 0.320 |
| N females (%) | 47 (54.7%) | 11 (42.3%) | 19 (52.8%) | 17 (70.8%) | 0.126 |
| Mean time since injury (SD) | 3.5 (4.4) | 3.9 (6.5) | 3.1 (2.9) | 3.8 (3.3) | 0.731 |
| Mean GCS (SD; N) | 13.1 (3.4; N = 30) | 12.8 (4.0) | 12.6 (3.9) | 14.4 (0.9) | 0.496 |
| Mean ASI (SD) | 24.7 (13.6) | 12.1 (6.1) | 22.6 (7.9) | 41.5 (8.0) | <0.001 |
| Mean AAQ (SD) | 24.2 (12.6) | 10.7 (4.0) | 24.3 (6.8) | 39.0 (12.6) | <0.001 |
*Note: AAQ = Acceptance and Action Questionnaire; ASI = Anxiety Sensitivity Index; GCS = Glasgow Coma Scale.
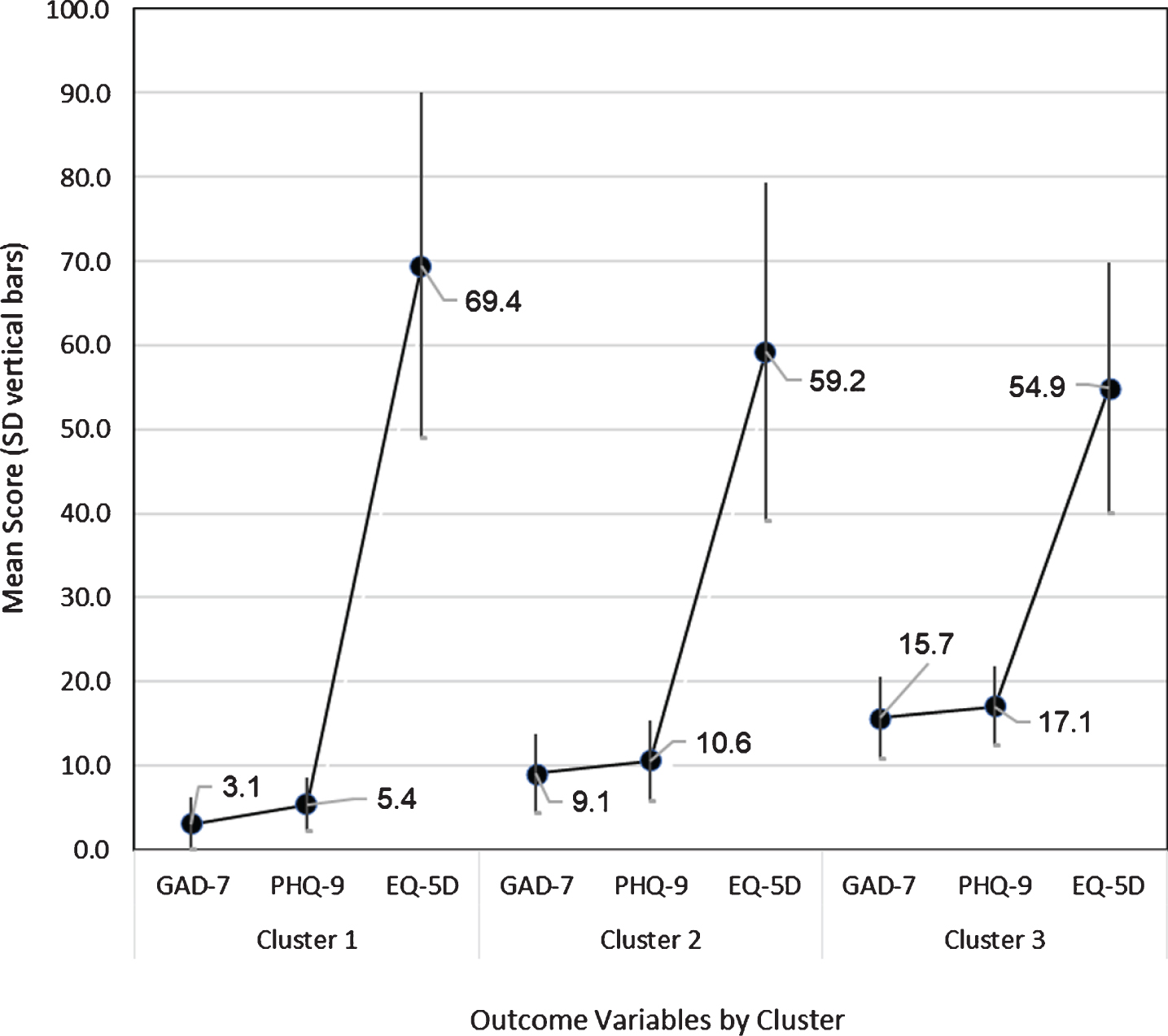
As shown in Table 2 and Fig. 1, when comparing between the three clusters, there was a significant main effect (between clusters) for GAD-7(F (2, 78) = 46.85, p < 0.001), PHQ-9 (F (2, 74) = 40.89, p < 0.001), and EQ-5D (F (2, 79) = 3.68, p < 0.030). Post hoc analysis demonstrated a number of significant differences among the clusters on anxiety, depression, and QoL (Fig. 2). Cluster 3 (those with high AS and EA) scored significantly higher than Clusters 2 (moderate AS and EA) and 1 (low AS and EA) on both the GAD-7 (p < 0.001 for both), and PHQ-9 (p < 0.001 for both). Additionally, Cluster 2 scored significantly higher than Cluster 1 on both the GAD-7 (p < 0.001), and PHQ-9 (p < 0.001). There was no significant difference in EQ-5D between Clusters 1 and 2 (p = 0.140) or Cluster 2 and 3 (p = 1.000); however, Cluster 3 scored significantly lower on EQ-5D than Cluster 1 (p = 0.032).
Table 2
Mean values (standard deviation) in anxiety, depression, and quality of life of overall sample and subdivided into the three clusters
| Overall | Cluster 1 | Cluster 2 | Cluster 3 | F | p | |
| (N = 86) | (N = 26) | (N = 36) | (N = 24) | |||
| GAD-7 | 9.3 (6.4) | 3.1 (3.2) | 9.1 (4.7) | 15.7 (4.9) | 46.85 | <0.001 |
| PHQ-9 | 10.8 (6.2) | 5.4 (3.2) | 10.6 (4.8) | 17.1 (4.7) | 40.89 | <0.001 |
| EQ-5D | 61.0 (19.6) | 69.4 (20.6) | 59.2 (20.1) | 54.9 (15.0) | 3.68 | 0.030 |
*Note: GAD-7 = General Anxiety Disorder 7-item; PHQ-9 = Patient Health Questionnaire 9-item.
Fig. 1
Two-step cluster subgroups with mean score and standard deviation (y-axis) for clustering variables (x-axis). Note: AAQ = Acceptance and Action Questionnaire; ASI = Anxiety Sensitivity Index.
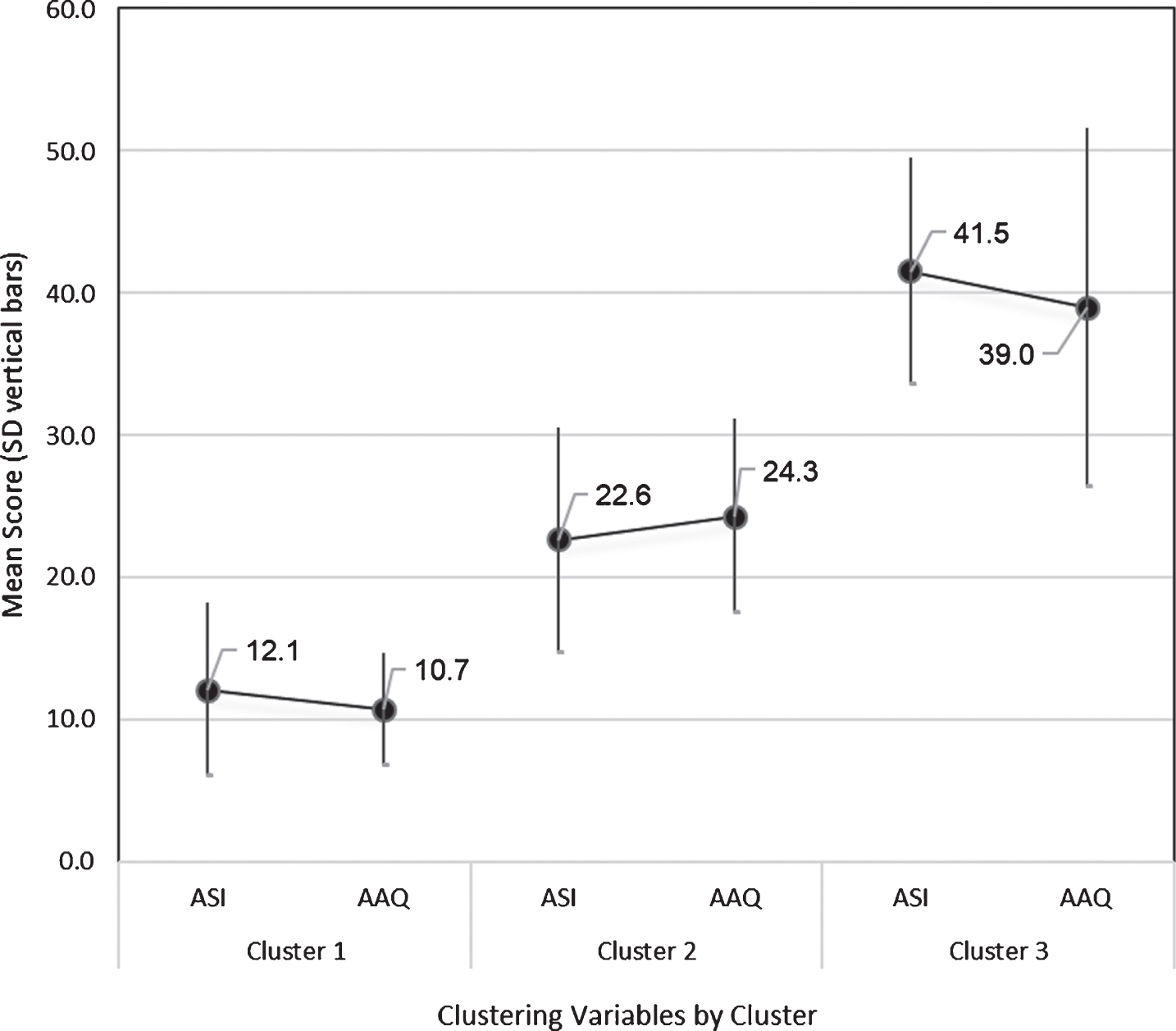
Fig. 2
Two-step cluster subgroups with mean score and standard deviation (y-axis) for outcome variables (x-axis). Note: GAD-7 = Generalized Anxiety Disorder 7-item; PHQ-9 = Patient Health Questionnaire 9 item.
4Discussion
In the present study we identified three meaningful subgroups of individuals with an ABI based on their levels of AS and EA. The presence of depression and anxiety symptoms significantly differed between the three clusters; those that reported increasingly higher symptoms of anxiety and depressive symptoms also scored higher on AS and EA (Cluster 3). QoL was also reported as being substantially lower among individuals with the highest AS and EA as compared to those reporting the least (Cluster 1). These findings align with the allostatic load stress theory (Juster, McEwen, & Lupien, 2010) of which AS and EA are both factors that can contribute to stress, subsequently increasing allostatic load (E. Bay & Donders, 2008).
Our findings demonstrate that among individuals with ABI, those that report increased trait-like characteristics of AS and EA constitute a subgroup of individuals with poorer mood and QoL while coping during rehabilitation. Importantly, the subgroup of individuals reporting the greatest AS and EA included almost 25% of our sample and reported symptoms above the thresholds for moderate anxiety and moderately-severe depressive symptoms. A second subgroup (Cluster 2) also reported mild anxiety symptoms and moderate depressive symptoms. The remaining subgroup (Cluster 1) reported anxiety within normal range and mild depressive symptoms. Individuals in clusters 2 and 3 (highest AS and EA) accounted for 60% of our study sample. This highlights the presence of significant distress among individuals who have experienced ABI and the role that certain personality-trait characteristics has on that distress and coping. Dysregulated stress networks post ABI have been found to decrease the physiological mechanisms in place to manage daily stress, which may account for the considerable portion of individuals reporting traits known to negatively impact coping (E. Bay & Donders, 2008). Findings from Bay and Donders (2008) showed that heightened reports of perceived stress have previously explained a substantial amount of variance in depressive symptoms among individuals who have experienced a TBI; this aligns with the findings of our study. Comparatively, individuals in Cluster 1 who reported substantially less fear of anxiety and psychological inflexibility may represent those with more adaptive coping mechanisms in place, resulting in decreased reports of stress and associated mental distress.
This study is the first to examine subgroups of individuals with ABI based on personality traits in relation to QoL. These findings can be compared to studies conducted in individuals with other chronic health conditions such as rheumatoid arthritis; (Mehta, Rice, Janzen, Pope, et al., 2016; Rice et al., 2016) and chronic pain (Mehta, Rice, Janzen, Serrato, et al., 2016). Dispositional traits such as AS and EA, resulted in significantly greater depressive and anxiety symptoms with fewer differences between subgroups on QoL (Mehta, Rice, Janzen, Pope, et al., 2016; Rice et al., 2016). In our study, the proportion of individuals having at least moderate depressive symptoms were higher than those observed in rheumatoid arthritis (Mehta, Rice, Janzen, Pope, et al., 2016; Rice et al., 2016) and chronic pain populations (Mehta, Rice, Janzen, Serrato, et al., 2016). Rice et al. (2016) reported that the majority of individuals’ anxiety and depressive symptoms were within normative ranges. In comparison, our study found that 60% of the sample had at least moderate symptoms of depression and mild symptoms of anxiety. Reports of mental health among these subgroups should be considered within the context of overall recovery, whereby increased depression hinders recovery after brain injury (Jorge et al., 2004). A longitudinal analysis among individuals with chronic pain found that those with higher levels of maladaptive traits reported higher levels of distress, as well as greater long-term disability, as compared to those reporting fewer maladaptive traits (Mehta, Rice, Janzen, Pope, et al., 2016). This demonstrates the multifaceted nature of recovery and the impact that allostatic load can have on physical and psychological well-being. In addition to understanding the effect of maladaptive traits, it is also important to examine how specific characteristics of those with effective coping, a high QoL, and overall mood may facilitate improved well-being post brain injury.
Increased allostatic load negatively influences one’s adaptive coping skills after an ABI and results in a series of physical, emotional, and interpersonal difficulties (E. Bay et al., 2002). The role of stress, more generally, has been considered among individuals with brain injuries; however, to our knowledge this is the first study to consider the specific components of stress that can be targeted during rehabilitation employing a more holistic and personalized approach. Addressing maladaptive traits such as AS and psychological inflexibility can allow for the delivery of tailored psychosocial interventions. Psychosocial interventions focused on stress management exist and are commonly applied among individuals that have experienced a brain injury (Arundine et al., 2012). Teaching patients Dialectic Behavior Therapy skills such as progressive relaxation, distraction, and self-soothing can help reduce immediate distress by decreasing their fight or flight responses. Mindfulness breathing and/or imagery can help patients learn to acknowledge and accept their maladaptive thoughts without judging or avoiding them. Formalized interventions such as Acceptance and Commitment Therapy (ACT) which aim to increase individuals’ ability to manage stress through increasing flexibility, to allow fear and anxiety to occur without attempting to avoid or change this experience (Hayes, Strosahl, & Wilson, 1999) are important for long term management and behavioural change. Studying the effectiveness of ACT among individuals after ABI has been described as an important area of study for future research (Kangas & McDonald, 2011). Preliminary findings of ACT among pilot studies of individuals with TBI have been promising (Whiting, Deane, McLeod, Ciarrochi, & Simpson, 2019). Providing individuals with heightened distress the appropriate referrals and interventions to address the psychosocial aspects of rehabilitation is an important component in ensuring a person-centred approach is taken for those with brain injury.
This study should be interpreted within the context of relevant limitations. The cross-sectional study design does not allow for cause and effect to be inferred. Additionally, since this study was conducted at a single outpatient clinic within an urban rehabilitation hospital, it may not be generalizable to all individuals with brain injury. While mean time since injury did not significantly differ between clusters, future studies should recruit and follow-up with individuals at more focused time periods. This could provide important implications for rehabilitation based on a specific stage of recovery. A further consideration is the overlap between somatic symptoms on mental health measures and deficits that can occur due to brain injury. For example, the PHQ-9 includes questions about sleeping, concentration, and memory, all of which can be impacted by a brain injury. This would not be expected to differ between identified subgroups but could be a result of an over-representation of ABI sequelae on the PHQ-9. Despite these limitations, this study provides important information that should be considered in the rehabilitation of individuals with brain injury.
In conclusion, this study demonstrated that there exist subgroups of individuals with brain injury based on trait-like characteristics and that significant differences can be observed with respect to mood and QoL. Understanding the influence of AS and EA may allow for better management of mood symptoms and the facilitation of education related to healthy coping in the context of ABI. Addressing avoidant patterns in behaviour through modestly resource-intensive and easily accessible interventions may provide an important set of skills to individuals with brain injury struggling with depression and anxiety symptoms and a reduced QoL.
Conflict of interest
None to report.
Funding
As Vanier Scholars, Amanda McIntyre and Danielle Rice are supported by the Government of Canada, Vanier Canada Graduate Scholarships. The project was funded by St. Josephs Health Care Foundation, London, Ontario. Neither funding source had a role in this study.
Acknowledgments
We would like to gratefully acknowledge Danielle Vanderlaan and Mitch Longval for their assistance in recruiting participants and data entry.
References
1 | Arnau, R. C , Broman-Fulks, J. J , Green, B. A , & Berman, M. E. ((2009) ). The anxiety sensitivity index—revised: confirmatory factor analyses, structural invariance in Caucasian and African American samples, and score reliability and validity. Assessment 16: (2), 165–180. |
2 | Arundine, A , Bradbury, C. L , Dupuis, K , Dawson, D. R , Ruttan, L. A , & Green, R. E. ((2012) ). Cognitive behavior therapy after acquired brain injury: maintenance of therapeutic benefits at 6 months posttreatment. J Head Trauma Rehabil 27: (2), 104–112. doi: 10.1097/HTR.0b013e3182125591. |
3 | Bay, E , & Donders, J. ((2008) ). Risk factors for depressive symptoms after mild-to-moderate traumatic brain injury. Brain Inj 22: (3), 233–241. doi: 10.1080/02699050801953073. |
4 | Bay, E , Hagerty, B. M , Williams, R. A , Kirsch, N , & Gillespie, B. ((2002) ). Chronic stress, sense of belonging, and depression among survivors of traumatic brain injury. J Nurs Scholarsh 34: (3), 221–226. |
5 | Bay, E , Kirsch, N , & Gillespie, B. ((2004) ). Chronic stress conditions do explain posttraumatic brain injury depression. Research and Theory for Nursing Practice: An International Journal, 18: (2-3), 213–228. Retrieved from http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=psyc4&AN=2004-20308-009 |
6 | |
7 | Bond, F. W , Hayes, S. C , Baer, R. A , Carpenter, K. M , Guenole, N , Orcutt, H. K ,... & Zettle, R. D. ((2011) ). Preliminary psychometric properties of the Acceptance and Action Questionnaire–II: A revised measure of psychological inflexibility and experiential avoidance. Behavior Therapy 42: (4), 676–688. |
8 | Deacon, B. J , Abramowitz, J. S , Woods, C. M , & Tolin, D. F. ((2003) ). The Anxiety Sensitivity Index-Revised: psychometric properties and factor structure in two nonclinical samples. Behav Res Ther 41: (12), 1427–1449. |
9 | Donders, J , & Pendery, A. ((2017) ). Clinical utility of the Patient Health Questionnaire-9 in the assessment of major depression after broad-spectrum traumatic brain injury. Archives of Physical Medicine and Rehabilitation 98: (12), 2514–2519. |
10 | Fann, J. R , Bombardier, C. H , Dikmen, S , Esselman, P , Warms, C. A , Pelzer, E ,... & Temkin, N. ((2005) ). Validity of the Patient Health Questionnaire-9 in assessing depression following traumatic brain injury. J Head Trauma Rehabil 20: (6), 501–511. |
11 | Faul M , Xu L , Wald, M. M , VG, C. ((2010) ). Traumatic Brain Injury in the United States: Emergency Department Visits, Hospitalizations and Deaths 2002-2006. Atlanta, GA: National Center for Injury Prevention and Control. |
12 | Geraerds, A , Bonsel, G. J , Janssen, M. F , de Jongh, M , Spronk, I , Polinder, S , & Haagsma, J. A. ((2019) ). The added value of the EQ-5D with a cognition dimension in injury patients with and without traumatic brain injury. Quality of Life Research 28: (7), 1931–1939. |
13 | Grauwmeijer, E , Heijenbrok-Kal, M. H , Peppel, L. D , Hartjes, C. J , Haitsma, I. K , de Koning, I , & Ribbers, G. M. ((2018) ). Cognition, Health-Related Quality of Life, and Depression Ten Years after Moderate to Severe Traumatic Brain Injury: A Prospective Cohort Study. J Neurotrauma 35: (13), 1543–1551. doi: 10.1089/neu.2017.5404. |
14 | Hayes, S. C , Strosahl, K , Wilson, K. G , Bissett, R. T , Pistorello, J , Toarmino, D ,... & Bergan, J. ((2004) ). Measuring experiential avoidance: A preliminary test of a working model. The Psychological Record 54: (4), 553–578. |
15 | Hayes, S. C , Strosahl, K. D , & Wilson, K. G. ((1999) ). Acceptance and Commitment Therapy: An Experiential Approach to Behavior Change. New York, NY: Guilford Press. |
16 | Hayes, S. C , Wilson, K. G , Gifford, E. V , Follette, V. M , & Strosahl, K. ((1996) ). Experiential avoidance and behavioral disorders: A functional dimensional approach to diagnosis and treatment. Journal of Consulting and Clinical Psychology 64: (6), 1152–1168. |
17 | Jorge, R. E , Robinson, R. G , Moser, D , Tateno, A , Crespo-Facorro, B , & Arndt, S. ((2004) ). Major depression following traumatic brain injury. Arch Gen Psychiatry 61: (1), 42–50. doi: 10.1001/archpsyc.61.1.42. |
18 | Juster, R. P , McEwen, B. S , & Lupien, S. J. ((2010) ). Allostatic load biomarkers of chronic stress and impact on health and cognition. Neurosci Biobehav Rev 35: (1), 2–16. doi: 10.1016/j.neubiorev.2009.10.002. |
19 | Kangas, M , & McDonald, S. ((2011) ). Is it time to act? The potential of acceptance and commitment therapy for psychological problems following acquired brain injury. Neuropsychol Rehabil 21: (2), 250–276. doi: 10.1080/09602011.2010.540920. |
20 | Kashdan, T. B , Barrios, V , Forsyth, J. P , & Steger, M. F. ((2006) ). Experiential avoidance as a generalized psychological vulnerability: Comparisons with coping and emotion regulation strategies. Behav Res Ther 44: (9), 1301–1320. |
21 | Kroenke, K , Spitzer, R. L , & Williams, J. B. ((2001) ). The PHQ-9: validity of a brief depression severity measure. Journal of General Internal Medicine 16: (9), 606–613. |
22 | Maillard, J , De Pretto, M , Delhumeau, C , & Walder, B. ((2019) ). Prediction of long-term quality of life after severe traumatic brain injury based on variables at hospital admission. Brain Inj, 1-10. doi:10.1080/02699052.2019.1683227 |
23 | McEwen, B. S. ((1998) ). Protective and damaging effects of stress mediators. N Engl J Med 338: (3), 171–179. doi: 10.1056/nejm199801153380307. |
24 | Mehta, S , Rice, D , Janzen, S , Pope, J. E , Harth, M , Shapiro, A. P , & Teasell, R. W. ((2016) ). Mood, Disability, and Quality of Life among a Subgroup of Rheumatoid Arthritis Individuals with Experiential Avoidance and Anxiety Sensitivity. Pain Res Manag 2016: , 7241856. doi: 10.1155/2016/7241856. |
25 | Mehta, S , Rice, D , Janzen, S , Serrato, J , Getty, H , Shapiro, A ,... & Teasell, R. ((2016) ). The long term role of anxiety sensitivity and experiential avoidance on pain intensity, mood, and disability among individuals in a specialist pain clinic. Pain Research & Management, 2016, 2016, ArtID 6954896, 2016. |
26 | Peterson, R , & Reiss, S. ((1992) ). Anxiety Sensitivity Index: Lawrence Erlbaum Associates. |
27 | Reiss, S , & McNally, R. ((1985) ). Expectancy model of fear. In Reiss S & Bootzin R. R. (Eds.), Theoretical Issues in Behavior Therapy Inside. San Diego, California, USA: Academic Press. |
28 | Reiss, S , Peterson, R. A , Gursky, D. M , & McNally, R. J. ((1986) ). Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behav Res Ther 24: (1), 1–8. doi: 10.1016/0005-7967(86)90143-9. |
29 | Rice, D. B , Mehta, S , Pope, J. E , Harth, M , Shapiro, A , & Teasell, R. W. ((2016) ). Dispositional Affect in Unique Subgroups of Patients with Rheumatoid Arthritis. Pain Res Manag 2016: , 1024985. doi: 10.1155/2016/1024985. |
30 | Rodriguez, B. F , Bruce, S. E , Pagano, M. E , Spencer, M. A , & Keller, M. B. ((2004) ). Factor structure and stability of the Anxiety Sensitivity Index in a longitudinal study of anxiety disorder patients. Behav Res Ther 42: (1), 79–91. |
31 | Ruiz, M. A , Zamorano, E , García-Campayo, J , Pardo, A , Freire, O , & Rejas, J. ((2011) ). Validity of the GAD-7 scale as an outcome measure of disability in patients with generalized anxiety disorders in primary care. Journal of Affective Disorders 128: (3), 277–286. |
32 | Saulnier, K. G , Allan, N. P , Raines, A. M , & Schmidt, N. B. ((2018) ). Anxiety sensitivity cognitive concerns drive the relation between anxiety sensitivity and symptoms of depression. Cognitive Behaviour Therapy 47: (6), 495–507. |
33 | Scholten, A. C , Haagsma, J. A , Cnossen, M. C , Olff, M , van Beeck, E. F , & Polinder, S. ((2016) ). Prevalence of and Risk Factors for Anxiety and Depressive Disorders after Traumatic Brain Injury: A Systematic Review. J Neurotrauma 33: (22), 1969–1994. doi: 10.1089/neu.2015.4252. |
34 | Silverberg, N. D , Panenka, W. J , & Iverson, G. L. ((2018) ). Fear Avoidance and Clinical Outcomes from Mild Traumatic Brain Injury. J Neurotrauma 35: (16), 1864–1873. doi: 10.1089/neu.2018.5662. |
35 | Spinhoven, P , Drost, J , de Rooij, M , van Hemert, A. M , & Penninx, B. W. ((2016) ). Is experiential avoidance a mediating, moderating, independent, overlapping, or proxy risk factor in the onset, relapse and maintenance of depressive disorders? Cognitive Therapy and Research 40: (2), 150–163. |
36 | Spitz, G , Schonberger, M , & Ponsford, J. ((2013) ). The relations among cognitive impairment, coping style, and emotional adjustment following traumatic brain injury. J Head Trauma Rehabil 28: (2), 116–125. doi: 10.1097/HTR.0b013e3182452f4f. |
37 | Spitzer, R. L , Kroenke, K , Williams, J. B , & Löwe, B. ((2006) ). A brief measure for assessing generalized anxiety disorder: the GAD-. Arch Intern Med 166: (10), 1092–1097. |
38 | Taylor, S , Zvolensky, M. J , Cox, B. J , Deacon, B , Heimberg, R. G , Ledley, D. R ,... & Cardenas, S. J. ((2007) ). Robust Dimensions of Anxiety Sensitivity: Development and Initial Validation of the Anxiety Sensitivity Index-3. Psychological Assessment 19: (2), 176–188. doi: 10.1037/1040-3590.19.2.176. |
39 | The EuroQol Group ((1990) ). EuroQol-a new facility for the measurement of health-related quality of life. Health Policy 16: (3), 199–208. |
40 | Whiting, D , Deane, F , McLeod, H , Ciarrochi, J , & Simpson, G. ((2019) ). Can acceptance and commitment therapy facilitate psychological adjustment after a severe traumatic brain injury? A pilot randomized controlled trial. Neuropsychol Rehabil, 1-24. doi:10.1080/09602011.2019.1583582 |
41 | Zhang, T , Ramakrishnan, R , & Livny, M. ((1996) ). BIRCH: an efficient data clustering method for very large databases. Paper presented at the ACM SIGMOD Conference on Management of Data, Montreal, Canada. |
42 | Zinbarg, R. E , Barlow, D. H , & Brown, T. A. ((1997) ). Hierarchical structure and general factor saturation of the Anxiety Sensitivity Index: Evidence and implications. Psychological Assessment 9: (3), 277. |




