Spirituality and resilience among family caregivers of survivors of stroke: A scoping review
Abstract
BACKGROUND:
Stroke is the leading cause of disability in Australia and the third-leading cause of disability worldwide and a significant burden on caregivers.
OBJECTIVE:
To map the extent, range and nature of the literature investigating spirituality and resilience among family caregivers of survivors of stroke.
METHOD:
A scoping review.
RESULTS:
Six studies were identified, conducted in the United States, United Kingdom, China and Turkey. These included two quantitative, one experimental and three qualitative designs. No studies linked spirituality to resilience. For the qualitative studies, spirituality was the primary focus of one, and the secondary focus of two others. Qualitative data reflected the lived experience of caregivers drawing upon spirituality to help cope with the burden of caregiving. For the two quantitative studies, spirituality was measured as a secondary focus and showed no significant links between spirituality or adjustment in caregivers. The one experimental study comprised a psycho-educational intervention focused on building resilience, finding a significant increase in social support not reflected in a matched control group. Clinical implications suggested the need for strength-based interventions, including spiritual needs and religious beliefs of the family caregiver.
CONCLUSIONS:
Spirituality and resilience following stroke are essential factors in caregiver adjustment following stroke. Further research with a focus on causality and the link between spirituality, resilience and adjustment in this population is needed.
1Introduction
Stroke is a major contributor to the global burden of disease (Feigin, Lawes, Bennett, & Anderson, 2003; Mukherjee & Patil, 2011). In the Australian context, although stroke deaths have fallen by 74% since 1980, stroke remains the nation’s leading cause of disability accounting for 3% of the national burden of disease (Australian Institute of Health & Welfare, 2018). On an average day, 100 Australians experience a stroke, causing disability in 35% of cases (Australian Institute of Health & Welfare, 2018). The Australian Stroke Foundation (2017) forecasts the number of stroke survivors to double by 2050.
While caring for a stroke survivor can be rewarding, the time involved can affect the caregiver’s participation in the workforce and community, and their health (Hayley, Roth, Howard & Safford, 2010). Quality of life for caregivers can be reduced by changes in physical functioning of the relative with stroke (Adams 2003; Backstrom, Asplund & Sundin, 2010; Pucciarelli et al., 2017), resulting in high burden, anxiety and depressive symptoms (Jaracz et al., 2015; Kruithof et al., 2016). In some cases, caregiver depression exceeds the depression of the person with stroke (Han & Hayley, 1999; Berg et al., 2005).
On the other hand, coping and social support have been found to protect family caregivers from the negative impact of caregiving. Coping strategies are designed to modify the stressful circumstances and regulate the emotional distress connected to the situation (Penley, Tomake & Wiebe, 2002) and buffering theory proposes that social support serves as a defensive barrier against the negative effects of problems under conditions of high distress (Cohen & Wills, 1985). Concerning family caregivers after stroke, problem focused coping strategies and perceived high levels of social support contribute to a better quality of life and lower levels of depression and high mental wellbeing (Ali & Kausar, 2016; Cheng, Chair & Chau, 2018; Yu Hu, Efrid, & McCoy, 2013).
Another factor that could act as a protective factor or buffer against negative caregiver outcomes is spirituality (Walsh, 2003). Spirituality has been defined as a “unique and dynamic process” encompassing connectedness “with oneself, others, nature, or God” (Meraviglia, 1999) and “a universal and fundamental human quality involving the search for a sense of meaning, purpose, morality, well-being, and profundity in relationships with ourselves, others, and ultimate reality” (Canda & Furman, 2009, pp.59, 87). Spirituality is generally considered to be a much broader construct than religious faith, although the two concepts may overlap (Canda & Furman, 2009).
To the best of our knowledge, no reviews have been conducted of the literature around the role of spirituality among caregivers after stroke. At a theoretical level, Smith and colleagues (2012) have asserted that healthy spirituality can contribute to better health outcomes, and this is supported by reviews of patient studies across the general health literature (Koenig, 2012). In the field of neurologic insult, initial studies that investigated the applicability of this research to the lives of family caregivers (after spinal cord injury (SCI) or traumatic brain injury (TBI)), found that spirituality had a protective (inverse) association to negative affect, depression and burden, and a positive association with positive affect (Jones et al., 2019; Simpson et al., 2020). These results reflect findings from studies among people with SCI or TBI which have found a positive association between spirituality and better life satisfaction, quality of life, and positive mental health (Jones et al., 2016; Jones et al., 2018). Given these results, is there a similar relationship between spirituality and caregiver outcomes after stroke?
The theoretical work on spirituality has also highlighted the close links between spirituality and resilience, with many multi-dimensional definitions of resilience including spirituality (e.g., Walsh, 2003; Smith, Ortiz, Wiggind, Bernard, & Dalen, 2012; Richardson, 2002; White, Driver, & Warren, 2008). Resilience can be defined as “a dynamic process encompassing positive adaptation within the context of significant adversity” (Luthar, Cicchetti, & Becker, 2000, p. 543), and can also play an important role in mediating outcomes for family caregivers after neurologic insult (Anderson, Daher, & Simpson, 2019). Empirical evidence for the relationship between spirituality and resilience among caregivers has been found in two recent observational studies of family caregivers after SCI and TBI (Jones et al., 2019; Simpson et al., 2020). Therefore, the span of the proposed review was broadened to include resilience.
Given the lack of previous reviews examining spirituality or resilience among family caregivers of people with stroke, a scoping methodology was employed. Scoping reviews have particular utility when the literature around a topic is embryonic or fragmented (Arksey & O’Malley, 2005). The purpose of this scoping review was to map the literature investigating spirituality and/or resilience among family caregivers of people with stroke. Some implications for rehabilitation practice will also be discussed.
2Methods
This scoping review utilised Arksey and O’Malley’s (2005) method, which was refined by Levac, Colquhoun & O’Brien (2011). Five steps were recommended; identifying the research question, identifying the relevant studies, study selection, charting the data, collating, summarising and reporting results, and consultation.
2.1Identifying the research question
Articulation of the research question involves defining the concept, population of interest and health outcomes (Arksey & O’Malley, 2005; Levac, Colquhoun & O’Brien, 2010). The conceptualisations of spirituality by Meraviglia (1999) and Canda and Furman (2009), outlined earlier, will be used for the purposes of study. These definitions illustrate the breadth of the term, which extends beyond religious belief alone, and may encompass connectedness, meaning-making and purpose. Likewise, the understanding of resilience as a dynamic process encompassing positive adaptation during a time of adversity (Luthar, Cicchetti & Becker, 2000) will inform this review.
The target population was defined as the family caregivers (i.e., informal care) of adults who have survived a stroke. Paid carers were excluded. Health outcomes of interest were drawn from two other scoping reviews conducted within the fields of SCI and TBI (Jones, Simpson, Briggs & Dorsett, 2016; Jones, Pryor & Care-Unger, Simpson, 2018) and included quality of life, life satisfaction, and positive psychological health. Constructs associated with positive emotions, resilience and spirituality included “personal meaning”, “purpose in life”, and “post-traumatic growth” (Smith, 2012).
2.2Identifying the relevant studies
Search strategies included a search of electronic databases, as well as reviewing reference lists and author tracing (Arksey & O’Malley, 2005). Five databases, MEDLINE, PsycINFO, Emcare, Embase and PubMed, were systematically searched. Search terms were agreed by all team members and used to capture the target population as follows; “family”, “caregiver”, “spouse”, “couple*”, “husband”, “wife”, “parent” or “carer” combined with “stroke”, “cerebrovascular accident”, “CVA”, “cerebrovascular incident”, “cerebrovascular insult” or “brain attack.” The search was focused on constructs associated with both spirituality and resilience separately. “Spirituality”, “religion”, “hope”, “faith”, “connectedness”, “meaning in life”, “purpose in life”, “personal meaning” or “transcend*” were used to identify studies on spirituality. “Resilience”, “coping” or “post-traumatic growth” were used to identify studies on resilience in the population of family caregivers of survivors of stroke.
The search was limited to peer-reviewed journals in the English language between 1998 and 2018. Reference lists of literature reviews and systematic reviews were also checked for relevant articles, although this yielded no additions. Author tracing, a search strategy available on all databases, was used during the screening stage and is discussed in the section on study selection below. EndNote was used to manage the large volume of references, identify duplicates and request articles that were not readily available.
2.3Study selection
Studies were included if they contained empirical data from qualitative or quantitative studies, as reported by the population of caregivers of survivors of stroke, not the survivors themselves. Studies with mixed diagnostic groups were included only when discrete data were reported separately for the stroke group. Literature reviews, study protocols, editorials, case studies and commentaries were excluded. Studies reporting on populations with mixed diagnosis (if data on stroke was not reported separately), the experience of paid caregivers and the paediatric population were excluded.
The screening was conducted in two stages. An initial screen of titles and abstracts was conducted to exclude articles unrelated to the stroke population. Of the first 643 articles excluded, it was necessary to obtain the full text of 22 due to insufficient information in the title and abstract. Literature reviews and research protocols were conserved up to this stage so that author tracing and examination of reference lists could also be undertaken. The same five databases were used to trace the authors of two study protocols (Brasier et al., 2016; Terrill et al., 2016) but did not uncover additional studies; nor did an examination of reference lists of one literature review, and these articles were then dropped.
The remaining 319 papers concerned the population of family caregivers and adult survivors of stroke. The second stage of screening yielded 35 articles focused on family caregivers of adult stroke survivors, either describing their experience or reporting on observations of resilience, spirituality or related constructs. These were examined for eligibility by the first author.
2.4Charting the data
Descriptive information was collected from the studies. Data on first author, year of publication, location, study design, study focus, caregiver demographics, relative with stroke demographics and stroke severity were collected for all studies. For qualitative studies key themes relevant to the review were identified. For quantitative studies, data on any measures employed and key findings were extracted. Experimental studies also collected information on treatment type, duration, setting and provider. The study focus was classified as primary, if spirituality or resilience was the principle focus/purpose of the study. If the study had a different focus (e.g. overall state of caregivers) among which spirituality was one of a larger group of variables or factors investigated, then the focus on spirituality was classed as secondary. To encompass the differing study designs, multiple data charting forms were devised, similar to those used by Simpson and Baguley (2012) and Jones, Simpson, Briggs and Dorsett (2016).
2.5Collating, summarising and reporting results
Information collected about the studies were grouped into three Tables for observational (qualitative, quantitative) and experimental studies and summary data generated. Given the heterogeneity of the studies, no data pooling was possible, and all findings are reported on a study-by-study basis. The quantitative studies were examined for statistically significant links between spirituality, resilience and adjustment in family caregivers, including a randomised control trial (RCT) classified as Level II evidence in the evidence hierarchy; a mechanism for determining which study designs have the most power to predict cause and effect among variables. Evidence is ranked from the highest (Level 1), namely systematic reviews or meta-analyses through to the lowest (Level VII) type of evidence such as the opinion of authorities, reports or experts in the field (Melnyk & Fineout-Overholt, 2019).
3Results
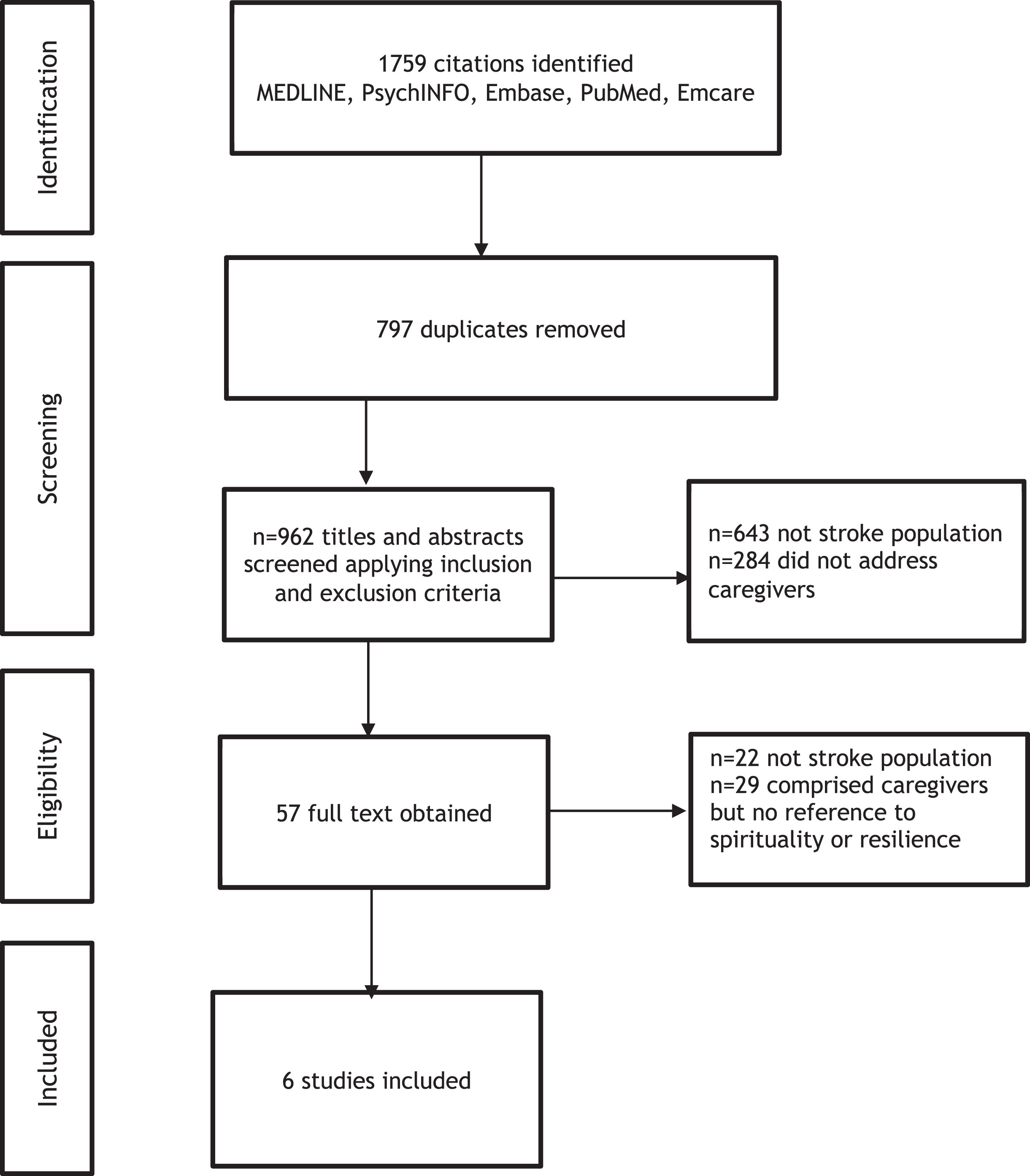
The initial search yielded 1759 citations with 962 remaining after duplicates were removed. The authors (LG, MA, GS, KJ) identified six articles for inclusion. Of these six studies, three were descriptive qualitative designs (Table 1), two were quantitative studies (one cross-sectional; one longitudinal) (Table 2) and one was a randomised controlled trial (Table 3). Papers were conducted in the United States (2), China (2), United Kingdom (1), and Turkey (1). One qualitative investigation focused explicitly on spirituality as a construct (Pierce, Steiner, Havens & Tormoehlen, 2008) while the other two qualitative approaches (Strudwick & Morris, 2010; Qui, Sit & Koo, 2017) reported incidentally on spirituality or religious faith in family caregivers. Turning to the two quantitative studies (Qiu & Li, 2008; Teel, Duncan, Lai & Min, 2001) spirituality was a secondary finding as measured by the well-validated Brief Cope scale (Carver, Scheier, & Weintraub, 1989) and Spiritual Perspective Scale (SPS) (Reed, 1986) respectively. One study focused on multiple constructs of resilience (Inci & Temel, 2016) as measured by the Family Index of Regenerativity and Adaptation – General (FIRA-G). No research was found examining the relationship between spirituality and resilience in family caregivers of individuals with stroke.
Table 1
Qualitative studies
| First author, year, country | Study design | Study focus | Caregiver demographics | Characteristics of relative and severity of stroke | Key findings relevant to the review |
| Pierce (2008) USA | Descriptive qualitative | Primary, Spirituality | 36 family caregivers | 36 relatives with first time stroke | Spirituality was a strategy for coping with day to day burden of caregiving. Four themes- “feeling the presence of a greater power”, “practicing rituals”, “being one with nature”, interacting with family and friends” |
| Age range 31–80 years | |||||
| Web-based discussion groups | Female n = 25 (69.4%) | Severity of stroke not documented | |||
| Male n = 11 (30.6%) | |||||
| Strudwick (2010) United Kingdom | Qualitative | Secondary, Spirituality | 9 African-Caribbean carers | 9 relatives with stroke | One major theme: “Faith in God” supported by three subthemes- “religious beliefs, “praying” and “reading the bible” which helped caregivers cope with the demands of caregiving |
| Average age 62 (range 30–72) | |||||
| Semi-structured interviews | Female n = 9 | Severity of stroke not documented | |||
| Male n = 1 | |||||
| Qiu (2018) China | Qualitative descriptive | Secondary, Spirituality | 25 family caregivers | 25 relatives with ischaemic stroke n = 17 (68%); haemorrhagic stroke n = 8 (32%) | Spirituality or religious faith was a personal resource employed for coping with the burden of caregiving |
| Semi-structured interviews | Average age 66±15.90; Female 76% Male 24% | Bartel Index (BI) mean 55.45±33.09 suggesting dependency was in the severe range |
Table 2
Quantitative studies
| First author, year, country | Study design | Study focus | Caregiver demographics | Severity of stroke | Measures | Main findings relevant to the review |
| Teel (2001) Kansas, USA | Longitudinal study over 1,3- and 6-months post stroke | Secondary, Spirituality | 83 caregivers | 83 relatives with minor (40%); moderate (49%); or major (11%) stroke | Visual Analog Scale for Fatigue (VAS-F); Spiritual Perspective Scale (SPS); Recurrent Sorrow Inventory (RSI); Perceived Stress Scale (PSS); Center for Epidemiological Studies Depression Scale (CES-D); Caregiver Reaction Assessment (CRA) | Spirituality was not a predictor of mental (PSS) or physical health (CRA) over time |
| Average age 57±14.2 Female n = 59 (71%) Male n = 24 (29%) | ||||||
| Qiu (2008) China | Cross-sectional design | Secondary, Spirituality | 92 caregivers | 92 relatives | Brief COPE: Emotion focused coping-religion; Center for Epidemiologic Studies Depression (CES-D) | Depression was positively associated with religion (r = .252, p < 0.01). Caregivers who used religion as a coping strategy experienced increased symptoms of depression suggesting religion was a temporary escape mechanism that gave no long term relief from the stressors of caregiving |
| Average age 47±14 Female n = 66 (71.7%) Male n = 17 (28.3%) | Bartel Index (BI) mean 42.5±14.5 | Scale | ||||
| Thirty-two (34.8%) were independent for activities of daily living. Other stroke survivors had either total, severe, moderate or slight dependence | Multiple regression showed denial, planning and functional status explained 27.4% of the variance in depression. All other variables including religion failed to enter the equation | |||||
| Short Portable Mental Status Questionnaire (SPMSQ) mean 1.9±2.2 | ||||||
| Nearly a third (28.3%) had either mild, moderate or severe cognitive impairment |
Table 3
Experimental study
| First author, year and country | Study design, study focus | Caregiver demographics and severity of stroke | Treatment type | Treatment duration | Setting and provider | Study focus | Measure | Outcome | Quality of trial |
| Inci (2016) Turkey | Randomised controlled trial with pre-test, post-test and 6-month follow-up. | 70 (34 experimental and 36 control) female family caregivers. | Support programme consisting of social support based on resilience model alongside routine home care | 5 weeks | Denizli State Hospital Clinic of Home Care Services, Turkey | Primary, Resilience | Family Index of Regenerativity and Adaptation-General (FIRA-G); Family Stressors Index (FSI), The Family Strains Index (TFSI); Relative and Friend Support Index (RFSI); Social Support Index (SSI), The Family Coping-Coherence Index (TFCCI); Family Hardiness Index (FHI), Family Distress Index (FDI). | Significant improvement (p = .001) in experimental vs control group across the three time points (group×time interaction) in 1/7 outcome domains (SSI) but test statistic not provided. | Class II |
| Primary, resilience | Stroke severity not documented | 2 sessions per week: 90 and 60 min respectively | Nurse researcher | Authors conclude that the support programme improves resilience. |
3.1Qualitative studies
The three qualitative studies showed spirituality was a personal resource for coping with the day-to-day burden and stress of caring for family members with stroke. As seen in Table 1, the construct of interest was spirituality, although it was the primary focus of only one of the three studies. Sample sizes of the studies ranged from nine to thirty-six consisting of mostly female caregivers of individuals with stroke. Two of the studies did not report on the severity of stroke. The researchers employed a range of theoretical and philosophical perspectives for understanding spirituality in caregivers with one study offering health professionals an extensive rationale for addressing the spiritual needs of family caregivers.
The study by Peirce et al., (2008) was the only study within this group to explicitly focus upon spirituality as a construct. Drawing from Friedemann’s (1995) framework of schematic organization, spirituality was defined as ‘the beliefs and practices that connect people with sacred or meaningful entities and give purpose to life’ (p.607). From a yearlong e-mail discussion group with 36 caregivers the majority (69%) had responses that were coded to spirituality data: (i) feeling the presence of a greater power, (ii) practising rituals, (iii) being one with nature, and (iv) interacting with family and friends, which helped caregivers cope with the day-to-day burden of caregiving. Implications for nursing practice were discussed extensively identifying spiritual care as an important part of the nursing process with strategies and interventions structured around each theme identified in the study. This study provides health professionals with a detailed, theoretically based rationale to address spirituality for families caring for relatives with stroke. Overall, this study provided a better understanding of how spirituality helped caregivers achieve a sense of well-being. The researchers did not document the severity of the stroke, and the majority of participants were female and Caucasian, which limits the transferability of findings.
Fig. 1
Database search.
The research by Qui, Sit and Koo (2018) did not directly focus upon spirituality, instead drawing upon the Revised Sociocultural Stress and Coping Model (Bob & Sayegh, 2009) the cultural values of 25 Chinese caregivers of relatives with stroke were explored. Three themes emerged; (i) the caregiving role perception in which caregiving was viewed as a natural, expected part of life, a culturally prescribed obligation and an expression of reciprocal love. (ii) Coping strategies which included connecting with family resources and inner strength. Spirituality, religious faith, praying, clinging to something beyond human power and fatalism were described by caregivers as ways of coping. (iii) Self-sacrifice including self-reliance, restraint in using formal services and neglecting caregivers’ own health. Respondents reported always putting the patient first. The authors acknowledge the influence of Confucian philosophy and its associated fatalism, “duty-bound obligations” particularly “filial piety” defined as “children’s respect, obedience, loyalty, material provision and physical care of their parents” (Qiu et al., 2018, p. 310). The authors inferred that cultural and religious background could positively influence the mental well-being of caregivers as they accept the indisputable aspects of caregiving. Implications for practice highlighted the need for health professionals to adopt strength-based interventions, including the spiritual needs of the caregiver. Methodological limitations were not documented by the researchers.
Strudwick and Morris (2010) explored a range of constructs including spirituality, religious beliefs and ways of coping, drawing upon the perspective of eight African-Caribbean stroke carers. Carer experiences were coded using thematic analysis as described by Braun and Clarke (2006). “Faith in God” as a self-described way of coping was a theme common to almost all carers. A belief that God was in control, praying and reading the Bible were also commonly reported. The authors recommend supporting the spiritual needs and religious beliefs of this ethnic minority. Limitations included no documentation on the severity of the stroke, small sample size and lack of matching interviewer-interviewee ethnicity.
3.2Quantitative studies
The primary focus of the two quantitative studies was on global caregiver adjustment following stroke, and the results in relation to spirituality (Teel, Duncan, Lai & Min, 2001) and religion (Qiu & Li, 2008) were secondary findings (Table 2). Sample sizes for the two studies were 83 and 92 caregivers, respectively. The majority of caregivers in both studies were females who were caring for a relative with a minor, moderate or major stroke (Teel et al. 2001) or a relative with a functional disability rated as independent, slight, moderate, severe or total dependence (Qui & Li, 2008). Multivariate and univariate analyses were employed in both studies to determine the importance of spirituality and religion in predicting caregiver adjustment.
Teel and colleagues observed family caregivers at three different times post-stroke (1 month, three months and six months) and found most caregivers (94.9%) reported a religious preference, but spirituality and esteem declined over time and correlated with more physical health problems. However, once spirituality was entered into multiple regression equations spirituality was not a predictor of mental or physical health. Instead, at three and six months, there was a reciprocal relationship between physical health and depressive symptoms. Perceived stress was related to mental health difficulties at three and six months. There was no relationship between the physical or mental health of caregivers and survivor characteristics or caregiver characteristics. This study demonstrates temporal changes; correlational waning, spiritual perspective and esteem in the target population after stroke.
Qiu & Li (2008) identified significant correlations between coping strategies and depression in family caregivers. There was a positive correlation between caregiver depression and burden, caregiver denial and self-blame. Planning and religion were coping strategies associated with increased depressive symptoms, suggesting religion was only a temporary escape that gave no long-term relief from the stressors of caregiving. Although religion was significantly associated with depression, its contribution was no longer significant when the severity of a stroke, coping strategies planning and denial were included in the regression analysis. A limitation was that the study was conducted in Wuhan city in China while the instruments were developed in Western culture.
3.3Experimental studies
This scoping review did not identify research that examined the links between spirituality and resilience in family caregivers of individuals with stroke. However, there was one study that focused on resilience in this population. Employing “The Resiliency Model of Family Stress, Adjustment, and Adaptation” (McCubbin & McCubbin, 1996) Inci and Temel (2016) conducted a randomised controlled trial to determine the effect of a support program on resilience in family caregivers. They found the social support intervention increased the social support dimension of the resilience model, suggesting the program improved community integration amongst caregivers for seeking emotional support, building esteem and networking. This study had several limitations. Male caregivers were excluded; severity of stroke was not documented, and the researcher was not blinded to group assignment during data collection and intervention stages of the trial.
4Discussion
Only a small number of studies were identified that had investigated either spirituality or resilience among family caregivers after stroke. This finding is echoed by the lack of research into spirituality or resilience among people with stroke more broadly (Sadler, Sarre, Tinker et al, 2017; Sarre, Redlich, Tinker et al., 2014). It is also consistent with the state of caregiver research among other neurologic groups (SCI, Jones et al., 2016; TBI, Jones et al., 2018). The dominant theme that could be identified from the qualitative studies was the role of spirituality in helping to cope with the burden of care. In the two quantitative studies, spirituality was non-significant in predicting outcomes in the multivariate and some univariate analyses. The one intervention trial, a psycho-educational program, highlighted the important link between resilience and social support, but did not incorporate an element of spirituality into the program.
In the qualitative studies, the themes suggested that spirituality did help alleviate day to day burden. Previous reviews of caregiver burden after stroke have not identified a potential role for spirituality (Rigby, Gubitz & Phillips, 2009), but this initial qualitative data suggests that it is an important area for further investigation. A study published in the current issue has found that spirituality has an inverse relationship to caregiver burden after TBI and SCI (Simpson et al., 2020), and this could also be tested empirically after stroke.
Potential mechanisms by which spirituality might help alleviate the stresses of caregiving are flagged by both Pierce and colleagues (2008) and Strudwick & Morris (2010) whose thematic findings both highlighted a theme of ‘feeling the presence of a greater power’. This dimension of transcendence is a core aspect of spirituality (Meraviglia, 2999), and can be experienced either within an institutionalised religious setting, or as a more individualized experience as reflected in various spirituality measures (Bufford, Paloutzian, & Ellison, 1991; Peterman, Fitchett, Brady, Hernandez, & Cella, 2002; Fetzer Institute & National Institute on Aging Working Group, 1999).
Practising rituals was another way spirituality was identified by Pierce and colleagues (2008) to assist family caregivers after stroke. Although there is limited information about this in the wider literature, one study of individuals affected by TBI found that attending religious ceremonies was associated with life satisfaction (Philippus et al., 2016). Furthermore, the practice of prayer and reading religious texts, was found to contribute towards hope among both individuals and family members after SCI (Jones et al., 2018). These studies suggest that religious rituals may play an important role in assisting individuals with religious beliefs to cope, as they adjust to a long-term disability.
Like the findings of the study by Pierce et al., (2008), the benefits of communing with nature has also been identified in a range of studies (Jones et al., 2018; Davis et al., 2015). Both Jones et al., (2018) and Davis et al., (2015) have identified the natural world as a source of spirituality. Activities which helped bring about connection with the natural world, such as bird watching or stargazing, were identified by individuals with SCI and their family members to bring about feelings of comfort, and the sense of being part of something bigger than themselves (Jones et al., 2018).
Last, social support derived from communities of faith is another important dimension of spirituality. This is an aspect of spirituality measured by the FACIT-SP Expanded (Peterman et al., 2002) and has been identified as a key component of mental health among both individuals with SCI and TBI (Franklin, Yoon, Acuff, & Johnstone, 2008; Johnstone, Yoon, Rupright, & Reid-Arndt, 2009). Social support has been studied as a stand-alone factor within studies of family caregivers after stroke (Condon, Benford, Kontou, Thomas & Walker, 2019; Northcott, Moss, Harrison & Hilari, 2016). However, it can also be considered one element within a multi-dimensional understanding of resilience. This association was demonstrated experimentally in the one intervention study that was identified by the review (Inci & Temel, 2016), advancing previous observational family caregiver studies in other neurologic groups between resilience and social support (e.g., TBI, Anderson et al., 2019).
In terms of the quantitative observational studies, the one finding of note was a weak positive association between spirituality and depression (Qiu & Li, 2018), and the authors speculated that this link might indicate that religion was a temporary escape mechanism but without providing long-term relief from the stresses of caregiving. However, observational studies among caregivers with SCI and TBI have found the opposite, with spirituality acting as a buffer or protective factor, either in direct association with depression (Simpson et al., 2020) or as mediated through resilience (Jones, Simpson, Briggs et al., 2019). So further research will be required to help clarify this issue among caregivers of people with stroke. In undertaking such at task, the religion subscale in the Brief COPE (Carver, 1997) has only two items (‘I usually pray or meditate’; ‘I usually try to find comfort in my religion or spiritual beliefs’), so may not fully capture the construct of spirituality, and more comprehensive spirituality-specific measures may be preferable.
Overall, the methodological rigour of the qualitative studies identified in the review reflected many of the same limitations identified by Greenwood and colleagues (2019) in earlier qualitative studies investigating the experience of family caregivers after stroke. The findings with the quantitative studies that (i) there were no significant correlations between spirituality and other study variables (Teel et al., 2001) or (ii) significant findings of univariate association which disappeared once multivariate analyses were conducted (Qiu et al., 2008), was similar to findings for the review of spirituality studies after SCI (Jones et al., 2016). However, the employment of more robust measures of spirituality may help solve this issue.
5Conclusion
Future research would benefit from clearly defining spirituality and resilience and utilising instruments that are culturally appropriate and specifically designed. Descriptive studies with a focus on establishing a clear link between spirituality and resilience would justify further research and development of support programmes in the target population. Longitudinal observation would help to identify temporal changes that may be relevant to the development of support programmes. Experimental studies testing the efficacy of support programmes with a spiritual component in the target population are also indicated for future research. In a systematic review and meta-analysis of psychosocial interventions for stroke survivors and/or their family caregivers, Minshall and colleagues (2019) concluded while there was evidence that current interventions could reduce depressive symptoms, there was little or no evidence for improvements in quality of life or self-efficacy, with an associated reduction in caregiver strain. However, new resilience programs are emerging for stroke survivors (e.g., Sadler, Sarre, Tinker, Bhalla, & McKevitt, 2017) and it may be possible to adapt such a program for family caregivers. Addressing these gaps may clarify the link between spirituality and resilience in the family caregivers of survivors of stroke and assist in development of policies and programmes that better support the target population.
Conflict of interest
None to report.
References
1 | Anderson, M. , Daher, M. , & Simpson, G. ((2019) ). A predictive model of resilience among family caregivers supporting relatives with traumatic brain injury (TBI): A structural equation modelling approach. Neuropsychological Rehabilitation. doi: 10.1080/09602011.2019.1620787 |
2 | Arksey, H. , & O’Malley, L. ((2005) ). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology, 8: , 19–32. |
3 | Australian Institute of Health and Welfare (2018). Australia’s Health. Retrieved on 10 Nov 2018 from: https://www.aihw.gov.au/reports/australias-health/australias-health-2018/contents/table-of-contents. |
4 | Ali, N. , & Kauser, R. ((2016) ). Social support and coping as predictors of psychological distress in family caregivers of stroke patients. Pakistan Journal of Psychological Research, 31: , 587–608. |
5 | Berg, A. , Palomaki, H. , Lonnqvist, J. , Lehtihalmes, M. , & Kaste, M. ((2005) ). Depression among caregivers of stroke survivors. Stroke, 36: , 639–643. |
6 | Braun, V. , & Clarke, V. ((2006) ). Using thematic analysis in psychology. Qualitative Research in Psychology, 3: , 77–101. |
7 | Brasier, C. , Ski, C. , Thompson, D. , Cameron, J. , O’Brien, C. , Lautenschlager, N. , Gonzales, G. , Hsueh, Y. , Moore, G. , Knowles, S. , Rossell, S. , Haselden, R. , & Castle, D. ((2016) ). The Stroke and Carer Optimal Health Program (SCOHP) to enhance psychosocial health: Study protocol for a randomized controlled trial. Trial, 17: , 446. |
8 | Canda, E. R. , & Furman, L. D. ((2009) ). Spiritual diversity in social work practice: The heart of helping. Cary, NC: Oxford University Press. |
9 | Carver, C. S. ((1997) ). You want to measure coping but your protocol’s too long: Consider the brief COPE. International Journal of Behavioral Medicine, 4: , 92–100. |
10 | Cheng, H. Y. , Chair, S. Y. , Chau, J. P. C. ((2018) ). Effectiveness of a strength -orientated psychoeducation on caregiving competence, problem-solving abilities, psychosocial outcomes and physical health among family caregiver of stroke survivors: A randomised controlled trial. International Journal of Nursing Studies, 87: , 84–93. |
11 | Cohen, S. , & Wills, T. A. ((1985) ). Stress, social support, and the buffering hypothesis. Psychological Bulletin, 98: , 310–357. |
12 | Condon, L. , Benford, P. , Kontou, E. , Thomas, S. , & Walker, M. ((2019) ). The use of carer perspectives and expert consensus to define key components of a biopsychosocial support intervention for stroke carers. Topics in stroke rehabilitation, 1–8. |
13 | Feigin, V. L. , Lawes, C. M. , Bennett, D. A. , & Anderson, C. S. ((2003) ). Stroke epidemiology: A review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. The Lancet Neurology, 2: (1), 43–53. |
14 | Friedman, M. ((1995) ). The framework of systemic organisation: A conceptual approach to families and nursing. California, Sage publications. Retrieved on 8 Nov 2018 from ProQuest Ebook central: https://ebookcentral.proquest.com/lib/avondale/reader.action?docID=997211&query= |
15 | Giaquinto, S. , Spiridigliozzi, C. , & Caracciolo, B. ((2007) ). Can faith protect from emotional distress after stroke? Stroke, 38: (3), 993–997. |
16 | Greenwood, N. , Mackenzie, A. , Cloud, G. C. , & Wilson, N. ((2009) ). Informal primary carers of stroke survivors living at home-challenges, satisfactions and coping: A systematic review of qualitative studies. Disability and Rehabilitation, 31: , 337–351. DOI: 10.1080/09638280802051721 |
17 | Hallam, W. , & Morris, R. ((2014) ). Post-traumatic growth in stroke carers: A comparison of two theories. British Journal of Health Psychology, 19: , 619–635. |
18 | Han, B. , & Hayley, W. ((1999) ). Family caregiving for patients with stroke, review and analysis. Stroke, 30: , 1478–1485. |
19 | Hayley, W. , Roth, D. , Coleton, M. , Ford, G. , West, C. , & Collins, R. ((1996) ). Appraisal, coping and social support as mediators of wellbeing in black and white family caregivers patients with Alzheimer’s disease. Journal of Consulting and Clinical Psychology, 64: , 121–129. |
20 | Hayley, W. , Roth, D. , Howard, G. , & Safford, M. ((2010) ). Caregiving, strain and estimated risk for stroke and coronary heart disease among spouse caregivers: Differential effects by race and sex. Stroke: A Journal of Cerebral Circulation, 41: , 331–336. |
21 | Hayley, W. , Roth, D. , Hovater, M. , & Clay, O. ((2010) ). Long-term impact of stroke on family caregiver well-being: A population-based case-control study. Neurology, 84: , 1323–1329. |
22 | Inci, F. , & Temel, A. ((2016) ). The effects of the support program on the resilience of female family caregivers of stroke patients: Randomised controlled trial. Applied Nursing Research, 32: , 233–240. |
23 | Johnstone, B. , Franklin, K. L. , Yoon, D. P. , Burris, J. , & Shigaki, C. ((2008) ). Relationships among religiousness, spirituality, and health for individuals with stroke. Journal of Clinical Psychology in Medical Settings, 15: , 308–313. |
24 | Jones, K. , Simpson, G. , Briggs, L. , Dorsett, P. , & Anderson, M. ((2019) ). A study of whether individual and dyadic relations between spirituality and resilience contribute to psychological adjustment among individuals with spinal cord injuries and their family members. Clinical Rehabilitation, doi: 10.117/0269215519845034 |
25 | Jones, K. , Simpson, G. , Briggs, L. , & Dorsett, P. ((2016) ). Does spirituality facilitate adjustment and resilience among individuals and families after SCI? Disability and Rehabilitation, 38: , 921–935. |
26 | Jones, K. , Pryor, J. , Care-Unger, C. , & Simpson, G. ((2018) ). Spirituality and its relationship with positive adjustment following traumatic brain injury: A scoping review. Brain Injury, 32: , 1612–1622, doi: 10.1080/02699052.2018.1511066 |
27 | Koenig, H. G. ((2012) ). Religion, spirituality, and health: The research and clinical implications. ISRN Psychiatry, 1–33, doi: 10.5402/2012/278730 |
28 | Levac, D. , Colquhoun, H. , & O’Brien, K. ((2010) ). Scoping studies: Advancing the methodology. Implementation Science, 5: , 5–69. |
29 | Luthar, S. S. , Cicchetti, D. , & Becker, B. ((2000) ). The construct of resilience: A critical evaluation and guidelines for future work. Child Development, 71: , 543–562. |
30 | Meraviglia, M. G. ((1999) ). Critical analysis of spirituality and its empirical indicators. Journal of Holistic Nursing, 17: , 18–33. |
31 | Minshall, C. , Pascoe, M. C. , Thompson, D. R. , Castle, D. J. , McCabe, M. , Chau, J. P. , & Ski, C. F. ((2019) ). Psychosocial interventions for stroke survivors, carers and survivor-carer dyads: A systematic review and meta-analysis. Topics in Stroke Rehabilitation, 1–11. |
32 | Mukherjee, D. , & Patil, C. G. ((2011) ). Epidemiology and the global burden of stroke. S-S. World Neurosurgery, 76: , 90. |
33 | Penly, J.A. , Tomaka, J. , & Wiebe, J.S. ((2002) ). The association of coping to physical and psychological health outcomes: A meta-analytic review. Journal of Behavioral Medicine, 25: , 551–603. |
34 | Pierce, L. , Steiner, V. , Havens, H. , & Tormoehlen, K. ((2008) ). Spirituality expressed by caregivers of stroke survivors. Western Journal of Nursing Research, 30: , 606–619. |
35 | Qiu, X. , Sit, J. , & Koo, F. ((2017) ). The influence of Chinese culture on family caregivers of stroke survivors: A qualitative study. Journal of Clinical Nursing, 27: , 309–319. |
36 | Qui, Y. , & Li, S. ((2008) ). Stroke: Coping strategies and depression among Chinese caregivers of survivors during hospitalisation. Journal of Clinical Nursing, 17: , 1563–1573. |
37 | Rigby, H. , Gubitz, G. , & Phillips, S. ((2009) ). A systematic review of caregiver burden following stroke. International Journal of Stroke, 4: (4), 285–292. |
38 | Sadler, E. , Sarre, S. , Tinker, A. , Bhalla, A. , & McKevitt, C. ((2017) ). Developing a novel peer support intervention to promote resilience after stroke. Health & Social Care in the Community, 25: , 1590–1600. |
39 | Sarre, S. , Redlich, C. , Tinker, A. , Sadler, E. , Bhalla, A. , & McKevitt, C. ((2014) ). A systematic review of qualitative studies on adjusting after stroke: Lessons for the study of resilience. Disability and Rehabilitation, 36: , 716–726. |
40 | Simpson, G.K. , Anderson, M. , Jones, K. , Genders, M. , Gopinath, B. , ((2020) ). Do spirituality, resilience and hope mediate outcomes among family caregivers after traumatic brain injury or spinal cord injury? A structural equation modelling approach. NeuroRehabilitation, 46: (1), 3–15. |
41 | Simpson, G. K. , & Baguley, I. J. ((2012) ). Prevalence, correlates, mechanisms and treatment of sexual health problems after traumatic brain injury: A scoping review. Critical Reviews in Physical Medicine and Rehabilitation, 23: , 215–250. |
42 | Smith, B. , Ortiz, J. , Wiggind, K. , Bernard, J. , & Dalen, J. ((2012) ). Spirituality, resilience and positive emotions. In L. J. Miller (Ed.), The Oxford Handbook of Psychology and Spirituality (pp. 437-454). New York: Oxford University Press. |
43 | Stroke Foundation ((2017) ). No Postcode Untouched. Retrieved on 10 Nov 2018 from: https://strokefoundation.org.au/en/What-we-do/Research/No-postcode-untouched. |
44 | Strudwick, A. , & Morris, R. ((2010) ). A qualitative study exploring the experiences of African-Caribbean informal stroke carers in the UK. Clinical Rehabilitation, 24: , 159–167. |
45 | Teel, C. , Duncan, P. , & Lai, S. ((2001) ). Caregiving experience after stroke. Nursing Research, 50: , 53–60. |
46 | Terrill, A. , Reblin, M. , MacKenzie, J. , Cardell, B. , Einerson, J. , Berg, C. , Majersik, J. , & Richards, L. ((2018) ). Development of a novel positive psychology-based intervention for couples post-stroke. Rehabilitation Psychology, 63: , 43–54. |
47 | Yu, Y. , Hu, J. , Efird, J.T. , & McCoy, TP. ((2013) ). Social support, coping strategies and health-related quality of life among primary caregivers of stroke survivors in China. Journal of Clinical Nursing, 22: , 2160–2171. |
48 | Walsh, F. ((2003) ). Family resilience: A framework for clinical practice. Family Processes, 42: , 1–18. |
49 | White, B. , Driver, S. , & Warren, A. ((2008) ). Considering resilience in the rehabilitation of people with traumatic disabilities. Rehabilitation Psychology, 53: , 9–17. |




