Constraint Induced Aphasia Therapy: Volunteer-led, unconstrained and less intense delivery can be effective
Abstract
BACKGROUND: Constraint Induced Aphasia Therapy (CIAT) has been shown to be effective in the treatment of aphasia, but clinicians have expressed concern regarding how far CIAT is practical to implement in clinical practice.
OBJECTIVE: To determine whether CIAT delivered in a less-intense, lower dose, reduced constraint and volunteer-led format could produce positive outcomes in people with chronic aphasia.
METHODS: Two groups were run, each with two people with chronic aphasia. Treatment involved a standard CIAT card-exchange game, supplemented by a home activity. Spoken language was required for responses but alternative modalities of communication were also permitted. Each group was led by a trained volunteer, lasted 90 minutes and was delivered twice a week for four weeks.
RESULTS: Three of the four participants showed significant improvements in target word retrieval following treatment. No significant improvements were observed for untreated stimuli or language tasks. Two participants showed increases in the elaboration of their responses, and the same two showed an increase in the frequency with which they engaged in communication activities.
CONCLUSIONS: Clear gains in performance were observed for the majority of people with aphasia who participated in a less intense format, considerably lower dose and less constrained form of CIAT led by trained volunteers. This suggests that this ‘clinically realistic’ service delivery model for CIAT could be added to the clinical repertoire of speech pathologists.
1Introduction
Constraint Induced Aphasia Therapy (CIAT, also known as Constraint Induced Language Therapy, CILT, or Intensive Language Action Therapy, ILAT) is one of the few specific forms of aphasia therapy to have an evidence base supported by randomised controlled trials. Consequently, it is one of the few specific treatment programmes to be recommended in aphasia guidelines (e.g., National Stroke Foundation Clinical Guideline for Stroke Management 2010; Australian Aphasia Rehabilitation Pathway, http://www.aphasiapathway.com.au/ (Power et al., 2015)). This has led to a great deal of interest in the use of the programme by clinicians.
CIAT is a group-based treatment programme which has at its core the principles of massed practice (intensive and high dose delivery), constraint (forced oral language use) and shaping (provide a gradual transition from the communicative behaviour that initially is characteristic of the person with aphasia to progressively improved linguistic behaviour) delivered in a behaviourally relevant context (Meinzer, Rodriguez & Rothi, 2012). Barthel, Meinzer, Djundja and Rockstroh (2008) found that group-based CIAT provided equivalent gains to individually-delivered model-oriented aphasia therapy of the same intensity. This suggests that CIAT should provide a cost-saving relative to individual provision of therapy.
However, while a group-based treatment may be seen as offering cost-savings, Rose and Attard (2015) found that lack of resources (e.g. staffing/funding) was a significant barrier for many Australian speech pathologists in their attempts to provide aphasia groups. Indeed, CIAT poses additional costs given that the intensity of the programme is greater than the usual level of service provision in many centres in Australia and worldwide. Page and Wallace (2014), in a survey of US clinicians, found great concern regarding CIAT primarily because of the quantity and intensity of treatment that is required. Clinicians were also concerned that some people with aphasia may not be able to comply with an intensive schedule. Indeed, Cherney (2012) notes that higher levels of drop out have been reported from intensive treatment regimes compared to less intense regimes.
While early research appeared to suggest that more intensive treatment was more effective, more recently the discussion has become more nuanced. Cherney (2012) suggested that “more” is not necessarily “better", with the determination of optimal treatment intensity being a complex issue depending on, for example, the type of intervention, the characteristics of the participant and the environment.
The combination of these factors led us to investigate the effectiveness of CIAT when implemented at a lower intensity in an outpatient setting (Osborne & Nickels, 2012; in preparation). We found significant benefits from CIAT even when delivered for only 90 minutes, twice a week for four weeks. Nevertheless, even at reduced intensity, the time (and therefore cost) commitment for speech pathologists remains not inconsiderable. Hence, in the context of funding constraints on speech pathology services, it is of relevance that Meinzer, Streiftau and Rockstroh (2007) found that CIAT administered by trained laypeople produced comparable results to CIAT administered by speech pathologists. With this in mind, we extended our previous study (Osborne & Nickels, 2012; in preparation) to investigate whether less intense CIAT could also be effectively delivered by trained volunteers.
There have also been questions raised regarding the role of constraint in CIAT. Pulvermüller et al. (2001) suggested that people with aphasia often used the path of least communicative effort, using gestures or drawing instead of spoken language and, even within spoken language, preferring to produce those utterances they could produce easily. Pulvermüller et al. (2001) state that “Such strategies need to be suppressed in CI therapy in favor of verbal communication” and “For improving their communicative effectiveness and for avoiding further nonuse of verbal utterances difficult for them, it is imperative to induce them to use words that they normally tend to neglect” (p1621). More recently, other authors have suggested that this initial description was misleading. Pulvermüller and Berthier (2008) note “As the word “constraint” can be misunderstood in the negative sense of “restraint”, it may appear more appropriate to speak about “focusing” in this context: The idea is to help the patient focus on those language tools that are in their range of capabilities although they frequently remain unused” (p570; see also Meinzer et al., 2012 pS36; Difrancesco, Pulvermüller & Mohr, 2012). Similarly, following their finding of similar outcomes between CIAT and an unconstrained, model-oriented, aphasia therapy, Barthel et al. (2008) suggest that constraining nonverbal compensatory communication could be a dispensable element of CIAT. While some studies have suggested a benefit for CIAT over group programmes of the same intensity which do not constrain communication to oral language (e.g. Kurland, Pulvermüller, Silva, Burke and Andrianopoulos, 2012; Maher et al., 2006), others have failed to find a consistent advantage for CIAT (e.g., Rose, Attard, Mok, Lanyon, & Foster, 2013). In our earlier study (Osborne & Nickels, 2012; in preparation) we also found no advantage for the programme when implemented with constraint when use of alternative modalities was actively discouraged, compared to an unconstrained format where participants were free to use any means of communication. Consequently, in the study reported here, while we did not facilitate or model the use of alternative, nonverbal, forms of communication (cf., e.g., Rose et al., 2013), participants were regularly reminded that they were free to use these if they so wished.
In summary, based on the literature and our previous research, we wished to investigate the effectiveness of a modified form of CIAT with reduced intensity, relatively low dose and no constraint, as delivered by volunteers in a clinical setting.
2Method
2.1Participants
Four people with aphasia (3 males and 1 female) participated in this study. They were recruited from the present and past caseloads of a metropolitan outpatient department in Sydney, Australia. Inclusion criteria were a diagnosis of aphasia with expressive language impairments due to a single stroke in the left hemisphere at least fifteen months prior to the start of the study, no significant illnesses precluding their participation and fluency in English prior to the onset of aphasia. All participants had previously received at least one significant block of therapy in inpatient rehabilitation, home based therapy and/or outpatient therapy and had been discharged from treatment due to a plateauing of improvement. While participating in the study, individuals did not undertake any other form of language rehabilitation. Potential participants were excluded if they had cognitive deficits that did not allow them to participate in the assessment or therapy. This study was approved by the ethics review committee at the Royal Rehabilitation Centre Sydney and informed consent was obtained from all participants and/or carers involved in the study prior to commencement. Table 1 provides details of the participants and Appendix A provides comprehensive background language assessment details from the Comprehensive Aphasia Test (CAT; Swinburn, Porter and Howard, 2004).
2.2Design
Participants were randomly assigned to two groups, TF and CB in one group and LL and AM in the other. Each group was facilitated by a psychology student.
The data was analysed as four single-participant experimental designs with the participants acting as their own controls. All outcome measures were tested at four week intervals, twice before treatment in order to provide a measure of change without treatment and once immediately following the four week treatment block. To increase experimental control (Nickels, Best & Howard, 2015), the design included assessment of items treated in the therapy period and a matched set that were not treated, and a control task tapping a language process that was unlikely to show improvement as the result of treatment (nonword reading, PALPA subtest 36, Kay, Lesser & Coltheart, 1992). Outcome measures and the motivation for inclusion are detailed in Table 2.
Three outcome measures were used to examine improved word retrieval (treated experimental stimuli) and generalisation of word retrieval (untreated experimental stimuli, Boston Naming Test (Kaplan, Goodglass & Weintrab, 1983)). Also, given the need to listen to sentences and select the correct picture, it was possible that sentence comprehension might improve as a result of the intervention. Consequently we used the Test for Reception of Grammar (TROG-2; Bishop, 2003) to evaluate any change in this domain.
In addition to these impairment-focused outcome measures, we used three rating scales to evaluate the impact of the intervention beyond formal assessment.
1. The Communication Effectiveness Index (CETI; Lomas et al., 1989) was developed in collaboration with people with aphasia and their spouses to enable evaluation of communication in a variety of communication settings that they felt were important in their day-to-day lives. It was completed by someone close to the participant: their significant other, family member or close friend. Using a 10 cm visual analogue scale they indicated where on the scale they would judge the person with aphasia to be, from “ not at all able” to “as able as before the stroke”. There were 16 items to rate, for example, “Giving Yes/No answers” or “Describing and discussing something in depth”.
2. The Communication Activity Log (CAL; Pulvermüller et al., 2001) is a questionnaire that is completed by someone close to the participant. It requires rating of the frequency of communication of the participant with aphasia in everyday life situations. For example, “How frequently would the patient communicate with a relative or good friend?” or “How frequently would the patient verbally express criticisms or make complaints?” The 18 items are rated on a 6-point scale comprising never, almost never, rarely, sometimes, frequently, or very frequently.
3. The Communication Disability Profile (CDP; Swinburn & Byng, 2006) was designed to be an outcome measure tool that enabled people with aphasia to express their views and experience of what life with stroke and aphasia was like for them. We used the first 20 items that relate to the impact of aphasia on communication activities and require the participant to rate their talking, ability to express themselves, understanding, reading and writing in various everyday communication situations (e.g. in the last week how easy was it for you to … .express yourself with a group of friends; read and follow a headline). For each item, participants provide a self-rating on a 5-point pictorial rating scale with a minimum score of 0, and a maximum of 4.
2.3Treatment protocol
Therapy was conducted for 11/2 hours per day, twice a week for four weeks. Hence there was a total of 12 hours of therapy for each group.
The treatment protocol was based on the CIATplus protocol (Meinzer, Djundja, Barthel, Elbert, & Rockstroth, 2005) comprising both group sessions and homework tasks. However, as noted above, following our earlier study (Osborne & Nickels, 2012; in preparation) we did not prevent the use of alternative modalities of communication if the participants chose to use them.
As is standard for CIAT, therapy targeted expressive language within the card-exchange game – “Go Fish”. In addition to the two participants with aphasia, there was one volunteer per group who also played the game. The aim of the game was to collect pairs of cards. The participant was required to choose one of the cards set before them (there were always at least three cards before each player) and explicitly address one of the other co-players and request a card with the depicted item. The participant who was addressed was then required to answer the question. If the co-player had the requested card a match was made and these items were removed from the game. If the co-player did not have the card, which was frequently the case given the number of cards in the pack, then they would say “No I don’t have the picture of the … ” and the game would continue. In any given session 45 of the 60 noun/verbs were targeted and these were rotated so that each of the cards received as much play time as the others across the four weeks of the study.
The protocol included ‘shaping’: Initially participants in both groups were allowed to use single word requests and answers (e.g. “cup”). However, even in the first session an elaborated phrase was modelled (e.g. ‘the green cup’) for the participant to repeat. As therapy progressed, and if the participants were able, they were encouraged to elaborate and expand further on their descriptions and requests (e.g. “Mary, Do you have a picture of the green cup?”). Elaboration and expansion included both the use of more descriptors within their sentences and also the use of the names of other co-players. In both groups the participants were required to say the word/phrase/sentence that best described the picture. If the participant was not able to say the word after being given time to attempt it, the clinician provided the response for the participant, who was required to attempt to repeat it prior to moving onto the next turn.
Participants were also able to use other communication strategies including gesture, drawing, circumlocution and writing. They were not forced to use these during the session but were sporadically reminded (approximately 3 times per session) that they were able to use these strategies at any time.
Following the CIATplus protocol (Meinzer et al., 2005), participants were also given one task per day to complete at home, aiming to provide practice of their communication in the ‘real world’. Participants had to use speech when completing these tasks, but were allowed to use other communication modes as an adjunct. At each session, with the assistance of the facilitator, participants were required to identify a task for that day. Tasks were based on the level of the participant’s communication difficulties. For example, tasks could include speaking with their spouse for 5 minutes, ordering a coffee, or making a phone call. Participants were required to complete their homework task and give themselves a rating out of 5 where 1 = very poor, 2 = poor, 3 = ok, 4 = good and 5 = very good.
2.4Volunteers
Two undergraduate psychology students volunteered to participate in the study by running the groups. They received training and support which was intended to be similar to that usually provided to speech pathology volunteers. They first received a 3 hour training session from a speech pathologist experienced in running CIAT groups (the second author, Osborne). This began with general education regarding aphasia including observation of videos of people with aphasia. Then the CIAT approach and literature was outlined, before more specific details regarding the study were provided including the protocol. The training session included role play and discussion of how to respond to potential scenarios. In the first group session, the second author ran the first half of the group while observed by the volunteer, before roles were reversed. The volunteers received feedback after this first session. Subsequent sessions were not observed as this would not be standard in the use of volunteers in speech pathology. However the speech pathologist was available for feedback and discussion if required.
2.5Experimental stimuli
Two sets of thirty coloured photographs of nouns and thirty of verbs were selected from images available on the internet. Photographs selected targeted both high and low frequency words. Two adults without language impairment named these photographs prior to use to provide name agreement data and so that alternative responses could be noted. Any alternative names produced were accepted as alternative correct targets for the people with aphasia.
Participants with aphasia were provided with the pictures to name in a random order but blocked into noun and verb sets. The noun block was always presented before the verb block. The participants were instructed to describe the picture.
The nouns and verbs were each divided into two sets, which were matched for spoken and total word frequency (Baayen, Piepenbrock & van Rijn, 1995), number of phonemes, number of syllables, number of letters, position of primary stress, number of phonological neighbours and imageability (Davis, 2005; only available for a subset of stimuli). In addition, for nouns, the sets were matched for the number of nouns that appeared as objects in the verb pictures. The verb sets were also matched for whether an SV or SVO structure was required and for the following properties of the object noun (e.g. ‘dog’ in ‘the man is walking the dog’), spoken and total word frequency, number of phonemes, number of syllables, number of letters, position of primary stress, number of phonological neighbours and imageability (only available for a subset of stimuli).
2.6Analysis
The data were analysed using weighted statistics (WEST; Howard, Best & Nickels, 2015), first by evaluating the change across the whole study using WEST-Trend (coefficients: -1 0, 1). In addition, to determine whether the change could be unambiguously be attributed to the effects of treatment, we used WEST-Rate of Change (WEST-ROC), which examines whether the change in performance is significantly greater during the treatment phase compared to the no treatment (baseline) phase of the study (coefficients: 1, –2, 1). For both analyses, accuracy of each item is multiplied by the appropriate coefficient for that time point and summed. The resulting weighted scores are compared to the null hypothesis (no change for WEST-Trend, and no difference between the phases for WEST-ROC) using a one-sample t-test. Only when both the WEST-Trend and the WEST-ROC are significant, can it confidently be concluded that treatment has resulted in improved performance.
3Results
All participants attended every group session, and, with the exception of LL, they completed all assigned homework tasks.
3.1Control task
There was no significant change in the control task (nonword reading) for any of the participants (see Table 3). This makes it unlikely that there was any general spontaneous recovery of language processes or that there were placebo effects occurring during the study.
3.2Experimental stimuli
Figure 1 shows the performance at each time point on treated and untreated nouns for each participant, and Fig. 2 shows the performance for treated and untreated verb stimuli. Statistics are reported in Table 4.
We first analysed performance combined across nouns and verbs, and then separately for each word class.
For untreated stimuli, no individual showed any significant improvement for untreated stimuli that could be attributed to the effects of treatment. This was true for analyses combining both nouns and verbs and when the word classes were analysed individually. While some participants did show significant improvement for untreated items across the course of the study (WEST-Trend: CB, all stimuli & nouns; AM, all stimuli and verbs), there was no significant difference in the rate of change across phases indicating that the improvement across the course of the study is most likely due to practice effects on this task.
TF, the most severely impaired individual, was close to floor at all testing points, and showed no significant change in production of either treated nouns or treated verbs, when analysed combined or individually. When verbs and nouns were analysed together, the other three participants (CB, AM & LL) all showed significant treatment-related improvement for treated items (significant improvement across the course of the study (WEST-Trend) and greater improvement in the treatment phase (WEST-ROC)).
When nouns and verbs were analysed individually, there were stronger improvements for verbs than nouns:
CB showed marked improvement in production of both treated nouns and treated verbs across the study. The difference in rate of change across treated and untreated phases was significant for treated verbs and close to significance for treated nouns.
AM also showed marked improvement in production of both treated nouns and treated verbs across the study. However, when analysed individually, the difference in rate of change across treated and untreated phases was only approaching significance for both groups.
LL showed more modest improvement in performance, but there was significant treatment-related improvement for treated verbs.
3.3Elaboration of responses
As the CIAT programme also has an emphasis on increasing the complexity of the utterances used to request pictures during the game, we were also interested in how far the participant’s descriptions of the stimulus pictures were more elaborated following the treatment which may have been independent of changes in word retrieval accuracy. For example, CB, produced “knocking on the door” at pretest but “someone doing market research and knocking at someones door” at post test. To evaluate this aspect, we asked an independent rater, who was blind to order of testing, to rate the participants descriptions of the verb stimulus pictures for elaboration at the first pre-test and the post-test. Rating was on a 7 point scale where 1 corresponded to “No content words” (ie zero elaboration) and 7 corresponded to “Sentence completely elaborating all aspects of the picture, even if content words are inaccurate”.
Table 5 shows the mean elaboration ratings with one-sample t-tests evaluating the significance of the change across these two time points.
Two of the participants showed significant improvement in verb retrieval, of these one, CB, also showed significantly increased elaboration, importantly this also extended to untreated verb pictures, despite these not showing significant improvements in verb retrieval. In contrast, LL while showing improved verb retrieval did not increase in elaboration. AM, who showed marginally significant verb retrieval improvements, also showed significantly greater elaboration, but only for the treated pictures.
Finally, TF, who showed no improvement in verb retrieval, showed a pattern of less elaboration on the treated pictures following the group (significant in the opposite direction to that predicted and significant on a two-tailed test). In fact, this pattern most probably also represents and improvement for TF, whose descriptions prior to treatment were characterised by large quantities of jargon. Following treatment his responses comprising less jargon, although they were not necessarily morerelevant.
3.4Further measures of generalisation: Boston Naming Test and Test for Reception of Grammar
No participant showed a clear effect of treatment in their performance on either the Boston Naming Test, or the TROG-2 (see Table 6). In other words, there was no evidence of generalisation to these tasks.
3.5Impact on activity and participation: CETI, CAL & CDP
LL’s significant other failed to complete the CAL at the second pre-test and LL did not complete the CDP at post-test. Consequently we cannot analyse the effects of treatment on these ratings. LL was variable across the baseline for CETI ratings and showed no evidence of an effect of treatment.
In general there was a great deal of variability in the CDP ratings of all three individuals with complete data, and there was no evidence of an impact of treatment on ratings (see Table 6).
TF was variable on both the CETI and CAL over baseline, showing improved ratings. TF’s CETI showed steadily improving ratings across the course of the whole study.
CB showed large variability in over baseline for CETI and CDP, but was more consistent for CAL and showed a significant improvement in his ratings which was specific to the treatment phase.
AM showed consistency in his CETI ratings, but no change across the course of the study, but did show some indication that the treatment may have affected his ratings on the CAL.
4Discussion
In this study we aimed to identify whether it was possible to achieve positive outcomes using a form of Constraint Induced Aphasia Therapy (CIAT) that would be more feasible to deliver in the context of current clinical speech pathology practice. Hence we examined whether a modified, less intense, reduced constraint and volunteer-led implementation of Constraint Induced Aphasia Therapy (CIAT) could result in improved language in people with chronic aphasia. Participants were all individuals with chronic aphasia who had been discharged from therapy due to plateauing performance. Three of these participants showed clear, treatment-related improvements in production of target words (nouns and verbs). The final participant (TF), who had the most severely impaired word retrieval, showed no change in word retrieval performance as a result of treatment. We also examined whether there was elaboration of descriptions of the verb picture stimuli. Two of the three individuals who showed improved lexical retrieval showed greater elaboration following treatment for the treated pictures. The one participant who did not show evidence of improved lexical retrieval showed significantly less elaboration – we suggest that this may be reflective of a benefit of treatment in terms of less jargon and more concise productions. There was no change in performance on a control task (nonword reading) nor in the production of untreated items allowing us to confidently conclude that our results were treatment-specific.
There was no evidence for improvement in lexical retrieval of untreated items – either our control (untreated) stimuli or a standardised measure (Boston Naming Test). That is, there was no evidence for generalisation across items (stimulus generalisation) for lexical retrieval. This pattern is consistent with other studies where data has been examined at the level of the individual and direct comparison made of treated and untreated stimuli (e.g. Attard et al., 2013; Osborne & Nickels, 2012; in preparation). As Attard et al. (2013) used an intensive protocol and with a larger overall dose of treatment (32 hours in total across two weeks), we believe that it is unlikely that these results are due to either the dose or the less intensive delivery. Instead, it is likely to reflect the well attested pattern of item specific improvements when treatments target lexical retrieval in aphasia (Nickels, 2002).
However, importantly, one participant did show significantly greater elaboration in their responses for both treated and untreated stimuli. This suggests that while benefits for lexical retrieval may be item specific, improvements in processing may generalise more readily for some participants. Nevertheless, no similar gains were found for sentence comprehension.
In sum, the effects of treatment (and the variability across participants) were similar to those found in our earlier study where a trained speech pathologist implemented the treatment (Osborne & Nickels, 2012; in preparation) suggesting that using volunteers can be effective for treatment delivery.
We also attempted to examine the broader impact of the treatment on communication activities and confidence using the Communication Effectiveness Index (CETI; Lomas et al., 1989) the Communication Activity Log (CAL; Pulvermüller et al., 2001) and the Communication Disability Profile (CDP; Swinburn & Byng, 2006). However, despite being reported as having good reliability (e.g. Chue, Rose & Swinburn, 2010), these measures showed considerable variability in ratings, even across the baseline period. Only one measure, the CAL, showed both stability and a significant change as a result of the treatment: CB showed a significant increase in the frequency of his engagement in communicative activities as rated on the CAL, and AM a marginally significant increase. It is interesting that these are also the two participants who showed increased elaboration following treatment. Thus it is clear that, at least for some participants, this implementation of CIAT can produce an impact beyond lexical retrieval. However, it is also apparent that there are limitations to our assessment tools that hinder our ability to reliably measure sucheffects.
5Conclusion
This study demonstrates that a less intense form of Constraint Induced Aphasia Therapy, without strict constraint and delivered by a trained volunteer can produce improvements in both word retrieval, elaboration of responses and frequency of engagement in communicative activity for some (but not all) people with chronic aphasia. We would suggest that this delivery model is more likely to be implemented given the demands of clinical practice. However, we cannot be sure that greater gains might not be obtained with a more intense delivery model and/or a greater total dose of treatment. This would be a fruitful area for future research.
Conflict of interest
The authors declare no conflict of interest.
Appendices
Appendix A
Background Language Assessments (Comprehensive Aphasia Test)
Cut-off represents the score that least 95% of healthy controls exceed, with the exception of “line bisection” in which case a score below cut-off is unimpaired. Scores which are below cut-off are indicated are in bold font. Scores for all subtests except the cognitive screen, comprehension of paragraphs, digit span, repetition of sentences, spoken picture description and the writing subtests use a 0–2 scale where only an immediate correct response scores 2, slow and self-corrected responses score 1 and all other responses 0.
N/A - not attempted.
*Only half of this assessment was attempted.
Appendix B
Therapy protocol Summary provided to volunteers in conjunction with training.
2-3 participants per group
• Sessions will run for 1 1/2 hours, twice a week for 4 weeks. A total of 12 hours.
• At the beginning of all sessions the facilitator runs through the names of all the targeted cards in therapy and have participants repeat the word/phrase depending on their level – e.g. “The green cup”. For the verb cards a sentence will also be provided for each card – e.g. “The girl is brushing her hair”
• Participants will be reminded they can use gesture, write, draw, point, as well as verbally describe. However the aim of the session is still to produce the accurate word form and a sentence if able.
• Data should be collected on how often each participant said the target word within the group, and also on when the participant initiated the word compared to when the participant repeated what another participant had just said – e.g. “ No I don’t have a picture of the green cup”.
• Data will be collected on the formation of their sentence structure e.g. 0 = sentence not attempted. 1 = some correct elements of a sentence 2 = completely correct sentence structure. 3 = elaborated sentences (more than basic information). Those participants consistently achieving targeted words and sentences will be asked to elaborate on their sentences if they are not already doing so.
• In each session both nouns and verbs will be targeted. 1 1/2 hour session allows for one complete run through of one set and half through the other set – eg. all nouns and half verbs and then all verbs half nouns in the next session.
• Barriers (a manila folder) will be used between participants to enable the participants to keep their cards private, however, these did not prevent gestures being observed.
• If a participant says the word correctly but not in a sentence – SP will say the desired word in a sentence and have the participant repeat this sentence if he/she is able. Yes from the beginning – but normally just a short one at the beginning eg the green cup.
• If a participant is unable to say the word after 15 seconds SP will say the desired word in a sentence and have the participant repeat this if able. If a participant is only at word level SP will still say the sentence and then have the participant just repeat the word.
• Participants will be encouraged to have a practice task each day at their own level that targets using any means to communicate (e.g. with gesture, drawing, pointing etc) in their everyday life.
• Participants are required to complete their homework task and give themselves a rating out of 5 where 1 = very poor, 2 = poor, 3 = ok, 4 = good and 5 = very good.
• Small token prize given after each session for the winner of Go Fish.
Acknowledgments
We gratefully acknowledge the enthusiastic participation in this research of the four people with aphasia and their significant others We would like to thank the psychology students who volunteered to run the groups, and Catherine Mason for assistance in formatting the manuscript. This research was funded by a National Stroke Foundation Clinical Research Development Award. During the preparation of this paper Lyndsey Nickels was funded by an Australian Research Council Future Fellowship (FT120100102).
References
1 | Attard M. , Rose M. , & Lanyon L. ((2013) ). The comparative effects of multi modality aphasia therapy and constraint induced aphasia therapy-plus for severe chronic Broca’s aphasia: An in-depth pilot study. Aphasiology, 27: (1), 80–111. |
2 | Barthel G. , Meinzer M. , Djundja D. , & Rockstroh B. ((2008) ). Intensive language therapy in chronic aphasia: Which aspects contribute most?. Aphasiology, 22: (4), 408–421. DOI: 10.1080/02687030701415880 |
3 | Baayen R. H. , Piepenbrock R. , & van Rijn H. ((1995) ). The CELEX Lexical Database. Release 2 [CD-ROM]. Linguistic Data Consortium, University of Pennsylvania, Philadelphia. |
4 | Bishop D. ((2003) ). Test for Reception of Grammar, Version 2. London: The Psychological Corporation |
5 | Cherney L. R. ((2012) ). Aphasia treatment: Intensity dose parameters and script training. International Journal of Speech-Language Pathology, 14: , 424–431. |
6 | Chue W. L. , Rose M. , & Swinburn K. ((2010) ). The reliability of the Communication Disability Profile: A patient-reported outcome measure for aphasia. Aphasiology, 24: (6-8), 940–956. DOI: 10.1080/02687030903490541 |
7 | Davis C. ((2005) ). N-Watch: A program for deriving neighbourhood size and other psycholinguistic statistics. Behor Research Methods, 37: (1), 65–70. |
8 | Difrancesco S. , Pulvermüller F. , & Mohr B. ((2012) ). Intensive language-action therapy (ILAT): The methods. Aphasiology, 26: (11), 1317–1351. DOI: 10.1080/02687038.2012.705815 |
9 | Holland A. L. , ((1980) ) Communication Abilities in Daily Living. Baltimore, MD: University Park Press. |
10 | Howard D. , Best W. , & Nickels L. ((2015) ). Optimising the design of intervention studies: Critiques and ways forward. Aphasiology, 29: (5), 526–562. DOI: 10.1080/02687038.2014.985884 |
11 | Kaplan E. , Goodglass H. , & Weintrab S. ((1983) ). The Boston Naming Test. Philadelphia: Lea & Febiger. |
12 | Kay J. , Lesser R. , & Coltheart M. , ((1992) ). Psycholinguistic Assessments of Language Processing in Aphasia (PALPA). Hove: Lawrence Erlbaum Associates. |
13 | Kurland J. , Pulvermüller F. , Silva N. , Burke K. , & Andrianopoulos M. ((2012) ). Constrained versus unconstrained intensive language therapy in two individuals with chronic, moderate-to-severe aphasia and apraxia of speech: Behoral and fMRI outcomes. American Journal of Speech-Language Pathology, 21: , S65–S87. doi: 10.1044/1058-0360(2012/11-0113) |
14 | Lomas J. , Pickard L. , Bester S. , Elbard H. , Finlayson A. , & Zoghaib C. ((1989) ). The communicative effectiveness index. development and psychometric evaluation of a functional communicative measure for adult aphasia. Journal of Speech and Hearing Disorders, 113–124. |
15 | Maher L. M. , Kendall D. , Swearengin J. A. , Rodriguez A. , Leon S. A. , Pingel K. , Holland A. , & Rothi L. J. ((2006) ). A pilot study of use-dependent learning in the context of constraint induced language therapy. Journal of the International Neuropsychological Society, 12: , 843–852. |
16 | Meinzer M. , Djundja D. , Barthel G. , Elbert T. , & Rockstroth B. ((2005) ). Long-term stability of improved language functions in chronic aphasia after constraint-induced aphasia therapy. Stroke, 36: , 1462–1466. doi: 10.1161/01.STR.0000169941.29831 |
17 | Meinzer M. , Streiftau S. , & Rockstroh B. ((2007) ). Intensive language training in the rehabilitation of chronic aphasia: Efficient training by laypersons. Journal of the International Neuropsychological Society, 13: , 846–853. |
18 | Meinzer M. , Rodriguez A. , & Gonzalez Rothi L. ((2012) ). First decade of research on constrained-induced treatment approaches for aphasia rehabilitation. Archives of Physical Medicine and Rehabilitation, 93: (1), 35–45. doi: 10.1016/j.apmr.2011.06.040 |
19 | National Stroke Foundation. ((2010) ) Clinical guidelines of stroke management 2010. Melbourne, Australia. http://strokefoundation.com.au/site/media/clinical_guidelines_stroke_managment_2010_interactive.pdf (accessed 23 Apr 2011). |
20 | Nickels L. A. ((2002) ). Therapy for naming disorders: Revisiting, revising and reviewing. Aphasiology, 16: , 935–980. |
21 | Nickels L. , Best W. , & Howard D. ((2015) ). Optimising the ingredients for evaluation of the effects of intervention. Aphasiology, 29: (5), 619–643. doi: 10.1080/02687038.2014.1000613 |
22 | Osborne A. , & Nickels L. ((2012) ). Constraint in aphasia therapy. Is it important for clinical outcomes?. International Journal of Stroke, 7: (Suppl 1), 53–54. |
23 | Osborne A. , & Nickels L. , (in preparation). Constraint induced aphasia therapy. Which elements are important?. Manuscript in preparation. |
24 | Page S. , & Wallace S. ((2014) ). Speech language pathologists’ opinions of constraint-induced language therapy. Topics in Stroke Rehabilitation, 21: (4), 332–338. DOI: 10.1310/tsr2104-332 |
25 | Power E. , Thomas E. , Worrall L. , Rose M. , Togher L. , Nickels L. , Hersh D. , Godecke E. , O’Halloran R. , Lamont S. , O’Connor C. , & Clarke K. ((2015) ). Development and validation of Australian aphasia rehabilitation best practice statements using the RAND/UCLA appropriateness method. BMJ Open, e007641. doi: 10.1136/bmjopen-2015-007641 |
26 | Pulvermüller F. , & Berthier M. ((2008) ). Aphasia therapy on a neuroscience basis. Aphasiology, 563–599. doi: 10.1080/02687030701612213 |
27 | Pulvermuller F. , Neininger B. , Elbert T. , Mohr B. , Rockstroh B. , Koebbel P. , & Taub E. ((2001) ). Constraint-induced therapy of chronic aphasia after stroke. Stroke, 32: , 1621–1626. doi: 10.1161/01.STR.32.7.162 |
28 | Rose M. , & Attard M. ((2015) ). Practices and challenges in community aphasia groups in Australia: Results of a national survey. International Journal of Speech-Language Pathology, 17: (3), 241–251. doi: 10.3109/17549507.2015.1010582 |
29 | Rose M. , Attard M. , Mok Z. , Lanyon L. , & Foster A. ((2013) ). Multi-modality aphasia therapy is as efficacious as a constraintinduced aphasia therapy for chronic aphasia: A phase study. Aphasiology, 27: (8), 938–971. DOI: 10.1080/02687038.2013.810329 |
30 | Swinburn K. , & Byng S. , ((2006) ). The Communication Disability Profile. London: Connect Press. |
31 | Swinburn K. , Porter G. , & Howard D. , ((2004) ). The Comprehensive Aphasia Test. Hove, UK: Psychology Press. |
32 | Webster J. , Whitworth A. , & Morris J. ((2015) ). Is it time to stop “fishing”? A review of generalisation following aphasia intervention. Aphasiology, 29: (11), 1240–1264. doi: 10.1080/02687038.2015.1027169 |
Figures and Tables
Fig.1
Noun retrieval accuracy (y-axis scale represents number of items produced accurately; Total n = 60; Treated n = 30, Untreated n = 30).
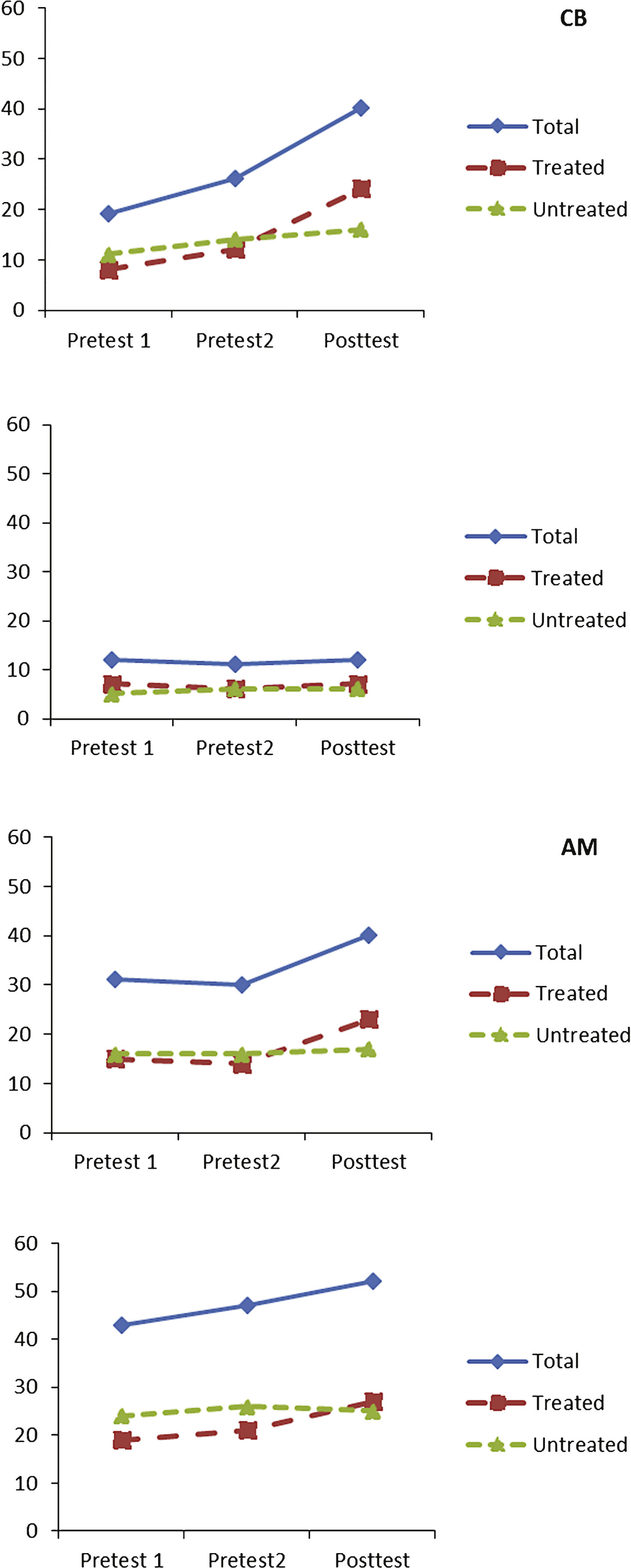
Fig.2
Verb retrieval accuracy (y-axis scale represents number of items produced accurately; Total n = 60; Treated n = 30; Untreated n = 30).
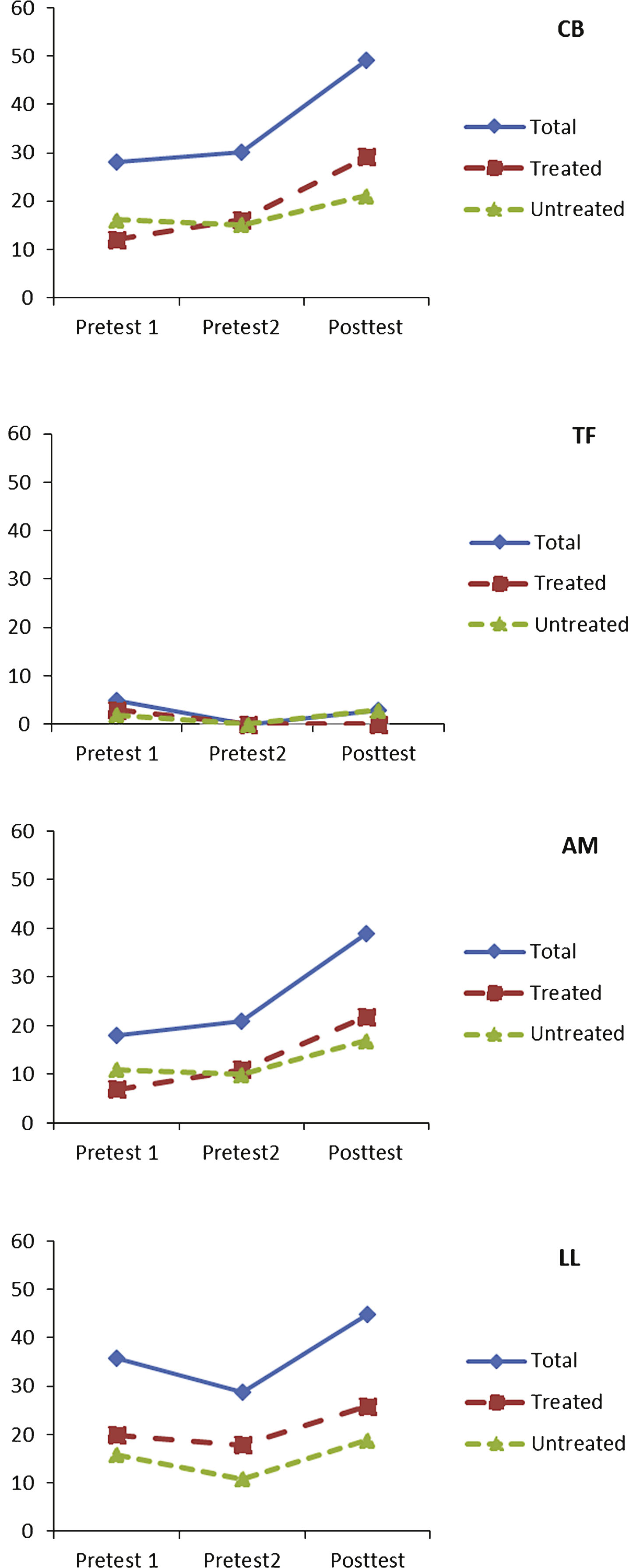
Table 1
Demographic data
| Name | Age (years) | Sex | Aphasia Type | Time since onset (years; months) | Lesion |
| CB | 34 | M | Transcortical Sensory | 1;3 | Large left parietal-occipital parenchymal haemorrhage |
| TF | 73 | M | Global | 2;6 | Left ICA infarct |
| AM | 74 | M | Global | 3;6 | Left MCA CVA |
| LL | 58 | F | Anomic | 1;4 | Large left sided intracerebral haemorrhage due to MCA aneurysm |
ICA: Internal Carotid Artery; MCA: Middle Cerebral Artery; CVA: cerebro-vascular accident.
Table 2
Outcome measures and their focus for interpretation of treatment effects
| Task | Focus |
| Describing treated noun/verb pictures | Direct effect of treatment |
| Describing untreated noun/verb pictures | Generalisation across items within task |
| Boston Naming Test | Generalisation across itemsin a standardised test |
| Test for Reception of Grammar- 2nd Edition (TROG-2) | Generalisation across modalities (sentence comprehension) |
| Nonword reading (PALPA, subtest 36) | Control task (controllingfor nonspecific treatment effects) |
| Communication Effectiveness Index (CETI) | Impact on communicative effectiveness |
| Communication Activity Log (CAL) | Impact on activity &participation |
| Communication Disability Profile (CDP): Activity section | Impact on communicative activity |
Table 3
Performance on control task - nonword reading
| Participant | Pre 1 | Pre 2 | Post |
| CB | 0 | 1 | 1 |
| TF | 1 | 0 | 0 |
| AM | 0 | 0 | 0 |
| LL | 2 | 4 | 1 |
Table 4
Summary of results of statistical analyses for word retrieval for experimental stimuli
| Treated Items | Untreated Items | |||||||||
| Trend | ROC | Treatment-specific improvement? | Trend | ROC | Treatment-specific improvement? | |||||
| t (29) | p one tailed | t (29) | p one tailed | t (29) | p one tailed | t (29) | p one tailed | |||
| ALL STIMULI (Nouns &Verbs combined) | ||||||||||
| CB | 7.972 | <0.001 | 2.481 | 0.008 | Yes | 2.199 | 0.016 | 0.814 | 0.209 | No |
| TF | –0.830 | 0.795 | 0.869 | 0.194 | No | 0.903 | 0.185 | 0.574 | 0.284 | No |
| AM | 5.077 | <0.001 | 1.966 | 0.027 | Yes | 1.843 | 0.035 | 1.137 | 0.130 | No |
| LL | 3.617 | <0.001 | 2.031 | 0.023 | Yes | 1.070 | 0.144 | 1.321 | 0.096 | No |
| NOUNS | ||||||||||
| CB | 5.113 | <0.001 | 1.610 | 0.059 | Marginal | 1.720 | 0.048 | –0.215 | 0.584 | No |
| TF | <0.001 | 0.500 | 0.360 | 0.361 | No | 0.328 | 0.373 | –0.215 | 0.584 | No |
| AM | 2.504 | 0.009 | 1.624 | 0.058 | Marginal | 0.328 | 0.373 | 0.197 | 0.423 | No |
| LL | 3.247 | 0.001 | 0.891 | 0.190 | No | 0.372 | 0.356 | –0.902 | 0.813 | No |
| VERBS | ||||||||||
| CB | 6.158 | <0.001 | 1.874 | 0.036 | Yes | 1.409 | 0.085 | 1.229 | 0.115 | No |
| TF | –1.795 | 0.958 | 1.795 | 0.042 | No | 0.571 | 0.286 | 1.980 | 0.029 | No |
| AM | 4.785 | <0.001 | 1.424 | 0.083 | Marginal | 2.693 | 0.006 | 1.313 | 0.100 | No |
| LL | 1.989 | 0.028 | 1.904 | 0.033 | Yes | 1.140 | 0.132 | 1.987 | 0.028 | No |
Table 5
Changes in ratings of elaboration of descriptions of verb pictures
| Treated | Untreated | |||||||
| Pre1 | Post | t (29) | p (1-tailed) | Pre1 | Post | t (29) | p (1-tailed) | |
| CB | 3.37 | 4.27 | 2.177 | 0.019 | 3.60 | 4.47 | 2.443 | 0.01 |
| TF | 2.33 | 1.93 | –3.026 | 0.997 | 2.17 | 2.27 | 0.501 | 0.620 |
| AM | 3.27 | 3.83 | 2.169 | 0.038 | 3.70 | 4.00 | 1.104 | 0.279 |
| LL | 4.33 | 4.13 | –0.881 | 0.385 | 4.00 | 4.43 | 1.439 | 0.080 |
Table 6
Results and statistics for additional outcome measures *significant at p < 0.05; x marginally significant (0.05 < p < 0.1); TROG results not analysed statistically due to the raw data being unavailable.
| Pre 1 | Pre 2 | Post | WEST-Trend | WEST-ROC | Treatment-specific improvement? | ||||
| Participant | t | p 1 tailed | t | p 1 tailed | df | ||||
| Boston Naming Test (n = 60) | |||||||||
| CB | 15 | 15 | 23 | 2.634 | 0.005* | 1.463 | 0.074 X | 59 | Marginal |
| TF | 10 | 20 | 15 | 0.101 | 0.101 | –2.641 | 0.995 | 59 | No |
| AM | 26 | 28 | 34 | 0.085 | 0.023* | 0.547 | 0.293 | 59 | No |
| LL | 24 | 30 | 29 | 1.386 | 0.085 | –1.297 | 0.900 | 59 | No |
| Test for Reception of Grammar (n = 80) | |||||||||
| CB | 53 | 57 | 63 | No | |||||
| TF | 31 | 36 | 37 | No | |||||
| AM | 39 | 45 | 50 | No | |||||
| LL | 61 | 67 | 57 | No | |||||
| Communication Effectiveness Index | |||||||||
| CB | 43 | 58 | 50 | 1.386 | 0.093 | –5.402 | 1.000 | 15 | No |
| TF | 41 | 59 | 72 | 2.905 | 0.005 | –0.419 | 0.659 | 15 | No |
| AM | 51 | 52 | 52 | 0.427 | 0.338 | –0.179 | 0.570 | 15 | No |
| LL | 70 | 78 | 70 | 0.000 | 0.500 | 3.004 | 0.996 | 15 | No |
| Communication Activity Log | |||||||||
| CB | 40 | 41 | 53 | 3.010 | 0.004* | 2.170 | 0.022* | 17 | Yes |
| TF | 35 | 47 | 46 | 1.451 | 0.082 | –1.493 | 0.923 | 17 | No |
| AM | 42 | 37 | 46 | 1.719 | 0.052 X | 3.500 | 0.001* | 17 | Marginal |
| LL | 69 | N/A | 66 | – | – | – | – | – | No |
| Communication Disability Profile | |||||||||
| CB | 51 | 64 | 56 | 1.751 | 0.048* | –2.666 | 0.992 | 19 | No |
| TF | 46 | 39 | 47.5 | 0.529 | 0.301 | 2.770 | 0.006* | 19 | No |
| AM | 56 | 44.5 | 42 | –2.896 | 0.995 | 0.975 | 0.171 | 19 | No |
| LL | 45.5 | 47 | N/A | – | – | – | – | – | N/A |
Table 7
| CB | TF | AM | LL | Cut-Off | |
| Cognitive Screen | |||||
| Line Bisection | 0.5 | –5 | 0 | –2 | 2.5 |
| Memory Total | 10 | 4 | 19 | 18 | 18 |
| Word Fluency | 10 | 0 | 5 | 10 | 14 |
| Gesture Object Use | 10 | 0 | 9 | 5 | 10 |
| Arithmetic | 3 | 2 | 0 | 5 | 2 |
| Spoken Comprehension | |||||
| Auditory Comprehension Words | 29 | 15 | 22 | 29 | 26 |
| Auditory Comprehension Sentences | 17 | 15 | 12 | 12 | 28 |
| Auditory Comprehension Paragraphs | 3 | 1.5 | 2 | 4 | 3 |
| Auditory Comprehension Total | 49 | 31.5 | 36 | 45 | 57 |
| Written Comprehension | |||||
| Visual Comprehension Words | 6 | 11 | 28 | 20 | 28 |
| Visual Comprehension Sentences | 2 | 0 | 16 | 24 | 24 |
| Visual Comprehension Total | 8 | 11 | 44 | 44 | 54 |
| Repetition | |||||
| Repetition Words | 32 | 28 | 30 | 32 | 30 |
| Repetition Complex Words | 6 | 4 | 4 | 6 | 6 |
| Repetition Nonwords | 10 | 4 | 0 | 8 | 6 |
| Digit Span | 14 | 8 | 6 | 6 | 10 |
| Repetition Sentences | 12 | 6 | 0 | 6 | 12 |
| Repetition Total | 74 | 50 | 40 | 58 | 68 |
| Naming | |||||
| Naming Nouns | 3 | 2 | 27 | 37 | 44 |
| Naming Verbs | 5 | 0 | 1 | 5 | 9 |
| Word Fluency | 10 | 0 | 5 | 10 | 14 |
| Naming Total | 14 | 2 | 33 | 52 | 70-71 |
| Spoken Picture Description | 13 | 0 | 0 | 38 | 35-36 |
| Reading | |||||
| Reading Words | 4 | 4 | N/A | 14* | 46 |
| Reading Complex Words | 0 | 2 | N/A | N/A | 5 |
| Reading Function Words | 0 | 0 | N/A | N/A | 4 |
| Reading Nonwords | 0 | 0 | N/A | 2 | 7 |
| Reading Total | 4 | 6 | N/A | 16 | 63 |
| Writing | |||||
| Copying | 16 | 1 | N/A | 27 | 26 |
| Written Naming | 0 | 0 | N/A | 11 | 16 |
| Writing to Dictation | 8 | 0 | N/A | N/A | 25 |
| Writing Total | 24 | 1 | N/A | 38 | 68-69 |
| Written Picture Description | 0 | 0 | N/A | N/A | 19–21 |




