Feasibility of temperature monitoring smart socks in adolescents and young adults with spina bifida
Abstract
PURPOSE:
The purpose of the study was to determine if the use of continuous temperature monitoring smart socks is feasible in adolescents with spina bifida (SB) by obtaining user feedback on comfort.
METHODS:
Participants were provided temperature monitoring socks and a 4 G hub. Follow-up phone calls were performed to answer questions or discuss barriers. Sock temperatures were monitored throughout four weeks. Following sock wear, participants were asked to complete a satisfaction survey.
RESULTS:
Seventeen of the 33 participants enrolled (eight males, nine females) with a mean age of 14.8 years completed the study. Average sock wear was 8.0 hours per day for four weeks. The mean temperature was 83.4°F with a mean temperature differential between feet of –0.74°F (left–right). The duration of sock wear varied from 14.6 to 595.9 hours over the four-week period. Lastly, eleven participants (84.6%) reported that the socks were comfortable and very easy to put on.
CONCLUSION:
Continuous temperature monitoring smart socks are an option for monitoring risk for developing pressure injuries in adolescents with SB. Future directions would include increasing sample size, obtaining normative data for temperature ranges in this population, and correlating to clinical outcomes.
1Introduction
Pressure injuries are a significant source of morbidity in youth with spina bifida (SB). A prior study found that one out of 10 ambulatory youth with SB are at risk for pressure injuries [1]. The most significant risk was found for those between the ages of 11 to 15 years with foot deformities who wore braces. The prevalence of foot pressure injuries in ambulatory pediatric patients with SB is 14%. In a National SB Patient Registry study, additional risk factors reported for all types of pressure injuries were the level of lesion, use of a wheelchair, urinary incontinence, presence of a shunt, above the knee orthopedic surgery, recent surgery, and male sex [2]. One consequence of chronic pressure injuries is amputation. Graham reported that, while SB is a rare cause of amputation, those patients with SB who did require amputation were younger than those with peripheral vascular disease and required it secondary to chronic skin ulceration [3]. Prevention and early detection of pressure injuries through monitoring temperature may be important in this population.
In adults with diabetic neuropathy, another population prone to foot pressure injuries, early detection and screening of pressure injuries have been effective in reducing complications such as sepsis and amputation [4]. Pedal temperature elevation is an early sign of pressure injury [5]. This principle has been applied to the development of continuous temperature monitoring socks. In a case control study, wireless continuous temperature monitoring through embedded sensors in smart socks was found to be reliable and accurate at detecting temperature differences, was able to correlate clinically to development of pressure injuries, and reported favorable user experiences [6].
The primary objective of the study was to determine the feasibility of continuous temperature monitoring smart socks in adolescents with SB by examining adherence to wearing the socks and obtaining user feedback on comfort. The secondary objective was to measure temperature metrics as a baseline in this population and assess for any differences.
2Materials and methods
Institutional review board approval was obtained before conducting this single-center pilot study at a tertiary referral center from January 2022 to February 2023. Continuous temperature monitoring socks were used for in-home and community ambulation (Siren Diabetic Socks, Neurofabric, Siren Care Inc, San Francisco, CA); they are designed to be reusable and are machine washable and dryable. The socks are made of “smart textile” material with microsensors woven directly into the fabric. These sensors are seamlessly integrated into the socks to monitor temperature changes on the bottom of the feet.
The sensors embedded in the socks are connected to a small tag on the sock, which encases a microcontroller unit, battery, and Bluetooth chip (Fig. 1A). The six sensors take temperature measurements at 10-second intervals to track temperature increases at the bottom of the wearer’s feet, specifically at the hallux; metatarsal points (MTPs) 1, 3, and 5; midfoot; and heel (Fig. 1B). Data was stored in the tag and sent via a 4 G hub to the HIPAA compliant cloud server. Each hub was paired with a pair of socks. These socks have been previously validated for use in patients with diabetes [6].
Fig. 1A
Siren Socks. Image of socks with tag (circled). The tag includes the battery, microcontroller unit, and Bluetooth chip. Image of Siren hub, micro-USB cable, and power adapter.
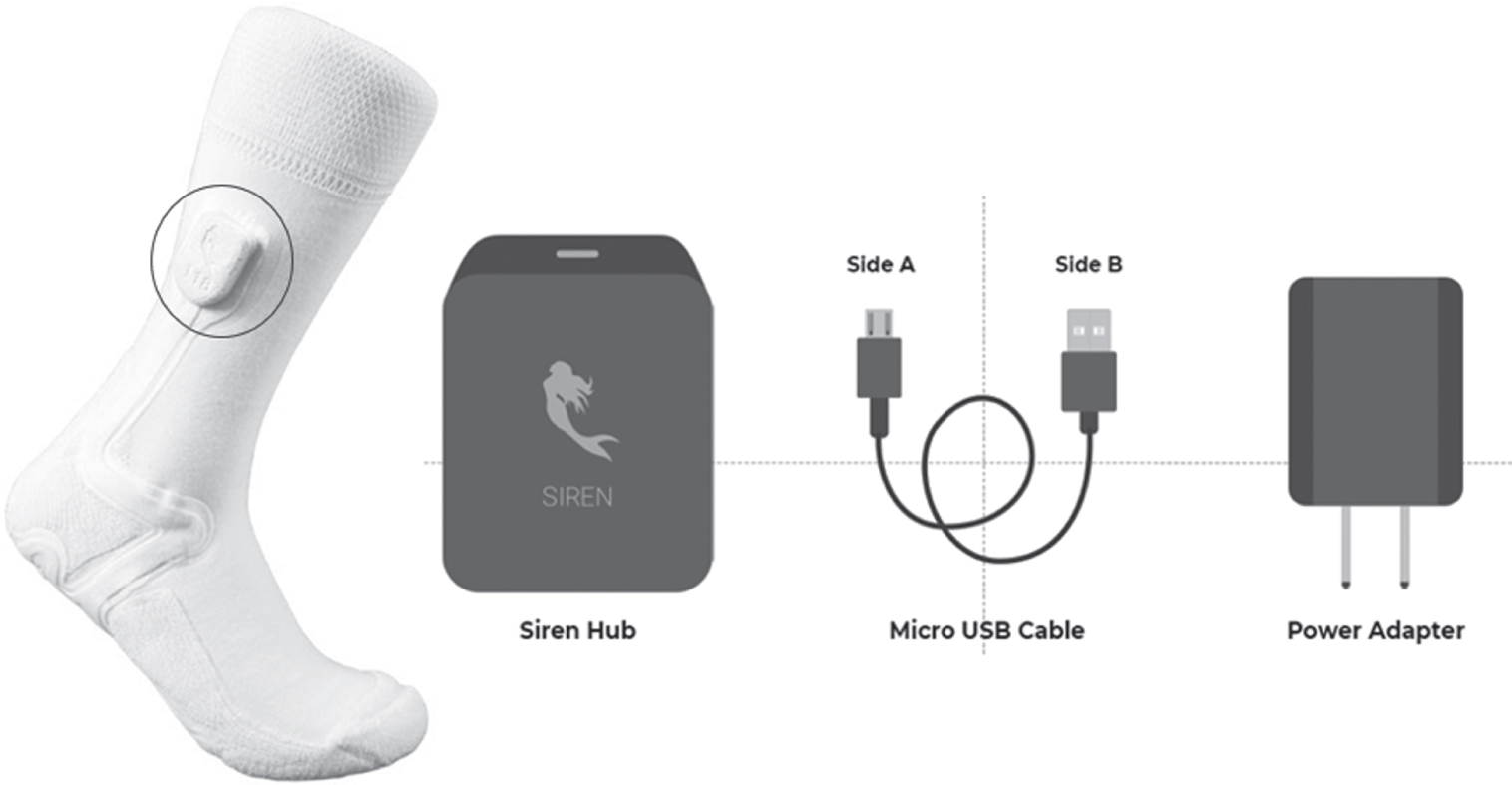
Fig. 1B
Location of Sock Sensors. Bottom of the sock where sensors are placed at the hallux (sensor 1); metatarsal points 1, 3, and 5 (sensors 2–4); midfoot (sensor 5); and heel (sensor 6). More information can be found at https://www.pngkit.com/view/u2e6r5t4q8o0r5w7_bottom-sock-bottom-of-foot-sock/.

Participants were approached for this study if they were ages 11–21 years old, had a diagnosis of SB, ambulated without assistance, either wore no braces or wore posterior leaf spring ankle foot orthoses (AFOs), supramalleolar orthoses (SMOs), or ground reaction ankle foot orthoses (GRAFOs), and did not have any active pressure injuries. Participants were excluded if they wore other types of orthoses because they interfered with the sock sensors. Participants were recruited from a multidisciplinary SB care clinic at a tertiary hospital in a large metropolitan area. Informed consent was obtained for all study participants and was completed by parents for minors, who gave their assent. Each participant participated in this study for a total of four weeks.
Upon enrollment, participants were provided with a sock kit, consisting of five pairs of temperature monitoring socks, a 4 G hub, and an instruction manual. They were shown how to put the socks on and how to connect the socks to the hub. Follow-up phone calls were made at weeks one, three, and four by the research team to answer any questions and discuss barriers to sock use.
The sock temperatures were monitored throughout the four weeks, and the physician and patient were notified if clinically significant elevated temperatures were detected. During the final week of the study after sock wear ended, participants were asked to complete a satisfaction survey which aimed to assess their experience with Siren Socks. Univariate and multivariate analysis was performed using STATA (version 14.2, StataCorp LP, College Station, TX).
3Results
3.1Adherence
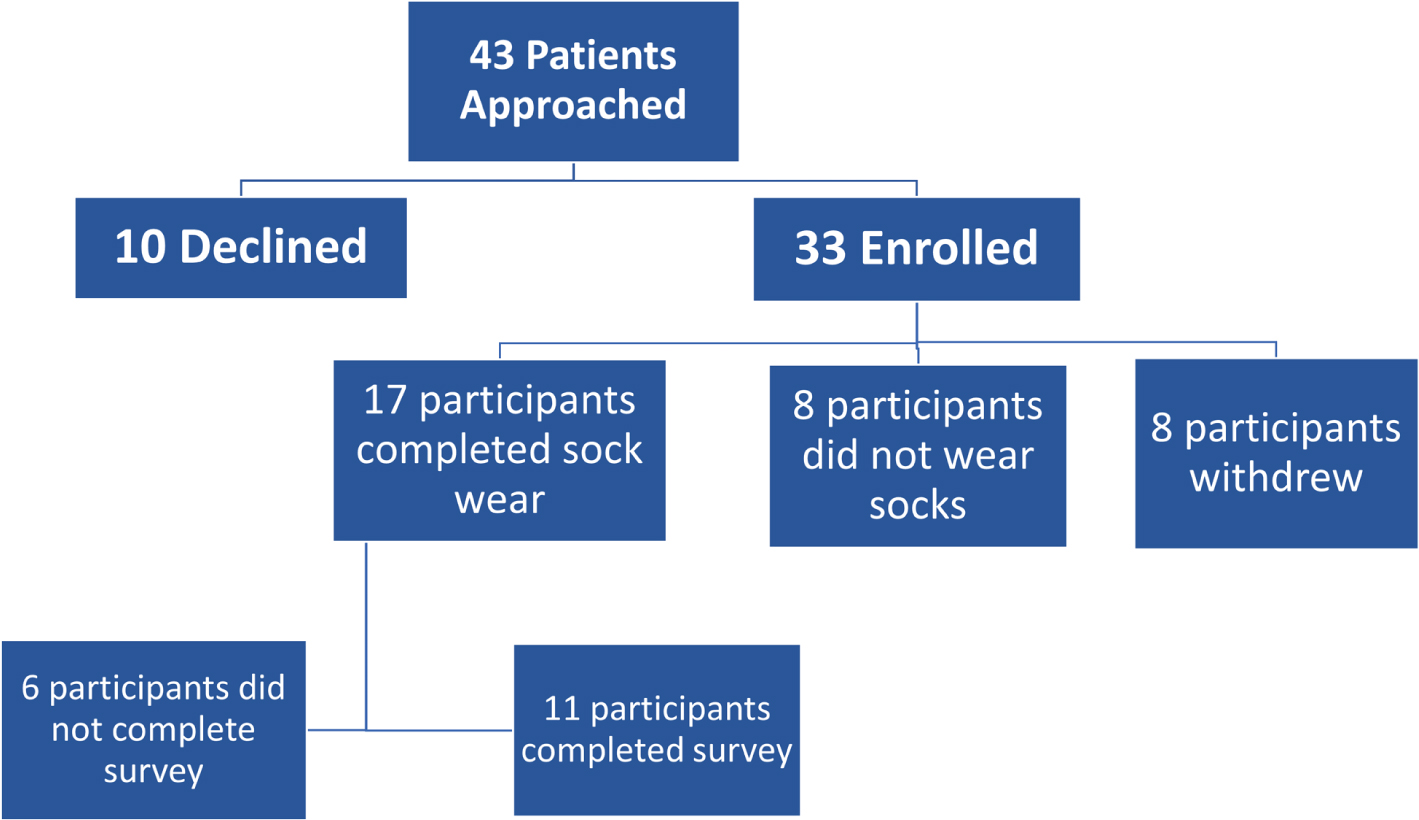
Overall, 33 participants were enrolled in the study; however, eight participants withdrew, and eight participants did not wear the smart socks during the four-week period (Fig. 2). Seventeen participants (51.5%) completed the study by wearing the smart socks. Most participants that did not wear the smart socks did not provide a reason; however, one participant did not wear the smart socks because they were on vacation for the duration of the study, and one participant reported equipment issues. There were no statistically significant differences in age, sex, functional level, brace usage, previous foot pressure injuries, and previous orthopedic surgeries between those who did not wear the socks and those who completed the study. The participants who completed the study wore the socks for a median of 10 days during the four weeks with a median time of 8.3 hours for each day of wear. The duration of wear varied greatly from participant to participant with a range of 14.6 to 595.9 hours.
Fig. 2
Participant flow chart.
3.2Patient demographics
Seventeen participants (eight males, nine females) with a mean age of 14.8 years (range 11–21) completed the study. Thirteen participants (76.5%) identified as Hispanic. Among the 17 participants, SB functional levels were mid/high lumbar (three), low lumbar (three), and sacral (11). Seven participants (41.2%) wore braces, including AFOs, GRAFOs, SMOs, and articulated ankle foot orthoses (AAFOs). Four participants (23.5%) had prior foot pressure injuries, and four (23.5%) had prior orthopedic surgeries on the feet. All participants (100%) were Medi-Cal insured (Table 1).
Table 1
Demographics, N = 33
| Completed | Not Completed | |
| (N = 17) | (N = 16) | |
| Sex: | ||
| Male | 8 (47.1%) | 8 (50%) |
| Female | 9 (52.9%) | 8 (50%) |
| Ethnicity: | ||
| Hispanic | 13 (76.5%) | 14 (87.5%) |
| Non-Hispanic | 2 (11.8%) | 2 (12.5%) |
| Unknown | 2 (11.8%) | 0 (0%) |
| Spina Bifida Level: | ||
| Sacral | 11 (64.7%) | 10 (62.5%) |
| Low Lumbar | 3 (17.7%) | 3 (18.8%) |
| Mid/High Lumbar | 3 (17.7%) | 2 (12.5%) |
| Seen by Wound Care Previously: | ||
| Yes | 4 (23.5%) | 4 (26.7%) |
| No | 13 (76.5%) | 11 (73.3%) |
| Braced: | ||
| Yes | 7 (41.2%) | 7 (50%) |
| No | 10 (58.8%) | 7 (50%) |
| Orthopedic Surgeries on Feet: | ||
| Yes | 4 (23.5%) | 3 (18.8%) |
| No | 13 (76.5%) | 13 (81.2%) |
| Age (years) | 14.8 (2.9) | 13.7 (1.9) |
Values are N (%) or mean (standard deviation).
3.3Sock outcome measures
The median temperatures for the left and right feet were the same: 85.1°F. (Table 2) The median temperature differential between feet was –0.8°F (left –right). The median temperatures differed between SB functional levels with sacral level of lesion having the highest median temperature of 87.2°F in comparison to median temperatures of 82.9°F (low lumbar) and 76.9°F (mid-high lumbar) (p = 0.09) (Fig. 3). While this difference was not statistically significant, there appeared to be a trend. There were no significant differences in temperature or temperature differential based on brace wear, previous orthopedic surgeries, or prior pressure injuries (Table 3). Despite having no significant difference in median temperature, the participants who wore braces included a much smaller range of temperature values compared to a wide distribution of temperature values for participants without braces.
Table 2
Sock data
| Braced (N = 7) | Not Braced (N = 10) | Total (N = 17) | |
| Total Days Worn | 10 (6, 18) | 11.5 (8, 16) | 10 (7, 16) |
| Average Hours Worn per Day | 8.1 (3.9, 10.7) | 8.3 (1.9, 9.7) | 8.3 (3.9, 9.7) |
| Average Temperature Left Foot | 86.1 (82.4, 87.7) | 81.7 (76.6, 86.1) | 85.1 (77.9, 87.3) |
| Average Temperature Right Foot | 86.1 (83.7, 87.5) | 80.8 (77.0, 86.6) | 85.1 (78.9, 87.3) |
| Average Delta (Difference Left –Right) | –0.1 (–2.0, 3.6) | –1.2 (–2.7, 1.0) | –0.8 (–2.2, 1.3) |
| Average Temperature (both feet) | 86.6 (83.4, 87.4) | 82.9 (77.2, 86.7) | 85.1 (77.5, 87.4) |
Values are median (interquartile range).
Fig. 3
Average Temperature (°F) and Spina Bifida Level. Plot of average temperatures for sacral, low lumbar, and mid/high lumbar levels. Median temperatures for sacral, low lumbar, and mid/high lumbar were 87.2°F, 82.9°F, and 76.9°F, respectively.
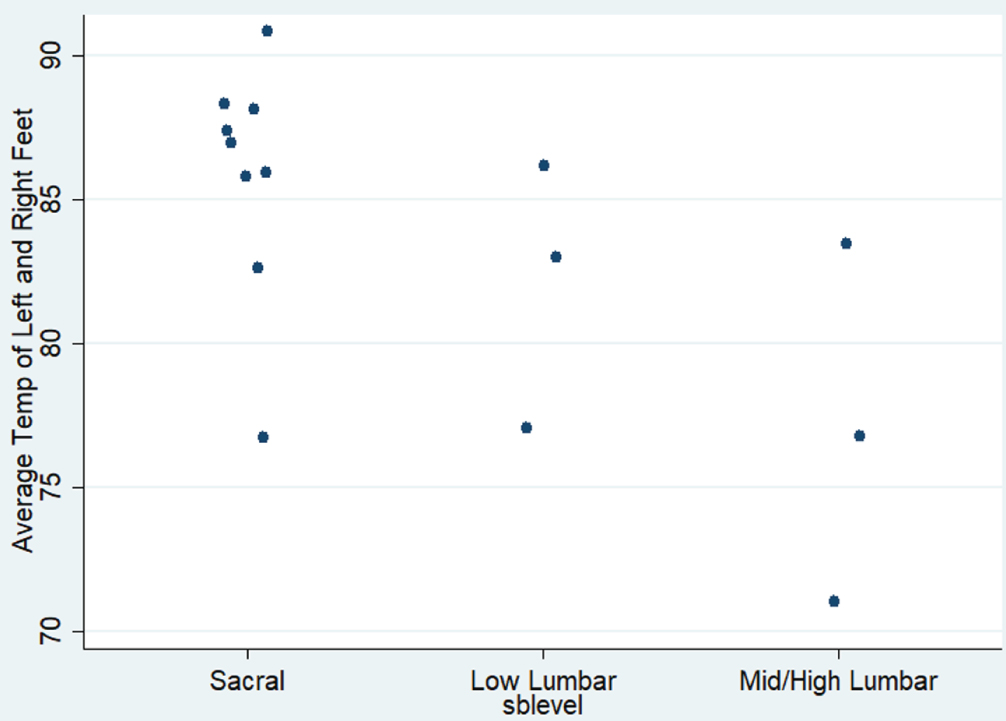
Table 3
Median temperature and differentials
| N | Median temperature | Median differential | |
| (°F) | (°F) | ||
| All | 17 | 85.1 (77.4, 87.4) | –0.8 (–2.2, 1.2) |
| Spina bifida level | |||
| Sacral | 11 | 87.2 (85.1, 88.1) | –1.2 (–2.2, –0.1) |
| Low lumbar | 3 | 82.9 (77.4, 86.6) | 1.2 (0.9, 2.5) |
| Mid-high lumbar | 3 | 76.9 (71.5, 83.4) | –2.1 (–5.8, 0.8) |
| Bracing | |||
| No | 10 | 82.9 (77.2, 86.7) | –1.3 (–2.7, 1.0) |
| Yes | 7 | 86.6 (83.4, 87.4) | –0.2 (–2.0, 3.6) |
| Previous sore | |||
| No | 13 | 85.7 (82.8, 88.1) | –0.8 (–2.2, 2.5) |
| Yes | 4 | 80.5 (77.2, 85.0) | –0.6 (–3.9, 1.1) |
| Prior orthopedic surgeries | |||
| No | 13 | 85.4 (80.1, 87.7) | –0.5 (–1.7, 1.9) |
| Yes | 4 | 83.4 (76.9, 86.6) | –2.1 (–5.8, 0.9) |
| Left foot deformity | |||
| Valgus | 2 | 87.9 (85.1, 90.8) | –1.3 (–1.3, –1.2) |
| Varus | 5 | 85.7 (83.4, 87.2) | –0.8 (–2.0, –0.1) |
| None | 4 | 85.5 (77.2, 88.2) | 1.7 (–0.6, 3.3) |
| Rightfootdeformity | |||
| Valgus | 3 | 85.1 (76.9, 90.8) | –1.3 (–5.8, –1.2) |
| Varus | 5 | 86.6 (83.4, 87.2) | –0.8 (–2.0, –0.1) |
| None | 4 | 85.5 (77.2, 88.2) | 1.7 (–0.6, 3.3) |
Values are median (interquartile range).
3.4Survey outcome measures
Of the 17 participants who wore the smart socks, 11 completed the survey. (Table 4) Nine participants (81.8%) reported that the smart socks were comfortable, very easy to put on, and very soft. Seven (63.6%) reported that the socks were light, with responses of “slightly light” (one), “moderately light” (three), and “very light” (three). The responses varied from “very tight” to “moderately loose” when asked about the fit of the socks. Lastly, patients gave varying responses for the type of shoes worn with the smart socks including none, slippers, and sneakers.
Table 4
Survey results
| Overall comfort, 10 responses | |
| Comfortable | 9 (90%) |
| Slightly Uncomfortable | 1 (10%) |
| Ease of putting on, 11 responses | |
| Very Easy | 9 (82%) |
| Slightly Easy | 1 (9%) |
| Very Difficult | 1 (9%) |
| Softness, 11 responses | |
| Very Soft | 9 (82%) |
| Moderately Soft | 1 (9%) |
| Very Harsh | 1 (9%) |
| Weight, 10 responses | |
| Very Light | 3 (30%) |
| Moderately Light | 3 (30%) |
| Slightly Light | 1 (10%) |
| Neutral | 2 (20%) |
| Slightly Heavy | 1 (10%) |
| Fit, 11 responses | |
| Moderately Loose | 2 (18%) |
| Slightly Loose | 3 (27%) |
| Neutral | 3 (27%) |
| Moderately Tight | 1 (9%) |
| Very Tight | 2 (18%) |
| Temperature comfort, 10 responses | |
| Much Too Warm | 1 (10%) |
| Moderately Warm | 2 (20%) |
| Slightly Warm | 2 (20%) |
| Just Right | 5 (50%) |
| Types of shoes worn with socks, 11 responses | |
| Sneakers | 7 (64%) |
| No Shoes or Slippers | 4 (36%) |
Values are N (%).
4Discussion
This study was the first to look at the application of wearable continuous temperature monitoring socks in adolescents and young adults with SB. Pedal temperature in this population is not well established. This study was underpowered by the small sample size and therefore no differences in median temperature or median temperature differences could be detected. Those with higher SB functional levels tended to have lower mean foot temperatures compared to those with lower-level lesions. This may be related to circulation issues as one study reported increased duration of retrograde flow and venous insufficiency in children with myelomeningocele compared to typically developing children [7]. A lower temperature in the lower extremities of less ambulatory persons could be an alternate explanation. In the diabetic neuropathic population, more active persons tended to have higher foot temperatures compared to those who were less active [4, 6]. More studies to establish baseline temperature standards in those with SB are needed to further understand these findings.
Another finding to highlight was the role of braces in interpreting temperature metrics. In a prior study, brace wear was identified as a risk factor for development of pressure injuries [1]. Those with braces tended to have less temperature variability, higher median temperatures, and larger temperature differences between feet. Less variability and higher temperatures are potentially related to the fact that those who wore braces typically wore them with socks and shoes, adding material that might retain heat and increase temperature; comparatively, those without braces may have worn socks only or socks with closed or open toe shoes, which could impact the temperature variability seen. Braces may contribute to both temperature and pressure differences that can result in the development of pressure injuries.
History of prior pressure injuries was noted for four of the participants: two mid-lumbar and two low lumbar. Most participants were at the sacral functional level, which could mean they were at less risk of developing pressure injuries. This may be related to the fact that adolescents and young adults with sacral level function often do not wear braces, which is a risk factor for pressure injury formation. Conklin et al. reported that the diagnosis of myelomeningocele and thoracic and lumbar levels were independent risk factors for skin breakdown in the foot [8]. Deshpande et al. found that ambulatory SB patients with lower extremity pressure injuries were at significantly higher risk of requiring an amputation than patients who did not walk [9]. In their cohort, all patients wore braces and, of the 11 patients, four had sacral and seven had lumbar functional level. Additionally, more information is needed on the pathophysiology of pressure injuries in SB and whether it is mainly pressure or temperature related.
Reyzelman et al. reported similar user experience findings in their study looking at temperature sensing sock wear in the adult, diabetic neuropathic population [6]. They reported a similar wear time of 3–21 hours a day with a median of seven hours, compared with this study which reported 2–21 hours per day with a median duration of eight hours. This cohort reported overall high satisfaction with the socks among those who tried them. In the adolescent and young adult population, for whom adherence can be an issue, this finding is important to highlight.
This study had several limitations. It is recognized that almost 50% of those who enrolled in the study never wore the socks, indicating that adherence to sock wear was an issue. Linquist et al. reported that people with SB have executive dysfunction which can significantly impact activities of daily living and autonomy [10]. This can contribute to barriers to participation. Hydrocephalus has been shown to be an important risk factor for intellectual difficulties [11]. In this cohort, 27% (9/33) of enrolled participants had underlying hydrocephalus, which could contribute to the multi-faceted issues related to challenges with adherence.
The sample mainly consisted of patients who had no history of prior pressure injuries (24%), which have been found in other studies to be a major risk factor for developing additional pressure injuries [8]. The current design of the socks used is structurally limited for young people with SB. The lateral tag is a barrier to use in those who wear the most common type of braces. The feedback obtained from this study may inform more appropriate designs by adjusting the position of the lateral tag in future studies. Additionally, although the location of prior injuries requiring wound care consultation was primarily on the heel, some pressure injuries develop outside of the area covered by the sock sensors, which are only plantar-based, including the dorsal foot and lateral malleoli. Finally, patients were followed for a relatively short duration of time, only one month, compared to other studies that followed patients for six months or more to allow for the development of a clinically significant pressure injury [4, 6].
5Conclusions
This study was the first to explore the use of wireless continuous temperature monitoring for home use in adolescent patients with SB. Participants rated the socks favorably. When worn, the socks were able to consistently measure temperature data, indicating that those most at risk for pedal pressure injuries in the SB population could benefit by wearing these socks, with some modifications. While there was no clinical correlation to development of active pressure injuries detected during this short-term pilot study, this technology has the potential to be explored further in this vulnerable population. Future directions should include increasing sample size, obtaining normative data for temperature ranges in SB, and correlating to clinical outcomes and other measures such as pedobarography that may help to detect risk in the development of foot pressure injuries.
Acknowledgments
The authors acknowledge Maia Hauschild and the Spina Bifida Clinic Team for contributions to this study.
Conflict of interest
The authors have no conflict of interest to report. Siren Care, Inc donated the socks used but were not directly involved in this study.
Ethical considerations
This study has been carried out with approval from the Institutional Review Board at Children’s Hospital Los Angeles #CHLA-21-00127.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
[1] | Rethlefsen S , Mueske N , Wren T , Murgai R , Bent M . The prevalence and risk factors for foot pressure ulcers in ambulatory pediatric patients with spina bifida. Disabil Rehabil. (2021) ;43: (9):1287–91. doi: 10.1080/09638288.2019.1660915. |
[2] | Kim S , Ward E , Dicianno BE , et al. Factors associated with pressure ulcers in individuals with spina bifida. Arch Phys Med Rehabil. (2015) ;96: (8):1435–41.e1. doi: 10.1016/j.apmr.2015.02.029. |
[3] | Graham L . Spina bifida and lower limb amputation in Northern Ireland: A retrospective study of demographics and outcome. Prosthet Orthot Int.. (2017) ;41: (5):503–6. doi: 10.1177/0309364616683820. |
[4] | Najafi B , Mohseni H , Grewal GS , Talal TK , Menzies RA , Armstrong DG . An Optical-Fiber-Based Smart Textile (Smart Socks) to Manage Biomechanical Risk Factors Associated With Diabetic Foot Amputation. J Diabetes Sci Technol. (2017) ;11: (4):668–77. doi: 10.1177/1932296817709022. |
[5] | Lavery LA , Higgins KR , Lanctot DR , et al. Home monitoring of foot skin temperatures to prevent ulceration. Diabetes Care. (2004) ;27: (11):2642–7. doi: 10.2337/diacare.27.11.2642. |
[6] | Reyzelman A , Shih C , Tovmassian G , et al. An Evaluation of Real-world Smart Sock–Based Temperature Monitoring Data as a Physiological Indicator of Early Diabetic Foot Injury: Case-Control Study. JMIR Form Res.e0. (2022) ;6: (4):e31870. doi: 10.2196/31870. |
[7] | Domagalska-Szopa M , Szopa A , Puchner M , et al. Leg Venous Properties in Children With Myelomeningocele. Front Pediatr.. (2020) ;8: :531. doi: 10.3389/fped.2020.00531. |
[8] | Conklin MJ , Hopson B , Arynchyna A , Atchley T , Trapp C , Rocque BG . Skin breakdown of the feet in patients with spina bifida: Analysis of risk factors. J Pediatr Rehabil Med.. (2018) ;11: (4):237–41. doi: 10.3233/PRM-170520. |
[9] | Deshpande S , Gormley C , Gormley ME . Acquired amputations in patients with spina bifida. J Pediatr Rehabil Med.. (2022) ;15: (4):615–20. doi: 10.3233/PRM-210032. |
[10] | Lindquist B , Jacobsson H , Strinnholm M , Peny-Dahlstrand M . A scoping review of cognition in spina bifida and its consequences for activity and participation throughout life. Acta Paediatr. (2022) ;111: (9):1682–94. doi: 10.1111/apa.16420. |
[11] | Vachha B , Adams R . Language differences in young children with myelomeningocele and shunted hydrocephalus. Pediatr Neurosurg. (2003) ;39: (4):184–9. doi: 10.1159/000072469. |




