The role of ultrasound in pediatric rehabilitation
Dear colleagues,
Pediatric Rehabilitation Medicine, a specialized branch of Physical Medicine and Rehabilitation (PM&R), integrates traditional medical rehabilitation expertise. It primarily addresses temporary or lifelong disability conditions that stem from developmental, congenital, or childhood-acquired origins across all ages. Its core aim is to enhance function and encourage active participation in daily life [1].
The integration of ultrasound (US) into PM&R has significantly transformed the approach of physiatrists and pediatric rehabilitation specialists in diagnosing and treating a broad spectrum of musculoskeletal disorders. Hence, this editorial aims to spotlight the role of US in pediatric rehabilitation, particularly emphasizing its scarcity in this field and encouraging researchers focused on pediatric musculoskeletal disorders and rehabilitation to contribute to the Journal of Back and Musculoskeletal Rehabilitation (JBMR) [2].
In pediatric rehabilitation, US serves as a pivotal tool for navigational assistance during botulinum toxin injections and nerve blocks to manage spasticity [3]. Additionally, it facilitates US-guided botulinum toxin administration for managing drooling [2]. Furthermore, using neuromuscular US, a painless and swift assessment method in the pediatric population, stands out alongside established electrodiagnostic methods. The diagnostic approach to neuromuscular pathologies has undergone a significant evolution. Electrodiagnostic methods, including nerve conduction studies and electromyography, play an essential role in clinical decision-making by providing basic neurophysiological information. Complementing these established modalities, neuromuscular US has emerged as a valuable adjunctive tool for both adult and pediatric populations, especially for pediatric populations [4]. Specifically, the challenge lies in children’s reduced capacity to endure pain and discomfort, potentially restricting a thorough assessment during electroneuromyography (ENMG). Practically, conducting US scans before ENMG is quick and pain-free. US findings may be helpful in guiding the next steps for taking samples from nerves and muscles during ENMG testing [4]. For example, in a patient with toe walking and pes cavus during an investigation of etiology, nerve US can be helpful before performing nerve conduction studies and needle electromyography. Like ENMG studies, it can be used as an extension of physical examination [5]. Both myopathic and neuropathic disorders can cause increased muscle echo density (i.e., a muscle appears whiter). In neurogenic disorders, however, nerve changes such as increased cross-sectional area and loss of normal fascicular architecture accompany increased muscle echogenicity [6]. Typically, Charcot-Marie-Tooth disease displays consistent enlargement across all nerves [4]. US can be helpful in identifying carpal tunnel syndrome in mucopolysaccharidoses. Neuromuscular US does not cause pain or discomfort, making it an appealing choice for pediatric patients who cannot actively participate in ENMG testing or are hard to tolerate. In pediatric rehabilitation, US can also be used to evaluate and examine peripheral nerve injuries caused by injury (e.g., penetrating trauma, traction) and iatrogenic injury [7]. A good example of this is the assessment of nerve injuries after a supracondylar fracture of the humerus, which is a common childhood injury and the most common elbow fracture seen in children. Traumatic or iatrogenic nerve injuries (e.g., related to pinning) are one of the frequent complications that are observed related to supracondylar fractures and their treatment. Nerve injuries following supracondylar humeral fractures predominantly result from nerve compression or trapping against the sharp proximal humeral fragment. Additionally, iatrogenic injuries may arise during closed manipulation or percutaneous fixation of the fracture fragments and sometimes during open procedures [8]. Managing a closed injury coupled with peripheral nerve palsy remains a subject of debate. Spontaneous recovery rates are high, prompting a watchful waiting approach for nerve palsy. If no improvement shows after about four months, ENMG is conducted. However, prolonged waiting is not viable as nerve tissue and muscles lose their regrowth capacity over time. Identifying patients for early surgical intervention becomes crucial due to the direct relation between preoperative time and nerve repair outcomes. ENMG assessment might not always offer sufficient details regarding the precise location or type of nerve damage [9]. For example, pathologic findings can be found in muscles innervated by the anterior interosseous nerve (AIN) rather than all muscles innervated by the median nerve main trunk in relation to supracondylar fossa in electromyographic evaluation. The affected nerve area may be perceived as more distal on electromyography, even if it is more proximal. However, the fascicles of the AIN can be affected by direct contusion by the free edge of the proximal fracture fragment, where the AIN is still in the nerve before exiting the median nerve. In this situation, anatomical information can be obtained by US nerve tracing, and physiologic information (such as the stage, degree, and type of nerve injury) can be obtained by ENMG examinations. Also, nerves can be buried in the fracture callus at the fracture site, or pins may irritate the nerves, which can be visualized by US. Preoperative US can offer details about nerve continuity or the extent of nerve damage post-injury when paired with neurophysiological assessments.
US can also be used to evaluate the stump for pain in pediatric amputations. Bony overgrowth is the most common complication in skeletally immature children. Screening and visualizing bony overgrowth or spurs can be achieved using US without radiation exposure [10].
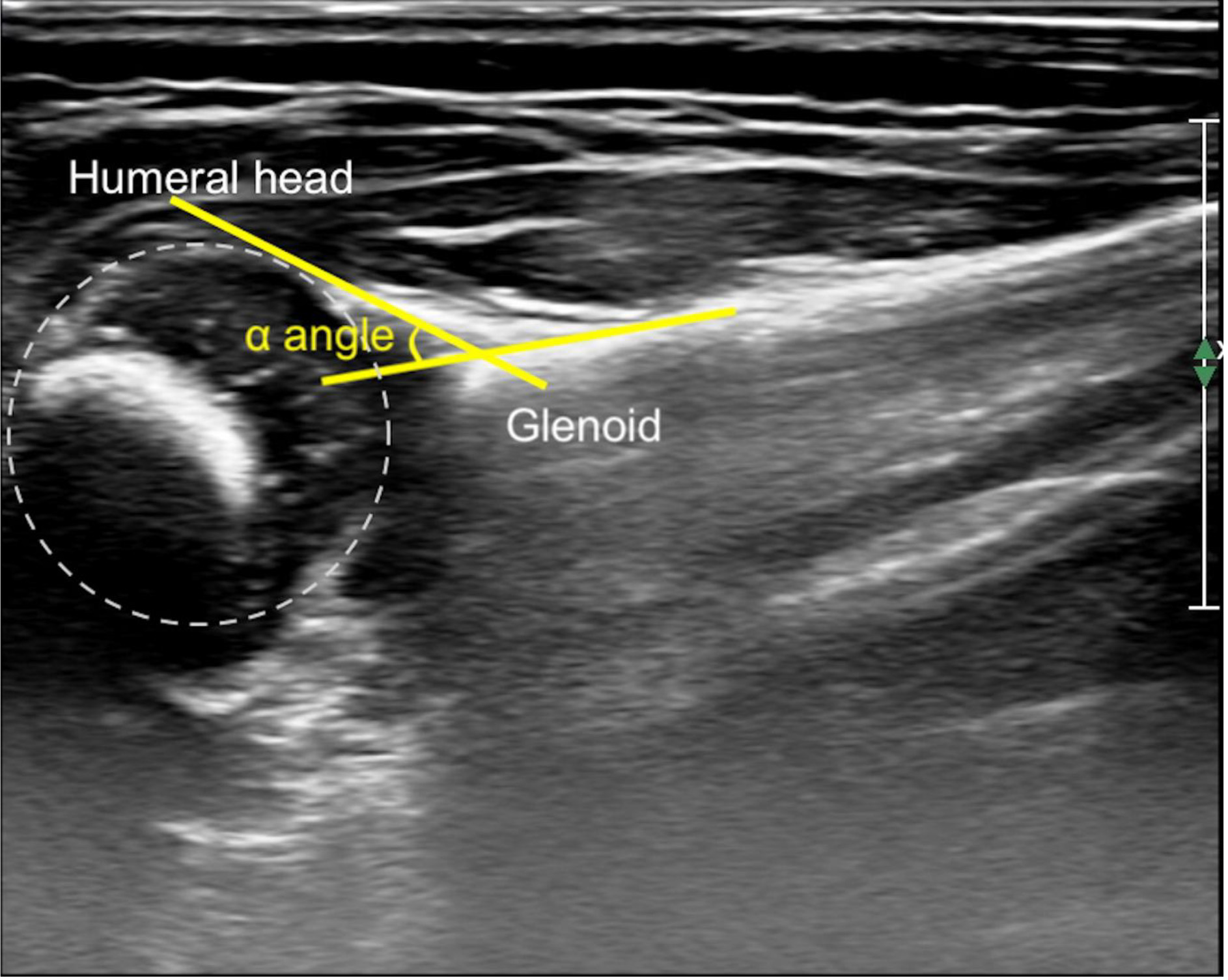
Another situation where US is used in pediatric rehabilitation is the follow-up of the shoulder in neonatal brachial plexus palsy [11]. Due to an imbalance between the strength of the relatively unaffected internal rotators and the paralytic external rotator, internal rotation contracture of the shoulder occurs. The dominance of an internally rotated position negatively affects the shoulder’s growth. If left untreated, internal contracture of the diseased shoulder commonly leads to glenohumeral deformity (i.e., glenohumeral dysplasia, posterior humeral head subluxation). This deformity has been noted to be progressive with age and appears early in infancy [12]. Glenohumeral dysplasia typically emerges within the initial year of a child’s life and can manifest as early as three months in cases of NBPP. The dysplasia initiates with glenohumeral subluxation, where the humeral head gradually moves backward out of its normal position within the glenoid. Clinical indicators, such as reduced passive external rotation range of motion, serve as cues for detecting glenohumeral subluxation. However, US examinations have demonstrated the ability to detect subluxation even in the absence of these clinical signs as early as three months of age [13]. Detecting infantile glenohumeral dysplasia associated with NBPP at an early stage is crucial for effective management. Early identification allows for prompt intervention to minimize the effects on the glenohumeral joint, promoting a more natural shoulder development by preventing or reducing permanent skeletal changes. This could also potentially reduce the necessity for more complex shoulder surgeries later on [11]. The alpha angle and percentage of the humeral head displaced posterior to the axis of the scapula are calculated and followed up for this purpose (Fig. 1) [14].
Figure 1.
Ultrasound image of an affected shoulder of an infant with neonatal brachial plexus palsy. The
Pediatric musculoskeletal problems are among the most common disorders in pediatric rehabilitation practice. In a child presenting with arthralgia, in diagnostic work-up, still based on clinical examination, US can be beneficial for differential diagnosis of noninflammatory conditions like overload syndromes (e.g., Osgood Schlatter disease, jumper’s knee) and inflammatory conditions. The use of US allows for confirming the diagnosis in case of doubt and better characterizing the inflammatory involvement of the joint structures, ultimately helping to define the disease extension [15, 16, 17]. For example, US is the first choice as it is an easy and fast way to assess a child presenting with knee pain. Depending on the course of Osgood Schlatter disease, the presence of a hypoechoic zone superficial to the apophysis of the anterior tibial tubercle representing pretibial cartilaginous swelling with forward displacement of the subcutaneous tissues and elevation of the patellar tendon from the tibial outline, fragmented and hypoechoic ossification center, diffuse thickening of the insertion portion of the patellar tendon, fluid collection in the retrotendineal soft tissues representing infrapatellar bursitis can be visualized on the US (Fig. 2) [18]. In case of jumper’s knee, US examinations commonly reveal changes in the patellar tendon structure where it connects to the bone such as thickening and a hypoechoic area at the proximal part of the patellar tendon and that the presence of neovascularization can be demonstrated by color Doppler US (Fig. 2) [17, 19]. When evaluated together with clinical assessment, synovial thickening, synovial effusion, and power Doppler (active synovitis) presence may support the diagnosis of juvenile idiopathic arthritis. Enthesis can be considered depending on the presence or absence of the entheseal changes of hypoechogenicity, thickening, enthesophyte, erosions, and Doppler signal at enthesis sites including achilles tendon, quadricipital tendon, and distal insertion of the patellar ligament [15, 20, 21].
Figure 2.
A. Evaluation of the attachment site of the patellar tendon to the tibial tuberosity on the left and right sides in Osgood-Schlatter disease. The left patellar tendon was measured to be thicker than the right side (5.23 mm vs. 4.83 mm). Cortical irregularity in the tibial tuberosity is notable bilaterally (asterisk). B. Ultrasound image of a patient’s knee with Jumper’s knee showing thickening and a hypoechoic area at the proximal part of the patellar tendon [16].
![A. Evaluation of the attachment site of the patellar tendon to the tibial tuberosity on the left and right sides in Osgood-Schlatter disease. The left patellar tendon was measured to be thicker than the right side (5.23 mm vs. 4.83 mm). Cortical irregularity in the tibial tuberosity is notable bilaterally (asterisk). B. Ultrasound image of a patient’s knee with Jumper’s knee showing thickening and a hypoechoic area at the proximal part of the patellar tendon [16].](https://content.iospress.com:443/media/bmr/2024/37-3/bmr-37-3-bmr245002/bmr-37-bmr245002-g002.jpg)
To sum up, US provides high-resolution imaging of joints, tendons, ligaments, muscles and nerves in the pediatric population and has numerous applications in the broad field of Pediatric Rehabilitation Medicine. While the utilization of US increases throughout Pediatric Rehabilitation Medicine, appropriate clinical applications must continue to be searched. We, therefore, actively welcome new studies on US in the rehabilitation of pediatric musculoskeletal disorders.
I’m humbled and grateful to write the Guest Editorial for this issue of JBMR. Deniz et al. have been awarded the free to read Editor’s Choice article for their study, which examined disparities in sagittal-frontal posture during upright standing and stiffness of superficial postural muscles in adolescent boys with haemophilia compared to age-matched peers [22]. Their aim was to explore the effects of muscle stiffness and joint health on posture in haemophilia. We congratulate the authors on their significant contributions to the field of pediatric musculoskeletal rehabilitation research, as their work illuminates the assessment and rehabilitation of haemophilia, which is an important rare disease.
On behalf of the editorial board, I hope you enjoy reading this issue!
Esra Giray
Conflict of interest
In the interest of full transparency, I declare that I have no conflicts of interest in presenting this editorial and that I approach this as an independent researcher dedicated to advancing the field of pediatric rehabilitation.
References
[1] | Turk MA, Gans BM, Kim H, Alter KE. A call for action: Increasing the pediatric rehabilitation medicine workforce. Journal of Pediatric Rehabilitation Medicine. (2023) (Preprint): 1-7. |
[2] | Kim H, Lee Y, Weiner D, Kaye R, Cahill AM, Yudkoff M. Botulinum toxin type a injections to salivary glands: combination with single event multilevel chemoneurolysis in 2 children with severe spastic quadriplegic cerebral palsy. Arch Phys Med Rehabil. (2006) ; 87: (1): 141-4. |
[3] | Giray E, Karadağ-Saygı E, Yağı İ. Ultrasound and electromyography and electrical stimulation-guided botulinum toxin injection of salivary glands for drooling: A case report with a description of the technique. Turk J Phys Med Rehabil. (2021) ; 67: (1): 120-1. |
[4] | VanHorn TA, Cartwright MS. Neuromuscular Ultrasound in the Pediatric Population. Diagnostics (Basel). (2020) ; 10: (12). |
[5] | Preston DC, Shapiro BE. Electromyography and neuromuscular disorders e-book: clinical-electrophysiologic-ultrasound correlations: Elsevier Health Sciences. (2020) . |
[6] | Pillen S, van Alfen N. Skeletal muscle ultrasound. Neurol Res. (2011) ; 33: (10): 1016-24. |
[7] | Vanderhave KL, Brighton B, Casey V, Montijo H, Scannell B. Applications of musculoskeletal ultrasonography in pediatric patients. J Am Acad Orthop Surg. (2014) ; 22: (11): 691-8. |
[8] | Ramachandran M, Birch R, Eastwood DM. Clinical outcome of nerve injuries associated with supracondylar fractures of the humerus in children: the experience of a specialist referral centre. J Bone Joint Surg Br. (2006) ; 88: (1): 90-4. |
[9] | Lee J, Bidwell T, Metcalfe R. Ultrasound in pediatric peripheral nerve injuries: can this affect our surgical decision making? A preliminary report. J Pediatr Orthop. (2013) ; 33: (2): 152-8. |
[10] | Subedi N, Heire P, Parmer V, Beardmore S, Oh C, Jepson F, et al. Multimodality imaging review of the post-amputation stump pain. Br J Radiol. (2016) ; 89: (1068): 20160572. |
[11] | Verchere C, Durlacher K, Bellows D, Pike J, Bucevska M. An early shoulder repositioning program in birth-related brachial plexus injury: a pilot study of the Sup-ER protocol. Hand (N Y). (2014) ; 9: (2): 187-95. |
[12] | Pearl ML. Shoulder problems in children with brachial plexus birth palsy: evaluation and management. J Am Acad Orthop Surg. (2009) ; 17: (4): 242-54. |
[13] | Osorio M, Lewis S, Tse RW. Promoting recovery following birth brachial plexus palsy. Pediatr Clin North Am. (2023) ; 70: (3): 517-29. |
[14] | Bauer AS, Lucas JF, Heyrani N, Anderson RL, Kalish LA, James MA. Ultrasound screening for posterior shoulder dislocation in infants with persistent brachial plexus birth palsy. J Bone Joint Surg Am. (2017) ; 99: (9): 778-83. |
[15] | Borocco C, Anselmi F, Rossi-Semerano L. Contribution of ultrasound in current practice for managing juvenile idiopathic arthritis. J Clin Med. (2022) ; 12: (1). |
[16] | Esra G, İlleez ÖG, Ercişli AK, Akpınar P, Sözeri B, Özkan FÜ, et al. Ön Diz Ağrısı ile Başvuran Çocuk Hastada Pediatrik Kas-İskelet Sistemi Ultrasonografisinin Tanıya Katkısı. J PMR Sci. (2022) ; 25: (3). |
[17] | Draghi F, Danesino GM, Coscia D, Precerutti M, Pagani C. Overload syndromes of the knee in adolescents: Sonographic findings. J Ultrasound. (2008) ; 11: (4): 151-7. |
[18] | Blankstein A, Cohen I, Heim M, Diamant L, Salai M, Chechick A, et al. Ultrasonography as a diagnostic modality in Osgood-Schlatter disease. A clinical study and review of the literature. Arch Orthop Trauma Surg. (2001) ; 121: (9): 536-9. |
[19] | Suzue N, Matsuura T, Iwame T, Higashino K, Sakai T, Hamada D, et al. State-of-the-art ultrasonographic findings in lower extremity sports injuries. J Med Invest. (2015) ; 62: (3-4): 109-13. |
[20] | Vega-Fernandez P, Rogers K, Sproles A, Thornton S, Huggins J, Lovell DJ, et al. Diagnostic accuracy study of the pediatric-specific ultrasound scoring system for the knee joint in children with juvenile idiopathic arthritis. Arthritis Care Res (Hoboken). (2023) . |
[21] | Mosa DM, Abdelrahman AM, El-Bahnasawy ASJR. Ultrasound features across subtypes of juvenile idiopathic arthritis. (2022) ; 2: (1): 2-14. |
[22] | Deniz V, Güzel NA, Kelle B, Antmen AB. Comparison of posture and muscle stiffness between adolescent boys with haemophilia and age-matched healthy peers: An observational comparative study. J Back Musculoskelet Rehabil. (2024) ; 37: (4). |




