The efficacy of ultrasonography-guided oxygen-ozone therapy versus corticosteroids in patients with knee osteoarthritis: A multicenter randomized controlled trial
Abstract
BACKGROUND:
Osteoarthritis (OA) is a widely-known disease distinguished by the breakdown of joint cartilage, leading to pain and morning stiffness. In this context, the role of corticosteroids is well known, but there is still a gap of knowledge on the duty of oxygen-ozone therapy (O2-O3).
OBJECTIVE:
To evaluate for effectiveness of ultrasound-guided O2-O3 injections compared with corticosteroid injections among patients diagnosed with knee OA.
METHODS:
This randomized controlled clinical trial was conducted on participants with knee OA who were randomly sorted into two groups: group A, undergoing corticosteroid group (
RESULTS:
Ninety-six participants completed this study. Based on repeated measurement analysis of variance, a significant effect of time was found for all outcome measures in both groups. Both groups showed clinically significant improvements in knee pain, quality of life and, function. Baseline, 4-week post-injection and 12-week post-injection WOMAC scores (mean
CONCLUSION:
The study demonstrates the efficacy of O2-O3 compared to steroid injections regarding functioning and pain relief among patients with diagnosed knee OA.
1.Introduction
Knee osteoarthritis (OA) is a ubiquitous leisurely progressive complaint in which diminished capacity is resulting in pain and increased joint limitation [1]. Global occurrence of knee OA has been approximated to 3.8% [2]. Radiographic evidence indicative of knee OA is identified in approximately 19% of the Framingham adult population aged 50–60 years [3]. Individuals diagnosed with knee OA customarily demonstrate tenderness, pain, loss of flexibility, grating sensation, and crepitus inside their joints. Diagnosis is fundamentally derived from this clinical presentation, accompanied by incorporating radiological imaging modalities.
Non-surgical treatment of KOA commonly includes pharmacological therapy, nutraceuticals, physical therapy, physical agent modalities, intra-articular injections of hyaluronic acid (HA), corticosteroids, and oxygen-ozone therapy (O2-O3) [4, 5, 6]. The latter consists of a concoction of oxygen and ozone and can enhance cellular oxygenation and expedite the development of reactive oxygen species, and thereby could attenuate the secretion saof proinflammatory cytokines, which frustrates the activation and thus regains the symptoms of knee OA [7]. In this context, previous studies suggested promising effects of oxygen and ozone injections contrast to HA injection in patients with knee OA [8, 9].
Taken together, these findings underline that there is still insufficient knowledge concerning the effectiveness of oxygen and ozone in improving symptoms of partipicants diagnosed with knee OA. Thus, the primary objective of this study was to investigate the efficacy of ultrasound-guided O2-O3 injections with corticosteroid injections in terms of functioning in the cohort of subjects characterized by knee OA. The study hypothesized that ozone therapy will be effective on pain and the functions of patients with knee OA in long-term follow-ups.
2.Methods
2.1Study design
This randomized trial was conducted following the CONSORT guidelines [10]. All study procedures were conducted according to the ethical principles derived from the Declaration of Helsinki and the study researchers guarantee the privacy of all study participants. Before study initiation, the study protocol was submitted to the clinical trial registry under number NCT04830423. The study protocol and design were approved by the Duzce University Ethics Committee (approval number: 2020-7-4) and informed consent was obtained from all participants.
2.2Participants
Inclusion criteria: (1) Knee OA following the criteria established by the American College of Rheumatology; (2) grade I, II , and III based on Kellgren-Lawrence classification system; (3) knee pain persists for more than 6 months; and (4) people aged 40–75. Exclusion criteria: (1) Individuals diagnosed with inflammatory arthritis (Rheumatoid arthritis, connective tissue disease, crystal arthropathies) (2) participants include individuals with a documented history of trauma or knee operations; (3) history of any infection and malignancy; (4) pregnancy; (5) patients who have undergone knee injections within the last three months; (6) uncontrolled diabetes or consumption of anticoagulants; (7) insufficient G6PD, uncontrolled hyperthyroidism, or leukemia.
A physical medicine and rehabilitation specialist, who was unaware of the treatment assignments, conducted both the physical examinations and medical history assessments.
2.3Baseline assessment
Participants in the research took part in a baseline visit at which the following procedures were performed: medical records (age, gender, body mass index), physical examination of knee, evaluation of knee radiographs and application of the following assesment surveys: Visual Analogue Scale (VAS) [11], Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) [12, 13].
The measurement of active flexion knee range of motion (ROM) was conducted with patients in a prone posture, maintaining a neutral hip position. A goniometer was utilized, with its axis positioned on the lateral part of the knee joint. An ultrasound examination was carried out to evaluation effusion by scanning the region over the supra-patellar recess. The ultrasonographic evaluations were carried out employing a 5–12 MHz curvilinear transducer (Logice portable; GE Healthcare, China), administered by the same physiatrist with a decade of experience in musculoskeletal ultrasonography.
Patients were positioned in a supine posture, with their knees flexed at 20∘ and underpinned by a rolled towel. Initially, the transducer was longitudinally placed on the quadriceps muscle and tendon and the suprapatellar recess was demonstrated, situated between the pre-femoral fat-pad posteriorly and the quadriceps tendon and suprapatellar fat-pad at the anterior edge, presenting as a hypoechoic or anechoic fluid-containing area through high-frequency ultrasound.
2.4Randomization
Individuals who fulfilled the inclusion criteria were randomized into two groups with a computer-assisted program. This concluded in groups with evenly distributed samples and balanced distribution of important controlled variables (age, gender, timeframe of knee pain). The physician who evaluates the results after treatment; was blinded from data analysis and which group the participants were in.
Participicants diagnosed with knee OA who met the study participation criteria were randomized into two groups: group A received corticosteroids and group B received oxygen–ozone injection. With the objective of avoiding selection bias, all included participants were sequentially assigned to the oxigen-ozone group or corticosteroid group by a predetermined method. An independent physiatrist that evaluated the implications did not know which group the patients were distributed to. The participants and the physiatrist that administered the injection were not blinded to group allocation due to the inherent nature of the interventions (liquid versus gas).
2.5Intervention
Injections in both groups were performed under US guidance (with a 5–12 MHz linear transducer [Logic e portable; GE Healthcare, Jiangsu, China]) by the same physiatrist. The injections were administered into the femorotibial articular interline 1.5 cm laterally to the patellar tendon and 1.5 cm below the apex of patella with an in-plane superolateral approach, mixture of 1 mL corticosteroid (betamethasone 3 mg/mL) and 1 ml of 2% lidocaine solution (without vasoconstrictor) in the corticosteroid injection group. Three sessions (1 session/week) of 10 mL of ozone (O2-O3) (with a concentration of 10
Prior to the injection, all patients received instructions to engage in quadriceps muscle strengthening exercises. Each participant was supplied written instructions these exercises, which included, hamstring stretch, seated hip march, and quad sets. They were instructed to perform these exercises ten times, three times per day over the study period. Following the injection, patients were advised to apply a cold pack to the knee for a duration of 5 to 10 minutes. This cold pack application could be repeated three to four times a day. After the knee injection, patients were advised to avoid making efforts for at least 24 hours.
2.6Outcome measures
The primary endpoint parameter was the change in the WOMAC score between the pre-treatment and 12-weeks post-treatment. Secondary endpoint parameter enrolled the VAS at rest and activity scores. Observations were recorded at pre-treatment and at 4-weeks and 12-weeks post-treatment. Patients were questioned for side effects at each assessment. A self-conducted assessment, tool, the WOMAC, has been used for knee ostheoarthritis [13]. The WOMAC is frequently employed in the evaluation of hip and knee OA [12]. It is a self-conducted questionnaire consisting of three subscales: Pain, Stiffness and Physical Function. Turkish validity and reliability study was conducted [13].
For the VAS, patients were asked to circle the number between 0 and 10 that fits best to their pain intensity. Pain affliction was determined using the standard 10 cm (at rest, at motion and at night) [11].
The mentioned indices were reassessed based on the study criteria at the baseline, as well as at one month and three months afterward, with the evaluations being conducted by an investigator who was blinded to the study. At the 3rd month follow-up, the patients’ joint ROM and the presence of effusion in the joint were evaluated with ultrasonography.
2.7Statistical analysis
Sample size calculation was performed with GPower software. Based on Choi et al., a potency of 0.80 with an alpha of 0.05 and accounting for 10% dropout, a subset of 96 participants was sufficient to detect a 15% difference in the change in VAS between control and RF group respectively (baseline-1 week: 33.7
SPSS version 25 was used to analyse data, using descriptive statistics including means and standard deviations where applicable. Preliminary evaluation involved subjecting the data to a Shapiro-Wilk test to assess the normality of its distribution. Results indicated non-significance, affirming the data’s adherence to a normal distribution. Continuous data were represented by the mean
Nominal data were subjected to analysis using the Pearson
The primary outcome (WOMAC) displayed a normal distribution, thereby warranting employment of the independent samples
3.Results
Figure 1.
CONSORT diagram.
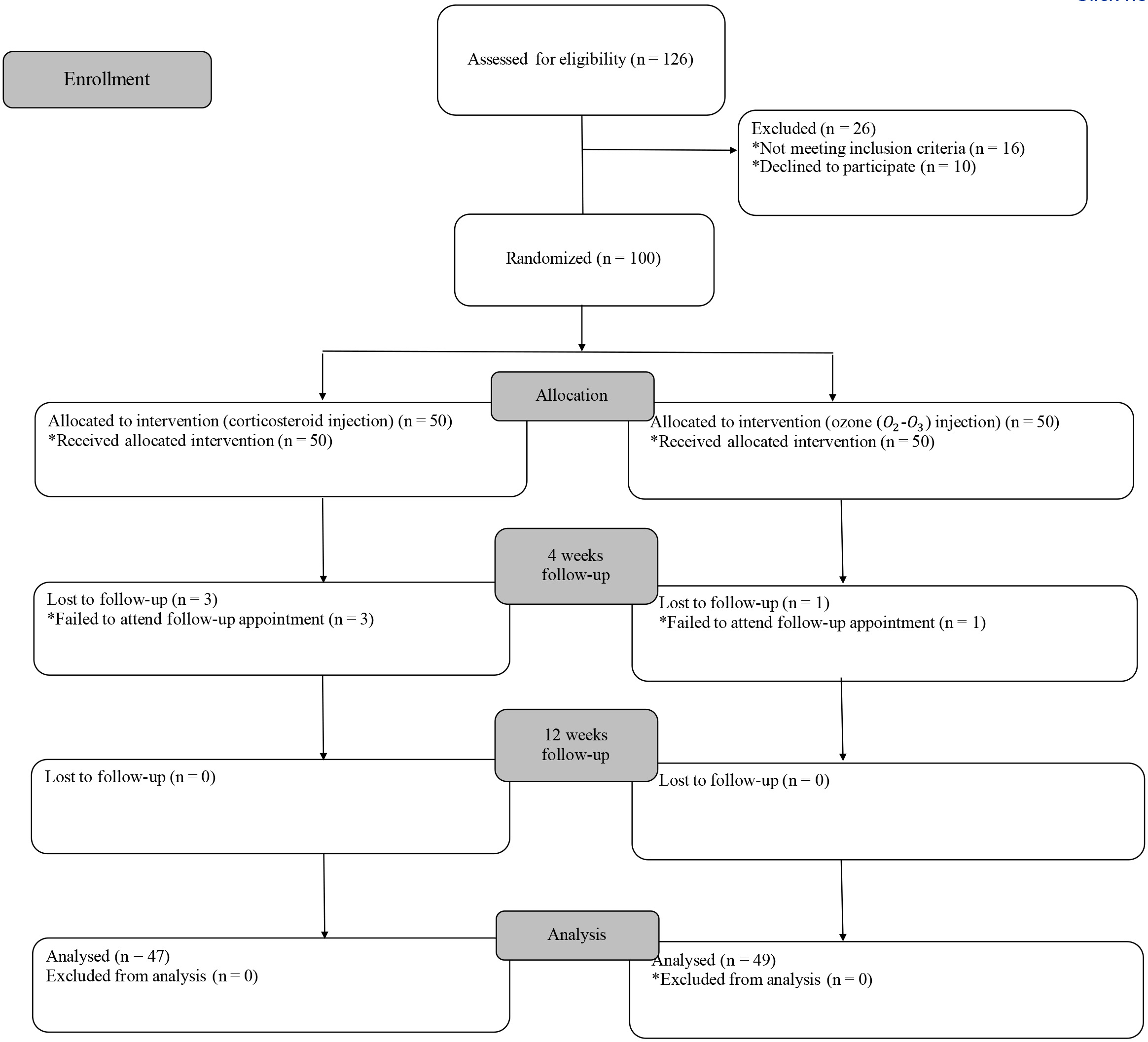
One hundred and twenty-six patients were initially assessed for study eligibility, and ultimately 100 participants were assigned randomly to either the corticosteroid group or the ozone (O2-O3) group. In the first month of follow-up, 4 patients were unable to participate in the study, while 96 patients successfully completed it. The graphical representation of participant flow is shown in Fig. 1, utilizing the CONSORT diagram.
Table 1
Participant characteristics and clinical attributes of the corticosteroid and ozone (O2-O3) groups at baseline
| Parameters | Corticosteroid group ( | Ozone (O2-O3) group ( | p |
|---|---|---|---|
| Age (years) | 62.51 | 62.59 | 0.965 |
| Gender, | |||
| Female | 42 (89.4) | 41 (83.7) | |
| Male | 5 (10.6) | 8 (16.3) | |
| Occupation, | |||
| Retired | 5 (10.6) | 23 (46.9) | |
| Working | 8 (17) | 4 (8.2) | |
| Never worked | 34 (72.3) | 22 (44.9) | |
| BMI (kg/m2) | 30.02 | 29.62 | 0.697 |
| Flexion ROM (Right) (∘) | 126.80 | 127.04 | 0.956 |
| Flexion ROM (Left) (∘) | 130.21 | 127.12 | 0.387 |
| Kellgren-Lawrence (right) | 2.80 | 2.87 | 0.554 |
| Kellgren-Lawrence (left) | 2.91 | 2.95 | 0.739 |
| VAS-rest (0–10) | 5.53 | 5.26 | 0.535 |
| VAS-move (0–10) | 7.87 | 7.32 | 0.059 |
| WOMAC (0–100) | 57.91 | 69.03 | 0.052 |
Data are showcased as mean
At baseline (study initiation), no significant differences in demographic, ultrasonographic, or clinical characteristics were evident between the corticosteroid and ozone (O2-O3) injection groups, as tabulated in Table 1.
Table 2
Summary of implications for principal outcomes
| Score (mean | Within-group change score (mean (95%CI)) | Repeated measure ANOVA | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 4 weeks | 12 weeks | Baseline vs. 4 weeks | Baseline vs. 12 weeks | 4 weeks vs. 12 weeks | Time | Time*group | |
| VAS rest | ||||||||
| Corticosteroid | 5.53 | 2.68 | 2.27 | 2.85 (2.31, 3.38)* | 3.25 (2.62, 3.88)* | 0.40 (0.05, 0.75)* | 259.29 ( | 1.12 (0.31) |
| Ozone (O2-O | 5.26 | 2.85 | 2.18 | 2.40 (1.88, 2.93)* | 3.08 (2.46, 3.70)* | 0.67 (0.32, 1.08)* | ||
| VAS movement | ||||||||
| Corticosteroid | 7.87 | 4.48 | 4.17 | 3.38 (2.64, 4.12)* | 3.70 (2.9, 4.48)* | 0.31 ( | 283.17 ( | 2.02 (0.135) |
| Ozone (O2-O | 7.32 | 4.20 | 3.18 | 3.12 (2.39, 3.84)* | 4.14 (3.37, 4.91)* | 1.02 (0.56, 1.47)* | ||
| WOMAC | ||||||||
| Corticosteroid | 72.54 | 45.95 | 37.10 | 26.59 (21.18, 31.99)* | 35.44 (28.87,42.00) | 8.85 (6.24, 11.45)* | 305.3 ( | 0.105 (0.79) |
| Ozone (O2-O | 68.23 | 42.99 | 33.43 | 25.23 (19.94, 30.53)* | 34.80 (19.94, 30.53)* | 9.56 (7.01,12.11)* | ||
*p< 0.000; **p< 0.05; VAS: Visual analog scale; WOMAC: The western ontario and mcmaster universities osteoarthritis index.
Figure 2.
Change of the evaluation parametres throughout time in corticosteroid and ozone (O2-O3) groups on the basis of the repeated-measure analysis of variance (estimated marginal means are shown). (A) Visual analog scale (VAS rest). (B) Visual analog scale (VAS movement) (C) The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC).
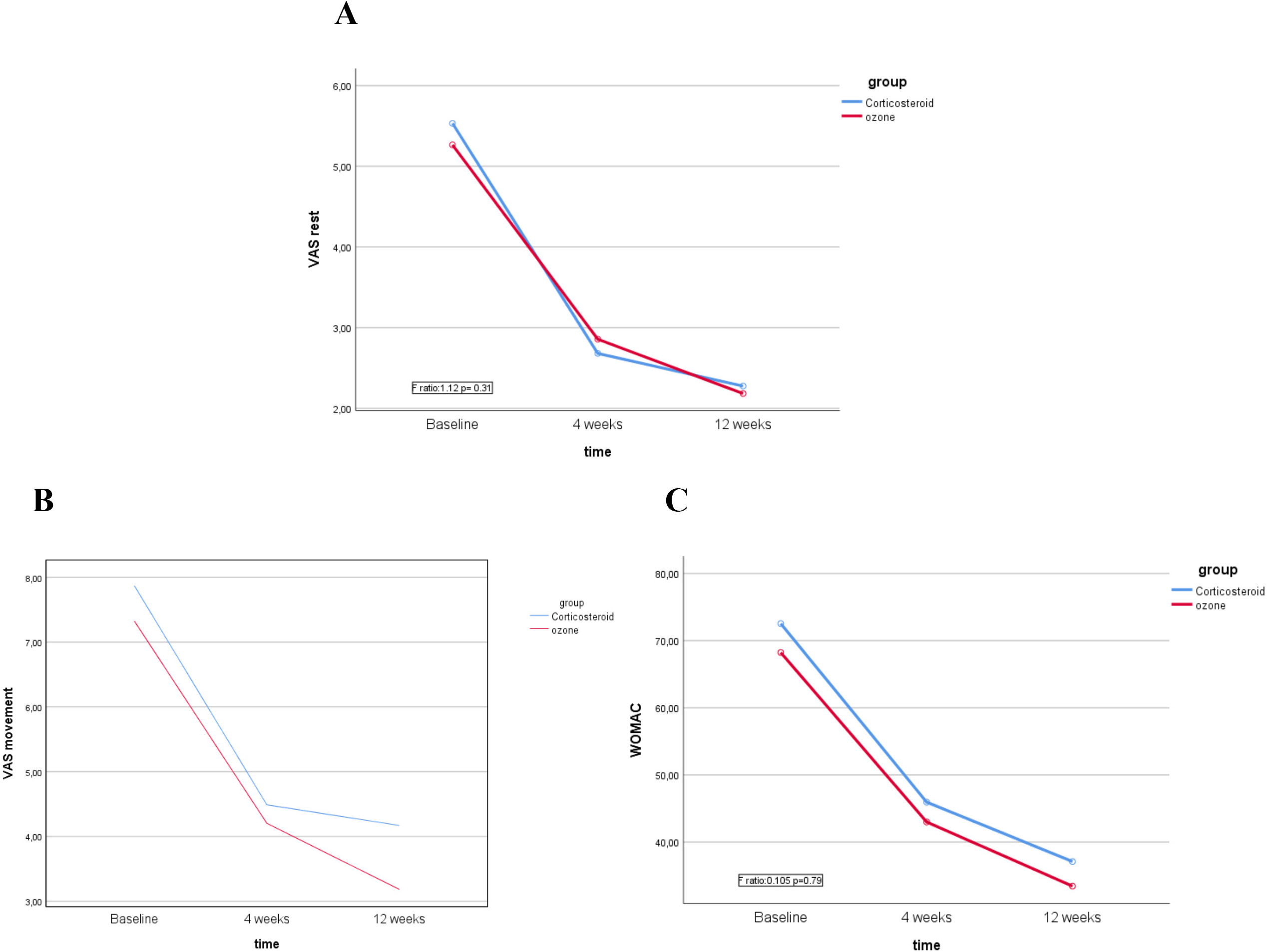
The outcomes obtained from the repeated-measure analysis of variance are presented comprehensively in Table 2 and graphically displayed in Fig. 2. A noteworthy temporal effect was identified for all outcome measures within both groups (Table 2). When comparing the baseline measurements to those taken at 4 weeks post-injection (
Moreover, regarding the VAS at rest, VAS on movement and WOMAC scores, no significant interaction between the groups and time was ascertained (
In the steroid group, initially, effusion was observed in 38.3% of patients during ultrasound evaluation. Subsequent evaluations at weeks 4 and 12 revealed effusion in 12.8% of the patients. Conversely, in the ozone group, effusion was initially detected in 55.1% of patients’ knees. However, by the conclusion of weeks 4 and 12, the percentage of patients with knee effusion had decreased to 10.2%.
4.Discussion
In the realm of OA, the tandem occurrence of advancing articular cartilage degeneration and inflammatory processes precipitates the emergence of both pain and joint deformities. The paramount therapeutic goals revolve around the mitigation of pain and the preservation of joint mobility. In pursuit of these objectives, an array of intra-articular injection modalities has been utilized. Within this spectrum, the preeminent options frequently employed in clinical practice encompass non-steroidal anti-inflammatory drugs, glucocorticoids, HA, platelet-rich plasma (PRP), and ozone [9].
The aim of the present investigation was to assess and check against the effects of two treatment approaches, ultrasound-guided knee corticosteroid injection and ozone (O2-O3) injection, in patients suffering from knee OA. The study’s results indicated that both corticosteroid and ozone (O2-O3) injections led to meaningful and clinically significant improvements in various aspects, including knee pain, disability, and overall knee function. However, the study found significant differences between the outcomes of a single corticosteroid injection and the application of three consecutive ozone (O2-O3) injections. In summary, this study suggests that both treatments (corticosteroid injection and ozone (O2-O3) injection) offer comparable benefits in alleviating symptoms and enhancing the overall well-being of patients with knee OA.
Ozone, chemically denoted as O3, constitutes the allotropic manifestation of oxygen. Its application extends to the administration of diverse situations, encompassing infections, autoimmune disorders, and orthopedic ailments [15]. Notably, ozone is characterized by analgesic, anti-inflammatory, modulator of the immune system, and trophic attributes [16]. It is imperative to acknowledge that ozone does not fall within the category of homeopathic drugs. In contrast, ozone distinctly adheres to a dose-effect relationship, thus departing from the principles of homeopathy [17].
Ozone exhibits the ability to impede the formation of inflammatory bradykinin and prostaglandins, thereby promoting a decrease in pain perception and promoting the reabsorption of edema [18]. A pivotal aspect of the adjustable response to the sustained oxidative state induced by ozone is the stimulation of antioxidant enzyme synthesis, encompassing superoxide dismutase, catalase, and glutathione peroxidase. This rationale underscores the initial administration of ozone at lower dosages [19]. Diverse therapeutic applications necessitate varying dosages to attain optimal effects, falling within a therapeutic range of 10 to 80
Nevertheless, O2-O3 injection is considered a relatively safe and effective therapeutic approach. Several studies have highlighted the safety of ozone injections in musculoskeletal disorders [21, 22, 23]. However, to guarantee safety, it is essential to set ozone concentrations within a prescribed range. Within the scope of this study, the ozone concentrations used were determined based on the recommendations provided by the International Scientific Committee of Ozonotherapy (ISCO3) for musculoskeletal treatment [24]. Using convenient and carefully controlled ozone concentrations can contribute to the safety and effectiveness of ozone injection therapy, making it a promising option for certain medical conditions.
Ozone intervention has a longstanding history in the handling of OA treatment [18]. Moreover, experimental evidence substantiates that it does not reveal a substantial inflammatory process or contribute to cartilage corruption [20]. Several investigations have been undertaken to determine the impact of ozone (O2-O3) therapy in the context of knee disorders [25, 26, 27]. These studies exhibit changeability with respect to all-important parameters, including the concentration and volume of ozone (O2-O3) administered, the frequency of injection sessions, and the specific injection methodology employed.
Ozone constitutes a triatomic variant of oxygen, predominantly harnessed for its application in rheumatoid arthritis and OA [16]. Additionally, ozone therapy engenders the favorable outcome of stimulating angiogenesis and vasodilation, thereby enhancing the oxygen supply to tissues [16]. The practice of intra-articular administration of oxygen-ozone has spanned several decades. Numerous investigations have acknowledged that ozone represents an efficacious and safe alternative for addressing knee OA. However, it is noteworthy that these studies have encompassed diverse treatment protocols, and the duration of follow-up have exhibited variability.
Ozone’s mechanisms encompass the initiation of cellular metabolism and the impediment of prostaglandin synthesis, which collectively engender antioxidative, anti-inflammatory, and analgesic effects [28]. In the study conducted by Babaei-Ghazani et al. [29], which involved 62 patients, the efficacy of corticosteroid and ozone treatments was compared. The evaluation at the conclusion of the 3rd month of the study revealed that the enhancements in VAS scores were similar in both groups (steroid group
The optimal therapeutic protocol for ozone treatment remains shrouded in uncertainty, particularly concerning ozone concentration, injection volume, frequency of injections, and intervals between administrations. Indeed, the possibility exists that suboptimal outcomes observed in ozone therapy, as compared to control groups, might stem from a lack of uniformity in the injection protocol employed. Inconsistencies in these procedural parameters could potentially contribute to divergent results in the efficacy of ozone therapy [30].
Giombini et al. [31] compared the consequences of intra-articular injections of HA, oxygen-ozone, and a integration of both for the management of knee OA. Their findings demonstrated that each subset of the three groups exhibited improvements in Knee Injury and Osteoarthritis Outcome Scores (KOOS) for up to two months after the treatment. These applications were administered once per week for a total of five weeks. The outcome measures assessed were limited to KOOS and VAS, conducted prior to the treatment, after the fifth injection, and at the two-month post-treatment mark. These results were similar to the findings of this study. The patients in this study applied to a third injection of oxygen-ozone and a single injection corticosteroid using four endpoint parametres and conducted a three-month follow-up.
Duymuş et al. [32] carried out a randomized controlled study on patients with knee OA and compared the efficiency of intra-articular injection of PRP, HA and ozone (O2-O3) injection. Intra-articular injection of PRP was applied twice to group 1, a single dose of HA was administered to group 2, and group 3 (Ozone group) received ozone at a concentration of 30
The authors accredit the considerable improvements observed in endpoint parametres within the O2-O3 group to the affirmative biological attributes inherent to the O2-O3 molecule. Potential mechanisms of action for O2-O3 therapy in managing musculoskeletal conditions include the initiation of tissue-level repair processes, augmentation of analgesic and anti-inflammatory effects, and promotion of cellular oxygenation through the activation of anti-nociceptive systems [21, 35]. The utilization of intra-articular glucocorticoids offers advantages in extenuating symptomatic relief [36]. However, their usage warrants deliberateness, as recurrent administration may aggravate damage to the articular cartilage [37].
HA symbolizes a multifaceted polysaccharide encompassing glucosamine and glucuronic acid, components intrinsic to joint fluid [38]. Notably, the pain mitigation achieved via HA injections in individuals afflicted by knee OA is on par with that derived from glucocorticoid injections [39].
A study conducted by Zhang et al. [40] found that the intra-articular administration of PRP did not conspicuously surpass HA in the context of knee OA. Consequently, the outcomes garnered from the application of these three therapeutic approaches often exhibit comparability. Side effects of intra-articular administered corticosteroid injection may include subchondral insufficiency fracture, tendon rupture, accelerated of pain, skin hypopigmentation and infectious arthritis.
A study comparing the effects of ozone and HA [8] found that the VAS scores in the ozone group were significantly lower in the first month. In the sixth month, the VAS scores were not statistically different between the two groups, and the authors found a similar prevalence of patients requiring a second treatment cycle (VAS
The findings derived from the present study suggest that O2-O3 injections could be contemplated as an diversified treatment modality to corticosteroid injections for patients afflicted with knee OA, underscoring the clinical significance of this research. It is essential to acknowledge that, given the 12-week post-treatment time frame in this study, further investigations employing extended follow-up intervals and diverse outcome measures are warranted to exhaustively ascertain whether O2-O3 therapy may Illustrate superior long-term efficacy when compared to corticosteroids.
To maintain the effectiveness of O2-O3 injection and achieve long-term clinical recuperation, it is necessary to carry out the injections three times a week at regular intervals on average. This approach may help maintain the positive effects of O2-O3 treatment over an extended period. Furthermore, weight control of patients should be taken into account, as lifestyle changes (e.g., increasing physical activity, exercise, etc.), including weight management, can have a meaningful impact on the management of OA.
The study is not free from noticeable limitations that warrant consideration while construing the findings. Firstly, a significant restriction of this study is the deficiency in a suitable control group that would receive no injection. The inclusion of such a control group would have allowed for a more extensive comparison of the intervention effects. Secondly, the essential characteristics of the interventions led the injecting physiatrist and the participants were unable to be blinded. The inadequacy of blinding introduces the possibility of bias influencing the study outcomes. The third restriction of is the comparison between a three-time ozone injection and a one-time steroid injection, along with variations in injectate volume between the two groups, may introduce bias and confound the consequences. Lastly, there was a relatively short follow-up duration utilized in this study may limit the ability to thoroughly analyze the long-term effects and sustainability of the interventions.
5.Conclusions
Overall, the findings of this study indicate that three times ozone (O2-O3) injection is not superior to one-time corticosteroid injection for improving function and providing pain relief in patients with knee OA. It may be as effective as corticosteroid injection in terms of relieving pain and improving quality of life and function at four weeks and twelve weeks post-injection.
Data availability
The dataset is available from the corresponding author upon reasonable request.
Funding
No funding sources were disclosed for the study.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The study protocol and design were approved by the Duzce University Ethics Committee (approval number: 2020-7-4).
Informed consent
Informed consent was obtained from all participants included in the study.
Acknowledgments
None to report.
Conflict of interest
The authors have no conflict of interest to report.
References
[1] | Wang-Saegusa A, Cugat R, Ares O, Seijas R, Cuscó X, Garcia-Balletbó M. Infiltration of plasma rich in growth factors for osteoarthritis of the knee short-term effects on function and quality of life. Arch Orthop Trauma Surg. (2011) ; 131: (3): 311-7. |
[2] | Cross M, Smith E, Hoy D, Nolte S, Ackerman I, Fransen M, et al. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. (2014) ; 73: (7): 1323-30. |
[3] | Litwic A, Edwards MH, Dennison EM, Cooper C. Epidemiology and burden of osteoarthritis. Br Med Bull. (2013) ; 105: : 185-99. |
[4] | Iolascon G, Gimigliano F, Moretti A, De Sire A, Migliore A, Brandi M, et al. Early osteoarthritis: How to define, diagnose, and manage. A systematic review. European Geriatric Medicine. (2017) ; 8: (5–6): 383-96. |
[5] | Rabini A, De Sire A, Marzetti E, Gimigliano R, Ferriero G, Piazzini DB, et al. Effects of focal muscle vibration on physical functioning in patients with knee osteoarthritis: A randomized controlled trial. Eur J Phys Rehabil Med. (2015) ; 51: : 513-20. |
[6] | de Sire A, Marotta N, Marinaro C, Curci C, Invernizzi M, Ammendolia A. Role of physical exercise and nutraceuticals in modulating molecular pathways of osteoarthritis. International Journal of Molecular Sciences. (2021) ; 22: (11): 5722. |
[7] | Raeissadat SA, Rayegani SM, Forogh B, Hassan Abadi P, Moridnia M, Dehgolan S. Intra-articular ozone or hyaluronic acid injection: Which one is superior in patients with knee osteoarthritis? A 6-month; randomized clinical trial. J Pain Res. (2018) ; 11: : 111-7. |
[8] | de Sire A, Stagno D, Minetto MA, Cisari C, Baricich A, Invernizzi M. Long-term effects of intra-articular oxygen-ozone therapy versus hyaluronic acid in older people affected by knee osteoarthritis: A randomized single-blind extension study. J Back Musculoskelet Rehabil. (2020) ; 33: (3): 347-54. |
[9] | de Sire A, Agostini F, Lippi L, Mangone M, Marchese S, Cisari C, et al. Oxygen–Ozone therapy in the rehabilitation field: state of the art on mechanisms of action, safety andeffectiveness in patients with musculoskeletal disorders. Biomolecules. (2021) ; 11: (3): 356. |
[10] | Moher D, Hopewell S, Schulz KF, Montori V, Gotzsche PC, Devereaux PJ, et al. CONSORT 2010 Explanation and Elaboration: updated guidelines for reporting parallel group randomised trials. BMJ. (2010) ; 340: (mar23 1): c869-c. |
[11] | Price DD, McGrath PA, Rafii A, Buckingham B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain. (1983) ; 17: (1): 45-56. |
[12] | Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. (1988) ; 15: (12): 1833-40. |
[13] | Tüzün EH, Eker L, Aytar A, Daşkapan A, Bayramoğlu M. Acceptability, reliability, validity and responsiveness of the Turkish version of WOMAC osteoarthritis index. Osteoarthritis Cartilage. (2005) ; 13: (1): 28-33. |
[14] | Choi WJ, Hwang SJ, Song JG, Leem JG, Kang YU, Park PH, Shin JW. Radiofrequency treatment relieves chronic knee osteoarthritis pain: a double-blind randomized controlled trial. Pain. (2011) Mar; 152: (3): 481-487. doi: 10.1016/j.pain.2010.09.029. Epub 2010 Nov 4. PMID: 21055873. |
[15] | Zanardi I, Borrelli E, Valacchi G, Travagli V, Bocci V. Ozone: A multifaceted molecule with unexpected therapeutic activity. Curr Med Chem. (2016) ; 23: (4): 304-14. |
[16] | Bocci VA. Scientific and medical aspects of ozone therapy. State of the art. Arch Med Res. (2006) ; 37: (4): 425-35. |
[17] | Velio B. Ozone-A new medical drug. Netherlands: Springer. (2005) ; 20: : 83. |
[18] | Bocci V, Zanardia I, Valacchi G, Borrelli E, Travagli V. Validity of oxygen-ozone therapy as integrated medication form in chronic inflammatory diseases. Cardiovasc Hematol Disord Drug Targets. (2015) ; 15: (2): 127-38. |
[19] | Manoto SL, Maepa MJ, Motaung SK. Medical ozone therapy as a potential treatment modality for regeneration of damaged articular cartilage in osteoarthritis. Saudi J Biol Sci. (2018) ; 25: (4): 672-9. |
[20] | Qi WN, Scully SP. Extracellular collagen modulates the regulation of chondrocytes by transforming growth factor-beta 1. J Orthop Res. (1997) ; 15: (4): 483-90. |
[21] | de Sire A, Marotta N, Ferrillo M, Agostini F, Sconza C, Lippi L, et al. Oxygen-ozone therapy for reducing pro-inflammatory cytokines serum levels in musculoskeletal and temporomandibular disorders: A comprehensive review. International journal of molecular sciences. (2022) ; 23: (5): 2528. |
[22] | Sconza C, Di Matteo B, Queirazza P, Dina A, Amenta R, Respizzi S, et al. Ozone therapy versus hyaluronic acid injections for pain relief in patients with knee osteoarthritis: Preliminary findings on molecular and clinical outcomes from a randomized controlled trial. International Journal of Molecular Sciences. (2023) ; 24: (10): 8788. |
[23] | Ferrillo M, Giudice A, Marotta N, Fortunato F, Di Venere D, Ammendolia A, et al. Pain management and rehabilitation for central sensitization in temporomandibular disorders: a comprehensive review. International Journal of Molecular Sciences. (2022) ; 23: (20): 12164. |
[24] | Alexandre A, Baeza J, Kumar VS. Ozone in non-rheumatic locomotor system pathologies. ISCO3-International; Scientific Committee of Ozone Therapy. Madrid. (2014) . |
[25] | Rahimzadeh P, Imani F, Azad Ehyaei D, Faiz SHR. Efficacy of oxygen-ozone therapy and platelet-rich plasma for the treatment of knee osteoarthritis: A meta-analysis and systematic review. Anesth Pain Med. (2022) ; 12: (4): e127121. |
[26] | Raeissadat SA, Ghazi Hosseini P, Bahrami MH, Salman Roghani R, Fathi M, Gharooee Ahangar A, et al. The comparison effects of intra-articular injection of Platelet Rich Plasma (PRP), Plasma Rich in Growth Factor (PRGF), Hyaluronic Acid (HA), and ozone in knee osteoarthritis; a one year randomized clinical trial. BMC Musculoskelet Disord. (2021) ; 22: (1): 134. |
[27] | Sconza C, Respizzi S, Virelli L, Vandenbulcke F, Iacono F, Kon E, et al. Oxygen-ozone therapy for the treatment of knee osteoarthritis: A systematic review of randomized controlled trials. Arthroscopy. (2020) ; 36: (1): 277-86. |
[28] | Andreula CF, Simonetti L, De Santis F, Agati R, Ricci R, Leonardi M. Minimally invasive oxygen-ozone therapy for lumbar disk herniation. AJNR Am J Neuroradiol. (2003) ; 24: (5): 996-1000. |
[29] | Babaei-Ghazani A, Najarzadeh S, Mansoori K, Forogh B, Madani SP, Ebadi S, et al. The effects of ultrasound-guided corticosteroid injection compared to oxygen-ozone (O(2)-O(3)) injection in patients with knee osteoarthritis: a randomized controlled trial. Clin Rheumatol. (2018) ; 37: (9): 2517-27. |
[30] | Oliviero A, Giordano L, Maffulli N. The temporal effect of intra-articular ozone injections on pain in knee osteoarthritis. Br Med Bull. (2019) ; 132: (1): 33-44. |
[31] | Giombini A, Menotti F, Di Cesare A, Giovannangeli F, Rizzo M, Moffa S, et al. Comparison between intrarticular injection of hyaluronic acid, oxygen ozone, and the combination of both in the treatment of knee osteoarthrosis. Journal of biological regulators and homeostatic agents. (2016) ; 30: (2): 621-5. |
[32] | Duymus TM, Mutlu S, Dernek B, Komur B, Aydogmus S, Kesiktas FN. Choice of intra-articular injection in treatment of knee osteoarthritis: platelet-rich plasma, hyaluronic acid or ozone options. Knee surgery, sports traumatology, arthroscopy. (2017) ; 25: : 485-92. |
[33] | Faúndez J, Cotoras P, Irarrázaval S. Are intraarticular steroids effective for knee osteoarthritis? Medwave. (2016) ; 16: (Suppl 5). |
[34] | Fatimah N, Salim B, Raja E-u-H, Nasim A. Predictors of response to intra-articular steroid injections in patients with osteoarthritis of the knee joint. Clinical rheumatology. (2016) ; 35: : 2541-7. |
[35] | de Sire A, Baricich A, Minetto MA, Cisari C, Invernizzi M. Low back pain related to a sacral insufficiency fracture: role of paravertebral oxygen-ozone therapy in a paradigmatic case of nociplastic pain. Funct Neurol. (2019) ; 34: (2): 119-122. PMID: 31556392. |
[36] | McCrum C. Therapeutic review of methylprednisolone acetate intra-articular injection in the management of osteoarthritis of the knee – part 1: clinical effectiveness. Musculoskeletal Care. (2017) ; 15: (1): 79-88. |
[37] | Hart LE. In knee OA, intraarticular triamcinolone increased cartilage loss and did not differ from saline for knee pain. Ann Intern Med. (2017) ; 167: (6): Jc27. |
[38] | Balazs EA. Viscosupplementation for treatment of osteoarthritis: from initial discovery to current status and results. Surg Technol Int. (2004) ; 12: : 278-89. |
[39] | Ran J, Yang X, Ren Z, Wang J, Dong H. Comparison of intra-articular hyaluronic acid and methylprednisolone for pain management in knee osteoarthritis: A meta-analysis of randomized controlled trials. Int J Surg. (2018) ; 53: : 103-10. |
[40] | Zhang HF, Wang CG, Li H, Huang YT, Li ZJ. Intra-articular platelet-rich plasma versus hyaluronic acid in the treatment of knee osteoarthritis: a meta-analysis. Drug Des Devel Ther. (2018) ; 12: : 445-53. |




