Efficacy of Self-Natural Posture Exercise (SNPE) programs on chronic low back pain: A randomized controlled feasibility trial with waitlist control
Abstract
BACKGROUND:
Low back pain (LBP) is a significant source of disability and decreased quality of life. The Self-Natural Posture Exercise (SNPE) intervention can be used effectively in many cases, but feasibility and impact has not been fully explored.
OBJECTIVE:
The current study explores the feasibility and efficacy of face-to-face (FtF) and virtual (Vir) SNPE programs on chronic low back pain.
METHODS:
This is a randomized single-blinded waitlist control study with 10 participants in the FtF group (age 45.8
RESULTS:
Rates of retention were 80% in the FtF group and 78% in the Vir group. Attendance rates were 88% in the FtF group and 60% in the Vir group. ODI, VAS, and some SF-36 domains improved in both the FtF and Vir groups. Overall, the FtF group improved in more domains and by a larger degree than the Vir group and both groups improved relative to Con.
CONCLUSION:
A 12-week SNPE program, done virtually or in person, shows promise in improving ODI, VAS, and some SF-36 domains. FtF appears to be more effective. Future studies would benefit from sampling a larger and more diverse population.
1.Introduction
Low back pain (LBP) is a major health concern across the United States, resulting in a significant socio-economic burden, considerable disability, and reduction in quality of life [1]. The direct economic impact of LBP in the U.S is at least $34 billion and continues to grow [2]. It is estimated that up to 80 percent of all people experience LBP some time in their life and the rate of recurrence is about 20 percent [3, 4, 5]. Chronic low back pain (CLBP) is defined as pain that has been present for 3 months or longer, and patients are generally diagnosed based on their history [5]. Clinical practice guidelines for CLBP by the American College of Physicians recommend nonpharmacologic treatment including exercise, massage, spinal manipulation, or cognitive behavioral therapy [6]. There is a growing body of research that supports exercise as an effective nonpharmacologic treatment for CLBP to reduce pain, help maintain or restore flexibility, improve strength, and increase endurance [7, 8, 9].
One such non-pharmacologic treatment is Self-Natural Posture Exercise (SNPE), a series of exercises developed by a chiropractor and influenced by orthodontic bracing principles [10, 11]. The system was designed to specifically target back and neck pain. Its aim is to restore the natural curvature of the individual’s spine by normalizing muscle strength and muscle tone in the axial body via independently performed exercises and independently performed myofascial massage. The term “Self-Natural Posture Exercise” is derived directly from this proposed mechanism of pain relief. As patients engaging in exercise programs for LBP [12] and other conditions [13] often do not demonstrate proper exercise technique, SNPE utilizes orthodontics-inspired bracing tools to enforce proper body alignment so that individuals can easily practice the standard eight exercises without professional oversight or follow-up. A Pelvic Correction Belt is worn around the hips and a Posture Correction Belt is worn around the legs, and a typical program targets the entire axial skeleton. The exercises can be practiced anywhere and are expected to be widely accessible as the exercises are simple and of low- to moderate-intensity [10, 11].
There are several studies examining the efficacy of SNPE; however, prior research on SNPE examined overall pain levels rather than CLBP specifically and did not include control groups. Additionally, there are no studies from outside the country of South Korea [10, 11]. As such, there is little data on the generalizability of SNPE, its feasibility for CLBP, the degree of cultural acceptance in other countries, and of the all-important rate of adherence to a home exercise program. The Virtual (Vir) courses may be of particular promise, given the self-directed nature of SNPE lends itself to such a method of instruction and also in light of the recent COVID pandemic which limited patient access to in-person care. The impact of finding efficacious clinical applications of SNPE, especially Vir sessions, to the global CLBP patient population could be significant. First, comparatively inexpensive courses could bring treatment to those with limited financial means who may not be able to afford other options [14, 15]. Second, the Vir courses would bring this intervention to those in areas where other options, such as intervention by a skilled physical therapist, chiropractor, acupuncturist, etc. are not available. Third, it would serve as an additional intervention to trial for the diagnosis of CLBP, which can be refractory to current approaches [16].
The present study seeks to repeat the previously described positive clinical impact of SNPE [10, 11] in a new population, examine adherence, and compare the trends of the effects of FtF and Vir courses.
2.Methods
2.1Study design
We conducted an assessor-blinded randomized controlled trial (RCT) with waitlist control evaluating the feasibility of an SNPE program for CLBP reduction between Face-to-Face (FtF), Vir, and Control (Con) groups. The waitlist Con group received the online SNPE intervention after serving as a control group for both the FtF and Vir groups. By nature of this study design and intervention, the participants and instructor were unavoidably aware of if they were in the FtF or Vir group and it was not possible to blind them to that information. Consequently, our blinding efforts emphasized blinding the assessors to the participants’ assigned groups and the primary researcher (AS) to the data collection process. The protocol was approved by Advarra IRB (Pro00055003) on 16 August 2021. The study’s ClinicalTrials.gov identifier is NCT05136729.
2.2Participants
Participants were recruited from December 2021 to April 2022 in Billings, MT, USA through flyers, social media, and referrals from community healthcare providers. Recruitment messages included relevant information about the study, benefits, and inclusion criteria as well as a link to a study-specific website recapitulating this information with additional details (https://xppizim.wixsite.com/snpestudy). Interested individuals completed an online survey (www.surveymonkey.com) which included the Oswestry Disability Index (ODI) Questionnaire [17] and the Visual Analog Scale (VAS) [18] for pain severity. Data from the online survey was reviewed to determine eligibility.
The eligibility criteria included: have a LBP score of 1 or higher on the VAS for at least 3 months duration with a low to moderate disability score (less than 50% on the ODI), have internet access with a mobile or desktop device capable of video streaming, not currently receiving manual or physical interventions for low back pain, no opioid medication for low back pain used in the last 30 days, and no plan to have back pain treatment in the next 12 months. Individuals were excluded if they had: history or evidence of functionally significant musculoskeletal deformity and balance dysfunction, a history of spine or pelvis orthopedic or neurological surgery, a significant medical (e.g., cardiac or pulmonary) condition limiting exercise safety or tolerance, pregnancy, or a body mass index (BMI)
Individuals were informed of their eligibility through email and, if eligible, set up an appointment for the first assessment. At the first visit, participants were provided documentation of informed consent and signed a Health Insurance Portability and Accountability Act (HIPAA) form before the assessment was started. After the first assessment, one of our researchers (JJ) who was not involved in intervention nor assessment randomly assigned participants to either the FtF or Vir groups using random numbers derived from a random number table in Microsoft Excel.
A statistical power analysis was conducted using G*Power (3.1) [19] to estimate the sample size required for between-group comparisons. This analysis was guided by previous findings showing large effect sizes (ie,
2.3Outcome measures
2.3.1Primary measures
Our primary outcome measure was feasibility. To assess feasibility, we evaluated the rate of completion of the intervention, rate of attendance, and rate of adverse events. The rate of completion for both groups was defined as the number of participants who completed the 12-week intervention (via either the FtF or Vir exercise programs) followed by completion of the post-intervention assessment.
2.3.2Secondary measures
Secondary outcome measures were participant-reported outcomes and outcomes measured by the research team. Participant-reported outcomes measures addressed disability from low back pain, pain severity, and quality of life. The disability from low back pain was measured by The Oswestry Disability Index (ODI) Questionnaire version 2.0 [17]. It consisted of ten topics, each followed by six statements describing scenarios related to the topic. Patients scored each statement on a scale of 0–5, with higher scores indicating greater disability [17, 22]. The Visual Analog Scale (VAS) was used to measure pain severity at rest and during activity. Participants marked their pain intensity on a 10-cm line, where 0 represented no pain and 10 represented the worst possible pain [23]. The SF-36 (based on the RAND 36-Item Health Survey 1.0) assessed quality of life [24]. The survey covered eight domains of health and used three- or five-point Likert scales for responses, with a higher score indicating better quality of life. All self-reported data in this study were collected and exported via www.surveymonkey.com, which is compliant with data privacy regulations like General Data Protection Regulation (GDPR).
Pressure pain threshold (PPT) and muscle tone (MT) were measured by the research team. MT, expressed in frequency (Hz), was measured using a non-invasive muscle tone meter. This same muscle tone meter was also used to assess PPT, an indicator of sensitivity to pain, and is defined as the minimum force applied which induces pain.
2.4Assessments
Feasibility was examined by qualitatively evaluating adherence and the number of adverse events. Adherence was considered to be a combination of study completion and attendance rate [25]. Completion rate was simply the number of participants who completed the study divided by the total number of participants in the respective group. The attendance rate had to be measured differently between the groups secondary to the nature of the study design and self-directed nature of the Vir group. For the FtF group, AS simply noted physical attendance. For the Vir group, it was calculated by examining participant-submitted weekly exercise diaries over 12 weeks. As 7 Vir participants completed the study, 84 (7 participants
All outcome measures were standardized and documented. To maintain consistent test conditions, outside noise and vibration were limited, and appropriate temperature (22–25∘C) and humidity (45–60%) were maintained. Additionally, participants were instructed to avoid any pain medications, including over the counter, for 24 hours before undergoing a measurement session.
When participants arrived at the laboratory, they were requested to complete the ODI, VAS and SF-36 on an electronic tablet while sitting in a comfortable chair. Height and weight were measured barefoot via a stadiometer. Prior to assessing muscle tone and pain threshold participants sat for 10 minutes, breathing naturally, without external stimulus. During the measurement process, participants were instructed to relax as much as possible.
To measure PPT [26], the examiner used a gauge with a flat circular probe with an area of 1 cm2 placed vertically on the muscle to be measured and pressure was gradually applied. The participants verbally notified the examiner when they started to feel pain. The examiner then released the probe, and the pressure at the time of removal appeared on the screen in units of kg/cm2. MT and PPT were measured at the latissimus dorsi, gluteus medius, and bilateral L4 erector spinae as well as 1 cm above and below to estimate L3 and L5, respectively. To measure MT [27], a handheld device with a small probe was positioned perpendicularly over the center of the muscle to be tested and pressed into it. The device applied a mechanical impulse of 15 ms duration and total mechanical force of 0.58 N. The resulting muscle vibration was recorded. MT was displayed on the device by automatically calculating biomechanical parameters. All sites were measured twice, and when the coefficient of variation (CV) was 3% or less, the average value was recorded; when the CV was 3% or more, re-measurement was performed.
All outcomes were assessed by the same evaluation team before the intervention, after the intervention, and at the 12-week follow-up. The evaluators were completely independent from both the intervention administered and the data analysis process.
2.5Intervention
Participants in the FtF group were required to attend two sessions of SNPE training per week for a duration of 12 weeks. The SNPE training was conducted at a local physiotherapy clinic with 2–5 participants per session, led by a certified SNPE instructor (AS).
Participants in the Vir group received weekly emails for a duration of 12 weeks containing two instructional exercise videos and a link to a self-reported exercise diary. In addition, the email encouraged them to perform SNPE training at least twice a week and to complete the self-reported exercise diary, which tracked their attendance, completion of the provided program, physical exertion, and any adverse events.
Table 1
Basic one-hour SNPE program
| Category | Type of exercise | Duration/frequency |
|---|---|---|
| Warm-up | Myofascial release using the SNPE wave pillow. | 5 min |
| Main exercise | SNPE Movement 1: Invisible chair pose with both hands clasped behind the back. | 30 s |
| SNPE Movement 2: Leaning back while kneeling, with SNPE belts. | 1–3 min | |
| SNPE Movement 3: Prone hip extensions, with SNPE belts. | 10–30 s | |
| SNPE Movement 4: Rolling back and forth across the whole spine, with SNPE belts. | 3–5 min | |
| SNPE C-move: While supine with a SNPE wave pillow or Danason under the neck, the head is rolled from left to right. | 5–10 min | |
| SNPE T-move: A SNPE wave pillow is placed under the back vertically while bridging. | 50–150 times | |
| SNPE L-move: Placing the SNPE wave pillow under the posterior superior iliac spine horizontally, using the core to repeatedly pull the knees above the hips. | 50–100 times | |
| SNPE SC-move: Placing the SNPE wave pillow under the SI joints and rock left and right. | 3–5 min | |
| Cool down | Resting supine with SNPE wave pillow under natural lumbar lordosis. | 5 min |
Note: SNPE, self-natural posture exercise; L-move, lumbar movement; T-move, thoracic movement; C-move, cervical movement; SC-move, sacrococcygeal movement.
The details of basic SNPE exercise training [10, 11] are provided in Table 1. In general, the training includes body weight exercises in conjunction with belts to align and stabilize body posture and joints. Up to four belts were used in this study, positioned around the hips, thighs, below the knees, and above the ankles. Part of the intervention also involved self-performed myofascial release using SNPE equipment. As with physical therapy, small adjustments to positioning or technique were often required for those in the FtF group during training. These adjustments could not be provided to the Vir group due to the one-way communication inherent in the study design. After completing the FtF group sessions, AS created videos with the same exercise program content. They were presented to the Vir group in progressive order, matching the progressive nature of the exercise program administered to the FtF group. While the FtF sessions were 60 minutes in length, the videos were 35–45 minutes in length as the instructional process was more streamlined without the presence of interpersonal interaction.
Although the potential for discomfort during exercise including headache, bruising, dizziness, or nausea was written in the informed consent, the instructor mentioned it again before beginning the FtF classes and at the beginning of the Vir video series.
2.6Data analysis
All data were exported from the website for SurveyMonkey, an online cloud-based survey development service company (www.surveymonkey.com) and analyzed using SPSS software version 29 (IBM Corp., Armonk, NY, USA). Descriptive statistics were used to summarize demographic variables. To determine changes in outcome measures, group (FtF, Vir, and Con) by time (pre-, post-, and follow-up) Repeated Measures Analysis of Variance (RMANOVA) was utilized. Prior to conducting the RMANOVA, assumptions of sphericity, homogeneity of variances, and independence were assessed. When the assumption of sphericity was violated (i.e., Mauchly’s test was significant), the corrections were used based on the value of epsilon (
3.Results
Table 2
Descriptive characteristics of study participants
| Variable | All participants ( | Face-to-face ( | Virtual ( |
|---|---|---|---|
| Demographic characteristics | |||
| Mean | 48.8 | 45.8 | 52.2 |
| Female, no. (%) | 16 (84) | 9 (90) | 7 (78) |
| Race, no. (%) | |||
| Asian | 1 (5) | 1 (10) | 0 (0) |
| Caucasian | 18 (95) | 9 (90) | 9 (100) |
| Hispanic or Latino, no. (%) | 1 (5) | 0 (0) | 0 (0) |
| Health Characteristics | |||
| Mean | 24.9 | 25.3 | 24.4 |
| BMI range, no. (%) | |||
| Healthy range | 11 (58) | 5 (50) | 6 (67) |
| Overweight | 7 (37) | 5 (50) | 2 (22) |
| Obese | 1 (5) | 0 (0) | 1 (11) |
| Mean | 18.1 | 19.2 | 16.9 |
| Mean | 3.2 | 3.3 | 3.3 |
Note. S.D.
Figure 1.
Consort flow diagram. Participant flow is reported in accordance with CONSORT. *Post-intervention assessment for the control group, and pre-intervention assessment for the Vir group.
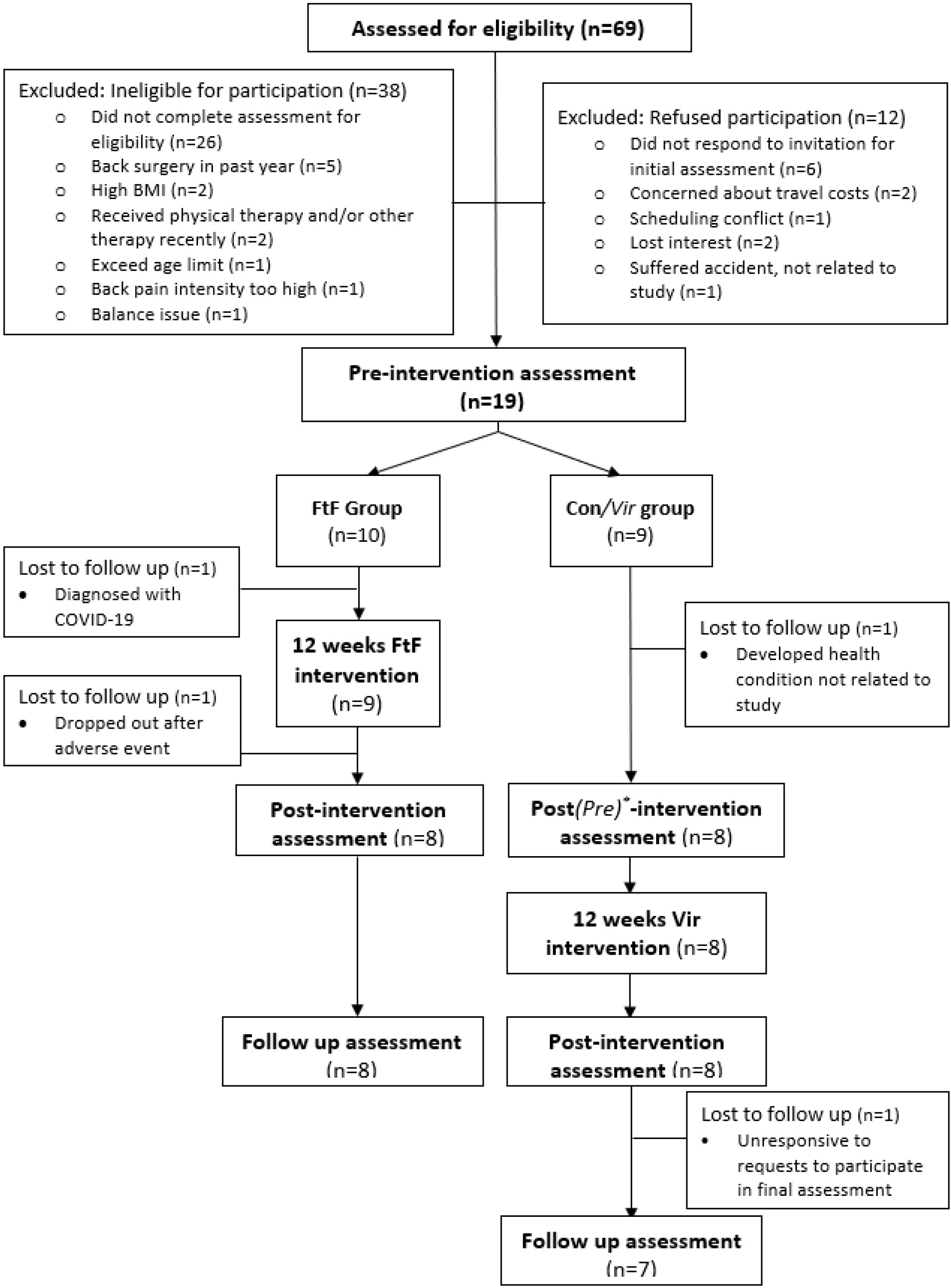
A total of 69 participants were assessed for eligibility for this study, and 19 participants were ultimately allocated into study groups. Of the 50 excluded, the majority (26 participants) simply never completed the required assessment for eligibility, and a significant number (12 participants) refused to participate for various reasons (see Fig. 1). While 42 participants were desired based on power analysis, the authors had to proceed with fewer due to slow recruitment. Due to the waitlist control study design and scheduled group exercise sessions, rolling recruitment was impossible. Only three participants dropped out over the course of the intervention, including one participant who dropped out after finishing the exercise intervention. There was no significant difference between groups in the baseline demographic characteristics (Table 2). There are 22 data points (FtF
3.1Feasibility
3.1.1Retention rate and completion rate
The retention rate of participants over the course of the entire study including follow up was 78.9% (15 of 19 participants) across both groups, and individual group retention rates were 80% (8 of 10 participations) in the FtF group and 77.8% (7 of 9 participations) in the Vir group. Prior to starting the intervention, one participant in each group independently acquired a significant health condition unrelated to the study and discontinued participation. The rate of completion of the intervention for the remaining participants was 88.9% (8 of 9) in the FtF group and 100% (8 of 8) in the Vir group.
3.1.2Attendance rate
Attendance rates were calculated only for participants who completed the entire exercise intervention. The attendance rate of the FtF group was 88.5
3.1.3Reported adverse events
In the FtF group, one participant reported experiencing moderate dizziness and nausea while performing myofascial cervical massage during the last fifteen minutes of the initial exercise class. This incident led to the participant’s withdrawal from the study. Additionally, in the Vir group, at the 9th week, one participant reported experiencing an exacerbation of back pain; however, they were able to resume after a 5-day break. These two reported events were considered to be related to the exercise intervention. We did not report them to the IRB as they were categorized as “not unanticipated” events, given their expected nature in the context of exercise or massage interventions. The participants were informed of these and other possible negative experiences prior to initiating the interventions. The instructor noted that a few participants mentioned feeling fatigued, experiencing muscle soreness, or mild nausea during and after some of the exercise classes, but during each of those instances participants declined to file a report when the instructor asked if they wished to do so. No severe or unexpected adverse events were observed at any point.
3.2Participant-reported outcomes
An evaluation of our dataset revealed that 45.0% of the data satisfied the requisite assumptions for conducting an RMANOVA. We observed a statistically significant time effect between pre- and post-intervention on ODI (F(1, 19)
Figure 2.
Modified Oswestry Low Back Pain Disability Questionnaire (range 0–100); (B) Visual Analog Scale (range 0–10); (C–J) 36-Item Short Form Survey domains (range 0–100). For the Face-to-Face (FtF) and Virtual (Vir) groups, the pre-intervention data was compared to postintervention and follow-up data. For the Control group, the pre-intervention data was compared to the postintervention data; follow-up data does not exist due to the study design.
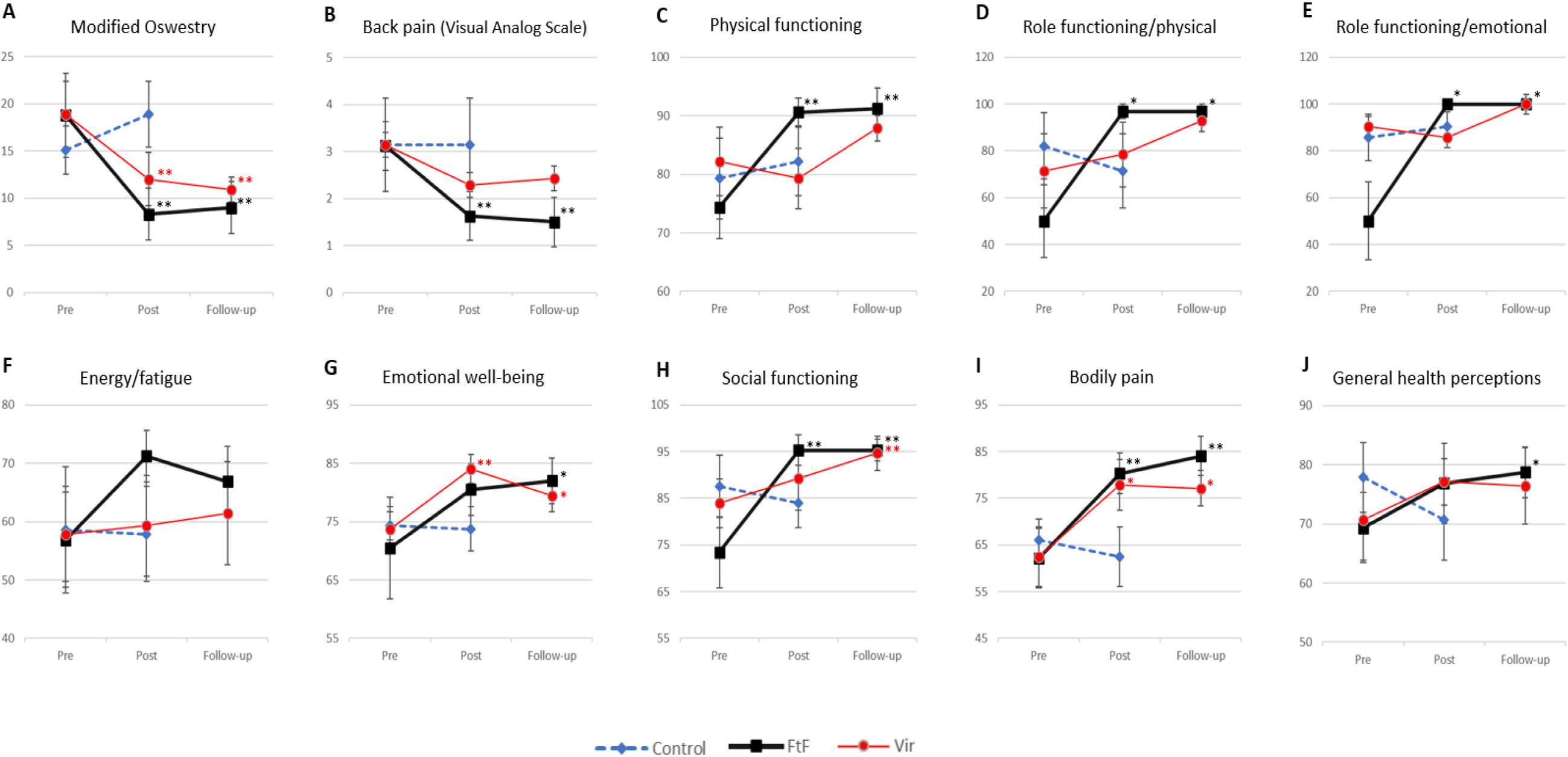
Figure 2 summarizes the ODI, VAS, and SF-36 for the pre-intervention, post-intervention, and follow-up assessment time points and significant differences with results of the Wilcoxon test.
3.3Researcher-measured outcomes
Figure 3.
Changes in researcher-measured outcomes by Wilcoxon testing. * P0.10, **P 0.05. (A–J) The pain pressure threshold (PPT) of different muscles assessed. A higher value means more pressure was required to elicit pain. For the Face-to-Face (FtF) and Virtual (Vir) groups, the pre-intervention data was compared to post-intervention and follow-up data. For the Control group, the pre-intervention data was compared to the post-intervention data; follow-up data does not exist due to the study design. Abbreviations: L, left; R, right.
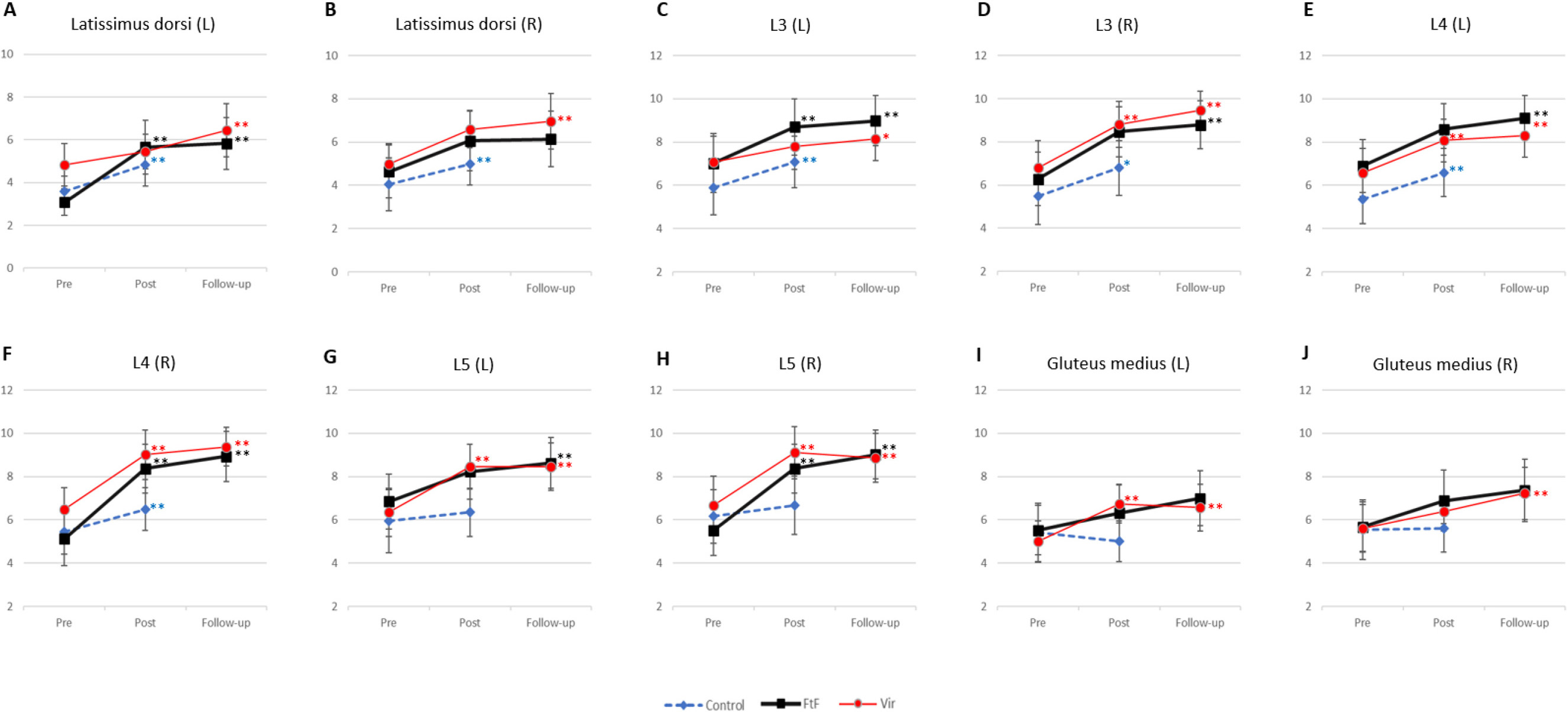
Figure 4.
Changes in researcher-measured outcomes by Wilcoxon testing. * P0.10, **P 0.05. (A–T) The muscle tone (MT) of different muscles assessed. A higher MT frequency creates a higher value. For the Face-to-Face (FtF) and Virtual (Vir) groups, the pre-intervention data was compared to post-intervention and follow-up data. For the Control group, the pre-intervention data was compared to the post-intervention data; follow-up data does not exist due to the study design. Abbreviations: LF, left frequency; RF, right frequency; LS, left stiffness; RF, right stiffness.
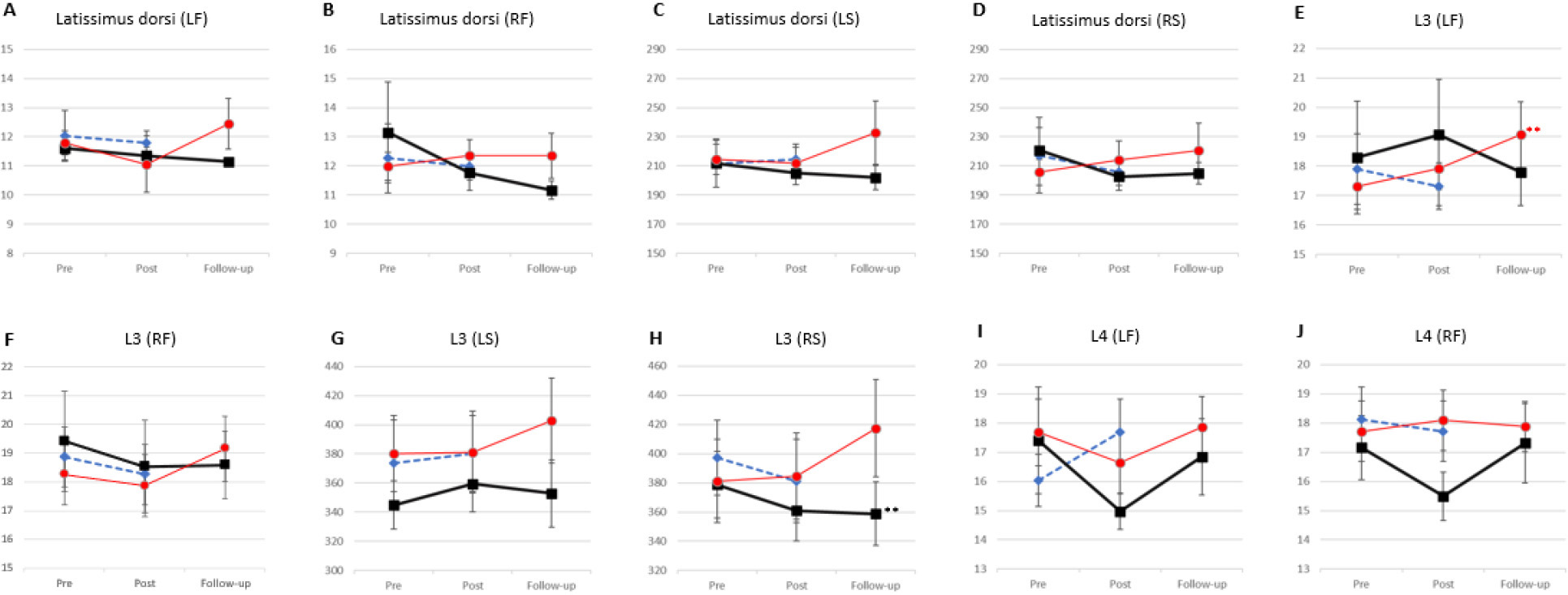
Figure 4.
continued.
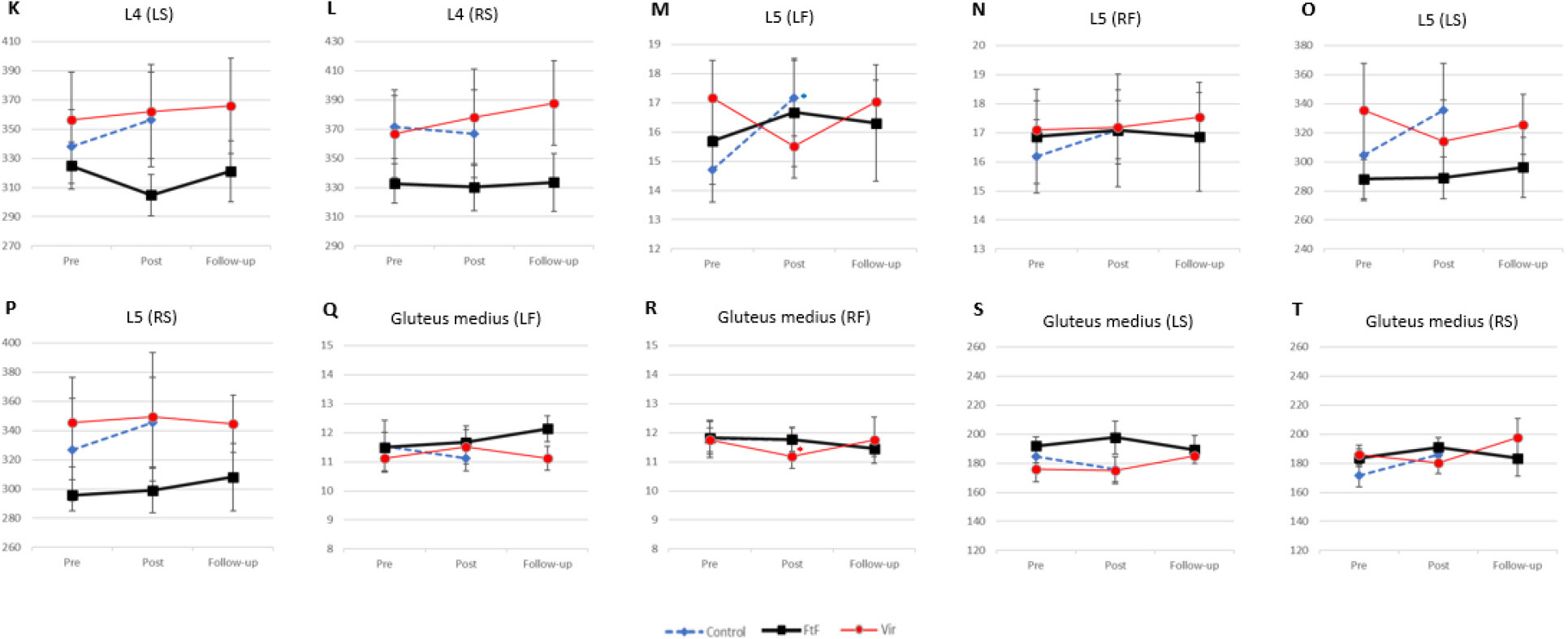
For the purposes of statistical analysis, 37.1% of data met assumptions for conducting RMANOVA. We observed a statistically significant time effect between pre- and post-intervention on pain of gluteus medius on the left (F(1, 19)
4.Discussion
This study examined the feasibility and efficacy of a 12-week SNPE program for chronic low back pain in both the FtF and Vir contexts. The results showed improvements in ODI, VAS, and several domains of quality-of-life measures on SF-36 as well as high rates of program adherence with a low rate of adverse events. These data suggest that SNPE programs for chronic low back pain are feasible and could potentially reduce pain and improve quality of life.
Tracking adherence data such as retention, attendance, and adverse events in a feasibility study is essential for evaluating the practicality, safety, and potential success of the intervention as prior studies have shown adherence to be an important connection between the process and outcome of health interventions [28]. In the current study, both the FtF and Vir groups had high retention rates and attendance rates. This is qualified, however, by noting that the data in the literature regarding monitoring adherence is quite variable, as different studies use different exercise interventions and there is no accepted standard for monitoring this parameter [28]. The closest approximation of the current study to our knowledge was a 2018 investigation into the efficacy of a stretching exercise program on CLBP done over 24 weeks, which reported a retention rate of 70% and that participants attended an average of 42% of the classes in the program [29]. This is significantly lower than what our data show. Participant withdrawal did affect our adherence rate; however, only a single patient withdrew and the reason for withdrawal was an adverse event. Our low rate of participant withdrawal is consistent with prior studies on chronic low back pain [30].
After 12 weeks of training, participant-reported outcomes data showed that both experimental groups improved on several parameters, while there were essentially no improvements in the control group. Our data showed a statistically significant improvement in ODI by 10.5% in the FtF group and 6.9% in the Vir group. The improvement in ODI for the FtF group is notable in that it exceeds the minimally clinically important change (MCIC) threshold of 10% [31]. These findings underscore the effectiveness of our intervention in improving functional outcomes among individuals with low back pain in the FtF group. The authors of the current study believe the change in the Vir group is relevant as well, though it is less than the MCIC. The reason for this assertion is that our scale width was especially narrow, i.e. our participant’s baseline ODI were clustered around low values (18.8 in FtF, 18.9 in Vir, and 15.1 in Con). A comparative study examining psychometric tests for LBP including the ODI determined scale width to be adequate if fewer than 15% of the participants had pre-intervention values at the lower or upper end of the scale [32]. Thus, the baseline scores in the present study may be insufficient to allow change to be reliably detected, and the typical MCIC threshold may not be as relevant. The improvement seen in the Vir group may indeed represent meaningful change, but larger studies are needed [33].
The data also showed a statistically significant 15% improvement in VAS scores in the FtF group, which exceeds the minimally important difference of an absolute reduction of 10% described by Dworkin et al. [34]. While VAS improved by 9% in the Vir group, the change was not statistically significant. The authors propose the lack of statistical significance may have been driven in part by low baseline values and small sample size [33, 35].
Health-related quality of life, as measured by the SF-36, improved in multiple domains in both the FtF and Vir groups after 12 weeks of SNPE. There were statistically significant improvements in the FtF group in the domains of bodily pain (BP), physical function (PF), role limitation due to physical (RP) / emotional health (RE), and social functioning (SF). In the Vir group there were statistically significant improvements in BP and emotional well-being (EW). While many other studies in the literature have assessed quality of life, no consistent measurement has been used, making comparisons to other studies difficult [36, 37]. A systematic review and meta-analysis on the efficacy of Pilates in CLBP patients, however, did report improvements in PF, RP, BP, and general health, which aligns with our findings [38].
Our RMANOVA testing revealed no significant differences in the magnitude of improvements between the FtF and Vir groups. However, upon further analysis using non-parametric testing, areas of significant improvement were observed in the FtF group. The control group did not show any statistically significant improvements. No group showed statistically significant worsening on participant-reported outcomes. All statistically significant improvements in ODI, VAS, and SF-36 were found to be persistent on 12-week follow up.
Researcher-reported outcomes, PPT and MT, were also assessed. The authors judged PPT and MT to be appropriate outcome measures for this study as muscle pain sensitivity can be a cause of pain and dysfunction, and MT reflects the intrinsic stiffness of muscles at rest and can significantly impact overall physical comfort [26, 39]. Measuring these parameters can provide objective data on changes to the body after an intervention, in addition to subjective data from surveys and pain reports. We expected statistically significant improvements in PPT and MT after the intervention; however, these outcomes were not captured. PPT improved in most muscles in all groups, including the control group. MT did not have a clear trend in any group. Previous studies demonstrated that pain and muscle tension in the cervical and lumbar regions were effectively reduced through techniques like massage and acupressure, irrespective of whether they were administered by a practitioner or as self-directed interventions [40]. In the present study, self-directed interventions in the form of SNPE tools were used. It is unclear why our findings are not consistent with prior studies. Regardless, the PPT and MT data contribute to the body of research on interventions for CLBP and underscore the need for further investigation.
The present study has several strengths. We put considerable effort into addressing possible bias by ensuring complete blinding between the data collector, the participant assessors, and the data analysts. Additional efforts to maintain scientific rigor included keeping participant data secure via a robust online platform throughout all stages of data management and opting to monitor adverse events. The data produced supports the primary research goal of demonstrating the feasibility of SNPE as an intervention for CLBP. Bowen et al have identified eight general areas of focus around which they create feasibility studies in the public health sphere, and the stated goal of publishing this framework was to supplement the paucity of available guidelines [41]. Our study touched upon several areas: acceptability, demand, implementation, practicality, and limited-efficacy testing.
The present study has several limitations, as well. The most salient limitation of our study is the small sample size. In our case, recruitment was slow, and many potential participants who approached the research team later declined communication after details of the study were given. This is thought to be secondary to strict eligibility criteria, concerns about COVID-19 exposure, the requirement for dedication to nine months of intervention and follow up, and the study being conducted in a very low population density area. Excluding those who were planning interventions for low back pain, those with BMI
Due to the waitlist control study design in which the participants who were ultimately allocated to the Vir group started the study as the Con group, it was not possible to perform a follow-up assessment on the Con group for any outcome measure. The waitlist control design with in-person instruction also presents an inherent possibility of performance bias, as psychological factors related to in-person versus virtual training, or the knowledge of to which group the participant has been assigned, could influence motivation and performance of participants as well as scoring of subjective outcome measures of pain or quality of life such as VAS, ODI and SF-36. Subjective outcome measures can also vary greatly between individuals and this can potentially impact statistical analysis, especially in smaller sample sizes.
The results of the statistical analysis of adherence between the FtF and Vir groups bear special note, as by necessity direct comparison was not methodologically possible. The experience of a person participating in an in-person or online SNPE program outside the context of a research study may indeed be different, however; for example, in-person participants may be more likely to attend for long periods of time due to social reasons, and those using online courses may exercise more sporadically as their schedule allows [42]. The benefits realized through these different modalities may differ in some ways and our study design does not allow such granular evaluation.
Statistical analysis was further limited by our data being non-normally distributed. Our data therefore did not meet all assumptions necessary to use the desired statistical test repeated measures ANOVA, which can provide valuable information about the overall patterns of change and group differences. To address this, we complemented the parametric analysis with non-parametric Wilcoxon tests. These tests are less sensitive to data distribution and provide a robust alternative for confirming the patterns of change and time differences observed [43]. In addition, given the relatively small sample size and the exploratory nature of our study, the level of statistical significance was set at
Finally, it bears mentioning that the participant demographic characteristics do not approximate the US nor global population. Participants were primarily female and Caucasian, and overall frequency of participants with overweight or higher BMI was significantly lower (42%) than the US average (82.3%) [44]. Future studies would benefit from evaluating a larger and more diverse population especially with regards to gender, age, and geographic location as well as evaluate the sustainability of the captured benefits.
5.Conclusion
Our data support the feasibility of SNPE exercise programs, done in person or virtually, for CLBP. It is unlikely these programs cause harm, and likely that they create benefit in a number of domains. Our results should not be overinterpreted, as this study was limited by small sample size, focused demographics, non-normal data distribution, and methodological constraints on directly comparing the FtF and Vir groups. Future studies would benefit from evaluating a larger and more diverse population especially with regards to gender, age, and geographic location as well as evaluate the sustainability of the captured benefits.
Author contributions
AS, JJ, and JB designed the study. AS is primary investigator and secured funding. Data collection and management performed by JL and JB. Analysis and interpretation of data performed by AS, JJ, and JB. AS and JJ drafted the article. All authors performed critical revision of the article for important intellectual content and approved the final version of the manuscript.
Data availability
The data supporting the findings of the present study are available from the corresponding author upon reasonable request.
Ethical approval
This research was conducted in accordance with the Declaration of Helsinki and approved by Advarra IRB (Pro00055003). The clinical trial is registered on ClinicalTrials.gov (NCT05136729).
Funding
This work was supported by Curing Co., Ltd.
Informed consent
All participants provided signed informed consent for their inclusion in the research.
Acknowledgments
The authors wish to acknowledge all participants for so kindly giving their time. They would also like to acknowledge Laurie Riemann, Yvonne Mullowney, and the rest of the team in the Collaborative Science and Innovation department at Billings Clinic involved in the administration, data management, and coordination for this project. They also acknowledge Heejin Lee, PhD and Jiyoo Yoon, PhD, for their tireless work facilitating communication between Curing, Co., Ltd. and the research team.
Conflict of interest
The authors received compensation from the following grant for their work on this project. A pre-trial agreement between the authors and Curing ensured that the results would be published regardless of the outcome. Otherwise, they have no conflicts of interest to disclose.
References
[1] | Waterman BR, Belmont PJ, Schoenfeld AJ. Low back pain in the United States: incidence and risk factors for presentation in the emergency setting. Spine J Off J North Am Spine Soc. (2012) ; 12: (1): 63-70. |
[2] | Research CI of M (U S) C on AP. Relieving Pain in America? A Blueprint for Transforming Prevention, Care, Education, and Research. National Academies Press; (2011) . |
[3] | Rubin DI. Epidemiology and risk factors for spine pain. Neurol Clin. (2007) ; 25: : 353-71. doi: 10.1016/j.ncl.2007.01.004. |
[4] | Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, et al. What low back pain is and why we need to pay attention. Lancet Lond Engl. (2018) ; 391: : 2356-67. doi: 10.1016/S0140-6736(18)30480-X. |
[5] | Low Back Pain Fact Sheet |
[6] | Qaseem A, Wilt TJ, McLean RM, Forciea MA. Noninvasive treatments for acute, subacute, and chronic low back pain: A clinical practice guideline from the American college of physicians. Ann Intern Med. (2017) ; 166: : 514-30. doi: 10.7326/M16-2367. |
[7] | Searle A, Spink M, Ho A, Chuter V. Exercise interventions for the treatment of chronic low back pain: a systematic review and meta-analysis of randomised controlled trials. Clin Rehabil. (2015) ; 29: : 1155-67. doi: 10.1177/0269215515570379. |
[8] | Hayden JA, van Tulder MW, Malmivaara A, Koes BW. Exercise therapy for treatment of non-specific low back pain. Cochrane Database Syst Rev. (2005) ; CD000335. doi: 10.1002/14651858.CD000335.pub2. |
[9] | Rainville J, Hartigan C, Martinez E, Limke J, Jouve C, Finno M. Exercise as a treatment for chronic low back pain. Spine J. (2004) ; 4: : 106-15. doi: 10.1016/S1529-9430(03)00174-8. |
[10] | Yoon J, Choi J, Shin M. Self-natural posture exercise and chronic pain reduction. Soc Behav Personal Int J. (2019) ; 47: : 1-11. doi: 10.2224/sbp.8273. |
[11] | Choi J, Yoon J, Shin M. Effects of pain reduction by self-natural posture exercise on affective complexity in women: the moderating effect of self-regulation. Front Psychol. (2020) ; 11. doi: 10.3389/fpsyg.2020.01317. |
[12] | Anar SÖ. The effectiveness of home-based exercise programs for low back pain patients. J Phys Ther Sci. (2016) ; 28: : 2727-30. doi: 10.1589/jpts.28.2727. |
[13] | Williams G, Ada L. The safety and accuracy of home-based ballistic resistance training for people with neurological conditions. Physiother Theory Pract. (2023) ; 39: : 2015-24. doi: 10.1080/09593985.2022.2059422. |
[14] | Cooley D, Bailey J, Jermyn R. Cost comparison of osteopathic manipulative treatment for patients with chronic low back pain. (2021) ; 121: : 635-42. doi: 10.1515/jom-2020-0238. |
[15] | Miyamoto GC, Lin C-WC, Cabral CMN, Dongen JM van, Tulder MW van. Cost-effectiveness of exercise therapy in the treatment of non-specific neck pain and low back pain: a systematic review with meta-analysis. Br J Sports Med. (2019) ; 53: : 172-81. doi: 10.1136/bjsports-2017-098765. |
[16] | Deckers K, De Smedt K, Mitchell B, Vivian D, Russo M, Georgius P, et al. New therapy for refractory chronic mechanical low back pain – Restorative neurostimulation to activate the lumbar multifidus: One year results of a prospective multicenter clinical trial. Neuromodulation Technol Neural Interface. (2018) ; 21: : 48-55. doi: 10.1111/ner.12741. |
[17] | Fairbank JCT, Pynsent P. The Oswestry Disability Index. Spine. (2000) ; 25: (22): 2940-52; discussion 2952. |
[18] | Delgado DA, Lambert BS, Boutris N, McCulloch PC, Robbins AB, Moreno MR, et al. Validation of digital visual analog scale pain scoring with a traditional paper-based visual analog scale in adults. JAAOS Glob Res Rev. (2018) ; 2. |
[19] | Faul F, Erdfelder E, Buchner A, Lang A-G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav Res Methods. (2009) ; 41: : 1149-60. doi: 10.3758/BRM.41.4.1149. |
[20] | Owen PJ, Miller CT, Mundell NL, Verswijveren SJJM, Tagliaferri SD, Brisby H, et al. Which specific modes of exercise training are most effective for treating low back pain? Network meta-analysis. Br J Sports Med. (2020) ; 54: : 1279-87. doi: 10.1136/bjsports-2019-100886. |
[21] | Lakens D. Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front Psychol. (2013) ; 4: : 863. doi: 10.3389/fpsyg.2013.00863. |
[22] | Smeets R, Köke A, Lin C-W, Ferreira M, Demoulin C. Measures of function in low back pain/disorders: Low Back Pain Rating Scale (LBPRS), Oswestry Disability Index (ODI), Progressive Isoinertial Lifting Evaluation (PILE), Quebec Back Pain Disability Scale (QBPDS), and Roland-Morris Disability Questionnaire (RDQ). Arthritis Care Res. (2011) ; 63: : S158-73. doi: 10.1002/acr.20542. |
[23] | Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res. (2011) ; 63: (Suppl 11): S240-252. doi: 10.1002/acr.20543. |
[24] | Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36); (1992) . |
[25] | Hawley-Hague H, Horne M, Skelton DA, Todd C. Review of how we should define (and measure) adherence in studies examining older adults’ participation in exercise classes. BMJ Open. (2016) ; 6. doi: 10.1136/bmjopen-2016-011560. |
[26] | Falaguera-Vera FJ, Garcia-Escudero M, Bonastre-Férez J, Zacarés M, Oltra E. Pressure point thresholds and ME/CFS comorbidity as indicators of patient’s response to manual physiotherapy in fibromyalgia. Int J Environ Res Public Health. (2020) ; 17: . |
[27] | Wang J-S. Therapeutic effects of massage and electrotherapy on muscle tone, stiffness and muscle contraction following gastrocnemius muscle fatigue. Soc Phys Ther Sci. (2017) ; 29: : 144-7. doi: 10.1589/jpts.29.144. |
[28] | Jordan JL, Holden MA, Mason EE, Foster NE. Interventions to improve adherence to exercise for chronic musculoskeletal pain in adults. Cochrane Database Syst Rev. (2010) . doi: 10.1002/14651858.CD005956.pub2. |
[29] | Brodsky M, Hansen A, Bjerke W. Randomized Pilot Trial for a Community-Based Group Stretching Exercise Program for Chronic Low Back Pain. Glob Adv Health Med. (2019) ; 8. doi: 10.1177/2164956119846055. |
[30] | Saragiotto BT, Maher CG, Yamato TP, Costa LO, Menezes Costa LC, Ostelo RW, et al. Motor control exercise for chronic non-specific low-back pain. Cochrane Database Syst Rev 2016; (2016) . doi: 10.1002/14651858.CD012004. |
[31] | Ostelo RWJG, Vet HCW de. Clinically important outcomes in low back pain. Best Pract Res Clin Rheumatol. (2005) ; 19: : 593-607. doi: 10.1016/j.berh.2005.03.003. |
[32] | Davidson M, Keating JL. A comparison of five low back disability questionnaires: reliability and responsiveness. Phys Ther. (2002) ; 82: : 8-24. doi: 10.1093/ptj/82.1.8. |
[33] | Sainani KL. Putting p values in perspective. PM&R. (2009) ; 1: : 873-7. doi: 10.1016/j.pmrj.2009.07.003. |
[34] | Dworkin RH, Turk DC, Wyrwich KW, Beaton D, Cleeland CS, Farrar JT, et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain. (2008) ; 9: : 105-21. doi: 10.1016/j.jpain.2007.09.005. |
[35] | Page P. Beyond statistical significance: Clinical interpretation of rehabilitation research literature. (2014) ; 9: . |
[36] | Geneen LJ, Moore RA, Clarke C, Martin D, Colvin LA, Smith BH. Physical activity and exercise for chronic pain in adults: an overview of Cochrane reviews. Cochrane Database Syst Rev 2017; (2020) . doi: 10.1002/14651858.CD011279.pub3. |
[37] | Hayden JA, Ellis J, Ogilvie R, Malmivaara A, Van Tulder MW. Exercise therapy for chronic low back pain. Cochrane Database Syst Rev 2021; (2021) . doi: 10.1002/14651858.CD009790.pub2. |
[38] | Yu Z, Yin Y, Wang J, Zhang X, Cai H, Peng F. Efficacy of pilates on pain, functional disorders and quality of life in patients with chronic low back pain: A systematic review and meta-analysis. Int J Environ Res Public Health. (2023) ; 20: : 2850. doi: 10.3390/ijerph20042850. |
[39] | Janda V. Introduction to Assessment of the most common shortened muscle groups. Muscle Funct Test. Elsevier; (1983) ; 224-7. doi: 10.1016/B978-0-407-00201-2.50069-0. |
[40] | Kerautret Y, Di Rienzo F, Eyssautier C, Guillot A. Selective effects of manual massage and foam rolling on perceived recovery and performance: Current knowledge and future directions toward robotic massages. Front Physiol. (2020) ; 11: : 598898. doi: 10.3389/fphys.2020.598898. |
[41] | Bowen DJ, Kreuter M, Spring B, Cofta-Woerpel L, Linnan L, Weiner D, et al. How We Design Feasibility Studies. Am J Prev Med. (2009) ; 36: : 452-7. doi: 10.1016/j.amepre.2009.02.002. |
[42] | Couper MP, Alexander GL, Zhang N, Little RJ, Maddy N, Nowak MA, et al. Engagement and retention: Measuring breadth and depth of participant use of an online intervention. J Med Internet Res. (2010) ; 12: : e52. doi: 10.2196/jmir.1430. |
[43] | Erceg-Hurn DM, Mirosevich VM. Modern robust statistical methods: An easy way to maximize the accuracy and power of your research. Am Psychol. (2008) ; 63: : 591-601. doi: 10.1037/0003-066X.63.7.591. |
[44] | Ogden CL, Fryar CD, Martin CB, Freedman DS, Carroll MD, Gu Q, et al. Trends in Obesity Prevalence by Race and Hispanic Origin – 1999–2000 to 2017–2018. JAMA. (2020) ; 324: : 1208. doi: 10.1001/jama.2020.14590. |




