Effects of anti-osteoporosis treatment in elderly patients with osteoporosis and lumbar discectomy and fusion
Abstract
BACKGROUND:
The effect of anti-osteoporosis treatment in elderly patients with osteoporosis and lumbar discectomy and fusion (LIF) for lumbar degenerative diseases is not well known.
OBJECTIVE:
This study aimed to evaluate the effect of perioperative anti-osteoporosis treatment in the patients with osteoporosis and LIF.
METHODS:
From January to December 2022, patients were divided into three groups according to the inclusive criteria: the normal group (Group A), the osteopenia group (Group B) and the osteoporosis group (Group C). Quantitative computed tomography (QCT), height of the intervertebral space (HIS), segmental sagittal angle (SSA), visual analogue scale (VAS) score and Oswestry Disability Index (ODI) were compared between the groups at the follow-up time. The serum Ca2 + , osteocalcin (OC), propeptide of type I procollagen (PINP) C-terminal cross-linking telopeptide of type I collagen (
RESULTS:
There were 165 patients in this study. There were significant differences in the mean age, mean score, HIS and SSA between the groups at the different follow-up times. There were significant differences in the concentrations of serum Ca2 + , OC,
CONCLUSION:
In elderly patients with LIF and osteoporosis, anti-osteoporosis therapy could reduce bone resorption and thus facilitate fusion. Anti-osteoporosis medication tends to enhance radiological, functional, and fusion short-term outcomes.
1.Introduction
Posterior lumbar interbody fusion (PLIF) and transforaminal lumbar interbody fusion (TLIF) with segmental pedicle screws are common procedures for treating lumbar degenerative disorders that relieve pain and enhance function [1, 2]. However, as more people experience spinal fusion, the number of fusion-related problems has risen [3, 4]. There have been reports of adjacent vertebral body fractures caused by rigid pedicle screw fixation [5, 6]. The reason for this is that arthrodesis may modify spinal kinematics, resulting in relative hypermobility of spinal segments next to the fused level [7, 8]. This alteration in segmental spinal biomechanics could lead to a higher rate of vertebral compression fractures (VCFs). Especially among elderly patients, osteoporosis further increases fracture risk.
After spinal fusion surgery, rigid spinal instrumentation can cause device-related osteoporosis of the fused segment, as well as a decrease in the bone mineral density (BMD) of adjacent vertebrae, which can contribute to adjacent level VCFs [9, 10, 11]. Moreover, osteoporosis increases the risk of fractures in elderly individuals. The decrease in BMD could be due to immobilization or to changes in biomechanics caused by arthrodesis. However, the mechanism of BMD loss after spinal fusion surgery, is yet unknown. Zoledronic acid (ZA) has been shown to be an effective osteoporosis treatment in postmenopausal women in several studies, as it significantly reduces the risk of vertebral, hip, and other fractures [12]. Additionally perioperative ZA treatment may offer protection against a significant decrease in the BMD of cephalad vertebrae after spinal fusion surgery among postmenopausal women with osteoporosis [13].
Denosumab is a biological product that blocks the RANK ligand (RANKL)-mediated activation of osteoclasts. It has been demonstrated to be useful in treating osteoporosis [14], with effectiveness comparable to that of bisphosphonate [15]. However, to our knowledge, no previous study has evaluated the effect of denosumab on the change in the BMD of the adjacent vertebral body after instrumented intervertebral fusion, fusion time, or operation. As a result, the goal of this study was to determine whether denosumab can increase the BMD of the adjacent vertebral body after spinal surgery while also improving the fusion time and outcome of the operative segment.
2.Methods
2.1Study design
This study was conducted from January to December 2022. The study protocol was approved by the Ethics Committee of Tianjin First Central Hospital (approval ID: 2022N122KY).
Written informed consent was obtained from all study participants and confidentiality of information was assured.
2.2Study patients
The medical records of consecutive patients admitted for lumbar degenerative diseases (LDDs), including lumbar disc herniation (LDH) with instability, lumbar spinal stenosis (LSS), degenerative spondylolisthesis (DSI), isthmic spondylolisthesis (IS) and degenerative scoliosis (DS) to the hospital from January to December 2022 were collected.
Figure 1.
HIS before and after surgery.
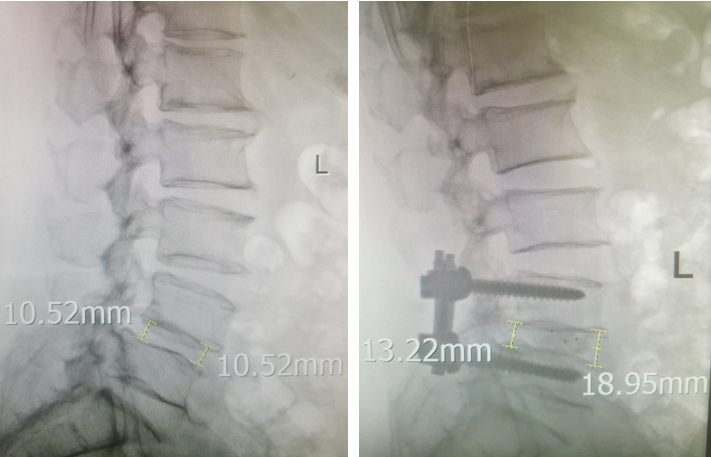
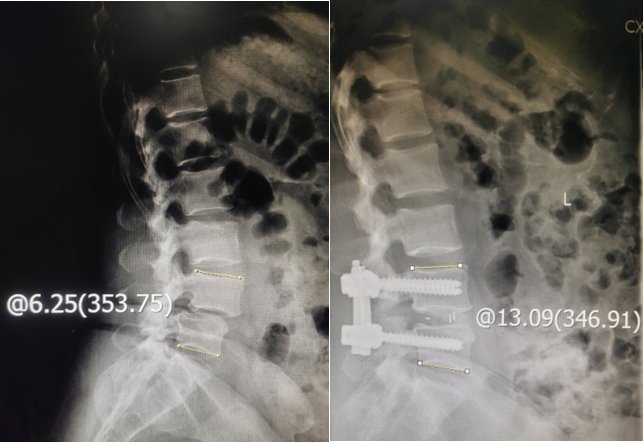
Figure 2.
SSA before and after surgery.
Inclusion criteria: 1) X-ray, computed tomography (CT) and quantitative computed tomography (QCT, Siemens Edge, the measuring software was QCT Pro from Midways, www.QCT.com) and magnetic resonance imaging (MRI) results were obtained; 2) Serum Ca2 + , osteocalcin (OC), propeptide of type I procollagen (PINP) C-terminal cross-linking telopeptide of type I collagen (
Exclusion criteria: 1) required intervertebral fusion of
2.3Surgical procedure
All patients underwent PLIF or TLIF. A posterior midline incision was made and the posterior elements of the spine were exposed. After pedicle screw insertion, a medial facetectomy was performed. Then the nerve root was mobilized medially to access the disc space. In the TLIF procedure, the superior and inferior articular processes of the facet joint are resected and the disc in the neuroforamen is exposed. After removal of the disc and scraping of the endplates, the anterior part of the disc space is packed with autologous bone chips. The disc space is measured by trial insertion of variously sized spacers and a sizeable cage is inserted. All patients were asked to use a lumbar brace while walking for 4–6 weeks after surgery.
2.4Imaging parameters
HIS was measured via X-ray before surgery, after surgery and at the last follow-up (Fig. 1). The HIS was the average of the anterior and posterior HISs at the same intervertebral space. SSA was measured via X-ray before surgery, after surgery and at the last follow-up (Fig. 2).
2.5Bone metabolic markers
Serum Ca2 + , OC, PINP
2.6Anti-osteoporosis treatment
The anti-osteoporosis treatments used were 1200 mg/ day oral calcium, 800IU/day activated vitamin D and 60 mg subcutaneous injection of denosumab every 6 months for the patients in Group C. Denosumab (American Amgen Inc.) was injected on the sixth day after surgery when the incision was not swollen and exuding. The treatment for patients in Group B was 1200 mg/day oral calcium and 800IU/day activated vitamin D.
2.7Clinical treatment assessment
Table 1
Demographic characteristic of 165 patients with LIF (n-165)
| Characteristics | Group A ( | Group B ( | Group C ( |
|
|---|---|---|---|---|
| Mean age(yr) | 50.7 | 66.0 | 69.1 | |
| Sex, M/F | 13/39 | 12/50 | 2/49 | |
| Follow-up duration (month) | 10.7 | 10.8 | 10.8 | |
| Fusion level | ||||
| 1 level | 30 | 25 | 19 | |
| 2 levels | 20 | 25 | 20 | |
| 3 levels | 2 | 12 | 12 | |
| Total | 76 | 111 | 95 | |
| Mean level | 1.5 | 1.8 | 1.9 |
Figure 3.
According to Mayer’s research, Grade 3, Grade 2 and Grade 1 were idectified at the sixth month after surgery (from left to right).
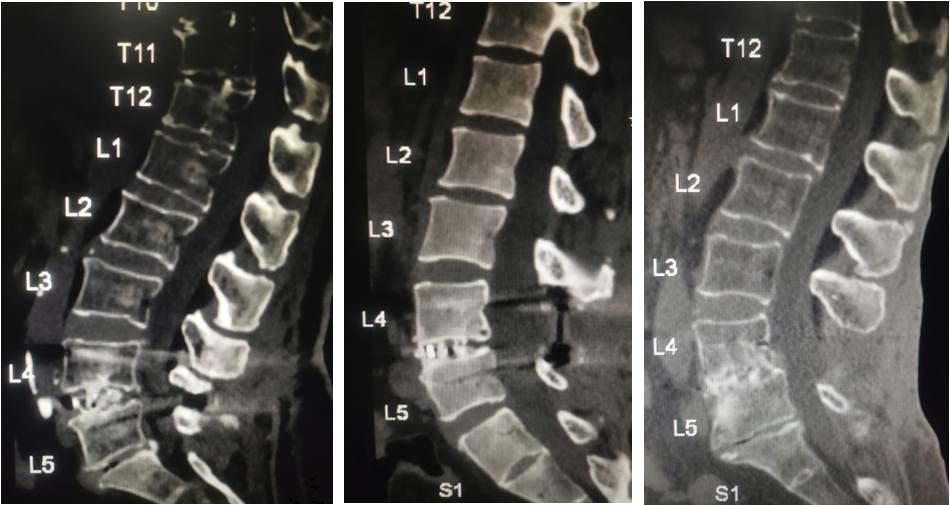
The VAS and ODI scores were assessed before the operation, after the operation and at the last follow-up. Interbody fusion was graded on the X-ray by the method of Brantigan and Steffee [16] as modified to describe the Fraser definition of locked pseudarthrosis (BSF scale) [17] at the third month and last follow-up after surgery. Interbody fusion by CT was performed as described by Mayer et al. [18] at the sixth month after surgery (Fig. 3). According to the CT results of Mayer et al. the definite fusion is Grade 1 or Grade 2.
2.8Statistical analysis
Variables were compared among the three groups using one-way ANOVA and
3.Results
3.1Demography
There were 165 patients in this study including 52 patients in Group A, 62 in Group B and 51 in Group C. Table 1 displays the mean age, follow-up duration, and sex and fusion level of the different groups. There were significant differences in the mean age (
3.2Imaging parameters
Table 2
Comparison of image parameters between different groups (
| Group A ( | Group B ( | Group C ( |
| |
|---|---|---|---|---|
| Preoperative HIS (mm) | 7.9 | 8.9 | 9.0 | |
| Postoperative HIS (mm) | 10.9 | 11.5 | 11.9 | |
| Last follow-up HIS (mm) | 10.5 | 10.9 | 11.8 | |
|
| ||||
| Preoperative SSA (∘) | 15.6 | 16.3 | 17.4 | |
| Postoperative SSA (∘) | 18.8 | 20.5 | 21.3 | |
| Last follow-up SSA (∘) | 18.7 | 19.8 | 21.3 | |
|
|
HIS: Height of intervertebral space; SSA: segmental sagittal angle.
Table 3
Comparison of QCT results between different groups (
| Group A ( | Group B ( | Group C ( |
| |
| BMD (g/cm3) | ||||
| Pre-operation | 138.8 | 108.2 | 64.7 | |
| At the sixth month | 137.5 | 99.1 | 72.1 | |
| | ||||
| T score | ||||
| Pre-operation | 1.3 | |||
| At the sixth month | 1.3 | |||
| |
BMD: Bone mineral density.
Table 2 displays the preoperative, postoperative and last follow-up HIS and SSA. There were significant differences in the HIS among the three groups (
Table 4
Comparison of bone metabolic markers results between different groups (
| Group A ( | Group B ( | Group C ( |
| |
| Serum Ca2 + (mmol/L) | ||||
| Preoperative | 2.3 | 2.3 | 2.2 | |
| At the sixth month after surgery | 2.3 | 2.2 | 2.2 | |
| | ||||
| OC (ng/ml) | ||||
| Preoperative | 21.8 | 18.3 | 16.3 | |
| At the sixth month after surgery | 22.9 | 18.1 | 17.8 | |
| | ||||
| PINP (ng/ml) | ||||
| Preoperative | 42.3 | 39.1 | 40.7 | |
| At the sixth month after surgery | 43.5 | 37.7 | 41.8 | |
| | ||||
| Preoperative | 0.3 | 0.5 | 0.6 | |
| At the sixth month after surgery | 0.3 | 0.6 | 0.5 | |
| | ||||
| 25-OH VD (ng/ml) | ||||
| Preoperative | 37.8 | 15.8 | 16.7 | |
| At the sixth month after surgery | 36.9 | 18.3 | 27.3 | |
| |
OC: Osteocalcin; PINP: Propeptide of type I procollagen;
3.3Bone metabolic markers
Table 4 shows the serum Ca2 + , OC, PINP,
Table 5
Comparison of interbody fusion results between different groups (
| Group A ( | Group B ( | Group C ( |
| |
| X-ray assessment | ||||
| Third month after surgery | ||||
| BSF-1 | 6 | 3 | ||
| BSF-2 | 35 | 48 | 41 | |
| BSF-3 | 17 | 8 | 7 | |
| Last follow-up after surgery | ||||
| BSF-1 | 3 | 1 | ||
| BSF-2 | 3 | 3 | 2 | |
| BSF-3 | 49 | 56 | 48 | |
| CT assessment | ||||
| Sixth month after surgery | ||||
| Grade 1 | 47 | 21 | 19 | |
| Grade 2 | 3 | 19 | 24 | |
| Grade 3 | 2 | 16 | 6 | |
| Grade 4 | 6 | 2 | ||
| VAS | ||||
| Pre-operation | 6.8 | 6.8 | 6.9 | |
| Post-operation | 2.2 | 3.3 | 3.4 | |
| Last follow-up | 0.8 | 1.3 | 1.1 | |
| | ||||
| ODI | ||||
| Pre-operation | 66.2 | 69.2 | 70.1 | |
| Post-operation | 32.9 | 35.8 | 36.2 | |
| Last follow-up | 8.3 | 11.7 | 10.9 | |
| |
VAS: visual analogue scale; ODI: Oswestry Disability Index.
Table 6
Comparison of interbody fusion results of the different diseases according to CT assessment (
| LDH | LSS | DSI | IS | DS | |
|---|---|---|---|---|---|
| Grade 1 | 66 | 11 | 2 | 7 | 1 |
| Grade 2 | 24 | 14 | 1 | 6 | 1 |
| Grade 3 | 2 | 3 | 7 | 5 | 6 |
| Grade 4 | 2 | 2 | 4 |
LDH: lumbar disc herniation with instability; LSS: lumbar spinal stenosis; DSI: degenerative spondylolisthesis, IS: isthmic spondylolisthesis; DS: degenerative scoliosis.
3.4Fusion assessment
Table 5 shows the X-ray results for the BSF at the third month and last follow-up after surgery and Mayer Grade results on the CT scan at the sixth month after surgery. According to the BSF scale, the prevalence of BSF-3 was 94.2% in Group A, 90.3% in Group B and 92.3% in Group C. Grade 1 and Grade 2 were defined according to Mayer’s grade and were 96.2% in Group A, 64.5% in Group B and 78.4% in Group C. There was a significant difference in the percentage of patients with definite fusion between Groups B and C (
Figure 4.
Female patient, 52 yrs, lumbar spondylolisthesis and lumbar disc herniation before surgery, and noramal patient. PLIF was carried out. At the sixth month after surgery the interbody fusion was Grade 1 according to Mayer’s research. The trabeculae were filled with interbody space.
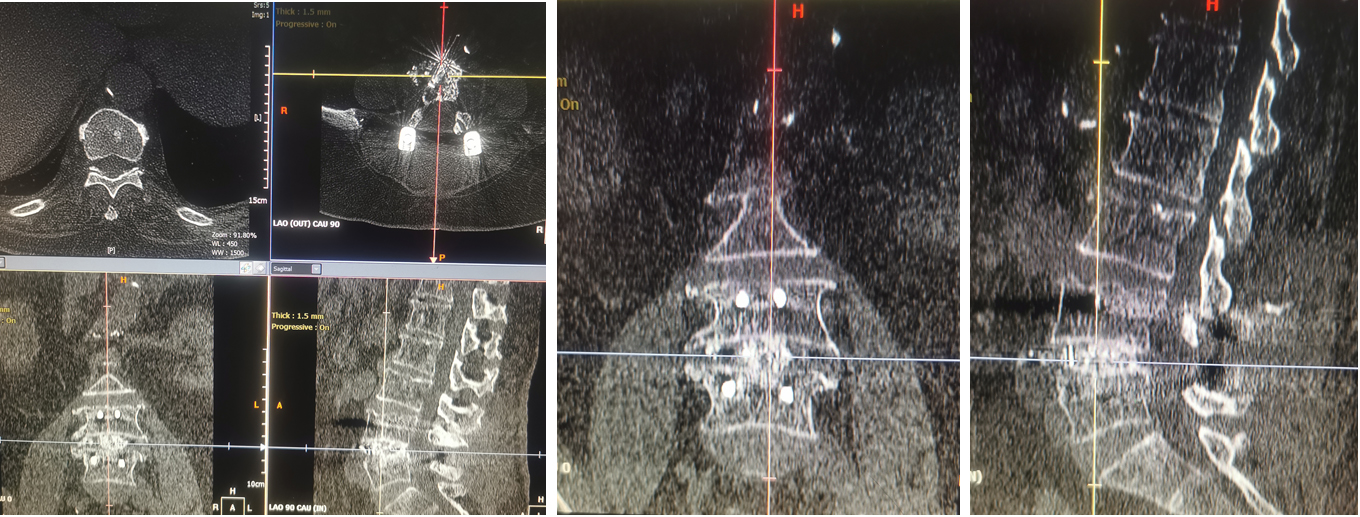
Figure 5.
Female patient, 63 years old, with lumbar spondylolisthesis and lumbar disc herniation before surgery; osteoponia; PLIF; oral calcium 1200mg/day; activated vitamin D 800IU/day before and after sugery. At the sixth month after surgery, the interbody fusion was Grade 3 according to Mayer’s research. The red arrows show the unfused areas; and the trabeculae exhibited a palisade pattern.
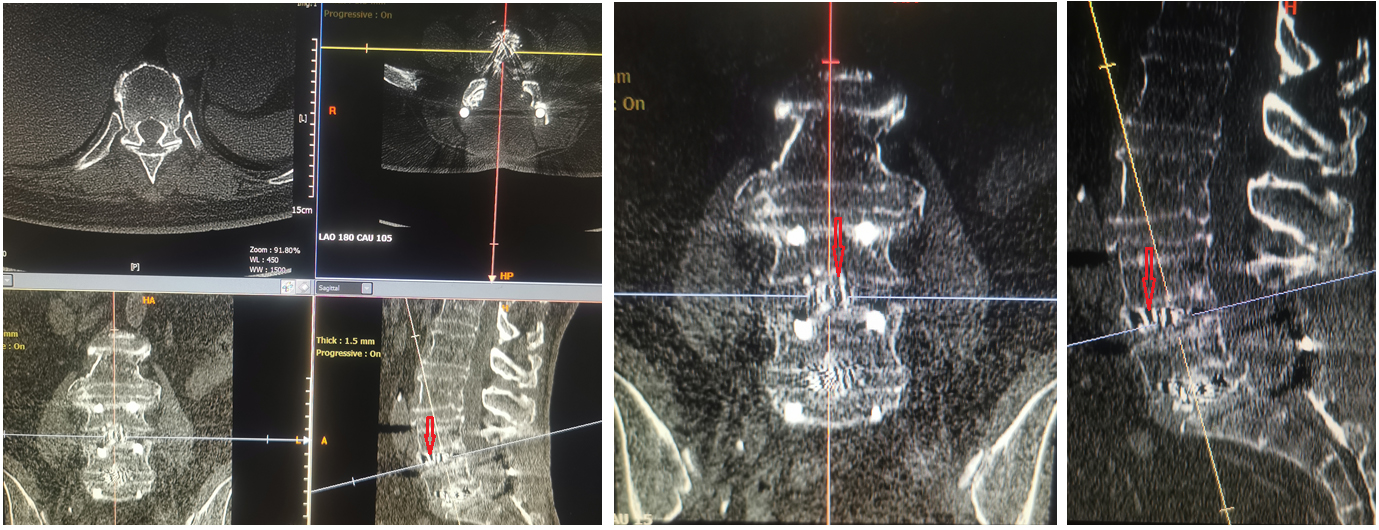
Figure 6.
Female patient, 66 years old, with lumbar spondylolisthesis and lumbar disc herniation before surgery; osteoporosis; PLIF; oral calcium 1200mg/day; and activated vitamin D 800IU/day before and after surgery. Denosumab was injected at the sixth day after surgery. At the sixth month after surgery, the interbody fusion was Grade 2 according to Mayer’s research. The red arrows show the unfused area, which was just a small area, and the other areas were fused.
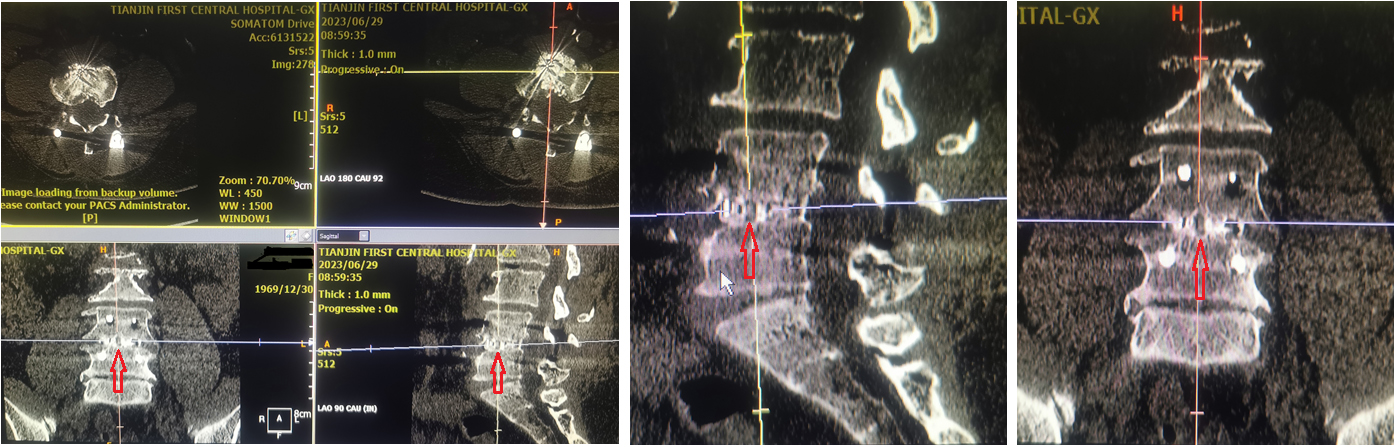
Figure 7.
Female patient, 67 yrs, with lumbar spondylolisthesis and lumbar disc herniation before surgery; osteoponia; PLIF; oral calcium 1200mg/day; and activated vitamin D 800IU/day before and after sugery. At the third month after surgery, the screw pedicle was cut out; and fusion failure occurred.

3.5Clinical treatment assessment
The VAS and ODI scores before surgery, after surgery and at the last follow-up are displayed in the Table 5. There were significant differences in VAS and ODI scores between the same group at the different follow-up times and among the three groups at the last follow-up time. At the sixth month after surgery, Fig. 4 shows a typical case in Group A, Fig. 5 displays a typical case in Group B and Fig. 6 shows a typical case in Group C. Figure 7 displays the screw pedicle cut out and fusion failure at the third month after surgery in Group B.
4.Discussion
Osteoporosis is a silent killer of human health and a major public health concern. In 2006 there were approximately 70 million osteoporotic patients and more than 200 million patients with osteopenia in China [19]. According to previous research, Asians have a lower bone mass than Caucasians and Afro-Caribbeans [20]. LDH, LSS, DSI, IS and DS are common LDDs that occur mostly in elderly patients and need LIF for treatment. In elderly individuals, the osteoporosis and LDD often coexist. Osteoporosis, a degenerative disease characterized by bone loss and structural deterioration, is the most common challenge of LIF. The main cause of osteoporosis in women is menopause, while aging is main cause in men, and is also the main cause of osteopenia.
To restore spinal stability and decompress nerves in elderly patients with LDD and osteoporosis, there have been some reports about the use of cement-augmented pedicle screw fixation to restore spinal stability [21, 22], but these complications may be fatal [23, 24]. One study revealed that the strong pedicle screw fixation could be achieved by increasing the BMD around the screw and prevent fatal complication, this treatment involved anti-osteoporosis treatment during the spinal surgery and the follow-up period [25]. In our study, one patient with osteopenia, spondylolisthesis and lumbar disc herniation underwent PLF, but at the third month after surgery, the screw pedicle was cut out, the reduction effect on lumbar spondylolisthesis was lost, and fusion failed. This patient had no other uncomfortable symptoms except for mild low back pain and was still being followed up. Anti-osteoporosis agents have been shown to result in strong pedicle screw fixation with an increase in the BMD around the screw, but there have been few reports about the effectiveness of anti-osteoporosis agents for fusion of LIF. Our study focused on the short-term effect of LIF fusion during the spinal surgery in combination with denosumab for preventing osteoporosis.
In this study, the HIS and SSA were greater at the last follow-up than at the pre-operation, which demonstrated that the LIF could increase the HIS and improve lumbar lordosis. In the osteopenia group the HIS and SSA at the last follow-up were lower than those at the post-operation, but not in the osteoporosis group. According to some studies patients with low lumbar BMD may have a relatively high incidence of interbody fusion cage-related complications; for example, sinking of the interbody fusion cage may lead to gradual narrowing of the HIS, which affects anterior support of the spine and prevents successful fusion [26]. Several researchers have shown that BMD is related to the stable failure load of the endplate and cage [27, 28]. Additionally the correlation between the BMD and subsidence was very weak, and patients with a score
In our study the serum Ca2 + and 25-OH VD concentrations were greater at six months after surgery than before surgery in the osteopenia and osteoporosis groups, which proves the 1200 mg/day calcium and 00IU/day activated vitamin D 8 was necessary for patients with osteopenia or osteoporosis. There was little change in the bone formation markers including the OC and PINP in the osteopenia and osteoporosis groups, but there was a high variability in the bone resorption marker, which is the
The VAS and ODI scores were improved at the last follow-up compared to the pre-operation. At six months after surgery the rate of definite fusion in the osteoporosis group were greater than that in the osteopenia group. The incidence of osteopenia and osteoporosis was lower than the normal group. According to these studies, the fusion rates were different after treatment with different anti-osteoporosis drugs; for example, one year after surgery, the fusion rate was 95% in the alendronate group [31], but the rate of bone fusion tended to be greater in the weekly teriparatide group than in the bisphosphonate group at the sixth month after surgery (46.8% vs. 32.7%) [32]. One study showed that alendronate does not influence the fusion process in osteoporotic patients, and in alendronate group, fusion was achieved in 66.7% of patients compared to 73.9% of patients in control group (no medication) [33]. The fusion rate was greater in the osteoporosis group than in the osteopenia group, but this difference was detected at only the sixth month according to the QCT. There were three typical cases from three groups: in the normal group the trabeculae fill the intervertebral space and fusion was complete at the sixth month after surgery; but in the osteopenia group the shape of trabeculae was like palisade, there was no trabeculae growth at some areas and lack of bone support, fusion effect was poor at the sixth month after surgery; in the osteoporosis group there was also lack of trabeculae at some areas which were smaller than in the osteopenia group and no shape of palisade area, and the fusion effect was better than the osteopenia group and worse than normal group.
Denosumab is an anti-resorptive agent with a novel mechanism of action [34, 35] and a fully human monoclonal antibody that binds RANKL, preventing RANKL from activating RANK, its receptor on the osteoclast surface [35]. Reducing RANK-RANKL binding inhibits osteoclast formation, function, and survival, which results in a decrease in bone resorption and an increase in bone mass [35, 36, 37]. The mechanism of action of denosumab is different from that of bisphosphonates. The mechanism of action of bisphosphonates includes: 1) a strong affinity for bone embedding in the bone mineral, and crossing cell membranes when osteoclasts resorb the bone matrix; 2) clearance from the circulation via renal excretion or adsorption to bone minerals, but bone-associated drugs must first be released by osteoclast-mediated bone resorption; and 3) residue in the bone for a period of weeks to years. The mechanism of action of denosumab includes: 1) not embedding within bone tissue, binding to RANKL in the extracellular fluid and circulation, and inhibiting osteoclast formation, function and survival; 2) clearing from the bloodstream through the reticuloendothelial system; and 3) maintaining a half-life of approximately 26 days and not inducing the formation of neutralizing antibodies.
The follow-up time varied according to the detection type. Bone metabolic markers were detected at the sixth month after surgery due to injection of denosumab every 6 months. X-ray imaging was carried out at the third and sixth month to assess the degree of facet joint fusion. QCT was assessed at the sixth month to determine the degree of interbody fusion. The detections were carried out as little as possible to avoid unnecessary radiation and pain, except for necessary tests.
This study has several limitations. First, the follow-up time in this study was relatively short, but we think that follow-up time was long enough for patients to preliminarily recover, at which time all patients needed to complete interbody fusion after surgery. However, a prospective study with a larger sample size and longer term follow up should be conducted in the future. Second, this was a single-center-study, and the sample size was small. A multicenter study will be ideal. In addition, the study lacked detailed classification of patients with osteoporosis due to deficiencies in related detection methods.
5.Conclusions
In elderly patients with LIF and osteoporosis anti-osteoporosis therapy could reduce bone resorption and thus facilitate fusion. Anti-osteoporosis medication tends to enhance radiological, functional, and fusion short-term outcomes. The anti-osteoporosis treatment should also be advocated for patients with LIF and osteopenia.
Author contributions
T.S.: initial idea, wrote and revised manuscript and acquired funding. F.Y.S.: data collection, editing and statistical analysis. X.Q.: methodology. T.Z.: data collection. T.D.H.: data collection. W.L.J.: data collection. Q.Z.: data collection. All authors read and approved the final manuscript.
Data availability
The datasets used and/or analyzed in this study are available from the corresponding author on reasonable request.
Ethics approval
Ethical approval was obtained from the Committee for Medical Ethics of Tianjin First Central Hospital (2022N122KY).
Funding
This study was supported by the Osteoporosis Innovation Award Fund of the Chinese Association of Medical Education (2022-011).
Informed consent
Written informed consent was obtained from all study participants and confidentiality of information was assured.
Acknowledgments
The authors are grateful for the support of the Osteoporosis Innovation Award Fund of the Chinese Association of Medical Education.
Conflict of interest
The authors declare that they have no conflict of interest.
References
[1] | Gertzbein SD, Betz R, Clements D, Errico T, Hammerberg K, Robbins S, et al. Semirigid instrumentation in the management of lumbar spinal conditions combined with circumferential fusion. A multicenter study. Spine (Phila Pa 1976). (1996) ; 21: (16): 1918-1925. doi: 10.1097/00007632-199608150-00018. |
[2] | Wang JC, Mummaneni PV, Haid RW. Current treatment strategies for the painful lumbar motion segment: posterolateral fusion versus interbody fusion. Spine (Phila Pa 1976). (2005) ; 30: (16 Suppl): S33-S43. doi: 10.1097/01.brs.0000174559.13749.83. |
[3] | Machado GC, Maher CG, Ferreira PH, Harris IA, Deyo RA, McKay D, et al. Trends, complications, and costs for hospital admission and surgery for lumbar spinal stenosis. Spine (Phila Pa 1976). (2017) ; 42: (22): 1737-1743. doi: 10.1097/BRS.0000000000002207. |
[4] | Rometsch E, Spruit M, Zigler JE, Menon VK, Ouelle JA, Mazel C, et al. Screw-related complications after instrumentation of the osteoporotic spine: a systematic literature review with meta-analysis. Global Spine J. (2020) ; 10: (1): 69-88. doi: 10.1177/2192568218818164. |
[5] | Chiu Y-C, Tsai T-T, Yang S-C, Chen H-S, Kao Y-H, Tu Y-K. Impact of instrumented spinal fusion on the development of vertebral compression fracture. Medicine (Baltimore). (2016) ; 95: (17): e3455. doi: 10.1097/MD.0000000000003455. |
[6] | Li Y-C, Yang S-C, Chen H-S, Kao Y-H, Tu Y-K. Impact of lumbar instrumented circumferential fusion on the development of adjacent vertebral compression fracture. Bone Joint J. (2015) ; 97-B: (10): 1411-1416. doi: 10.1302/0301-620X.97B10.34927. |
[7] | Axelsson P, Johnsson R, Strom̈qvist B. The spondylolytic vertebra and its adjacent segment. Mobility measured before and after posterolateral fusion. Spine (Phila Pa 1976). (1997) ; 22: (4): 414-417. doi: 10.1097/00007632-199702150-00012. |
[8] | Bastian L, Lange U, Knop C, Tusch G, Blauth M. Evaluation of the mobility of adjacent segments after posterior thoracolumbar fixation: a biomechanical study. Eur Spine J. (2001) ; 10: (4): 295-300. doi: 10.1007/s005860100278. |
[9] | Bogdanffy GM, Ohnmeiss DD, Guyer RD. Early changes in bone mineral density above a combined anteroposterior L4-S1 lumbar spinal fusion. A clinical investigation. Spine (Phila Pa 1976). (1995) ; 20: (15): 1674-1678. doi: 10.1097/00007632-199508000-00005. |
[10] | Lipscomb HJ, Grubb SA, Talmage RV. Spinal bone density following spinal fusion. Spine (Phila Pa 1976). (1989) ; 14: (4): 477-479. doi: 10.1097/00007632-198904000-00028. |
[11] | Balci A, Kalemci O, Kaya FG, Akyoldas G, Yucesoy K, Ozaksoy D. Early and long-term changes in adjacent vertebral body bone mineral density determined by quantitative computed tomography after posterolateral fusion with transpedicular screw fixation. Clin Neurol Neurosurg. (2016) ; 145: : 84-88. doi: 10.1016/j.clineuro.2016.04.014. |
[12] | Reid DM, Devogelaer J-P, Saag K, Roux C, Lau C-S, Reginster J-Y. et al. Zoledronic acid and risedronate in the prevention and treatment of glucocorticoidinduced osteoporosis (HORIZON): a multicentre, double-blind, double-dummy, randomised controlled trial. Lancet. (2009) ; 373: (9671): 1253-1263. doi: 10.1016/S0140-6736(09)60250-6. |
[13] | Fan J, Liu T, Dong X, Sun S, Zhang H, Yang C, et al. Effect of Zoledronic Acid on the Vertebral Body Bone Mineral Density After Instrumented Intervertebral Fusion in Postmenopausal Women With Osteoporosis. Global Spine Journal. (2023) ; 13: (5): 1280-1285. doi: 10.1177/21925682211027833. |
[14] | Cummings SR, Martin JS, McClung MR, Siris ES, Eastell R, Reid IR, et al. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. New England Journal of Medicine. (2009) ; 361: (8): 756-65. doi: 10.1056/NEJMoa0809493. |
[15] | Brown JP, Prince RL, Deal C, Recker RR, Kiel DP, de Gregorio LH, et al. Comparison of the effect of denosumab and alendronate on BMD and biochemical markers of bone turnover in postmenopausal women with low bone mass: a randomized, blinded, phase 3 trial. Journal of Bone & Mineral Research. (2009) ; 24: (1): 153-61. doi: 10.1359/jbmr.0809010. |
[16] | Brantigan JW, Steffee AD. A carbon fiber implant to aid interbody lumbar fusion. Two-year clinical results in the first 26 patients. Spine (Phila Pa 1976). (1993) ; 18: (14): 2106-2107. doi: 10.1097/00007632-199310001-00030. |
[17] | Santos ERG, Goss DG, Morcom RK, Fraser RD. Radiologic assessment of interbody fusion using carbon fiber cages. Spine (Phila Pa 1976). (2003) ; 28: (10): 997-1001. doi: 10.1097/01.BRS.0000061988.93175.74. |
[18] | Siepe CJ, Stosch-Wiechert K, Heider F, Amnajtrakul P, Krenauer A, Hitzl W, et al. Anterior stand-alone fusion revisited: a prospective clinical, X-ray and CT investigation. Eur Spine J. (2015) ; 24: (4): 838-851. doi: 10.1007/s00586-014-3642-y. |
[19] | Chinese health promotion fundation editorial board of Chinese White Papers of osteoporosis ((2009) )Chinese White Papers of osteoporosis, Chin J Health Manag. 3: 148-154 |
[20] | Mittal S, Kumar A, Gupta RK, Kapoor S, Gulati P, Shukla DK. Comparison of bone mineral density and its variables between premenopausal and postmenopausal women. J Obstet Gynaecol India. (2011) ; 61: : 200-204. doi: 10.1007/s13224-011-0024-9. |
[21] | Kanno H, Onoda Y, Hashimoto K, Aizawa T, Ozawa H. Reinforcement of Percutaneous Pedicle Screw Fixation with Hydroxyapatite Granules in Patients with Osteoporotic Spine: Biomechanical Performance and Clinical Outcomes. Medicina (Kaunas). (2022) ; 58: (5): 579. doi: 10.3390/medicina58050579. |
[22] | Amendola L, Gasbarrini A, Fosco M, Simoes CE, Terzi S, De Iure F, et al. Fenestrated pedicle screws for cement-augmented purchase in patients with bone softening: a review of 21 cases. J Orthopaed Traumatol. (2011) ; 12: (4): 193-199. doi: 10.1007/s10195-011-0164-9. |
[23] | Zhang J, Wang G, Zhang N. A meta-analysis of complications associated with the use of cement-augmented pedicle screws in osteoporosis of spine. Orthopaedics & Traumatology: Surgery & Research. (2021) ; 107: (7): 102791. doi: 10.1016/j.otsr.2020.102791. |
[24] | Morimoto T, Kobayashi T, Hirata H, Tsukamoto M, Yoshihara T, Toda Y, et al. Cardiopulmonary Cement Embolism Following Cement-Augmented Pedicle Screw Fixation: A Narrative Review. Medicina (Kaunas). (2023) ; 59: (2): 407. doi: 10.3390/medicina59020407. |
[25] | Tani S, Ishikawa K, Kudo Y, Tsuchiya K, Matsuoka A, Maruyama H, et al. The effect of denosumab on pedicle screw fixation: a prospective 2-year longitudinal study using finite element analysis. Journal of Orthopaedic Surgery and Research. (2021) ; 16: (1): 219. doi: 10.1186/s13018-021-02360-2. |
[26] | Fukuta S, Miyamoto K, Hosoe H, Shimizu Katsuji. Kidneytype intervertebral spacers should be located anteriorly in cantilever transforaminal lumbar interbody fusion: analyses of risk factors for spacer subsidence for a minimum of 2 years. Journal of Spinal Disorders & Techniques. (2011) ; 24: (3): 189-195. doi: 10.1097/BSD.0b013e3181e9f249. |
[27] | Hou Y, Yuan W. Influences of disc degeneration and bone mineral density on the structural properties of lumbar end plates. The Spine Journal. (2012) ; 12: (3): 249-256. doi: 10.1016/j.spinee.2012.01.021. |
[28] | Jones C, Okano I, Salzmann SN, Reisener M-J, Chiapparelli E, Shue J, et al. Endplate volumetric bone mineral density is a predictor for cage subsidence following lateral lumbar interbody fusion: a risk factor analysis. The Spine Journal. (2021) ; 21: (10): 1729-1737. doi: 10.1016/j.spinee.2021.02.021. |
[29] | Oh KW, Lee JH, Lee J-H, Lee D-Y, Shim HJ. The correlation between cage subsidence, bone mineral density, and clinical results in posterior lumbar interbody fusion. Clinical Spine Surgery. (2017) ; 30: (6): E683-E689. doi: 10.1097/BSD.0000000000000315. |
[30] | Cho JH, Hwang CJ, Kim H, Joo Y-S, Lee D-H, Lee CS. Effect of osteoporosis on the clinical and radiological outcomes following one-level posterior lumbar interbody fusion. Journal of Orthopaedic Science. (2018) ; 23: (6): 870-877. doi: 10.1016/j.jos.2018.06.009. |
[31] | Stone MA, Jakoi AM, Iorio JA, Pham MH, Patel NN, Hsieh PC, et al. Bisphosphonate’s and Intermittent Parathyroid Hormone’s Effect on Human Spinal Fusion: A Systematic Review of the Literature. Asian Spine J. (2017) ; 11: (3): 484-493. doi: 10.4184/asj.2017.11.3.484. |
[32] | Oba H, Takahashi J, Yokomichi H, Hasegawa T, Ebata S, Mukaiyama K, et al. Weekly Teriparatide Versus Bisphosphonate for Bone Union During 6 Months After Multi-Level Lumbar Interbody Fusion for Osteoporotic Patients. Spine (Phila Pa 1976). (2020) ; 45: (13): 863-871. doi: 10.1097/BRS.0000000000003426. |
[33] | Kim SM, Rhee W, Ha S, Lim JH, Jang IT. Influence of alendronate and endplate degeneration to single level posterior lumbar spinal interbody fusion. Korean J Spine. (2014) ; 11: (4): 221-226. doi: 10.14245/kjs.2014.11.4.221. |
[34] | Belavic JM. Denosumab (Prolia): a new option in the treatment of osteoporosis. Nurse Pract. (2011) ; 36: (1): 11-12. doi: 10.1097/01.NPR.0000391178.47878.73. |
[35] | Prolia Product Monograph. Amgen Canada Inc, October (2011) . |
[36] | Lipton A, Goessl C. Clinical development of anti-RANKL therapies for treatment and prevention of bone metastasis. Bone. (2011) ; 48: (1): 96-99. doi: 10.1016/j.bone.2010.10.161. |
[37] | Bone HG, Bolognese MA, Yuen CK, Kendler DL, Miller PD, Yang Y-C, et al. Effects of denosumab treatment and discontinuation on bone mineral density and bone turnover markers in postmenopausal women with low bone mass. J Clin Endocrinol Metab. (2011) ; 96: (4): 972-980. doi: 10.1210/jc.2010-1502. |




