Efficacy of scapulothoracic exercises on proprioception and postural stability in cranio-cervico-mandibular malalignment: A randomized, double-blind, controlled trial
Abstract
BACKGROUND:
Cranio-cervico-mandibular (CCM) malalignment is associated with forward head posture (FHP) and temporomandibular joint (TMJ) disorders and affects masticatory muscles.
OBJECTIVE:
This randomized, double-blind controlled trial aimed to compare the efficacy of scapula-thoracic (ST) exercises on temporomandibular and cervical joint position sense and postural stability in individuals with CCM malalignment.
METHODS:
Fourty-nine participants with CCM malalignment were randomly assigned to the ST exercise group (STEG,
RESULTS:
The TMJ and cervical joint position sense, total sway degree, area gap percentage, sway velocity and antero-posterior body sway results showed significant improvement in the STEG compared to the CG (
CONCLUSIONS:
Postural stability, TMJ and cervical joint position sense appear to be affected in individuals with CCM malalignment. Our results showed that an exercise program including ST stabilization, proprioception and strengthening of the scapular muscles may be effective in the management of CCM malalignment and will allow clinicians to plan holistic treatment.
1.Introduction
Cervical spine malalignment can be seen in the sagittal and frontal planes. In particular, head anterior tilt or forward head posture (FHP) is the most common postural disorder characterized by hyperextension in the upper cervical region and flexion in the lower cervical region. Due to malalignment, compensation also occurs in other segments such as the temporomandibular joint (TMJ) and scapula-thoracic (ST) joint to maintain the balance of the spinal column. Thus, the TMJ and ST joints may also be affected [1, 2]. Cranio-cervico-mandibular (CCM) malalignment is associated with FHP and temporomandibular joint disorders (TMJD) and affects masticatory muscles [3].
TMJD and FHP are seen in 5–16% and 66–73% of the population respectively, and have become large-scale public health issues. Both conditions are most commonly seen between the ages of 18–45, and the incidence is higher in females. Although, studies have shown that the incidence of development of cranio-mandibular dysfunction is higher in patients with cranio-cervical problems [4, 5], to our knowledge there are no prevalence studies in which these 2 conditions were seen together.
According to biomechanical principles, there is a reciprocal relationship between the structure of body parts and active movement. In other words, the muscular performance required for various functions in our body is closely related to the ideal posture and musculoskeletal balance in which the body segments are in harmony with each other. Therefore, the effect of cranio-cervical posture on the functionality of the stomatognathic system can be attributed to the concept of the CCM system, which includes the musculoskeletal relationship of the head, neck, hyoid bone, mandible, and the ST region [6].
CCM malalignment changes the length-tension relationship of the muscles in the adjacent segments, and accordingly, the function of the scapular muscles, muscle activation patterns and normal scapular kinematics may be affected. However, muscle imbalance due to abnormal scapular biomechanics and deterred neuromuscular control can also cause CCM malalignment and postural problems such as FHP. It has been stated that shortening in neck extensors, weakness in the flexors and functional changes in the trapezius and serratus anterior muscles may cause such postural disorders [7, 8].
To ensure effective and coordinated TMJ movement, the muscles in the cranio-mandibular and cranio-cervical region must work in harmony. Alignment disorders in these regions or an imbalance of strength and tension between the muscles result in disturbed function of both the TMJ and cervical region. Moreover, the mechanics of the muscles in the cervical region also change as a result of the malposition of the mandible in people with CCM malalignment [9, 10].
The fact that there are a higher number of mechanoreceptors in the cervical region than in the thoracic and lumbar regions indicates that this region is more sensitive in terms of proprioception [11]. CCM malalignment affects neuromuscular control of the stomatognathic system, leading to abnormal afferent information, which consequently causes impaired muscle function in the cervical region and mandibular malposition [12]. Additionally, FHP disrupts the normal position of the hyoid and mandible bones by changing the natural kinematics of the TMJ and suprahyoid muscles [13].
Many physiotherapy methods are used to treat CCM malalignment. In 1997, Feine and Lund emphasized that dentists valued physiotherapy as an effective option in the treatment of TMJD [14]. A recent survey study revealed that 72% of respondents considered physiotherapy to be an effective treatment option for TMJD, with jaw exercise (79%), ultrasound (52%), manual therapy (48%), acupuncture (41%), and laser therapy (15%) as the most effective modalities for managing TMJD [3].
When the body is considered as a whole, it is clear that a problem in any part of the musculoskeletal system or kinetic chain will affect other parts. For example, some studies have reported that malalignment in the foot may affect the activation of the masticatory muscles [15, 16, 17, 18]. The ST region serves as a bridge between the cervical and lumbar regions as well as between the shoulder and the cervical region. The optimal position of the scapula and the stabilization of the ST muscles play a crucial role in fulfilling this task. In this context, the aim of our study was to investigate the effectiveness of ST exercises on postural stability and on cervical and TMJ proprioception in individuals with CCM malalignment.
2.Materials and methods
2.1Study design and subjects
This randomized double-blinded controlled study was performed in accordance with the Declaration of Helsinki. All participants were informed about the study, and written informed consent was obtained. The study was approved by the Eastern Mediterranean University Scientific Research and Publication Ethics Committee (Number: 2022-0232; Date: 25.10.2022). The clinical trial registration number is “NCT05966103”.
A total of 52 patients between the ages of 18–45 who met the inclusion criteria were selected among 176 screened individuals, who applied to the Cyprus International University physiotherapy department. Each participant was asked to choose a number from 1–52 using the lottery method. After matching each participant to their particular number, a random number generator (https://www.randomizer.org) is used to assign all numbers randomly into two groups. An experienced physiotherapist, who did not participate to the study performed all randomisation procedures and concealed the allocation.
Individuals with a sedentary lifestyle, cranio-vertebral angle (CVA)
2.2Sample size
The sample size was calculated with the G*Power program (version 3.1.9.2). When the power analysis was performed, the number of participants to be included in the study was calculated as 42 when the type I error (alpha value) was 0.05, the type II error (1-
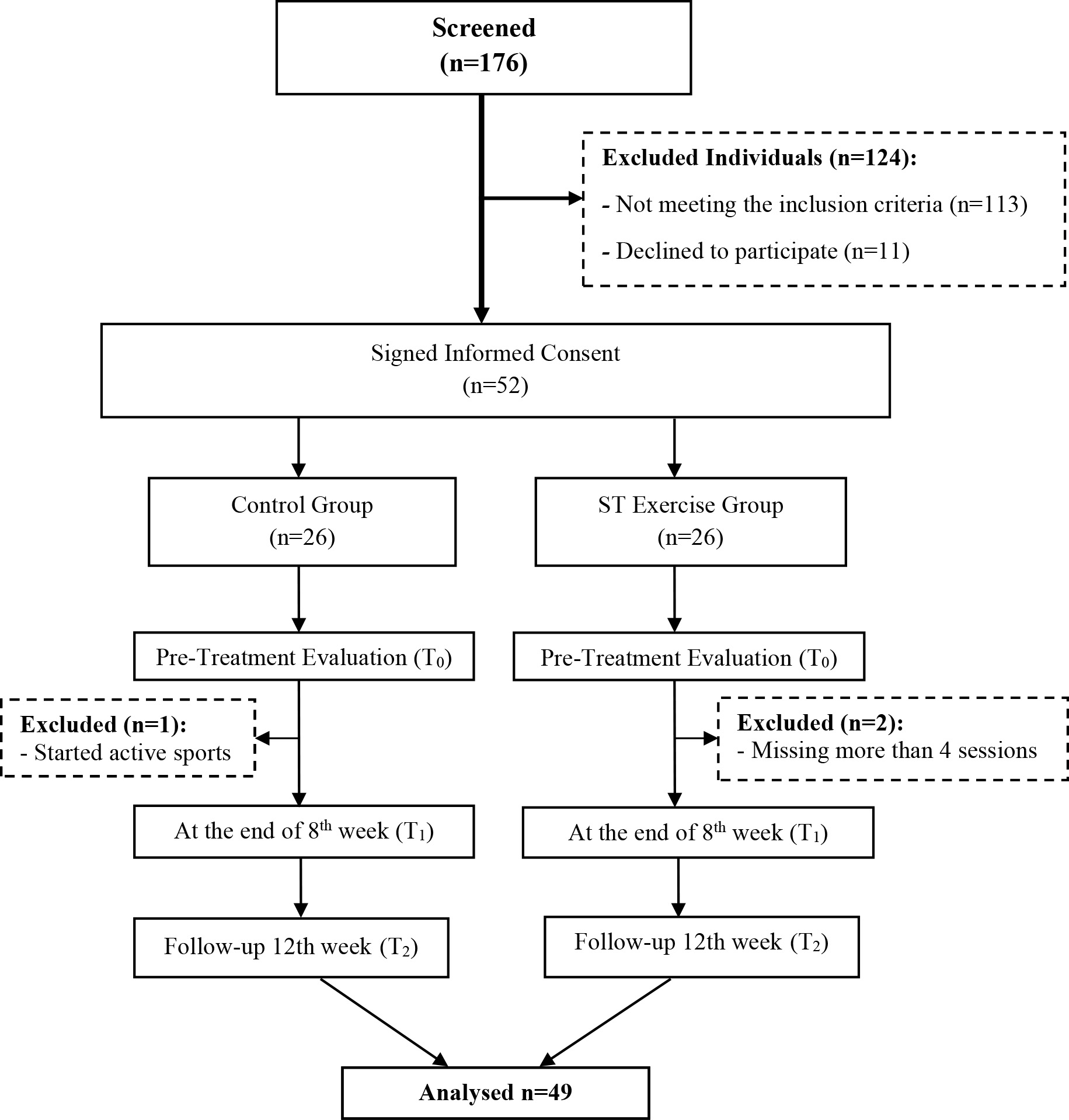
Figure 1.
Flow chart of the individuals included in the study.
2.3Data collection and outcome measures
The participants’ age, weight, height, body mass index (BMI), history, lifestyle habits, presence of chronic disease and parafunctional habits were recorded.
2.3.1Forward head posture (FHP)
CVA measurement was used in the evaluation of FHP. To determine the CVA, the lateral photographing method was used by placing markers on the ear tragus and the spinous process of the seventh cervical vertebra (C7). The digital camera recorded the CVA at a distance of 200 cm from the participant, with the height of the camera at the level of the acromion. The camera was fixed on a tripod. This technique shows high reliability (intraclass correlation coefficient 0.94). Individuals with a CVA less than 50
2.3.2Temporomandibular joint disorders (TMJDs)
The “Fonseca Questionnaire” and “Helkimo Clinical Dysfunction Index”, which were reported to be valid and reliable for the presence of TMJD, were used [20, 21]. The Fonseca questionnaire consists of 10 questions. The questionnaire included questions about joints, head and neck pain, pain during masticatory activity, parafunctional habits, decreased joint movement, impaired occlusion, and emotional stress. Participants were asked to answer each question as ‘yes’ (10 points), ‘no’ (0 points), and ‘sometimes’ (5 points). The results of the questionnaire were classified as no TMJD (0–15), mild TMJD (20–40), moderate TMJD (45–65), and severe TMJD (70–100) according to the answers given by the participants. The validity and reliability study of the Turkish version of the Fonseca questionnaire was performed by Kaynak et al., and the intraclass correlation coefficient (ICC) values were found to be 0.73–0.89 [22]. In an earlier study, the original version of the Fonseca Questionnaire also showed high accuracy at 86.30–91.90% when compared to the Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD), which is counted as the gold standard [21]. The Helkimo clinical dysfunction index was used to detect the presence of clinical findings such as limitation of jaw movements, dysfunction of the TMJ, pain with palpation of the masticatory muscles and the TMJ, and pain with lower jaw movements. According to the dysfunction index scoring, classification was made as the group with no clinical symptoms (0 points), mild symptoms of TMJD (1–4 points), moderate symptoms of TMJD (5–9 points) and severe symptoms of TMJD (10–25 points) [23, 24]. It has been stated that the Helkimo clinical dysfunction index has a sensitivity of 86.67% and a specificity of 68.09% for TMJD prediction [20].
2.3.3Temporomandibular joint position sense (TMJPS)
For the TMJPS measurement, a 6 mm thick reference wooden stick and 9 wooden test sticks from 4 mm to 8 mm thickness (increment 0.5 mm) were used. First, the participants were asked to sense the position by biting the 6 mm thick reference test stick with their front teeth for 1 minute. Then, they were asked to randomly bite each of the 9 test sticks and compare each of them with a 6 mm reference test stick. Each of the test sticks was administered in a random order 5 times (45 tests in total). The participants were asked how thick they felt compared to the reference stick that they bite off and indicated their answers as “thinner”, “thicker” or “equal” [25, 26]. During the test, the participant’s eyes were closed and the answers given about the stick thicknesses were recorded as true (1 point) or false (0 point) (Fig. 2).
Figure 2.
TMJPS measurement.

Figure 3.
CJPET measurement (a: Initial position for flexion and extension, b: Extension, c: Initial position for rotations, d: Left rotation).

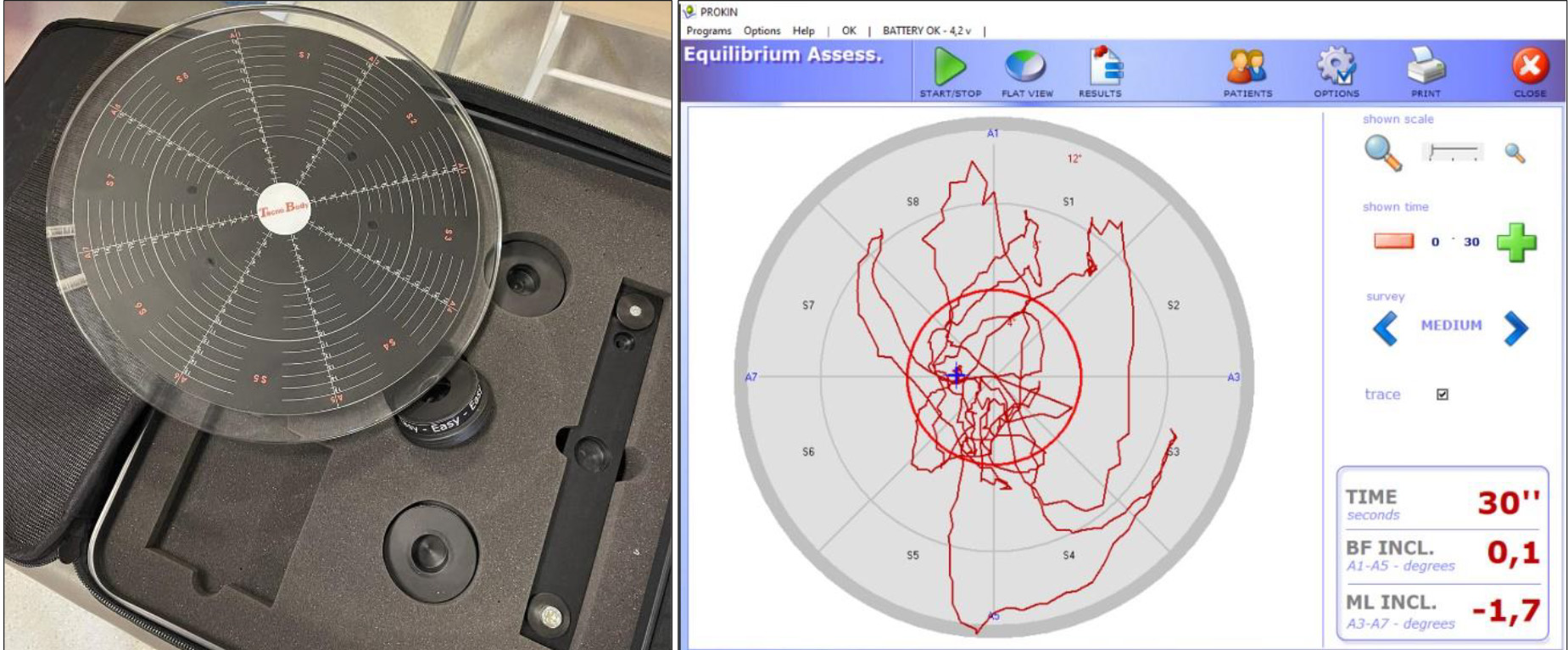
Figure 4.
Prokin device and postural stability measurement (red circle represents reference circle).
2.3.4Cervical joint position error test (CJPET)
Cervical joint position error test measurements were performed with an AOS PropPoint® device with a laser apparatus. The validity and reliability study of the AOS PropPoint® device was performed by Köseoğlu et al. (2022), and according to the results obtained, it was found that the device is a valid and reliable method for the measurement of cervical proprioception [27]. A hundred- and eighty-degree platform drawn with 1
2.3.5Postural stability
The PROKIN-PK200W* (Tecnobody, Italy) device was used for postural stability assessment. The Prokin device has a mobile circular platform, which detects angular movements thanks to the chip on the platform and transfers the information from the platform to the computer. Four different parts can be placed under the mobile platform: easy, medium, hard and rectangular. Changes in stability can be tracked on a computer [29]. For assessment, 2 measurements were made during 30 seconds of standing on both legs with the easy mode of the device, and the average values were recorded (Fig. 4). A total of five different data were obtained, including the total sway degree (the number of total degrees done during the test), area gap percentage (the percentage of the area included in the drawn-on flat view trace with respect to the reference circle), sway velocity value (the average number of covered degrees for second), medium equilibrium center antero-posterior (AP) (the average among the values reached on backward-forward axis) and medium equilibrium center medio-lateral (ML) (the average among the values reached on medial-lateral axis) [30, 31]. In the literature, the ICC values of the device have been shown to be between 0.89 and 0.98 [32, 33].
2.4Interventions
Cervical posture corrective exercises were applied to both the CG and the STEG 3 times a week for 8 weeks. In addition to cervical posture corrective exercises, ST exercises including strengthening, proprioceptive, and stabilization exercises, were added to the STEG. Exercise diary tracking was used to follow the exercise program. For the progression of the exercise programs, the progressive changes in theraband colour and the increase in the number of weights, sets and repetitions were added (Appendix 1). All treatment was carried out by the same physiotherapist. Assessments were made 3 times as pretreatment (T0), at the end of the 8th week treatment program (T1), and at the 12th week post-treatment follow-up (T2). A double-blind study was designed, all assessments were carried out by a physiotherapist who was blinded to the treatment, and participants did not know which group they were in.
Control Group: Chin tuck exercises in a sitting position, cervical range of motion exercises, cervical isometric exercises in flexion, extension and lateral flexion, stretching exercises combined with breathing to sternocleidomastoid (SCM), suboccipital, pectoral, upper trapezius and levator scapula muscles were applied (Appendix 1).
Table 1
Comparison of participants’ age, BMI, CVA and TMJD scores
| Group |
| Mean |
| |
|---|---|---|---|---|
| Average age (years) | Control | 25 | 22.36 | 0.406¥ |
| STEG | 24 | 22.83 | ||
| BMI (kg/m2) | Control | 25 | 23.25 | 0.492ϵ |
| STEG | 24 | 22.64 | ||
| CVA ( | Control | 25 | 45.75 | 0.649ϵ |
| STEG | 24 | 46.02 | ||
| Fonseca score | Control | 25 | 46.80 | 0.912ϵ |
| STEG | 24 | 47.29 | ||
| Helkimo score | Control | 25 | 5.62 | 0.894¥ |
| STEG | 24 | 5.80 |
¥: Mann-Whitney
Table 2
Within- and between-group comparison of participants’ CVA, TMJPS and CJPET measurement results
| Outcome | Group | T0 | T1 | T2 | Within group comparison | ||
|---|---|---|---|---|---|---|---|
| Mean | Mean | Mean |
|
|
| ||
| CVA ( | Control ( | 45.75 | 46.47 | 46.35 | 0.005* | 0.023* | 0.733 |
| STEG ( | 46.02 | 49.47 | 49.30 | 0.001* | 0.001* | 0.341 | |
| Between group comparison ( | 0.649 | 0.001* | 0.001* | ||||
| TMJPS (Number of correct answers) | Control ( | 32.76 | 33.64 | 33.32 | 0.160 | 0.609 | 0.440 |
| STEG ( | 32.92 | 37.63 | 37.21 | 0.001* | 0.001* | 0.198 | |
| Between group comparison ( | 0.880 | 0.001* | 0.001* | ||||
| CJPET flexion ( | Control ( | 4.92 | 4.48 | 4.56 | 0.114 | 0.225 | 0.824 |
| STEG ( | 5.58 | 3.64 | 3.70 | 0.001* | 0.001* | 0.851 | |
| Between group comparison ( | 0.166 | 0.006* | 0.013* | ||||
| CJPET extension ( | Control ( | 5.28 | 4.70 | 4.60 | 0.232 | 0.130 | 0.692 |
| STEG ( | 5.79 | 3.70 | 3.77 | 0.001* | 0.001* | 0.769 | |
| Between group comparison ( | 0.397 | 0.012* | 0.024* | ||||
| CJPET right rotation ( | Control ( | 7.34 | 6.94 | 7.12 | 0.525 | 0.632 | 0.657 |
| STEG ( | 7.23 | 6.17 | 6.27 | 0.002* | 0.026* | 0.791 | |
| Between group comparison ( | 0.826 | 0.013* | 0.007* | ||||
| CJPET left rotation ( | Control ( | 7.76 | 7.52 | 7.42 | 0.573 | 0.403 | 0.593 |
| STEG ( | 7.54 | 6.31 | 6.42 | 0.020* | 0.026* | 0.585 | |
| Between group comparison ( | 0.755 | 0.001* | 0.020* | ||||
Scapulothoracic Exercise Group (STEG): In addition to the exercises applied to the CG, exercises aiming to stabilize, strengthen and stimulate the proprioceptive input of the ST region were given to the STEG. Exercises in the STEG included punch, rowing, bilateral external rotation and scapular adduction exercises with theraband, ST neuromuscular control exercise, towel sliding on the wall, stabilization against the wall with the help of a small ball, push-up plus on bosu-ball, ST alignment on foam roller, retraction in Y position, T position, W position on an exercise ball, and protraction with dumbbells (Appendix 1).
2.5Statistical analysis
IBM Statistical Package for Social Sciences (SPSS) 26.0 software was used for statistical analysis for the data obtained from the individuals included in the study. The normal distribution of the variables was analysed with the Kolmogorov-Smirnov test. The Mann–Whitney
3.Results
A total of 176 individuals were screened for the study. Fifty-two individuals who met the inclusion criteria were included in the study. One participant in the CG (due to starting active sports) and 2 participants in the STEG (not participating in more than 4 sessions) were dropped from the study. The present study was completed with a total of 49 individuals, 25 in the control group and 24 in the STEG group. The study was carried out to determine the efficacy of ST exercises on TMJPS, CJPET and postural stability in sedentary individuals aged 18–45 with CCM malalignment.
There were no statistically significant baseline differences between groups in age, BMI, CVA or TMJD score values (
The repeated-measures ANOVA of the TMJPS and CJPET measurements of the participants in the CG and STEG, pretreatment (T
Figure 5.
Time-dependent changes in CVA, TMJPS and CJPET measurement results of the groups (a: CVA, b: TMJPS, c: CJPET for flexion, d: CJPET for extension, e: CJPET for right rotation, f: CJPET for left rotation).
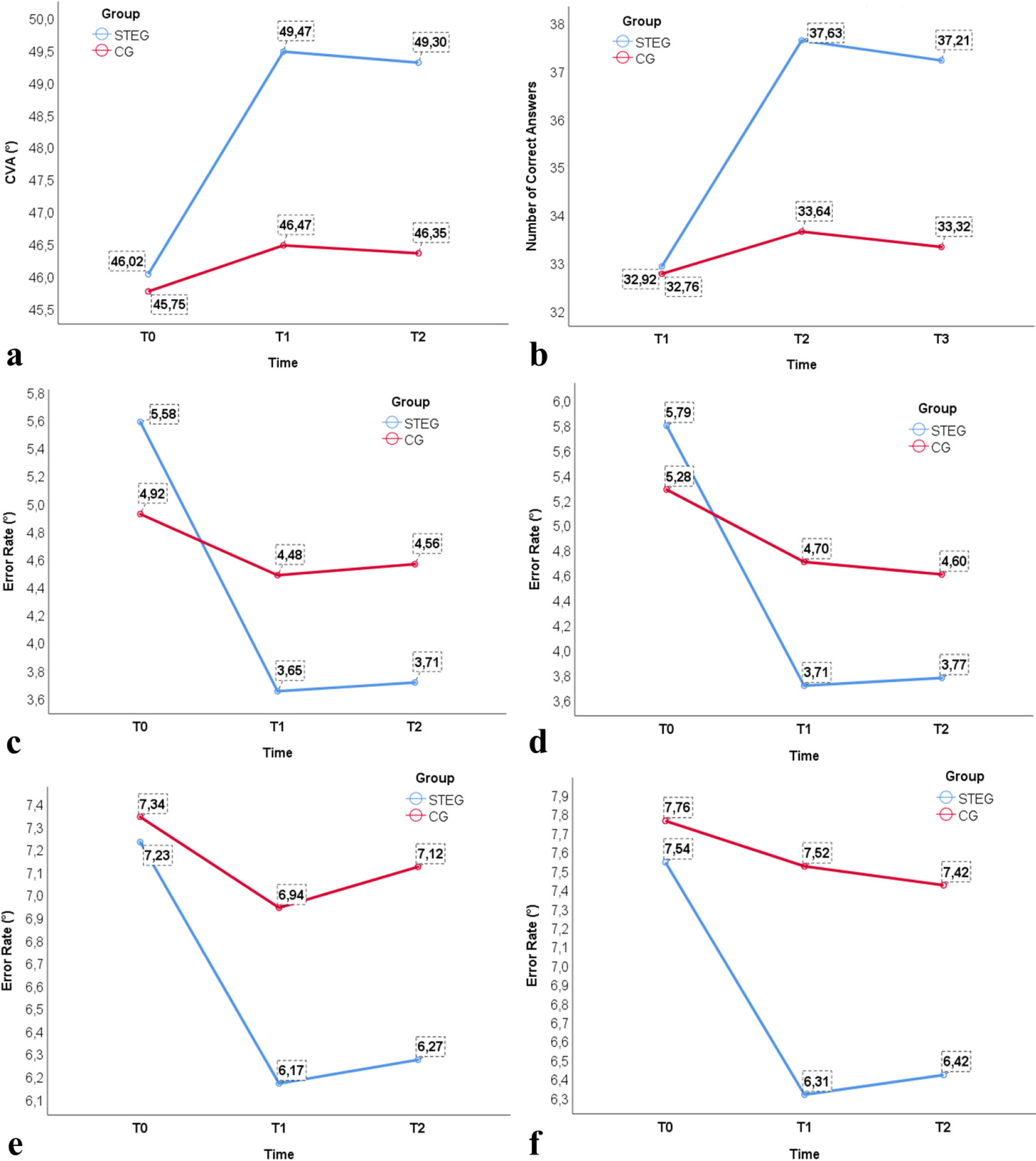
Figure 5 shows changes in three measurement results for the CVA, TMJPS, flexion, extension, right rotation and left rotation CJPET in both groups.
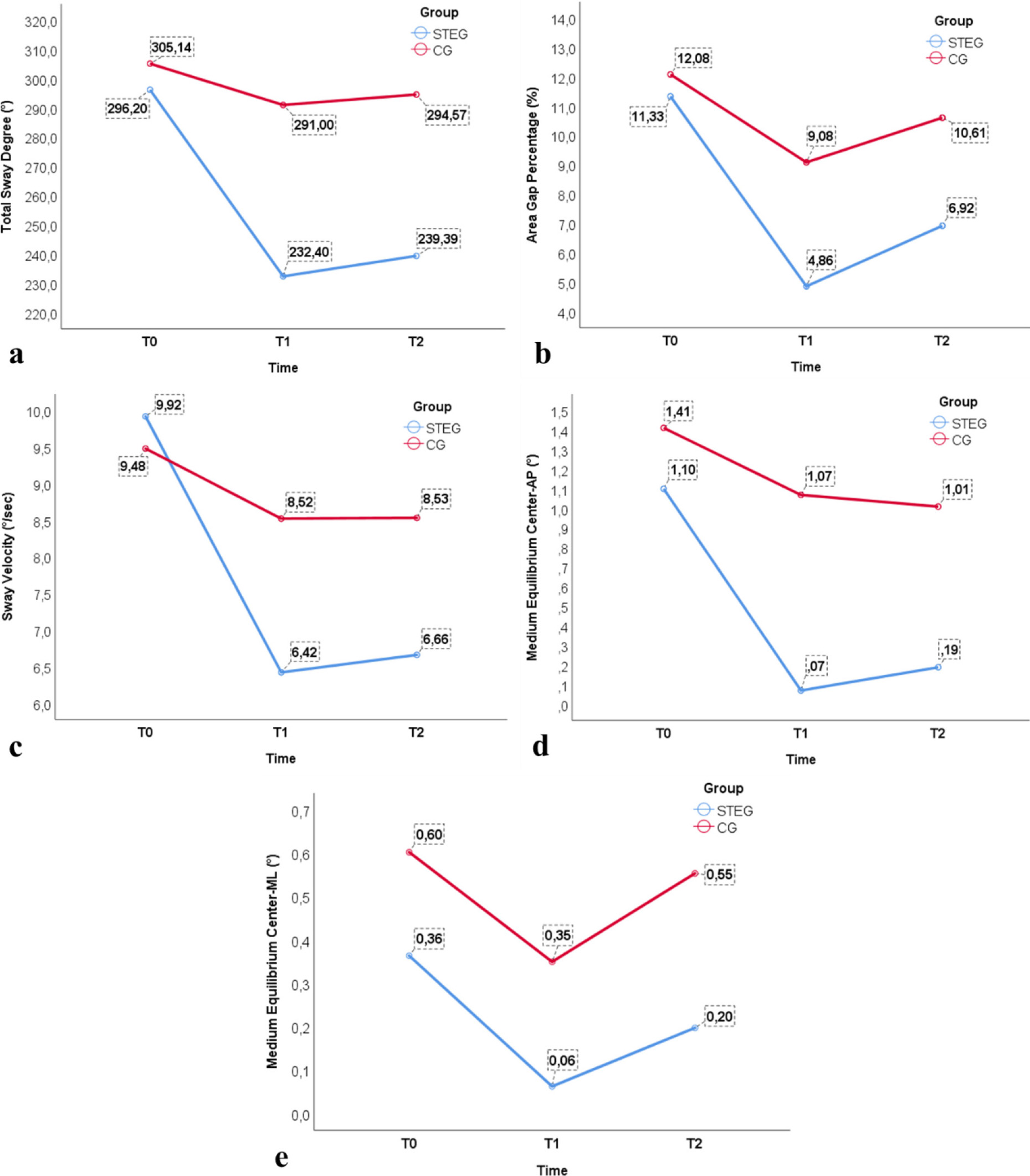
The repeated-measures ANOVA for the postural stability measurements in the CG and STEG, pretreatment (T
Table 3
Within- and between-group comparison of participants’ postural stability measurement results
| Outcome | Group | T0 Mean | T1 Mean | T2 Mean |
|
|
|
|---|---|---|---|---|---|---|---|
| Total sway degree ( | Control ( | 305.13 | 291.08 | 294.57 | 0.410 | 0.770 | 0.968 |
| STEG ( | 296.19 | 232.40 | 239.39 | 0.001* | 0.001* | 0.609 | |
| Between group comparison ( | 0.605 | 0.001* | 0.001* | ||||
| Area gap percentage (%) | Control ( | 12.07 | 9.08 | 10.60 | 0.086 | 0.575 | 0.510 |
| STEG ( | 11.33 | 4.85 | 6.91 | 0.001* | 0.001* | 0.212 | |
| Between group comparison ( | 0.765 | 0.038* | 0.042* | ||||
| Sway velocity ( | Control ( | 9.47 | 8.52 | 8.56 | 0.079 | 0.132 | 0.954 |
| STEG ( | 9.91 | 6.42 | 6.60 | 0.001* | 0.001* | 0.875 | |
| Between group comparison ( | 0.473 | 0.001* | 0.001* | ||||
| Medium equilibrium center-AP ( | Control ( | 1.41 | 1.07 | 1.01 | 0.381 | 0.346 | 0.904 |
| STEG ( | 1.09 | 0.07 | 0.19 | 0.009* | 0.004* | 0.761 | |
| Between group comparison ( | 0.565 | 0.013* | 0.042* | ||||
| Medium equilibrium center-ML ( | Control ( | 0.60 | 0.35 | 0.55 | 0.588 | 0.882 | 0.441 |
| STEG ( | 0.36 | 0.06 | 0.20 | 0.494 | 0.620 | 0.616 | |
| Between group comparison ( | 0.644 | 0.433 | 0.340 | ||||
The changes in the total sway degree, area gap percentage, sway velocity, medium equilibrium center-AP and medium equilibrium center-ML measurement results of the groups at 3 different times are shown in Fig. 6.
Figure 6.
Time-dependent changes in the postural stability measurement results of the groups (a: total sway degree, b: area gap percentage, c: sway velocity, d: AP sway, e: ML sway).
4.Discussion
The purpose of the study was to assess whether ST exercises, including progressive strengthening, proprioceptive and stabilization exercises (STEG), were more effective than conventional PT on TMJPS, CJPET and postural stability in individuals with CCM malalignment.
The results of the study showed that applying ST exercises increased TMJPS and decreased the error rate in CJPET in the STEG compared to the CG. Additionally, postural stability results showed that total sway degree, area gap percentage, sway velocity and medium equilibrium center-AP results decreased in favour of the STEG.
The CCM system is closely linked with the head, neck, hyoid bone, TMJ, ST region and shoulder girdle. Therefore, head and neck biomechanics are of great interest both in the field of dentistry and physiotherapy [34]. Many physiotherapy methods, such as joint mobilization and strengthening exercises, are used in CCM malalignment in addition to the cervical collar and manual therapy approaches for the cervical region. On the other hand, various methods, such as cervical stabilization exercises, mobilization and manipulation techniques for the cervical and thoracic region, postural corrective exercises, kinesio taping, instrument-assisted soft tissue mobilization techniques and clinical Pilates, are frequently used interventions for FHP. One systematic review and meta-analysis revealed that manual therapy and therapeutic exercises such as strengthening, stretching, stabilization, proprioceptive and motor control exercises have favourable effects in patients with TMJD [3]. Another meta-analysis study showed evidence that physiotherapy interventions are more effective than other treatment modalities (acupuncture, passive range of motion, etc.) and sham therapy in the management of TMJD [35]. Considering that the ST region serves as a bridge between the shoulder and the cervical region, it is clear that dysfunction in any part of this chain will affect adjacent parts. Indeed, a systematic review conducted by Chaves et al. found that individuals with TMJD could have scapular and cervical malalignment [15]. It has also been stated that even if positive improvements are achieved in symptoms with TMJ-oriented treatments or cervical region-focused treatments in such postural disorders, full recovery cannot be achieved in long-term follow-ups [36, 37, 38, 39]. The treatment of patients with TMJD needs extensive management, taking into account not only the treatment of the jaw but also the treatment that involves the entire CCM system and the spinal complex [40]. In the current study, therefore, we added scapular stabilization and proprioceptive and strengthening exercises for muscles of the ST region to the treatment program for patients with CCM malalignment.
A previous study carried out by Armijo and Magee found that subjects with TMJD presented increased resting EMG activity in the SCM and upper trapezius muscles. Hence, increased activity in the superficial muscles could be seen as a strategy to compensate for the weakness of the deep flexor muscles [41]. Therefore, we included strengthening of the ST muscles in our treatment program.
Data in the current study showed that proprioceptive sense in the TMJ and cervical region deteriorated with the increase in FHP defined by CVA. Our results are in concurrence with a study carried out by Goldstein and Makofsky in 2005. According to their study, “the natural kinematics of the TMJ and suprahyoid muscles is affected by FHP and results with loosening normal position of the hyoid and mandible bones which causes a change in the length-tension relationship of the muscles in the adjacent segments” [42]. Consequently, FHP disrupts the function of the scapular muscles, muscle activation patterns and normal scapular kinematics. While FHP leads to abnormal scapular muscle activity, the association may be bidirectional, as abnormal scapular muscle activity could also lead to FHP. The accessory nerve carries proprioceptive afferents from the neck and shoulder muscles through the atlanto-occipital joint [43], and therefore, changes in scapular biomechanics and neuromuscular control may cause FHP [8].
In the current study, there was a significant improvement in TMJPS and CJPET in the STEG after the specific exercise program, including proprioceptive, stabilization and strengthening exercises, over the conventional exercise program that was given to the CG. A previous study suggested that cervical and scapular stabilization exercises increase proprioception around the head and neck [44] and therefore correct FHP [45]. Furthermore, resistance training was found to be associated with increasing the sensitivity of Golgi tendon organs and muscle spindles and stimulation of mechanoreceptors around the cervical region [46]. In our opinion, the presence of resistance strengthening exercises in the content of the exercise program applied to the STEG may also explain the improvement in TMJPS and CJPET. Additionally, the review conducted by Winter et al. (2022) depicted that proprioceptive training results in improvements in somatosensory and sensorimotor functions. These exercises were found to be associated with adaptations in cortico-spinal systems, such as remapping in the motor cortex [47]. In the STEG, we also studied the effect of intensive proprioceptive inputs using materials such as foam rollers, Pilates balls, bosu balls and barbed balls. Therefore, based on the abovementioned evidence, we can suggest that ST proprioceptive exercises improved both TMJ and cervical proprioception in the STEG.
In our study, there were significant improvements in TMJ and cervical proprioception. The fact that there was no statistically significant difference between the results at the end of 8 weeks and the follow-up after 12 weeks indicates that the effects of the exercises lasted in the post-treatment period. In the literature, it was found that some of the studies conducted with the application of such exercises for an average of 3–6 weeks did not have positive results. Since there is no clear timeframe for exercise in the literature [37], we suggest that up to 8 weeks for such exercises may be effective in improving proprioceptive sensation and postural stability in patients with TMJD and FHP.
Many studies investigating the relationship between TMJD and FHP and postural stability have revealed different results [48, 49, 50, 51, 52]. CCM malalignment affects neuromuscular control of the stomatognathic system, leading to the formation of abnormal afferent information [12]. FHP can cause pain in the jaw, neck, back, shoulders and arms due to changes in the body’s center of mass (CoM) and balance between muscles [45]. When the head moves forward, the CoM shifts anteriorly with respect to the base of support (BoS). This malalignment can affect postural stability, and it may become difficult for individuals to maintain an upright posture without swaying or losing balance [51, 53]. Asymmetrical alignment of the head and neck also causes errors in the information received as visual and vestibular perception [54]. This ultimately reduces balance and increases the risk of falls and musculoskeletal injuries while performing activities [50]. TMJD is considered another leading cause of increased postural sway. It has been found that there were greater changes in the body CoM and poor postural stability in patients with TMJ dysfunction due to changes in the whole-body muscle chain [49, 55]. Providing a symmetrical function of TMJs corrects the dysfunctions in adjacent regions and relocates the position of the CoM [34, 40]. This assumption was also made based on a study by Sforza et al. (2006), in which a symmetrical mandibular position led to a more symmetrical contraction pattern in the SCM muscle and reduced postural sway [56] through intense proprioceptive information in the cervical and thoracic regions. Hence, proprioceptive sensing of the cervical and thoracic vertebrae transmits information and plays an important role in postural control. The proprioceptive sense works in tandem with the vestibular system and reacts sensitively to the fine movement of the head to act in coordination [57]. Studies suggest that individuals with FHP may have impaired proprioception in the neck and upper back regions. Reduced proprioceptive input can disrupt the body’s ability to make rapid and precise postural adjustments and results in poor postural stability [58, 59]. A decrease in the CJPET in the current study suggests that ST exercises could increase proprioceptive inputs and segmental realignment, thus improving postural stability and postural sway in the AP direction, as revealed by Bae and Park (2020) [60]. The current study has a few limitations. First, the duration of the symptoms was not recorded, and it could be considered a limitation. Second, an age- and gender-matched healthy group might be added to the study.
5.Conclusion
This study has a strong clinical emphasis. Postural stability, TMJ and cervical joint position sense appear to be affected in individuals with CCM malalignment. Designing exercise programs with the inclusion of ST stabilization, proprioception and strengthening of the scapular muscles may be effective in the management of CCM malalignment. The results of the study also showed that the treatment of the ST region should be considered in the extensive management of CCM malalignment.
Authors’ contributions
MM, IY and SA participated in the conception and design of the study. MM was responsible for data acquisition. MM, IY and SA analyzed and interpreted the data. MM drafted the manuscript and IY, MM and SA critically revised the manuscript for important intellectual content. All authors approved the final version of the manuscript.
Data availability statement
Data are available upon reasonable request.
Ethics approval and consent to participate
The study was approved by the Eastern Mediterranean University Scientific Research and Publication Ethics Committee (Number: 2022-0232; Date: 25.10.2022) and written informed consent was obtained from all participants before they received the interventions.
Funding
The authors report no funding.
Informed consent
Written informed consent was obtained for publication of the figures included in the manuscript.
Supplementary data
The supplementary files are available to download from http://dx.doi.org/10.3233/BMR-230323.
Acknowledgments
The authors would like to thank the participants who took part in the study and the reviewers and journal editor for meticulously critiquing this article. Special thanks to Professor Fatma Uygur for her contributions to language and scientific review.
Conflict of interest
The authors declare that they have no conflict of interest.
References
[1] | Hertling D, Kessler RM. Management of common musculoskeletal disorders: Physical therapy principles and methods. Lippincott Williams & Wilkins. (2006) . |
[2] | Sajjadi E, Olyaei GR, Talebian S, Hadian M-R, Jalaie S. The effect of forward head posture on cervical joint position sense. Archives of Advances in Biosciences. (2014) ; 5: . |
[3] | Armijo-Olivo S, Pitance L, Singh V, Neto F, Thie N, Michelotti A. Effectiveness of manual therapy and therapeutic exercise for temporomandibular disorders: Systematic review and meta-analysis. Phys Ther. (2016) ; 96: : 9-25. |
[4] | Ryan J, Akhter R, Hassan N, Hilton G, Wickham J, Ibaragi S. Epidemiology of temporomandibular disorder in the general population: a systematic review. Adv Dent Oral Health. (2019) ; 10: : 1-13. |
[5] | Vakili L, Halabchi F, Mansournia MA, Khami MR, Irandoost S, Alizadeh Z. Prevalence of common postural disorders among academic dental staff. Asian Journal of Sports Medicine. (2016) ; 7: . |
[6] | Weber P, Corrêa ECR, de Paula Bolzan G, dos Santos Ferreira F, Soares JC, da Silva AMT. Relationship between craniocervical posture, mandible and hyoid bone and influence on alimentary functions. Brazilian Journal of Oral Sciences. (2012) ; 11: : 141-7. |
[7] | Cagnie B, Struyf F, Cools A, Castelein B, Danneels L, O’leary S. The relevance of scapular dysfunction in neck pain: A brief commentary. Journal of Orthopaedic & Sports Physical Therapy. (2014) ; 44: : 435-9. |
[8] | Singla D, Veqar Z. Association between forward head, rounded shoulders, and increased thoracic kyphosis: A review of the literature. Journal of Chiropractic Medicine. (2017) ; 16: : 220-9. |
[9] | Quek J, Pua Y-H, Clark RA, Bryant AL. Effects of thoracic kyphosis and forward head posture on cervical range of motion in older adults. Manual Therapy. (2013) ; 18: : 65-71. |
[10] | Ries LGK, Bérzin F. Analysis of the postural stability in individuals with or without signs and symptoms of temporomandibular disorder. Brazilian oral research. (2008) ; 22: : 378-83. |
[11] | McLain RF, Raiszadeh K. Mechanoreceptor endings of the cervical, thoracic, and lumbar spine. The Iowa Orthopaedic Journal. (1995) ; 15: : 147. |
[12] | Moustafa IM, Youssef A, Ahbouch A, Tamim M, Harrison DE. Is forward head posture relevant to autonomic nervous system function and cervical sensorimotor control? Cross Sectional Study. Gait & Posture. (2020) ; 77: : 29-35. |
[13] | Sutter BA, Girouard P. Posture stability and forward head posture before and after disclusion time reduction (DTR). A Five-Year Cohort Study. Advanced Dental Technologies & Techniques. (2021) . |
[14] | Feine JS, Lund JP. An assessment of the efficacy of physical therapy and physical modalities for the control of chronic musculoskeletal pain. Pain. (1997) ; 71: : 5-23. |
[15] | Chaves TC, Turci AM, Pinheiro CF, Sousa LM, Grossi DB. Static body postural misalignment in individuals with temporomandibular disorders: a systematic review. Brazilian Journal of Physical Therapy. (2014) ; 18: : 481-501. |
[16] | Saito ET, Akashi PMH, Sacco IdCN. Global body posture evaluation in patients with temporomandibular joint disorder. Clinics. (2009) ; 64: : 35-9. |
[17] | Zonnenberg A, Van Maanen C, Oostendorp R, Elvers J. Body posture photographs as a diagnostic aid for musculoskeletal disorders related to temporomandibular disorders (TMD). CRANIO®. (1996) ; 14: : 225-32. |
[18] | Messina G, Amato A, Rizzo F, Dominguez LJ, Iovane A, Barbagallo M, et al. The Association between Masticatory Muscles Activation and foot pressure distribution in older female adults: A cross-sectional study. International Journal of Environmental Research and Public Health. (2023) ; 20: : 5137. |
[19] | Suvarnnato T, Puntumetakul R, Uthaikhup S, Boucaut R. Effect of specific deep cervical muscle exercises on functional disability, pain intensity, craniovertebral angle, and neck-muscle strength in chronic mechanical neck pain: A randomized controlled trial. Journal of Pain Research. (2019) ; 915-25. |
[20] | Alonso-Royo R, Sánchez-Torrelo CM, Ibáñez-Vera AJ, Zagalaz-Anula N, Castellote-Caballero Y, Obrero-Gaitán E, et al. Validity and reliability of the Helkimo clinical dysfunction index for the diagnosis of temporomandibular disorders. Diagnostics. (2021) ; 11: : 472. |
[21] | dos Santos Berni KC, Dibai-Filho AV, Rodrigues-Bigaton D. Accuracy of the Fonseca anamnestic index in the identification of myogenous temporomandibular disorder in female community cases. Journal of Bodywork and Movement Therapies. (2015) ; 19: : 404-9. |
[22] | Kaynak BA, TaşS Salkın Y. The accuracy and reliability of the Turkish version of the Fonseca anamnestic index in temporomandibular disorders. Cranio®. (2023) ; 41: : 78-83. |
[23] | Kurt H. Standardized schemes used for clinical evaluation of temporomandibular disorders. Turkish Journal of Physical Medicine and Rehabilitation. (2010) ; 56: : 46-8. |
[24] | Nokar S, Sadighpour L, Shirzad H, Shahrokhi Rad A, Keshvad A. Evaluation of signs, symptoms, and occlusal factors among patients with temporomandibular disorders according to Helkimo index. CRANIO®. (2019) ; 37: : 383-8. |
[25] | Bucci R, Lobbezoo F, Michelotti A, Orfanou C, Koutris M. Delayed-onset muscle soreness does not influence occlusal sensitivity and position sense of the mandible. Journal of Oral Rehabilitation. (2017) ; 44: : 655-63. |
[26] | Morimoto T, Takebe H, Hamada T, Kawamura Y. Oral kinesthesia in patients with Duchenne muscular dystrophy. Journal of the Neurological Sciences. (1981) ; 49: : 285-91. |
[27] | Köseoğlu A, Coşkunsu DK, Mutlu EK. Validity and reliability of a new method to measure cervical proprioception. Physikalische Medizin, Rehabilitationsmedizin, Kurortmedizin. (2022) ; 32: : 306-13. |
[28] | Abdelkader NA, Mahmoud AY, Fayaz NA, Mahmoud LSE-D. Decreased neck proprioception and postural stability after induced cervical flexor muscles fatigue. Journal of Musculoskeletal & Neuronal Interactions. (2020) ; 20: : 421. |
[29] | Eriş F, Uzun R, Hazir A, Güvenç C. Comparison of some anthropometric features and balance ability of basketball and volleyball athletes. European Journal of Molecular & Clinical Medicine. (2023) ; 10: : 2023. |
[30] | Gonener U, Gonener A. How balance training on different types of surfaces effect dynamic balance ability and postural sway of gymnast children? Progress in Nutrition. (2020) ; 22: : 131-7. |
[31] | Prokin. Tecnobody Rehabilitation Systems Operator’s Manual. PK-MANOPWL-01 EN ed. Levate Italy2008.55. |
[32] | Zawadzki J, Bober T, Siemienski A. Validity analysis of the Biodex System 3 dynamometer under static and isokinetic conditions. Acta Bioeng Biomech. (2010) ; 12: : 25-32. |
[33] | Zhao W, You H, Jiang S, Zhang H, Yang Y, Zhang M. Effect of Pro-kin visual feedback balance training system on gait stability in patients with cerebral small vessel disease. Medicine. (2019) ; 98. |
[34] | Di Giacomo P, Ferrara V, Accivile E, Ferrato G, Polimeni A, Di Paolo C. Relationship between cervical spine and skeletal class II in subjects with and without temporomandibular disorders. Pain Research and Management. (2018) . |
[35] | Paco M, Peleteiro B, Duarte J, Pinho T. The effectiveness of physiotherapy in the management of temporomandibular disorders: A systematic review and meta-analysis. J Oral Facial Pain Headache. (2016) ; 30: : 210-20. |
[36] | Cho J, Lee E, Lee S. Upper thoracic spine mobilization and mobility exercise versus upper cervical spine mobilization and stabilization exercise in individuals with forward head posture: a randomized clinical trial. BMC Musculoskeletal Disorders. (2017) ; 18: : 1-10. |
[37] | Dickerson SM, Weaver JM, Boyson AN, Thacker JA, Junak AA, Ritzline PD, et al. The effectiveness of exercise therapy for temporomandibular dysfunction: a systematic review and meta-analysis. Clinical Rehabilitation. (2017) ; 31: : 1039-48. |
[38] | Mylonas K, Angelopoulos P, Billis E, Tsepis E, Fousekis K. Combining targeted instrument-assisted soft tissue mobilization applications and neuromuscular exercises can correct forward head posture and improve the functionality of patients with mechanical neck pain: A randomized control study. BMC Musculoskeletal Disorders. (2021) ; 22: : 1-9. |
[39] | Shih H-S, Chen S-S, Cheng S-C, Chang H-W, Wu P-R, Yang J-S, et al. Effects of Kinesio taping and exercise on forward head posture. Journal of Back and Musculoskeletal Rehabilitation. (2017) ; 30: : 725-33. |
[40] | Craciun MD, Geman O, Leuciuc FV, Holubiac IS, Gheorghita D, Filip F. Effectiveness of physiotherapy in the treatment of temporomandibular joint dysfunction and the relationship with cervical spine. Biomedicines. (2022) ; 10: . |
[41] | Armijo-Olivo S, Magee D. Cervical musculoskeletal impairments and temporomandibular disorders. J Oral Maxillofac Res. (2013) ; 3: : e4. |
[42] | Goldstein L, Makofsky HW. TMD/facial pain and forward head posture. Practical Pain Management. (2005) . |
[43] | de Campos D, Rieger A, Mohr H, Ellwanger JH, de Borba Junior AM. Anatomy and evolution of accessory nerve: Cranial or spinal origins? – A review. Journal of Morphological Sciences. (2017) ; 28: . |
[44] | Lee S-H, Yoo B-H, Pyo H-S, Lee D, Hong J-H, Yu J-H, et al. Effects of cervical stabilization and scapular stabilization exercise on the proprioception and craniovertebral angle and upper trapezius muscle tone of people with forward head posture. Korean Society of Physical Medicine. (2022) ; 17: : 1-13. |
[45] | Kang N-Y, Im S-C, Kim K. Effects of a combination of scapular stabilization and thoracic extension exercises for office workers with forward head posture on the craniovertebral angle, respiration, pain, and disability: A randomized-controlled trial. Turkish Journal of Physical Medicine and Rehabilitation. (2021) ; 67: : 291. |
[46] | Fatima A, Veqar Z, Zaidi S, Tanwar T. Effects of scapular stabilization and upper limb proprioception as an adjunct to cervical stabilization in chronic neck pain patients: A randomized controlled trial. Journal of Bodywork and Movement Therapies. (2022) ; 29: : 291-301. |
[47] | Winter L, Huang Q, Sertic JV, Konczak J. The effectiveness of proprioceptive training for improving motor performance and motor dysfunction: A Systematic Review. Frontiers in Rehabilitation Sciences. (2022) ; 3: : 830166. |
[48] | Cuccia A, Caradonna C. The relationship between the stomatognathic system and body posture. Clinics. (2009) ; 64: : 61-6. |
[49] | Kim JY, Yeo SS. Change of balance ability in subjects with pain-related temporomandibular disorders. The Journal of Korean Physical Therapy. (2022) ; 34: : 321-5. |
[50] | Lee JH. Effects of forward head posture on static and dynamic balance control. J Phys Ther Sci. (2016) ; 28: : 274-7. |
[51] | Lin G, Zhao X, Wang W, Wilkinson T. The relationship between forward head posture, postural control and gait: A systematic review. Gait & Posture. (2022) . |
[52] | Nota A, Tecco S, Ehsani S, Padulo J, Baldini A. Postural stability in subjects with temporomandibular disorders and healthy controls: A comparative assessment. J Electromyogr Kinesiol. (2017) ; 37: : 21-4. |
[53] | Ahmadipoor A, Khademi-Kalantari K, Rezasoltani A, Naimi SS, Akbarzadeh-Baghban A. Effect of forward head posture on dynamic balance based on the biodex balance system. J Biomed Phys Eng. (2022) ; 12: : 543-8. |
[54] | Treleaven J. Sensorimotor disturbances in neck disorders affecting postural stability, head and eye movement control – Part 2: case studies. Man Ther. (2008) ; 13: : 266-75. |
[55] | Nation P. A literature review of the influence of the stomatognathic system on body posture. (2015) . |
[56] | Sforza C, Tartaglia GM, Solimene U, Morgun V, Kaspranskiy RR, Ferrario VF. Occlusion, sternocleidomastoid muscle activity, and body sway: A pilot study in male astronauts. CRANIO®. (2006) ; 24: : 43-9. |
[57] | Johnson MB, Van Emmerik RE. Effect of head orientation on postural control during upright stance and forward lean. Motor Control. (2012) ; 16: : 81-93. |
[58] | Proske U, Gandevia SC. The proprioceptive senses: Their roles in signaling body shape, body position and movement, and muscle force. Physiological Reviews. (2012) . |
[59] | Smith DL, Haug MJ, Walsh MS. The effect of posture on neck proprioception and head/neck stabilization in asymptomatic participants. J Can Chiropr Assoc. (2019) ; 63: : 100-10. |
[60] | Bae Y, Park Y. Head posture and postural balance in community-dwelling older adults who use dentures. Medicina (Kaunas). (2020) ; 56. |




