Determinants of outcomes for patients with chronic low back pain and fear-avoidance beliefs following treatment with specific stabilisation exercises
Abstract
BACKGROUND:
Specific stabilisation exercises (SSE) can combat the debilitating effects of chronic non-specific low back pain (CLBP), improve disability, pain and fear-avoidance beliefs (FAB).
OBJECTIVE:
To elicit the determinants of outcome in patients with CLBP with associated FABs after treatment with SSE.
METHOD:
Twenty-nine patients (20 females) with CLBP were classified using FAB questionnaire into high or low Work and Physical Activity (PA) subscales. After 4-week treatment, evaluations were done for pain, disability and lumbar spine active range of motion (AROM). Data was analysed exploratory-descriptively with a significance level set at
RESULTS:
Participants were aged 55.24
CONCLUSION:
SSE can potentially improve disability, pain and range of motion for patients with chronic low back pain regardless of FABQ status. Gender and baseline patient status are potential determinants of outcome of treatment using SSE.
1.Introduction
Non-specific chronic low back pain (NSCLBP) is a major health and socioeconomic problem in modern society and has attracted a significant amount of research [1, 2]. It is multi-factorial and with high age-related global prevalence and a potential for a substantial increase in the coming decades [3, 4, 5]. Reduced muscle strength and endurance have been identified in people with (NSCLBP), which may compromise functional capacity and flexibility [6]. Improving this capacity can be effective in the treatment and prevention of the recurrence of NSCLBP [7].
Non-specific chronic low back pain (NSCLBP) is closely associated with physical and complex prognostic factors which include distress and fear-avoidance beliefs (FAB) [8]. Supervised exercise therapies are among the most effective and advocated treatments to optimise patient outcomes [7, 9]. Specific stabilisation exercises (SSE) aims to re-establish the impairment or deficit around the spinal motion segment by restoring the normal function of local stabilizer muscles [7]. A recent study shows that although exercise training may be more effective, stabilisation exercises ‘are possibly the most effective treatments depending on the outcome of interest for adults with NSCLBP’ [10]. This is corroborated by previous studies which document improvement in pain relief, stability, disability and active range of lumbar spine motion following treatment with SSE [11, 12]. However, FABs on the other hand have also been shown in studies to play a role in the chronicity and consequent disability associated with NSCLBP and in some cases considered a key predictor of outcome [8, 9, 10, 11, 12, 13]. There is evidence that FABs in NSCLBP can be managed using specific graded exercises/activities [14]. SSE thus has the potential to reduce pain and disability by improving spinal stability and gradually exposing patients to activity thereby reducing FABs and preventing recurrence [7, 15, 16]. While complete recovery might now be feasible within a short period, there is evidence that these improvements in muscle strength, disability and pain could be seen early in treatment. In a study by Filiz et al., changes in spinal mobility and muscle properties were already been observed in a 2-week intervention [17]. One study had patients intervention for 6 weeks and presented significant improvement in muscle strength [18]. Several studies reported improvements in clinical outcome of pain, range of motion (ROM) and disability after intervention on chronic non-specific low back pain [19, 20]. Additionally, up-to-date evidence is seen in systematic reviews by Hayden et al. and Owen et al., showing that specific stabilisation exercises might be effective for pain and is more effective for disability ‘in the short and medium term’ [10, 21]. It is however, unclear which factors determine SSE treatment outcome within a limited time frame and its relationship with FABs related to work and physical activity. This study aimed to elicit the determinants of outcome in patients with NSCLBP with associated FABs after treatment with specific stabilisation exercises and establish the relationship between FAB and the outcome of 4 weeks of treatment using SSE in patients with NSCLBP.
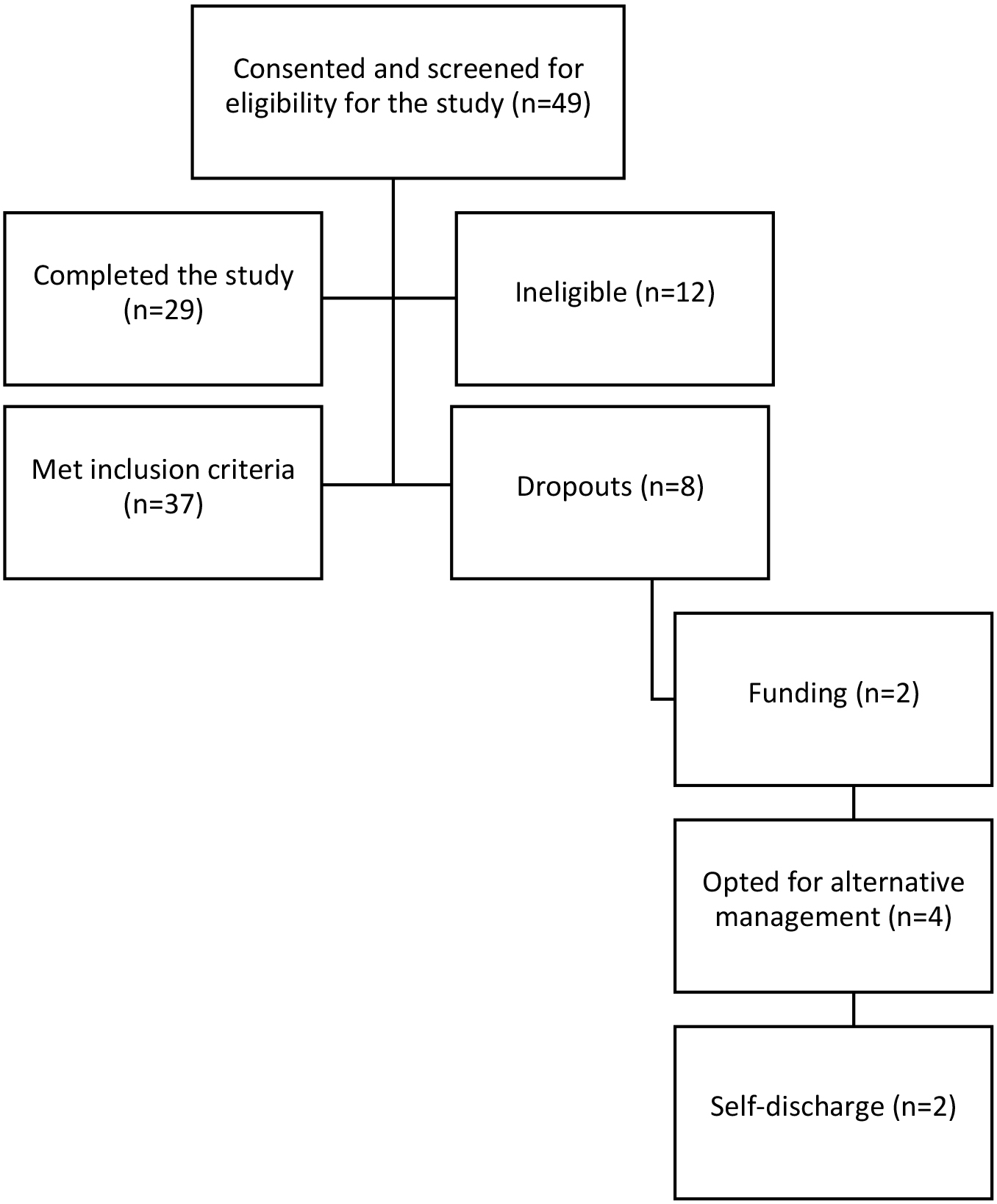
Figure 1.
Flowchart of participants’ recruitment. From the initial recruitment of forty-nine participants, a total of twenty participants were excluded: twelve participants due to ineligibility and eight participants due to purposeful withdrawal from the study. This resulted in the final twenty-nine participants who completed the study.
2.Methods
2.1Research design
This study employed a pre-test and post-test design. A consecutive sampling technique was adopted for the study. A total of forty-nine (49) participants presenting with NSCLBP were recruited from three physiotherapy clinics in Nigeria for this study out of which 12 were ineligible. However, 37 met the inclusion criteria out of these 29 completed the study. The 8 participants withdrew from the study hence data collection was discontinued for these ones as confirmed in the information sheet [22]. The dropout rate was thus calculated as 21.6% accepted in multiple published cohort studies [23, 24, 25]. There were no non-responders who completed the treatment. Figure 1 shows the flowchart of the participants and their reasons for withdrawal. Of these participants, 2 withdrew due to insufficient funding related to transportation and medical cost, 4 opted for alternative management citing personal preference, and 2 participants self-discharged. Further reasons for ineligibility and exclusion are shown in Supplement 1.
Included in this study were patients with clinical presentation of NSCLBP of not less than 3 months onset, above 18 years, who could speak and comprehend written material in English. Excluded from the study were patients with red flags such as a history of trauma to the low back, systemic disease or cancer, loss of bowel or bladder control, numbness or altered sensation in the groin region, hip, knee or spinal surgery or currently had a hip or knee injury, second and third trimesters of pregnancy and patients with cognitive impairment.
2.2Research instruments
The instruments used in this study were; I) Fear-avoidance belief questionnaire (FABQ): This was used to assess the participants’ level of FABs at baseline. Those who had a score of less than 15 on the FABQPA or less than 35 on the FABQW were classified as low on the FABQ [26]. Those who had a score of 15 or more on the FABQPA and 35 or more on the FABQW were classified as having elevated FABs. II) The Visual Analogue Scale (VAS): A self-reported scale used to rate the participants’ level of pain at various stages of intervention [27, 28]. III) Roland-morris Disability Questionnaire (RMDQ): This validated tool was used to rate the degree of participants’ disability level [29]. IV) Modified Schober’s Test (MST): This was used to measure the active range of motion (AROM) of lumbar flexion of the participants using a tape measure [30, 31]. The modified Schober test was used because of its added advantage in providing hints on patients’ pain-related fear [32]. La Touche et al. showed that patients with improvement in their LBP condition had better Lumber ROM as well as the psychosocial state [33]. Further details of the instruments’ method of use and rationale are described in Supplement 2.
2.3Procedures for data collection
After eligibility criteria were determined, demographic and anthropometric information such as name, age, gender, height, body weight and occupation were recorded for each participant. Participants’ FAB level, pain, disability and lumbar spine AROM were also assessed and recorded by the attending clinicians. All the participants performed 2 sessions of 45 minutes SSE per week for 4 weeks. Prior to the exercise, participants had a session of education and 10 minutes of infrared radiation to the lower back aimed at relaxation and to ensure optimum participation in the exercise programme. A recent systematic review also shows that infrared radiation could serve as a useful adjunct to initiate treatment of musculoskeletal conditions having the potential to provide relaxing, soothing and a placebo effect especially useful in patients with chronic pain with anxiety and fear of movement [34, 35].
The exercises were aimed to enhance neuromuscular control skills and to train deep abdominal and deep back muscles around the spine. They were divided into 3 stages as described in previous studies, which aimed to enhance neuromuscular control skills and to train deep abdominal and deep back muscles around the spine [36, 37, 38]. First, participants were given tailored illustrated information leaflets in lay language as a personal and home resource. These leaflets contain pictorial illustrations describing the anatomy and functions of the stabilizing muscles, the exercises, their purpose and how to perform them based on information from research materials aimed to increase physical activity regarding activities of daily living, and home exercises [39]. Feedback and support lines were provided in form of individualised visits and telephone calls. The follow-up time averages 15 minutes on off-clinic days and weekends. Detailed subjective records were kept using clinical notes.
The clinic and home-based exercises were all active exercises which were designed to be performed by the participants at home and without assistance. The participants were taught how to recognise if they were performing it correctly at each stage. The exercises concept was local stabilisation exercise approach, emphasizing specific training exercises for local muscles aimed at promotion of muscular endurance, stability and strength of the core local muscles that stabilize the spine such as the transversus abdominis (TrA) and lumbar multifidus (LM) [11].
The first stage of exercises was described to each of the participants with the aid of pictures illustrating the anatomy of the local stabilizing muscles such as lumbar multifidus and transversus abdominis. It involved gaining progressive sustained contraction of the deep abdominal muscles and co-activation of pelvic floor muscles. Stage 2 involved the integration of controlled movements into the movements of the extremities and in heavier loading positions. The aim of stage 3 exercises was to maintain local segmental control while a load is added through open kinetic chain movement of adjacent segments (Supplement 2).
The home exercises comprised a sequence of 10 contractions for 10 seconds of repetitions, daily. The total exercise time was approximately 45 min daily. Participants had their clinic and home re-assessed before progression. Participants were thoroughly monitored for compliance with their home activities by the researcher. Only after satisfactory compliance was achieved in line with the protocol, was the participant allowed to progress to the next stage. The outcome variables were measured at baseline, at the end of 2nd week and 4 weeks of intervention. This included the assessment and recording of pain, disability and lumbar spine AROM using VAS, RMDQ and MST respectively. The detailed exercise protocol is available in Supplement 3.
2.4Data analysis
The sample size of 32 participants was calculated a priori based on the objectives of the study. It was calculated using Cohen’s formula [
Table 1
Demographics and FAB classification of the participants
| Participants ( | n (%) | Mean |
|---|---|---|
| Gender | ||
| Female | 20 (69) | |
| Male | 9 (31) | |
| Age (Years) | 55.24 | |
| Height(m) | 1.62 | |
| Weight(kg) | 72.70 | |
| BMI (kg/m2) | 27.22 | |
| FABQW | ||
| High | 5 (17.2%) | |
| Low | 24 (82.8%) | |
| FABQPA | ||
| High | 19 (65.5%) | |
| Low | 10 (35.5%) |
FABQ: Fear-Avoidance Beliefs Questionnaire; FABQW: Fear-Avoidance Beliefs Questionnaire Work subscale; FABQPA: Fear-Avoidance Beliefs Questionnaire Physical Activity subscale. BMI: Body Mass Index.
3.Results
Table 2
Participants’ baseline outcome variables in relation to their score on the FABQW and FABQPA subscales
| Disability (RMDQ) (X | Pain (VAS) (X | AROM (MST) (X | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Low | High | Total | Low | High | Total | Low | High | Total | |
| FABQW | |||||||||
| Baseline | 11.12 (6.20) | 14.60 (2.30) | 11.72 (5.84) | 5.92 (1.61) | 6.40 (1.95) | 6.00 (1.65) | 4.23 (4.16) | 5.18 (2.19) | 4.39 (3.88) |
| 2wk | 5.83 (4.55) | 8.80 (3.96) | 6.34 (4.53) | 2.96 (1.92) | 4.40 (1.82) | 3.21 (1.95) | 6.11 (3.95) | 6.80 (2.22) | 6.23 (3.69) |
| 4wk | 1.75 (2.57) | 2.60 (3.29) | 1.90 (2.66) | 1.13 (1.26) | 1.60 (0.89) | 1.21 (1.20) | 7.85 (3.70) | 8.28 (2.46) | 7.93 (3.48) |
| FABQPA | |||||||||
| Baseline | 9.80 (5.94) | 12.74 (5.68) | 11.72 (5.84) | 4.90 (1.44) | 6.58 (1.46) | 6.00 (1.65) | 5.32 (5.65) | 3.91 (2.59) | 4.39 (3.88) |
| 2wk | 5.30 (4.57) | 6.89 (4.53) | 6.34 (4.53) | 1.50 (1.84) | 4.11 (1.33) | 3.21 (1.95) | 7.45 (5.28) | 5.58 (2.45) | 6.23 (3.69) |
| 4wk | 0.80 (1.23) | 2.47 (3.04) | 1.90 (2.66) | 0.30 (0.48) | 1.68 (1.20) | 1.21 (1.21) | 8.99 (5.16) | 7.37 (2.15) | 7.93 (3.48) |
*Significance at
Table 3
Relationship between patients’ FABQW and outcome variables
| Disability | Pain | AROM | ||||
|---|---|---|---|---|---|---|
| Sig. | Partial eta squared | Sig. | Partial eta squared | Sig. | Partial eta squared | |
| FABQW | ||||||
| Within groups | 0.001 | 0.80* | 0.001 | 0.86 | 0.01 | 0.66 |
| Between groups | 0.28 | 0.99 | 0.58 | |||
| FABQPA | ||||||
| Within groups | 0.79 | 0.90 | 0.77 | |||
| Between groups | 0.52 | 0.63 | 0.79 | |||
*Significance at
A total of 37 patients consented and met the inclusion criteria for this study, out of these 29 completed the study. Nine (31%) of the participants were males while 20 (69%) were females. Participants’ mean age was 55.24
Table 4
Correlation between outcome (pain, disability and AROM) and score on the FABQPA and FABQW subscales
| Disability | Pain | AROM | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline | 2Wk | 4Wk | Baseline | 2Wk | 4Wk | Baseline | 2Wk | 4Wk | |
| High FABQPA | |||||||||
| Pearson correlation | 0.25 | 0.16 | 0.22 | 0.45* | 0.60* | 0.49* | |||
| Sig. | 0.19 | 0.42 | 0.25 | 0.02 | 0.01 | 0.01 | 0.59 | 0.32 | 0.37 |
| High FABQW | |||||||||
| Pearson correlation | 0.40* | 0.25 | 0.12 | 0.11 | 0.28 | 0.15 | 0.09 | 0.07 | 0.05 |
| Sig. | 0.04 | 0.18 | 0.53 | 0.56 | 0.14 | 0.43 | 0.63 | 0.72 | 0.82 |
FABQPA: Fear avoidance belief questionnaire for physical activity subscale. FABQW: Fear avoidance belief questionnaire for work subscale. (High FABQP
Table 5
Multiple regression to derive determinants predicting disability outcome after 4-weeks of treatment with SSE
| Predictor | Estimate | SE |
|
|
| df | p | Adjusted |
|---|---|---|---|---|---|---|---|---|
| Intercept | 1.47 | 0.03 | 8.72 | 1,26 | 0.40 | |||
| RMDQ_Baseline | 0.26 | 0.07 | 3.74 | |||||
| GENDER | 1.75 | 0.86 | 2.03 | 0.05 |
RMDQ: Roland Morris disability questionnaire. Dependent Variable: RMDQ_4Wk. Predictors: GENDER and RMDQ_Baseline. SSE: Specific Stabilisation Excercise.
Table 6
Multiple regression to derive determinants predicting pain outcome after 4-weeks of treatment with SSE
| Predictor | Estimate | SE |
|
|
| df |
| Adjusted |
|---|---|---|---|---|---|---|---|---|
| Intercept | 0.78 | 0.14 | 6.12 | 1,24 | 0.003 | 0.62 | ||
| VAS_Baseline | 0.30 | 0.09 | 3.24 | 0.01 | ||||
| GENDER | 0.30 | 0.33 | 0.87 | 0.39 | ||||
| AROM_Baseline | 0.04 | 0.27 | ||||||
| RMDQ_4Wk | 0.20 | 0.06 | 3.47 | 0.02 |
Dependent Variable: VAS_4Wk. VAS: Visual analogue scale. Predictors: GENDER, VAS_Baseline, AROM_Baseline and RMDQ_4wk. SSE: Specific Stabilisation Excercise.
A significant difference was seen (
The results showed a significant difference (
Table 7
Multiple regression to derive determinants predicting AROM outcome after 4-weeks of treatment with SSE
| Predictor | Estimate | SE |
|
|
| df | Sig | Adjusted |
|---|---|---|---|---|---|---|---|---|
| Intercept | 6.84 | 0.91 | 7.48 | 8.60 | 1,26 | 0.81 | ||
| AROM_Baseline | 0.78 | 0.07 | 10.58 | |||||
| GENDER | 0.61 | 0.01 |
Dependent Variable: MST_4Wk. MST: Modified Schober’s test. AROM: Active Range of Motion, Predictors: GENDER and AROM_Baseline. SSE: Specific Stabilisation Excercise.
Significant correlations (
In the testing impact of variables on participants’ post-treatment outcomes, a multivariate Linear Regression was carried out with the dependent variables 4th week pain, disability and AROM. These were regressed on relevant predicting variables. Table 5 shows the predictors of outcome for disability outcome at 4th week include: baseline disability and gender. These can be viable predictors of disability after four weeks of treatment using specific stabilisation exercises since the model significance can be reported as (F (1,26)
Predictors of outcome for pain outcome at 4th week include: baseline pain level, gender, baseline AROM and disability at 4th week. These can be viable predictors of pain after four weeks of treatment using specific stabilisation exercises since the model significance can be reported as (F (1,24)
4.Discussion
This study aimed to elicit the determinants of outcome in patients with chronic non-specific LBP with associated FABs after treatment with SSE. In this study, patients had significant improvements which could be attributed to the intervention in pain relief, disability and AROM in all weeks regardless of their FAB status. This shows that SSE has the potential to improve outcomes regardless of patients’ FAB, suggesting an effective reduction in physical and psychological obstacles to recovery. The education component and graded pattern of exercises have been reported to reduce psychological obstacles to recovery in chronic pain cases possibly responsible for the outcomes in patients with high FABQ [48] and the effects of stabilisation exercise have been attributed to improving the ability to control the spine, re-education, and coordination of deep trunk muscles during static, dynamic, and functional tasks, hence reducing pain and disability for patients with low FABQ [9, 12].
This observation is similar to studies which show the effectiveness of specific stabilisation exercises on NSCLBP related outcomes [9, 38, 47]. The comparable degree of improvement in the level of disability, pain and AROM between the participants with elevated FABQW and FABQPA and those without may be because in addition to patient education, the treatment involved exercise which required participants’ active participation. This was highlighted in a study that a more tailored and intensive treatment approach, such as graded exposure to disconfirm patients’ FAB in addition to education optimises treatment outcomes [48]. Even though patient education was not directly targeted at reducing FABs, Turk and Wilson assert that most rehabilitation programs for chronic pain patients contain at least some components that are likely to be effective at reducing FABs [49].
Significant correlations were seen in this study between FABQW and disability, and FABQPA correlated significantly with pain. These subgrouping based on multiple fear avoidance measures related to work or physical activity can be seen as potentially beneficial for assessment and intervention [50]. The relationship between FAB and disability is consistent with literature reporting increased disability with elevated FAB and showing that early interventions are not only feasible but can potentially improve or prevent chronic LBP problems [51, 52].
This study also reveals that baseline AROM can predict pain outcomes after treatment with stabilisation exercises but there was a lack of correlation between lumbar spine AROM and FAB. This is consistent with other studies on pain-related fear and ROM in chronic LBP cases [53, 32]. The reason for no difference in the pain level of the participants with elevated FABQW and those with low scores post-treatment seen in this study can be explained by the FABQ validation study. It reported a poor discriminative ability of the FABQ and that the work subscale was designed to detect FAB specifically about work, therefore might be challenging in patients with non-work-related LBP [54]. A similar result was obtained from patients regarding FABQPA, there was no significant difference in pain level between patients with high and low FABQPA post-treatment. The reason may be that the participants who had a low score still exhibited some level of FAB as they performed the exercises which in turn affected their recovery [45]. Participants’ AROM recovery at the end of 2 weeks and 4 weeks of treatment were not associated with their FABQW and FABQPA scores, as noted in previous research [55], the FABQ was seen to have no association with trunk range of motion. This may also be the reason why both participants in this study who had high scores and those that had low scores responded relatively the same way to treatment.
Another reason could be because FAB associated with pain often prevent people with chronic pain from the realization that these activities may not lead to increased pain. Research shows that fear of pain and harm will likely serve as impediments to adherence to exercise regimens, leading to premature termination of treatment [49, 56]. In support of this assertion, this study recorded 2 withdrawals from the participants who found the exercises strenuous and did not want to continue. The authors noted that when patients are not directly exposed to the activity, they obtain no feedback disconfirming their maladaptive beliefs, thereby promoting disuse and disability. It was observed in this study that as participants were given the command to bend forward and reach their outstretched hands towards the floor, most of the participants initially thought that they could not perform the action. However, as they initiated the first step of the movement without feeling as intense pain as they thought, they were able to reach further down accounting for a comparable range between those who had high and those who had low FABs.
The time frame of 4 weeks duration of this study was also significant. Notably this might be considered short for full and long-term recovery and participants might have a recurrence of symptoms after the period of care since data collection discontinued after the study period. However, this recovery timeframe can be explained from several peer-reviewed publications showing this expected ‘saw-tooth’ (flare-ups and recovery) pattern of non-organic chronic low back pain behaviour [57]. Huijenen et al. and Linton et al. point to the multi-factorial nature of chronic low back pain in the absence of notable tissue damage as having significant contributions from psychosocial factors. Hence a multi-factorial approach with the potential to improve enablement, reduce fear-avoidance beliefs e.g. components of cognitive behavioural therapy and graded exposure, can be helpful in aiding rapid recovery [58, 59]. There is evidence that recovery can be rapid and bouts of relapses/episodes can occur in some patients after three months and in most cases within 12 months after intervention affecting up to 85% of chronic cases [8, 58, 60]. The clinical implication of this is that with proper therapeutic intervention and home monitoring, therapists can expect to see signs of recovery early in care but should expect to equip patients with capacity for self-care and resilience since recurrences are expected.
The predictive models developed show that gender is a predictor of outcome for disability, pain and AROM after four weeks of treatment using SSE. This can be confirmed by consistent evidence that gender as a risk factor plays a role in the prevalence and outcome of low back pain treatment globally [59]. Studies explain that this could be due to differences in sensitivity and pain thresholds, anatomical and physiological differences related to muscle strength, girth, exercise performance and participation [62]. These findings are important as disability, pain and range of motion influence the outcome of treatment in patients with LBP. Improvements in outcomes have the potential to reduce chronicity and ultimately influence the quality of life [61].
4.1Strengths and limitations
A strength of this study is its rigorous method and the strict observance of the treatment protocols and monitoring of the home exercise program. All interventions were handled by the same therapists thus providing added advantage regarding the quality and consistency of interventions. Since recommended protocols for treatment and assessment were followed the outcomes could be replicated with a good level of accuracy. In this study, the post-treatment level of FABs of the participants in this study was not assessed to see if the improvement attained was a result of an improvement in FABs score. Additionally, the level of adherence to the exercise regimen was not objectively quantified and long-term follow-up procedure beyond the duration of the study was not established. The authors think that the improvements could be attributed to FAB scores since they were consistent and occurred across all outcomes measured. Further, the level of adherence to the protocol in-home programs was monitored subjectively. Regarding the dropout rate, the researchers realise that there might be bias associated with as little as 20% lost to follow-up and this might influence the outcome. As a result, follow-up was intensified early in the study to prevent further drop-outs. In future studies, further considerations could be given to closer monitoring, real-time feedback and patients’ satisfaction could be tested which could potentially reduce the dropout rates by minimising cost and improving compliance [63].
A limitation of our study was not blinding both therapist and patients to the treatment allocation and not including a placebo/control group. The authors drew from literature that exercise therapy (regardless of the type of exercise) is at least 10 points (on a scale of 0–100 points) more effective than no treatment, hence this was justified. Further, more specific tests could be recommended based on availability and relevance to the study as an alternative to the chosen Schober test since many people with LBP might not have limitations in flexion. Care should be taken when generalising the results of this study to patients in varying contexts due to the small sample size, dropout rate and short duration of intervention. Participants were from three clinics in a specific region and the intervention was offered for a limited duration of 4 weeks. However, keeping these things in mind, the sample though small varied sufficiently in distribution and also enabled a thorough follow-up which can be seen as a strength. We think that the study’s rigor allows for some interesting comparisons to be drawn based on its findings.
5.Conclusion and recommendations
Specific stabilisation exercises may be recommended in the management of LBP patients with elevated FAB. Effective education, monitoring and grading exercises may be incorporated for optimised results affecting disability, pain and range of motion. Since pain is seen to correlate more with FABQPA and disability with FABQW, treatment aimed at pain reduction can be the focus of patients with high FABQPA and disability the focus for patients with high FABQW. Gender and baseline patient status can determine the outcome (pain, -disability, range of motion) of treatment using SSE. Therefore, these factors can inform the choice of treatment. It is recommended that measures to deal with these non-modifiable determinants should be considered preceding the management of patients with LBP. The long-term effects and sustainability of these gains could be further investigated. Based on these findings, it is recommended that further study could have a 6-month to 1-year follow-up assessment of the outcome variables utilising closer monitoring systems to observe the long-term treatment effect.
Author contributions
SI: Designed the study, recruited participants, organised data collection, analysed and interpreted the data and drafted the manuscript.
BT: Designed the study, interpreted the data, and critically revised the manuscript.
SA: Designed the study and critically revised the manuscript.
ON: Drafted the manuscript and critically revised the manuscript.
MA: Designed the study, analysed and interpreted the data, drafted the manuscript, and critically revised the document.
All authors read and approved the final version of the manuscript and are responsible for the content.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplemental information.
Ethical approval
Ethical approval for this research was sought and obtained from the Health Research and Ethics Committee (HREC) of two institutions; Lagos University Teaching Hospital, Idi-Araba, Lagos (ADM/DCST/HREC/APP/317) and Lagos State University Teaching Hospital, Ikeja, Lagos (REC/10/06/579) respectively. This study was registered on the Open Science Framework (OSF) (https://osf.io/registries/drafts/623c458c4774f103bcb54488/metadata).
Funding
The authors declare that no external source of funding was allocated to this project.
Informed consent
Informed consent was obtained from the participants prior to the commencement of the study.
Supplementary data
The supplementary files are available to download from http://dx.doi.org/10.3233/BMR-230312.
Acknowledgments
The authors would like to thank the non-academic staff members of the College of Medicine, the University of Lagos for their assistance during this research project.
Conflict of interest
The authors report no conflicts of interest.
References
[1] | Kahere M, Hlongwa M, Ginindza TG. A Scoping Review on the Epidemiology of Chronic Low Back Pain among Adults in Sub-Saharan Africa. Int J Environ Res Public Health. (2022) ; 19: (5). |
[2] | O’Sullivan K, O’Sullivan PB, O’Keeffe M. The Lancet series on low back pain: reflections and clinical implications. Br J Sports Med. (2019) ; 53: (7): 392-3. |
[3] | Fatoye F, Gebrye T, Odeyemi I. Real-world incidence and prevalence of low back pain using routinely collected data. Rheumatol Int. (2019) ; 39: (4): 619-26. |
[4] | Ge L, Pereira MJ, Yap CW, Heng BH. Chronic low back pain and its impact on physical function, mental health, and health-related quality of life: a cross-sectional study in Singapore. Sci Rep. (2022) ; 12: (1): 20040. |
[5] | Fullen B, Morlion B, Linton SJ, Roomes D, van Griensven J, Abraham L et al. Management of chronic low back pain and the impact on patients’ personal and professional lives: Results from an international patient survey. Pain Pract. (2022) ; 22: (4): 463-77. |
[6] | Lee T, Kim YH, Sung PS. A comparison of pain level and entropy changes following core stability exercise intervention. Med Sci Monit. (2011) ; 17: (7): CR362-8. |
[7] | Hlaing SS, Puntumetakul R, Khine EE, Boucaut R. Effects of core stabilization exercise and strengthening exercise on proprioception, balance, muscle thickness and pain related outcomes in patients with subacute nonspecific low back pain: a randomized controlled trial. BMC Musculoskelet Disord. (2021) ; 22: (1): 998. |
[8] | Stevans JM, Delitto A, Khoja SS, Patterson CG, Smith CN, Schneider MJ et al. Risk Factors Associated With Transition From Acute to Chronic Low Back Pain in US Patients Seeking Primary Care. JAMA Netw Open (2021) ; 4: (2): e2037371. |
[9] | Suh JH, Kim H, Jung GP, Ko JY, Ryu JS. The effect of lumbar stabilization and walking exercises on chronic low back pain: A randomized controlled trial. Medicine (Baltimore). (2019) ; 98: (26): e16173. |
[10] | Owen PJ, Miller CT, Mundell NL, Verswijveren SJJM, Tagliaferri SD, Brisby H et al. Which specific modes of exercise training are most effective for treating low back pain? Network meta-analysis. Br J Sports Med. (2020) ; 54: (21): 1279-87. |
[11] | Brumitt J, Matheson JW, Meira EP. Core stabilization exercise prescription, part 2: a systematic review of motor control and general (global) exercise rehabilitation approaches for patients with low back pain. Sports Health. (2013) ; 5: (6): 510-3. |
[12] | Smrcina Z, Woelfel S, Burcal C. A Systematic Review of the Effectiveness of Core Stability Exercises in Patients with Non-Specific Low Back Pain. Int J Sports Phys Ther. (2022) ; 17: (5): 766-74. |
[13] | Trinderup JS, Fisker A, Juhl CB, Petersen T. Fear avoidance beliefs as a predictor for long-term sick leave, disability and pain in patients with chronic low back pain. BMC Musculoskelet Disord. (2018) ; 19: (1): 431. |
[14] | Yihunie M, Abich Y, Demissie SF, Kassa T, Ranganathan P, Janakiraman B. Fear-Avoidance Beliefs for Physical Activity Among Chronic Low Back Pain: A Multicenter Cross-Sectional Study. J Pain Res. (2023) ; 16: : 233-43. |
[15] | Minobes-Molina E, Nogués MR, Giralt M, Casajuana C, Souza de DLB, Jerez-Roig J et al. Effectiveness of specific stabilization exercise compared with traditional trunk exercise in women with non-specific low back pain: a pilot randomized controlled trial. Peer J. (2020) ; 8: : e10304. |
[16] | Hanel J, Owen PJ, Held S, Tagliaferri SD, Miller CT, Donath L et al. Effects of Exercise Training on Fear-Avoidance in Pain and Pain-Free Populations: Systematic Review and Meta-analysis. Sports Med. (2020) ; 50: (12): 2193-207. |
[17] | Filiz MB, Firat SC. Effects of Physical Therapy on Pain, Functional Status, Sagittal Spinal Alignment, and Spinal Mobility in Chronic Non-specific Low Back Pain. Eurasian J Med. (2019) ; 51: (1): 22-6. |
[18] | Kumar T, Kumar S, Nezamuddin M, Sharma VP. Efficacy of core muscle strengthening exercise in chronic low back pain patients. J Back Musculoskelet Rehabil. (2015) ; 28: (4): 699-707. |
[19] | Akodu A, Okonkwo S, Akinbo S. Comparative efficacy of core stabilization exercise and pilates exercise on patients with non-specific chronic low back pain. Physiotherapy. (2016) ; 102: : e243-e244. |
[20] | Ulger O, Oz M, Ozel Asliyuce Y. The Effects of Yoga and Stabilization Exercises in Patients With Chronic Low Back Pain: A Randomized Crossover Study. Holistic Nursing Practice. (2023) ; 37: (4). |
[21] | Hayden JA, Ellis J, Ogilvie R, Malmivaara A, van Tulder MW. Exercise therapy for chronic low back pain. Cochrane Database Syst Rev. (2021) ; 9: (9): CD009790. |
[22] | Ross LF, Loup A, Nelson RM, Botkin JR, Kost R, Smith GR et al. Nine key functions for a human subjects protection program for community-engaged research: points to consider. J Empir Res Hum Res Ethics. (2010) ; 5: (1): 33-47. |
[23] | Sleith C. (2012). Methodology Checklist 3: Cohort Studies; 2023 [cited 2023 Aug 20]. Available from: URL: https://www.sign.ac.uk/what-we-do/methodology/checklists/. |
[24] | Sommer CG, Jørgensen LB, Blume B, Møller T, Skou ST, Harrison A et al. Dropout during a 12-week transitional exercise-based cardiac rehabilitation programme: a mixed-methods prospective cohort study. Eur J Cardiovasc Nurs. (2022) ; 21: (6): 578-86. |
[25] | Kristman V, Manno M, Côté P. Loss to Follow-Up in Cohort Studies: How Much is Too Much? European Journal of Epidemiology. (2004) ; 19: (8): 751-60. |
[26] | Williamson E. Fear Avoidance Beliefs Questionnaire (FABQ). Australian Journal of Physiotherapy. (2006) ; 52: (2): 149. |
[27] | Boonstra AM, Schiphorst Preuper HR, Reneman MF, Posthumus JB, Stewart RE. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int J Rehabil Res. (2008) ; 31: (2): 165-9. |
[28] | Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken). (2011) ; 63: (Suppl 11: ): S240-52. |
[29] | Roland M, Fairbank J. The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine (Phila Pa 1976). (2000) ; 25: (24): 3115-24. |
[30] | Castro MP, Stebbings SM, Milosavljevic S, Bussey MD. Construct validity of clinical spinal mobility tests in ankylosing spondylitis: a systematic review and meta-analysis. Clin Rheumatol. (2016) ; 35: (7): 1777-87. |
[31] | Rezvani A, Ergin O, Karacan I, Oncu M. Validity and reliability of the metric measurements in the assessment of lumbar spine motion in patients with ankylosing spondylitis. Spine (Phila Pa 1976). (2012) ; 37: (19): E1189-96. |
[32] | Matheve T, Baets de L, Bogaerts K, Timmermans A. Lumbar range of motion in chronic low back pain is predicted by task-specific, but not by general measures of pain-related fear. Eur J Pain. (2019) ; 23: (6): 1171-84. |
[33] | La Touche R, Grande-Alonso M, Arnes-Prieto P, Paris-Alemany A. How Does Self-Efficacy Influence Pain Perception, Postural Stability and Range of Motion in Individuals with Chronic Low Back Pain? Pain Physician. (2019) ; 22: (1): E1-E13. |
[34] | Tsagkaris C, Papazoglou AS, Eleftheriades A, Tsakopoulos S, Alexiou A, Găman M-A et al. Infrared Radiation in the Management of Musculoskeletal Conditions and Chronic Pain: A Systematic Review. Eur J Investig Health Psychol Educ. (2022) ; 12: (3): 334-43. |
[35] | van Lennep JPA, Trossèl F, Perez RSGM, et al. Placebo effects in low back pain: A systematic review and meta-analysis of the literature. Eur J Pain. (2021) ; 25: : 1876-1897. |
[36] | Koumantakis GA, Watson PJ, Oldham JA. Trunk muscle stabilization training plus general exercise versus general exercise only: randomized controlled trial of patients with recurrent low back pain. Phys Ther. (2005) ; 85: (3): 209-25. |
[37] | Mannion AF, Helbling D, Pulkovski N, Sprott H. Spinal segmental stabilisation exercises for chronic low back pain: programme adherence and its influence on clinical outcome. Eur Spine J. (2009) ; 18: (12): 1881-91. |
[38] | Puntumetakul R, Areeudomwong P, Emasithi A, Yamauchi J. Effect of 10-week core stabilization exercise training and detraining on pain-related outcomes in patients with clinical lumbar instability. Patient Prefer Adherence. (2013) ; 7: : 1189-99. |
[39] | Royal College of General Practitioners and NHS Executive. The back book: The best way to deal with back pain; get back active. 2nd ed. London: Stationery Office; (2002) . |
[40] | Cohen J. A power primer. Psychol Bull. (1992) ; 112: (1): 155-9. |
[41] | Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hoboken: Taylor and Francis; (2013) . |
[42] | AlWahaibi ISH, AlHadabi DAMY, AlKharusi HAT. Cohen’s criteria for interpreting practical significance indicators: A critical study. Cypriot Journal of Educational Science. (2020) ; 15: (2): 246-258. |
[43] | Lakens D. Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front Psychol. (2013) Nov 26; 4: : 863. |
[44] | Wertli MM, Rasmussen-Barr E, Weiser S, Bachmann LM, Brunner F. The role of fear avoidance beliefs as a prognostic factor for outcome in patients with nonspecific low back pain: a systematic review. The Spine Journal. (2014) ; 14: (5): 816-836e4.. |
[45] | Christe G, Aussems C, Jolles BM, Favre J. Patients With Chronic Low Back Pain Have an Individual Movement Signature: A Comparison of Angular Amplitude, Angular Velocity and Muscle Activity Across Multiple Functional Tasks. Front Bioeng Biotechnol. (2021) ; 9: : 767974. |
[46] | Cuschieri S. The STROBE guidelines. Saudi J Anaesth. (2019) ; 13: (Suppl 1): S31-S34. |
[47] | Akodu AK, Tella BA, Olujobi OD. Effect of stabilization exercise on pain and quality of life of patients with non-specific chronic low back pain. Af Jrl. Phys Rehab Sci. (2016) ; 7: (1-2): 7. |
[48] | Ferlito R, Blatti C, Lucenti L, Boscarino U, Sapienza M, Pavone V et al. Pain Education in the Management of Patients with Chronic Low Back Pain: A Systematic Review. J Funct Morphol Kinesiol. (2022) ; 7: (4): 74. |
[49] | Turk DC, Wilson HD. Fear of pain as a prognostic factor in chronic pain: conceptual models, assessment, and treatment implications. Curr Pain Headache Rep. (2010) ; 14: (2): 88-95. |
[50] | Ganesh GS, Sahu PK, Das SP, Mishra C, Dhiman S. A subgroup analysis to compare patients with acute low back pain classified as per treatment-based classification. Physiother Res Int. (2019) ; 24: (1): e1747. |
[51] | Adje M, Steinhäuser J, Stevenson K, Mbada C, Karstens S. Patients’ and physiotherapists’ perspectives on implementing a tailored stratified treatment approach for low back pain in Nigeria: a qualitative study. BMJ Open. (2022) ; 0: : e059736. |
[52] | Langenmaier A-M, Amelung VE, Karst M, Krauth C, Püschner F, Urbanski D et al. Subgroups in chronic low back pain patients – a step toward cluster-based, tailored treatment in inpatient standard care: On the need for precise targeting of treatment for chronic low back pain. Ger Med Sci. (2019) ; 17. |
[53] | Thomas JS, France CR. The relationship between pain-related fear and lumbar flexion during natural recovery from low back pain. Eur Spine J. (2008) ; 17: (1): 97-103. |
[54] | Cleland JA, Fritz JM, Brennan GP. Predictive validity of initial fear avoidance beliefs in patients with low back pain receiving physical therapy: is the FABQ a useful screening tool for identifying patients at risk for a poor recovery? Eur Spine J. (2008) ; 17: (1): 70-9. |
[55] | Karayannis NV, Smeets RJEM, van den Hoorn W, Hodges PW. Fear of Movement Is Related to Trunk Stiffness in Low Back Pain. PLoS One. (2013) ; 8: (6): e67779. |
[56] | Adje M, Steinhäuser J, Laekeman M, Rogan S, Karstens S. Evaluation of a blended learning approach on stratified care for physiotherapy bachelor students. BMC Medical Education. (2023) ; 23: (1): 545. |
[57] | Huijnen IPJ, Rusu AC, Scholich S, Meloto CB, Diatchenko L. Subgrouping of low back pain patients for targeting treatments: evidence from genetic, psychological, and activity-related behavioral approaches. Clin J Pain. (2015) ; 31: (2): 123-32. |
[58] | Cuomo A, Cascella M, Vittori A, Marinangeli F. Chronic low back pain as a biopsychosocial disease: time to change our point of view. J Anesth Analg Crit Care. (2021) ; 1: (1): 7. |
[59] | Alamam DM, Moloney N, Leaver A, Alsobayel HI, Mackey MG. Multidimensional prognostic factors for chronic low back pain-related disability: a longitudinal study in a Saudi population. Spine J. (2019) ; 19: (9): 1548-58. |
[60] | Freburger JK, Holmes GM, Agans RP, Jackman AM, Darter JD, Wallace AS et al. The rising prevalence of chronic low back pain. Arch Intern Med. (2009) ; 169: (3): 251-8. |
[61] | Nieminen LK, Pyysalo LM, Kankaanpää MJ. Prognostic factors for pain chronicity in low back pain: a systematic review. Pain Rep. (2021) ; 6: (1): e919. |
[62] | Alnojeidi AH. Gender Differences in Low Back Pain and Self-Reported Muscle Strengthening Activity Among US.. Adults [cited 2022 May 29]. Available from: URL: https//digitalcommons.unf.edu/cgi/viewcontent.cgi?article=1626&context=etd. |
[63] | Mahmoud IAM. Usability of Telemedicine in Physical Therapy Rehabilitation: Systematic review. JMIR Rehabil Assist Technol (2021) . |




