Effects of breathing exercises on chronic low back pain: A systematic review and meta-analysis of randomized controlled trials
Abstract
BACKGROUND:
A range of studies concerning the effects of breathing exercises on chronic low back pain (CLBP) have been proven inconclusive.
OBJECTIVE:
The study aimed to evaluate the effectiveness of breathing exercises for the treatment of CLBP.
METHODS:
We considered randomized controlled trials in English or Chinese that used breathing exercises for the treatment of CLBP. An electronic search was performed in the MEDLINE, EMBASE, Web of Science, Cochrane Library, CNKI, Wan Fang, and CBM databases for articles published up to November 2022. Two reviewers independently screened the articles, assessed the risk of bias using the Cochrane risk of bias tool, and extracted the data. The outcomes included pain, lumbar function and pulmonary function post-intervention.
RESULTS:
A total of thirteen studies (
CONCLUSION:
Breathing exercises can reduce pain, assist people with lumbar disabilities, and improve pulmonary function, and could be considered as a potential alternative treatment for CLBP.
1.Introduction
Low back pain (LBP) is clinically defined as pain, muscle tension, or stiffness localized below the costal margin and above the inferior gluteal folds, with or without leg pain [1]. Chronic low back pain (CLBP) is characterized as experiencing LBP for more than 12 weeks [2]. It causes pain and functional impairment and has in recent years, been the leading cause of disability across the globe [3, 4]. The lifetime prevalence of LBP is approximately 80% while the prevalence of CLBP is in the region of 23% [5] with more than half a billion people suffering from CLBP globally [6]. As global incidents of CLBP have escalated, it has impacted its sufferers physically and psychologically; additionally, it has placed overwhelming financial strain on economies around the world, due to the expense of medical treatment and widespread absenteeism from work in all socio-economic areas [7, 8].
Currently, there is no well-defined, established paradigm for the treatment and management of CLBP. Although patients with CLBP are frequently managed with pharmacological therapy, a lack of efficacy combined with adverse events can result in unresolved complications [9]. Nonpharmacologic therapies, including exercise and psychosocial management, are the preferred approach for the majority of patients and may be supplemented with adjunctive drug therapies [10, 11, 12]. According to clinical practice guidelines, the implementation of exercise therapy is advocated as a primary treatment as it performs a fundamental role in pain reduction and developing improved levels of mobility and function [13, 14]. Clinical observations have noted that breathing exercises are crucial to the treatment and prevention of CLBP [15, 16, 17]. Breathing exercises support muscle activation which strengthens core muscles; greatly improves spinal stabilization via the co-contracting of deep muscles such as the internal oblique abdominals, multifidus, and pelvic floor muscles; and significantly increases muscle thickness (in contraction); and improves contraction rates [18, 19]. Additionally, breathing exercises modify the patient’s pulmonary function by improving their forced vital capacity alongside other oxygenation and blood volume indicators, allowing for the development of enhanced breathing patterns and improving lumbar pain and function [20]. A combination of these physical factors creates a scenario whereby a patient will experience reduced levels of anxiety concerning their motor performance and improvements in their mental well-being [21].
While some studies have demonstrated the potential benefits of breathing exercises for the treatment of CLBP, it remains whether breathing exercises are more effective than the current rehabilitation therapy paradigm [22]. Therefore, this systematic review and meta-analysis intend to quantitatively analyze clinical studies concerning the implementation of breathing exercises for the treatment of CLBP as it relates to the symptoms (pain, lumbar function, and pulmonary function) and to conduct a direct comparison between breathing exercises and the current routine rehabilitation exercises.
2.Methods
This systematic review was performed in accordance with the preferred reporting items for systematic reviews and meta-analyses (PRISMA) and was registered in the PROSPERO database under identification number CRD42022380578.
2.1Search strategy
We searched for articles in PubMed, EMBASE, Web of Science, Cochrane, CNKI, Wan Fang, and the CBM databases from their inception to November 2022. The following Medical Subject Headings (MeSH) terms and keywords were used as the primary search terms: breathing exercise, respiratory exercise, expiratory training, respiratory muscle training, LBP, back pain, and CLBP. Reference lists of the relevant studies and reviews were manually screened to ascertain the existence of additional studies that were suitable for inclusion. The Appendix provides an example of PubMed’s search strategy.
2.2Inclusion and exclusion criteria
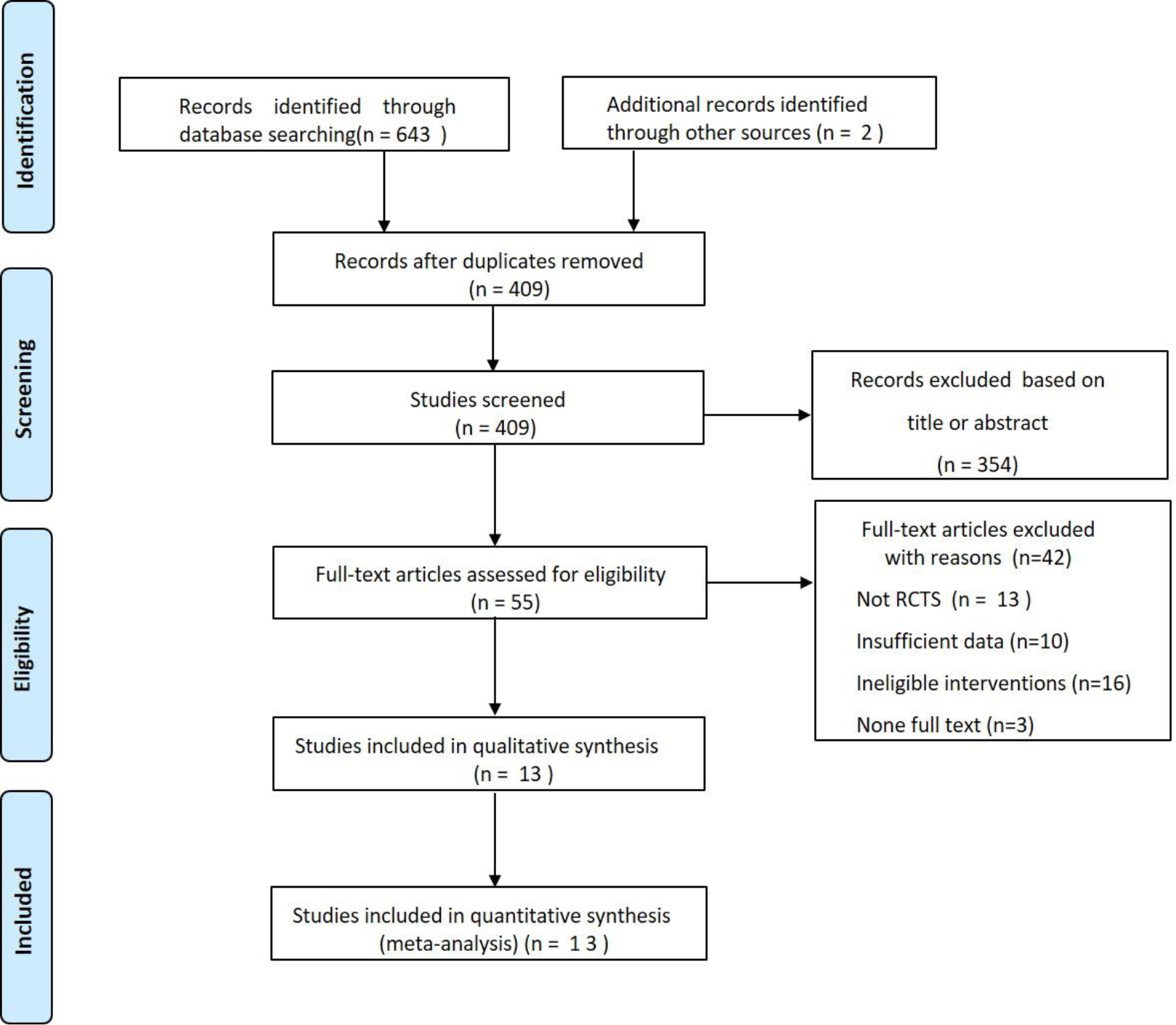
Figure 1.
Flowchart of search strategy and study selection.
Studies were eligible if they met the following criteria: (1) used the randomized controlled trial (RCT) design; (2) included participants diagnosed with CLBP (18 years of age or older), regardless of gender, social factors, or the clinical setting; (3) compared breathing exercises with the placebo (sham tape) or routine rehabilitation intervention (e.g., physical therapy, exercise therapy, spinal stabilization); (4) the study included at least one of the following outcome assessments: pain, pulmonary function, or lumbar function; and (5) where chronic pain was defined as lasting more than 12 weeks.
Studies were excluded if any of the following criteria were met: (1) studies were crossover trials, quasi-RCTs, case reports, animal experiments, conference abstracts, and review articles; (2) studies with unavailable data or low-quality; (3) included patients with LBP caused by pathological changes such as tumours, spinal infections, ankylosing spondylitis, spondylolisthesis, or any extensive neurological disorder.
2.3Literature screening and data extraction
After the titles and abstracts from the search results on the electronic databases were browsed, the full texts of all potentially eligible studies were downloaded and analyzed. Relevant data, including the title, first author, publication year, details of participants (size in each group, baseline characteristics), details of the study (study design; Randomization methods), interventions for each group (details of breathing exercises used), measurements of primary and secondary outcomes, statistical methods, exit conditions and reasons, information was independently extracted and confirmed by the independent researchers using standardized data extraction tables according to inclusion criteria. A research team obtained information from the included studies, and disagreements among the reviewers were resolved through discussion.
Table 1
Summary of included studies
| Author (year) | Country | Group (n): | Male/ | Description of intervention | Duration | Outcome | |
|---|---|---|---|---|---|---|---|
| age (mean | Female | Intervention group | Control group | measurements | |||
| Ahmadnezhad, 2020 [19] | Iran | E(23)21.43 | 11/12 12/12 | Breathing exercise | Strength Training | 8 ws, 2t/d, 7x/wk | FVC, FEV1, VAS, |
| Park, 2020 [20] | Korea | E(20)39.5 | 20 20 19 | Breathing exercise | Lumbar stabilization exercise | 6 ws, 10-min sessions, 5x/wk | FVC, FEV1 |
| Borujeni, 2020 [18] | Iran | E(24) 20.14 | 11/13 12/12 | Breathing exercise | Strength Training | 8 ws, 2t/d, 7x/wk | VAS |
| Park, 2019 [21] | South Korea | E(20)30.9 | 12/8 12/11 | Breathing exercise | lumbar stabilization exercises | 4 ws, 40-min sessions, 3x/wk | FVC, FEV1, FEV1/FVC, MVV, ODI |
| Mehling, 2005 [23] | USA | E(16)49.7 | 5/11 5/7 | Breathing exercise | physical therapy | 6 ws 45-min sessions, 12t/6ws | VAS |
| Oh, 2020 [16] | South Korea | E(22)46.14 | 0/22 0/22 | Breathing exercise | lumbar stabilization exercises | 4 ws, 50-min Sessions, 3x/wk | FVC, FEV1, FEV1/FVC, MVV, VAS, ODI |
| Kang, 2016 [24] | Korea | E(10)42.5 | 10/0 10/0 | Breathing exercise | spinal stabilization exercise | 6 ws. 20-min sessions, 5x/wk | ODI |
| Zhang, 2019 [25] | China | E(33)39.43 | 18/15 20/13 | Breathing exercise | core strength training | 4 ws, 10 to 30-min sessions, 5x/wk | VAS |
| Fan, 2018 [26] | China | E(30)40.87 | 17/13 15/15 | Breathing exercise | core strength training | 4 ws, 10 to 30-min sessions, 5x/wk | VAS, ODI |
| Fei, 2018 [27] | China | E(13)25.78 | 5/8 5/9 | Breathing exercise | sling exercise training | 8 ws, 30 to 55-min sessions, 3x/wk | VAS, ODI |
| Yang, 2020 [28] | China | E(42)28.26 | 27/15 24/18 | Breathing exercise | Postural control training | 6 ms, 3x/wk | VAS, ODI |
| Zhang, 2021 [29] | China | E(40)67.22 | 25/15 23/17 | Breathing exercise | Core strength training | 3 ms, 15-min sessions, 4x/wk | VAS, ODI |
| Liu, 2022 [30] | China | E(24)40.1 | 10/14 12/11 11/12 | Breathing exercise | Core strength training | 6 ws, 2t/d, 5x/wk | VAS, ODI |
Note: EG: experimental group; CG: control group; FVC: Forced Vital Capacity; FEV1: Forced Expiratory Volume in the first second; FEV1/FVC: Forced Expiratory Volume in the first second /Forced Vital Capacity; MVV: Maximal Voluntary Ventilation VAS: Visual Analog Scale; ODI: Oswestry Disability Index; ws: weeks; ms: months.
2.4Quality assessment
The quality of all included studies in this review was independently evaluated by the research team by using the Cochrane collaboration tool of risk of bias. Studies included low, unclear or high risk of bias in the following domains: random sequence generation, allocation concealment, blinding of participants, blinding of outcome assessment, incomplete outcome data, selective reporting and other sources of bias. Each study was independently assessed by the research team, and any discrepancies were resolved through discussion.
2.5Statistical analysis
Statistical analyses were performed using Cochrane Review Manager 5.3 and Comprehensive Meta-Analysis. Continuous data will use the weighted mean difference (MD) or standardized mean difference (SMD), while the corresponding 95% confidence interval (CI) will be reported. Heterogeneity among the studies was evaluated using the I
3.Results
3.1Literature selection
The flow diagram of the article screening process is exhibited in Fig. 1. 643 related articles were identified through database searching and 2 additional records were identified through reading the published reviews. After the whole selection process, 13 studies with 807 patients were included in the meta-analysis for statistical comparison.
3.2Characteristics of included literature
The main features of the included studies are recorded in Table 1. Sixteen studies (from China, the USA, Iran, and Korea) were included in this summary. All of the results were published between 2005 and 2022 and contained the details of a total of 807 participants. The baseline data of the included studies demonstrated no significant difference. Ten studies [20, 21, 28] chose VAS assessment as the primary method of pain assessment for CLBP patients. Eight studies [20, 21, 28] elected to use the ODI for lumbar function assessment. Four studies [23, 24, 25, 27, 29, 30, 33, 35] assessed pulmonary function by FEV1; four studies [22, 23, 24, 25, 32, 33, 35] assessed pulmonary function using FVC; three studies assessed pulmonary function by FEV/FVC, and two studies reported pulmonary function with MVV.
Figure 2.
Plot of the risk of bias of the included studies.
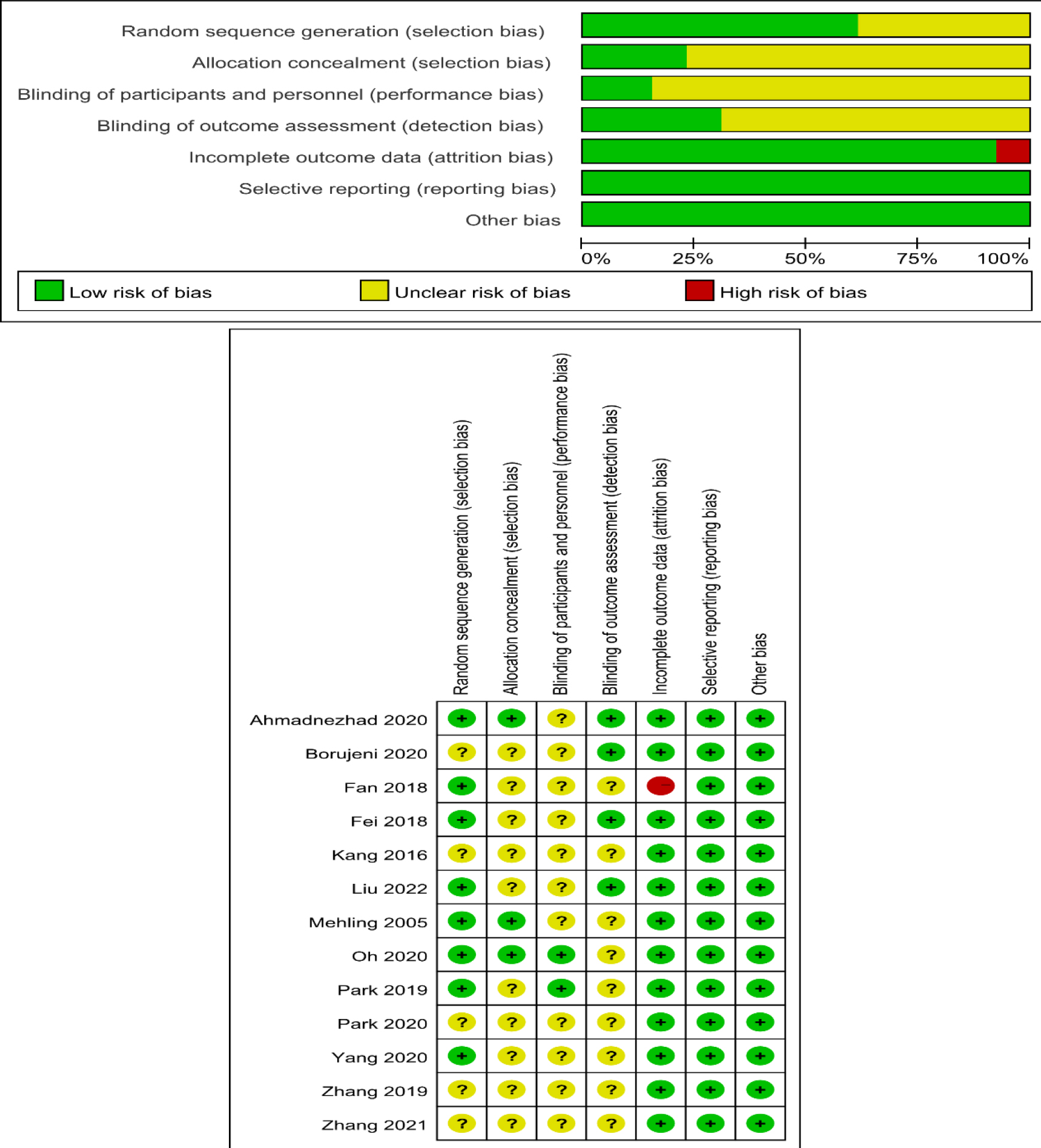
3.3Quality assessment
Figure 3.
Forest plot of pain. Abbreviation. VAS, Visual Analog Scale.
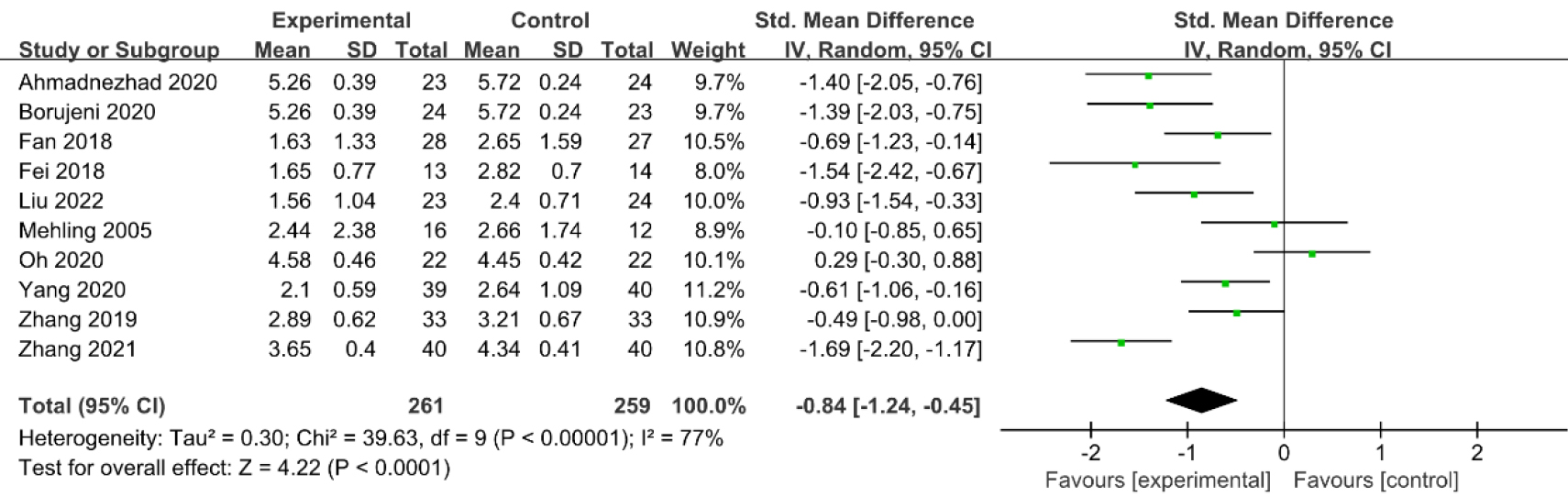
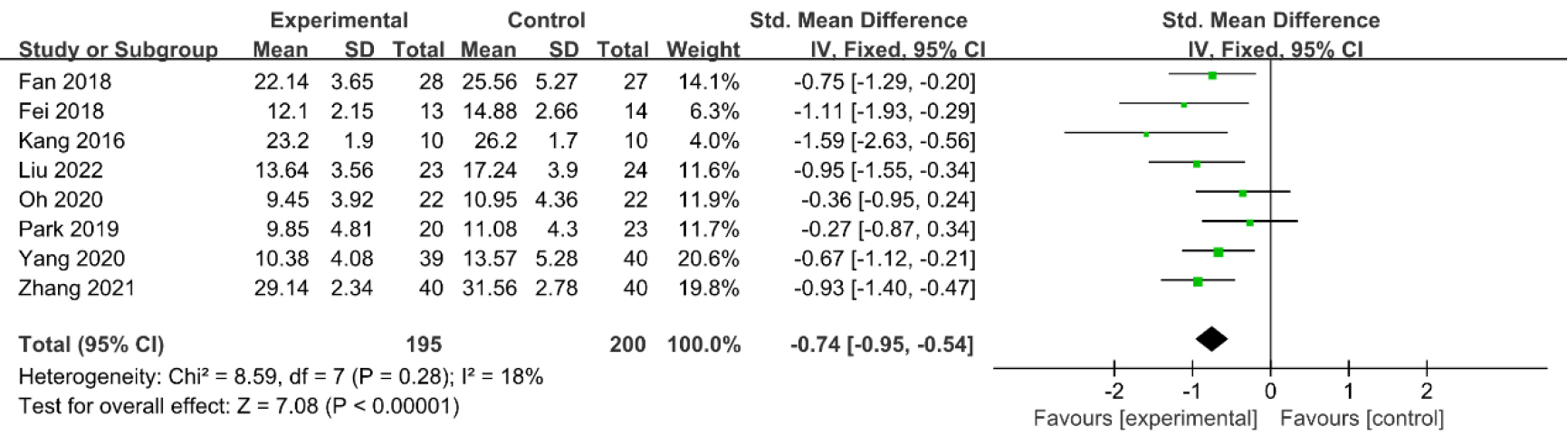
Figure 4.
Forest plot of lumbar function. Abbreviation. ODI, Oswestry Disability Index.
The quality assessment results for the included articles are shown in Fig. 2. Randomization was performed in all the studies, and eight of them detailed the randomization methods [16, 19, 21, 23, 26, 27, 28, 30]. The blinding of participants and personnel was mentioned in two articles [16, 19]; two studies reported the blinding of participants and personnel [16, 21], and four studies recorded the blinding of outcome assessment [18, 19, 27, 30]. Only one study [26] contained incomplete data as it should have reported dropout reasons and was, therefore, considered to demonstrate high-risk detection bias. The overall risk of bias was assessed as low when considering incomplete outcome data, selective reporting, and other forms of bias.
3.4Results of meta-analysis
3.4.1VAS
Ten studies [16, 18, 19, 23, 25, 26, 27, 28, 29, 30] reported that VAS was employed to evaluate lumbar pain. The meta-analysis indicated that breathing exercises could significantly improve lumbar pain when compared with the control group (SMD
3.4.2ODI
Eight studies [16, 21, 24, 26, 27, 28, 29, 30] reported that ODI was used to evaluate lumbar function. The meta-analysis indicated that breathing exercise could significantly improve lumbar function when compared with the control group (SMD
Figure 5.
Forest plot of lung function. Abbreviation. FEV1, Forced Expiratory Volume in the first second.
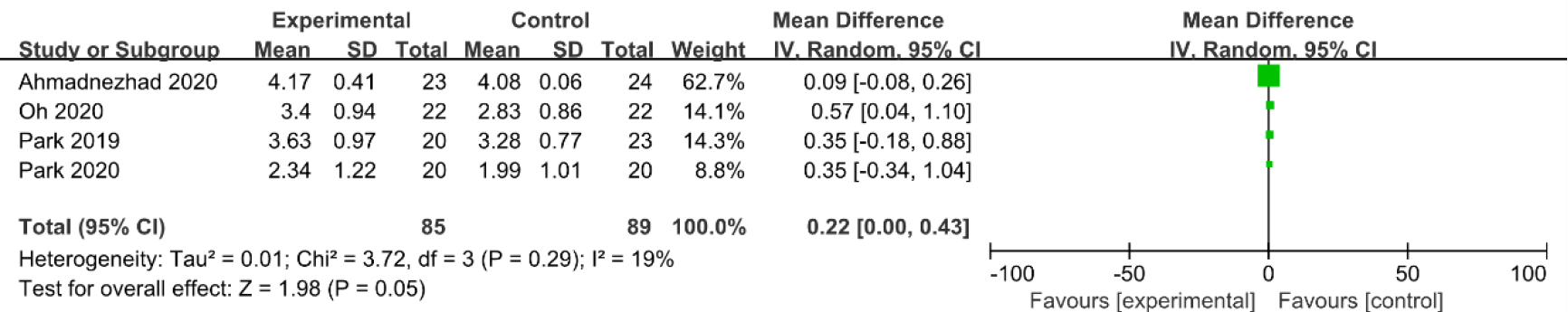
3.4.3FEV1
Four studies [16, 19, 20, 21] reported that FEV1 was used to evaluate pulmonary function. The meta-analysis indicated that breathing exercises could not significantly improve pulmonary function when compared with the control group (MD
Figure 6.
Forest plot of lung function. Abbreviation. FVC, Forced Vital Capacity.
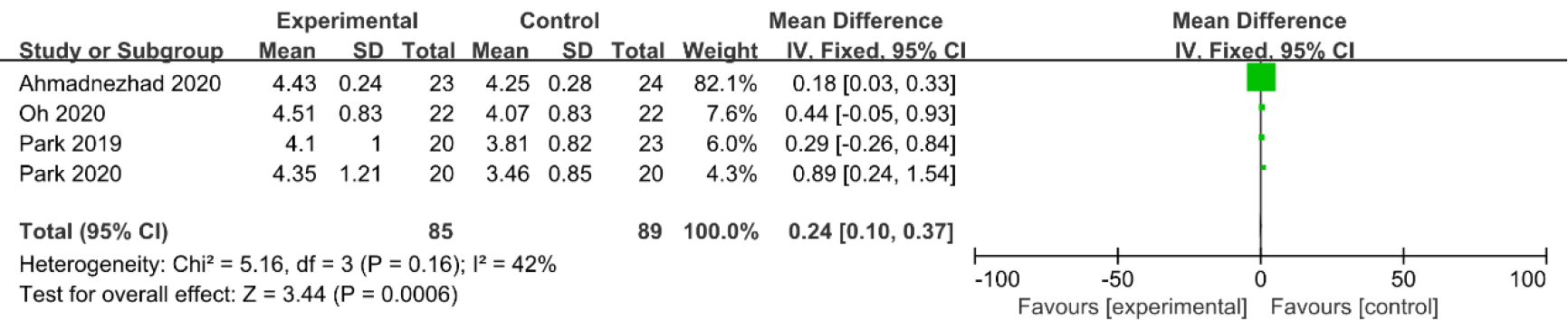
3.4.4FVC
Four studies [16, 19, 20, 21] reported that FVC was used to evaluate pulmonary function. The meta-analysis indicated that breathing exercises could significantly improve pulmonary function when compared with the control group (MD
3.4.5FEV/FVC
Three studies [16, 19, 21] reported that FVC/FEV1 was used to evaluate pulmonary function. The meta-analysis indicated that breathing exercises could significantly improve pulmonary function compared with the control group (MD
Figure 7.
Forest plot of lung function. Abbreviation. FEV1/FVC, Forced Expiratory Volume in 1 second /Forced Vital Capacity.
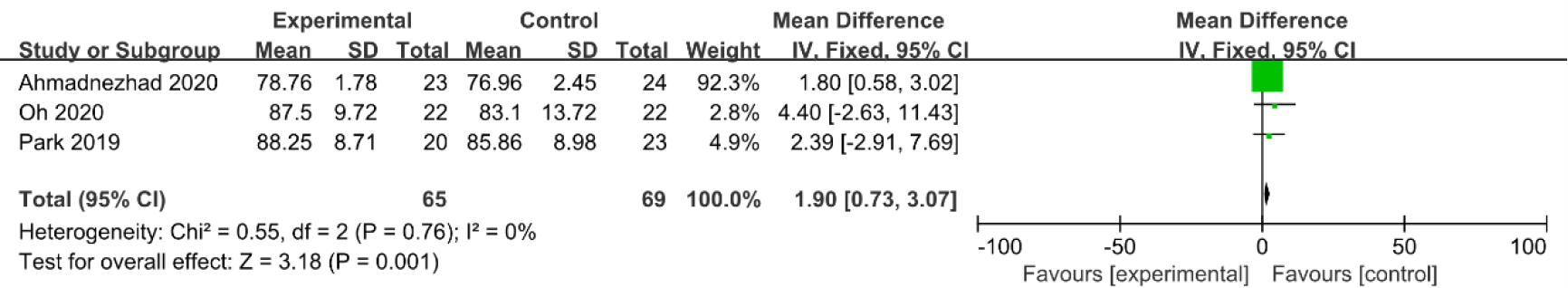
Figure 8.
Forest plot of lung function. Abbreviation. MVV, Maximal Voluntary Ventilation.
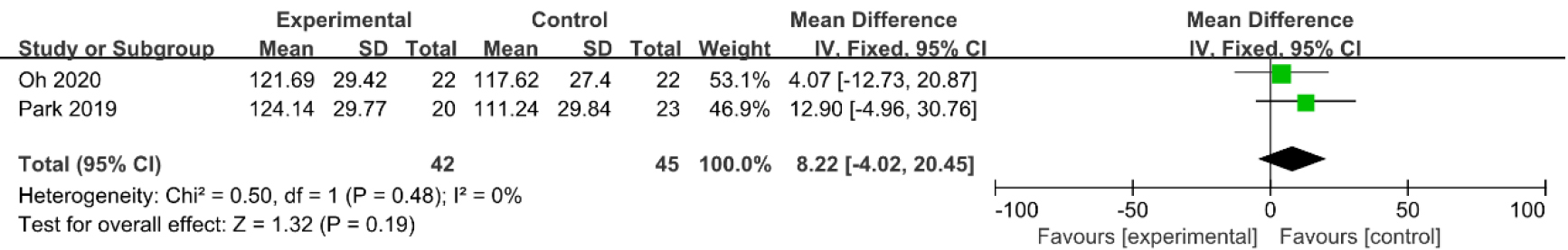
3.4.6MVV
Two studies [16, 21] reported that the MVV was used to evaluate pulmonary function. The meta-analysis indicated that breathing exercises could not significantly improve pulmonary function when compared with the control group (MD
4.Discussion
CLBP is a complex musculoskeletal disorder characterized by pain, reduced muscle strength, imbalance and motor dysfunction [29]. The primary cause of LBP is lumbar instability and muscle imbalances [3, 30]. Additionally, many studies have demonstrated that CLBP patients are susceptible to respiratory diseases and respiratory muscle atrophy, and there may be an association between respiratory function, breathing patterns, core stability, and CLBP [12, 31]. Clinical studies have revealed that breathing exercises can enhance respiratory function, reduce pain, and improve low back function in patients experiencing CLBP [27, 28]. This study was the first meta-analysis to evaluate the effectiveness and safety of breathing exercises for treating CLBP. Following a comprehensive search of the major academic databases, thirteen studies with 677 participants were involved in this meta-analysis. The results of the meta-analysis conclude that breathing exercises were effective for the treatment of CLBP: in cases involving the use of VAS and ODI, breathing exercises provided improved pain relief and enhanced lumbar function in comparison with the control group. In addition, when examining the indicators of pulmonary function outcomes such as FVC and FEV/FVC, the implementation of breathing exercises improved pulmonary function more effectively than the control group. However, no statistical significance was demonstrated in FEV1 and MVV: these results should be interpreted with care due to the low number of studies available for FEV1 and MVV pulmonary function outcomes (
The meta-analysis revealed that breathing exercises significantly improved VAS and ODI scores compared to the control group, indicating that breathing exercises are effective for relieving and enhancing low back function in CLBP patients. The underlying mechanisms of breathing exercises for the treatment of CLBP were unclear; however, chronic pain can occur when the muscles of the low back experience instability caused by dysfunction and motor control damage [31]. Studies have revealed that postural control and respiratory function are mechanically and neuromuscularly co-dependent [32]. Respiration and spinal stabilization involve the diaphragm, the transverse abdominal muscle, the pelvic floor muscle, and the intercostal and internal oblique muscles [33, 34]. The pain experienced by CLBP patients can be effectively managed and reduced via increased local muscle activity. Co-contraction of the muscles, instigated by breathing exercises, combined with sustained muscle activity, proper muscle length and muscle strength, promotes the development of the deep abdominal muscles [32, 35]. As a result, the distribution of stimuli on pain receptor tissues surrounding the spine, articular capsules, and ligaments will decrease [33]. As well as being vital to respiration, the respiratory muscles play a fundamental role in controlling posture, acting as core stabilizing muscles. Therefore, breathing exercises are likely to impact postural control by affecting the core stabilisers and altering posture, increasing co-contraction of the core muscles that determine trunk stabilisation, improving the intervertebral joints and increasing motor control, which may lead to an increase in a patient’s spinal stability and balance ability [36, 37].
Many studies have demonstrated that respiratory muscle function and back proprioception control are mechanically and physiologically dependent on each other [38]. The intense contraction of the abdominal muscles caused by breathing exercises increases intra-abdominal pressure, which may lower the lumbar curve and significantly reduce the pressure exerted vertically, helping to improve balance and proprioception [16, 39]. Breathing patterns have been demonstrated through improvement following the introduction of various forms of breathing exercises which activate the deep stabilizing muscles of the trunk to maintain spinal stability and control [35]. When focusing on diaphragmatic breathing, it is essential to re-establish correct breathing patterns and ensure lumbar spine stabilization by increasing intraabdominal pressure and activating core structures to transfer force from the centre of the body to the lower extremities [40]. Following the action of the diaphragm, intra-abdominal pressure increases and activates the pelvic floor muscle causing it to contract, which enables the transversus abdominis to be easily activated during breathing due to strong abdominal contractions [24]. Furthermore, the nerves of the associated muscles are stimulated by the movement, such as the thoracoabdominal nerve, are stimulated by the movement, which results in increased local muscle activity [19, 41]. Respiratory interventions can enhance the diaphragm’s trunk stabilizing function, enabling individuals to use lumbar proprioception and reduce postural sway during balance control [35].
The findings of this review have partially clarified that breathing exercises can improve the respiratory function of CLBP patients, as demonstrated by FVV and FEV/FVC. CLBP is closely correlated with respiratory disorders [42]. Patients with CLBP are reported to be susceptible to diaphragmatic and muscular fatigue, lung capacity deviations, and diaphragm biomechanics [35, 43]. Respiratory function is often overlooked when examining patients with CLBP, although it can contribute to the instability of the lumbar spine and injuries in this region [30]. Meanwhile, a bi-directional interconnection exists between pain and respiration: respiratory fluctuations can occur in response to pain. As established by previous theories, long-term respiratory exercise has the potential to influence core muscle activity and improve respiratory and lumbar function [19, 44]. The respiratory muscles may promote lung ventilation, improve lung function parameters, deliver oxygen to the blood, and relieve pain [45]. Local muscle activity may also alter lung function parameters [46, 47]. Enhancing the stability of the trunk muscle through appropriate breathing pattern training, has been demonstrated to be a vital factor in reducing CLBP and preventing recurrence [38]. When considering reports detailing the adverse effects of respiratory training included in the literature, it was found that only one patient, in a study conducted by Mehling et al. [19], chose to withdraw due to the resurfacing of old memories, which resulted in the participant experiencing uncomfortable emotions. Subsequent other studies found no other adverse events.
Breathing exercises appear to be a promising and practical approach to treating CLBP and may enhance performance, prevent injury, encourage rehabilitation, and improve breathing capacity, trunk stability and balance [34]. Currently, control intervention (passive physiotherapy) is not recommended by the National Institute for Health and Care Excellence (NICE) [48]. The current consensus is that any active component of the intervention is more likely to demonstrate improved long-term outcomes for pain than passive physiotherapy [48, 49]. Breathing exercises are aerobic exercises that focus on motor control and reinforcing proper breathing patterns, which can increase the strength of respiratory muscles, improve spinal stability, and can be easily incorporated into daily activities to prevent CLBP and its related conditions [19, 35]. A recent study also reported reduced diaphragm thickness and lower respiratory function in athletes who suffered from LBP compared to healthy athletes [50]. For sports people undergoing CLBP rehabilitation or sports training, it is essential to incorporate breathing exercises to effectively activate the deeper trunk muscles and nerves associated with the low back, improve muscle blood flow and muscle oxygenation to the low back, and enhance athletic physical performance [51]. For medical workers with CLBP, such as nurses, breathing exercises effectively lower the parasympathetic nerves, inhibit pain gate control, improve stress management, and relieve CLBP symptoms, preventing occurrences of LBP or accelerating recovery [49, 52, 53]. Therefore, it is recommended that athletes and workers employ breathing exercises in training or daily activities to strengthen the health management of CLBP.
4.1Strengths and limitations
Breathing exercises are beneficial and are proven clinically effective. They do not require any rehabilitation equipment and, once mastered, can be performed at home, at work or in a hospital as part of a prevention or recuperation programme. In addition, no adverse events were reported in the literature analysed by this study, and the employment of breathing exercises should be promoted. However, the meta-analysis conducted by this study does contain limitations which require consideration. Meta-analysis can increase diagnostic power by amalgamating small-scale, low-quality studies; however, its findings can be affected by certain factors, including the variety of exercises (abdominal breathing, inspiratory muscle training, and respiratory resistance training), the varied quality and heterogeneity of the studies selected for inclusion, and possible biases. There were significant variances between the ten clinical trials included in the meta-analysis; these disparities concerned factors such as sample size, study design, and outcome definition. Additionally, these studies lacked indicators such as balance function and long-term prognosis, and there is a requirement for additional, well-organised trials to further evaluate the efficacy of breathing exercises.
5.Conclusion
In this study, the evidence indicated that breathing exercises may be an effective treatment for CLBP. However, further studies with rigorous methodological quality are needed to support the conclusions of this research. Future studies should investigate different varieties, frequencies and intensities of breathing exercises to discover the most clinically effective breathing exercises.
Ethical approval
Not applicable.
Funding
The authors report no funding.
Informed consent
Not applicable.
Author contributions
X.J. and H.B. made substantial contributions to the conception and design of the work; Q.C. and Q.X. researched and selected materials and extracted data; X.J. wrote this manuscript; X.J., Q.C., G.C. and H.B. revised the paper carefully and contributed to the statistical analyses. All authors read and approved the final manuscript.
Supplementary data
The supplementary files are available to download from http://dx.doi.org/10.3233/BMR-230054.
Acknowledgments
The authors have no acknowledgments.
Conflict of interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
[1] | Vlaeyen JWS, Maher CG, Wiech K, et al. Low back pain. Nat Rev Dis Primers. (2018) ; 4: (1): 52. |
[2] | Koes BW, van Tulder MW, Thomas S. Diagnosis and treatment of low back pain. BMJ. (2006) ; 332: (7555): 1430-4. |
[3] | Hartvigsen J, Hancock MJ, Kongsted A, et al. What low back pain is and why we need to pay attention. Lancet. (2018) ; 391: (10137): 2356-67. |
[4] | Stewart Williams J, Ng N, Peltzer K, et al. Risk Factors and Disability Associated with Low Back Pain in Older Adults in Low- and Middle-Income Countries. Results from the WHO Study on Global AGEing and Adult Health (SAGE). PLoS One. (2015) ; 10: (6): e0127880. |
[5] | Balagué F, Mannion AF, Pellisé F, et al. Non-specific low back pain. Lancet. (2012) ; 379: (9814): 482-91. |
[6] | Hurwitz EL, Randhawa K, Yu H, et al. The Global Spine Care Initiative: a summary of the global burden of low back and neck pain studies. Eur Spine J. (2018) ; 27: (Suppl 6): 796-801. |
[7] | Alleva J, Hudgins T, Belous J, et al. Chronic low back pain. Dis Mon. (2016) ; 62: (9): 330-3. |
[8] | Ge L, Pereira MJ, Yap CW, et al. Chronic low back pain and its impact on physical function, mental health, and health-related quality of life: a cross-sectional study in Singapore. Sci Rep. (2022) ; 12: (1): 20040. |
[9] | Urits I, Burshtein A, Sharma M, et al. Low Back Pain, a Comprehensive Review: Pathophysiology,Diagnosis, and Treatment. Curr Pain Headache Rep. (2019) ; 23: (3): 23. |
[10] | Chou R. Low Back Pain. Ann Intern Med. (2021) ; 174: (8): Itc113-itc28. |
[11] | Farì G, de Sire A, Fallea C, et al. Efficacy of Radiofrequency as Therapy and Diagnostic Support in the Management of Musculoskeletal Pain: A Systematic Review and Meta-Analysis. Diagnostics (Basel). (2022) ; 12: (3): 600. |
[12] | Farì G, Santagati D, Pignatelli G, et al. Collagen Peptides, in Association with Vitamin C, Sodium Hyaluronate, Manganese and Copper, as Part of the Rehabilitation Project in the Treatment of Chronic Low Back Pain. Endocr Metab Immune Disord Drug Targets. (2022) ; 22: (1): 108-15. |
[13] | Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. (2007) ; 147: (7): 478-91. |
[14] | Oliveira CB, Maher CG, Pinto RZ, et al. Clinical practice guidelines for the management of non-specific low back pain in primary care: an updated overview. Eur Spine J. (2018) ; 27: (11): 2791-803. |
[15] | Anderson BE, Bliven KCH. The Use of Breathing Exercises in the Treatment of Chronic, Nonspecific Low Back Pain. J Sport Rehabil. (2017) ; 26: (5): 452-8. |
[16] | Oh YJ, Park SH, Lee MM. Comparison of Effects of Abdominal Draw-In Lumbar Stabilization Exercises with and without Respiratory Resistance on Women with Low Back Pain: A Randomized Controlled Trial. Med Sci Monit. (2020) ; 26: : e921295. |
[17] | Del Negro CA, Funk GD, Feldman JL. Breathing matters. Nat Rev Neurosci. (2018) ; 19: (6): 351-67. |
[18] | Borujeni BG, Yalfani A. Effect of respiratory muscle training session on ankle muscle activity in athletes with chronic low back pain performing overhead squats: a randomized controlled trial. Int J Evid Based Healthc. (2020) ; 18: (2): 256-64. |
[19] | Ahmadnezhad L, Yalfani A, Gholami Borujeni B. Inspiratory Muscle Training in Rehabilitation of Low Back Pain: A Randomized Controlled Trial. J Sport Rehabil. (2020) ; 29: (8): 1151-8. |
[20] | Park SJ, Kim YM, Yang SR. Effects of lumbar segmental stabilization exercise and respiratory exercise on the vital capacity in patients with chronic back pain. J Back Musculoskelet Rehabil. (2020) ; 33: (5): 841-8. |
[21] | Park SH, Lee MM. Effects of a Progressive Stabilization Exercise Program Using Respiratory Resistance for Patients with Lumbar Instability: A Randomized Controlled Trial. Med Sci Monit. (2019) ; 25: : 1740-8. |
[22] | Usman A, Tanwar T, Veqar Z. Exploring the role of respiratory intervention as an effective adjunct tool in the management of chronic low back pain: A scoping systematic review. J Bodyw Mov Ther. (2023) ; 33: : 60-8. |
[23] | Mehling WE, Hamel KA, Acree M, et al. Randomized, controlled trial of breath therapy for patients with chronic low-back pain. Altern Ther Health Med. (2005) ; 11: (4): 44-52. |
[24] | Kang JI, Jeong DK, Choi H. Effect of exhalation exercise on trunk muscle activity and oswestry disability index of patients with chronic low back pain. J Phys Ther Sci. (2016) ; 28: (6): 1738-42. |
[25] | Zhang L, Zang L. Prospective study of core strength training combined with breathing exercise in the treatment of nonspecific low back pain. The Journal of Cervicodynia and Lumbodynia. (2019) ; 40: (03): 380-2. |
[26] | Fan XY, Yan BX, Ding JY, et al. Effects of Breathing Exercise on Nonspecific Low Back Pain. Chinese Journal of Rehabilitation Theory and Practice. (2018) ; 24: (01): 93-6. |
[27] | Fei LP, Zhu J, Hou YK, et al. Effect Effect of Breathing Training on Clinical Symptoms of patients with Non-Specific Low Back Pain. China School Physical Education. (2018) ; 5: (10): 88-93. |
[28] | Yang M, Xu M, Sun ZL, et al. Respiratory training combined with postural control training can relieve lower back pain. Chinese Journal of Physical Medicine and Rehabilitation. (2020) ; 42: (12): 1081-4. |
[29] | Zhang B, Zhang N, Xu C, et al. Effect of Abnormal Breathing Pattern Training in Treatment of Chronic Nonspecific Low Back Pain in Elderly Patients. Chinese Manipulation and Rehabilitation Medicine. (2021) ; 12: (05): 5-7. |
[30] | Liu XJ, Li YZ, Hao Y, et al. Observation on the efficacy of core muscle strength training combined with respiratory training in the treatment of patients with chronic lower back pain. Chinese Journal of Physical Medicine and Rehabilitation. (2022) ; 44: (2): 160-2. |
[31] | Cohen KR. Management of Chronic Low Back Pain. JAMA Intern Med. (2022) ; 182: (2): 222-3. |
[32] | Janssens L, Pijnenburg M, Claeys K, et al. Postural strategy and back muscle oxygenation during inspiratory muscle loading. Med Sci Sports Exerc. (2013) ; 45: (7): 1355-62. |
[33] | Babina R, Mohanty PP, Pattnaik M. Effect of thoracic mobilization on respiratory parameters in chronic non-specific low back pain: A randomized controlled trial. J Back Musculoskelet Rehabil. (2016) ; 29: (3): 587-95. |
[34] | Otadi K, Ansari N, Sharify S, et al. Effects of combining diaphragm training with electrical stimulation on pain, function, and balance in athletes with chronic low back pain: a randomized clinical trial. BMC Sports Sci Med Rehabil. (2021) ; 13: (1): 20. |
[35] | Finta R, Boda K, Nagy E, et al. Does inspiration efficiency influence the stability limits of the trunk in patients with chronic low back pain? J Rehabil Med. (2020) ; 52: (3): jrm00038. |
[36] | Kolar P, Sulc J, Kyncl M, et al. Postural function of the diaphragm in persons with and without chronic low back pain. J Orthop Sports Phys Ther. (2012) ; 42: (4): 352-62. |
[37] | Finta R, Nagy E, Bender T. The effect of diaphragm training on lumbar stabilizer muscles: a new concept for improving segmental stability in the case of low back pain. J Pain Res. (2018) ; 11: : 3031-45. |
[38] | Janssens L, McConnell AK, Pijnenburg M, et al. Inspiratory muscle training affects proprioceptive use and low back pain. Med Sci Sports Exerc. (2015) ; 47: (1): 12-9. |
[39] | Ki C, Heo M, Kim HY, et al. The effects of forced breathing exercise on the lumbar stabilization in chronic low back pain patients. J Phys Ther Sci. (2016) ; 28: (12): 3380-3. |
[40] | Mohan V, Paungmali A, Sitilertpisan P, et al. The effect of core stability training with ball and balloon exercise on respiratory variables in chronic non-specific low back pain: An experimental study. J Bodyw Mov Ther. (2020) ; 24: (4): 196-202. |
[41] | Medrano-Escalada Y, Plaza-Manzano G, Fernández-de-Las-Peñas C, et al. Structural, Functional and Neurochemical Cortical Brain Changes Associated with Chronic Low Back Pain. Tomography. (2022) ; 8: (5): 2153-63. |
[42] | Janssens L, Brumagne S, Polspoel K, et al. The effect of inspiratory muscles fatigue on postural control in people with and without recurrent low back pain. Spine (Phila Pa 1976). (2010) ; 35: (10): 1088-94. |
[43] | Vicente-Campos D, Sanchez-Jorge S, Terrón-Manrique P, et al. The Main Role of Diaphragm Muscle as a Mechanism of Hypopressive Abdominal Gymnastics to Improve Non-Specific Chronic Low Back Pain: A Randomized Controlled Trial. J Clin Med. (2021) ; 10: (21): 4983. |
[44] | Vasconcelos T, Hall A, Viana R. The influence of inspiratory muscle training on lung function in female basketball players – a randomized controlled trial. Porto Biomed J. (2017) ; 2: (3): 86-9. |
[45] | Mohan V, Paungmali A, Sitilertpisan P. Altered breathing pattern valuation relatively to dyspnea assessment and treatment for low back pain: Effects of clinical practice. Musculoskelet Sci Pract. (2017) ; 27: : e1-e2. |
[46] | Marugán-Rubio D, Chicharro JL, Becerro-de-Bengoa-Vallejo R, et al. Effectiveness of Ultrasonography Visual Biofeedback of the Diaphragm in Conjunction with Inspiratory Muscle Training on Muscle Thickness, Respiratory Pressures, Pain, Disability, Quality of Life and Pulmonary Function in Athletes with Non-Specific Low Back Pain: A Randomized Clinical Trial. J Clin Med. (2022) ; 11: (15). |
[47] | Okrzymowska P, Kurzaj M, Seidel W, et al. Eight Weeks of Inspiratory Muscle Training Improves Pulmonary Function in Disabled Swimmers-A Randomized Trial. Int J Environ Res Public Health. (2019) ; 16: (10). |
[48] | Low Back Pain and Sciatica in Over 16s: Assessment and Management. London: National Institute for Health and Care Excellence (NICE), December 11, (2020) . |
[49] | Van Hoof W, O’Sullivan K, O’Keeffe M, et al. The efficacy of interventions for low back pain in nurses: A systematic review. Int J Nurs Stud. (2018) ; 77: : 222-31. |
[50] | Mohan V, Paungmali A, Sitilerpisan P, et al. Respiratory characteristics of individuals with non-specific low back pain: A cross-sectional study. Nurs Health Sci. (2018) ; 20: (2): 224-30. |
[51] | Gholami-Borujeni B, Yalfani A, Ahmadnezhad L. Eight-Week Inspiratory Muscle Training Alters Electromyography Activity of the Ankle Muscles During Overhead and Single-Leg Squats: A Randomized Controlled Trial. J Appl Biomech. (2021) ; 37: (1): 13-20. |
[52] | Farì G, Santagati D, Macchiarola D, et al. Musculoskeletal pain related to surfing practice: Which role for sports rehabilitation strategies? A cross-sectional study. J Back Musculoskelet Rehabil. (2022) ; 35: (4): 911-7. |
[53] | de Sire A, Ammendolia A, Lippi L, et al. Percutaneous Electrical Nerve Stimulation (PENS) as a Rehabilitation Approach for Reducing Mixed Chronic Pain in Patients with Musculoskeletal Disorders. Applied Sciences-Basel. (2021) ; 11: (9). |




