A preliminary exploration of attitudes, beliefs, and barriers to physical therapists’ practices in ordering diagnostic imaging
Abstract
BACKGROUND:
Diagnostic imaging (DI) studies are useful resources for examining musculoskeletal (MSK) conditions. When DI is used appropriately, it is an important tool for physical therapists (PTs).
OBJECTIVE:
The purpose of this study was to explore the attitudes, beliefs, and barriers to PTs’ practices in referring to DI in Saudi Arabia (SA).
METHODS:
For this quantitative cross-sectional study, an online self-reported questionnaire was designed and distributed. A total of 138 PTs participated in the study.
RESULTS:
Although most PTs had access to DI, few reported being able to order DI. The PTs demonstrated positive attitudes regarding their ability to refer patients for DI. Nevertheless, some PTs have adopted several beliefs and awareness of PTs regarding the clinical appropriateness of referring to DI, which may increase the unnecessary utilisation of DI requests. More than half of the PTs in this study reported that they were unfamiliar with the clinical rules used for prescribing imaging.
CONCLUSION:
This study highlights recommendations to improve PTs’ practices towards DI in SA, such as providing more DI courses targeting PTs and including clinical rules within DI education in undergraduate studies. Furthermore, a clear governmental policy is needed to permit PTs to refer to DI when specific criteria are met.
1.Introduction
Diagnostic imaging (DI), such as plain radiography (X-ray), magnetic resonance imaging (MRI), and computerised tomography (CT) scans, are essential tools for the differential diagnosis of musculoskeletal (MSK) conditions [1]. The results of DI are utilized by radiologists and other healthcare professionals; physical therapists (PTs) in particular should be able to both identify the need for DI studies and use the results of imaging in patient management [2]. Knowledge of medical imaging material enables clinicians to understand, with greater depth and precision, the extent of a specific disease or condition during a patient’s evaluation, diagnosis, prognosis, and intervention [3]. In this context, the interest of PTs in DI is rising, as reflected in the increasing focus on it in physical therapy education, scientific papers, and books [4]. The American Physical Therapy Association (APTA) has highlighted the importance of PTs having the necessary tools to properly assess patients [5]. The ability of PTs, based on patient examinations and red flags, to determine if they should be treated or referred to other healthcare professionals for appropriate tests and measures, including DI, is an important part of their clinical decision-making [6]. Understanding the use of DI studies in guiding the clinical decision-making of PTs can inform curriculum development in physical therapist education [4]. As the physical therapy profession is progressing towards more autonomy in its practice, PTs must have the necessary preparation in terms of education and training to serve as first-access providers for the best patient outcomes [7].
There is much evidence demonstrating the increasing capability of physical therapists (PTs) to provide first-access services for people with MSK conditions [8, 9, 10, 11, 12, 13]. PTs have emerged as leaders in the conservative management of MSK conditions, as they have demonstrated expertise in providing better patient-related outcomes in managing MSK disorders [8, 9, 10, 11, 13]. PTs are trained medical professionals who need to order MSK imaging to allow them to effectively function as first-access providers. In reviewing this research, it is important to point out that PTs undergo different education and training in different parts of the world and in different contexts. Thus, the corresponding results represent the potential performance of PTs in other settings (although this would necessitate structural changes and consideration of underlying factors). In one study, PTs have been shown to be similar to orthopaedic surgeons in terms of the accuracy of their imaging referrals with regard to a subset of patients who had been referred for MRIs due to musculoskeletal complaints in the spine or extremities [14]. Moreover, military PTs in the United States (US) are privileged by being permitted to refer patients directly for DI; they were trained specifically to serve in that role and subsequently demonstrated appropriate use of DI in 91% of reviewed cases [12]. Nevertheless, PTs in the US have been shown to order MSK imaging in only 11%–15% of cases, compared with 82% in physician-led cases [8]. Worldwide, there are disparities regarding the authority of PTs to order imaging. In some countries, PTs are allowed to request imaging, while others limit them based on either governmental or institutional restrictions [8]. PTs have been shown to be interested in ordering DI [15] and believe that they have a sufficient knowledge base and skills for recommending MRIs and plain radiographs [7]. However, a study by Little and Lazaro indicated that not all PTs are confident in their ability to interpret the information provided by imaging [3]. Moreover, limited knowledge about the indications for ordering DI was identified as a barrier [15].
The PT standards of care in Saudi Arabia (SA) are not clearly defined, but PTs follow various regulatory codes, such as those described by the Saudi Commission for Health Specialties (SCFHS), which grants privileges for ordering DI to only physicians [16]. Depending on the specific clinic or hospital, when MSK imaging is needed, a PT requires a referral by another healthcare professional. PTs in SA may demonstrate similar practice barriers mentioned by PTs in previous studies [3, 7, 15]. However, the practice of Saudi PTs in ordering and interpreting DI has not been previously investigated formally. Understanding PTs’ attitudes, beliefs, and knowledge regarding DI can assist with related policy considerations and the enhancement of PT education, which will promote recognition of the PT profession as improvements in regulations and education occur. To the best of our knowledge, no previous studies have explored PTs’ practices in SA. Therefore, this study aimed to explore the practices, attitudes, and beliefs of PTs in SA regarding ordering DI. Additionally, it explored barriers encountered in current practice regarding the education and regulations of PTs in SA regarding ordering DI.
2.Materials and methods
2.1Design
A quantitative cross-sectional descriptive study was performed among PTs with a bachelor’s degree or above who were practicing in SA, regardless of speciality or practice setting. A survey was conducted from February 14 to March 25, 2021 using a convenience sampling method.
2.2Participants
The study was performed among PTs with a bachelor’s degree or above who were practicing in SA, regardless of speciality or practice setting. Undergraduate PTs, those with diploma degrees, and interns were excluded. The participants were recruited through social media, flyers, and personal contacts at facilities that had practicing PTs.
2.3Questionnaire
A questionnaire was constructed to assess the practices, attitudes, beliefs, and barriers regarding DI referrals of the participating PTs. It contained 27 questions and required approximately 20–25 minutes to complete. The questions were arranged into six sections: demographics, current practice, education, attitudes, barriers, and knowledge of the usage of DI in SA.
The questionnaire was developed by the authors. Four specialists experienced in the subject area evaluated the face validity of the survey; they assessed the survey design and logic regarding the questions, display of the survey questions and answers, clarity of the content, and time to complete the survey. The survey was piloted with 10% of the sample (14 participants); no changes were deemed necessary, and these participants were therefore included in the total sample analysed and reported in this article.
The first section consisted of questions regarding demographic information: gender, nationality, age, practice licence, professional accreditation certificate, university, practice years, highest education degree, practice (settings and areas), practice role speciality in PT, and work region. The second section contained four questions about education and privileges for ordering and accessing DI studies.
The third section was composed of 10 questions about attitudes towards ordering DI studies. It was divided into two subsections: the PT’s ability to recommend DI studies and the contribution of ordering DI to enhancing the PT’s practice. All responses were recorded using a five-point Likert scale (strongly agree
The fourth section was about the beliefs of the PT towards the appropriateness of ordering DI studies. It contained seven questions asking about the safety of applying PT management without DI, the ability of DI to localise a source of pain, and the appropriateness of ordering DI for mechanical pain. All responses were recorded using the same five-point Likert scale as described in the previous section. Four questions in this section used reverse scoring. The internal consistency of the belief items was calculated as 0.73.
The fifth section assessed the barriers to ordering DI. It contained six questions assessing educational and policy barriers. All responses were recorded using the same five-point Likert scale as in the previous two sections; no reverse scoring was used for any of these questions. The internal consistency of the barrier items was calculated as 0.72.
The last section of the survey was the respondent’s awareness of clinical rules and clinical case scenarios related to DI indications; it contained eight questions. Two questions were asked regarding the knowledge and usage of clinical rules (the Canadian C-spine, Ottawa ankle, and Ottawa knee rules). The last six questions were in the form of scenarios, which were written by the authors based on the Canadian C-spine, Ottawa knee, and Ottawa ankle rules. The three rules are well known for their diagnostic accuracy in excluding fractures with regard to trauma cases [17, 18, 19]. The respondents were presented with three possible answer choices (indicated, not indicated, and not enough information to decide). The clinical case scenario questions 23, 24, and 27 indicated DI; questions 25, 26, and 28 did not indicate DI. Regarding scoring, a correct answer was assigned a score of one, while an incorrect answer received a score of zero.
The study received prior ethical approval from the Institutional Review Board (IRB) of Princess Nourah bint Abdulrahman University (IRB No. 21-0081). An informed consent form was included at the beginning of the survey, which presented the necessary information and recorded the participant’s willingness to participate in the study.
2.4Data analysis
The statistical analysis was accomplished with the SPSS software (version 24.0). The descriptive results are presented as means and standard deviations (SDs) and as percentages. The internal consistency of sections of the survey were assessed using Cronbach’s alpha. The significance (alpha) level was set at 0.05; thus,
3.Results
A total of 140 participants were recruited; two were excluded (because of a different speciality and having a diploma degree). The mean age was 31
Table 1
Demographic characteristics
| Responses ( | ||
|---|---|---|
| Frequency | Percentage | |
| Gender | ||
| Male | 70 | 51 |
| Female | 68 | 49 |
| Nationality | ||
| Saudi | 124 | 90 |
| Non-Saudi | 14 | 10 |
| Highest PT degree | ||
| Bachelor’s | 72 | 52 |
| Doctor of PT | 11 | 8 |
| Master’s | 34 | 25 |
| Doctoral | 21 | 15 |
| Current profession accreditation certificate | ||
| PT technician | 2 | 1 |
| PT | 79 | 57 |
| Senior PT | 43 | 43 |
| PT consultant specialist | 10 | 7 |
| Other | 4 | 3 |
| Years of experience | ||
| 0 to 2 | 53 | 38 |
| 3 to 5 | 23 | 17 |
| 6 to 9 | 21 | 15 |
| 10 to 15 | 20 | 14 |
| 15 to 20 | 11 | 8 |
| Over 20 | 10 | 7 |
| Work region of SA | ||
| Northern region | 9 | 7 |
| Southern region | 16 | 12 |
| Central region | 64 | 46 |
| Eastern region | 18 | 13 |
| Western region | 31 | 22 |
| PT practice area | ||
| Orthopaedics | 80 | 27 |
| Sports injuries | 54 | 18 |
| Cardiovascular and pulmonary rehabilitation | 24 | 8 |
| Neurological rehabilitation | 57 | 19 |
| Paediatric rehabilitation | 43 | 14 |
| Women’s health | 10 | 3 |
| Geriatrics | 29 | 10 |
| Other | 4 | 1 |
| PT practice setting | ||
| Sports facility | 18 | 10 |
| Governmental hospital | 54 | 29 |
| Private hospital or clinic | 42 | 23 |
| University/education facility | 33 | 18 |
| Rehabilitation centre | 28 | 15 |
| Research facility | 4 | 2 |
| Other | 6 | 3 |
| PT practice role | ||
| Administration/management | 42 | 23 |
| Academic (PT related) | 35 | 18 |
| Research | 18 | 10 |
| Direct patient care | 81 | 45 |
| Other | 3 | 2 |
| Method of education you used to learn about DI | ||
| No previous education | 10 | 4 |
| Academic PT program (undergrad PT education) | 90 | 40 |
| Academic PT postgrad (postgraduate PT education) | 37 | 16 |
| Continuing education courses/workshop | 39 | 17 |
| Self-study | 51 | 22 |
Figure 1.
Percentage of PTs for referral, accessibility, and recommendation (
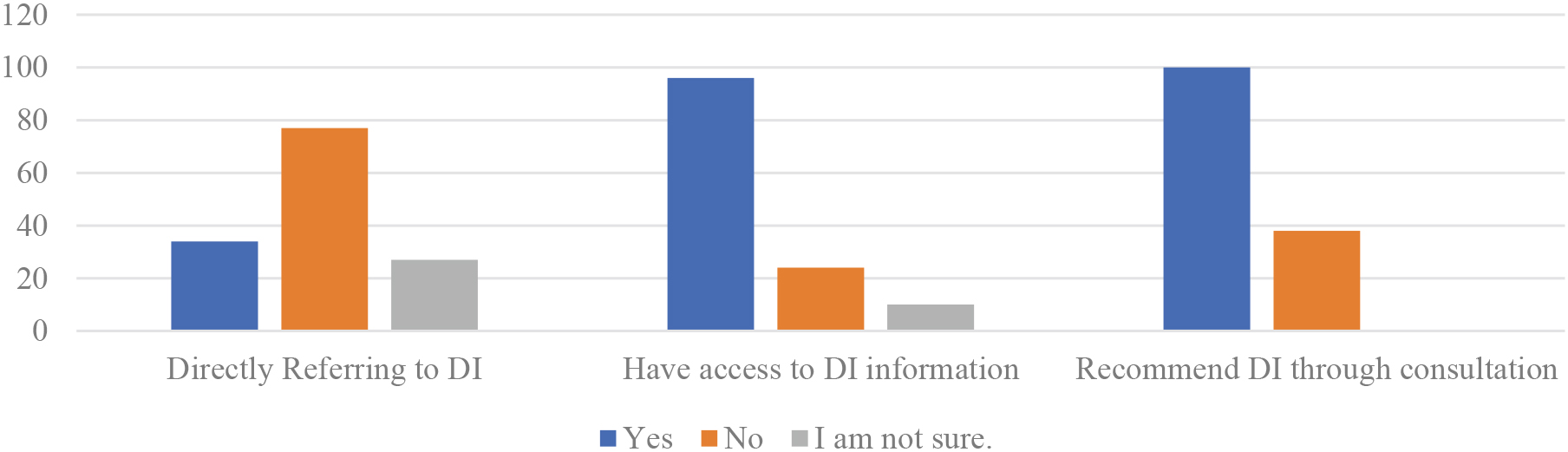
Figure 2.
Attitudes of PTs towards their ability to recommend and order DI studies (
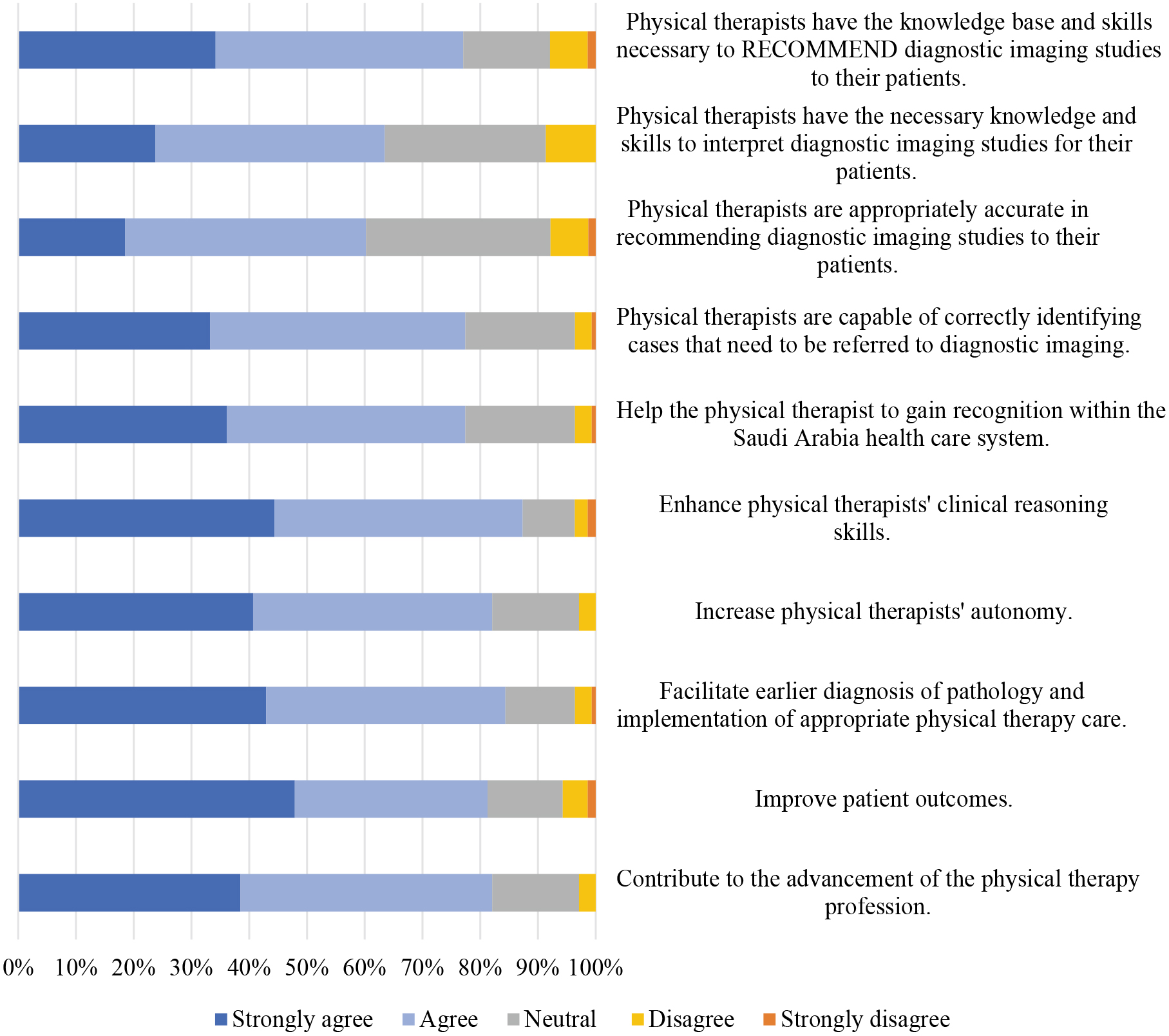
3.1Attitudes towards DI studies
In our study, the Cronbach’s alpha measure of internal consistency for the attitude section of the survey was 0.86. The results showed that 76.9% of the participants believed that PTs have the knowledge base and skills necessary to recommend DI studies for their patients. Similarly, 77.5% believed that PTs can correctly identify cases that need to be referred for DI (Fig. 2). Regarding their attitudes towards the contribution of ordering DI to the advancement of the PT profession, the survey results revealed that 77.8% agreed that ordering DI would help PTs gain recognition within the SA healthcare system. Furthermore, 87% of the participants thought that the use of DI enhanced the clinical reasoning skills of PTs. In addition, 81.9% agreed that DI would increase the autonomy of PTs (see Fig. 2).
Table 2
Responses to the familiarity and utilisation of clinical rules for ordering DI
| Responses as percentages and counts (in parentheses) ( | ||||||
| Canadian C-spine rule | NEXUS C-spine rule | Ottawa ankle rule | Ottawa knee rule | None | Other | |
| Rule familiarity | 26.8% (37) | 14.4% (20) | 26.8% (37) | 21% (29) | 55.1% (76) | 0.7% (1) |
| Rule utilisation | 19.6% (27) | 8.7% (12) | 16% (22) | 16% (22) | 60.9% (84) | 1.4% (2) |
Figure 3.
Beliefs of PTs regarding the appropriateness of ordering DI for patient care (
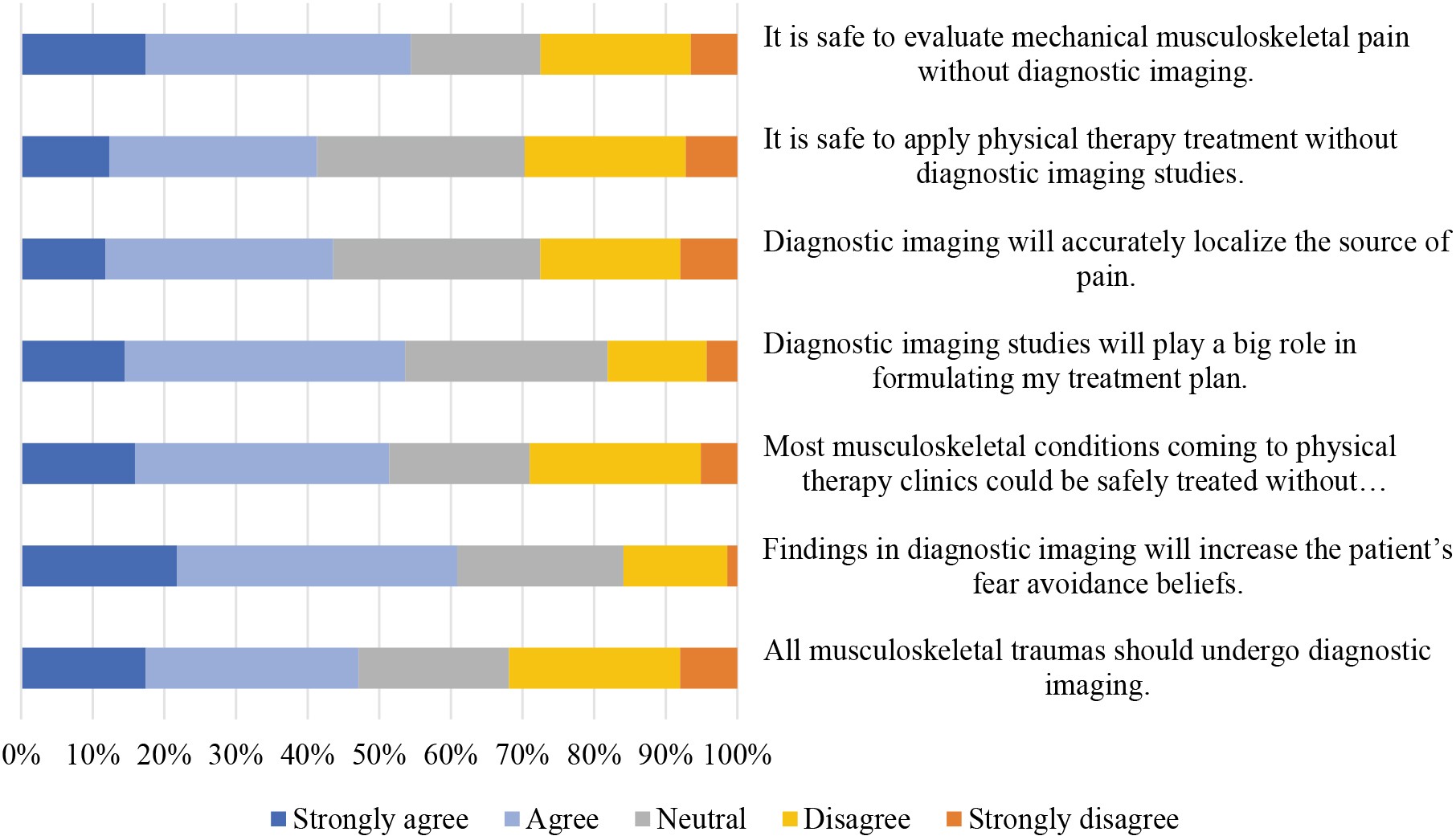
3.2Beliefs and awareness of PTs regarding the clinical appropriateness of ordering DI
In our study, the Cronbach’s alpha measure of internal consistency for the beliefs section of the survey was 0.72. The beliefs of PTs regarding the clinical appropriateness of ordering DI for patient care are shown in Fig. 3. Of the participants surveyed, 54.4% believed that it was safe to evaluate mechanical MSK pain without DI. However, 47.1% agreed with the statement that all MSK traumas should undergo DI. In addition, 53.6% of the participants agreed that DI studies play a significant role in formulating a treatment plan, and 60.8% agreed that DI findings increase a patient’s fear avoidance beliefs.
Further exploration of the familiarity of PTs with the clinical rules to prescribe imaging are summarised in Table 2. The results indicated that between 55.1% and 60.9% of PTs were unfamiliar or had never used the presented clinical rules. The Canadian C-spine rule and the Ottawa ankle rule were the most recognised clinical rules. The most utilised clinical rule was the Canadian C-spine rule, as reported by 19.6% of the PTs, and the Ottawa ankle and knee rules were tied in second, as reported by 16.0% of the respondents. The NEXUS C-spine rule came last on our list, as reported by 8.7% of the respondents. In the clinical case scenarios, 60% of the participants chose the correct answer in both Ottawa knee rule case scenarios. Moreover, 77% correctly identified the answer for the Ottawa ankle rule case scenario. Also, based on the cervical clinical rules for the fifth case, 83% of the participants chose imaging, which was the correct answer (see Table 3).
Table 3
Responses to the need to refer to a DI based on clinical scenarios
| Responses as percentages and counts (in parentheses) ( | ||||
|---|---|---|---|---|
| Clinical rule | Case scenario | Correct identification | Incorrect identification | Unable to decide |
| Ottawa knee | An adult patient with a history of uninvestigated trauma of the knee with intermittent locking unrelieved by four weeks of conservative care. (Indicated) | 60% (83) | 10% (14) | 30% (41) |
| A 36 y/o patient with knee pain and limping after falling while playing soccer, no swelling or tenderness around patella. He can flex his knee actively | 60% (83) | 30% (22) | 18% (25) | |
| Ottawa ankle | An adult female has fallen while descending from the stairs with twisting mechanism on the Rt ankle. She has tenderness in the distal fibula along the posterior edge of the lateral malleolus (distal 6 cm). She has tenderness at the base of the fifth metatarsal. (Indicated) | 77% (106) | 14% (20) | 9% (12) |
| An adult obese patient with pain in the sole of the Rt foot. The pain increases at the start of the morning and with prolonged standing and walking. Decreased ankle dorsiflexion | 60% (83) | 26% (36) | 14% (19) | |
| Cervical spine | A 68 y/o male patient fell down six stairs. He experienced an immediate pain in his neck radiating to his left forearm, with intermittent tingling in his left thumb. Neck rotation was painfully limited to 35 | 83% (114) | 12% (16) | 6% (8) |
| A 40 y/o male underwent a simple rear-end car accident with delayed onset of neck pain. There is no tenderness in the midline of the C-spine. Neck rotation was painfully limited to 50 | 41% (56) | 45% (62) | 14% (20) | |
Note. Table 3 describes the scenarios based on specific clinical rules.
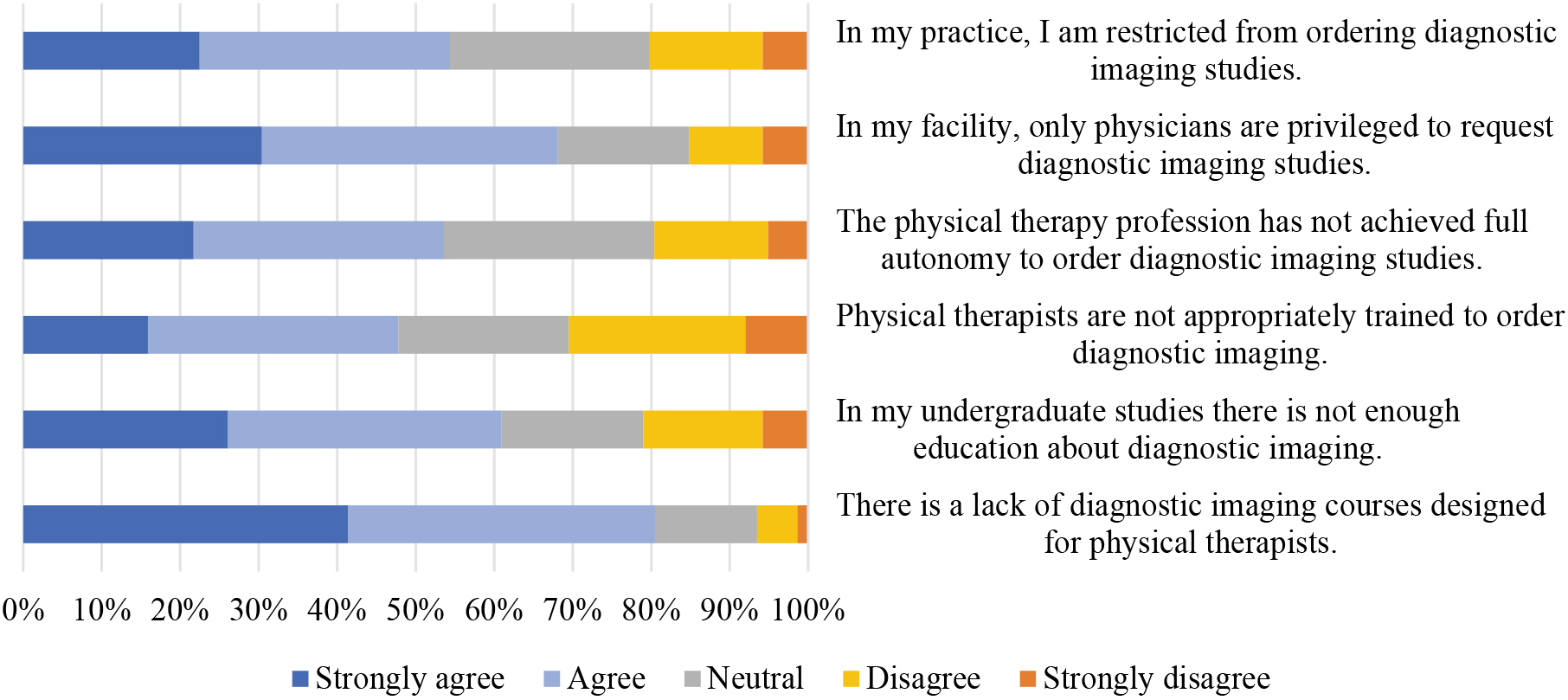
3.3Barriers in practice towards DI studies
In our study, the Cronbach’s alpha measure of internal consistency for the barriers section of the survey was 0.86. The barriers in PTs’ practice towards DI studies are shown in Fig. 4. Approximately 54.4% of the participants reported being restricted from ordering DI studies. Additionally, 53.6% of the participants believed that the PT profession had not achieved full autonomy to order DI studies. Likewise, 80.4% of the participants agreed that there was a lack of DI courses designed for PTs.
Figure 4.
Barriers towards DI from policies, practice autonomy, and education as reported by the PTs (
4.Discussion
This study explored the attitudes of PTs about their ability to recommend DI studies and DI’s contribution to their profession, the barriers in PTs’ practice across SA in ordering DI, the beliefs of PTs towards the necessity of ordering DI for patient care, and PTs’ awareness of clinical appropriateness when ordering DI. This study found that the PTs were mostly restricted from directly referring patients for DI. Additionally, the PTs demonstrated positive attitudes regarding their ability to refer patients for DI, and they perceived that the privilege to refer for DI would enhance the profession. However, the PTs in this study reported several barriers related to policies and education. More than half of the PTs in this study reported that they were unfamiliar with the clinical rules used to prescribe imaging. Nevertheless, some PTs had several beliefs that may increase the unnecessary utilisation of DI requests.
In this study, 76% of PTs reported that they were restricted from ordering DI directly. This finding is in accordance with other studies that have indicated similar restrictions worldwide. For example, this has been reported in Canada [15], Austria, Belgium, the Czech Republic, France, Germany, Japan, Hong Kong, Jordan, Malaysia, the Philippines, Romania, and the United Arab Emirates [8], based on either governmental or institutional restrictions. Likewise, Rundell et al. [7] stated that it was common for a therapist to recommend imaging, although many did not have the direct authority to request the imaging themselves. No data are readily available on how often these recommendations are followed.
Approximately 76.9% of participants perceived themselves to have the necessary skills for appropriately referring patients for imaging, as well as for interpreting DI. In addition, 87% of participants perceived that ordering DI would enhance their clinical reasoning skills. These findings are similar to the study of Rundell et al. [7], which found that PTs in the US believed that they had a sufficient knowledge base and skills to order DI. This study highlighted the high desire of PTs to have more autonomy in ordering DI, which was shown by the PTs’ positive attitudes towards their ability to refer patients for DI. In addition, 53.6% of the participants agreed that DI studies play a significant role in formulating treatment plans. Nevertheless, some exhibited several beliefs regarding the necessity of DI, which may lead to an unnecessary increase in DI requests. For example, 41% of the participants believed that imaging would accurately localise a source of pain. Such beliefs may highlight a tendency towards an overutilisation of DI, even with clinical guidelines that advise against it [20]. In addition, 47.1% of the participants agreed with the statement that all MSK traumas should undergo DI. However, patients are not likely to need an initial DI if there is insufficient trauma to cause fractures or dislocations or present red flags. This may highlight the lack of PTs’ understanding of when to order DI. It is important to remember that this study explored the beliefs of PTs who currently are restricted from directly ordering DI; in other words, it is not a current part of their responsibilities, and many have not received training in this area or have pursued self-study on their own. Therefore, further research on this aspect is required.
Although the participants in this study had positive attitudes towards their ability to request imaging, they identified barriers to the practice of PTs utilising DI. These barriers were related to policies and practice autonomy, in addition to a lack of DI undergraduate education and professional training specially designed for PTs. These identified barriers agree with the results of Bussières et al. [21], who indicated that a lack of certain standards and educational guidelines for imaging might be the biggest barrier facing the emerging PT field [21]. This might be due to the variety of DI courses in undergraduate studies among Saudi universities, as there is a lack of a unified guideline for the PT undergraduate curriculum. Bindawas [22] indicated the radiology is one of the areas that has to be emphasised in entry-level physical therapy programs [22]. Even though imaging is included in the Saudi curricula [16], inconsistencies in the content of DI instruction and the method of assessing and integrating educational material can influence students’ competencies. Additionally, 80% of the participants agreed that there was a lack of professional DI courses designed for PTs. This current finding agrees with the results of a study by Boyles et al. [5] that suggested the implementation of a direct-access model that includes a DI training pre-requisite to allow imaging privileges.
Understanding the current DI standards and recommendations for certain conditions will help facilitate the proper decision-making that PTs need [1]. In this study, most of the participants had an academic undergraduate education accompanied by self-study of DI. This study did not further explore the methods used for self-study or their extent. It would be safe to say that the range and depth of knowledge the PTs acquired on their own regarding DI likely varied dramatically as indicated by the responses to other questions. For example, about 60% of the participants in this study reported that they were not aware of the international imaging rules (the Ottawa knee and ankle, Canadian C-spine, and NEXUS C-spine rules). The clinical scenarios used in this study were designed by the authors to merely explore the clinical awareness of participants to international imaging rules. They would not be considered valid as measures or indicators of the PTs’ specific knowledge regarding DI to a greater extent. With this limitation in mind, according to the responses of the participants to the given clinical scenarios for each rule, between 60% and 80% of the PTs in this study showed an awareness of the correct indication of when to order DI for each scenario. However, appropriate care should be taken in disseminating these findings in that regard. Knowledge of the imaging rules could be an important part of a standardised curriculum for PTs regarding DI. More formal instruction on DI would be desirable for PTs in SA. However, they do not need the same in-depth education on the subject or attempt to replace the roles of radiologists, doctors, and other healthcare professionals in this area.
The limitations of this study are primarily those inherent in questionnaire-based, descriptive research. Survey respondents are susceptible to bias, and the responses may not accurately represent real practice. In addition, the sample collected and the method for contacting them were not sufficient to generalise the results to the entire population of PTs in SA. Moreover, this study included all PT specialties with different educational degrees and experiences in the stated population without assessing the effect of these differences on their practice towards DI. However, as no prior research has been done in this area with PTs in SA; the data collected can spur additional research and discussions about this topic by interested parties.
5.Conclusion
PTs in SA reported that they were mostly restricted from directly referring patients for DI. The PTs in this study demonstrated positive attitudes regarding their ability to refer patients for DI. Nevertheless, some PTs have adopted several beliefs and awareness of PTs regarding the clinical appropriateness of ordering DI, which may increase unnecessary utilisation of DI requests. Additionally, PTs in SA identified limited education and a lack of authority to prescribe DI as barriers to practice.
The findings in this study highlight the importance of some recommendations to improve PTs’ practices towards DI in SA. These are related to education, such as providing more DI courses targeting PTs and including clinical rules within DI education in undergraduate studies. Further studies are needed to determine if PTs in SA possess enough knowledge regarding DI in general, and knowledge of international imaging rules through more extensive assessment methods with established reliability and validity procedures. Future studies should include a larger representative sample to measure the abilities and practices of PTs in SA when ordering DI.
Funding
The authors report no funding.
Informed consent
An informed consent form was included at the beginning of the survey, which presented the necessary information and recorded the participant’s willingness to participate in the study.
Author contributions
All named authors have made an active contribution to the conception and design, analysis, interpretation of the data, drafting of the paper and have critically reviewed its content. All authors read and approved the final version submitted for publication.
Acknowledgments
The authors acknowledge the support provided through the Princess Nourah Bint Abdulrahman University Researchers Supporting Project (No. PNURSP2023R285), Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia.
Conflict of interest
The authors declare that they have no conflicts of interest.
References
[1] | Deyle GD. Musculoskeletal imaging in physical therapist practice. J Orthop Sports Phys Ther. (2005) ; 35: (11): 708-21. doi: 10.2519/jospt.2005.35.11.708. |
[2] | American Physical Therapy Association. A normative model of physical therapist professional education. Alexandria, VA: Coalition for Consensus, APTA Education Division. (2004) . |
[3] | Little T, Lazaro R. Physiotherapists’ perceptions and use of medical imaging information in practice. Physiother Res Int. (2006) ; 11: (1): 14-23. doi: 10.1002/pri.37. |
[4] | Agustsson H. Diagnostic musculoskeletal imaging: How physical therapists utilize imaging in clinical decision-making [Doctoral dissertation]. Nova Southeastern University. (2018) . Available from: https://nsuworks.nova.edu/hpd_pt_stuetd/72. |
[5] | American Physical Therapy Association. Vision statement for the physical therapy profession. (2019) . Available from: https://www.apta.org/apta-and-you/leadership-and-governance/policies/vision-statement-for-the-physical-therapy-profession. |
[6] | McKinnis L. Radiologic evaluation, search patterns, and diagnosis. In: McKinnis L, editor. Fundamentals of musculoskeletal imaging. 4th ed. Philadelphia, PA: FA Davis. (2014) . pp. 39-75. |
[7] | Rundell S, Maitland M, Manske R, Beneck G. Survey of physical therapists’ attitudes, knowledge, and behaviors regarding diagnostic imaging. Phys Ther. (2020) ; 101: (1): 4-14. doi: 10.1093/ptj/pzaa187. |
[8] | Mabry LM, Boyles RE, Brismée J, Agustsson H, Smoliga JM. Physical therapy musculoskeletal imaging authority: A survey of the World Confederation for Physical Therapy Nations. Physiother Res Int. (2019) ; 25: (2): 1-4. doi: 10.1002/pri.1822. |
[9] | Boyles RE, Gorman I, Pinto D, Ross MD. Physical therapist practice and the role of diagnostic imaging. J Orthop Sports Phys Ther. (2011) ; 41: (11): 829-37. doi: 10.2519/jospt.2011.3556. |
[10] | Ross MD, Childs JD, Middel C, Kujawa J, Brown D, Corrigan M, et al. Physical therapist vs. family practitioner knowledge of simple low back pain management in the U.S. Air Force. Mil Med. (2014) ; 179: (2): 162-68. doi: 10.7205/MILMED-D-13-00099. |
[11] | Demont A, Bourmaud A, Kechichian A, Desmeules F. The impact of direct access physiotherapy compared to primary care physician led usual care for patients with musculoskeletal disorders: A systematic review of the literature. Disabil Rehabil. (2021) ; 43: (12): 1-12. doi: 10.1080/09638288.2019.1674388. |
[12] | Keil AP, Baranyi B, Mehta S, Maurer A. Ordering of diagnostic imaging by physical therapists: A 5-year retrospective practice analysis. Phys Ther. (2019) ; 99: (8): 1020-26. doi: 10.1093/ptj/pzz015. |
[13] | Crowell MS, Dedekam EA, Johnson MR, Dembowski SC, Westrick RB, Goss DL. Diagnostic imaging in a direct-access sports physical therapy clinic: A 2-year retrospective practice analysis. Int J Sports Phys Ther. (2016) ; 11: (5): 708-17. |
[14] | Moore JH, Goss DL, Baxter RE, DeBerardino TM, Mansfield LT, Fellows DW, et al. Clinical diagnostic accuracy and magnetic resonance imaging of patients referred by physical therapists, orthopaedic surgeons, and nonorthopaedic providers. J Orthop Sports Phys Ther. (2005) ; 35: (2): 67-71. doi: 10.2519/jospt.2005.35.2.67. |
[15] | Chong JN, De Luca K, Goldan S, Imam A, Li B, Zabjek K, et al. Ordering diagnostic imaging: A survey of Ontario physiotherapists’ opinions on an expanded scope of practice. Physiother Can. (2015) ; 67: (2): 144-56. doi: 10.3138/ptc.2014-09. |
[16] | Alghadir A, Zafar H, Iqbal ZA, Anwer S. Physical therapy education in Saudi Arabia. J Phys Ther Sci. (2015) ; 27: (5): 1621-23. doi: 10.1589/jpts.27.1621. |
[17] | Michaleff ZA, et al. Accuracy of the Canadian C-spine rule and NEXUS to screen for clinically important cervical spine injury in patients following blunt trauma: A systematic review. CMAJ. (2012) ; 184: (16): E867-76. doi: 10.1503/cmaj.120675. |
[18] | Yao K, Haque T. The Ottawa knee rules: A useful clinical decision tool. Australian Family Physician. (2012) ; 41: (4): 223-224. Available from: doi: 10.3316/informit.157959939560771. |
[19] | Bachmann LM, et al. Accuracy of Ottawa ankle rules to exclude fractures of the ankle and mid-foot: Systematic review. British Medical Journal. (2003) ; 326: (7386): 417-419. |
[20] | Sharma S, Traeger A, Reed B, Hamilton M, O’Connor D, Hoffmann T, et al. Clinician and patient beliefs about diagnostic imaging for low back pain: A systematic qualitative evidence synthesis. BMJ Open. (2020) ; 10: (8): e037820. doi: 10.1136/bmjopen-2020-037820. |
[21] | Bussières AE, Peterson C, Taylor JA. Diagnostic imaging guideline for musculoskeletal complaints in adults – an evidence-based approach – Part 2: Upper extremity disorders. J Manipulative Physiol Ther. (2008) ; 31: (1): 2-32. doi: 10.1016/j.jmpt.2007.11.002. |
[22] | Bindawas SM. Physical therapy entry-level education and post-professional training in Saudi Arabia: A comparison of perceptions of physical therapists from five regions. J. Phys. Ther. Sci. (2014) ; 26: : 1377-1382. |




