The 50 most-cited articles on temporomandibular disorders: A bibliometric analysis
Abstract
BACKGROUND:
Temporomandibular disorders (TMD) are musculoskeletal conditions involving masticatory muscles and temporomandibular joints. Bibliometric analysis has been introduced as a new method for collecting and analyzing information on scientific articles.
OBJECTIVE:
The aim of this study was to identify the 50 most cited articles on TMD, performing a bibliometric analysis of the identified papers to favor research and clinical practice.
METHODS:
On December 17, 2021 a systematic research was performed to find all papers on TMD published in the literature. The Incites Journal Citation Reports dataset and Scopus database was used to obtain bibliometric indexes of the authors and metrics data of the journals, including Impact Factor, Eigenfactor Score, and Normalized Eigenfactor. VOSviewer was used to visualize the keyword mapping networking, with the nodes standing for keywords and the edges for keyword relationships.
RESULTS:
Out of 24372 papers obtained by the search strategy, the 50 most cited articles on TMD were analyzed. The paper with the highest number of citations (
CONCLUSION:
This bibliometric study showed an increasing number of citations for articles on TMD, testifying a high interest in the last years. Starting from this analysis, future studies might provide high-quality evidence on TMD management.
1.Introduction
Temporomandibular disorders (TMD) are defined as a set of musculoskeletal and neuromuscular conditions involving masticatory muscles, temporomandibular joints (TMJ), and associated structures [1]. The Research Diagnostic Criteria for TMD (RDC/TMD) introduced by Dworkin and LeResche in 1992 [2] have been considered the most widely used diagnostic tools during the last two decades. In 2014, the Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) [3] were developed from RDC/TMD and have been shown to provide excellent reliability and validity [4, 5]. DC/TMD have two assessment components. Axis I allows to classify TMD into three groups: Group I, muscular disorders (Ia myofascial pain; Ib myofascial pain with mouth opening limitation); Group II, disc displacement (IIa disc displacement with reduction, IIb disc displacement without reduction with limited opening, IIc disc displacement without reduction without limited opening); and Group III arthralgia (IIIa), arthritis (IIIb), and arthrosis (IIIc) [3]. Axis II evaluates the pain-related disability, relevant behavioral, psychological status, and psychosocial functioning (e.g., anxiety and depression and somatization) [3]. TMD had a multifactorial etiology with several risk factors recently identified, including parafunctional habits (e.g., bruxism grinding and clenching), clenching of teeth, grinding, anatomical factors, trauma or hypermobility of the joints, cervical posture, and psychosocial issues, (e.g., anxiety and depressive syndrome) [6, 7, 8, 9, 10, 11, 12, 13]. In light of the several etiological causes, diagnosis of TMD is still challenging and clinical examination should play a pivotal role, while imaging assessment should be reserved for selected cases [14].
More specifically, studies on TMD patients [15, 16] reported an overall prevalence of 45.3% for group I muscle disorder diagnoses, 41.1% for group II disc displacements, and 30.1% for group III joint disorders, whereas studies on general populations reported an overall 9.7% prevalence for group I, 11.4% for group IIa, and 2.6% for group IIIa. TMD affects primarily young and middle-aged adults, rather than children or the elderly, and according to The Orofacial Pain: Prospective Evaluation and Risk Assessment (OPPERA) study, only the chronic form of TMD predominantly affected women, whereas the acute form had equal prevalence between the sexes [17, 18].
Pain is the most common clinical manifestation of TMD, followed by irregular and limited jaw motion, that could lead to discomfort or difficulty in performing daily activities such as chewing, talking, swallowing, yawning, with a significantly reduced health-related quality of life (HRQoL) [19, 20]. TMD could cause limitations in basic activities of daily living (ADLs) and have severe family and socio-occupational repercussions owing to its effects on mental wellbeing, HRQoL, and limiting workplace performance [21].
Thus, the management goals in TMD are to decrease joint pain, swelling, and reflex masticatory muscle spasm/pain, to increase joint function, and prevent further joint damage [22]. The main treatments for pain relief in TMD could include occlusal splints, extracorporeal shock wave therapy, laser therapy, transcutaneous electrical nerve stimulation, rehabilitation exercises, and oxygen-ozone therapy [23, 24, 25, 26, 27].
In recent years, bibliometric analysis has been introduced as a new method for retrieving, collecting, and analyzing any measurable information about published scientific articles [28]. Bibliometric analysis is an emerging research design highlighting the most common topics the researchers focused on, filling the gap of knowledge about current trends in literature, and emphasizing the most expanding novelty in a specific field [28].
Citations are the most common way to quantify the impact and, in some cases, the quality of a publication in a particular field; they also reveal a link between authors, groups of researchers, study topics, or countries [28]. More specifically, bibliometric analysis could provide a metric in the larger examination of overall quality and remains a useful tool to assess the scientific journals, although self-citation could bias the number of times an article is cited [29, 30, 31]. Furthermore, the establishment of a citation ranking list identifies published works that can potentially influence trends in clinical practice and future research [32]. In addition, the use of visualized analyses to map bibliometric networks, often referred to as science mapping, can provide an intuitive yet comprehensive overview of a large dataset [33].
Bibliometric analysis has been widely used in several fields of rehabilitation and dentistry [34, 35, 36, 37, 38], but to the best of our knowledge, there is a lack of bibliometric studies on the TMD in the scientific literature. Therefore this study aimed to perform a bibliometric analysis of the 50 most cited papers on TMD to obtain a representation, which will favor future clinical studies to uncover gaps in the existing evidence.
2.Materials and methods
The study was designed to answer the following research question: “What are the most cited articles on temporomandibular joint disorders?”
On December 17, 2021 three authors independently conducted a computerized database search to find all published papers about TMD. The Scopus database was used to identify all potentially relevant studies regardless of the year, type of publication, or language because of its ability to provide a systematic citation search across multiple repositories.
The following search query was adopted for the search: (“temporomandibular” OR “temporomandibular joint” OR “TMJ”) AND (disorder* OR disease*). Titles and abstracts were independently screened by two authors to assess the eligibility of the studies. Any disagreement was resolved through discussion or, if necessary, consultation with a third reviewer. The articles not directly relevant to TMD and those written in a language different than English were excluded.
Then, two reviewers independently collected data from the included studies using a customized data extraction on a Microsoft Excel sheet, entering the full records of the retrieved publications [39, 40, 41].
The articles were listed among the remaining texts, which were sorted in descending order based on their total number of citations. In accordance with previous studies, the first 50 manuscripts were considered in the present bibliometric analysis.
2.1Bibliometric analysis
Data extracted for each article, by two researchers were three sets of parameters: (1) article-based parameters (title, authors, journal, publication year, study design, total citations); (2) journal-based parameters (2020 Journal Impact Factor – JIF – (if available), quartile of the Category “Dentistry, Oral Surgery & Medicine” (if available), Eigenfactor Score, Normalized Eigenfactor, Article influence score, 5-year Journal Impact Factor (5-JIF), Immediacy Index, number of manuscripts among the 50 most cited articles on TMD, citations of the papers among the 50 most cited articles on TMD); and (3) author-based parameters (name, affiliation, country, h-index, number of articles and position in the 50 most cited articles on TMD, citations of the papers included in the 50 most cited articles on TMD).
All these metrics were identified using two databases: Incites Journal Citation Reports and Scopus. The latter was used to obtain information on the author’s affiliations, country of origin, and h-index. To produce normalized data, the most productive universities were identified using author-level fractional counting, in which the total citations and number of publications in the top 50 were evenly distributed among the number of their authors.
2.2Visualized analysis
Based on bibliographic data, keywords were automatically extracted from the dataset and used to build a co-occurrence network. Full counting was used to count keywords, which meant that each co-occurrence link had the same weight. Two authors manually inspected and revised all terms to create a custom thesaurus to avoid redundancy. The requested minimum number of keyword occurrences was set to 4 to include keywords in the analysis dataset. As a result, each keyword was tabled alongside its occurrences and total link strength. Keyword mapping was performed through the VOSviewer. The generated networks are made up of nodes standing for keywords, while keyword relationships were represented by edges.
To visualize the network, a distance-based approach was chosen; the distance between two nodes would roughly indicate the nodes’ relatedness. Keywords that were similar were grouped together in clusters. The level of detail in the clustering process is determined by the cluster resolution. The higher the value, the more keyword subgroups will be created. Small clusters were merged into larger clusters when the cluster resolution was set to 1.0.
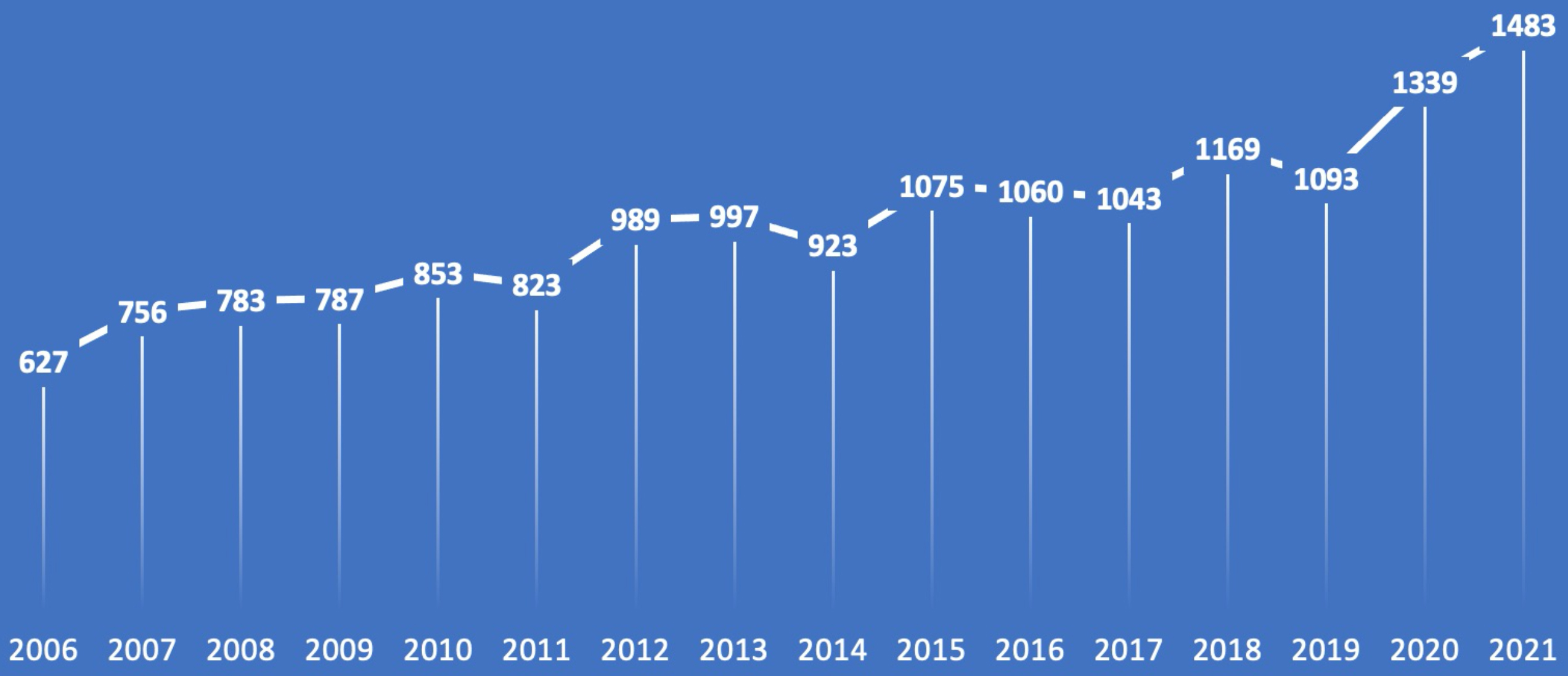
Figure 1.
The total number of citations per year (2006–2021).
3.Results
Out of 24372 papers obtained by the search strategy, the list of the top 50 most cited articles [2, 9, 16, 17, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83, 84, 85, 86, 87] was created according to the Scopus database. No studies were excluded due to language restrictions. The oldest article selected was published in 1971 and the most recent one in 2014. The 50 most cited articles are described in Table 1 and listed in descending order according to the total number of citations received. The highest number of citations received by the most cited paper [2] was 3020, whereas the lowest number of citations collected by the 50
As shown in Fig. 1, the rate of citations per year collected by the 50 most cited articles on TMD has been increasing over time (from 627 citations in 2006 to 1483 citations in 2021).
The most cited paper on TMD was published by Dworkin & LeResche on the Journal of Craniomandibular Disorders in 1992, with the title “Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique” [2], collecting 3020 citations. It is followed by another article by Dworkin et al. published in the same year 1992 entitled “Grading the severity of chronic pain”, that collected 2052 citations. Concerning the study design, it was noted that most papers were cross-sectional studies (
Concerning the study objective of the 50 most cited papers on TMD, diagnosis was assessed in 9 studies [2, 16, 42, 43, 47, 48, 52, 56, 81], prevalence in 16 studies [16, 17, 44, 45, 50, 52, 72, 77, 78, 79, 81, 82, 83, 84, 85, 87], pathophysiology in 8 studies [53, 54, 68, 69, 73, 74, 76, 86], etiology in 5 studies [47, 51, 52, 55, 63], risk factors in 14 studies [9, 17, 44, 51, 55, 57, 59, 60, 61, 62, 64, 65, 67, 70], clinical presentation in 7 studies [45, 46, 52, 53, 54, 59, 69], and treatment in 8 studies [47, 49, 52, 58, 66, 75, 80, 84]. Further details are depicted in Table 1.
The 50 most cited papers on TMD were published in 20 different scientific Journals, as shown by Table 2. The scientific Journal with the highest number of citations (
Out of 142 authors contributing to the 50 most cited articles on TMD, the main characteristics of the 10 authors with the highest number of citations are analyzed in Table 3. More specifically, their h-index ranged from 27 to 123 (mean: 56.4
Table 1
The 50 most cited articles on temporomandibular disorders
| Ranking | Title | Authors | Journal | Year of publication | Study design | Citations | Study objective |
|---|---|---|---|---|---|---|---|
| 1 | Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique [2] | Dworkin SF LeResche LA | Journal of Craniomandibular Disorders | 1992 | Guidelines | 3020 | Diagnosis |
| 2 | Grading the severity of chronic pain [42] | Von Korff M Ormel J Keefe FJ Dworkin SF | Pain | 1992 | Prospective study | 2052 | Diagnosis |
| 3 | Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for clinical and research applications: Recommendations of the international RDC/TMD consortium network and orofacial pain special interest group [43] | Schiffman E Ohrbach R Truelove E Look J Anderson G Goulet JP List T Svensson P Gonzalez Y Lobbezoo F Michelotti A Brooks SL Ceusters W Drangsholt M Ettlin D Gaul C Goldberg LJ Haythornthwaite JA Hollender L Jensen R John MT De Laat A de Leeuw R Maixner W van der Meulen M Murray GM Nixdorf DR Palla S Petersson A Pionchon P Smith B Visscher CM Zakrzewska J Dworkin SF | Journal of Oral and Facial Pain and Headache | 2014 | Guidelines | 1447 | Diagnosis |
| 4 | Epidemiology of temporomandibular disorders: Implications for the investigation of etiologic factors [17] | LeResche LA | Critical Reviews in Oral Biology and Medicine | 1997 | Narrative review | 650 | Prevalence, risk factors |
|
Table 1, continued | |||||||
|---|---|---|---|---|---|---|---|
| Ranking | Title | Authors | Journal | Year of publication | Study design | Citations | Study objective |
| 5 | Epidemiology of signs and symptoms in temporomandibular disorders: clinical signs in cases and controls [44] | Dworkin SF Huggins KH LeResche L Von Korff M Howard J Truelove E Sommers E | Journal of the American Dental Association | 1990 | Cross-sectional study | 643 | Prevalence, risk factors |
| 6 | Overlapping conditions among patients with chronic fatigue syndrome, fibromyalgia, and temporomandibular disorder [45] | Aaron LA Burke MM Buchwald D | Archives of Internal Medicine | 2000 | Cross-sectional study | 455 | Prevalence, clinical presentation |
| 7 | Internal Derangements of the Temporomandibular Joint: Pathological Variations [46] | Wilkes CH | Archives of Otolaryngology-Head and Neck Surgery | 1989 | 407 | Clinical presentation | |
| 8 | Degenerative disorders of the Temporomandibular joint: etiology, diagnosis, and treatment [47] | Tanaka E Detamore MS Mercuri LG | Journal of Dental Research | 2008 | Narrative review | 403 | Etiology, diagnosis, treatment |
| 9 | Research diagnostic criteria for temporomandibular disorders (RDC/TMD): development of image analysis criteria and examiner reliability for image analysis [48] | Ahmad M Hollender L Anderson Q Kartha K Ohrbach R Truelove E John MT Schiffman EL | Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontology | 2009 | Cross-sectional study | 372 | Diagnosis |
| 10 | Temporomandibular joint arthrocentesis: A simplified treatment for severe, limited mouth opening [49] | Nitzan DW Dolwick MF Martinez GA | Journal of Oral and Maxillofacial Surgery | 1991 | Prospective study | 352 | Treatment |
| 11 | Gender Differences in Pain [50] | Dao TT LeResche L | Journal of Orofacial Pain | 2000 | Narrative review | 351 | Prevalence |
| 12 | The temporomandibular joint: A morphologic study on a human autopsy material [51] | Oberg T Carlsson GE Fajers CM | Acta Odontologica Scandinavica | 1971 | Cross-sectional study | 333 | Etiology, risk factors |
| 13 | Temporomandibular disorders [52] | Scrivani SJ Keith DA Kaban LB | New England Journal of Medicine | 2008 | Narrative review | 332 | Prevalence, etiology, diagnosis, clinical presentation, treatment |
| 14 | Research diagnostic criteria for temporomandibular disorders: A systematic review of axis I epidemiologic findings [16] | Manfredini D Guarda-Nardini L Winocur E Piccotti F Ahlberg J Lobbezoo F | Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontology | 2011 | Systematic review | 346 | Prevalence, diagnosis |
|
Table 1, continued | |||||||
|---|---|---|---|---|---|---|---|
| Ranking | Title | Authors | Journal | Year of publication | Study design | Citations | Study objective |
| 15 | Sensitivity of patients with painful temporomandibular disorders to experimentally evoked pain [53] | Maixner W Fillingim RB Booker D Sigurdsson A | Pain | 1995 | Cross-sectional study | 316 | Clinical presentation, pathophysiology |
| 16 | Sensitivity of patients with painful temporomandibular disorders to experimentally evoked pain: Evidence for altered temporal summation of pain [54] | Maixner W Fillingim RB Sigurdsson A Kincaid S Silva S | Pain | 1998 | Prospective study | 352 | Clinical presentation, pathophysiology |
| 17 | A Multiple Logistic Regression Analysis of the Risk and Relative Odds of Temporomandibular Disorders as a Function of Common Occlusal Features [55] | Pullinger AG Seligman DA Gornbein JA | Journal of Dental Research | 1993 | Cross-sectional study | 303 | Risk factors, etiology |
| 18 | Temporomandibular joint: Diagnostic accuracy with sagittal and coronal MR imaging [56] | Tasaki MM Westesson PL | Radiology | 1993 | Cross-sectional study | 290 | Diagnosis |
| 19 | Idiopathic pain disorders – Pathways of vulnerability [57] | Diatchenko L Nackley AG Slade GD Fillingim RB Maixner W | Pain | 2006 | Narrative review | 288 | Risk factors |
| 20 | A protocol for management of temporomandibular joint ankylosis [58] | Kaban LB Perrott DH Fisher K | Journal of Oral and Maxillofacial Surgery | 1990 | Retrospective study | 285 | Treatment |
| 21 | Changes in temporomandibular pain and other symptoms across the menstrual cycle [59] | LeResche L Mancl L Sherman JJ Gandara B Dworkin SF | Pain | 2003 | Prospective study | 284 | Risk factors, clinical presentation |
| 22 | Occlusion, orthodontic treatment, and temporomandibular disorders: A review [60] | McNamara JA Jr Seligman DA Okeson JP | Journal of Oral and Facial Pain and Headache | 1995 | Narrative review | 273 | Risk factors |
| 23 | Use of exogenous hormones and risk of temporomandibular disorder pain [61] | LeResche L Saunders K Von Korff MR Barlow W Dworkin SF | Pain | 1997 | Retrospective study | 272 | Risk factors |
| 24 | Classification and prevalence of temporomandibular joint disk displacement in patients and symptom-free volunteers [62] | Tasaki MM Westesson PL Isberg AM Ren YF Tallents RH | American Journal of Orthodontics and Dentofacial Orthopedics | 1996 | Cross-sectional study | 266 | Risk factors |
|
Table 1, continued | |||||||
|---|---|---|---|---|---|---|---|
| Ranking | Title | Authors | Journal | Year of publication | Study design | Citations | Study objective |
| 25 | Review of aetiological concepts of temporomandibular pain disorders: Towards a biopsychosocial model for integration of physical disorder factors with psychological and psychosocial illness impact factors [63] | Suvinen TI Reade PC Kemppainen P Könönen M Dworkin SF | European Journal of Pain | 2005 | Narrative review | 263 | Etiology |
| 26 | First onset of common pain symptoms: a prospective study of depression as a risk factor [64] | Von Korff M Resche LL Dworkin SF | Pain | 1993 | Prospective study | 261 | Risk factors |
| 27 | Risk factors for diagnostic subgroups of painful Temporomandibular Disorders (TMD) [65] | Huang GJ LeResche L Critchlow CW Martin MD Drangsholt MT | Journal of Dental Research | 2002 | Cross-sectional study | 259 | Risk factors |
| 28 | Ultrasound therapy for musculoskeletal disorders: A systematic review [66] | van der Windt DAWM van der Heijden GJMG van den Berg SGM Ter Riet G de Winter AF Bouter LM | Pain | 1999 | Systematic review | 256 | Treatment |
| 29 | Anatomic disorders of the temporomandibular joint disc in asymptomatic subjects [67] | Katzberg RW Westesson PL Tallents RH Drake CM | Journal of Oral and Maxillofacial Surgery | 1996 | Cross-sectional study | 249 | Risk factors |
| 30 | Modulation of pain by estrogens [68] | Craft RM | Pain | 2007 | Narrative review | 247 | Pathophysiology |
| 30 | Craniofacial Muscle Pain: Review of Mechanisms and Clinical Presentations [69] | Svensson P Graven-Nielsen T | Journal of Orofacial Pain | 2001 | Narrative review | 247 | Pathophysiology, clinical presentation |
| 32 | Relationship between bruxism and temporomandibular disorders: A systematic review of literature from 1998 to 2008 [9] | Manfredini D Lobbezoo F | Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontology | 2012 | Systematic review | 244 | Risk factors |
| 32 | Magnetic resonance imaging of the TMJ disc in asymptomatic volunteers [70] | Kircos LT Ortendahl DA Mark AS Arakawa M | Journal of Orofacial Pain | 1987 | Cross-sectional study | 244 | Risk factors |
| 32 | Inferior joint space arthrography and characteristics of condylar paths in internal derangements of the TMJ [71] | Farrar WB McCarty WL Jr | The Journal of Prosthetic Dentistry | 1979 | Cross-sectional study | 244 | Etiology |
| 35 | A Longitudinal Epidemiologic Study of Signs and Symptoms of Temporomandibular Disorders from 15 to 35 Years of Age [72] | Magnusson T Egermark I Carlsson GE | Journal of Orofacial Pain | 2000 | Prospective study | 240 | Prevalence |
| 36 | Progressive mandibular retrusion-idiopathic condylar resorption. Part I [73] | Arnett GW Milam SB Gottesman L | American Journal of Orthodontics and Dentofacial Orthopedics | 1996 | Narrative review | 239 | Pathophysiology |
|
Table 1, continued | |||||||
|---|---|---|---|---|---|---|---|
| Ranking | Title | Authors | Journal | Year of publication | Study design | Citations | Study objective |
| 37 | Catechol-O-methyltransferase inhibition increases pain sensitivity through activation of both | Nackley AG Tan KS Fecho K Flood P Diatchenko L Maixner W | Pain | 2007 | Animal study | 226 | Pathophysiology |
| 38 | Management of temporomandibular disorders: Concepts and controversies [75] | McNeill C | The Journal of Prosthetic Dentistry | 1997 | Narrative review | 222 | Treatment |
| 39 | Deficiency in endogenous modulation of prolonged heat pain in patients with Irritable Bowel Syndrome and Temporomandibular Disorder [76] | King CD Wong F Currie T Mauderli AP Fillingim RB Riley JL 3rd | Pain | 2009 | Cross-sectional study | 220 | Pathophysiology |
| 39 | Prevalence of temporomandibular disorder subtypes, psychologic distress, and psychosocial dysfunction in Asian patients [77] | Yap AU Dworkin SF Chua EK List T Tan KB Tan HH | Journal of Orofacial Pain | 2003 | Cross-sectional study | 220 | Prevalence |
| 39 | Prevalence in the Dutch Adult Population and a Meta-analysis of Signs and Symptoms of Temporomandibular Disorder [78] | De Kanter RJ Truin GJ Burgersdijk RC Van ’t Hof MA Battistuzzi PG Kalsbeek H Käyser AF | Journal of Dental Research | 1993 | Cross-sectional study | 220 | Prevalence |
| 42 | Oro-facial pain in the community: Prevalence and associated impact [79] | Macfarlane TV Blinkhorn AS Davies RM Kincey J Worthington HV | Community Dentistry and Oral Epidemiology | 2002 | Cross-sectional study | 218 | Prevalence |
| 43 | Oral splints: The crutches for temporomandibular disorders and bruxism [80] | Dao TT Lavigne GJ | Critical Reviews in Oral Biology and Medicine | 1998 | Narrative review | 214 | Treatment |
| 44 | Temporomandibular joint: Relationship between MR evidence of effusion and the presence of pain and disk displacement [81] | Westesson PL Brooks SL | American Journal of Roentgenology | 1992 | Cross-sectional study | 213 | Prevalence, diagnosis |
| 45 | Functional disorders of the masticatory system I. Distribution of symptoms according to age and sex as judged from investigation by questionnaire [82] | Agerberg G Carlsson GE | Acta Odontologica Scandinavica | 1972 | Cross-sectional study | 210 | Prevalence |
|
Table 1, continued | |||||||
|---|---|---|---|---|---|---|---|
| Ranking | Title | Authors | Journal | Year of publication | Study design | Citations | Study objective |
| 46 | The prevalence and treatment needs of subjects with temporomandibular disorders [83] | Schiffman EL Fricton JR Haley DP Shapiro BL | Journal of the American Dental Association | 1990 | Cross-sectional study | 209 | Prevalence |
| 47 | Arthroscopic surgery of the temporomandibular joint: Treatment of internal derangement with persistent closed lock [84] | Sanders B | Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontology | 1986 | Prospective study | 208 | Treatment |
| 48 | Prevalence of Temporomandibular Dysfunction and Its Association with Malocclusion in Children and Adolescents: An Epidemiologic Study Related to Specified Stages of Dental Development [85] | Thilander B Rubio G Pena L de Mayorga C | Angle Orthodontist | 2002 | Cross-sectional study | 205 | Prevalence |
| 49 | Progressive mandibular retrusion-idiopathic condylar resorption. Part II [86] | Arnett GW Milam SB Gottesman L | American Journal of Orthodontics and Dentofacial Orthopedics | 1996 | Narrative review | 204 | Pathophysiology |
| 50 | Epidemiology and Treatment Need for Temporomandibular Disorders [87] | Carlsson GE | Journal of Orofacial Pain | 1999 | Narrative review | 203 | Prevalence |
The articles are ordered by number of citations.
Table 2
Journals that published the 50 most cited articles on temporomandibular disorders
| Journal | 2020 Journal Impact Factor | Quartile of the Category “Dentistry, | |||||||||
| Oral | |||||||||||
| Surgery & | |||||||||||
| Medicine” | Eigenfactor Score | Normalized Eigenfactor | Article influence score | 5-Year Impact Factor | Immediacy Index | Number of manuscripts | Citations | ||||
| 1 | Pain | 6.961 | N/A | 0.03099 | 649. | 635 | 2.234 | 7.704 | 1.909 | 11 | 4728 |
| 2 | Journal of Craniomandibular Disorders | N/A | N/A | N/A | N/A | N/A | N/A | N/A | 1 | 3020 | |
| 3 | Journal of Oral and Facial Pain and Headache | 1.871 | Q4 | 0.00101 | 0. | 21243 | 0.432 | 2.123 | 0.682 | 2 | 1720 |
| 4 | Journal of Orofacial Pain | 2.824 | N/A | 0.00194 | 0. | 22109 | 0.897 | 2.678 | N/A | 6 | 1505 |
| 5 | Journal of Dental Research | 6.116 | Q1 | 0.01702 | 356. | 864 | 1.747 | 7.199 | 4.531 | 4 | 1185 |
| 6 | Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology | 2.589 | Q2 | 0.00599 | 125. | 721 | 0.593 | 2.537 | 0.573 | 4 | 1170 |
| and Endodontology | |||||||||||
| 7 | Journal of Oral and Maxillofacial Surgery | 1.895 | Q3 | 0.01116 | 234. | 045 | 0.575 | 2.256 | 0.617 | 3 | 886 |
| 8 | Critical Reviews in Oral Biology and Medicine | 6.000 | N/A | N/A | N/A | N/A | N/A | N/A | 2 | 864 | |
| 9 | Journal of the American Dental Association | 3.634 | Q1 | 0.00508 | 106. | 526 | 1.076 | 3.983 | 0.902 | 2 | 852 |
| 10 | American Journal of Orthodontics and Dentofacial Orthopedics | 2.650 | Q2 | 0.00673 | 141. | 114 | 0.738 | 2.880 | 0.676 | 3 | 709 |
| 11 | Acta Odontologica Scandinavica | 2.331 | Q3 | 0.00246 | 0. | 51599 | 0.535 | 2.360 | 0.453 | 2 | 543 |
| 12 | The Journal of Prosthetic Dentistry | 3.426 | Q2 | 0.00991 | 207. | 821 | 0.750 | 3.846 | 1.366 | 2 | 466 |
| 13 | Archives of Internal Medicine | 17.333 | N/A | 0.06673 | 747. | 380 | 5.869 | 13.098 | N/A | 1 | 455 |
| 14 | Archives of Otolaryngology-Head and Neck Surgery | 2.327 | N/A | 0.00855 | 0. | 95791 | 0.790 | 2.305 | N/A | 1 | 407 |
| 15 | New England Journal of Medicine | 91.253 | N/A | 0.63202 | 13.247.856 | 37.313 | 89.676 | 162.030 | 1 | 332 | |
| 16 | Radiology | 11.105 | N/A | 0.05293 | 1.109.612 | 2.984 | 10.389 | 35.141 | 1 | 290 | |
| 17 | European Journal of Pain | 3.934 | N/A | 0.00909 | 190. | 668 | 1.109 | 4.068 | 0.873 | 1 | 263 |
| 18 | Community Dentistry and Oral Epidemiology | 3.383 | Q2 | 0.00278 | 0. | 58272 | 0.824 | 3.500 | 0.561 | 1 | 218 |
| 19 | American Journal of Roentgenology | 3.959 | N/A | 0.02458 | 515. | 341 | 1.130 | 4.073 | 5.850 | 1 | 213 |
| 20 | Angle Orthodontist | 2.079 | Q3 | 0.00423 | 0. | 88828 | 0.683 | 2.599 | 0.792 | 1 | 205 |
The journals are ordered by number of citations. Abbreviations: N/A
Table 3
Top 10 authors that wrote the 50 most cited articles on temporomandibular disorders
| Ranking | Author | Affiliation | Country | h-index | Number of articles | First author | Last author | Coauthor | Citations |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Dworkin SF | University of Washington | United States, Seattle | 51 | 9 | 2 | 6 | 1 | 8462 |
| 2 | LeResche LA | University of Washington | United States, Seattle | 46 | 7 | 3 | 2 | 2 | 5479 |
| 3 | Truelove E | University of Washington | United States Seattle | 39 | 3 | 0 | 0 | 3 | 4924 |
| 4 | Lobbezoo F | Academic Centre for Dentistry Amsterdam | Netherlands, Amsterdam | 50 | 3 | 0 | 2 | 1 | 4074 |
| 5 | Schiffman EL | School of Dentistry | United States, Minneapolis | 33 | 3 | 2 | 1 | 0 | 4056 |
| 6 | List T | Skånes Universitetssjukhus | Sweden, Lund | 43 | 2 | 0 | 0 | 2 | 3334 |
| 7 | Von Korff M | University of Washington | United States, Seattle | 123 | 4 | 2 | 0 | 2 | 3228 |
| 8 | Maixner W | Duke University Medical Centre | United States, Durham | 71 | 4 | 2 | 2 | 0 | 2583 |
| 9 | Brooks SL | University of Michigan, Ann Arbor | United States, Ann Arbor | 27 | 2 | 0 | 1 | 1 | 1660 |
| 10 | Fillingim RB | University of Florida | United States, Gainesville | 81 | 4 | 0 | 0 | 4 | 1130 |
The authors are ordered by the number of citations of their papers included in the 50 most cited articles on temporomandibular disorders.
The keywords of the 50 most cited articles in TMD were collected and a map was created. It shows temporomandibular joint disorder as the bigger node, it has been used for the greatest number of times in common to more articles. Temporomandibular joint disorder collected 31 occurrences and 226 total link strengths. Also, TMD and temporomandibular joint were highly strength terms. Other big nodes are represented by female and male respectively with 29 and 26 occurrences. Also, adult and adolescent are two terms with high occurrences, 29 for adult and 20 for adolescent.
4.Discussion
To the best of our knowledge, this is the first bibliometric analysis study that explored the 50 most cited articles on TMD and one of the very few in the field of dentistry. According to other comparable published publications, the sample size was selected at 50 manuscripts to give a manageable and significant number of papers to be studied [88].
4.1Number of citations
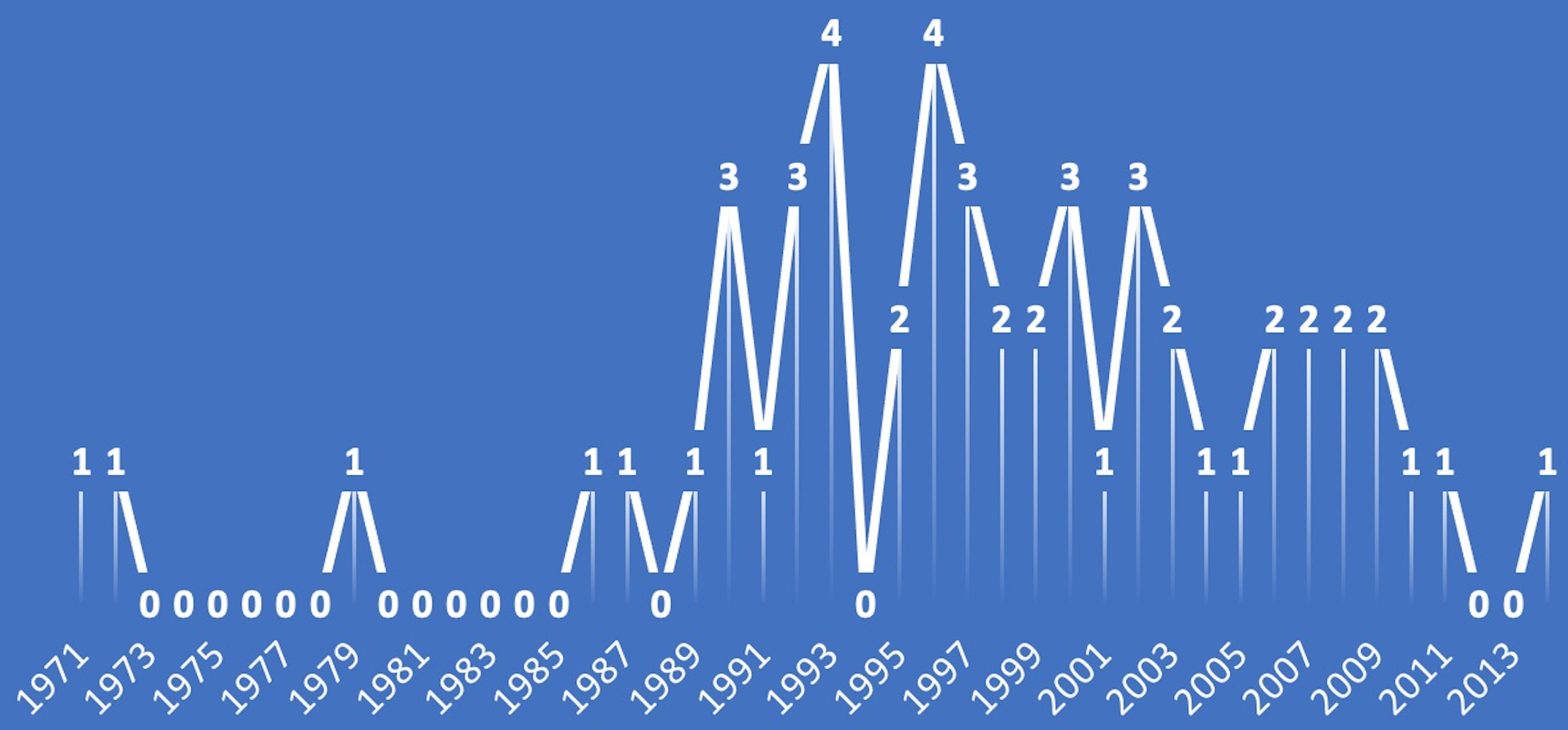
A progressive number of citations over the year is registered from the available data in the field of TMD, as shown in Fig. 1. Most of the publications in this bibliometric analysis were published between 1990 and 2003. There was a peak of 4 papers published in 1993 and in 1996; thus the 90s might be considered the decade with the highest number of publications of the top 50 most cited articles on TMD (see Fig. 2 for further details).
Figure 2.
Number of articles published per year.
4.2Study design
The 50 most cited papers on TMD were quite heterogeneous in terms of study design. It is interesting to note that almost the 80% of them was the sum of the number of cross-sectional studies (
4.3Journals
According to the results, 34.00% of the listed article were published just in two journals (Pain and Journal of Orofacial Pain) collecting 31.12% of total citations (6233 over 20031). This aspect demonstrated how a relevant number of papers was concentered in a limited number of scientific Journals. Moreover, it should be noted that the last JIF of the Journal of Orofacial Pain was reported in 2014, probably due to the newborn Journal of Oral and Facial Pain and Headache, that with only 2 papers (among the 50 most cited ones) obtained 1720 citations (third Journal for citations).
The JIF, defined as the frequency with which the average article in a journal has been referenced in the previous years, could be considered as the most prevalent metric of journal prestige. Despite JIF is largely used, for sure it has obvious limitations. First, the time-constrained of the JIF that is not sufficient for judging the impact of papers published, most of the papers reach the maximal scientific impact over 2 years beyond the publication.
All multidisciplinary journals tend to have higher value of both JIF and 5-JIF respect to the journals how treat more specific fields, this because reach readers from more disciplines. The case just described concerns the journals in the dental field compared to those in the medical field, the latter tend to have a higher number of citations.
Another factor that could have a significant impact on the JIF is the misuse of self-citations. The self-citation percentage in the presented list was low (5.44%), lower than the average reported in dentistry [89] and lower than a recent study’s median self-citation rate of 12.7% [90].
4.4Authors
The data extraction showed the presence of 142 authors in the 50 most cited articles on TMD. Considering that each document has several authors, it is difficult to pinpoint each author’s particular contribution and, as a result, their role. Traditionally the name of the first author is the name of the main contributor and the name of the last author represent by the supervisor of the scientific work and usually the last name is also the corresponding author. The most impacted authors in TMD articles usually take place one of the two positions described above, less frequently they took position as coauthor. Indeed, Dworkin, the most impacted author, contributed to nine papers and in seven of these as first or last author, also LeResche second in this list, contributed with seven articles and in 5 of these she was first or last author. The disparity in h-index among authors of the top 50 papers suggests contributions from researchers with varying levels of academic expertise. Also, the origin of the publications was considered. In this analysis it emerges that North America, both USA and Canada, contributed with 33 articles (30 for USA and 3 for Canada) and Europe with 13 papers (most contributions were from Sweden with 7 and Italy with 2); the outsider is Japan with less contributions given by two articles. This pattern could be explained by accumulative geographic advantage, as citations are more likely to come from institutions in the same nation as the author [91]. Furthermore, the USA benefits from a large scientific community and generous science funding regulations. The findings evidenced a collaboration between institutions, the highest number of citations is associated with authors affiliated with the universities.
4.5Time period
Most articles ranked in the top 50 more cited in TMD were published from 1990 to 2005 with 35 articles. In lasts fifteen years from 2006 to 2021 just 11 articles were published with no articles listed published after 2014. This maybe could be affected by the shortest timeframe that articles published after 2014 received to be highly cited. In contrast to this trend authors took over the number of citations of the top 50 articles in TMD occurred every year. The data showed how this number increased among the years, authors detected from 2006 when just 627 citations were done to 2021 when the number reach the peak with 1483 citations (see Fig. 2 for further details). Therefore, the citations have been continuously increasing such as the interest in the scientific research on the management of TMD, a cornerstone in dental clinical practice.
4.6Keywords
A visualized analysis of the keywords co-occurrence was performed, considered as a technique for mapping the study domain in a particular topic by looking at the relationship between different terms [91]. Keywords commonly allow for accurate indexing in computerized databases, allowing for more scientific publications to be found easily. According to the keywords map the central node is represented by temporomandibular joint disorder. It is followed by the nodes representing female and male.
As could be expected, the first term is “temporomandibular joint disorder”, considering that it represented the main topic of the included papers. Other two terms highly represented were “female” and “male”, two nodes related with a smaller one targeted with “sex differences”, thus showing how TMD might be influenced by sex, with different prevalence for male and female. Moreover, “age” and “age difference” are interconnected with “prevalence”, thus meaning that TMD could be considered as problems related to different age groups.
Another important field of research was represented by the investigation on the potential risk factors. There were two smaller nodes named “risk factors” and “risk” that were strictly interconnected to the nodes described above representing sex differences and age as well as some specific time bands such as adolescence or middle age. Moreover, there was also a relationship between “depression” and “chronic pain”, thus underling the potential influence of these components on patients with TMD.
Lastly, there were connections to other nodes showing several anatomical parts of temporomandibular joint, as articular cartilage, condyle, mandibular, masticatory muscle, osteoarthritis, malocclusion, and bruxism (see Fig. 3 for further details).
Figure 3.
Network analysis of keywords (visualized analysis).

4.7Study limitations
This paper is not without limitations. First, some keywords of the search strategy might be included also in other articles not of interest for our bibliometric analysis; however, we chose to be more inclusive in the first phases to minimize potential selection biases. Second, the citations per year have not been assessed; thus, the impact of more recent studies might be underestimated. Lastly, this bibliometric analysis might present a bias considering that older articles might have more citations, due to their timing on the scientific literature. In this scenario, a similar bibliometric analysis [92] has recently been published, but the authors focused on the last 20 years, without providing a broad overview about the whole scientific literature. On the other hand, to the best of our knowledge, this is the first bibliometric analysis assessing TMD via the Scopus database without time restrictions, potentially filling a gap of knowledge on TMD.
5.Conclusions
The findings of this bibliometric study showed an increasing number of citations for papers on TMD, synonymous of a high interest in the scientific research in the last years. The paper with the highest number of citations was on the research diagnostic criteria on TMD.
Starting from the analysis of the most cited articles in this field, this bibliometric analysis might provide information to researchers for an adequate knowledge of previous literature on a well-debated topic such as TMD.
In light of these considerations, the results of our bibliometric analysis might pave the way to future research focusing on the gap of knowledge in scientific literature highlighted by the mapping network of the present study. Thus, further studies should be performed based on the knowledge on the most relevant articles in the literature regarding TMD.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contribution
Conceptualization: MF, VG, AdS; Methodology: MF, VG, AdS; Formal analysis: VG, AB, RM; Data curation: MF, VG, LL; Writing-original draft preparation, MF, VG, LL; Writing-review and editing: MM, AdS; Visualization: AB, RM, CC, DC, MI; Supervision: MI, MM, AdS. All authors read and approved the final version of the manuscript.
Acknowledgments
None to report.
Conflict of interest
The authors report that there are no competing interests to declare.
References
[1] | American Academy of Orofacial Pain; de Leeuw R, Klasser GD, eds. Orofacial pain: Guidelines for assessment, diagnosis, and management, 6th ed. Hanover Park, IL: Quintessence Publishing. (2018) ; 143: : 207. |
[2] | Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: Review, criteria, examinations and specifications, critique. J Craniomandib Disord. (1992) ; 6: (4): 301-55. PMID: 1298767. |
[3] | Schiffman E, Ohrbach R, Truelove E, et al. International RDC/TMD Consortium Network, International association for Dental Research; Orofacial Pain Special Interest Group, International Association for the Study of Pain. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group†. J Oral Facial Pain Headache. (2014) Winter; 28: (1): 6-27. doi: 10.11607/jop.1151. |
[4] | Skeie MS, Frid P, Mustafa M, Aßmus J, Rosén A. DC/TMD examiner protocol: Longitudinal evaluation on interexaminer reliability. Pain Res Manag. (2018) ; 2018: : 7474608. doi: 10.1155/2018/7474608. |
[5] | Ohrbach R, Dworkin SF. The evolution of TMD diagnosis: Past, present, future. J Dent Res. (2016) ; 95: (10): 1093-1101. doi: 10.1177/0022034516653922. |
[6] | Kavuncu V, Sahin S, Kamanli A, Karan A, Aksoy C. The role of systemic hypermobility and condylar hypermobility in temporomandibular joint dysfunction syndrome. Rheumatol Int. (2006) ; 26: : 257-260. |
[7] | Wongwatana S, Kronman JH, Clark RE, Kabani S, Mehta N. Anatomic basis for disk displacement in temporomandibular joint (TMJ) dysfunction. Am J Orthod Dentofacial Orthop. (1994) ; 105: : 257-264. doi: 10.1016/S0889-5406(94)70119-9. |
[8] | Kobs G, Bernhardt O, Kocher T, Meyer G. Oral parafunctions and positive clinical examination findings. Stomatologija. (2005) ; 7: (3): 81-3. |
[9] | Manfredini D, Lobbezoo F. Relationship between bruxism and temporomandibular disorders: A systematic review of literature from 1998 to 2008. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. (2010) ; 109: (6): e26-50. doi: 10.1016/j.tripleo.2010.02.013. |
[10] | Iodice G, Danzi G, Cimino R, et al. Association between posterior crossbite, masticatory muscle pain, and disc displacement: A systematic review. Eur J Orthod. (2013) ; 35: (6): 737-44. doi: 10.1093/ejo/cjt024. |
[11] | Dıraçoglu D, Yıldırım NK, Saral İ, et al. Temporomandibular dysfunction and risk factors for anxiety and depression. J Back Musculoskelet Rehabil. (2016) ; 29: (3): 487-491. doi: 10.3233/BMR-150644. |
[12] | Ferrillo M, Marotta N, Giudice A, et al. Effects of occlusal splints on spinal posture in patients with temporomandibular disorders: A systematic review. Healthcare (Basel). (2022) ; 15; 10(4): 739. doi: 10.3390/healthcare10040739. |
[13] | Çebi A, Yilmaz N, Karayürek F, Gülses A. Depression and anxiety levels in a group of elderly with Temporomandibular Disorders. Turkish Journal of Geriatrics. (2021) ; 24: (3): 397-406. doi: 10.31086/Tjgeri.2021.237. |
[14] | Li DTS, Leung YY. Temporomandibular disorders: Current concepts and controversies in diagnosis and management. Diagnostics (Basel). (2021) Mar 6; 11: (3): 459. doi: 10.3390/diagnostics11030459. |
[15] | Walczyńska-Dragon K, Baron S, Nitecka-Buchta A, Tkacz E. Correlation between TMD and cervical spine pain and mobility: Is the whole body balance TMJ related? Biomed Res Int. (2014) ; 2014: : 582414. doi: 10.1155/2014/582414. |
[16] | Manfredini D, Guarda-Nardini L, Winocur E, Piccotti F, Ahlberg J, Lobbezoo F. Research diagnostic criteria for temporomandibular disorders: A systematic review of axis I epidemiologic findings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. (2011) ; 112: (4): 453-462. doi: 10.1016/j.tripleo.2011.04.021. |
[17] | LeResche L. Epidemiology of temporomandibular disorders: Implications for the investigation of etiologic factors. Crit Rev Oral Biol Med. (1997) ; 8: (3): 291-305. doi: 10.1177/10454411970080030401. |
[18] | Slade GD, Bair E, Greenspan JD, et al. Signs and symptoms of first-onset TMD and sociodemographic predictors of its development: The OPPERA prospective cohort study. J Pain. (2013) ; 14: (12 Suppl): T20-32.e323. doi: 10.1016/j.jpain.2013.07.014. |
[19] | Sipilä K, Ylöstalo PV, Joukamaa M, Knuuttila ML. Comorbidity between facial pain, widespread pain, and depressive symptoms in young adults. J Orofac Pain. (2006) ; 20: (1): 24-30. PMID: 16483017. |
[20] | Raya CR, Plaza-Manzano G, Pecos-Martín D, Ferragut-Garcías A, Martín-Casas P, Gallego-Izquierdo T, Romero-Franco N. Role of upper cervical spine in temporomandibular disorders. J Back Musculoskelet Rehabil. (2017) Nov 6; 30: (6): 1245-1250. doi: 10.3233/BMR-169620. |
[21] | Gerber LH, Sikdar S, Armstrong K, et al. A systematic comparison between subjects with no pain and pain associated with active myofascial trigger points. PM R. (2013) ; 5: (11): 931-938. doi: 10.1016/j.pmrj.2013.06.006. |
[22] | Tanaka E, Detamore MS, Mercuri LG. Degenerative disorders of the temporomandibular joint: Etiology, diagnosis, and treatment. J Dent Res. (2008) ; 87: (4): 296-307. doi: 10.1177/154405910808700406. |
[23] | Deregibus A, Ferrillo M, Piancino MG, Domini MC, de Sire A, Castroflorio T. Are occlusal splints effective in reducing myofascial pain in patients with muscle-related temporomandibular disorders? A randomized-controlled trial. Turk J Phys Med Rehabil. (2021) ; 67: (1): 32-40. doi: 10.5606/tftrd.2021.6615. |
[24] | Marotta N, Ferrillo M, Demeco A, et al. Effects of radial extracorporeal shock wave therapy in reducing pain in patients with temporomandibular disorders: A pilot randomized controlled trial. Appl Sci. (2022) ; 12: (8): 3821. doi: 10.3390/app12083821d. |
[25] | Xu GZ, Jia J, Jin L, Li JH, Wang ZY, Cao DY. Low-level laser therapy for temporomandibular disorders: A systematic review with meta-analysis. Pain Res Manag. (2018) ; 2018: : 4230583. doi: 10.1155/2018/4230583. |
[26] | Ferrillo M, Ammendolia A, Paduano S, et al. Efficacy of rehabilitation on reducing pain in muscle-related temporomandibular disorders: A systematic review and meta-analysis of randomized controlled trials. J Back Musculoskelet Rehabil. (2022) ; 10.3233/BMR-210236. doi: 10.3233/BMR-210236. |
[27] | de Sire A, Marotta N, Ferrillo M, et al. Oxygen-ozone therapy for reducing pro-inflammatory cytokines serum levels in musculoskeletal and temporomandibular disorders: A comprehensive review. Int J Mol Sci. (2022) ; 23: (5): 2528. doi: 10.3390/ijms23052528. |
[28] | Donthu N, Kumar S, Mukherjee D, et al. How to conduct a bibliometric analysis: An overview and guidelines. Journal of Business Research. (2021) ; 133: : 285-296. doi: 10.1016/j.jbusres.2021.04.070. |
[29] | Miller CS. Impact versus impact factor and Eigenfactor. Oral Surg Oral Med Oral Pathol Oral Radiol. (2012) ; 113: (2): 145-146. doi: 10.1016/j.tripleo.2011.08.009. |
[30] | Peritz BC. On the association between journal circulation and impact factor. J Inf Sci. (1995) ; 21: : 63-67. |
[31] | Duyx B, Urlings MJE, Swaen GMH, Bouter LM, Zeegers M. Scientific citations favor positive results: A systematic review and meta-analysis. J Clin Epidemiol. (2017) ; 88: : 92-101. doi: 10.1016/j.jclinepi.2017.06.002. |
[32] | Garfield E. What is a citation classic. Clin Chem. (2013) ; 147-57. |
[33] | Kodonas K, Fardi A, Gogos C, Economides N. Top 50 cited articles on dental stem cell research. Restor Dent Endod. (2020) ; 45: (2): e17. Published 2020 Feb 11. doi: 10.5395/rde.2020.45.e17. |
[34] | Bruni A, Serra FG, Gallo V, Deregibus A, Castroflorio T. The 50 most-cited articles on clear aligner treatment: A bibliometric and visualized analysis. Am J Orthod Dentofacial Orthop. (2021) ; 159: (4): e343-e362. doi: 10.1016/j.ajodo.2020.11.029. |
[35] | Huang F, Zheng B, Wu C, Zhao S, Xu Y, Li Z, Huang C, Fan Z, Wu S. International publication trends in low back pain research: A bibliometric and visualization analysis. Front Public Health. (2022) Mar 2; 10: : 746591. doi: 10.3389/fpubh.2022.746591. |
[36] | Grillo R. Orthognathic surgery: A bibliometric analysis of the top 100 cited articles. J Oral Maxillofac Surg. (2021) ; 79: (11): 2339-2349. doi: 10.1016/j.joms.2021.06.004. |
[37] | Yılmaz B, Familiari F, Castricini R, Galasso O, Gasparini G, Iannò B, Ranuccio F. The 50 highest cited papers on rotator cuff tear. Arthroscopy. (2021) Jan; 37: (1): 61-68. doi: 10.1016/j.arthro.2020.07.044. |
[38] | Sarode SC, Sarode GS, Yuwanati M, Gadbail A, Gondivkar S. A brief overview of 100 best-cited papers on oral submucous fibrosis in Oral Oncology. Oral Oncol. (2022) ; 126: : 105769. doi: 10.1016/j.oraloncology.2022.105769. |
[39] | Brito J, Nassis GP, Seabra AT, Figueiredo P. Top 50 most-cited articles in medicine and science in football. BMJ Open Sport Exerc Med. (2018) ; 4: (1): e000388. doi: 10.1136/bmjsem-2018-000388. |
[40] | Varghese VS, Atwal PK, Dua KK, Kurian N, Cherian JM, Sabu AM. A bibliometric analysis of the top 50 most cited articles published in the Journal of Conservative Dentistry. J Conserv Dent. (2021) ; 24: (4): 341-347. doi: 10.4103/jcd.jcd_320_21. |
[41] | Kodonas K, Fardi A, Gogos C, Economides N. Top 50 cited articles on dental stem cell research. Restor Dent Endod. (2020) ; 45: (2): e17. doi: 10.5395/rde.2020.45.e17. |
[42] | Von Korff M, Ormel J, Keefe FJ, Dworkin SF. Grading the severity of chronic pain. Pain. (1992) ; 50: (2): 133-149. doi: 10.1016/0304-3959(92)90154-4. |
[43] | Schiffman E, Ohrbach R, Truelove E, et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group†. J Oral Facial Pain Headache. (2014) ; 28: (1): 6-27. doi: 10.11607/jop.1151. |
[44] | Dworkin SF, Huggins KH, LeResche L, et al. Epidemiology of signs and symptoms in temporomandibular disorders: Clinical signs in cases and controls. J Am Dent Assoc. (1990) ; 120: (3): 273-281. doi: 10.14219/jada.archive.1990.0043. |
[45] | Ayouni Aaron LA, Burke MM, Buchwald D. Overlapping conditions among patients with chronic fatigue syndrome, fibromyalgia, and temporomandibular disorder. Arch Intern Med. (2000) ; 160: (2): 221-7. |
[46] | Wilkes CH. Internal derangements of the temporomandibular joint. Pathological variations. Arch Otolaryngol Head Neck Surg. (1989) ; 115: (4): 469-477. doi: 10.1001/archotol.1989.01860280067019. |
[47] | Tanaka E, Detamore MS, Mercuri LG. Degenerative disorders of the temporomandibularjoint: Etiology, diagnosis, and treatment. J Dent Res. (2008) ; 87: (4): 296-307. |
[48] | Ahmad M, Hollender L, Anderson Q, et al. Research diagnostic criteria for temporomandibular disorders (RDC/TMD): Development of image analysis criteria and examiner reliability for image analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. (2009) ; 107: (6): 844-860. doi: 10.1016/j.tripleo.2009.02.023. |
[49] | Nitzan DW, Dolwick MF, Martinez GA. Temporomandibular joint arthrocentesis: A simplified treatment for severe, limited mouth opening. J Oral Maxillofac Surg. (1991) ; 49: (11): 1163-1170. doi: 10.1016/0278-2391(91)90409-f. |
[50] | Dao TT, LeResche L. Gender differences in pain. J Orofac Pain. (2000) ; 14: (3): 169-84; discussion 184-95. PMID: 11203754. |
[51] | Oberg T, Carlsson GE, Fajers CM. The temporomandibular joint. A morphologic study on a human autopsy material. Acta Odontol Scand. (1971) ; 29: (3): 349-384. doi: 10.3109/00016357109026526. |
[52] | Scrivani SJ, Keith DA, Kaban LB. Temporomandibular disorders. N Engl J Med. (2008) Dec18; 359: (25): 2693-705. |
[53] | Maixner W, Fillingim R, Booker D, Sigurdsson A. Sensitivity of patients with painful temporomandibular disorders to experimentally evoked pain. Pain. (1995) ; 63: (3): 341-351. doi: 10.1016/0304-3959(95)00068-2. |
[54] | Maixner W, Fillingim R, Sigurdsson A, Kincaid S, Silva S. Sensitivity of patients with painful temporomandibular disorders to experimentally evoked pain: Evidence for altered temporal summation of pain. Pain. (1998) ; 76: (1-2): 71-81. doi: 10.1016/s0304-3959(98)00028-1. |
[55] | Pullinger AG, Seligman DA, Gornbein JA. A multiple logistic regression analysis of the risk and relative odds of temporomandibular disorders as a function of common occlusal features. J Dent Res. (1993) ; 72: (6): 968-979. doi: 10.1177/00220345930720061301. |
[56] | Tasaki MM, Westesson PL. Temporomandibular joint: Diagnostic accuracy with sagittal and coronal MR imaging. Radiology. (1993) ; 186: (3): 723-729. doi: 10.1148/radiology.186.3.8430181. |
[57] | Diatchenko L, Nackley AG, Slade GD, Fillingim RB, Maixner W. Idiopathic pain disorders-pathways of vulnerability. Pain. (2006) ; 123: (3): 226-230. doi: 10.1016/j.pain.2006.04.015. |
[58] | Kaban LB, Perrott DH, Fisher K. A protocol for management of temporomandibular joint ankylosis. J Oral Maxillofac Surg. (1990) ; 48: (11): 1145-1152. doi: 10.1016/0278-2391(90)90529-b. |
[59] | LeResche L, Mancl L, Sherman JJ, Gandara B, Dworkin SF. Changes in temporomandibular pain and other symptoms across the menstrual cycle. Pain. (2003) ; 106: (3): 253-261. doi: 10.1016/j.pain.2003.06.001. |
[60] | McNamara JA Jr, Seligman DA, Okeson JP. Occlusion, Orthodontic treatment, and temporomandibular disorders: A review. J Orofac Pain. (1995) ; 9: (1): 73-90. |
[61] | LeResche L, Saunders K, Von Korff MR, Barlow W, Dworkin SF. Use of exogenous hormones and risk of temporomandibular disorder pain. Pain. (1997) ; 69: (1-2): 153-60. doi: 10.1016/s0304-3959(96)03230-7. |
[62] | Tasaki MM, Westesson PL, Isberg AM, Ren YF, Tallents RH. Classification and prevalence of temporomandibular joint disk displacement in patients and symptom-free volunteers. Am J Orthod Dentofacial Orthop. (1996) ; 109: (3): 249-262. doi: 10.1016/s0889-5406(96)70148-8. |
[63] | Suvinen TI, Reade PC, Kemppainen P, Könönen M, Dworkin SF. Review of aetiological concepts of temporomandibular pain disorders: Towards a biopsychosocial model for integration of physical disorder factors with psychological and psychosocial illness impact factors. Eur J Pain. (2005) ; 9: (6): 613-633. doi: 10.1016/j.ejpain.2005.01.012. |
[64] | Von Korff M, Resche LL, Dworkin SF. First onset of common pain symptoms: A prospective study of depression as a risk factor. Pain. (1993) ; 55: (2): 251-258. doi: 10.1016/0304-3959(93)90154-H. |
[65] | Huang GJ, LeResche L, Critchlow CW, Martin MD, Drangsholt MT. Risk factors for diagnostic subgroups of painful temporomandibular disorders (TMD). J Dent Res. (2002) ; 81: (4): 284-288. doi: 10.1177/154405910208100412. |
[66] | van der Windt DAWM, van der Heijden GJMG, van den Berg SGM, Ter Riet G, de Winter AF, Bouter LM. Ultrasound therapy for musculoskeletal disorders: A systematic review. Pain. (1999) ; 81: (3): 257-271. doi: 10.1016/S0304-3959(99)00016-0. |
[67] | Katzberg RW, Westesson PL, Tallents RH, Drake CM. Anatomic disorders of the temporomandibular joint disc in asymptomatic subjects. J Oral Maxillofac Surg. (1996) ; 54: (2): 147-155. doi: 10.1016/s0278-2391(96)90435-8. |
[68] | Craft RM. Modulation of pain by estrogens. Pain. (2007) ; 132: (Suppl 1): S3-S12. doi: 10.1016/j.pain.2007.09.028. |
[69] | Svensson P, Graven-Nielsen T. Craniofacial muscle pain: Review of mechanisms and clinical manifestations. J Orofac Pain. (2001) ; 15: (2): 117-45. |
[70] | Kircos LT, Ortendahl DA, Mark AS, Arakawa M. Magnetic resonance imaging of the TMJ disc in asymptomatic volunteers. J Oral Maxillofac Surg. (1987) ; 45: (10): 852-854. doi: 10.1016/0278-2391(87)90235-7. |
[71] | Farrar WB, McCarty WL Jr. Inferior joint space arthrography and characteristics of condylar paths in internal derangements of the TMJ. J Prosthet Dent. (1979) ; 41: (5): 548-555. doi: 10.1016/0022-3913(79)90092-1. |
[72] | Magnusson T, Egermark I, Carlsson GE. A longitudinal epidemiologic study of signs and symptoms of temporomandibular disorders from 15 to 35 years of age. J Orofac Pain. (2000) ; 14: (4): 310-319. PMID: 11203765. |
[73] | Arnett GW, Milam SB, Gottesman L. Progressive mandibular retrusion-idiopathic condylar resorption. Part I. Am J Orthod Dentofacial Orthop. (1996) ; 110: (1): 8-15. doi: 10.1016/s0889-5406(96)70081-1. |
[74] | Nackley AG, Tan KS, Fecho K, Flood P, Diatchenko L, Maixner W. Catechol-O-methyltransferase inhibition increases pain sensitivity through activation of both beta2- and beta3-adrenergic receptors. Pain. (2007) ; 128: (3): 199-208. doi: 10.1016/j.pain.2006.09.022. |
[75] | McNeill C. Management of temporomandibular disorders: Concepts and controversies. J Prosthet Dent. (1997) ; 77: (5): 510-522. doi: 10.1016/s0022-3913(97)70145-8. |
[76] | King CD, Wong F, Currie T, Mauderli AP, Fillingim RB, Riley JL 3rd. Deficiency in endogenous modulation of prolonged heat pain in patients with Irritable Bowel Syndrome and Temporomandibular Disorder. Pain. (2009) ; 143: (3): 172-178. doi: 10.1016/j.pain.2008.12.027. |
[77] | Yap AU, Dworkin SF, Chua EK, List T, Tan KB, Tan HH. Prevalence of temporomandibular disorder subtypes, psychologic distress, and psychosocial dysfunction in Asian patients. J Orofac Pain. (2003) ; 17: (1): 21-28. |
[78] | De Kanter RJ, Truin GJ, Burgersdijk RC, et al. Prevalence in the Dutch adult population and a meta-analysis of signs and symptoms of temporomandibular disorder. J Dent Res. (1993) ; 72: (11): 1509-1518. doi: 10.1177/00220345930720110901. |
[79] | Macfarlane TV, Blinkhorn AS, Davies RM, Kincey J, Worthington HV. Oro-facial pain in the community: Prevalence and associated impact. Community Dent Oral Epidemiol. (2002) ; 30: (1): 52-60. doi: 10.1034/j.1600-0528.2002.300108.x. |
[80] | Dao TT, Lavigne GJ. Oral splints: The crutches for temporomandibular disorders and bruxism? Crit Rev Oral Biol Med. (1998) ; 9: (3): 345-361. doi: 10.1177/10454411980090030701. |
[81] | Westesson PL, Brooks SL. Temporomandibular joint: Relationship between MR evidence of effusion and the presence of pain and disk displacement. AJR Am J Roentgenol. (1992) ; 159: (3): 559-563. doi: 10.2214/ajr.159.3.1503025. |
[82] | Agerberg G, Carlsson GE. Functional disorders of the masticatory system. I. Distribution of symptoms according to age and sex as judged from investigation by questionnaire. Acta Odontol Scand. (1972) ; 30: (6): 597-613. doi: 10.3109/00016357209019791. |
[83] | Schiffman EL, Fricton JR, Haley DP, Shapiro BL. The prevalence and treatment needs of subjects with temporomandibular disorders. J Am Dent Assoc. (1990) ; 120: (3): 295-303. doi: 10.14219/jada.archive.1990.0059. |
[84] | Sanders B. Arthroscopic surgery of the temporomandibular joint: Treatment of internal derangement with persistent closed lock. Oral Surg Oral Med Oral Pathol. (1986) ; 62: (4): 361-372. doi: 10.1016/0030-4220(86)90282-3. |
[85] | Thilander B, Rubio G, Pena L, de Mayorga C. Prevalence of temporomandibular dysfunction and its association with malocclusion in children and adolescents: An epidemiologic study related to specified stages of dental development. Angle Orthod. (2002) ; 72: (2): 146-154. doi: 10.1043/0003-3219 (2002)072<0146:POTDAI>2.0.CO;2. |
[86] | Arnett GW, Milam SB, Gottesman L. Progressive mandibular retrusion-idiopathic condylar resorption. Part II. Am J Orthod Dentofacial Orthop. (1996) ; 110: (2): 117-127. doi: 10.1016/s0889-5406(96)70099-9. |
[87] | Carlsson GE. Epidemiology and treatment need for temporomandibular disorders. J Orofac Pain. (1999) ; 13: (4): 232-237. |
[88] | Van Eck NJ, Waltman L. Visualizing bibliometric networks. In: Ding Y, Rousseau R, Wolfram D, editors. Measuring Scholarly Impact. Cham, Switzerland: Springer; (2014) ; pp. 285-320. |
[89] | Livas C, Delli K. Journal self-citation rates and impact factors in dentistry, oral surgery, and medicine: A 3-year bibliometric analysis. J Evid Based Dent Pract. (2018) ; 18: (4): 269-274. doi: 10.1016/j.jebdp.2017.09.001. |
[90] | Ioannidis JPA, Baas J, Klavans R, et al. A standardized citation metrics author database annotated for scientific field. PLoS Biol. (2019) ; 17: (8): e3000384. doi: 10.1371/journal.pbio.3000384. |
[91] | Waltman L, Van Eck NJ, Noyons ECM. A unified approach to mapping and clustering of bibliometric networks. J Inform. (2010) ; 4: : 629-35. |
[92] | Al-Sharaee Y, Al-Moraissi EA, Christidis N, Galvão EL, Falci SGM. Top 100 cited publications in the field of temporomandibular disorders: A bibliometric analysis. Front Oral Health. (2022) ; 3: : 864519. doi: 10.3389/froh.2022.864519. |




