Effectiveness of ischemic compression on myofascial trigger points in relieving neck pain: A systematic review and meta-analysis
Abstract
BACKGROUND:
Ischemic compression is widely used to clinically treat neck pain. However, no meta-analysis has been conducted to evaluate the effects of this process on neck pain.
OBJECTIVE:
This study aimed to evaluate the effects of ischemic compression on the myofascial trigger points for improving neck pain-related symptoms (mainly pain, joint mobility limitation and function limitation) and to compare ischemic compression with other therapies.
METHODS:
Electronic searches were conducted in PubMed, OVID, Web of Science, EBSCO, SCOUPS, Cochrane Library, PEDro, Wanfang, CNKI and Chinese VIP Database in June 2021. Only randomised controlled trials on the effects of ischemic compression on neck pain were included. The major outcomes were pain intensity, pressure pain threshold, pain-related disability and range of motion.
RESULTS:
Fifteen studies involving 725 participants were included. Significant differences were observed between ischemic compression and sham/no treatment group in pain intensity, pressure pain threshold and range of motion immediately and in the short term. Significant effect sizes of dry needling were observed over ischemic compression in terms of improving pain intensity (SMD
CONCLUSION:
Ischemic compression can be recommended in the immediate and short-term pain relief and increase in the pressure pain threshold and range of motion. Dry needling is superior to ischemic compression in relieving pain and improving pain-related disability and range of motion immediately after treatment.
1.Introduction
Neck pain is a prevalent symptom nowadays, and it may be closely related to office work and computer use [1, 2]. The prevalence of neck pain worldwide ranges from 16.7% to 75.1% of the global population [3]. According to the Global Burden of Disease Study [4], neck pain is one of the two major global contributors to disability, the other contributor being low back pain. Neck pain can be caused by a variety of factors, including tumour, fracture, radiculopathy and chronic rheumatic disease [5, 6]. In addition, muscle disorders have been proposed to be important factors in the development of neck pain [7, 8].
Myofascial trigger points (MTrPs) are tender nodules (3–6 mm) in the skeletal muscles that are discovered during palpatory examination [9]. Mechanical stimulation of MTrPs by rapid transverse pressure or needling could induce localised muscle jumping. Myofascial pain syndrome is characterized by MTrP-induced symptoms, including local/referred pain, stiffness and high sensitivity, and can occasionally cause a variety of conditions, such as dizziness, abdominal pain and dysmenorrhoea [10, 11]. Pain is the most prevalent clinical symptom of myofascial pain syndrome, and several strategies have been used to help ease the pain caused by MTrPs.
Ischemic compression is one of the most popular amongst these strategies due to its convenience, safety and good effects. In ischemic compression, the therapist gradually applied increasing pressure to the MTrPs until the onset of pressure or pain. The pressure was maintained until tension decreased, pain relieved or the treatment passed 1 min, whichever came first. At that time, the pressure was increased until discomfort was felt again. The therapist repeated this procedure approximately 3–4 times during a 90 s period [12]. Pressure could help reduce muscle tone and increase the local blood supply, thereby improving the peripheral ‘energy crisis’ [13]. Clinical research [14, 15] has shown that ischemic compression on MTrPs can improve neck pain. In a systematic review[16] that compared dry needling, ischemic compression and other therapies for improving neck pain-related symptoms, dry needling and ischemic compression had been found to be effective in reducing pain and increasing lateral flexion. However, a quantitative analysis on the effects of ischemic compression of MTrPs on neck pain-related symptoms has yet to be conducted, and whether ischemic compression is superior than other therapies in improving neck pain-related symptoms has yet to be determined.
Therefore, this systematic review and meta-analysis was aimed to quantitatively analyse clinical studies on the effects of ischemic compression on MTrPs for improving neck pain-related symptoms (pain, function limitation and joint mobility limitation) and to compare ischemic compression with other therapies.
2.Methods
The study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement and registered in the PROSPERO database (registration number: CRD42017071521).
2.1Search strategy
Two authors searched PubMed, OVID, Web of Science, EBSCO, SCOUPS, Cochrane Library, Physiotherapy Evidence Database (PEDro), Wanfang Database, China National Knowledge Infrastructure Databases and Chinese VIP Database from their inception to March 30, 2021. The following MeSH terms and/or keywords were used as the main search terms: trigger points, myofascial pain syndrome, neck pain, cervical pain, pressure release and ischemic compression. The reference lists of the identified studies in full text were also searched. An experienced librarian was involved in the entire search process. The details of the search strategy are shown in Supplement 1.
2.2Selection criteria
This meta-analysis only included randomised controlled trials (RCTs) of ischemic compression treatment for neck pain. The specific inclusion criteria were as follows: (1) adults with neck pain and had one or more MTrPs on the cervical muscles; (2) at least one group received ischemic compression treatment on the MTrPs by hand or instrument; (3) acceptable comparator with sham/no/other treatment; and (4) outcome assessments, including pain intensity, pressure pain threshold, pain-related disability or range of motion. The exclusion criteria were as follows: (1) neck pain due to trauma, fibromyalgia, whiplash, cervical disc prolapse, malignant disease or any other neurological and orthopaedic conditions; (2) studies were not published as journal articles; (3) studies were in non-clinical designs; and (4) ischemic compression was not the main treatment.
2.3Study selection and data extraction
After the search was completed, duplicate articles were removed based on their titles. Titles together with the abstracts were screened again to rule out studies with inappropriate research designs, interventions or outcomes. Afterwards, a full-text check was conducted in accordance with the inclusion criteria. The data were extracted in the order of study design, sample size, age, neck pain duration, interventions, outcome measures and measurement time in a standardised form. Two authors were involved in the study selection and data extraction. In case of a lack of agreement, a third author mediated the final decision.
2.4Evaluation of the risk of bias and methodological quality
RevMan 5.3 software [17] and the PEDro scale [18] were used to analyse the risk of bias and methodological quality of the studies included in the meta-analysis, respectively. Two authors were involved in this process, and a third author mediated, when necessary.
The evaluation of the risk of bias contained eight items, including random assortment, concealment of allocation, blinding of subjects/therapists/assessors, incomplete outcome, selective reporting and other biases. Each item was divided into three levels, namely, low, high and unclear risks, according to the Cochrane Collaboration’s tool [17]. The PEDro scale included 10 items that were evaluated as ‘yes’ or ‘no’. One point was given if an item was regarded as ‘yes’, and zero was assigned for ‘no’. A trial with a PEDro score of
2.5Level of evidence
Two authors judged the evidence level by using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach [19]. Evidence was evaluated as very low, low, moderate or high on the basis of the following items: risk of bias, inconsistency, imprecision, indirectness of evidence and publication bias. The quality of a subgroup/meta-analysis was considered as follows: high, no item was at serious risk; moderate, only one item included serious risk; low, two items included serious risk/one included very serious risk; and very low, more items included serious or very serious risk [20]. When a disagreement occurred in the assessment of the risk of bias and quality level, a third author adjudicated the disagreement.
2.6Data synthesis and analysis
Revman 5.3 software was used to process all the data. The outcomes included pain intensity, pressure pain threshold, pain-related disability and range of motion. A follow-up was regarded as immediate (
Outcomes, including sample size, means and standard deviations, were extracted for analysis. Data in the form of mid-range, mid-quartile range and/or median were converted to mean and standard deviation if necessary [22, 23]. The mean difference (MD) with a confidence interval (CI) of 95% was used to measure outcomes. The results were converted to standardised MD (SMD) when more than one instrument was used for the same outcome, and the results were considered large (
Heterogeneity between studies in each meta-analysis was analysed using the I
3.Results
3.1Included studies
A total of 801 articles were obtained from the seven English databases and three Chinese databases. 567 articles remained after the duplicates were removed. Thereafter, 523 articles were removed based on titles and/or abstracts, leaving 44 for full-article review. In this round of screening, 29 articles were excluded because of the following reasons: ischemic compression was not the main treatment (
Figure 1.
PRISMA flow diagram of the study.
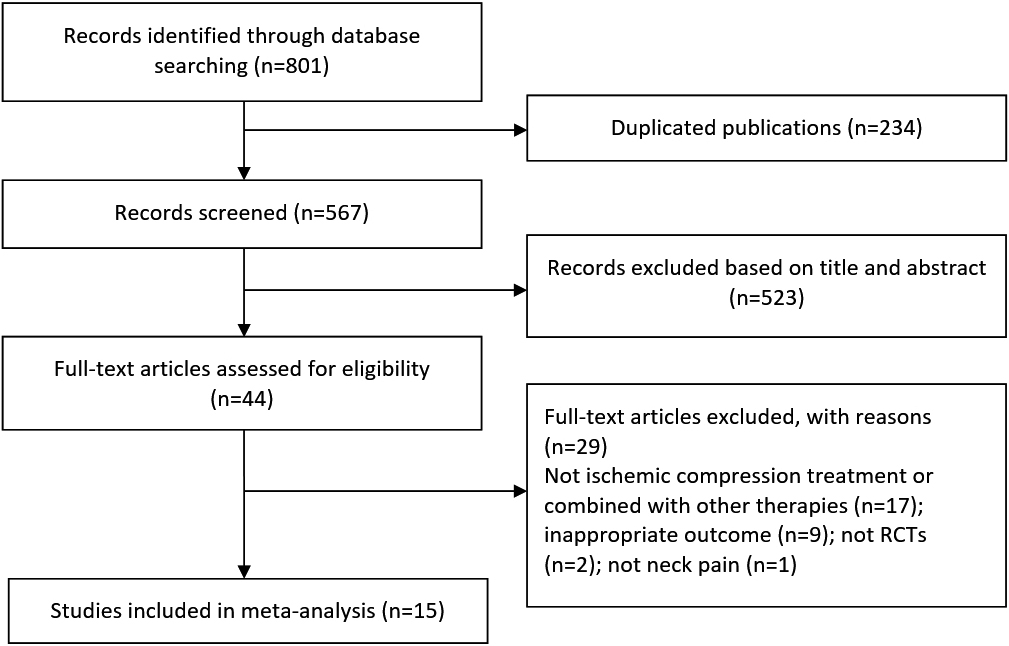
Figure 2.
Plot of the risk of bias of the included studies.

3.2Study characteristics
As shown in Table 1, all studies were RCTs published from 2006 to 2021. A total of 725 people were included, with the number of people in each study varying from 16 to 117. The frequency of treatment in each study ranged from once a week to every day. The duration of ischemic compression lasted from 1 week to 4 weeks,
Table 1
Characteristics of the included studies
| Study | Design | Sample size (M/F) | Age (y) | Duration of neck pain | IC treatment (frequency and times) | Comparison group (frequency and times) | Primary outcome measures | Measure time |
|---|---|---|---|---|---|---|---|---|
| Fernández-de-las-Peñas et al. (2006, Spain) [25] | RCT | Total: 40 (17/23) IC: 20 (8/12) TFM: 20 (9/11) | IC: 27.7 | Over 2 weeks | Once | Once | PPT VAS | Before treatment, immediately after treatment |
| Gemmell et al. (2008, UK) [26] | RCT | Total: 45 IC: 15 TPR: 15 Sham US: 15 | IC: 24 | Less than 3 months | Once | Once | PPT ROM VAS | Before treatment, immediately after treatment |
| Oliveira-Campelo et al. (2013, Spain) [27] | RCT | Total: 117 (32/85) IC: 24 (4/20) MET: 23 (7/16) PS: 23 (6/17) PL: 22 (8/14) WS: 25 (7/18) | IC: 20.08 | Not mentioned | Once | Once | PPT ROM VAS | Before treatment, 10 minutes/24 hours/1 week after treatment |
| Shah et al. (2015, India) [28] | RCT | Total: 30 (11/19) IC: 15 (5/10) MET:15 (6/9) | IC: 35.66 | Less than 3 months | Once/day for a week | Once/day for a week | PPT ROM VAS | Before treatment, immediately after whole treatment |
| Zheng et al. (2015, China) [29] | RCT | Total: 67 (29/38) IC: 34 (14/20) Physiotherapy: 33 (15/18) | IC: 39.74 | IC: 4.79 | 3 times/ week for 2 weeks | Once/day for 2 weeks | NDI VAS | Before treatment, immediately after whole treatment |
| Ganesh et al. (2016, India) [30] | RCT | Total: 90 (36/54) IC: 30 (13/17) Mobilization: 30 (14/16) Control: 30 (9/21) | IC: 22.06 | Not mentioned | Once/day for 5 days | Once/day for 5 days | PPT | Before treatment, immediately/24 hours/5 days/2 weeks after whole treatment |
| Kojidi et al. (2016, Iran) [31] | RCT | Total: 42 (0/42) IC: 14 (0/14) Active IC: 14 (0/14) Sham IC: 14 (0/14) | IC: 27.86 | Not mentioned | 3 times/ week for 1 week | 3 times/ week for 1 week | PPT ROM VAS | Before treatment, immediately/1 week after whole treatment |
| De Meulemeester et al. (2017, Belgium) [32] | RCT | Total: 38 (0/38) IC: 21 (0/21) DN: 17 (0/17) | IC: 40.5 | IC: < 3/3–12/> 12: 3/4/15 DN: < 3/3–12/> 12: 4/1/15 (months) | Once/week for 4 weeks | Once/week for 4 weeks | NDI NRS | Before treatment, after 1 |
| Kashyap et al. (2018, India) [33] | RCT | Total: 45 (0/45) IC: 15 (0/15) MET: 15 (0/15) WS: 15 (0/15) | IC: 21.27 | Not mentioned | Once/day for 5 days | Once/day for 5 days | NDI PPT VAS | Before treatment, after 1 |
| Ransone et al. (2019, America) [34] | RCT | Total: 30 (15/15) IC: 10 Sham IC: 10 Control: 10 | 22 | Not mentioned | 3 times/ week for 4 weeks | 3 times/ week for 4 weeks | PPT | After each treatment, take the mean value |
|
Table 1, continued | ||||||||
|---|---|---|---|---|---|---|---|---|
| Study | Design | Sample size (M/F) | Age (y) | Duration of neck pain | IC treatment (frequency and times) | Comparison group (frequency and times) | Primary outcome measures | Measure time |
| Tabatabaiee et al. (2019, Iran) [35] | RCT | Total: 60 (60/0) IC: 20 (20/0) PB: 20 (20/0) DN: 20 (20/0) | IC: 23.5 | Not mentioned | 3 times/ week for 2 weeks | PB: 3 times/week for 2 weeks DN: Twice/ week for 2 weeks | PPT ROM VAS | Before treatment, immediately after whole treatment |
| Ziaeifar et al. (2019, America) [36] | RCT | Total: 31 (0/31) IC: 15 (0/15) DN: 16 (0/16) | IC: 26.5 | Not mentioned | 3 times in 1 week | 3 times in 1 week | NPQ VAS | Before treatment, immediately/1 week/11 weeks after whole treatment |
| Arias-Buría et al. (2020, Spain) [37] | RCT | Total: 30 (21/9) IC: 15 (11/4) DN: 15 (10/5) | IC: 22 | IC: 8.0 | Once | Once | NRS NDI | Before treatment, one day/30 days after treatment |
| Nasb et al. (2020, China) [38] | RCT | Total: 16 (6/10) IC: 7 (3/4) Cupping: 9 (3/6) | IC: 33.1 | IC: 29.6 | Twice/week for 4 weeks | Twice/week for 4 weeks | NDI PPT | Before treatment, immediately after whole treatment |
| Stieven et al. (2021, Brazil) [39] | RCT | Total: 44 (13/31) IC: 14 (4/10) DN: 15 (5/10) Sham DN: 15 (4/11) | IC: 26.6 | Over 12 weeks | Once | Once | NRS PPT | Before treatment, Immediately/10 minutes after treatment |
DN, Dry needling; IC, Ischemic compression; MET, Muscle energy technique; NDI, Neck disability index; NPQ, Northwick Park neck pain questionnaire; NRS, Numeric rating scale; PB, Phonophoresis with betamethasone; PL, Placebo; PPT, Pressure pain threshold; PS, Passive stretching; RCT, Randomized controlled trial; ROM, Range of motion; TFM, Transverse friction massage; TPR, Trigger point pressure release; US, Ultrasound; VAS, Visual analog scale; WS, Wait and see.
with the total number of treatment sessions ranging from 1 to 14. The longest follow-up assessment was conducted in the third month after the last treatment, and all results were considered immediate (
Of the 15 studies, 12 studies [25, 26, 27, 28, 29, 31, 32, 33, 35, 36, 37, 39] used a visual analogue scale or a numeric rating scale to assess the pain intensity, and 11 studies [25, 26, 27, 28, 30, 31, 33, 34, 35, 38, 39] utilized the pressure pain threshold to measure the sensitivity of the MTrP-area. Six studies [29, 32, 33, 36, 37, 38] assessed the pain-related disability by using the Neck Disability Index (NDI) or the Northwick Park neck pain questionnaire (NPQ). Five studies [26, 27, 28, 31, 35] used the contralateral lateral flexion angle to measure the neck mobility.
3.3Risk of bias and methodological quality
Figure 2 shows the results of the risk of bias. Fourteen studies [25, 26, 27, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39]met the criteria of random allocation of participants, but six studies [25, 28, 33, 34, 35, 36] were at unclear risk in concealing the allocation. Only one study [31] was able to blind participants, and eight [28, 29, 31, 33, 34, 35, 36, 38] failed in assessor blinding. None of the studies was able to blind therapists during treatment. Table 2 shows the methodological score of the included studies. The numerical value of the methodological score ranged from five to nine (mean: 7.3, SD: 1.5) out of 10 points. Thirteen studies were regarded as high quality (
Table 2
PEDro score of included studies
| Study | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Fernández-de-las-Peñas et al. 2006 [25] | Y | N | Y | N | N | Y | Y | Y | Y | Y | 7 |
| Gemmell et al. 2008 [26] | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8 |
| Oliveira-Campelo et al. 2013 [27] | Y | Y | N | N | N | Y | N | N | Y | Y | 5 |
| Shah et al. 2015 [28] | N | N | Y | N | N | N | Y | N | Y | Y | 4 |
| Zheng et al. 2015 [29] | Y | Y | N | N | N | N | Y | N | Y | Y | 5 |
| Ganesh et al. 2016 [30] | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8 |
| Kojidi et al. 2016 [31] | Y | Y | Y | Y | N | N | Y | N | Y | Y | 7 |
| De Meulemeester et al. 2017 [32] | Y | Y | Y | N | N | Y | Y | N | Y | Y | 7 |
| Kashyap et al. 2018 [33] | Y | N | Y | N | N | N | Y | N | Y | Y | 5 |
| Ransone et al. 2019 [34] | Y | N | N | N | N | N | Y | N | Y | Y | 4 |
| Tabatabaiee et al. 2019 [35] | Y | N | Y | N | N | N | Y | N | Y | Y | 5 |
| Ziaeifar et al. 2019 [36] | Y | N | Y | N | N | N | Y | N | Y | Y | 5 |
| Arias-Buría et al. 2020 [37] | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8 |
| Nasb et al. 2020 [38] | Y | Y | Y | N | N | N | Y | N | Y | Y | 6 |
| Stieven et al. 2021 [39] | Y | Y | Y | N | N | Y | Y | N | Y | Y | 7 |
(1) Random Allocation; (2) Allocation Concealment; (3) Baseline Similarity; (4) Participant Blinding; (5) Therapist Blinding; (6) Assessor Blinding; (7) Dropouts Fewer than 15%; (8) Intention-to-Treat Analysis; (9) Between-Group Comparisons; (10) Point Measures and Variability Data. Y: Yes; N: No.
3.4Effects of ischemic compression on the neck pain intensity
The results of the meta-analysis demonstrated that ischemic compression exhibited no significant overall effect on relieving pain immediately after treatment (SMD
Figure 3.
Comparison between the effects of ischemic compression versus comparative groups on pain intensity in the (A) immediate and (B) short terms.
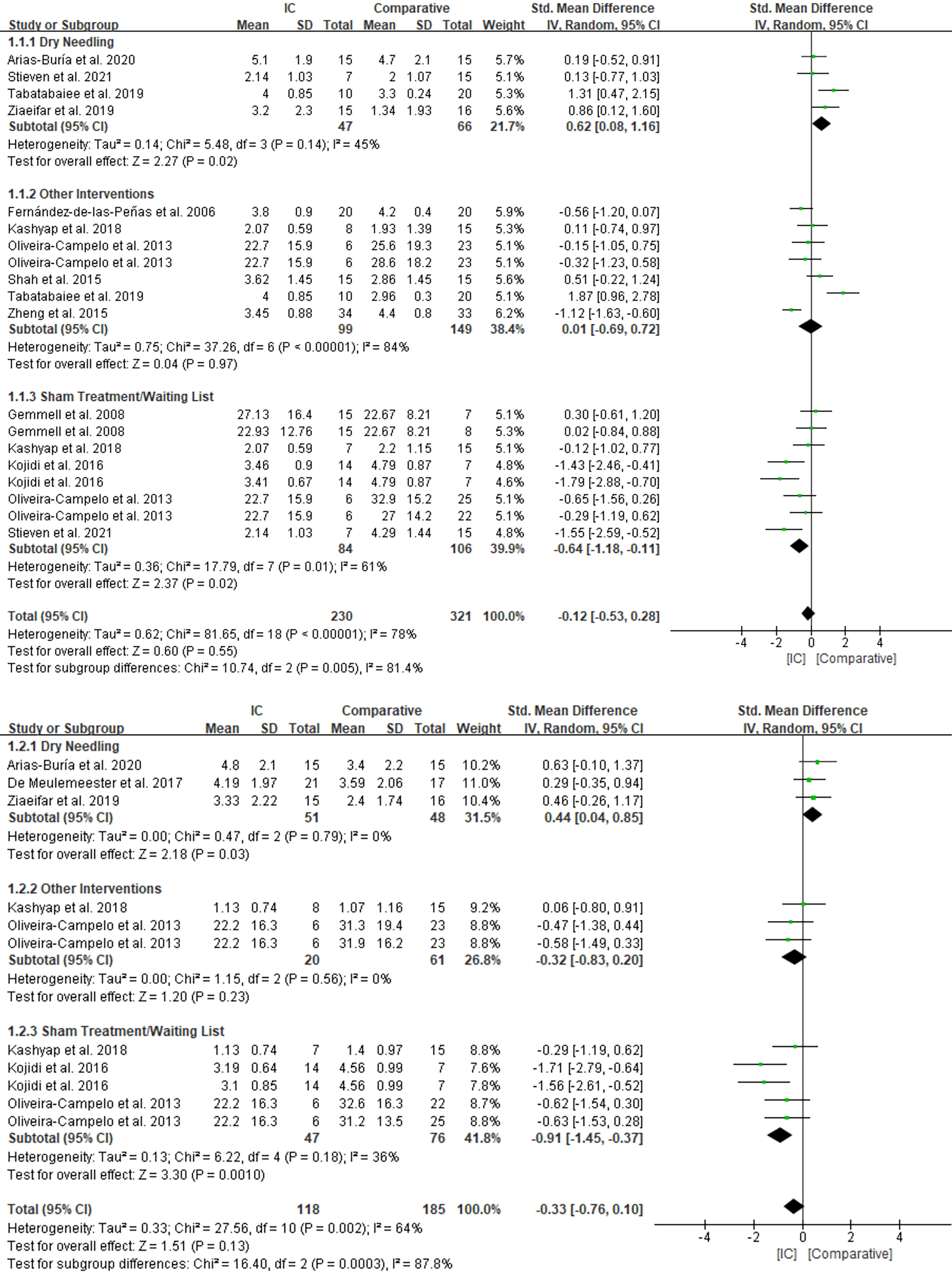
The meta-analysis revealed that ischemic compression did not demonstrate overall superiority in the short-term relief of pain and substantial heterogeneity amongst studies (I
3.5Effects of ischemic compression on the pressure pain threshold
The results revealed no significant overall effect of ischemic compression for the immediate improvement of the pressure pain threshold compared with those of the comparative groups (SMD
Figure 4.
Comparison between the effects of ischemic compression versus comparative groups on pressure pain threshold in the (A) immediate and (B) short terms.
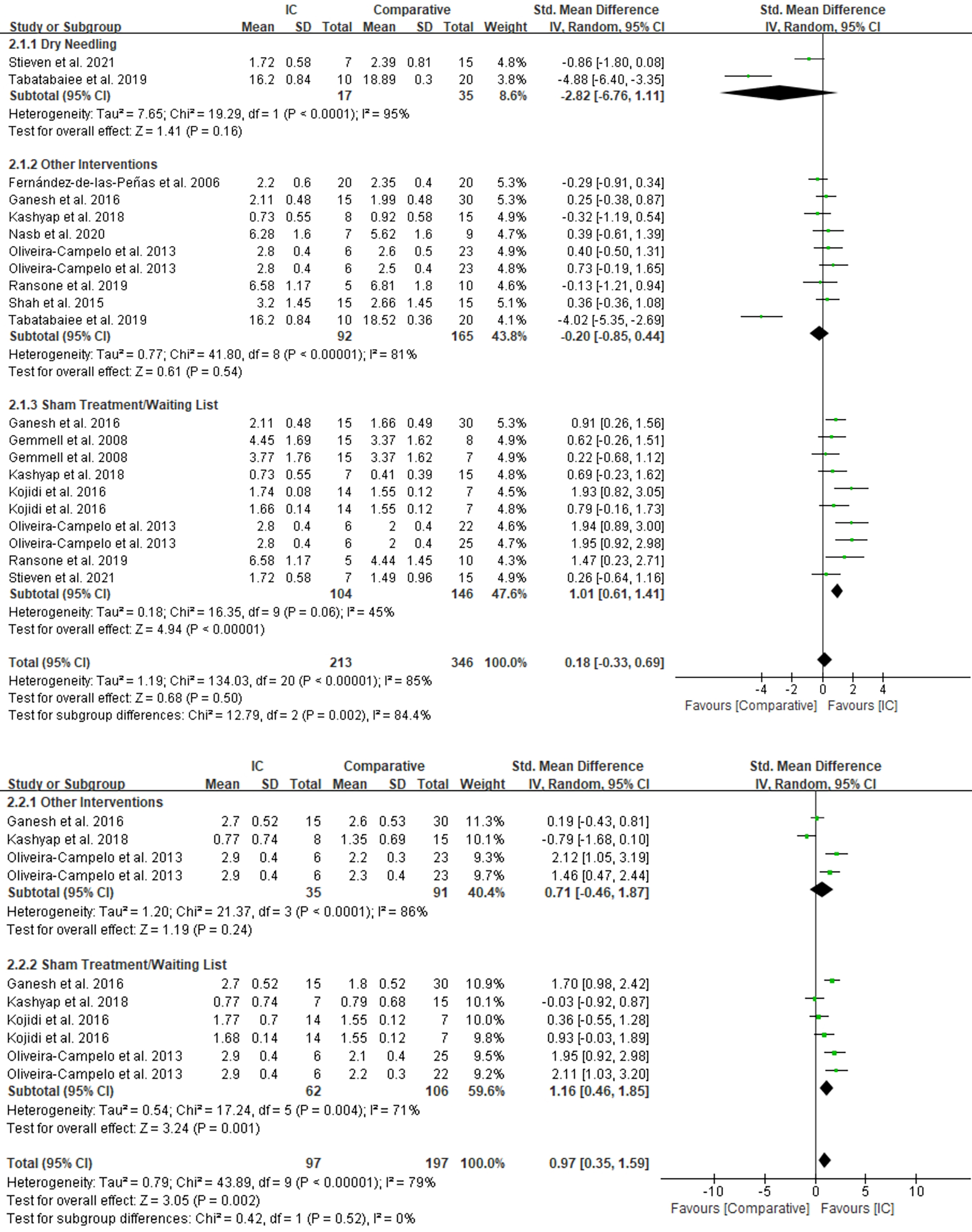
A large significant difference was found between the ischemic compression and comparative groups in the short-term improvement of the pressure pain threshold (SMD
3.6Effects of ischemic compression on the pain-related disability
Ischemic compression exhibited no significant overall effect in the immediate improvement in the NDI/NPQ when compared with the comparative groups (SMD
Figure 5.
Comparison between the effects of ischemic compression versus comparative groups on pain-related disability in the (A) immediate and (B) short terms.
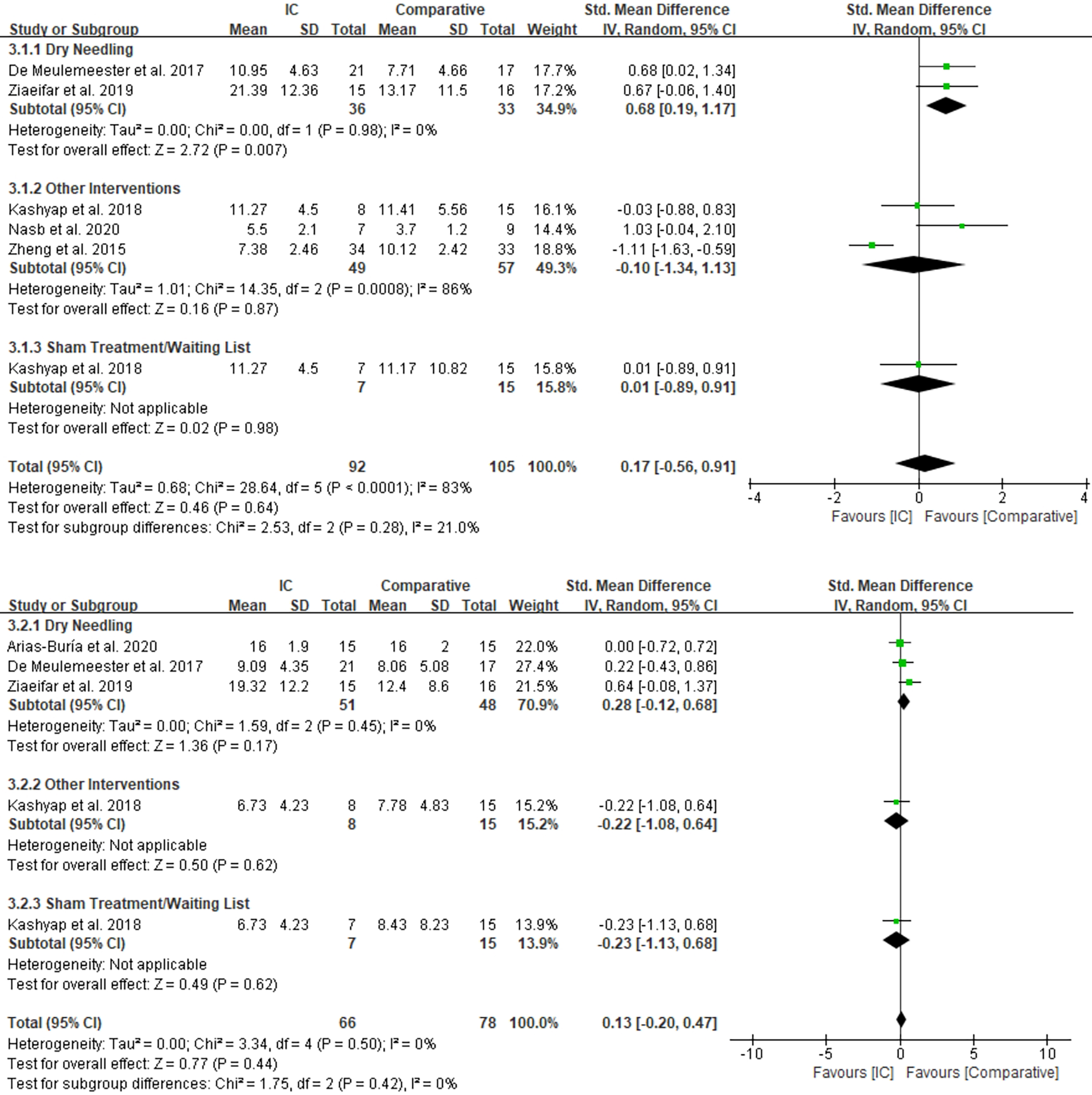
No significant difference was found between the ischemic compression and the comparative groups (SMD
3.7Effects of ischemic compression on the range of motion (contralateral lateral flexion)
Ischemic compression demonstrated no significant overall difference on immediately improving the range of motion compared with that of the comparative groups (MD
In comparison with the comparative groups, ischemic compression demonstrated better overall effects in the short-term improvement of the range of motion (MD
3.8Sensitivity analysis
Sensitivity analysis were performed to explore the source of high heterogeneity in some subgroups. The results revealed that the heterogeneity of the other intervention subgroup in the immediate pain intensity meta-analysis was reduced to low level (I
3.9Quality of evidence (GRADE)
The evidence level according to GRADE ranged from very low to moderate, and a high level of evidence was not observed. Table 3 displays the details of the GRADE assessment.
Table 3
GRADE evidence profile for ischemic compression on pain intensity, pressure pain threshold, pain-related disability and cervical range of motion in patients with neck pain
| Number of studies | Risk of bias | Inconsistency | Indirectness of evidence | Imprecision | Publication bias | Quality of evidence | SMD/MD (95% CI) |
| Ischemic compression vs. dry needling vs. other therapies vs. sham treatment/waiting list on pain intensity | |||||||
| Immediate follow-up (less than 1 week after treatment) | |||||||
| Overall effect | Serious | Serious (I | No | Serious | No | Very low | |
| Dry needling | Serious | Serious (I | No | Serious | No | Very low | 0.62 [0.08, 1.16] |
| Other therapies | Serious | Very serious (I | No | Serious | Yes | Very low | 0.01 [ |
| Sham/placebo/waiting list | Serious | Serious (I | No | Serious | Yes | Very low | |
| Short-term follow-up (1–12 weeks after treatment) | |||||||
| Overall effect | Serious | Serious (I | No | Serious | Yes | Very low | |
| Dry needling | No | No (I | No | Serious | No | Moderate | 0.44 [0.04, 0.85] |
| Other therapies | Serious | No (I | No | Very serious | No | Very low | |
| Sham/placebo/waiting list | Serious | No (I | No | Serious | Yes | Very low | |
| Ischemic compression vs. dry needling vs. other therapies vs. sham treatment/waiting list on pressure pain threshold | |||||||
| Immediate follow-up (less than 1 week after treatment) | |||||||
| Overall effect | Serious | Very serious (I | No | Serious | No | Very low | 0.18 [ |
| Dry needling | No | Very serious (I | No | Very serious | No | Very low | |
| Other therapies | Serious | Very serious (I | No | Serious | No | Very low | |
| Sham/placebo/waiting list | Serious | Serious (I | No | Serious | No | Very low | 1.01 [0.61, 1.41] |
| Short-term follow-up (1–12 weeks after treatment) | |||||||
| Overall effect | Serious | Serious (I | No | No | No | Low | 0.97 [0.35, 1.59] |
| Other therapies | Serious | Very serious (I | No | Very serious | No | Very low | 0.71 [ |
| Sham/placebo/waiting list | Serious | Serious (I | No | Serious | No | Very low | 1.16 [0.46, 1.85] |
| Ischemic compression vs. dry needling vs. other therapies vs. sham treatment/waiting list on pain-related disability | |||||||
| Immediate follow-up (less than 1 week after treatment) | |||||||
| Overall effect | Serious | Very serious (I | No | Very serious | No | Very low | 0.17 [ |
| Dry needling | Serious | No (I | No | Serious | No | Low | 0.68 [0.19, 1.17] |
| Other therapies | Serious | Very serious (I | No | Very serious | No | Very low | |
| Sham/placebo/waiting list | Serious | No (N/A) | No | Very serious | No | Very low | 0.01 [ |
| Short-term follow-up (1–12 weeks after treatment) | |||||||
| Overall effect | Serious | No (I | No | Very serious | No | Very low | 0.13 [ |
| Dry needling | Serious | No (I | No | Very serious | No | Very low | 0.28 [ |
| Other therapies | Serious | No (N/A) | No | Very serious | No | Very low | |
| Sham/placebo/waiting list | Serious | No (N/A) | No | Very serious | No | Very low | |
| Ischemic compression vs. dry needling vs. other therapies vs. sham treatment/waiting list on cervical range of motion | |||||||
| Immediate follow-up (less than 1 week after treatment) | |||||||
| Overall effect | Serious | Serious (I | No | Very serious | Yes | Very low | |
| Dry needling | No | No (N/A) | No | Very serious | No | Low | |
| Other therapies | Serious | Serious (I | No | Very serious | Yes | Very low | |
| Sham/placebo/waiting list | Serious | No (I | No | Very serious | Yes | Very low | 4.23 [1.99, 6.48] |
| Short-term follow-up (1–12 weeks after treatment) | |||||||
| Overall effect | Serious | No (I | No | Serious | Yes | Very low | 4.98 [2.57, 7.38] |
| Other therapies | Serious | No (I | No | Very serious | No | Very low | 3.23 [ |
| Sham/placebo/waiting list | Serious | Serious (I | No | Serious | Yes | Very low | 5.78 [2.63, 8.92] |
4.Discussion
This study was performed to explore the effects of ischemic compression against other therapies and sham/no treatment in reducing neck pain-related symptoms. According to the pooled results, ischemic compression was superior to sham treatment/waiting list in the immediate and short-term improvement of the pain intensity, pressure pain threshold and range of motion. Dry needling had better immediate effects than ischemic compression in improving the pain intensity, pain-related disability and range of motion. Dry needling was also superior to ischemic compression in the short-term improvement of pain intensity. High risk of bias and imprecision were found during quality assessments, which resulted in the low-GRADE score.
Sustained and deep force at the MTrPs during ischemic compression could relieve muscle tension and increase blood flow in the MTrP-area, and these actions could mitigate energy crisis and reduce pain [12, 13, 40]. A systematic review [16] of RCTs has explored the effects of ischemic compression on neck pain conditions, and ischemic compression was proven to be effective in relieving neck pain-related conditions, including pain intensity, pressure pain threshold, pain-related disability and range of motion. The current meta-analysis obtained similar results in pain intensity, pressure pain threshold and range of motion, whilst no significant difference was found between ischemic compression and sham treatment/waiting list in the pain-related disability. The results of the pain-related disability meta-analysis should be treated with caution because only one study [33] is involved in related subgroups, which may result in inaccurate results. In this study, all patients received quite a few conventional exercises at home, except for the corresponding treatment in each group. Accordingly, little difference was found amongst the three groups in all outcomes. In another systematic review about shoulder pain, ischemic compression was proven to be effective in relieving functional disability [41].
Apart from ischemic compression, some other methods are also used to treat neck pain in clinic. In our meta-analysis, ischemic compression and other therapies (except dry needling) had no remarkable differences in most indices. The results are reasonable because some totally different therapies were included in the same subgroup. For example, in the meta-analysis comparing the immediate effect of pain intensity, ultrasound drug penetration therapy [35] and thermomagnetic therapy [29] belong to the same subgroup. However, the treatment methods and principles of the two therapies are different, which may result in great differences in the comparison with ischemic compression: the former is significantly better than ischemic compression, whilst the thermomagnetic therapy in the same subgroup is not as good as ischemic compression. Compared with other therapies, our results favour ischemic compression more in the short term than in the immediate term. Hence, ischemic compression may be more stable in improving neck pain-related symptoms. The results were verified by the studies of Oliveira-Campelo et al. [27] and Benito-de-Pedro et al. [42], in which ischemic compression could maintain the effect size better than the other treatment methods.
Dry needling is another therapeutic intervention that involves inserting a solid filiform needle directly into the MTrPs. The needle is moved up and down to provoke a local twitch response, which was elicited for successful therapy [43]. The previous study [16] has proven that ischemic compression and dry needling are effective in improving neck pain intensity, pain-related disability and range of motion. Moreover, the study showed that dry needling has a higher evidence level than ischemic compression in some indices, but no specific comparison was made between these two therapies. Our results revealed that dry needling was superior to ischemic compression in improving pain intensity, pain-related disability and range of motion immediately after treatment. Nonetheless, the differences between the two therapies in most subgroups in the short term were not remarkable. One probable reason could be that the therapeutic effects of dry needling rapidly decreased over time. In a previous meta-analysis [44], dry needling showed considerable advantages over the control group in improving pain intensity and pressure pain threshold within 12 weeks. However, no remarkable difference was found in the long-term comparison. In the study of Navarro-Santana et al. [21], dry needling apparently showed better effects in improving pain intensity within a period of 1–12 weeks compared with manual therapies, including ischemic compression. Nevertheless, the difference decreased when the follow-up was longer than 3 months. The small number of studies may be another reason for the differences between the immediate and the short-term comparisons. In particular, only one study conducted short-term comparisons in some subgroups, resulting in imprecise results.
Some outcomes have a considerable degree of heterogeneity. Sensitivity analysis was conducted to find the main source of heterogeneity, and the main causes can be summarised as the follows: Firstly, although subgroups analysis was made to reduce the variations amongst different groups, therapies still widely vary in the other intervention subgroup. Different treatment methods and mechanisms could be the main sources of heterogeneity in this subgroup. Secondly, the level of neck pain varied amongst studies. Although active and latent trigger points were included in most studies, only patients with latent trigger points were included in the study of Tabatabaiee et al. [35], and the pressure pain threshold was much higher than those of other studies. Thirdly, the dosage (number and duration) during treatment is different. For example, the study of Kojidi [31] and others, which was the main source of heterogeneity, had a longer treatment duration of ischemic compression than other studies in the sham treatment/waiting list subgroup of pressure pain threshold meta-analysis in the immediate term.
This study has some potential limitations. Firstly, as previously mentioned, the operations of ischemic compression used in different studies were heterogeneous in terms of the duration and total number of treatments. Differences in operation could result in distinct therapeutic effects. For example, a study [45] found that 60 and 90 s of ischemic compression have better effects than 30 s of ischemic compression. Secondly, the number of studies was not adequate in some comparisons, especially in the analysis of pain-related disability and the short-term comparisons of all indices. This factor could be one of the main reasons for the heterogeneity and imprecision of the results. Additionally, only studies in Chinese and English were included, indicating that some high-quality studies in other languages could have been missed.
5.Conclusions
This systematic review and meta-analysis shows that ischemic compression was effective in relieving pain and increasing the threshold of pressure pain and range of motion for patients with neck pain immediately and in the short-term. Meanwhile, dry needling is better in relieving pain and pain-related disability and increasing the range of motion in the immediate term. Therefore, clinicians are advised to use ischemic compression and dry needling to release neck pain-related symptoms. The results should be treated with caution due to the high heterogeneity within subgroups and the low-quality level in most subgroups. Moreover, the lack of research in the short-term comparison could also affect the accuracy of the results. Additional high-quality clinical studies with large sample sizes are needed to explore the long-term effects of ischemic compression and its effects on neck pain-related symptoms.
Ethical approval
Not applicable.
Funding
This work was supported by the National Natural Science Foundation of China (Grant no. 81470105) and the Shanghai Municipal Health Commission Scientific Research Project (Grant no. 202040023).
Informed consent
Not applicable.
Author contributions
A.X. and J.R. conceived the idea of the study. A.X., Q.H. and J.R. designed the study. A.X. wrote the manuscript. All authors were involved in conducting the study, analyzing the data and revising the manuscript. All authors read and approved the final manuscript.
Supplementary data
The supplementary files are available to download from http://dx.doi.org/10.3233/BMR-220045.
Acknowledgments
None to report.
Conflict of interest
The authors confirm that this is an original article and there are not any conflicts of interest.
References
[1] | Paksaichol A, Lawsirirat C, Janwantanakul P. Contribution of biopsychosocial risk factors to nonspecific neck pain in office workers: A path analysis model. J Occup Health. (2015) ; 57: (2): 100-9. |
[2] | Leroux I, Dionne CE, Bourbonnais R, Brisson C. Prevalence of musculoskeletal pain and associated factors in the Quebec working population. Int Arch Occup Environ Health. (2005) ; 78: (5): 379-86. |
[3] | Fejer R, Kyvik KO, Hartvigsen J. The prevalence of neck pain in the world population: A systematic critical review of the literature. Eur Spine J. (2006) ; 15: (6): 834-48. |
[4] | Vos T, Allen C, Arora M, Barber RM, Bhutta ZA, Brown A, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015. Lancet. (2016) ; 388: : 1545-1602. |
[5] | Falco FJ, Erhart S, Wargo BW, Bryce DA, Atluri S, Datta S, et al. Systematic review of diagnostic utility and therapeutic effectiveness of cervical facet joint interventions. Pain Physician. (2009) ; 12: (2): 323-44. |
[6] | Ambrose NL, Cunnane G. Importance of full evaluation in patients who complain of neck pain. Ir J Med Sci. (2009) ; 178: (2): 209-10. |
[7] | Fougeront N, Fleiter B. Temporomandibular disorder and comorbid neck pain: Facts and hypotheses regarding pain-induced and rehabilitation-induced motor activity changes. Can J Physiol Pharmacol. (2018) ; 96: (11): 1051-9. |
[8] | Yahia A, Ghroubi S, Jribi S, Mâlla J, Baklouti S, Ghorbel A, et al. Chronic neck pain and vertigo: Is a true balance disorder present? Ann Phys Rehabil Med. (2009) ; 52: (7-8): 556-67. |
[9] | Simons DG. New views of myofascial trigger points: Etiology and diagnosis. Arch Phys Med Rehabil. (2008) ; 89: (1): 157-9. |
[10] | Hubbard JE. Myofascial trigger points. What physicians should know about these neurological imitators. Minn Med. (2010) ; 93: (5): 42-5. |
[11] | Yacubovich Y, Cohen N, Tene L, Kalichman L. The prevalence of primary dysmenorrhea among students and its association with musculoskeletal and myofascial pain. J Bodyw Mov Ther. (2019) ; 23: (4): 785-91. |
[12] | Simons DG, Travell JG, Simons LS. Travell & Simons’ Myofascial Pain and Dysfunction: The Trigger Point Manual. Philadelphia: Williams & Wilkins; (1999) . |
[13] | Bialosky JE, Bishop MD, Price DD, Robinson ME, George SZ. The mechanisms of manual therapy in the treatment of musculoskeletal pain: A comprehensive model. Manual Ther. (2009) ; 14: (5): 531-8. |
[14] | Abu TW, Rehan YA, Saleh A. The effectiveness of manual versus algometer pressure release techniques for treating active myofascial trigger points of the upper trapezius. J Bodyw Mov Ther. (2016) ; 20: (4): 863-9. |
[15] | Aguilera FJ, Martín DP, Masanet RA, Botella AC, Soler LB, Morell FB. Immediate effect of ultrasound and ischemic compression techniques for the treatment of trapezius latent myofascial trigger points in healthy subjects: A randomized controlled study. J Manipulative Physiol Ther. (2009) ; 32: (7): 515-20. |
[16] | Cagnie B, Castelein B, Pollie F, Steelant L, Verhoeyen H, Cools A. Evidence for the use of ischemic compression and dry needling in the management of trigger points of the upper trapezius in patients with neck pain: A systematic review. Am J Phys Med Rehabil. (2015) ; 94: (7): 573-83. |
[17] | Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al. Cochrane Handbook for Systematic Reviews of Interventions. 2nd Edition, vol 9. Chichester (UK): John Wiley & Sons; (2019) . doi: 10.1007/s00586-017-5121-8. |
[18] | Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. (2003) ; 83: (8): 713-21. |
[19] | Schünemann HJ, Oxman AD, Brozek J, Glasziou P, Bossuyt P, Chang S, et al. GRADE: Assessing the quality of evidence for diagnostic recommendations. ACP J Club. (2008) ; 149: (6): 2. |
[20] | Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. (2011) ; 64: (4): 401-6. |
[21] | Navarro-Santana MJ, Sanchez-Infante J, Fernández-de-Las-Peñas C, Cleland JA, Martín-Casas P, Plaza-Manzano G. Effectiveness of dry needling for myofascial trigger points associated with neck pain symptoms: An updated systematic review and meta-analysis. J Clin Med. (2020) ; 9: (10). doi: 10.3390/jcm9103300. |
[22] | Donner A, Piaggio G, Villar J. Statistical methods for the meta-analysis of cluster randomization trials. Stat Methods Med Res. (2001) ; 10: (5): 325-38. |
[23] | Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. (2018) ; 27: (6): 1785-805. |
[24] | Sullivan GM, Feinn R. Using effect size-or why the p value is not enough. J Grad Med Educ. (2012) ; 4: (3): 279-82. |
[25] | Fernández-de-las-Peñas C, Alonso-Blanco C, Fernández-Carnero J, Carlos Miangolarra-Page J. The immediate effect of ischemic compression technique and transverse friction massage on tenderness of active and latent myofascial trigger points: A pilot study. J Bodyw Mov Ther. (2006) ; 10: (1): 3-9. |
[26] | Gemmell H, Miller P, Nordstrom H. Immediate effect of ischaemic compression and trigger point pressure release on neck pain and upper trapezius trigger points: A randomised controlled trial. Clin Chiropr. (2008) ; 11: (1): 30-6. |
[27] | Oliveira-Campelo NM, de Melo CA, Alburquerque-Sendín F, Machado JP. Short- and medium-term effects of manual therapy on cervical active range of motion and pressure pain sensitivity in latent myofascial pain of the upper trapezius muscle: a randomized controlled trial. J Manipulative Physiol Ther. (2013) ; 36: (5): 300-9. |
[28] | Shah NA, Shah N. Comparison of two treatment techniques: Muscle energy technique and ischemic compression on upper trapezius trigger point in subjects with non-specific neck pain. Int J Therap Rehabil Res. (2015) ; 4: (5): 260-4. |
[29] | Zheng ZX, Gao Q, Shu D, Zhao D, Lu Y, Zhou P. Efficacy of ischemic compression technique on myofascial pain syndrome of neck and shoulder. Acad J Chin PLA Med Sch. (2015) ; (09): 908-10. |
[30] | Ganesh GS, Singh H, Mushtaq S, Mohanty P, Pattnaik M. Effect of cervical mobilization and ischemic compression therapy on contralateral cervical side flexion and pressure pain threshold in latent upper trapezius trigger points. J Bodyw Mov Ther. (2016) ; 20: (3): 477-83. |
[31] | Kojidi MM, Okhovatian F, Rahimi A, Baghban AA, Azimi H. Comparison between the effects of passive and active soft tissue therapies on latent trigger points of upper trapezius muscle in women: Single-blind, randomized clinical trial. J Chiropr Med. (2016) ; 15: (4): 235-42. |
[32] | De Meulemeester KE, Castelein B, Coppieters I, Barbe T, Cools A, Cagnie B. Comparing trigger point dry needling and manual pressure technique for the management of myofascial neck/shoulder pain: A randomized clinical trial. J Manipulative Physiol Ther. (2017) ; 40: (1): 11-20. |
[33] | Kashyap R, Iqbal A, Alghadir AH. Controlled intervention to compare the efficacies of manual pressure release and the muscle energy technique for treating mechanical neck pain due to upper trapezius trigger points. J Pain Res. (2018) ; 11: : 3151-60. |
[34] | Ransone JW, Schmidt J, Crawford SK, Walker J. Effect of manual compressive therapy on latent myofascial trigger point pressure pain thresholds. J Bodyw Mov Ther. (2019) ; 23: (4): 792-8. |
[35] | Tabatabaiee A, Ebrahimi-Takamjani I, Ahmadi A, Sarrafzadeh J, Emrani A. Comparison of pressure release, phonophoresis and dry needling in treatment of latent myofascial trigger point of upper trapezius muscle. J Back Musculoskelet Rehabil. (2019) ; 32: (4): 587-94. |
[36] | Ziaeifar M, Arab AM, Mosallanezhad Z, Nourbakhsh MR. Dry needling versus trigger point compression of the upper trapezius: A randomized clinical trial with two-week and three-month follow-up. J Man Manip Ther. (2019) ; 27: (3): 152-61. |
[37] | Arias-Buría JL, Monroy-Acevedo Á, Fernández-de-Las-Peñas C, Gallego-Sendarrubias GM, Ortega-Santiago R, Plaza-Manzano G. Effects of dry needling of active trigger points in the scalene muscles in individuals with mechanical neck pain: A randomized clinical trial. Acupunct Med. (2020) ; 38: (6): 380-7. |
[38] | Nasb M, Qun X, Ruckmal WC, Lingfeng X, Hong C. Dry cupping, ischemic compression, or their combination for the treatment of trigger points: A pilot randomized trial. J Altern Complement Med. (2020) ; 26: (1): 44-50. |
[39] | Stieven FF, Ferreira GE, de Araújo FX, Angellos RF, Silva MF, Da RL. Immediate effects of dry needling and myofascial release on local and widespread pressure pain threshold in individuals with active upper trapezius trigger points: A randomized clinical trial. J Manipulative Physiol Ther. (2021) ; 44: (2): 95-102. |
[40] | Moraska AF, Hickner RC, Kohrt WM, Brewer A. Changes in blood flow and cellular metabolism at a myofascial trigger point with trigger point release (ischemic compression): A proof-of-principle pilot study. Arch Phys Med Rehabil. (2013) ; 94: (1): 196-200. |
[41] | Da SA, De Noronha M, Liberatori-Junior RM, et al. The effectiveness of ischemic compression technique on pain and function in individuals with shoulder pain: A systematic review. J Manipulative Physiol Ther. (2020) ; 43: (3): 234-246. |
[42] | Benito-de-Pedro M, Becerro-de-Bengoa-Vallejo R, Losa-Iglesias ME, et al. Effectiveness between dry needling and ischemic compression in the triceps surae latent myofascial trigger points of triathletes on pressure pain threshold and thermography: A single blinded randomized clinical trial. J Clin Med. (2019) ; 8: (10). |
[43] | Dunning J, Butts R, Mourad F, Young I, Flannagan S, Perreault T. Dry needling: A literature review with implications for clinical practice guidelines. Phys Ther Rev. (2014) ; 19: (4): 252-265. |
[44] | Gattie E, Cleland JA, Snodgrass S. The effectiveness of trigger point dry needling for musculoskeletal conditions by physical therapists: A systematic review and meta-analysis. J Orthop Sports Phys Ther. (2017) ; 47: (3): 133-49. |
[45] | Pecos-Martin D, Ponce-Castro MJ, Jiménez-Rejano JJ, Nunez-Nagy S, Calvo-Lobo C, Gallego-Izquierdo T. Immediate effects of variable durations of pressure release technique on latent myofascial trigger points of the levator scapulae: A double-blinded randomised clinical trial. Acupunct Med. (2019) ; 37: (3): 141-50. |




