Efficacy of rehabilitation on reducing pain in muscle-related temporomandibular disorders: A systematic review and meta-analysis of randomized controlled trials
Abstract
BACKGROUND:
Patients with temporomandibular disorders (TMD) mostly suffer from muscle-related pain. Several conservative interventions have been suggested as treatments for TMD in the last years.
OBJECTIVE:
The aim of this systematic review with meta-analysis was to assess the efficacy of rehabilitative approaches in reducing pain in patients with muscle-related TMD.
METHODS:
PubMed, Scopus, and Web of Science were systematically searched from inception until April 28
RESULTS:
Out of 1997 papers suitable for title/abstract screening, 189 articles were assessed for eligibility. Sixteen RCTs were included and most of them (
CONCLUSION:
Findings of this systematic review with meta-analysis suggested that rehabilitative approaches might be effective in reducing pain in muscle-related TMD patients. However, the low number of RCTs evaluating conservative approaches might impair the synthesis of evidence regarding the different techniques, calling for caution in the interpretation of these results.
1.Introduction
Temporomandibular disorders (TMD) include several diseases involving masticatory muscles of the stomatognathic system, temporomandibular joint (TMJ), or both [1]. TMD have been accepted to have a multifactorial etiology [2], including as potential risk factors: a prolonged use of mastication muscles, grinding and clenching, malocclusion, repetitive trauma at the TMJ, psychological disorders (e.g. anxiety and depressive syndrome), and cervical posture [3, 4, 5, 6]. Moreover, it has been also hypothesized a correlation between TMD and the position of the cervical spine, albeit the potential differences in terms of skeletal maturation make this correlation still controversial [7, 8].
In this context, an adequate classification was considered as crucial to create a standard management of TMD. Thus, the Diagnostic Criteria for TMD (DC/TMD) were established by the International Research DC/TMD Consortium Network and the Orofacial Pain Special Interest Group [9]. According to DC/TMD, there is a dual-axis system for the diagnosis of TMD, consisting of: Axis I for the clinical examination, and Axis II for the assessment of pain-related disability. More in detail, DC/TMD Axis I includes: a) muscle disorders, including myofascial pain with and without mouth opening limitation; b) disc displacement with or without reduction or mouth opening limitation; c) arthralgia, arthritis, and arthrosis. DC/TMD Axis II evaluates relevant behavioral, psychological status, and psychosocial functioning (e.g., depression and somatization, pain status variables, and disability levels) [9].
Therefore, both myalgia and myofascial pain are considered as muscle-related disorders, according to the DC/TMD [9]. Local myalgia is characterized by pain localized to the area of palpation on examination. Myofascial pain originates in the muscle, as in myalgia, but it extends beyond the area identified by palpation. Referred myofascial pain is characterized by extension towards areas distant from the area identified in the examination and from the limits of the palpated muscle. Masseter and temporalis muscles are commonly associated with myofascial pain and considered as main causes of TMD [10]. However, it has been shown that around 85% of the general population has been shown to have at least one sign or symptom of myofascial pain, with an overall prevalence of approximately 46% [11, 12]. Myofascial pain could cause limitations in the activities of daily living with negative consequences in terms of mental well-being, work performance, and quality of life [13, 14].
The treatment of muscle-related pain in TMD commonly consisted of occlusal splint devices [15, 16], behavioral therapies [17], and other conservative non-pharmacological approaches such as manual therapy [18], acupuncture [19], laser therapy [20], transcutaneous electrical nerve stimulation (TENS) [21], and dry needling [22]. Conservative and physical therapies are recommended for the initial treatment of TMD, as they are considered effective in reducing painful symptoms and bringing comfort to the patient [23, 24]. Over the years, several systematic reviews have investigated the efficacy of different therapies for muscle-related pain in TMD [21, 25, 26, 27, 28, 29]. However, data resulted to be limited for specific techniques and not reproducible due to the lack of homogeneity in TMD classification, the combination of different therapies, and the absence of a placebo or sham treatment control group.
Thus, to the best of our knowledge, there is a lack of systematic reviews that have properly investigated the efficacy of conservative approaches in reducing muscle-related pain in TMD patients, comparing them to placebo or sham treatment. In this scenario, the treatment remains challenging for the multifactorial etiology, despite the wide number of therapeutic strategies.
Therefore, by means of the present systematic review and meta-analysis of randomized controlled trials (RCTs), we aimed to evaluate the efficacy of rehabilitative interventions in reducing pain in patients with muscle-related TMD.
2.Methods
2.1Search strategy
A Technical Expert Panel was established by 10 physicians (4 specialists in physical and rehabilitative medicine and 6 dentists) to propose a multidisciplinary approach for TMD patients. This panel defined the aim of this systematic review and proposed the search strategy.
PubMed, Scopus, and Web of Science databases were systematically searched for articles published from inception until April 28
Table 1
Search strategy
| PubMed (“temporomandibular disorders”) AND (“myofascial pain” OR “pain” OR “painful”) AND (“physiotherapy” OR “physical therapy” OR “electrical stimulation” OR “shock wave” OR “laser” OR “laser therapy” OR “splints” OR “acupuncture” OR “needling”) |
| Scopus TITLE-ABS-KEY(((“temporomandibular disorders”) AND (“myofascial pain” OR “pain” OR “painful”) AND (“physiotherapy” OR “physical therapy” OR “electrical stimulation” OR “shock wave” OR “laser” OR “laser therapy” OR “splints” OR “acupuncture” OR “needling”))) |
| Web of Science ((“temporomandibular disorders”) AND (“myofascial pain” OR “pain” OR “painful”) AND (“physiotherapy” OR “physical therapy” OR “electrical stimulation” OR “shock wave” OR “laser” OR “laser therapy” OR “splints” OR “acupuncture” OR “needling”)) |
This systematic review with meta-analysis was conducted according to the guidance of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [30] and the Cochrane Handbook for Systematic Reviews of Interventions [31]. The Institutional Review Board of the University of Eastern Piedmont approved the work (protocol number CE61/10,prot.392). The systematic review protocol was registered on the International Prospective Register of Systematic Reviews (PROSPERO) under number CRD42021251904.
2.2Eligibility criteria
All RCTs were assessed for eligibility according to the following patient/population, intervention, comparison, and outcomes (PICO) model:
P) Participants consisted of patients diagnosed with pain in muscle-related TMD with or without limitation of mouth opening according to the DC/TMD [9]; I) Intervention consisted of rehabilitative approa-ches aimed at pain reduction (e.g. physical therapy, TENS, laser therapy, occlusal splints, dry needling of trigger points, acupuncture, percutaneous needle electrolysis (PNE), ozone therapy, extracorporeal shockwave therapy (ESWT); C) Comparison consisted of placebo or sham treatments; O) Outcome measures consisted of pain intensity, using the visual analogue scale (VAS) [32] or the numerical rating scale (NRS) [33].
Two reviewers independently screened all potential articles for eligibility after duplication removal. Any disagreement were resolved through discussion or, if necessary, consultation with a third reviewer.
Only RCTs with a placebo or sham treatment control group, providing data at the end of the intervention (after 1 week later) were included.
The exclusion criteria were: children or adolescents during growth, patients with disc displacement, TMJ disorders, fibromyalgia, headache/migraine, pharmacological treatments as interventions, local pressure pain as assessment, cross-over study design, language different from English, full-text unavailability (i.e. posters and conference abstracts), and studies involving animals.
2.3Data extraction
Two reviewers independently extracted data from the included studies using a customized data extraction on a Microsoft Excel sheet. In case of disagreement, the consensus was achieved through a third reviewer.
The following data were extracted: first author, publication year, nationality, age of study participants, type of rehabilitative approach as an intervention, type of control (placebo or sham treatment), population and the number of patients included, pain intensity as an outcome measure, and main findings.
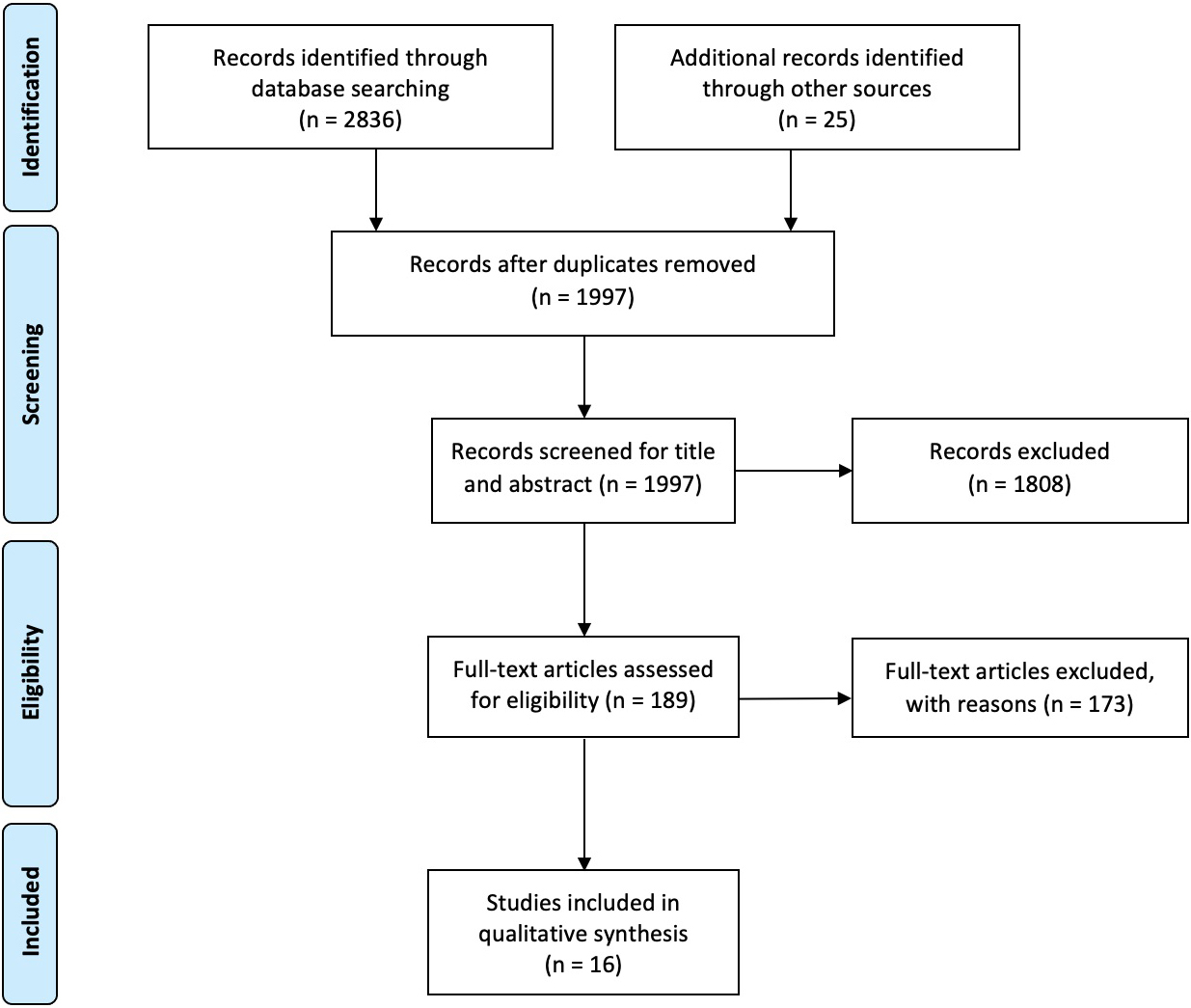
Figure 1.
PRISMA flow diagram.
2.4Data synthesis
The papers were synthesized describing extracted data. Study quality of the RCTs was independently assessed by two reviewers according to the Physiotherapy Evidence Database (PEDro) scale [34]. In case of disagreement, a third reviewer was asked to achieve a consensus. The included studies were classified as excellent (9–10 points), good (6–8 points), fair (4–5 points), or poor (
2.5Statistical analysis
Statistical analysis was performed on Stata 15.0 (Stata, College Station, TX, USA) and Review Manager RevMan (5.3.2 Version, Cochrane Collaboration). The heterogeneity among the comparisons was estimated by the Chi-squared and I2 tests. An I2
3.Results
3.1Study characteristics
At the end of the search, 2836 studies were identified. Then, we also included 25 additional records identified through the manual search. After the removal of duplicates, 1997 were considered suitable for title and abstract screening, and 1808 papers were excluded after title and abstract screening, according to the PICO model (see Table 2 for further details).
Table 2
Reasons for article exclusion by the present systematic review
| Articles excluded after title and abstract screening phase | |
|---|---|
| ( | |
| Not population of interest | 151 (8.4%) |
| Not intervention of interest | 726 (40.2%) |
| Not comparison of interest | 30 (1.7%) |
| Not outcome of interest | 45 (2.5%) |
| Study design different from RCTs | 1201 (66.4%) |
| Language different than English | 25 (1.4%) |
|
Articles excluded after full-text screening phase ( | |
| Not population of interest | 75 (43.4%) |
| Not intervention of interest | 18 (10.4%) |
| Not comparison of interest | 36 (20.8%) |
| Not outcome of interest | 30 (17.3%) |
| Study design different from RCTs | 1 (0.6%) |
| Full-text unavailability | 11 (6.4%) |
The exclusion of the articles followed the PICO model defined in the Methods Section. Data are expressed as counts (percentages).
Therefore, 16 RCTs [37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52] were included in this systematic review, as depicted by the PRISMA flow diagram in Fig. 1. The main characteristics of these studies are described in detail in Table 3. The included studies [37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52] have been published in the last 18 years (from 2002 to 2020).
Table 3
Main characteristics of the randomized controlled trials included in the present systematic review
| Article | Nationality | Study group | Control group | Intervention | Comparison | Outcome measure and time-point assessments | Main findings |
|---|---|---|---|---|---|---|---|
| Cetiner et al. [37] | Turkey | GaAlAs diode laser, 5 time per week x 2 weeks. Laser treatment was performed with Ga-Al-As applied over the four most painful area | Sham Laser, 5 time per week x 2 weeks | 10 cm VAS at baseline, at the end and after 1 month | Significant differences between groups were found in VAS scores in favor of study group after treatment and after 1 month ( | ||
| Da Cuhna et al. [38] | Brazil | GaAlAs low level laser,1 time per week x 4 weeks. Laser treatment was performed with Ga-Al-As applied over the painful area for 20 seconds | Sham Laser, 1 time per week x 4 weeks | 100 mm VAS at baseline and after treatment | No significant differences in VAS between the groups were found | ||
| Magri et al. [39] | Brazil | GaAlAs laser, 2 times/week x 4 weeks, was performed at predetermined points: the masseter (three points: upper, middle, and lower), the anterior temporal (three points: upper, middle, and lower), and the TMJ region (four points forming a cross and one central point) | Sham Laser, 2 times/week x 4 weeks | 10 cm VAS at baseline, at each session (T1-T8) and after 30 days from the end of treatment | Significant differences in pain intensity were found for both groups at the last session of treatment ( | ||
| Monteiro et al. [40] | Portugal | 635 nm Diode Laser, 1 time/week x 4 weeks. The laser beam was applied over the sensitive points where the pain was reported by the participants | Sham Laser, 1 time/week x 4 weeks | NRS at baseline, after treatment and after 3 months | Significant differences between groups were found in VAS scores in favor of study group after 4 weeks ( | ||
| Röhlig et al. [41] | Turkey | 820 nm Diode Laser, 10 sessions in 3 weeks. The laser beam was applied into five points: three points of the masseter muscle (superior point, middle point, inferior point), one point of the temporalis (anterior point) and one point of the sternocleidomastoid muscle (superior SCM) | Sham Laser, 3 sessions in 3 weeks | 100 mm VAS at 1 week, 2 week and at the end of the treatment | No significant differences in VAS between the groups were found | ||
| Sancakli et al. [42] | Turkey | 820 nm Diode Laser, 3 times/week x 4 weeks. Laser was applied to the greatest points of pain in the related muscle (masseter and/ or temporalis) | Sham Laser, 3 times/week x 4 weeks | 100 mm VAS at baseline and after the treatment | Significant differences in LLI were found in VAS ( |
|
Table 3, continued | |||||||
|---|---|---|---|---|---|---|---|
| Article | Nationality | Study group | Control group | Intervention | Comparison | Outcome measure and time-point assessments | Main findings |
| Dıraçoğlu et al. [43] | Turkey | Dry needling therapy, 1 time x 3 weeks. Intra- muscular stimulation was applied on the trigger points. The needle was inserted by the guide tube and was stimulated 3 or 5 times | Sham dry needling, 1 time/week x 3 weeks | 10 cm VAS at baseline and 1 week after last session | No significant differences in VAS between groups were found | ||
| Lopez-Martos et al. [44] | Spain | Percutaneous needle electrolysis (PNE), 1 time/week x 3 weeks. The puncture needles were applied on trigger point of masticatory muscles and were connected to an electrosurgical device, and the electrotherapy equipment produced a continuous galvanic current of 2 mA for 3 seconds, three times through the cathode Dry needling, 1 time/week x 3 weeks. A deep intra- muscular puncture of trigger points of masticatory muscles was carried out without the introduction of any substance (dry puncture) | Sham needling procedure | 10 cm VAS at baseline, at the end of treatment, 42 days and 70 days after | Significant differences between the PNE and sham needling procedure groups were found for all times in favor of PNE ( | ||
| Barbosa et al. [45] | Brazil | Endurance exercises, 2 times/week x 8 weeks. The series were progressively increased, while the time of contraction, the interval between repetitions, and the rest between series were progressively decreased. | Sham laser, 2 times/week x 8 weeks | 100 mm VAS at baseline, 4 week and 8 week | Significant differences in VAS between groups were found in favor of intervention group at 8 weeks ( | ||
| Craane et al. [46] | Belgium | Physical therapy, 2 times/week x 3 weeks and 1 time/week x 3 weeks plus information and education | Behavioral oral education only during the visit | 100 mm VAS at baseline (T0) and at 5 visit (T1-T5) | No significant differences in VAS between groups were found. | ||
| Leite et al. [47] | Brazil | Diacutaneous fibrolysis, 2 time per weeks x 4 weeks. The mechanism of action is thought to be mechanical, by releasing adherences between adjacent musculoskeletal structures to recover the normal sliding between the tissue layers. | Sham diacutaneous fibrolysis, 2 time/weeks x 4 weeks | 10 cm VAS at baseline and after treatment | Significant differences between groups were found at VAS scores in favor of study group after 4 weeks ( | ||
|
Table 3, continued | |||||||
|---|---|---|---|---|---|---|---|
| Article | Nationality | Study group | Control group | Intervention | Comparison | Outcome measure and time-point assessments | Main findings |
| De Giorgi et al. [48] | Italy | TENS, 1 hour/day x 10 weeks. The electrodes were applied on the trapezius, on the line between the acromion and the spine on vertebra C7, on the masseter muscle, the electrode was placed on the muscular belly on the line between the gonial angle and cantus, 1 cm above the gonial angle | Nothing | 100 mm VAS at baseline, 5 week, 10 week, 15 week and 25 week | No significant differences in VAS between groups were found | ||
| Ferreira et al. [49] | Brazil | TENS, 50 minutes x 1 time. The electrodes were applied on the both masseter muscle and temporalis muscle beams according to electromyography surface exam | Sham TENS, 50 minutes x 1 time | 100 mm VAS at baseline, at the end of the treatment and 48 hours after | Significant differences in pain intensity were found in study group at the last session of treatment and at follow-up ( | ||
| De Selles-Neto et al. [50] | Brazil | Acupuncture, 1 time weekly x 5 weeks. Needles were inserted in the bilateral points on meridians that cross the area of pain or with analgesia and energy rebalancing function | Sham acupuncture, 1 time weekly x 5 weeks | 10 cm VAS at baseline, 1 week and 1 month after treatment | No significant differences in VAS between groups were found | ||
| Goddard et al. [51] | USA | Acupuncture, 1 time. 4 needles inserted to a depth of 10 to 30 mm at both right and left Hoku points (Large intestine 4) as well as at the right and left Stomach 6 points. The needles were left in for 30 minutes and twirled once for 5 seconds at the halfway point of the 30-minute period | Sham acupuncture, 1 time | 100 mm VAS at baseline and at the end of the treatment | No significant differences in VAS between groups were found | ||
| Celakil et al. [52] | Turkey | High-frequency bio-oxidative ozone with voltage power ozone therapy, 3 times/week x 2 weeks, was applied to the masticatory muscles of 20 participants 10 min | Sham Ozone therapy, 3 times/week x 2 weeks | 100 mm VAS at baseline, 1 month after the last session and 3 months after the last session | Significant differences between groups were found at VAS scores in favor of study group after 1 month ( | ||
Values are presented as means
Out of 663 subjects analyzed, 357 underwent a rehabilitative approach and 306 were included in the control groups (sham therapy, placebo, or control). Study cohorts of the RCTs included ranged from 18 [51] to 66 [39] patients, with a mean age ranging from 23.4 years [47] sto 46.6 years [38]. Concerning the follow-up evaluations, one RCTs performed a follow-up at 48 hours from last session [49], four studies after 4 weeks from last session [37, 39, 50, 52], two at 12 weeks [40, 52], one at 6 and 10 weeks [44], one at 15 and 25 weeks [48]. The duration of the rehabilitative approach was heterogeneous, varying from 1 session [49, 51] to 70 sessions [48]. Six RCTs [37, 38, 39, 40, 41, 42] investigated the effectiveness of laser therapy, 2 dry needling for trigger points [43, 44], 2 physical therapy [45, 46], 1 diacutaneous fibrolysis [47], 1 PNE [44], 2 TENS [48, 49], 2 acupuncture [50, 51], and 1 oxygen-ozone therapy [52]. Table 3 summarizes the main characteristics of all the RCTs included in the present systematic review.
Figure 2.
Risk of bias assessment, using the Quality Assessment of Diagnostic Accuracy Studies 2.
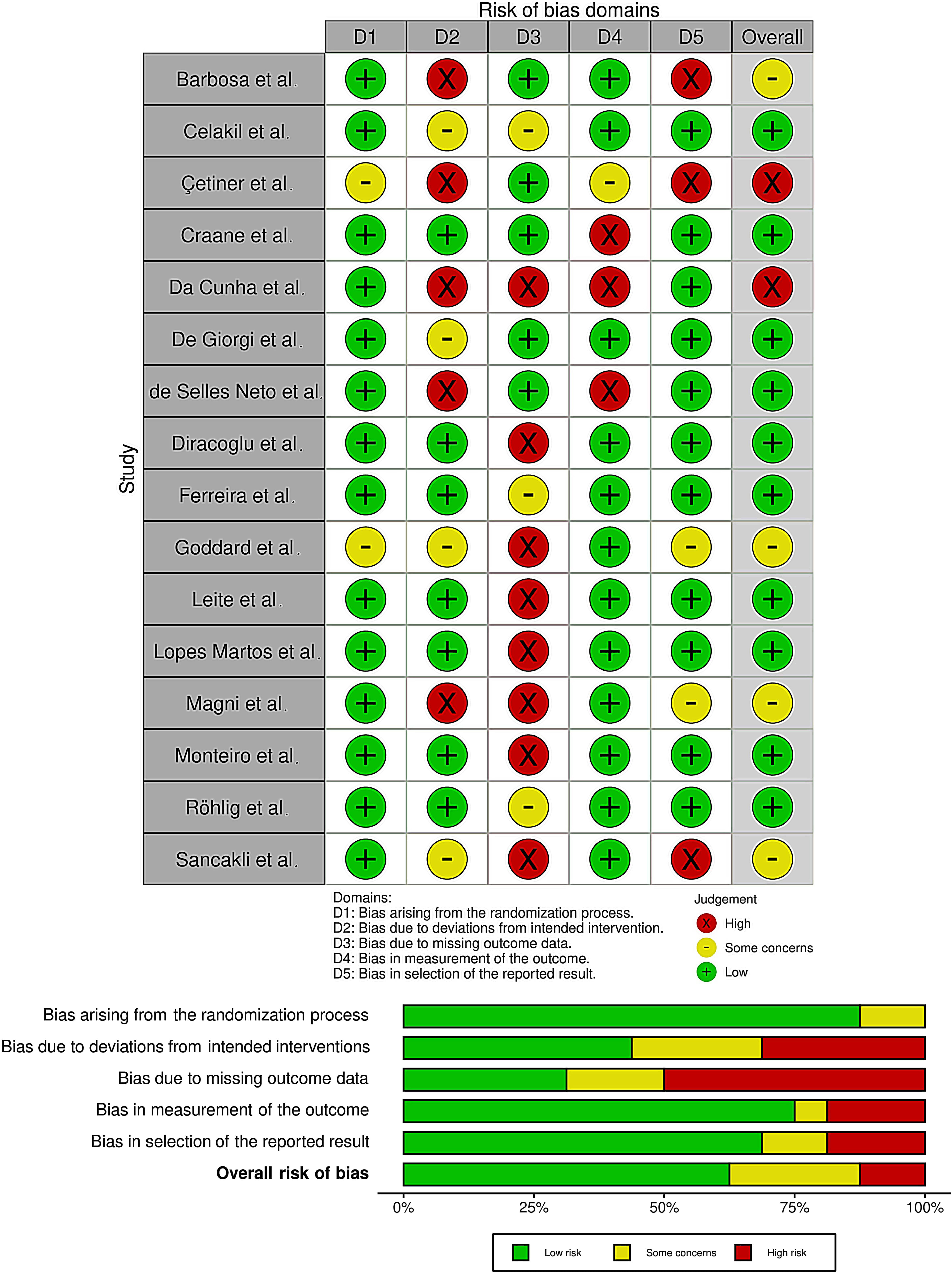
Figure 3.
Pairwise forest plot illustrating the comparison between the rehabilitative interventions versus placebo/sham therapy through a meta-analysis.
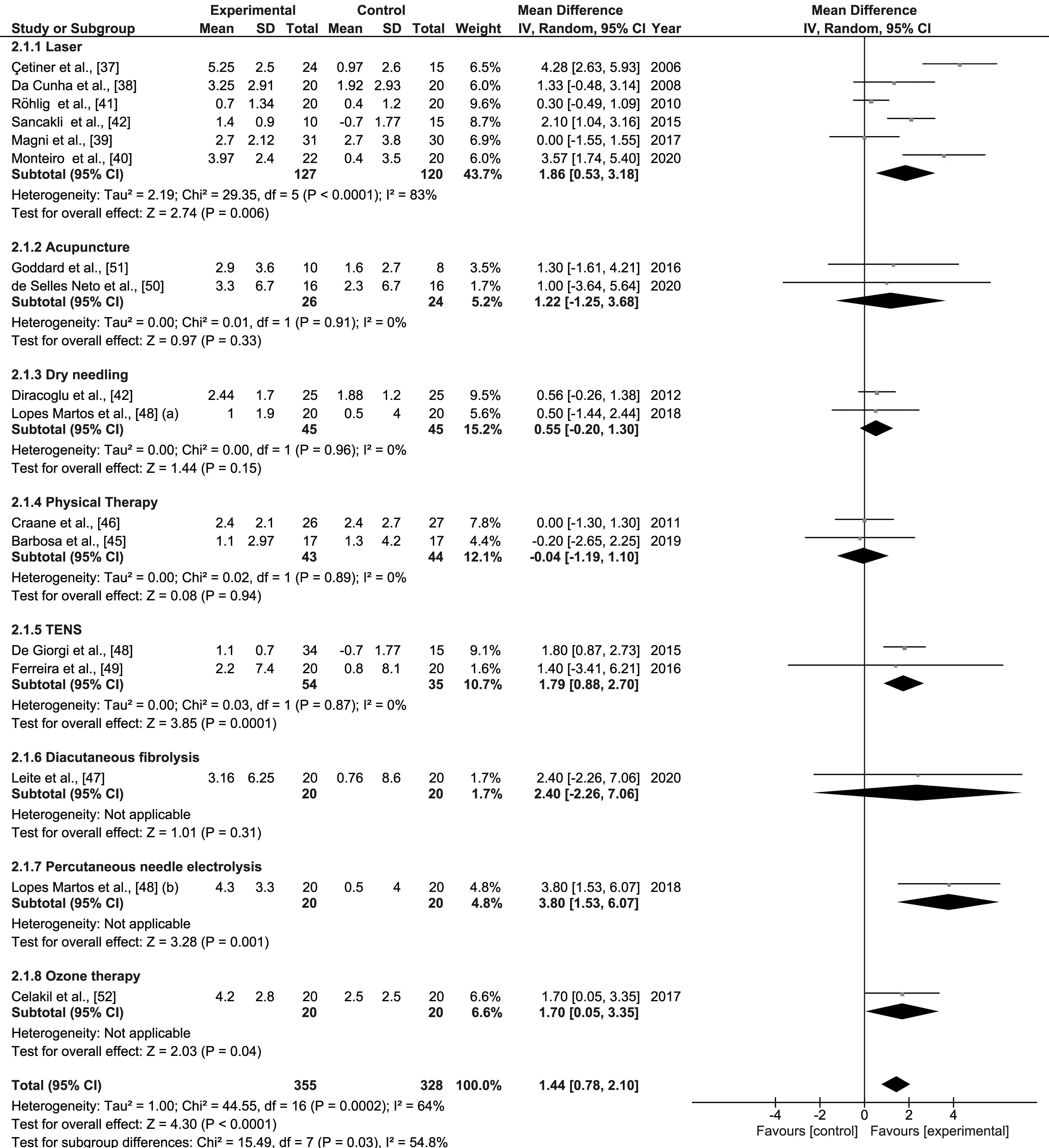
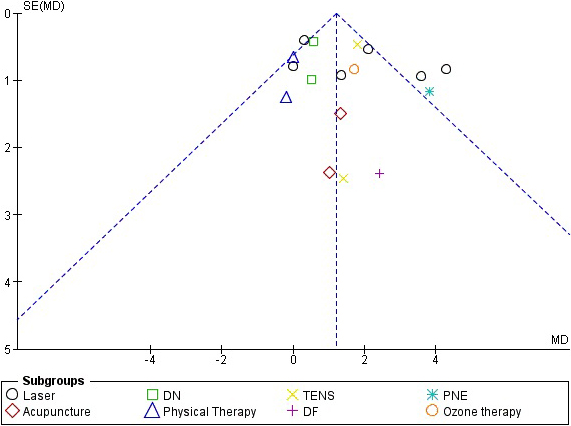
Figure 4.
Begg’s funnel plot analysis of publishing bias in the studies included in the present systematic review.
3.2Laser therapy
Six RCTs [37, 38, 39, 40, 41, 42] have evaluated laser therapy as an intervention, comparing it with sham treatment in TMD patients. Cetiner et al. [37] showed a significant reduction of pain intensity (
3.3Dry needling
Two studies [43, 44] investigated the efficacy of dry needling vs sham needling procedure. Dıraçoğlu et al. [43] reported a statistically significant decrease in 10 cm VAS score in the study group after treatment (6.32
3.4Percutaneous needle electrolysis
Lopez-Martos et al. [44] compared PNE with sham needle procedure (SNP), showing a statistically significant reduction in pain in 10 cm VAS at rest from day 0 to day 70 (6 [5–6.75] vs 1.5 [0.2–4] vs 1.25 [0–3] vs 1.5 [0–2];
3.5Physical therapy
The physical therapy plays a key role in patients with TMD and other facial diseases [45, 46, 53]. More in detail, two studies [45, 46] investigated the effects of physical therapy in TMD. Barbosa et al. [45] in 2019 compared the effects of an 8-week protocol of local endurance exercises of the masticatory muscles with the placebo group. The within-group comparisons for 100 mm VAS,showed a progressive decrease on perceived pain in intervention group between the baseline and 8 weeks (3.7 [2.2] vs 1.1 [1.3];
3.6Diacutaneous fibrolysis
In 2020, Leite et al. [47] evaluated the effects of the 4-week diacutaneous fibrolysis (DF) protocol compared with a sham treatment. The intervention group showed a significant improvement in VAS both at the end of treatment (3.9 [0.7–8.2] vs 0.6 [0–2.3]:
3.7TENS
Two studies [48, 49] investigated the efficacy of TENS in TMD. In 2016, De Giorgi et al. [48] investigated the efficacy of TENS in reducing pain in terms of 100 mm VAS in TMD patients, revealing a decreasing tendency in a 25-week period (
3.8Acupuncture
In a recent study, De Selles-Neto et al. [50] compared acupuncture based on the principles of the Traditional Chinese Medicine to a sham acupuncture. The study group showed a pain reduction in terms of VAS (6.5 [3–10] vs 2.5 [0–7] vs 1 [0–9];
3.9Ozone therapy
Oxygen-ozone therapy is an innovative technique whose application has considerably increased in the field of musculoskeletal pain [54, 55]. To date, there is only one RCT [52] that compared the effects of ozone therapy versus a sham treatment in terms of pain reduction in patients with a muscle-related TMD. In this study, Celakil et al. [52] showed that VAS significantly decreased over time in the ozone group (
3.10Quality assessment and risk of bias
According to the above-mentioned PEDro scale [34], the quality of the studies was classified as good-quality in twelve RCTs (75.0%) [40, 41, 43, 44, 45, 46, 47, 48, 49, 50, 51], and as fair-quality in four RCTs (35.0%) [37, 38, 39, 42] (the quality scoring for each assessment criteria is shown in detail in Table 4).
Using the RoB 2 [35], the risk of bias among the RCTs analyzed was estimated (see Fig. 2). Regarding the selection bias, 14 studies (87.5%) ensured a correct randomization. Five RCTs (31%) excluded performance bias. On the other hand, 12 studies (75%) provided guarantees on blinding of outcome assessment and 11 studies (69%) adequately assessed the attrition bias.
3.11Pairwise meta-analysis
A pairwise meta-analysis was performed to highlight the efficacy of rehabilitative approaches aimed at reducing myofascial pain (measured by VAS or NRS) in TMD patients. The meta-analysis showed that all these rehabilitative approaches had an overall ES of 1.44 ([0.8–2.1],
4.Discussion
This systematic review and meta-analysis of randomized placebo-controlled trials aimed at evaluating the efficacy of conservative approaches and physical therapies in reducing muscle-related pain in patients affected by TMD.
All the RCTs included patients with diagnosis of muscle-related TMD according to the DC/TMD [9],
Table 4
Quality assessment of the included studies according to the PEDro scale
| Eligibility | Randomized allocation | Concealed allocation | Baseline comparability | Blinding of subjects | Blinding of therapists | Blinding of assessors | Key outcomes | Intention to treat | Between- group comparison | Measures of variability | PEDro scale to tal score | |
| Barbosa et al. [45] | Y | Y | Y | N | Y | Y | Y | N | N | Y | Y | 7/10 |
| Celakil et al. [52] | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | 9/10 |
| Cetiner et al. [37] | Y | N | N | Y | N | N | N | Y | Y | Y | Y | 5/10 |
| Craane et al. [46] | Y | Y | Y | Y | N | Y | Y | N | Y | Y | Y | 8/10 |
| Da Cuhna et al. [38] | Y | Y | N | N | N | Y | N | N | N | Y | Y | 4/10 |
| Dıracoglu et al. [43] | Y | Y | Y | Y | Y | Y | N | Y | N | Y | Y | 8/10 |
| De Giorgi et al. [48] | Y | Y | Y | Y | Y | N | Y | Y | N | Y | N | 7/10 |
| De Selles-Neto et al. [50] | Y | Y | N | Y | Y | Y | Y | N | Y | Y | Y | 8/10 |
| Ferreira et al. [49] | Y | Y | Y | Y | Y | N | Y | N | Y | Y | Y | 8/10 |
| Goddard et al. [51] | Y | Y | N | N | Y | N | Y | Y | Y | Y | Y | 7/10 |
| Leite et al. [47] | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | 9/10 |
| Loperz-Martos et al. [44] | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | N | 8/10 |
| Magri et al. [39] | Y | Y | Y | N | Y | N | Y | Y | N | N | N | 5/10 |
| Monteiro et al. [40] | Y | Y | Y | Y | Y | N | N | Y | N | Y | Y | 7/10 |
| Röhlig et al. [41] | Y | Y | Y | Y | Y | N | Y | N | Y | N | Y | 7/10 |
| Sancakli et al. [42] | Y | Y | Y | N | Y | N | Y | N | N | N | Y | 5/10 |
Abbreviations: PEDro scale: Physiotherapy Evidence Database, Y: Yes, N: No.
excluding patients suffering from joint disorders. Myofascial pain in TMD involves a set of multiple clinical manifestations in which pain and limitation in mouth opening are prevalent, representing the reasons why patients seek treatment and assistance. Thus, conservative, noninvasive and reversible approaches are recommended as initial therapy for painful TMD [33].
The present meta-analysis highlighted that all the investigated conservative approaches (i.e., laser therapy [37, 38, 39, 40, 41, 42], dry needling [43, 44], physical therapy [45, 46], diacutaneous fibrolysis [47], PNE [44], TENS [48, 49], acupuncture [50, 51], and ozone therapy [52]) had a significant overall ES of 1.44 (
More in detail, in the subgroup meta-analysis, a significant ES was observed for laser therapy, TENS, PNE, and ozone therapy compared to placebo or sham therapy in reducing VAS in patients with muscle-related TMD.
It should be noted that laser therapy was the most investigated rehabilitative approach (6 RCTs [37, 38, 39, 40, 41, 42]), comparing it to sham treatment in TMD patients, and all of them showed a significant VAS improvement in laser group after therapy (ES
Da Cunha et al. [38] performed laser therapy with a 830 nm wavelength GaAlAs low level laser. Each area was irradiated for 20 seconds, once a week for four consecutive weeks. Magri et al. [39] used a 780 nm wavelength GaAlAs level laser. Each point was irradiated for 10 seconds, twice a week for 4 consecutive weeks at predetermined points: masseter muscle (three points: upper, middle, and lower), anterior temporal muscle (three points: upper, middle, and lower), and TMJ region (four points forming a cross and one central point). Monteiro et al. [40] performed laser therapy with a 635 nm wavelength diode laser, 20 seconds, one session per week for four consecutive weeks. Röhlig et al. used a 820 nm Diode Laser applying it into five points: three points of the masseter muscle (superior point, middle point, inferior point), one point of the temporalis (anterior point) and one point of the sternocleidomastoid muscle; the treatment consisted of 10 sessions in 3 weeks. Sancakli et al. [42] performed the treatment using 820 nm wavelength diode laser, 10 seconds, three sessions per week for four consecutive weeks. It is evident that in all RCTs there is a high heterogeneity in the intervention protocols with laser therapy, which probably affects its use in common clinical practice.
The PNE resulted to have a significant ES
Furthermore, a recent RCT [48], which investigated the efficacy of TENS in reducing pain in terms of 100 mm VAS in TMD patients, showed a decreasing trend over a 25-week period (ES
Our findings are in line with a recent systematic review by Fertout et al. [21], evaluated the effects of TENS in the management of TMD, and concluding that TENS was an effective nondrug-based conservative therapy. Aware of having included studies analyzing both articular and muscular TMD patients, authors concluded that further studies were necessary to establish an appropriate protocol for each type of disorder.
In this systematic review, only two RCTs [45, 46], investigating the efficacy of physical therapy on pain reduction in muscle-related TMD patients, were included. However, the heterogeneity in terms of protocols in the relevant studies is an important concern, such as the adherence to the exercises might be confounding factors to explain the lack of efficacy reported by this meta-analysis. In this context, Herrera-Valencia et al. [28] have recently evaluated the medium- and long-term efficacy of manual therapy on pain by a systematic review with meta-analysis. The authors concluded that manual therapy was effective for TMD in the medium-term, albeit the effects decreased over time.
Regarding the occlusal splints, high-quality RCTs still are needed to draw some conclusions. Due to the difficulty in designing a study with a sham or placebo treatment for splints, existing studies usually compare splints with another kind of therapy such as education [16] or compare two different splints [15].
We are aware that this systematic review with meta-analysis has some limitations. First, only RCTs comparing rehabilitative approaches with a placebo or sham treatment control groups were included in this review, thus excluding RCTs comparing two different interventions without a control group. Furthermore, it should be noted that we included only patients with muscle-related TMD, according to the DC/TMD [9], excluding subjects with temporomandibular joint dysfunctions, diagnosis of TMD related to headache or migraine [56]. Studies including pharmacological therapies were not considered. Lastly, the number of total subjects in each treatment modality is still small to draw strong conclusions.
5.Conclusions
Taken together, findings of this systematic review with meta-analysis suggested that rehabilitative approaches (in particular laser therapy) might be considered as effective in reducing pain in muscle-related TMD patients. However, the relatively low number of RCTs evaluating conservative approaches for treatment of muscle-related TMD calls for caution in the interpretation of these results. Therefore, further high-quality studies are warranted to obtain a scientific consensus regarding the best rehabilitative approach for pain relief in patients with muscle-related TMD.
Acknowledgments
None to report.
Conflict of interest
None of the authors declare any conflict of interest, funding sources or consultant relationships with any organizations involved in this research.
Author contributions
Study design and conceptualization: MF, AdS; Search strategy: MF, AA, SP, DC, NM, MM, LF, AG, AM, AdS; Databases searching: AdS; Data screening: MF, DC, AdS; Data extraction: MF, AA, AdS; Data synthesis and interpretation: MF, SP, AdS; Statistical analysis: NM; Manuscript drafting: MF; Critical revision: AM, AdS; Visualization: AA, SP, DC, NM, MM, LF, AG; Study supervision: AM, AdS; Study submission: AdS. All authors read and approved the final version of the manuscript.
References
[1] | Okeson JP. Bell’s Oral and Facial Pain, Quintessence Publishing, Hannover, Germany, 7th edition, (2014) . |
[2] | Okeson JP. Management of Temporomandibular Disorders and Occlusion, Missouri Elsevier Mosby, St. Louis, MI, USA, 7th; edition, 2012. |
[3] | Iodice G, Danzi G, Cimino R, Paduano S, Michelotti A. Association between posterior crossbite, masticatory muscle pain, and disc displacement: a systematic review. Eur J Orthod. (2013) ; 35: (6): 737-44. doi: 10.1093/ejo/cjt024. |
[4] | Bizzarro M, Generali C, Maietta S, Martorelli M, Ferrillo M, Flores-Mir C, Perillo L. Association between 3D palatal morphology and upper arch dimensions in buccally displaced maxillary canines early in mixed dentition. Eur J Orthod. (2018) Nov 30; 40: (6): 592-596. doi: 10.1093/ejo/cjy023. |
[5] | Fillingim RB, Ohrbach R, Greenspan JD, Knott C, Diatchenko L, Dubner R, et al. Psychological factors associated with development of TMD: the OPPERA prospective cohort study. J Pain. (2013) Dec; 14: (12 Suppl): T75-90. doi: 10.1016/j.jpain.2013.06.009. |
[6] | Dıraçoğlu D, Yıldırım NK, Saral İ, Özkan M, Karan A, Özkan S, Aksoy C. Temporomandibular dysfunction and risk factors for anxiety and depression. J Back Musculoskelet Rehabil. (2016) Aug 10; 29: (3): 487-91. doi: 10.3233/BMR-150644. |
[7] | Ferrillo M, Migliario M, Curci C, Roccuzzo A, Invernizzi M, de Sire A. Reliability of dental calcification compared to hand-wrist X-ray to evaluate skeletal maturation in growing subjects: a systematic review. J Biol Regul Homeost Agents. (2021) Mar-Apr; 35: (2): 717-723. doi: 10.23812/21-106-L. |
[8] | Ferrillo M, Curci C, Roccuzzo A, Migliario M, Invernizzi M, de Sire A. Reliability of cervical vertebral maturation compared to hand-wrist for skeletal maturation assessment in growing subjects: A systematic review. J Back Musculoskelet Rehabil. (2021) Apr 27. doi: 10.3233/BMR-210003. |
[9] | Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet JP, et al. International RDC/TMD Consortium Network, International association for Dental Research; Orofacial Pain Special Interest Group, International Association for the Study of Pain. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group†. J Oral Facial Pain Headache. (2014) Winter; 28: (1): 6-27. doi: 10.11607/jop.1151. |
[10] | Fleckenstein J, Zaps D, Ruâ•£er LJ, Lehmeyer L, Freiberg F, Lang PM, et al., Discrepancy between prevalence and perceived effectiveness of treatment methods in myofascial pain syndrome: results of a cross-sectional, nationwide survey. BMC Musculoskelet Disord (2010) ; 11: : 32. doi: 10.1186/1471-2474-11-32. |
[11] | Wieckiewicz M, Smardz J, Martynowicz H, Wojakovska A, Mazur G, Winocur E. Distribution of temporomandibular disorders among sleep bruxers and non-bruxers-A polysomnographic study. Journal of oral rehabilitation. (2020) ; 47: (7): 820-826. doi: 10.1111/joor.12955. |
[12] | Manfredini D, Guarda-Nardini L, Winocur E, Piccotti F, Ahlberg J, Lobbezoo F. Research diagnostic criteria for temporomandibular disorders: a systematic review of axis I epidemiologic findings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. (2011) ; 112: : 453-62. doi: 10.1016/j.tripleo.2011.04.021. |
[13] | Gerber LH, Sikdar S, Armstrong K, Diao G, Heimur J, Kopecky J, et al. A systematic comparison between subjects with no pain and pain associated with active myofascial trigger points. PM R. (2013) ; 5: : 931-8. doi: 10.1016/j.pmrj.2013.06.006. |
[14] | Pastore GP, Goulart DR, Pastore PR, Prati AJ, de Moraes M. Self-medication among myofascial pain patients: A preliminary study. Open Dent J. (2018) ; 12: : 347-53. doi: 10.2174/1874210601812010347. |
[15] | Deregibus A, Ferrillo M, Grazia Piancino M, Chiara Domini M, de Sire A, Castroflorio T. Are occlusal splints effective in reducing myofascial pain in patients with muscle-related temporomandibular disorders? A randomized-controlled trial. Turk J Phys Med Rehabil. (2021) ; 67: (1): 32-40. doi: 10.5606/tftrd.2021.6615. |
[16] | Michelotti A, Iodice G, Vollaro S, Steenks MH, Farella M. Evaluation of the short-term effectiveness of education versus an occlusal splint for the treatment of myofascial pain of the jaw muscles. J Am Dent Assoc. (2012) ; 143: (1): 47-53. doi: 10.14219/jada.archive.2012.0018. |
[17] | Story WP, Durham J, Al-Baghdadi M, Steele J, Araujo-Soares V. Self-management in temporomandibular disorders: a systematic review of behavioural components. J Oral Rehabil. (2016) ; 43: (10): 759-70. doi: 10.1111/joor.12422. |
[18] | Armijo-Olivo S, Pitance L, Singh V, Neto F, Thie N, Michelotti A. Effectiveness of manual therapy and therapeutic exercise for temporomandibular disorders: Systematic review and meta-analysis. Phys Ther. (2016) ; 96: (1): 9-25. doi: 10.2522/ptj.20140548. |
[19] | Cho SH, Whang WW. Acupuncture for temporomandibular disorders: a systematic review. J Orofac Pain. (2010) ; 24: (2): 152-62. PMID: 20401353 |
[20] | Xu GZ, Jia J, Jin L, Li JH, Wang ZY, Cao DY. Low-level laser therapy for temporomandibular disorders: a systematic review with meta-analysis. Pain Res Manag. (2018) ; 2018: : 4230583. doi: 10.1155/2018/4230583. |
[21] | Fertout A, Manière-Ezvan A, Lupi L, Ehrmann E. Management of temporomandibular disorders with transcutaneous electrical nerve stimulation: A systematic review. Cranio. (2019) ; 9: : 1-12. doi: 10.1080/08869634.2019.1687986. |
[22] | Machado E, Machado P, Wandscher VF, Marchionatti AME, Zanatta FB, Kaizer OB. A systematic review of different substance injection and dry needling for treatment of temporomandibular myofascial pain. Int J Oral Maxillofac Surg. (2018) ; 47: (11): 1420-1432. doi: 10.1016/j.ijom.2018.05.003. |
[23] | Calixtre LB, Moreira RF, Franchini GH, Alburquerque-Sendín F, Oliveira AB. Manual therapy for the management of pain and limited range of motion in subjects with signs and symptoms of temporomandibular disorder: a systematic review of randomised controlled trials. J Oral Rehabil. (2015) ; 42: (11): 847-861. doi: 10.1111/joor.12321. |
[24] | Gil-Martínez A, Paris-Alemany A, López-de-Uralde-Villanueva I, La Touche R. Management of pain in patients with temporomandibular disorder (TMD): challenges and solutions. J Pain Res. (2018) ; 11: : 571-587. doi: 10.2147/JPR.S127950. |
[25] | Fernandes AC, Duarte Moura DM, Da Silva LGD, De Almeida EO, Barbosa GAS. Acupuncture in temporomandibular disorder myofascial pain treatment: A systematic review. J Oral Facial Pain Headache. (2017) Summer; 31: (3): 225-232. doi: 10.11607/ofph.1719. |
[26] | Munguia FM, Jang J, Salem M, Clark GT, Enciso R. Efficacy of low-level laser therapy in the treatment of temporomandibular myofascial pain: A systematic review and meta-analysis. J Oral Facial Pain Headache. (2018) ; 32: (3): 287-297. doi: 10.11607/ofph.2032. |
[27] | van der Meer HA, Calixtre LB, Engelbert RHH, Visscher CM, Nijhuis-van der Sanden MW, Speksnijder CM. Effects of physical therapy for temporomandibular disorders on headache pain intensity: A systematic review. Musculoskelet Sci Pract. (2020) ; 50: : 102277. doi: 10.1016/j.msksp.2020.102277. |
[28] | Herrera-Valencia A, Ruiz-Muñoz M, Martin-Martin J, Cuesta-Vargas A, González-Sánchez M. Effcacy of manual therapy in temporomandibularjoint disorders and its medium-and long-termeffects on pain and maximum mouth opening: A systematic review and meta-analysis. J Clin Med. (2020) Oct 23; 9: (11): 3404. doi: 10.3390/jcm9113404. |
[29] | Al-Moraissi EA, Alradom J, Aladashi O, Goddard G, Christidis N. Needling therapies in the management of myofascial pain of the masticatory muscles: A network meta-analysis of randomised clinical trials. J Oral Rehabil. (2020) Jul; 47: (7): 910-922. doi: 10.1111/joor.12960. |
[30] | Moher D, Altman DG, Liberati A, Tetzlaff J. PRISMA statement. Epidemiology. (2011) ; 22: (1): 128. doi: 10.1097/EDE.0b013e3181fe7825. |
[31] | Cochrane Handbook for Systematic Reviews of Interventions Version 62. (updated February 2021). Cochrane, (2021) . Available from training.cochrane.org/handbook. |
[32] | Karcioglu O, Topacoglu H, Dikme O, Dikme O. A systematic review of the pain scales in adults: Which to use? Am J of Emerg Med. (2018) ; 36: (4): 707-714. doi: 10.1016/j.ajem.2018.01.008. |
[33] | Thong ISK, Jensen MP, Miró J, Tan G. The validity of pain intensity measures: What do the NRS, VAS, VRS, and FPS-R Measure? Scand J Pain. (2018) Jan 26; 18: (1): 99-107. doi: 10.1515/sjpain-2018-0012. |
[34] | Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Physical therapy. (2003) ; 83: (8): 713-721. PMID: 12882612. |
[35] | Sterne JAC, Savoviç J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. (2019) ; 366: : l4898. doi: 10.1136/bmj.l4898. |
[36] | Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. (2005) ; 5: : 13. doi: 10.1186/1471-2288-5-13. |
[37] | Cetiner S, Kahraman SA, Yücetaş S. Evaluation of low-level laser therapy in the treatment of temporomandibular disorders. Photomed Laser Surg. (2006) ; 24: (5): 637-41. doi: 10.1089/pho.2006.24.637. |
[38] | da Cunha LA, Macedo Firoozmand L, Pereira da Silva A, Afonso Camargo SE, de Oliveira W. Efficacy of low-level laser therapy in the treatment of temporomandibular disorder. Int Dent J. (2008) ; 58: (4): 213-7. doi: 10.1111/j.1875-595x.2008.tb00351.x. |
[39] | Magri LV, Carvalho VA, Rodrigues FC, Bataglion C, Leite-Panissi CR. Effectiveness of low-level laser therapy on pain intensity, pressure pain threshold, and SF-MPQ indexes of women with myofascial pain. Lasers Med Sci. (2017) ; 32: (2): 419-428. doi: 10.1007/s10103-016-2138-x. |
[40] | Monteiro L, Ferreira R, Resende T, Pacheco JJ, Salazar F. Effectiveness of photobiomodulation in temporomandibular disorder-related pain using a 635 nm diode laser: A randomized, blinded, and placebo-controlled clinical trial. Photobiomodul Photomed Laser Surg. (2020) ; 38: (5): 280-288. doi: 10.1089/photob.2019.4730. |
[41] | Röhlig BG, Kipirdi S, Meric U, Capan N, Keskin H. Masticatory muscle pain and low-level laser therapy: a double-blind and placebo-controlled study. Turkish Journal of Physical Medicine and Rehabilitation. (2011) ; 57: (1): 31-37. doi: 10.4274/tftr.57.06. |
[42] | Sancakli E, Gökçen-Röhlıg B, Balık A, Öngül D, Kıpırdı S, Keskın H. Early results of low-level laser application for masticatory muscle pain: a double-blind randomized clinical study. BMC Oral Health. (2015) ; 15: (1): 131. doi: 10.1186/s12903-015-0116-5. |
[43] | Dıraçoğlu D, Vural M, Karan A, Aksoy C. Effectiveness of dry needling for the treatment of temporomandibular myofascial pain: A double-blind, randomized, placebo controlled study. J Back Musculoskelet Rehabil. (2012) ; 25: (4): 285-90. doi: 10.3233/BMR-2012-0338. |
[44] | Lopez-Martos R, Gonzalez-Perez LM, Ruiz-Canela-Mendez P, Urresti-Lopez FJ, Gutierrez-Perez JL, Infante-Cossio P. Randomized, double-blind study comparing percutaneous electrolysis and dry needling for the management of temporomandibular myofascial pain. Med Oral Patol Oral Cir Bucal. (2018) ; 23: (4): e454-e462. doi: 10.4317/medoral.22488. |
[45] | Barbosa MA, Tahara AK, Ferreira IC, Intelangelo L, Barbosa AC. Effects of 8-week of masticatory muscles focused endurance exercises on women with orofacial pain and temporomandibular disorders: a placebo randomized controlled trial. J Oral Rehabil. (2019) Oct; 46: (10): 885-894. doi: 10.1111/joor.12823. |
[46] | Craane B, Dijkstra PU, Stappaerts K, De Laat A, One-year evaluation of the effect of physical therapy for masticatory muscle pain: A randomized controlled trial. Eur J Pain. (2012) ; 16: (5): 737-47. doi: 10.1002/j.1532-2149.2011.00038.x. |
[47] | Leite WB, Oliveira ML, Ferreira IC, Anjos CF, Barbosa MA, Barbosa AC. Effects of 4-week diacutaneous fibrolysis on myalgia, mouth opening, and level of functional severity in women with temporomandibular disorders: A randomized controlled trial. J Manipulative Physiol Ther. (2020) ; 43: (8): 806-815. doi: 10.1016/j.jmpt.2020.01.002. |
[48] | Giorgi I, Castroflorio T, Sartoris B, Deregibus A. The use of conventional transcutaneous electrical nerve stimulation in chronic facial myalgia patients. Clin Oral Investig. (2017) ; 21: (1): 275-280. doi: 10.1007/s00784-016-1787-2. |
[49] | Ferreira AP, Costa DR, Oliveira AI, Carvalho EA, Conti PC, Costa YM, et al. Short-term transcutaneous electrical nerve stimulation reduces pain and improves the masticatory muscle activity in temporomandibular disorder patients: a randomized controlled trial. J Appl Oral Sci. (2017) Mar-Apr; 25: (2): 112-120. doi: 10.1590/1678-77572016-0173. |
[50] | de Salles-Neto FT, de Paula JS, Romero JGAJ, Almeida-Leite CM. de Salles-Neto FT, de Paula JS, Romero JGAJ, et al. Acupuncture for pain, mandibular function and oral health-related quality of life in patients with masticatory myofascial pain: A randomised controlled trial. J Oral Rehabil. (2020) ; 47: (10): 1193-1201. doi: 10.1111/joor.13055. |
[51] | Goddard G, Karibe H, McNeill C, Villafuerte E. Acupuncture and sham acupuncture reduce muscle pain in myofascial pain patients. J Orofac Pain. (2002) ; 16: (1): 71-6. PMID: 11889662 |
[52] | Celakil T, Muric A, Gokcen Roehlig B, Evlioglu G, Keskin H. Effect of high-frequency bio-oxidative ozone therapy for masticatory muscle pain: a double-blind randomized clinical trial. J Oral Rehabil. (2017) Jun; 44: (6): 442-451. doi: 10.1111/joor.12506. |
[53] | Paolucci T, Cardarola A, Colonnelli P, Ferracuti G, Gonnella R, Murgia M, et al. Give me a kiss! An integrative rehabilitative training program with motor imagery and mirror therapy for recovery of facial palsy. Eur J Phys Rehabil Med. (2020) Feb; 56: (1): 58-67. doi: 10.23736/S1973-9087.19.05757-5. |
[54] | de Sire A, Agostini F, Lippi L, Mangone M, Marchese S, Cisari C, et al. Oxygen-ozone therapy in the rehabilitation field: state of the art on mechanisms of action, safety and effectiveness in patients with musculoskeletal disorders. Biomolecules. (2021) Feb 26; 11: (3): 356. doi: 10.3390/biom11030356. |
[55] | de Sire A, Stagno D, Minetto MA, Cisari C, Baricich A, Invernizzi M. Long-term effects of intra-articular oxygen-ozone therapy versus hyaluronic acid in older people affected by knee osteoarthritis: A randomized single-blind extension study. J Back Musculoskelet Rehabil. (2020) ; 33: (3): 347-354. doi: 10.3233/BMR-181294. |
[56] | van der Meer HA, Speksnijder CM, Engelbert RHH, Lobbezoo F, Nijhuis-van der Sanden MWG, Visscher CM. The Association Between Headaches and Temporomandibular Disorders is Confounded by Bruxism and Somatic Symptoms. Clin J Pain. (2017) Sep; 33: (9): 835-843. doi: 10.1097/AJP.0000000000000470. |




