Well-described exercises for chronic low back pain in Life Science Literature: A systematic review
Abstract
BACKGROUND:
Therapeutic exercise (TE) is recommended in multimodal treatment for patients with non-specific chronic back pain (cLBP).
OBJECTIVE:
The aim of this study is to identify an exercise or a spectrum of exercises, well described and reproducible by the clinician, for cLBP patients.
METHODS:
Systematic review by researching in the databases MEDLINE, EMBASE, PEDro, CINAHL, and Scopus. Evidence from Randomized Controlled Trials (RCTs) supported the TE in patients with non-specific cLBP, provided that it was well described and could be repeated by another therapist. Methodological evaluation was performed using the PEDro scale and only studies with a score of
RESULTS:
Twenty-one articles were included in this systematic review. The defective description and the poorly reporting of the intervention makes it more difficult for the clinician to include the TE into clinical practice.
CONCLUSIONS:
The findings of this study showed that the reporting of the intervention in high quality RCT on chronic low back pain is low, threatening the external validity of the results.
1.Introduction
Worldwide, low back pain (LBP) is the prime cause of disability [1, 2]; more than 80% of people have at least one episode of back pain in their life time [3]. LBP is the most common reason for medical consultation [4] among musculoskeletal disorders [3]; on the basis of these reports, LBP is associated with the high costs to companies, including those related to health care and indirect care, in terms of absence from work or reduced productivity [1]. The LBP is also classified according to the duration of the symptoms: acute (
To convert evidence of effective treatment into practice and to replicate the action recommended and described in a research, clinicians need to have precise information about the details of the interventions of the exercise including dose, frequency, and intensity. This requires clear, complete, and accessible reports of all elements of the exercise, as assessed in the research studies.
Given the importance of adequate reporting of physical activity interventions in clinical trials, it is necessary to consider the Template for Intervention Description and Replication (TIDieR) in order to improve the generalizability of the results. It was developed by an international group of experts and stakeholders [9] to guide the complete reporting on physical activity interventions. The TIDieR checklist contains the minimum information about the physical activity interventions, as reported by the authors, with sufficient details that allow their replication. In addition, the TIDieR checklist has been widely adopted by scientific journals to improve the reporting of physical activity interventions [10].
Yamato et al. reported that, for most physiotherapy trials, physical activity interventions are incompletely recorded and therefore, not reproducible [11]. Poorly reported interventions can create barriers to implementation of best clinical practices that may affect treatment effectiveness, not allowing patients to receive up-to-date evidence-based interventions [12].
Aspects of completeness and quality in reporting the physical activity interventions in the treatment for cLBP have not been evaluated in Life Science Literature. The present article aims to identify an exercise or a spectrum of exercises for cLBP patients, appropriately described and reproducible by the clinician, based on assessment, needs and preferences of the patient, that can be used in response to the physical, emotional, social and economic problems caused by LBP pain [2].
2.Objectives
To verify if Life Science Literature contains studies describing exercise programs for patients with cLBP that are reproducible by a physiotherapist, we performed a systematic review of RCTs, that evaluate the effectiveness of exercise therapy, as compared to non-treatment or other treatments in reducing the main outcomes, such as pain, disability, functions and quality of life, using the TIDieR checklist as an essential tool to evaluate the quality of interventions reported in RCTs.
3.Methods
The methodology and the reporting of this systematic review were based on the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Statement [13]. The protocol was a-priori registered on PROSPERO, an international prospective register of systematic reviews (registration number: CRD42018117317).
3.1Eligibility criteria
RCTs, assessing TE in adult patients aged 18 years and over with non-specific cLBP were included as the Population of the study. Moreover about the Intervention, studies assessing every type of TE (i.e., aerobic, endurance, stretching, motor control, core stability, strengthening, flexibility) performed individually or in groups, supervised or not, alone or within a multimodal treatment that was reproducible by another operator, were considered. To satisfy the criterion of reproducibility of the exercise, the RCT had to provide clear instructions, within the article itself, without referring to other protocols of articles, for example about execution, movement, timing and repetitions of the exercise in order to make it replicable by another operator within his working setting, without the use of a particular mechanical aid or tool. The control is represented by no treatments, usual care, manual therapy, multimodal treatment and other type of exercise or physiotherapy interventios; detailed information is given in Table 1.
Studies including pregnant patients or patients with acute or subacute or specific LBP or assessing pharmacological, surgical or physical therapies (i.e., laser therapy, ultrasound, etc.) or Pilates and Yoga treatments were excluded. Only studies with PEDro score
3.2Data sources and searches
The studies were identified through bibliographic research on the MEDLINE (through the interface PubMed), Excepta Medica dataBASE (EMBASE), the Physiotherapy Evidence Database (PEDro), the Cumulative Index to Nursing and Allied Health Literature (CINAHL) and Scopus databases from their inception
Table 1
Characteristics of the studies
| References | Characteristics of the experimental sample | Characteristics of the control sample | Intervention of the experimental group | Intervention of the control group | Outcome measures | Outcome results | Follow-up | Pedro score |
|---|---|---|---|---|---|---|---|---|
| Aasa et al., 2015 | N:35 Female: 54% Age: 42.0 | N:35 Female: 57% Age: 42.0 | Low load motor control exercises (LMC) | High load lifting exercises (HLL) | Pain: PSFS, VAS Function: Strenght, endurance and motor control tests | Both interventions resulted in significant improvements in pain, strength, and endurance. The LMC group showed greater improvement on the PSFS compared with the HLL group ( | 2 and 12 months | 7/10 |
| Bello et al., 2015 | N: 40 Female: 62.1% Age: 45.0 | N: 40 Female: 39.8% Age: 43.1 | Convention execise therapy (CET) | Behavioural graded activity (BGA) | Pain: NPRS Quality of life: SF-36 | The results indicate that CET and BGA have no significant differences ( | 12 weeks | 6/10 |
| Balthazars et al., 2012 | N: 20 Female: 30% Age: 44.0 | N: 22 Female: 36% Age: 42.0 | Manual therapy and active exercise (MT | Sham therapy | Pain: VAS Disability: ODI Fear: FABQ Endurance tests | MT | 8 weeks, 3 and 6 months | 6/10 |
| Bello et al., 2018 | N: 25 Female: NR Age: 42.2 | N: 25 Female: NR Age: 46.6 | Lumbar stabilization exercises | Treadmill walking | Pain: VAS Disability: ODI | Lumbar stabilisation exercises are more effective than treadmill walking exercises in activating the multifidus muscle, reducing pain intensity and functional disability ( | 8 weeks | 8/10 |
| Chen et al., 2014 | N: 64 Female: 100% Age: 30.6 | N: 63 Female: 100% Age: 30.6 | Stretching exercise program (SEP) | Usual activity | Pain: VAS Self-efficacy: The exercise Self-efficacy scale | SEP had significantly lower VAS scores ( | 2, 4 and 6 months | 7/10 |
| Costantino et al., 2014 | N: 28 Female: 48.2% Age: 73.6 | N: 28 Female: 40.7% Age: 73.3 | Back school exercises | Hydrotherapy exercises | Disability: RMDQ Quality of life: SF-36 | In both groups we observed a highly significant statistical difference in the values ( | 12 and 26 weeks | 6/10 |
| Franca et al., 2012 | N: 15 Female: not reported Age:42.0 | N: 15 Female: not reported Age: 41.5 | Segmental stabilization (SS) | Stretching | Pain: VAS, McGill pain questionnaire Disability: ODI Function: Contraction of TrA | Both treatments were effective in relieving pain and improving disability ( | 6 weeks | 8/10 |
|
Table 1, continued | ||||||||
|---|---|---|---|---|---|---|---|---|
| References | Characteristics of the experimental sample | Characteristics of the control sample | Intervention of the experimental group | Intervention of the control group | Outcome measures | Outcome results | Follow-up | Pedro score |
| Garcia et al., 2013 | N: 74 Female: 68.9% Age: 54.1 | N: 74 Female: 68.9% Age: 53.7 | McKenzie exercises | Back school exercises | Pain: NPRS Disability: RMDQ Quality of life: WHOQOL-BREF | McKenzie group had greater improvements in disability at 1 month ( | 1,3 and 6 months | 8/10 |
| Gatti et al., 2011 | N: 34 Female: 67.6% Age: 58.6 | N: 45 Female: 62.2% Age: 57.1 | Trunk balance exercises | Flexibility and strengthening exercises | Pain: VAS Disability: RMQ Quality of life: SF-12 | The improvement in RMQ score was significantly greater for the experimental group ( | 6 weeks | 7/10 |
| Jaromi et al., 2017 | N: 67 Female: 92,.5% Age: 41.7 | N: 70 Female: 94.2% Age: 41.3 | Back school program | Written lifestyle guidance | Pain: VAS Function: ROM, Lifting Technique | We found significant difference between the intervention and control group’s VAS score ( | 3 months | 6/10 |
| Kim et al., 2016 | N: 38 Female: 60.5% Age: 39.5 | N: 39 Female: 53.8% Age: 46.2 | Sling exercise with elastic | Trunk muscle stabilizing exercise | Pain: NPRS Disability: ODI | A sling exercise with elastic bands leads to a reduction in pain and disability when compared to a traditional stabilizing exercise ( | 12 weeks, 3 months | 8/10 |
| Michaelson et al., 2016 | N: 35 Female: 57.1% Age: 41.9 | N: 35 Female: 54.2% Age: 42.2 | High load lifting | Low load motor control | Pain: VAS Disability: RMDQ Quality of life: SF-36 | No difference was observed between the high low load lifting and low load motor control interventions | 2, 12 and 24 months | 8/10 |
| Monteiro et al., 2015 | N: 14 Female: 100% Age: 68.0 | N: 16 Female: 100% Age: 68.0 | Control exercises | Virtual physical training with Wii | Pain: NPRS Balance: Wii Balance Board Functional Autonomy: Sit-to-stand Mood: POMS | Exercises with Wii were more effective only for sitting capacity | 8 weeks | 6/10 |
| Nagrale et al., 2012 | N: 30 Female: 70% Age: 38.2 | N: 30 Female: 60% Age:37.7 | Slump stretching | Mobilization with exercise | Pain: NPRS Disability: ODI Fear: FABQ | The use of slump stretching shows a significantly greater improvement in ODI at 3 and 6 weeks ( | 1, 2, 3 and 6 weeks | 8/10 |
| Noormoh ammadpour et al., 2018 | N: 10 Female: 100% Age: 43.3 | N: 10 Female: 100% Age: 41.3 | Core stability exercise | Waiting list | Disability: RMDQ Quality of life: SF-36 Pain: VAS Diameter of lateral abdominal muscles | The results showed significant improvements in disability, quality of life and pain in the intervention group ( | 8 weeks | 7/10 |
|
Table 1, continued | ||||||||
|---|---|---|---|---|---|---|---|---|
| References | Characteristics of the experimental sample | Characteristics of the control sample | Intervention of the experimental group | Intervention of the control group | Outcome measures | Outcome results | Follow-up | Pedro score |
| Oliveira et al., 2017 | N: 33 Female: 75.7% Age: 46.6 | N: 33 Female: 72.7% Age: 47.2 | Exercise (stretching, strengthening, motor control) | Graded activity (aerobic training, strengthening) | Pain: NPRS, McGill Pain Questionnaire Disability: RMDQ Quality of life: SF-36 Kinesiophobia: TSK Daily physical activity: Baecke Questionaire of Habitual Physical Activity | No significant differences between groups after three and six month-follow ups were observed | 6 weeks, 3 and 6 months | 7/10 |
| Pardo et al., 2017 | N:28 Female:78.5% Age:49.2 | N: 28 Female: 78.5 % Age: 44.9 | Pain neurophysiology education | Therapeutic exercise | Pain: NPRS, PCS, Pressure pain thresholds Disability: RMDQ Kinesiophobia: TSK Change: PGIC Function: finger to floor distance | At 3-month follow-up, a large change in pain intensity ( | 1 and 3 months | 6/10 |
| Rabin et al., 2014 | N: 48 Female: 52.1% Age: 38.3 | N: 57 Female: 54.4% Age: 35.5 | Lumbar stabilization exercises | Manual therapy | Pain: NPRS Disability: MODI | The experimental intervention was more effective than the control intervention but not statistically significant. | 8 weeks | 6/10 |
| Segal-Snir et al., 2016 | N: 20 Female: 100% Age: 57.1 | N: 15 Female: 100% Age: 54.6 | Rotation Exercises in group | Only ADL guidance | Pain: VAS Function: ROM lumbar Disability: RMDQ | There were no significant differences for either group ( | 4 and 8 weeks | 6/10 |
| Vergas et al., 2011 | N: 24 Female: 58% Age: 37.6 | N: 25 Female: 54% Age: 39.8 | Multimodal physical therapy program | Multimodal physical therapy Program | Pain: VAS Disability: RMQ Quality of life: SF-12 Function: Strenght, mobility and endurance tests | No significant differences between groups; the outcomes measures improved in both groups | 15 weeks | 6/10 |
| Zafereo et al., 2018 | N: 20 Female: 75% Age: 46.7 | N: 20 Female: 50% Age: 38.2 | Regional manual therapy | Standard physical Therapy: motor control exercise program and lumbar spine manual therapy | Disability: ODI Pain: NPRS Fear: FABQ Pain catastrophizing PCS Effect of treatment: GROC | Both groups demonstrated improvements in disability level, pain intensity, pain catastrophizing, and fear avoidance beliefs across time ( | 2,4 and 12 weeks | 7/10 |
Abbreviations: ADL
tion to the 16
3.3Study selection
The research of the studies in the databases was carried out individually by two evaluators. After deleting the duplicates, the studies were evaluated first by their title, then by reading the abstract, and finally by assessing full texts; in case of disagreement between the two assessors, a third evaluator made the decision.
3.4Methodological quality
The methodological evaluation of the included RCTs was performed with the PEDro scale [14], extracting the total score on the PEDro website [www.pedro.org.au]. In case the score was not reported in the website, two assessors (EP and FS) individually attributed the score: in case of disagreement, a third assessor (FB) was involved in the decision. The PEDro scale is composed of 11 items, one point is awarded for each satisfied item and a high total score reflects a higher methodological quality. Authors suggested that scores of up to 4 points were considered ‘poor’, 4 to 5 points were considered ‘fair’, 6 to 8 points were considered ‘good’ and 9 to 10 points were considered ‘excellent’ [15]. Therefore, only studies with score
3.5Data extraction
Two researchers (EP and FS) collected data from the included studies, using a standardized data extraction form. They extracted from the studies information related to the characteristics of the patients (sample number, age, gender), the type of the experimental and control interventions, the outcome measures, and the follow-up.
For the extraction of data and information regarding the intervention, the TIDieR checklist [9] was used by the two evaluators (EP and FS). TIDieR is composed of 12 items: name, purpose, materials, procedure, who provided the intervention, how, where, when and how much, modifications, tailoring and adherence. In order to create a summary score for the description of the intervention, we added the scores for both TIDieR items, the intervention group and the control group. Each item was assessed on the 3-points Likert scale (0
3.6Risk of bias in individual studies
The assessment of the risk of bias in the included studies was performed individually by two reviewers (EP and FS), using the Cochrane Collaboration tool [18], which identifies five bias domains: selection bias, performance bias, detection bias, attrition bias and reporting bias. The risk of bias was assessed as “low” if it is unlikely to seriously alter the results, “high” if it can alter them, and “unclear” if it raises any doubts about the influence on the results.
4.Results
4.1Study selection
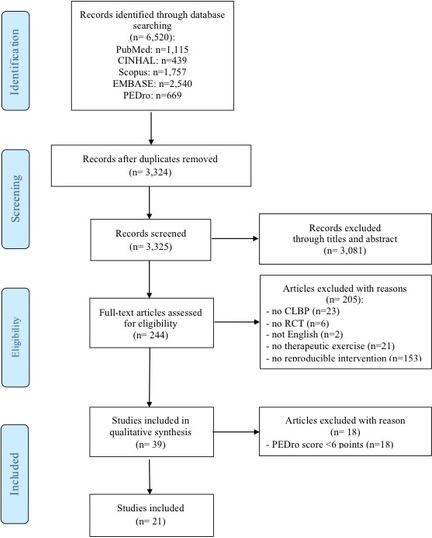
Of the 6520 articles retrieved from the electronic databases, only 21 articles qualified for inclusion in this systematic review, according to the eligibility criteria of the study especially as regards the intervention. Detailed information on each of the phases of the study selection is reported in Fig. 1.
Figure 1.
Flow diagram.
4.2Study characteristics
The studies included in this systematic review were RCTs published in English language, between 2011 and 2018. Detail about the included studies are reported in Table 1. A total of 702 subjects with cLBP in the intervention group and 725 in the control group were analyzed. The sample size in the intervention groups and in the comparison group varies from a minimum of 10 to a maximum of 74 with an average in the intervention group of 33.4 subjects (SD
In the intervention group 30% at least was female up to the maximum of 100% with an average age of 70.8 years (SD
In the experimental group of the included studies, the intervention involved TE in different forms: low load motor control exercises [21, 22], stretching [23], lumbar stabilization exercises [19], strengthening [24], trunk balance exercises [25], slump stretching [26], McKenzie exercise [27] that could be made alone [28] or within a multimodal program [29, 30] in combination with manual therapy [31, 32] or education on pain neurophysiology [33]. The comparison intervention in the included studies consists of other forms of TE: high load lifting exercises [21] stretching [20] motor control exercises [24, 34], aerobic activity [19], muscle strengthening [24], water exercises [35], advice on Activity of Daily Living [36], manual therapy [37], Behavioural Graded Activity [19], usual activity [23] , sham therapy [32], and in a wait list treatment [38]. These types of intervention could be associated with each other [29], as mobilization with exercise [26] or performed alone [27]. The interventions in the experimental groups were performed either in groups [39] or individually, the same thing for the comparison groups.
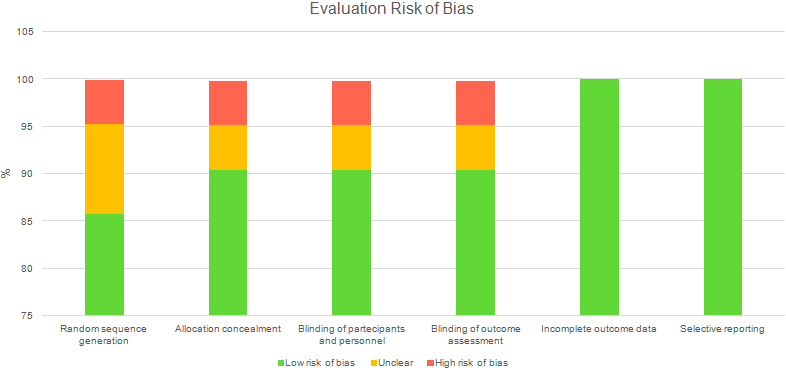
Figure 2.
Evaluation risk of bias.
The primary outcomes mainly concerned the measurement of the pain or disability, except for some studies that considered the displacement of lumbar movements and quality of life questionnaires as the primary outcome. Secondary outcomes concerned pain or disability or quality of life, while for some studies, secondary outcomes are represented by lumbar Range of Motion, strength tests, endurance and motor control, the presence of painful positions, and kinesiophobia. In the included studies, the outcomes were assessed with final follow up ranging from a minimum of 6 weeks [25] to a maximum of 24 months [24].
4.3Methodological quality
The included studies, through the evaluation with the PEDro scale, were of good quality as they scored 6 to 8 points, with an average of 6.8 points (SD
4.4Risk of bias within studies
The risk assessment of bias, performed through the Cochrane Collaboration tool, is reported in Fig. 2.
The risk of attrition bias and reporting bias was assessed as “low” in all studies included. The risk of selection bias, performance bias, detection bias, was assessed as “low” in 19 articles (90.4%), “unclear” in one article (4.8%) and “high” in one article (4.8%). The risk of selection bias (generation of the randomization sequence) was assessed as “low” in 18 articles (85.7%), “unclear” in 2 articles (9.5%) and “high” in one article (4.8%).
4.5Description of the interventions
The findings of the description, assessed through a TIDieR score, of the experimental and control interventions for each of the studies are reported in Table 2. Regarding the description of the experimental intervention a score ranging from a minimum of 8 to a maximum of 17 points (mean
5.Discussion
The aim of the systematic review was to assess reproducible therapeutic exercises for cLBP patients, using the TIDieR checklist. Reporting of interventions, especially in physiotherapy, is crucial as it influences the generalizability of the results; hence, the methods of the article should contain all the information necessary for the reader to be able to reproduce the intervention in clinical practice. The main findings on this topic consider the difficulty to have a clear description of the exercises, useful to combine the exercise therapy with new findings [40]. Our results showed that the TIDieR score is low in the description of both the experimental group and the control group in RCTs in patients with LBP; furthermore, many items were scarcely (or not at all) satisfied.
The interventions reported in Garcia et al. and in Aasa et al. RCT are the better reported [21, 27]. The study by Garcia et al. compares the effectiveness of Back School and McKenzie methods in patients with cLBP. The article provides detailed information about the intervention that makes it reproducible. For example, we know patients performed sessions of one-hour once a week for 4 weeks. All participants performed the exercises under the supervision of a physiotherapist. At the end of each session, the participants were asked to perform the same exercises at home, once a day, exercises well described and illustrated by photos. The directional preference could be modified during the sessions, if needed, and the therapist could increase the level of the exercises, tailoring the treatment according to the needs of each patient. The patient should perform the exercise of truck flexion for 3 sets of 10 repetitions
Table 2
TIDieR ’s score for experimental and control group
| Reference | Group | Item 1 Brief name | Item 2 Why | Item 3 What- Materials | Item 4 What- Procedures | Item 5 Who provided | Item 6 How | Item 7 Where | Item 8 When and how much | Item 9 Tailoring | Item 10 Modifications | Item 11 How well- Planned | Item 12 How well- Actual | Total score |
| Aasa et al., 2015 | Experimental | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 17 |
| Control | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 18 | |
| Bello et al., 2015 | Experimental | 2 | 1 | 0 | 2 | 0 | 0 | 2 | 2 | 0 | 0 | 0 | 0 | 9 |
| Control | 2 | 1 | 0 | 2 | 0 | 0 | 2 | 2 | 0 | 0 | 0 | 0 | 9 | |
| Balthazars et al., 2012 | Experimental | 2 | 2 | 0 | 2 | 2 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 10 |
| Control | 2 | 2 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 6 | |
| Bello et al., 2018 | Experimental | 2 | 2 | 0 | 2 | 0 | 1 | 0 | 2 | 0 | 0 | 0 | 0 | 9 |
| Control | 2 | 2 | 0 | 2 | 0 | 1 | 0 | 2 | 0 | 0 | 0 | 0 | 9 | |
| Chen et al., 2014 | Experimental | 0 | 2 | 0 | 2 | 1 | 0 | 2 | 2 | 0 | 0 | 0 | 0 | 9 |
| Control | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Costantino et al., 2014 | Experimental | 2 | 2 | 0 | 2 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 8 |
| Control | 2 | 2 | 0 | 2 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 8 | |
| Franca et al., 2012 | Experimental | 2 | 2 | 0 | 2 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 8 |
| Control | 2 | 2 | 0 | 2 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 8 | |
| Garcia et al., 2012 | Experimental | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 2 | 1 | 0 | 0 | 2 | 17 |
| Control | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 2 | 1 | 1 | 0 | 2 | 18 | |
| Gatti et al., 2011 | Experimental | 2 | 2 | 0 | 2 | 0 | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 14 |
| Control | 2 | 0 | 0 | 2 | 0 | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 10 | |
| Jaromi et al., 2017 | Experimental | 2 | 2 | 2 | 1 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 9 |
| Control | 2 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | |
| Kim et al., 2016 | Experimental | 2 | 2 | 0 | 2 | 0 | 2 | 1 | 2 | 0 | 0 | 0 | 2 | 13 |
| Control | 2 | 2 | 1 | 2 | 0 | 2 | 1 | 2 | 0 | 0 | 0 | 2 | 14 | |
| Michaelson et al., 2016 | Experimental | 2 | 2 | 0 | 2 | 0 | 2 | 0 | 2 | 0 | 0 | 0 | 2 | 12 |
| Control | 2 | 2 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 2 | 8 | |
| Monteiro et al., 2015 | Experimental | 2 | 2 | 0 | 2 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 8 |
| Control | 2 | 0 | 0 | 2 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 6 | |
| Nagrale et al., 2012 | Experimental | 2 | 2 | 0 | 2 | 0 | 1 | 2 | 2 | 0 | 0 | 0 | 0 | 11 |
| Control | 2 | 0 | 0 | 2 | 0 | 1 | 2 | 2 | 0 | 0 | 0 | 0 | 9 | |
| Noormohammadpour et al., 2018 | Experimental | 2 | 2 | 1 | 2 | 0 | 0 | 2 | 2 | 0 | 0 | 2 | 0 | 13 |
| Control | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | |
| Oliveira et al., 2017 | Experimental | 2 | 2 | 0 | 2 | 1 | 0 | 0 | 1 | 2 | 0 | 0 | 2 | 12 |
| Control | 2 | 0 | 0 | 2 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 2 | 8 | |
| Pardo et al., 2017 | Experimental | 2 | 2 | 0 | 2 | 0 | 2 | 0 | 2 | 1 | 0 | 0 | 0 | 11 |
| Control | 2 | 2 | 0 | 2 | 0 | 2 | 0 | 2 | 0 | 0 | 0 | 0 | 10 | |
| Rabin et al., 2014 | Experimental | 2 | 0 | 2 | 2 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 8 |
| Control | 2 | 0 | 2 | 2 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 8 | |
| Segal-Snir et al., 2016 | Experimental | 2 | 2 | 0 | 2 | 2 | 2 | 0 | 2 | 0 | 0 | 0 | 0 | 12 |
| Control | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | |
| Vergas et al., 2011 | Experimental | 2 | 2 | 0 | 2 | 0 | 2 | 0 | 2 | 0 | 0 | 0 | 0 | 10 |
| Control | 2 | 2 | 0 | 2 | 0 | 2 | 0 | 2 | 0 | 0 | 0 | 0 | 10 | |
| Zafereo et al, 2018 | Experimental | 2 | 2 | 0 | 2 | 2 | 0 | 2 | 2 | 0 | 0 | 0 | 0 | 12 |
| Control | 2 | 2 | 0 | 2 | 2 | 0 | 2 | 2 | 0 | 0 | 0 | 0 |
and the patient had three possible positions. The level of increase was considered only when symptoms remained unchanged, and stopped if the symptoms worsened.
The study by Aasa et al. compared the effects of low-load motor control (LMC) exercise and those of a high-load lifting (HLL) exercise. The LMC intervention was performed individually and the HLL included groups of 5 participants. Participants were offered 12 treatment sessions over an 8-weeks period. The duration of each session was 20 to 30 minutes for the LMC group and 60 minutes for the HLL group. The physiotherapists used different forms of feedback to teach and facilitate correct performance during the exercises. Participants in the HLL group were instructed that a pain intensity under 50 mm on a Visual Analog Scale was acceptable while performing the deadlift, provided that the pain subsided after each completed set and the movement pattern/spinal neutral position did not change. In the LMC group, the exercises were individually selected with the aim to normalize the dominating movement impairment for each participant. The strategy was to start from a basic level and continue to a gradually increased level of difficulty. It was considered important to always perform the movements ideally, preferably with an optimal muscle recruitment pattern. Regarding the home exercises, the participants were encouraged to make at least 10 repetitions, 2 to 3 times a day, with the goal to incorporate the new movement pattern into daily life. In stages 2 and 3, the participants were encouraged to focus on muscle recruitment and movement pattern during the activities and to perform them as often as possible. The physiotherapist selected appropriate initial weight on the bar, taught the participants an optimal lifting technique and ensured that the participants maintained a neutral alignment of the spine when performing the exercise. During the intervention period, the load was slowly increased, gradually increasing the number of lifts and/or the weight on the bar. The participants were encouraged to use the same lifting technique during daily activities. Both interventions resulted in significant within-group improvements in reduced pain intensity, strength, and endurance. The LMC group showed significantly greater improvement on the Patient-Specific Functional Scale compared with the HLL group (
The more relevant TIDieR items allowing replication are item 3 (What materials), item 8 (When and how much) and item (How)
In this review, in the interventions of the experimental groups, the item 3 (Materials) was not reported in 18 articles (85.7%), partially reported in two articles (9.5%) and adequately reported only in one (4.8%) study.
Item 6 (How) was not reported in 11 articles (52.4%), partially reported in two articles (9.5%) and adequately reported in item 8 (When and How Much) articles (38.1%).
Item 8 (When and How Much) was partially reported in one article (4.8%) and adequately reported in 20 articles (95.2%).
This review confirms the difficulty to find studies with a regular comprehensive reporting.
Figure 3.
TIDieR SCORE.
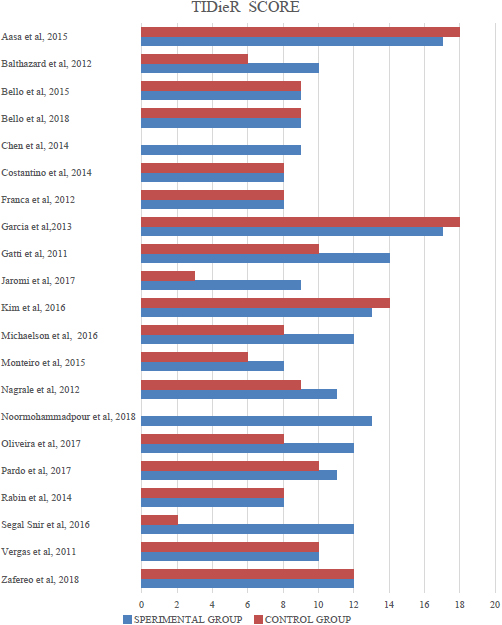
The items most poorly described in the experimental group, (Fig. 3) was item 3 (Materials), item 5 (Who provided), item 6 (How) [41], item 7 (Where), item 9 (Personalizing), item 10 (Modifications) and items 11 and 12 (Adherence). Lack of comprehensive reporting and monitoring of interventions makes it difficult for therapists to put exercises into practice and to make correct assumptions about exercise effectiveness, if it is unclear whether patients adhered to the protocol.
In control groups the interventions are less well-reported than in the experimental group, this is also documented in another study [42].
In addition, the items 11 and 12 (Adherence) in most of the cases are absent, even if it is considered as one of the important barriers for the efficacy of the exercise [43]. Hence, in clinical practice, during the planning of the exercise, the clinician implements strategies to improve the adherence of the exercise; these strategies should be reported in clinical trials to allow the clinician to be able to reproduce the exercise in all its aspects
The Good methodological quality of the studies considered does not coincide with an adequate and complete description of the interventions.
The results of the present study are in line with the study by Yamato et al. that considers the weakness of the exercise description in lots of trials. Of the intervention groups 23% report only half of the TIDieR items, and in the control group these data increase to 75% of the trials [11]. This is because most of the time exercises are described as “usual care” or “conventional treatment” without specifying the treatment modality, thus creating a barrier for the reproducibility [44]. For instance, the advice of an exercise is suggested to patients in only 19% of the cases during the usual care [44]. At the same time, the low reporting for the item Tailoring and Modification, items 9 and 10, is a serious shortcoming because during clinical practice often some modifications are needed [45].
The remarkable incompleteness of information necessary for intervention replication calls for actions [46, 47]. To address the problem of poor description of interventions within RCTs, we recommend that the TIDieR checklist be adopted by journals as a mandatory tool for guiding authors and reviewers [11, 48]. Many journals have limits on words; however, electronic resources can be used to provide more complete descriptions with interventions. For more complex interventions that are common in physiotherapy, using easily accessible videos or websites that demonstrate interventions used [49] should be considered. Such initiatives will reduce time wasted on futile and unproductive efforts and improve the applicability of the research. Finally, authors of systematic reviews and meta-analyses should consider the completeness of intervention descriptions as essential aspects for the evaluation of the usefulness of research evidence.
Wherever possible, the TIDieR checklist as well as other analytical reporting tools should guide the research of authors, reviewers and publishers in the various stages of publication. We need good quality research results that can be used and applied in a concrete and appropriate way.
This systematic review has limitations that should be discussed. Only 21 items were included out of over 6500 items found. Probably by broadening the inclusion criteria, probably more articles may have been included. Therefore this could limit the generalizability of the results to all types of low back pain. Furthermore, having included a wide range of age of patients (greater than 18 years), could be considered with a limit; on the other hand, the results of this systematic review can be applied to adult patients with LBP. Besides, it was not possible to perform a meta-analysis. For this reason, no new evidence can be seen throughout this study.
6.Conclusion
The findings of this study show defective reporting on interventions in high quality RCT on chronic low back pain (cLBP) is defective, jeopardizing the external validity of the results. More attention should be paid by researchers to the complete and accurate description of interventions reported in their studies in order to make them replicable in clinical practice. In the intervention of the exercise therapy proposed in a study the suggestion is to specify the intensity, the dose, the repetitions and the possibility to modify the program based for example in the improvement of the patient; in this way is very easy for the clinicians put into practice what the literature finds efficacy. Furthermore is important to considerate as outcome not only pain and the function but also the disability induced and perceived with cLBP.
The present authors wish to emphasize the urgent need for a call for action for researchers to use the TIDieR checklist in planning their exercise interventions to improve the replicability and the transparency of studies.
In the present study the interventions reported in Garcia et al. and in Aasa et al. RCTs, are considered as the better reported [21, 27]. In both these studies the score of the intervention description was 17 points for the experimental group and 18 points for the control group. Their articles provide detailed information about the interventions that make them reproducible by a physiotherapist.
Conflict of interest
None to report.
References
[1] | Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, et al. What low back pain is and why we need to pay attention. The Lancet. (2018) ; 391: (10137): 2356-67. |
[2] | Buchbinder R, van Tulder M, Oberg B, Costa LM, Woolf A, Schoene M, et al. Low back pain: a call for action. Lancet. (2018) ; 391: (10137): 2384-8. |
[3] | Wong JJ, Cote P, Sutton DA, Randhawa K, Yu H, Varatharajan S, et al. Clinical practice guidelines for the noninvasive management of low back pain: A systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Eur J Pain. (2017) ; 21: (2): 201-16. |
[4] | Qaseem A, Wilt TJ, McLean RM, Forciea MA. Noninvasive treatments for acute, subacute, and chronic low back pain: A clinical practice guideline from the american college of physicians. Annals of Internal Medicine. (2017) ; 166: (7). |
[5] | van Middelkoop M, Rubinstein SM, Verhagen AP, Ostelo RW, Koes BW, van Tulder MW. Exercise therapy for chronic nonspecific low-back pain. Best Pract Res Clin Rheumatol. (2010) ; 24: (2): 193-204. |
[6] | Excellence.NIfHaC, Low back pain and sciatica in over 16s: assessment and management, 2016. |
[7] | Miyamoto GC, Lin C-WC, Cabral CMN, van Dongen JM, van Tulder MW. Cost-effectiveness of exercise therapy in the treatment of non-specific neck pain and low back pain: a systematic review with meta-analysis. British Journal of Sports Medicine. (2019) ; 53: (3): 172-81. |
[8] | Smith BE, Littlewood C, May S. An update of stabilisation exercises for low back pain: a systematic review with meta-analysis. BMC Musculoskeletal Disorders. (2014) ; 15: (1). |
[9] | Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. (2014) ; 348: : g1687. |
[10] | Yamato T, Maher C, Saragiotto B, Moseley A, Hoffmann T, Elkins M, et al. Improving completeness and transparency of reporting in clinical trials using the template for intervention description and replication (TIDieR) checklist will benefit the physiotherapy profession. J Man Manip Ther. (2016) ; 24: (4): 183-4. |
[11] | Yamato TP, Maher CG, Saragiotto BT, Hoffmann TC, Moseley AM. How completely are physiotherapy interventions described in reports of randomised trials? Physiotherapy. (2016) ; 102: (2): 121-6. |
[12] | Yamato T, Maher C, Saragiotto B, Moseley A, Hoffmann T, Elkins M, Camargo PR. The TIDieR checklist will benefit the physical therapy profession. Brazilian Journal of Physical Therapy. (2016) ; 20: (3): 191-193. |
[13] | Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) ; 6: (7): e1000097. |
[14] | de Morton NA. The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Australian Journal of Physiotherapy. (2009) ; 55: (2): 129-33. |
[15] | Gonzalez GZ, Moseley AM, Maher CG, Nascimento DP, Costa L, Costa LO. Methodologic quality and statistical reporting of physical therapy randomized controlled trials relevant to musculoskeletal conditions. Arch Phys Med Rehabil. (2018) ; 99: (1): 129-36. |
[16] | Herbert RD, Gabriel M. Effects of stretching before and after exercising on muscle soreness and risk of injury: systematic review. Bmj. (2002) ; 325: (7362): 468. |
[17] | Yamato TP, Maher CG, Saragiotto BT, Catley MJ, Moseley AM. Rasch analysis suggested that items from the template for intervention description and replication (TIDieR) checklist can be summed to create a score. J Clin Epidemiol. (2018) ; 101: : 28-34. |
[18] | Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. (2011) ; 343: (Oct18 2): : d5928. |
[19] | Bello B, Adeniyi AF. Effects of lumbar stabilisation and treadmill exercise on function in patients with chronic mechanical low back pain. International Journal of Therapy and Rehabilitation. (2018) ; 25: (9): 493-9. |
[20] | Franca FR, Burke TN, Caffaro RR, Ramos LA, Marques AP. Effects of muscular stretching and segmental stabilization on functional disability and pain in patients with chronic low back pain: A randomized, controlled trial. J Manipulative Physiol Ther. (2012) ; 35: (4): 279-85. |
[21] | Aasa B, Berglund L, Michaelson P, Aasa U. Individualized low-load motor control exercises and education versus a high-load lifting exercise and education to improve activity, pain intensity, and physical performance in patients with low back pain: a randomized controlled trial. J Orthop Sports Phys Ther. (2015) ; 45: (2): 77-85, B1-4. |
[22] | Monteiro-Junior R, de Souza C, Lattari E, Rocha N, Mura G, Machado S, et al. Wii-workouts on chronic pain, physical capabilities and mood of older women: A randomized controlled double blind trial. CNS & Neurological Disorders – Drug Targets. (2015) ; 14: (9): 1157-64. |
[23] | Chen HM, Wang HH, Chen CH, Hu HM. Effectiveness of a stretching exercise program on low back pain and exercise self-efficacy among nurses in Taiwan: a randomized clinical trial. Pain Manag Nurs. (2014) ; 15: (1): 283-91. |
[24] | Michaelson P, Holmberg D, Aasa B, Aasa U. High load lifting exercise and low load motor control exercises as interventions for patients with mechanical low back pain: A randomized controlled trial with 24-month follow-up. J Rehabil Med. (2016) ; 48: (5): 456-63. |
[25] | Gatti R, Faccendini S, Tettamanti A, Barbero M, Balestri A, Calori G. Efficacy of trunk balance exercises for individuals with chronic low back pain: a randomized clinical trial. J Orthop Sports Phys Ther. (2011) ; 41: (8): 542-52. |
[26] | Nagrale AV, Patil SP, Gandhi RA, Learman K. Effect of slump stretching versus lumbar mobilization with exercise in subjects with non-radicular low back pain: a randomized clinical trial. J Man Manip Ther. (2012) ; 20: (1): 35-42. |
[27] | Garcia AN, Costa Lda C, da Silva TM, Gondo FL, Cyrillo FN, Costa RA, et al. Effectiveness of back school versus McKenzie exercises in patients with chronic nonspecific low back pain: a randomized controlled trial. Phys Ther. (2013) ; 93: (6): 729-47. |
[28] | Costantino C, Romiti D. Effectiveness of Back School program versus hydrotherapy in elderly patients with chronic non-specific low back pain: a randomized clinical trial. Acta Biomed. (2014) ; 85: (3): 52-61. |
[29] | Cuesta-Vargas AI, Garcia-Romero JC, Arroyo-Morales M, Diego-Acosta AM, Daly DJ. Exercise, manual therapy, and education with or without high-intensity deep-water running for nonspecific chronic low back pain: A pragmatic randomized controlled trial. Am J Phys Med Rehabil. (2011) ; 90: (7): 526-34; quiz 35-8. |
[30] | Magalhaes MO, Comachio J, Ferreira PH, Pappas E, Marques AP. Effectiveness of graded activity versus physiotherapy in patients with chronic nonspecific low back pain: midterm follow up results of a randomized controlled trial. Braz J Phys Ther. (2018) ; 22: (1): 82-91. |
[31] | Zafereo J, Wang-Price S, Roddey T, Brizzolara K. Regional manual therapy and motor control exercise for chronic low back pain: a randomized clinical trial. Journal of Manual & Manipulative Therapy. (2018) ; 26: (4): 193-202. |
[32] | Balthazard P, de Goumoens P, Rivier G, Demeulenaere P, Ballabeni P, Deriaz O. Manual therapy followed by specific active exercises versus a placebo followed by specific active exercises on the improvement of functional disability in patients with chronic non specific low back pain: a randomized controlled trial. BMC Musculoskelet Disord. (2012) ; 13: : 162. |
[33] | Bodes Pardo G, Lluch Girbes E, Roussel NA, Gallego Izquierdo T, Jimenez Penick V, Pecos Martin D. Pain neurophysiology education and therapeutic exercise for patients with chronic low back pain: A single-blind randomized controlled trial. Arch Phys Med Rehabil. (2018) ; 99: (2): 338-47. |
[34] | Kim YW, Kim NY, Chang WH, Lee SC. Comparison of the therapeutic effects of a sling exercise and a traditional stabilizing exercise for clinical lumbar spinal instability. J Sport Rehabil. (2018) ; 27: (1): 47-54. |
[35] | D.CCR, Effectiveness of Back School program versus hydrotherapy in elderly patients with chronic non-specific low back pain: a randomized clinical trial, Acta Biomed, 2014. |
[36] | Jaromi M, Kukla A, Szilagyi B, Simon-Ugron A, Bobaly VK, Makai A, et al. Back School programme for nurses has reduced low back pain levels: A randomised controlled trial. J Clin Nurs. (2018) ; 27: (5-6): e895-e902. |
[37] | Rabin A, Shashua A, Pizem K, Dickstein R, Dar G. A clinical prediction rule to identify patients with low back pain who are likely to experience short-term success following lumbar stabilization exercises: a randomized controlled validation study. J Orthop Sports Phys Ther. (2014) ; 44: (1): 6-B13. |
[38] | Noormohammadpour P, Kordi M, Mansournia MA, Akbari-Fakhrabadi M, Kordi R. The role of a multi-step core stability exercise program in the treatment of nurses with chronic low back pain: A single-blinded randomized controlled trial. Asian Spine Journal. (2018) ; 12: (3): 490-502. |
[39] | Segal-Snir Y, Lubetzky VA, Masharawi Y. Rotation exercise classes did not improve function in women with non-specific chronic low back pain: A randomized single blind controlled study. J Back Musculoskelet Rehabil. (2016) ; 29: (3): 467-75. |
[40] | Holden S, Rathleff MS, Jensen MB, Barton CJ. How can we implement exercise therapy for patellofemoral pain if we don’t know what was prescribed? A systematic review. British Journal of Sports Medicine. (2018) ; 52: (6): 385. |
[41] | Cotterill S, Knowles S, Martindale A-M, Elvey R, Howard S, Coupe N, et al. Getting messier with TIDieR: embracing context and complexity in intervention reporting. BMC Medical Research Methodology. (2018) ; 18: (1). |
[42] | Hariohm K, Jeyanthi S, Kumar JS, Prakash V. Description of interventions is under-reported in physical therapy clinical trials. Braz J Phys Ther. (2017) ; 21: (4): 281-6. |
[43] | Palazzo C, Klinger E, Dorner V, Kadri A, Thierry O, Boumenir Y, et al. Barriers to home-based exercise program adherence with chronic low back pain: Patient expectations regarding new technologies. Ann Phys Rehabil Med. (2016) ; 59: (2): 107-13. |
[44] | Kamper SJ, Logan G, Copsey B, Thompson J, Machado GC, Abdel-Shaheed C, et al. What is usual care for low back pain? A systematic review of health care provided to patients with low back pain in family practice and emergency departments. Pain. (2020) ; 161: (4): 694-702. |
[45] | Slade SC, Kent P, Patel S, Bucknall T, Buchbinder R. Barriers to primary care clinician adherence to clinical guidelines for the management of low back pain: A systematic review and metasynthesis of qualitative studies. Clin J Pain. (2016) ; 32: (9): 800-16. |
[46] | Pool J, Maissan F, de Waele N, Wittink H, Ostelo R. Completeness of the description of manipulation and mobilisation techniques in randomized controlled trials in neck pain; A review using the TiDieR checklist. Musculoskelet Sci Pract. (2020) ; 45: : 102098. |
[47] | Bartholdy C, Nielsen SM, Warming S, Hunter DJ, Christensen R, Henriksen M. Poor replicability of recommended exercise interventions for knee osteoarthritis: a descriptive analysis of evidence informing current guidelines and recommendations. Osteoarthritis Cartilage. (2019) ; 27: (1): 3-22. |
[48] | Hoffmann TC, Oxman AD, Ioannidis JP, Moher D, Lasserson TJ, Tovey DI, et al. Enhancing the usability of systematic reviews by improving the consideration and description of interventions. BMJ. (2017) ; 358: : j2998. |
[49] | Candy B, Vickerstaff V, Jones L, King M. Description of complex interventions: analysis of changes in reporting in randomised trials since 2002. Trials. (2018) ; 19: (1): 110. |
Appendices
Appendix
Search strings.
| Pubmed | ((Back pain [Mesh]) OR (Low Back Pain [Mesh]) OR (Back Injuries [Mesh]) OR (LBP) OR (CLBP) OR (Backache) OR (Lumbago) OR (Back Injur*) OR (Lumbar pain) OR (Back disorde*) OR (Back Pain)) AND (“Exercise”[Mesh] OR “Exercise Movement Techniques”[Mesh] OR “Exercise Therapy”[Mesh] OR (Exercis*)) AND ((randomized[Title/Abstract] AND controlled[Title/Abstract] AND trial [Title/Abstract]) OR (randomised[Title/Abstract] AND controlled[Title/Abstract] AND trial[Title/Abstract]) OR ((“Randomized Controlled Trials as Topic”[Mesh]) OR “Randomized Controlled Trial” [Publication Type])) Using filter HUMANS Using filter RANDOMIZED CONTROLLED TRIAL |
|---|---|
| CINAHL | (TX |
| PEDro | Exercise AND “back pain” Using filter Method: Clinica trial |
| EMBASE | (‘low back pain’/exp OR ‘low back pain’ OR (low AND (‘back’/exp OR back) AND (‘pain’/exp OR pain)) OR lbp OR clbp OR ‘backache’/exp OR backache OR ‘lumbago’/exp OR lumbago OR ‘lumbar pain’/exp OR ‘lumbar pain’ OR (lumbar AND (‘pain’/exp OR pain)) OR ((‘back’/exp OR back) AND disorde*) OR ‘back pain’/exp OR ‘back pain’ OR ((‘back’/exp OR back) AND (‘pain’/exp OR pain))) AND (‘exercise’/exp OR exercis*) AND ((randomized AND controlled AND trial) OR ‘randomized controlled trial’:it OR (randomised AND controlled AND trial)) |
| Scopus | (((TITLE-ABS-KEY (randomized AND controll ed AND trials) OR SRCTITLE (randomized A ND controlled AND trial)) AND DOCTYPE (ar OR re)) OR ((TITLE-ABS-KEY (randomised) AND TITLE-ABS-KEY (controlled) AND TITLE-ABS-KEY (trial)) AND DOCTYPE (ar OR re)) OR ((TITLE-ABS-KEY (randomized) AND TITLE-ABS-KEY (controlled) AND TIT LE-ABS-KEY (trial)) AND DOCTYPE (ar OR re))) AND ((TITLE-ABS-KEY (back AND pain) OR TITLE-ABS-KEY (low AND back AND pain) OR TITLE-ABS-KEY (back AND injures) OR TITLE-ABS-KEY (lbp) OR TITLE-ABS-K EY (clbp) OR TITLE-ABS-KEY (backache) OR TITLE-ABS-KEY (lumbago) OR TITLE-ABSKEY (back AND injur*) OR TITLE-ABS-KEY (lumbar AND pain) OR TITLE-ABS-KEY (back AND disorde*) OR TITLE-ABS-KEY (back AND pain)) AND DOCTYPE (ar OR re)) AN D ((TITLE-ABS-KEY (exercise) OR TITLE-AB S-KEY (exercise AND movement AND techniq ues) OR TITLE-ABS-KEY (exercis*) OR TITL E-ABS-KEY (exercise AND therapy))) AND (LI M IT-TO (DOCTYPE , ‘ar’)) |




