Physiotherapy treatment of lateral epicondylitis: A systematic review
Abstract
BACKGROUND:
Lateral epicondylitis is a tendinopathy with a prevalence of between 1–3% of the population aged 35–54 years. It is a pathology with a favorable evolution, but with frequent recurrences (which imply an economic extra cost).
OBJECTIVE:
The objective of this review was to determine the efficacy of physiotherapy treatment for the treatment of epicondylitis and, if any, to identify the most appropriate techniques.
METHODS:
A systematic search was carried out in October 2020 in the databases of PubMed, Cinahl, Scopus, Medline and Web of Science using the search terms: Physical therapy modalities, Physical and rehabilitation medicine, Rehabilitation, Tennis elbow and Elbow tendinopathy.
RESULTS:
Nineteen articles were found, of which seven applied shock waves, three applied orthoses, three applied different manual therapy techniques, two applied some kind of bandage, one applied therapeutic exercise, one applied diacutaneous fibrolysis, one applied high intensity laser, and one applied vibration.
CONCLUSIONS:
Manual therapy and eccentric strength training are the two physiotherapeutic treatment methods that have the greatest beneficial effects, and, furthermore, their cost-benefit ratio is very favorable. Its complementation with other techniques, such as shock waves, bandages or Kinesio
1.Introduction
Lateral epicondylitis (LE) is a tendinopathy of the forearm extensor muscles, often caused by overuse or repetitive use (mostly of the extensor carpi radialis brevis), forced extension or direct trauma in the epicondyle [1]. Histologically, it presents signs of tendon degeneration, such as the presence of fibroblasts, vascular hyperalgesia and disorganised collagen [2]. The pain is usually localised in the epicondyle, although in more severe cases it can expand to the shoulder and wrist, and it is usually triggered by exerting pressure on the epicondyle, resisting wrist and/or third finger extension and stretching of the epicondylar muscles [3]. LE has an approximate rate of 40% and a prevalence of 1–3% of the general population, being most common in the age range of 35–54 years [4, 5]. Regarding duration, its natural evolution is considered to be favourable at two years, since it usually relapses after asymptomatic periods. Due to the latter phenomenon, this disorder implies a great economic investment [4].
Table 1
Search strategy according to the focused question (PICO)
| Database | Search equation |
|---|---|
| PubMed | (“Physical Therapy Modalities”[Mesh]) AND “Tennis Elbow”[Mesh] |
| (“Physical Therapy Modalities”[Mesh]) AND “Elbow Tendinopathy”[Mesh] | |
| (“Rehabilitation”[Mesh] AND “Tennis Elbow”[Mesh]) | |
| (“Rehabilitation”[Mesh] AND “Elbow Tendinopathy”[Mesh]) | |
| Medline | (MH “Physical Therapy Modalities”) AND (MH “Tennis Elbow”) |
| (MH “Physical Therapy Modalities”) AND (MH “Elbow Tendinopathy”) | |
| (MH “Rehabilitation”) AND (MH “Tennis Elbow”) | |
| (MH “Rehabilitation”) AND (MH “Elbow tendinopathy”) | |
| Cinahl | (MH “Physical Therapy”) AND (MH “Tennis Elbow”) |
| (MH “Physical Therapy”) AND (MH “Elbow tendinopathy”) | |
| (MH “Rehabilitation”) AND (MH “Tennis Elbow”) | |
| (MH “Rehabilitation”) AND (MH “Elbow tendinopathy”) | |
| Web of science | TOPIC: (‘physical therapy modalities’) AND TOPIC: (‘tennis elbow’) |
| TOPIC: (‘physical therapy modalities’) AND TOPIC: (‘elbow tendinopathy’) | |
| TOPIC: (‘rehabilitation’) AND TOPIC: (‘elbow tendinopathy’) | |
| TOPIC: (‘rehabilitation’) AND TOPIC: (‘tennis elbow’) | |
| Scopus | ( TITLE-ABS-KEY (“Physical Therapy Modalities”) AND TITLE-ABS-KEY (“Tennis Elbow”)) AND PUBYEAR |
| (TITLE-ABS-KEY (“Physical Therapy Modalities”) AND TITLE-ABS-KEY (“Elbow tendinophaty”)) AND PUBYEAR | |
| (TITLE-ABS-KEY (“rehabilitation”) AND TITLE-ABS-KEY (“Tennis Elbow”)) AND PUBYEAR | |
| (TITLE-ABS-KEY (“rehabilitation”) AND TITLE-ABS-KEY (“Elbow tendinophaty”)) AND PUBYEAR |
Different treatment approaches have been proposed, such as the recommendation of rest, drugs, surgery, etc. [6]. The first therapeutic step usually involves rest and the administration of drugs that provide short-term pain relief, but also bad results for the resolution of the problem and for the prevention of relapses [7]. With the surgical approach, immediate pain relief is achieved in 80–97% of cases, although 1.5% of intervened patients underwent a second surgical procedure in the following 18–24 months [8]. Lastly, the physiotherapeutic treatment has been shown to be effective [2] and, in general, it must include manual therapy to relieve the pain and improve the joint’s range of motion (ROM) [6], taking into account that it must be performed under the pain threshold [9]. It is worth highlighting that, in this pathology, as in the rest of tendinopathies, good results are obtained from strengthening the affected area [10]; for example, eccentric training has been reported to decrease pain and improve functionality, since, during exercise: (a) the blood flow in the neovessels of the tendon is temporarily interrupted; (b) a constant mechanical stimulus is generated, which would lead to the remodeling of the tendon, and (c) collagen synthesis increases in damaged tendons [11, 12].
The aim of this review was to determine the efficacy of the new physical therapy (PT) techniques for the treatment of LE that have been studied in the last years and identify the most adequate techniques.
2.Materials and methods
2.1Search strategy and information sources
This study was registered on PROSPERO (ID: CRD42021230014) and followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guidelines and the recommendations from the Cochrane Collaboration [13, 14]. The PICO question was then chosen as follows: P – population: men and women diagnosed with LE; I – intervention: physical therapy techniques; C – control: different physiotherapy and/or pharmacological treatment interventions (platelet-rich plasma, corticosteroids and naproxen); O – outcome: intensity and frequency of pain, range of movement and degrees of functionality and perceived disability, mainly; S – study designs: experimental studies.
A systematic search of publications was conducted in Ocotber 2020 in the following databases: PubMed, SpringerLink, SportsDiscus, Medline, Scopus, and Web of Science. The search strategy included different combinations with the following Medical Subject Headings (MeSH) terms: Physical therapy modalities, Physical and rehabilitation medicine, Rehabilitation, Tennis elbow and Elbow tendinopathy. The search strategy according to the focused PICOS question is presented in Table 1.
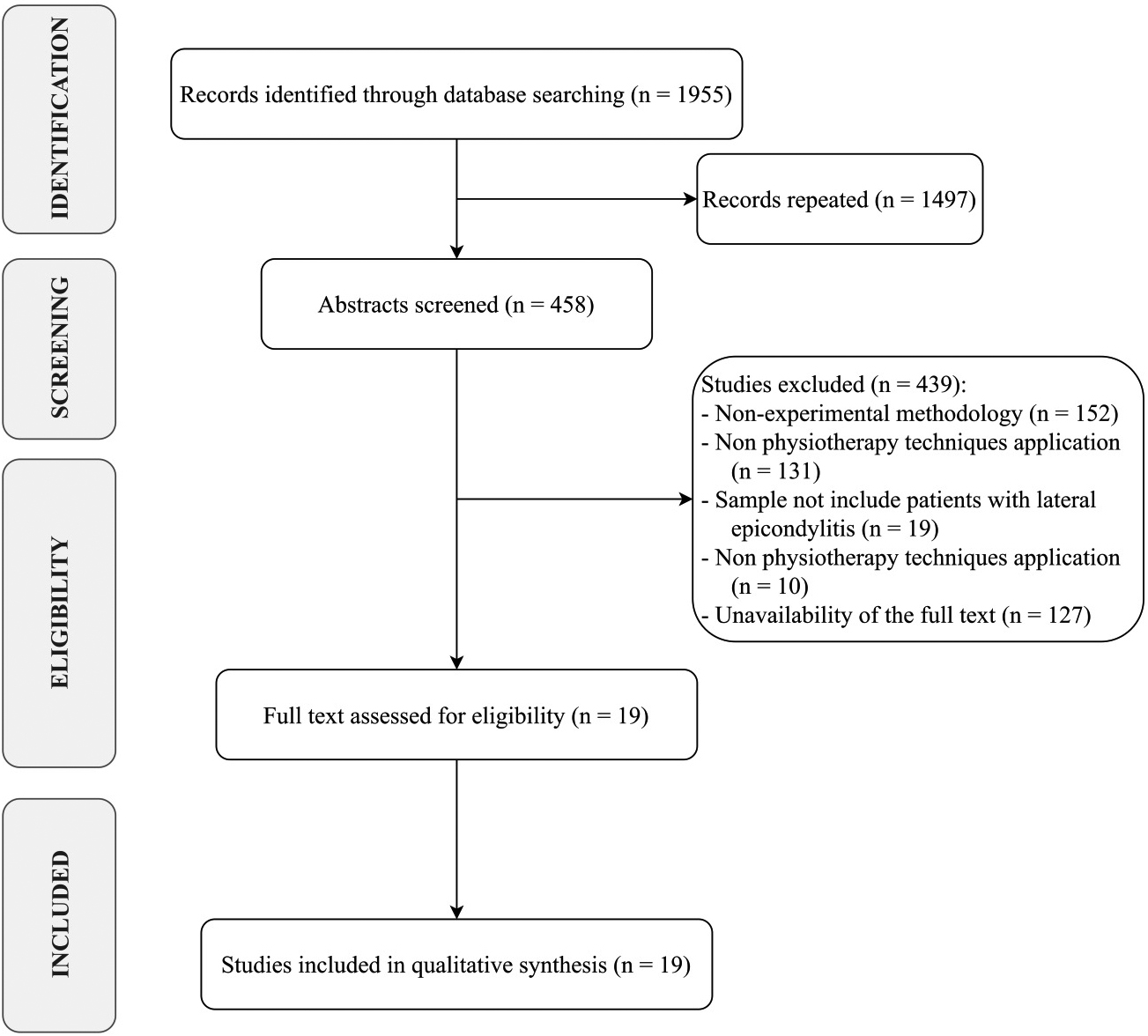
Figure 1.
PRISMA flow diagram.
2.2Eligibility criteria
After removing duplicates, two reviewers (L.L.-P. and R.L.-R.) independently screened articles for eligibility. In case of disagreement, both reviewers debated until an agreement was reached. For the selection of results, the inclusion criteria established that the articles must have been published in the last five years (from 2015 to the present), that the sample of studies consisted exclusively of patients with LE (regardless of its duration) and that the authors applied a treatment intervention that included at least one physical therapy technique. On the other hand, studies were excluded from this review if they had a non-experimental methodology and their full text was not available.
2.3Study selection, data collection process, data items and summary measures
After screening the data, extracting, obtaining and screening the titles and abstracts for inclusión criteria, the selected abstracts were obtained in full texts. Titles and abstracts lacking suficient information regarding inclusion criteria were also obtained as full texts. Full text articles were selected in case of compliance with inclusion criteria by the two reviewers using a data extraction form. The two reviewers mentioned independently extracted data from included studies using a customized data extraction table in Microsoft Excel. In case of disagreement, both reviewers debated until an agreement was reached.
The following data from the included articles for further analysis: demographic information (title, authors, journal and year), characteristics of the sample (age, inclusion and exclusion criteria, and number of participants), study-specific parameter (study type, duration of intervention, number of sessions, techniques of physical therapy included in the intervention, follow-up and drop-out) and results obtained. Tables were used to describe both the studies’ characteristics and the extracted data. When possible, the results were gathered based on type of intervention applied. The Oxford 2011 Levels of Evidence and the Jadad scale were used to assess the quality of studies.
3.Results
3.1Study selection
Out of 1955 search results, 458 studies were considered eligible for inclusion after removing duplicates. Among the 458 papers screened, 439 were excluded after abstract and title screening. Kappa score of reviewer 1 and 2 was 0.187, indicating slight agreement. Of the 19 full-text articles assessed for eligibility, all were finally included in the synthesis, as depicted by the PRISMA flowchart in Fig. 1.
3.2Study characteristics and risk of bias
All the studies have been published in the last 5 years (from 2015 to 2020). Of the 19 articles, seven applied extracorporeal shock waves (SW) [15, 16, 17, 18, 19, 20, 21], five applied ultrasounds (US) [15, 16, 19, 22, 23], five applied conventional physiotherapy techniques (thermotherapy [19], electrotherapy [19, 21, 23], cryotherapy [21], education [24, 25]), six manual therapy [22, 23, 24, 26, 27, 28], seven applied orthoses or taping techniques [21, 22, 25, 28, 29, 30, 31], nine applied therapeutic exercises [17, 21, 22, 24, 25, 28, 30, 31, 32], and one applied a laser [33]. The methodological characteristics of the analysed studies are shown in Table 2 and the characteristics of the interventions applied in them are presented in Table 3.
Regarding the experimental designs, 14 studies were randomized and controlled trials [15, 16, 17, 21, 22, 23, 24, 25, 26, 28, 30, 31, 32, 33] and the remaining five studies were quasi-experimental [18, 19, 20, 27, 29].
The methodological quality of the studies was three points or more on the JADAD scale in 52.6% of the studies [17, 21, 22, 23, 25, 30, 31, 33] but was zero in 26.3% of the results [18, 19, 20, 27, 29]. At the same time, as can be seen in Table 2, the level of evidence provided was between I (73.7%) [15, 16, 17, 21, 22, 23, 24, 25, 26, 28, 30, 31, 32, 33] and II (26.3%) [18, 19, 20, 27, 29].
3.3Results of individual studies
One of the revised studies evaluated the effect of SW [17] in combination and comparison with a programme of strength and mobility exercises. The application of SW was conducted in two stages: in the first stage, the energy density was 0.348 mJ/cm
Two studies were aimed at comparing the effects of US and SW [15, 16]. One of them applied the SW sessions divided into two phases: a first phase of 2000 pulses, at 8 Hz and 1.5–2.5 bar in the epicondylar region, and a second phase of 2000 pulses, at 8 Hz and 2.5–3.5 bar in the extensor carpi radialis brevis [16]. The other study applied a total of 2000 pulses at a frequency of 10–15 Hz and 1.5–2.5 bar, using ultrasound gel as the means of transmission [15]. The parameters of US application were also different. In one of the studies, the authors applied a first phase with a head of 5 cm
Alessio-Mazzola el al. [20] compared the efficacy of the platelet-rich plasma (PRP) treatment with that of SW. Their intervention with echo-guided SW had a frequency of 4 Hz, an intensity compatible with pain tolerance (initially 0.03–0.07 mJ/mm
Table 2
Methodological characteristics of the studies analyzed
| Authors | Design | Sample size | Inclusion criteria | Exclusion criteria | Jadad scale | LE | |||
|---|---|---|---|---|---|---|---|---|---|
| RD | BD | WD | FS | ||||||
| Alessio-Mazzola et al. (2018) | QES | 63 | Pain of more than six months of evolution, persistence of pain and functional deterioration refractory to rest, ice and pharmacological therapy. Persistence of symptoms after previous treatments (laser, radiofrequency, ultrasound and electrotherapy). Previous treatments completed more than six months before. | Consumption of simultaneous drug treatment. Carry a pacemaker. History of surgery or trauma to the affected elbow, neurological or musculoskeletal disorders. Diagnosis of systemic diseases, blood disorder, epilepsy or infections. Presence of malformations or open wounds on the affected arm. Pregnant or lactating women. | 0 | 0 | 0 | 0 | II |
| Altun et al. (2018) | QES | 73 | Pain of more than six weeks of evolution, age over 18 years, tenderness to palpation anterior and distal to the epicondyle, positive test in resisted wrist extension with the elbow in extension and the forearm in pronation. | Diagnosis of nerve compression syndrome or cervical radiculopathy. History of surgery or trauma to the region. No consent to participate in the study. | 0 | 0 | 0 | 0 | II |
| Dones III et al. (2018) | QES | 23 | Positive result in the Cozen, Mill or Maudsley tests. | Physiotherapy treatment of the elbow in the last six months. Presence of orthopedic alterations or paresthesias in the elbow. History of fracture, arthritis, or nerve compression of the elbow. Multiple sclerosis diagnosis. | 0 | 0 | 0 | 0 | II |
| Dundar et al. (2015) | RCT | 93 | Pain in the epicondyle of less than three months of evolution. Tenderness to palpation of the epicondyle. Pain on wrist movement and/or third finger extension against resistance. Positive result to Mill’s test. | Diagnosis of fibromyalgia, rheumatoid arthritis, osteoarthritis, inflammatory arthropathy, carpal and/or ulnar tunnel syndrome, cervical radiculopathy, neurological deficit, systemic metabolic diseases, cervical and/or shoulder disorders. Previous treatment of epicondylitis. History of surgery, fracture in the elbow. Bilateral elbow pain. | 1 | 1 | 1 | 3 | I |
| Eraslan et al. (2017) | RCT | 45 | Diagnosis of lateral epicondylitis of more than three months of evolution, pain in the epicondyle and during the grip strength test, to the wrist extension against resistance or to the passive stretching of the wrist extensors. | Receipt of any other treatment during the study period. Diagnosis of inflammatory, autoimmune, endocrine or kidney diseases, cubital or carpal tunnel syndrome, cervical radiculopathy, arthritis, allergy to bandages or other pathologies in the affected upper limb. History of surgery or trauma to the affected upper limb or corticosteroid treatment in the previous three months. | 2 | 0 | 1 | 3 | I |
| Furnes et al. (2018) | RCT | 45 | Diagnosis of lateral epicondylitis. Older than 18 years. Pain at wrist extension and third finger against resistance. | Diagnosis of inflammatory arthritis, deformity in the affected elbow. History of surgery, shock wave treatments or injections in the affected elbow. | 1 | 0 | 1 | 2 | I |
| Giray et al. (2019) | RCT | 30 | Pain of less than three months of evolution, presence of pain in the lateral epicondyle, positive result in the Maudley and/or Mill test. Diagnosis of lateral epicondylitis confirmed by ultrasound. | Diagnosis of cervical spondylosis or radiculopathy, diabetes mellitus, concomitant neuropathy, polyneuropathy, systemic arthritics. History of surgery or trauma to the elbow, injections and/or physical therapy treatment to the elbow. Bandage allergy. Pregnancy. | 2 | 2 | 1 | 5 | I |
|
Table 2, continued | |||||||||
| Authors | Design | Sample size | Inclusion criteria | Exclusion criteria | Jadad scale | LE | |||
| RD | BD | WD | FS | ||||||
| Gönen et al. (2017) | RCT | 46 | Result on the Visual Analogue Scale greater than 6, pain of less than three months of evolution, no previous treatment in the affected area, complete follow-up after receiving the intervention. | Other diagnoses in the cervical spine, upper limbs, vasculitis, infections, malignant diseases, connective tissue, rheumatic, dermatological or neurological. Pregnancy, Anticoagulant treatment. Age under 18 years. Invasive treatments in the previous three months. | 2 | 0 | 1 | 3 | I |
| Kachanat et al. (2019) | RCT | 40 | Pain of more than three months of evolution, limited range of motion of flexion and extension of the wrist and weakness in grip strength. | History of surgery, dislocation, fracture, osteoarthritis, or corticosteroid injection in the elbow. | 2 | 2 | 1 | 5 | I |
| Köksal et al. (2015) | QES | 54 | Diagnosis of lateral epicondylitis. | Diagnosis of local infection, arthritis, or bleeding disorder. Age under 18 years. Pregnancy. | 0 | 0 | 0 | 0 | II |
| Kubot et al. (2017) | RCT | 60 | Result on the Visual Analogue Scale higher than 6, pain of less than three months of evolution, no previous treatment in the affected area in the previous three months, complete follow-up after receiving the intervention. | Other diagnoses in the cervical spine, upper limbs, vasculitis, infections, malignant diseases, connective tissue, rheumatic, dermatological or neurological. Pregnancy, Anticoagulant treatment. Age under 18 years. Invasive treatments in the previous three months. | 2 | 0 | 0 | 2 | I |
| López-Celis et al. (2018) | RCT | 54 | Diagnosis of lateral epicondylitis. Presence of pain of more than three months of evolution. Positive result in the Cozen and/or Mill test. Age over 18 years. Delivery of informed consent for participation in the study. | Diagnosis of other concomitant pathologies in the affected upper limb, of inflammatory processes, contraindications for diacutaneous fibrolysis. History of previous surgery in the affected elbow or of injections in the previous three months in the affected elbow. | 2 | 2 | 1 | 5 | I |
| Nishizuka et al. (2016) | RCT | 110 | Pain of more than a week of evolution and on anterior and distal palpation of the epicondyle. Positive result to the Thomsen test. | Diagnosis of bilateral lateral epicondylitis or osteoarthritis History of elbow surgery. Previous treatments in the elbow or use of corticosteroids in the previous six months. | 2 | 0 | 1 | 3 | I |
| Nowotny et al. (2018) | RCT | 31 | Result in the Placzek score higher than 4. Delivery of informed consent for participation in the study. | History of surgery or elbow fracture. Diagnosis of rheumatic arthritis, elbow instability, extensor radius tendon rupture, or cervical radiculopathy. | 2 | 0 | 1 | 3 | I |
| Olaussen et al. (2015) | RCT | 177 | Presence of pain at the resisted dorsiflexion of the wrist with the elbow extended, at the resisted extension of the third finger and/or at the radial deviation of the wrist of less than three months of evolution. | Bilateral pain and/or of less than two months of evolution, treatment with corticosteroids and/or physiotherapy during the previous year. History of previous surgery on the elbow. Presence of deformities in the elbow, referred pain in the neck and/or shoulder, fractures or ruptures of tendons of the forearm. Diagnosis of cervical radiculopathy, systemic musculoskeletal diseases, contraindications to corticosteroids, lidocaine or anti-inflammatory drugs. Pregnant or lactating women. | 1 | 0 | 1 | 2 | I |
|
Table 2, continued | |||||||||
| Authors | Design | Sample size | Inclusion criteria | Exclusion criteria | Jadad scale | LE | |||
| RD | BD | WD | FS | ||||||
| Seo et al. (2018) | QES | 20 | Diagnosis of lateral epicondylitis. | Diagnosis of orthopedic or nervous system abnormalities affecting the arm or upper limb neuropathy. | 0 | 0 | 0 | 0 | II |
| Stasino-poulos et al. (2016) | RCT | 34 | Diagnosis of lateral epincondylitis of more than a month of evolution. Pain on palpation of the epicondyle. Positive result in at least two of the following tests: Thomsen test, third finger against resistance, mill, force with grip dynamometer. | Diagnosis of some dysfunction of the shoulder, neck and/or chest, arthritis, neurological deficit, radial nerve entrapment. History of surgery on the elbow or of previous treatments for lateral epicondylitis during the month before the study. | 1 | 2 | 1 | 4 | I |
| Yalvaç et al. (2018) | RCT | 50 | Medical diagnosis of lateral epicondylitis, pain of more than three months of evolution, positive tests in wrist extension, third finger extension and passive wrist flexion. | History of elbow surgery and/or elbow or arm fracture. Corticosteroid treatment in the previous month. Diagnosis of cervical radiculopathy, neuropathic entrapment, acute infection or vascular disorder, Carrier of pacemaker or interstitial implant. | 2 | 1 | 1 | 4 | I |
| Yi et al. (2018) | RCT | 34 | Pain of less than six months of evolution, age older than 18 years, sensitivity to palpation anterior and distal to the epicondyle, positive result in the resistance wrist extension tests with the elbow in extension and the forearm in pronation. Delivery of informed consent for participation in the study. | Diagnosis of nerve compression syndrome, cervical radiculopathy, pain of less than six weeks of evolution. History of previous surgery or trauma to the elbow. | 1 | 0 | 1 | 2 | I |
GD: Gestational diabetes; LE: Level of evidence; LOS: Longitudinal observational study; QES: Quasi-Experimental study; RCT: Randimized controlled trial.
Table 3
Characteristics of the interventions of the studies analyzed
| Authors | Intervention | Time of intervention | Number of sessions (frequency) | |
|---|---|---|---|---|
| Experimental group | Control group | |||
| Alessio-Mazzola et al. (2018) | Group 1: Extracorporeal shock waves. Group 2: Platelet Rich Plasma injection. | Not applicable. | 1 month | Group 1: 4 (weekly). Group 2: 1. |
| Altun et al. (2018) | Extracorporeal shock waves and CP. | CP (ultrasound and TENS). | 3 weeks | 3 (weekly). |
| Dones III et al. (2018) | Group 1: Biomechanical Taping (Standard Biomechanical Taping and two Vector Correction Dysfunction Techniques). Group 2: Biomechanical Taping (Vector Correction Dysfunction Technique, Standard Biomechanical Taping and other Vector Correction Dysfunction Technique). | Not applicable. | 5 days | 3 (alternating days). |
| Dundar et al. (2015) | Group 1: High Intensity Laser Therapy. Group 2: High Intensity Laser Therapy placebo. Group 3: ferule. | Not applicable. | Groups 1 and 2: 3 weeks. Group 3: 1 month. | Groups 1 and 2: 15 (5 each week). Group 3: 30 (daily). |
| Eraslan et al. (2017) | Group 1: extracorporeal shock waves and CP. Group 2: Kinesio | CP (cryotherapy, TENS, and eccentric exercises). | 3 weeks | Group 1: 1. Group 2 and control: 15 (5 each week). |
| Furnes et al. (2018) | Vibration and CP. | CP (educational tips). | 6 weeks | 45 (daily). |
| Giray et al. (2019) | Group 1: Kinesio | CP (educational tips, stretching and eccentric strengthening). | 2 weeks | 5 (one every five days). |
| Gönen et al. (2017) | Extracorporeal shock waves and CP. | CP (exercise routine). | 1 month | 4 (weekly). |
| Kachanat et al. (2019) | Orthotics and CP. | CP (ultrasound, friction massage and stretching). | 3 weeks | 3 (weekly). |
| Köksal et al. (2015) | Extracorporeal shock waves. | Not applicable. | 10 days | 3 (one every the first three days). |
| Kubot et al. (2017) | Group 1: Extracorporeal shock waves. Group 2: ultrasound. | Not applicable. | Group 1: 3 weeks. Group 2: 10 days. | Group 1: 3 (weekly). Group 2: 10 (daily). |
| López-Celis et al. (2018) | Group 1: diacutaneous fibrolysis and CP. Group 2: diacutaneous fibrolysis placebo and CP. | CP (ultrasound, TENS and stretching). | 3 weeks | Group 1: 15 (5 each week). Group 2: 6 (2 each week). |
| Nishizuka et al. (2016) | Orthotics and CP. | CP (stretching). | 6 months | 180 (daily). |
| Nowotny et al. (2018) | Orthotics and CP. | CP (eccentric strengthening). | 3 months | 90 (daily). |
|
Table 3, continued | ||||
| Authors | Intervention | Time of intervention | Number of sessions (frequency) | |
| Experimental group | Control group | |||
| Olaussen et al. (2015) | Group 1: corticosteroid injection, drug treatment with naproxen and CP. Group 2: injection placebo, drug treatment with naproxen and CP. | Drug treatment with naproxen and CP (friction massage, Mills manipulation and stretching). | 6 weeks | Groups 1 and 2: 2 (one session the first and the third weeks). Control group: 12 (two sessions each week). |
| Seo et al. (2018) | Eight variants of extensor carpi radialis brevis stretch. | Not applicable. | Not applicable. | Not applicable. |
| Stasino-poulos et al. (2016) | Group 1: eccentric-concentric and isometric strengthening. Group 2: eccentric-concentric strengthening. Group 3: eccentric strengthening. | Not applicable. | 1 month | 30 (daily). |
| Yalvaç et al. (2018) | Group 1: extracorporeal shock waves. Group 2: ultrasounds. | Not applicable. | Group 1: 3 weeks. Group 2: 2 weeks. | Group 1: 3 (weekly). Group 2: 10 (5 each week). |
| Yi et al. (2018) | Group 1: orthosis and deep friction massage. Group 2: orthosis. Group 3: orthosis and cortisone injections. | Not applicable. | Groups 1 and 3: 1 week. Group 2: 6 weeks. | Groups 1 and 3: 7 (daily). Group 2: 42 (daily). |
CP: conventional physiotherapy techniques.
session. The obtained results showed significant improvements in functionality and pain intensity in both groups (with no differences between them). However, the reincorporation of the participants to their usual activities was significantly faster with PRP. Lastly, Eraslan et al. [21] compared the effects of Kinesio
In addition to the above study, Nishizuka et al. [30] analysed the effects of Tennis Elbow Support (ALCARE), applied for over six hours per day in combination and comparison with the execution of stretching exercises for the wrist extensor muscles. After the treatment, pain intensity and the number of positive Thomsen tests decreased significantly in both cases (with no differences between them). They also evaluated the efficacy of a dynamic extension orthosis called CARP-X (Sporlastic) in combination and comparison with the execution of eccentric strength exercises [31]. In this case, the maximum grip strength, pain intensity and functionality improved in both groups progressively after the treatment and nine months after the end of the intervention, although strength did not improve significantly in any case. Lastly, Kachanathu et al. [22] evaluated the efficacy of the Futuro
Regarding the evaluation of bandages, Dones III et al. [29] analysed the effectiveness of different applications of Biomechanical Taping (BMT): one group received, firstly, the biomechanical bandage technique with muscular energy (Standard Biomechanical Taping, SBMT) and, subsequently, two vector correction dysfunction techniques (VCDT1 and VCDT2); the other group received the same techniques, with a different application sequence (first VCDT1, then SBMT and, lastly, VCDT2). The authors identified that pain intensity, maximum grip strength and functionality showed significant improvements in all patients. However, both immediately and one week after the intervention, the group that received SBMT as the first technique obtained better scores in pain intensity.
Finally, Giray et al. [25] evaluated the efficacy of KT [35, 36] in comparison with the application of a placebo bandage and a programme of conventional PT. All participants received the conventional PT intervention with instructions on activity modification and a home exercise programme of stretching and eccentric strengthening. The obtained results showed that functionality and pain intensity improved in all groups, although the KT group obtained significantly better results. On the other hand, grip strength also improved in the three groups, although with no statistical differences between them.
Two studies determined the efficacy of deep friction massage in comparison with a corticosteriod injection [26, 28]. In one of the cases, all participants received a wrist splint and a daily protocol of conventional PT, which included stretching and elbow and wrist mobility exercises [28]. The results showed that pain intensity, grip strength and functionality improved significantly and similarly both with the massage and with the injection, but not with the splint and the conventional PT protocol. However, at 6 months after the treatment, all groups showed improvements in all variables, although such improvements were only significant in the massage group. The other study applied corticosteroids invasively in combination and comparison with a PT intervention that included deep transverse friction massage at the origin of the tendon, Mill’s manipulation and wrist stretching exercises [26]. The results showed that, in the PT group, there was a progressive improvement in all variables, which was significant at 3, 6 and 12 months after the treatment. In the group the received corticosteroids, the improvement percentage was better at week 6 than in the subsequent evaluations. Between groups, the perception of improvement in the corticosteriod group showed better results in the first evaluation and worse results in the subsequent evaluations. Lastly, there were no statistical differences between groups one year after the evaluation.
On their part, the study of Seo et al. [27] was aimed at determining the most effective stretching position for the common extensor carpi radialis. They concluded that the shear modulus was always significantly higher when the wrist was flexed, especially with the elbow extended and the forearm in the prone position.
Regarding methods of assisted manual therapy with other instruments, studies have been conducted on diacutaneous fibrolysis (DF) [23] and vibration [24]. López-de-Celis et al. [23] evaluated the efficacy of DF in combination and comparison with US, TENS and stretching exercises with respect to a placebo group. Their results showed that, immediately after the treatment, the group that received DF presented significant improvements in all variables (pain intensity, maximum strength and functionality), whereas the conventional PT and placebo groups only presented significant changes in pain intensity, although with significantly lower changes compared to the DF group. However, at three months after the treatment, all variables improved in the three groups, with grip strength showing a significantly greater improvement in the DF group. Vibration assisted through a Tenease®device was evaluated in combination and comparison with a conventional treatment (information leaflet and education about LE, activities to be avoided and exercises to be performed) [24]. After the intervention, functionality improved in all participants, although such improvement was only significant with the conventional treatment. However, six months after the treatment, neither the quality of life nor pain intensity improved in any of the groups.
One study was aimed at comparing the efficacy of different modes of strength training for the wrist extensor muscles: eccentric, eccentric-concentric and eccentric-concentric combined with isometric training [32]. All participants showed significant improvements in pain intensity, functionality and maximum grip strength. In the intergroup comparison, the group that performed the eccentric-concentric training combined with isometric training obtained significantly better results with respect to the other two groups, both immediately after and one month after the intervention.
Lastly, Dundar et al. [33] explored the effects of high-intensity laser therapy (HILT) with pulse emissions (1064 nm), very high peak power (3 kW), high fluidity level (360–1780 mJ/cm
4.Discussion
The aim of this review was to determine the efficacy of PT for the treatment of LE and identify the most adequate techniques. After presenting the analysed studies, we can assert that, in general, PT techniques have a positive effect on the symptoms and resolution of the clinical characteristics of LE.
Pain intensity improved with all the applied treatments [15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 30, 31, 32, 33], although the interventions that included SW [15, 16, 17, 18, 19, 20], PRP [20], US, friction and stretching exercises [22] and bandages [29] achieved positive results in less time (between 3 and 9 sessions). This finding is in line with previous investigations about the SW treatment of other tendinopathies [37, 38]. For long-term pain relief, among the three studies that conducted more than one post-treatment evaluation [18, 26, 31], one of them applied SW and the other two carried out manual therapy [26], eccentric strengthening [26, 31] and corticosteroid infiltration [26]. The latter [26] carried out the latest evaluation, obtaining positive results one year after the intervention.
Regarding pain, other studies evaluated the pressure pain threshold (PPT) [15, 23, 33], which is a specially relevant variable in tendinopathies [39] and in the evaluation of chronic pain [40, 41]. This variable showed improvements with the interventions based on SW [15], orthosis [33], HILT [33], DF [23] and US, TENS and stretching exercises [23], since they can all affect hypercellularity, the collagen matrix, the proteoglycan content and neovascularisation, which is generated by the accumulation of microinjuries, due to the repetitive overload that exceeds the healing capacity of the tendon [42]. However, it is important to highlight that: (a) the combined application of US, TENS and stretching exercises obtained better results than DF [23]; and (b) the SW showed positive changes after only three sessions [15]. This could be due to the fact that the application of SW implies the administration of a series of short energy fluctuations that are rapidly transmitted, which is a method that has been revealed to be effective in the treatment of musculoskeletal disorders due to its angiogenic, analgesic and anti-inflammatory effects when applied on the painful area [43, 44].
Functionality improved in all the studies in which it was evaluated [15, 16, 19, 20, 21, 23, 24, 25, 28, 31, 32], although SW obtained better effects than US [16], probably due to the fact that the latter showed lower reliability in the application of the selected frequency and presented an unpredictable behavior of their acoustic diffraction [45]. On the other hand, SW are more reliable [39] and their efficacy increases when combined with strength exercises [46], as was also reported by Aydin et al. [17]. However, the use of orthoses did not show positive effects on functionality [28, 31], which could be explained by the fact that, by restricting movement, they may lead to muscle disuse; therefore, if orthoses are combined with strength exercises, they may show better results [32, 47]. The interventions based on conventional techniques (ortheses [28], stretching and mobility exercises [28] and education [24]) showed good results on functionality. Stretching exercises are commonly used in PT programmes, and it has been reported that the recovery time of a tendinopathy depends, to a great extent, on the frequency of their execution [48, 49]. Moreover, the article by Yi et al. [28] also obtained good results in the friction massage group, probably due to the capacity of this technique to soften the extracellular matrix and cause a slight inflammation that activates the restoration of the conjunctive tissue; in fact, it has been demonstrated to reduce pain and improve functionality in muscle and ligamentous pathologies [50]. DF was also capable of improving functionality after six sessions [23]. This could be explained by the fact that its mechanism of action consists in ripping the conjunctive tissue fibres that form adhesions, in order to recover the normal glide between the different tissue layers [51]; thus, it can improve the ROM and reduce myotendinous reflexes [52]. Lastly, with all the interventions, the improvement of this variable was achieved in the short term, especially with the application of SW [15, 16, 20, 21] and PRP [20] compared to US [15, 16]. The positive effects obtained with SW in several of the analysed variables can be due to the fact that their optimal effect is attained at a maximum depth of 3.5 cm, where epicondylar tendons can be fully treated regardless of the size of the patient [53]. Similarly, with a high concentration of growth factors, PRP favours the resolution of tendinopathies and muscle and cartilage injuries [54].
Another aspect closely related to functionality and objectively quantifiable is grip strength, which was also analysed [15, 17, 19, 22, 23, 25, 26, 28, 29, 30, 31, 32]. Regarding the improvement of this variable, the interventions based on therapeutic exercise [17, 31] and manual therapy [26] obtained good results in the long-term, and even significantly higher results compared to those based on ortheses [31], SW [15, 17, 19] and corticosteroids [26]. This could be due to the fact that corticosteroids regulate the immune function of inflammatory cells and chemical mediators, thus decreasing pain; however, injections increase protein catabolism and reduce type I collagen and the synthesis of glycosaminoglycans, thereby delaying the healing process in the long term [55]. DF improved grip strength after one session [18], thanks to its capacity to improve the mechanical and inflammatory pain of the musculoskeletal system by removing the tissue adhesions and allowing the optimal glide of the myofibrils [52]. In the short term, SW also obtained good results in this variable [15, 20, 30], although they proved to be less effective when compared to KT [21]. KT reduces pain and edema and facilitates motor activity by activating the circulatory and nervous systems with movement, improves the ROM by relieving abnormal muscle tension and stimulates the mechanoreceptors by applying pressure on the skin, which are effects that have a direct impact on the generation of strength [56]. On the other hand, the improvements obtained with KT reach a limit in time after the intervention [22, 25, 29], unless this technique is combined with conventional PT methods, such as ergonomic measures, stretching exercises and strength training [25].
The ROM was only evaluated in the studies that used orthoses [22, 31]; this variable was improved in both cases. However, also in both cases, the orthosis was applied in combination with strength exercises [31] or with US, friction and stretching exercises [22], which are techniques known for their improvement effect on joint mobility [11, 48, 50, 57]. In fact, the improvement was greater with the intervention that only included eccentric exercises [31], since this training modality is currently among the most effective techniques in the treatment of tendinopathies [58, 59, 60]. This type of training leads to the production of collagen, reduces the prevalence of inflammation and neovascularisation and decreases pain by increasing tendinous resistance and desensitising the central nervous pathways of pain transmission [11, 61].
Therefore, the treatment of LE should include eccentric strengthening, due to its benefits on pain reduction and the increase of tendinous resistance [11, 58], with techniques such as friction massage and DF (depending on the patient’s preferences), which are non-invasive and follow the same neurophysiological principles to reduce pain and inflammation, with the difference that DF can reach deeper layers [23, 50, 52], or KT, which stimulates circulation by displacing the skin, fascia and subcutaneous tissues, achieving the correction of the fascia, reducing pain and attaining neuromuscular reeducation with the stimulation of mechanoreceptors [56, 55]. If the patient presents a lot of pain, orthoses are a non-invasive method with short-term efficacy for the immediate relief of pain and the improvement of hand functionality [3], although, in these cases, complying with the guideline of exercises becomes more important for the prevention of their harmful effects. Lastly, it must be considered that, for the treatment of acute LE (processes of less than three months of evolution) [16, 17, 19, 25, 26, 28, 30, 33, 58], US and PRP are less effective. On the other hand, for the treatment of chronic LE [15, 18, 20, 21, 22, 23], no particularities were found in terms of suitability for any techniques.
With respect to the methodological limitations of this study, it must be pointed out that the inclusion of non-controlled and non-randomised experimental studies reduces the validity of the conclusions drawn in this review. Moreover, the small sample size of some of the analysed articles limits the generalisation of their results. Regarding the operationalisation of the study variables, many of them were evaluated through methods that depend on the patient’s subjectivity. Finally, in the results selection process, a considerable number of studies were eliminated because their full text was not available. On the other hand, this review has some strengths that must be highlighted, such as the comparison of different treatment techniques (including conventional low-cost techniques and other more recent methods that require greater economic investment and/or multidisciplinary intervention) and the fact that it is an update on the different PT techniques for the treatment of LE.
Future studies should conduct further RCT with larger sample sizes and compare the different combinations of the most effective techniques: manual therapy, strength training, SW and bandages. Furthermore, future research must compare and adequately define the particularities of the different approaches in acute and chronic LE.
5.Conclusions
Taken together, findings from papers included in the present systematic review suggested that manual therapy (e.g., stretching exercises and friction massages) and eccentric strength training are the two physiotherapy treatments with the most beneficial effects on LE, and their cost-benefit ratio is very favourable. Other techniques have positive effects, although they require greater economic investment, such as SW and the administration of PRP.
In any case, before deciding to perform surgical intervention, it is crucial to deplete all the conservative therapeutic options (drugs and PT), regardless of their economic cost. In addition, there are many PT tools that can complement the mentioned techniques, such as cryotherapy, electrotherapy, ultrasound therapy, and the application of tapes or orthoses.
Data availability
The data that support the findings of this study are available upon reasonable request from the corresponding author.
Funding
No financial support was received from any commercial company.
Conflict of interest
The authors report no conflict of interest.
References
[1] | Tarpada SP, Morris MT, Lian J, Rashidi S. Current advances in the treatment of medial and lateral epicondylitis. J Orthop. (2018) ; 15: (1): 107-110. |
[2] | Lenoir H, Mares O, Carlier Y. Management of lateral epicondylitis. Orthop Traumatol Surg Res. (2019) ; 105: (8): S241-S246. |
[3] | Barati H, Zarezadeh A, MacDermid JC, Sadeghi-Demneh E. The immediate sensorimotor effects of elbow orthoses in patients with lateral elbow tendinopathy: A prospective crossover study. J Shoulder Elbow Surg. (2019) ; 28: (1): e10-e17. |
[4] | Sandhu KS, Kahal KS, Singh J, Singh J, Grewal H. A comparative study of activated platelet rich plasma versus local corticosteroid injection for the treatment of lateral epicondylitis: A randomised study. Int J Orthop. (2020) ; 6: (1): 1274-1276. |
[5] | Bisset LM, Vicenzino B. Physiotherapy management of lateral epicondylalgia. J Physiother. (2015) ; 61: (4): 174-181. |
[6] | Zhong Y, Zheng C, Zheng J, Xu S. Kinesio tape reduces pain in patients with lateral epicondylitis: A meta-analysis of randomized controlled trials. Int J Surg. (2020) ; 76: : 190-199. |
[7] | Boden AL, Scott MT, Dalwadi PP, Mautner K, Amadeus R, Gottschalk MB. Platelet-rich plasma versus tenex in the treatment of medial and lateral epicondylitis. J Shoulder Elbow Surg. (2019) ; 28: (1): 112-119. |
[8] | Holmedal O, Olaussen M, Mdala I, Natvig B, Lindbaek M. Predictors for outcome in acute lateral epicondylitis. BMC Musculosket Disord. (2019) ; 20: : 375. |
[9] | Coombes BK, Bisset L, Vicenzino B. Management of lateral elbow tendinopathy: One size does not fit all. J Orthop Sports Phys Ther. (2015) ; 45: (11): 938-949. |
[10] | Ortega-Castillo M, Medina-Porqueres I. Effectiveness of the eccentric exercise therapy in physically active adults with symptomatic shoulder impingement or lateral epicondylar tendinopathy: A systematic review. J Sci Med Sport. (2016) ; 19: (6): 438-453. |
[11] | Peterson M, Butler S, Eriksson M, Svärdsudd K. A randomized controlled trial of accentric vs. concentric graded exercise in chronic tennis elbow (lateral elbow tendinopathy). Clin Rehabil. (2014) ; 28: (9): 862-872. |
[12] | Finestone HM, Rabinovitch DL. Tennis elbow no more: Practical eccentric and concentric exercises to heal the pain. Can Fam Physician. (2008) ; 54: (8): 1115-1116. |
[13] | Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J Clin Epidemiol. (2009) ; 62: (10): e1-e34. |
[14] | Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. Cochrane handbook for systematic reviews of interventions. New Jersey (NY): John Wiley & Sons; (2019) . |
[15] | Yalvaç B, Mesci N, Külcü DG, Yurdakul OV. Comparison of ultrasound and extracorporeal shock wave therapy in lateral epicondylosis. Acta Orthop Traumatol Turc. (2018) ; 52: (5): 357-362. |
[16] | Kubot A, Grzegorzewski A, Synder M, Szymcack W, Kozlowski P. Radial extracorporeal shockwave therapy and ultrasound therapy in the treatment of tennis elbow syndrome. Ortop Traumatol Rehabil. (2017) ; 19: (5): 415-426. |
[17] | Gönen C, Aykut S, Öztürk K, Arslanoglu F, Yalin C, Kocaer N. Long-term efficiency of extracorporeal shockwave therapy on lateral epicondylitis. Acta Orthop Belg. (2017) ; 83: : 438-444. |
[18] | Köksal İ, Güler O, Mahiroğulları M, Mutlu S, Çakmak S, Aksahin E. Comparison of extracorporeal shock wave therapy in acute and chronic lateral epicondylitis. Acta Orthop Traumatol Turc. (2015) ; 49: (5): 465-470. |
[19] | Altun RD, Incel NA, Cimen OB, Sahub G. Efficacy of ESWT for lateral epicondylitis treatment: Comparison with physical therapy modalities. J Musculosketeletal Res. (2018) ; 21: (1): 1850001. |
[20] | Alessio-Mazzola M, Repetto I, Biti B, Trentini R, Formica M, Felli L. Autologous US-guided PRP injection versus US-guided focal extracorporeal shock wave therapy for chronic lateral epicondylitis: A minimum of 2-year follow-up retrospective comparative study. J Orthop Surg. (2018) ; 26: (1): 2309499017749986. |
[21] | Eraslan L, Yuce D, Erbilici A, Baltaci G. Does kinesiotaping improve pain and functionality in patients with newly diagnosed lateral epicondylitis? Knee Surg Sports Traumatol Arthrosc. (2018) ; 26: (3): 938-945. |
[22] | Kachanathu SJ, Alenazi AM, Hafez AR, Algarni AD, Alsubiheen AM. Comparison of the effects of short-duration wrist joint splinting combined with physical therapy and physical therapy alone on the management of patients with lateral epicondylitis. Eur J Phys Rehabil Med. (2019) ; 55: (4): 488-493. |
[23] | López-de-Celis C, Barra-López M, González-Rueda V, Bueno-Gracia E, Rodríguez-Rubio PR, Tricás-Moreno JM. Effectiveness of diacutaneous fibrolysis for the treatment of chronic lateral epicondylalgia: A randomized clinical trial. Clin Rehabil. (2018) ; 32: (5): 644-653. |
[24] | Furness ND, Phillips A, Gallacher S, Sherard JC, Evans JP, Toms AD. Vibration therapy versus standard treatment for tennis elbow: A randomized controlled study. J Orthop Surg. (2018) ; 26: (3): 2309499018792744. |
[25] | Giray E, Karali-Bingul D, Akyuz G. The effectiveness of kinesiotaping, sham taping or exercises only in lateral epicondylitis treatment: A randomized controlled study. PM & R. (2019) ; 11: (7): 681-693. |
[26] | Olaussen M, Holmedal Ø, Mdala I, Brage S, Lindbaek M. Corticosteroid or placebo injection combined with deep transverse friction massage, mills manipulation, stretching and eccentric exercise for acute lateral epicondylitis: A randomised, controlled trial. Musculosket Disord. (2015) ; 16: (1): 122. |
[27] | Seo J, Yoon S, Lee J, Kim JK, Yoo JS. What is the most effective eccentric stretching position in lateral elbow tendinopathy? Clin Orthop Surg. (2018) ; 10: (1): 47-54. |
[28] | Yi R, Bratchenko WW, Tan V. Deep friction massage versus steroid injection in the treatment of lateral epicondylitis. Hand. (2018) ; 13: (1): 56-59. |
[29] | Dones VC, III., Serra MAB, Kamus III, Esteban AC, Mercado AMS, Rivera RGA, et al. The effectiveness of biomechanical taping technique on visual analogue scale, static maximum handgrip strength, and patient rated tennis elbow evaluation of patients with lateral epicondylalgia: A cross-over study. J Bodywork Movement Ther. (2019) ; 23: (2): 405-416. |
[30] | Nishizuka T, Iwatsuki K, Kurimoto S, Yamamoto M, Hirata H. Efficacy of a forearm band in addition to exercises compared with exercises alone for lateral epicondylitis: A multicenter, randomized, controlled trial. J Orthop Sci. (2017) ; 22: (2): 289-294. |
[31] | Nowotny J, El-Zayat B, Goronzy J, Biewener A, Bausenhart F, Greiner S, et al. Prospective randomized controlled trial in the treatment of lateral epicondylitis with a new dynamic wrist orthosis. Eur J Med Res. (2018) ; 23: (1): 43. |
[32] | Stasinopoulos D, Stasinopoulos I. Comparison of effects of eccentric training, eccentric-concentric training, and eccentric-concentric training combined with isometric contraction in the treatment of lateral elbow tendinopathy. J Hand Ther. (2017) ; 30: (1): 13-19. |
[33] | Dundar U, Turkmen U, Toktas H, Ulasli AM, Solak O. Effectiveness of high-intensity laser therapy and splinting in lateral epicondylitis; a prospective, randomized, controlled study. Lasers Med Sci. (2015) ; 30: (3): 1097-1107. |
[34] | Kase K. Clinical therapeutic applications of the kinesio® taping method. Albuquerque (NM): Kinesio. (2003) . |
[35] | MacDermid JC. The patient-rated tennis elbow evaluation (PRTEE) user manual. Hamilton, (Canada): School of Rehabilitation Science, McMaster University. (2007) . |
[36] | Shakeri H, Soleimanifar M, Arab AM, Behbahani SH. The effects of KinesioTape on the treatment of lateral epicondylitis. J Hand Ther. (2018) ; 31: (1): 35-41. |
[37] | Melikyan EY, Shalin E, Miles J, Bainbridge LC. Extracorporeal shock-wave treatment for tennis elbow. Bone Joint J. (2023) ; 85-B: (6): 852-855. |
[38] | Stasinopoulos D, Johnson MI. Effectiveness of extracorporeal shock wave therapy for tennis elbow. Br J Sports Med. (2005) ; 39: : 132-136. |
[39] | Zhang L, Cui Y, Liang D, Guan J, Liu Y, Chen X. High-energy focused extracorporeal shock wave therapy for bone marrow edema syndrome of the hip: A retrospective study. Medicine. (2020) ; 99: (16): e19747. |
[40] | Coombes BK, Bisset L, Vicenzino B. Cold hyperalgesia associated with poorer prognosis in lateral epicondylalgia: A 1-year prognostic study of physical and psychological factors. Clin J Pain. (2015) ; 31: (1): 30-35. |
[41] | Tondelli T, Götschi T, Camenzind RS, Snedeker JG. Assessing the effects of intratendinous genipin injections: Mechanical augmentation and spatial distribution in an ex vivo degenerative tendon model. Plos One. (2020) ; 15: (4): e0231619. |
[42] | Zhang X, Zhang Y, Cai W, Liu Y, Liu H, Zhang Z, et al. MicroRNA-128-3p alleviates neuropathic pain through targeting ZEB1. Neurosci Lett. (2020) ; 134946. |
[43] | Ji Q, Wang P, He C. Extracorporeal shockwave therapy as a novel and potential treatment for degenerative cartilage and bone disease: Osteoarthritis. A qualitative analysis of the literature. Prog Biophys Mol Biol. (2016) ; 121: (3): 255-265. |
[44] | Iglesias E, de Frutos J, de Espinosa FM. Modeling piezoelectric ultrasonic transducers for physiotherapy. Bol Soc Españ Cerám Vidrio. (2015) ; 54: (6): 231-235. |
[45] | Solanki CP, Chhatlani RM. A study to find out the effect of extracorporeal shock wave therapy for chronic musculoskeletal Conditions – A systematic review. Indian J Physiother Occup Ther. (2019) ; 13: (4): 428. |
[46] | Houck J, Neville C, Tome J, Flemister A. Randomized controlled trial comparing orthosis augmented by either stretching or stretching and strengthening for stage II tibialis posterior tendon dysfunction. Foot Ankle Int. (2015) ; 36: (9): 1006-1016. |
[47] | Umehara J, Nakamura M, Fujita K, Kusano K, Nishishita S, Araki K, et al. Shoulder horizontal abduction stretching effectively increases shear elastic modulus of pectoralis minor muscle. J Shoulder Elbow Surg. (2017) ; 26: (7): 1159-1165. |
[48] | Umegaki H, Ikezoe T, Nakamura M, Nishishita S, Kobayashi T, Fujita K, et al. The effect of hip rotation on shear elastic modulus of the medial and lateral hamstrings during stretching. Man Ther. (2015) ; 20: (1): 134-137. |
[49] | Stasinopoulos D, Johnson MI. Cyriax physiotherapy for tennis elbow/lateral epicondylitis. Br J Sports Med. (2004) ; 38: : 675-677. |
[50] | Leite WB, Oliveira, ML, Ferreira, IC, Anjos CF, Barbosa MA, Barbosa AC. Effects of 4-week diacutaneous fibrolysis on myalgia, mouth opening, and level of functional severity in women with temporomandibular disorders: A randomized controlled trial. J Manipulative Physiol Ther. (2020) ; 43: (8): 806-815. |
[51] | Fanlo-Mazas P, Bueno-Gracia E, de Escudero-Zapico AR, Tricás-Moreno JM, Lucha-López MO. The effect of diacutaneous fibrolysis on patellar position measured using ultrasound scanning in patients with patellofemoral pain syndrome. J Sport Rehab. (2019) ; 28: (6): 564-569. |
[52] | Radinmehr H, Nakhostin-Ansari N, Naghdi S, Olyaei G, Tabatabaei A. Effects of one session radial extracorporeal shockwave therapy on post-stroke plantarflexor spasticity: A single-blind clinical trial. Disabil Rehabil. (2017) ; 39: (5): 483-490. |
[53] | Formica M, Cavagnaro L, Formica C, Mastrogiacomo M, Basso M, Di Martino A. What is the preclinical evidence on platelet rich plasma and intervertebral disc degeneration? Eur Spine J. (2015) ; 24: (11): 2377-2386. |
[54] | Barnett J, Bernacki MN, Kainer JL, Smith HN, Zaharoff AM, Subramanian SK. The effects of regenerative injection therapy compared to corticosteroids for the treatment of lateral epicondylitis: A systematic review and meta-analysis. Arch Physiother. (2019) ; 9: (1): 12. |
[55] | Karabay I, Doğan A, Ekiz T, Füsun B, Ersöz M. Training postural control and sitting in children with cerebral palsy: Kinesio taping vs. neuromuscular electrical stimulation. Complement Ther Clin Pract. (2016) ; 24: : 67-72. |
[56] | Pieters L, Lewis J, Kuppens K, Jochems J, Brujistens T, Joosens L, et al. An update of systematic reviews examining the effectiveness of conservative physical therapy interventions for subacromial shoulder pain. J Orthop Sports Phys Ther. (2020) ; 50: (3): 131-141. |
[57] | Stasinopoulos D. The effectiveness of isometric contractions combined with eccentric contractions and stretching exercises on pain and disability in lateral elbow tendinopathy. A case report. J Nov Physiother. (2015) ; 5: (238): 2. |
[58] | Lepley LK, Lepley AS, Onate JA, Grooms DR. Eccentric exercise to enhance neuromuscular control. Sports Health. (2017) ; 9: (4): 333-340. |
[59] | Goodall S, Thomas K, Barwood M, Keane K, González JL, St Clair A, et al. Neuromuscular changes and the rapid adaptation following a bout of damaging eccentric exercise. Acta Physiol. (2017) ; 220: (4): 486-500. |
[60] | Martinez-Silvestrini JA, Newcomer KL, Gay RE, Schaefer MP, Kortebein P, Arendt KW. Chronic lateral epicondylitis: Comparative effectiveness of a home exercise program including stretching alone versus stretching supplemented with eccentric or concentric strengthening. J Hand Ther. (2005) ; 18: (4): 411-420. |
[61] | Toprak-Celenay S, Korkut Z, Oskay K, Aydin A. The effects of pelvic floor muscle training combined with kinesio taping on bladder symptoms, pelvic floor muscle strength, and quality of life in women with overactive bladder syndrome: A randomized sham-controlled trial. Physiother Theory Pract. (2020) ; 1-10. |




