Minimally invasive versus open transforaminal lumbar interbody fusion for single segmental lumbar disc herniation: A meta-analysis
Abstract
BACKGROUND:
Numerous studies on the comparison of minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) and open-transforaminal lumbar interbody fusion (O-TLIF) for the treatment of lumbar disc herniation (LDH) have been published, but there is no clear conclusion.
OBJECTIVE:
The aim of this study was to evaluate the efficacy of MIS-TLIF compared with O-TLIF in the treatment of LDH in the Chinese population by meta-analysis.
METHODS:
Studies on the treatment of LDH by MIS-TLIF versus O-TLIF were searched in Pubmed, Web of Science, Medline, Embase, CNKI, VIP and China Wanfang databases from the establishment of the databases to January 2020. The meta-analysis was used to analyze the pooled operation time, intraoperative blood loss, postoperative drainage, postoperative ground movement time, Waist and leg Visual Analogue Scale (VAS) score, Oswestry Disability Index (ODI) score and Japanese orthopaedic association (JOA) score. Mean difference (MD) and standard mean difference (SMD) were used as the effect size.
RESULTS:
Eleven studies with 1132 patients were included. The results showed that MIS-TLIF compared with O-TLIF, MD
CONCLUSION:
MIS-TLIF was superior to O-TLIF in the treatment of LDH, especially in the intraoperative blood loss, postoperative drainage, postoperative ground movement time and low back pain in the Chinese population.
1.Introduction
Lumbar disc herniation (LDH) is a clinical syndrome that stimulates and oppresses cauda equina and nerve root due to degeneration of lumbar intervertebral disc, rupture of peripheral annulus fibrosus and herniation of nucleus pulposus in the middle. The main clinical manifestation is low back pain [1]. The pathogenesis of LDH is as follows: the lumbar intervertebral disc is located between the upper and lower adjacent vertebrae of the human spine, which is composed of the nucleus pulposus of the middle part, the fibrous ring of the peripheral part and the cartilage endplate of the upper and lower parts. It has the characteristics of hydrodynamics and mechanical functions such as bearing the weight of the torso and upper limbs, dispersing stress and so on. In the case of excessive weight-bearing, violent impact and sudden change of posture, it is easy to break the annulus fibrosus and protrude the nucleus pulposus. At the same time, it is easy to degenerate because of the special physiological structure and biochemical components of lumbar intervertebral disc. Most of the LDH are L4-L5 segment and L5-S1 segment herniation [2, 3]. In recent years, the incidence of LDH is increasing. With a large number of cases and wide age distribution, it has developed into a social disease, seriously affecting people’s normal life and work [4]. It used to be a common disease that plagued the middle-aged and elderly, but it is now getting younger and younger [5]. LDH is characterized by low back pain and lower limb radiation pain. With the progress of the disease, some waist and leg pain symptoms are serious. After several months of conservative treatment was ineffective, the disease was gradually aggravated, and seriously affected one’s normal life and work. Patients with obvious manifestations of nerve involvement should receive surgical treatment in time [6].
In 1934, Mixter and Barr [7] first reported that sciatica caused by LDH and nerve root compression can be cured by operation, which ushered in the era of surgical treatment of LDH. Long-term clinical treatment research found that the accurate and satisfactory effect of LDH with the surgical treatment has been recognized by the majority of orthopedic doctors and patients. Nowadays, more and more patients with prolapse of lumbar intervertebral disc choose to receive surgical treatment. After the conservative treatment of LDH was ineffective, discectomy and interbody fusion through surgery was an effective method [8]. Harms and Rolinger first proposed transforaminal lumbar interbody fusion in 1982 [9]. The operation was located on the outside of the articular process, through the intervertebral foramen approach, less irritation to the nerve root during the operation, not entered the spinal canal, while well restored the physiological curvature of the lumbar spine. At present, TLIF surgery technique is widely used in clinic [10]. A large number of clinical studies have shown that the traditional posterior lumbar surgery requires large-scale muscle stripping, large amount of blood loss during the operation, large surgical trauma, serious postoperative lumbar pain, early shadow sound, and long hospital stay. Muscle scar increased, and multifida muscle atrophy became serious [11].
In order to reduce the muscle injury of thoracolumbar posterior approach, Wiltse proposed a surgical approach through paraspinal muscle space, which was relatively simple, easy to reach the articular surface and transverse process, and applied to cases of thoracolumbar fracture without spinal canal decompression, and the clinical effect was satisfactory [12]. At present, open-transforaminal lumbar interbody fusion (O-TLIF) has become one of the main surgical methods for the treatment of LDH. However, there are still several disadvantages, such as large amount of blood loss, large wound, slow healing, etc. Foley first put forward the MIS-TLIF technique in 2003 [13]. MIS-TLIF via intervertebral foramen approach has been widely used and improved in clinic. The purpose of this technique is to effectively solve the problems of low back and leg pain under the conditions of small skin incision and little soft tissue trauma. The basic principles of MIS-TLIF and O-TLIF in the treatment of single-segment LDH are the same: surgical removal of diseased intervertebral disc tissue, full decompression of nerve roots, interbody fusion with interbody fusion, internal fixation with nail-rod system, etc. These two surgical methods are commonly used in the treatment of single-segment LDH Compared to the traditional O-TLIF technology, some studies have shown that the MIS-TLIF had advantages in reducing trauma to the back muscles, postoperative blood loss, postoperative low back pain, bone damage, and shortening operation time. However, other studies have reported that the MIS-TLIF had long operation time and the same long-term clinical effect in MIS-TLIF when compared O-TLIF. Considering the inconsistencies in these results, this study made a comprehensive analysis of the previous literature on the comparative analysis of single-segment LDH compared MIS-TLIF with O-TLIF surgical methods, in order to provide evidence-based medicine for the clinical treatment of LDH.
2.Methods
2.1Document retrieval
Pubmed, Web of Science, Medline, Embase, CNKI, VIP and China Wanfang databases were searched, from the establishment of the database to January 2020, for randomized controlled trials or non-randomized controlled trials on the efficacy of MIS-TLIF and O-TLIF in the treatment of LDH. The keywords were “Lumbar disc herniation”, “Transforaminal Lumbar Interbody Fusion”, “TLIF”, “MIS-TLIF”, “Open-TLIF” and “Random control trial”. The comprehensive database retrieval was carried out independently by two researchers. The languages included are limited to English and Chinese.
2.2Inclusion and exclusion criteria
2.2.1Inclusion criteria
1) Randomized controlled trials (RCT) or non-RCT of MIS-TLIF and standard O-TLIF in the treatment of LDH were satisfied; 2) the baselines of the two groups were the same, such as age, sex and other demographic factors, the degree and duration of low back pain, the proportion of patients with neurological symptoms, the measured value of initial results, etc., regardless of language; 3) participants were the patients with single segmental LDH or lumbar instability diagnosed by physical examination and imaging (myelography or Computed Tomography or Magnetic Resonance Imaging) without history of lumbar disc surgery.
2.2.2Exclusion criteria
1) Multi-segmental LDH, degenerative spinal canal stenosis, secondary disc herniation, cauda equina syndrome, fracture, infection, intraspinal tumor, bone tumor, lumbar spondylolisthesis, osteoporosis or rheumatoid arthritis were excluded; 2) Other methods of lumbar fusion were excluded, such as (posterolateral fusion (PLF), (posterior lumbar interbody fusion (PLIF), anterior lumbar interbody fusion (ALIF), oblique lumber interbody fusion (OLIF), etc.
2.3Document quality evaluation
The methodological quality evaluation included in the study was carried out according to the five quality evaluation criteria of randomized controlled trials: 1) based on whether the random method was correct or not, the randomly assigned quality was divided into three grades, including the random method was correct, the random method was not described, and the random method was incorrect. 2) The quality of allocation hiding can be divided into four levels, including correct hiding method, undescribed hiding method, incorrect hiding method and no allocation hiding. 3) Whether the blind method was adopted for surgery or not, mainly depended on whether the evaluator blind method was adopted. 4) Whether there was loss of follow-up or withdrawal, the study of loss of follow-up or withdrawal should be analyzed by intention to treat. 5) The baseline situation was included to study whether the baseline conditions such as population and age were comparable in order to judge the influence of selective bias and opportunity. If the above five quality evaluation criteria were fully satisfied and the methodology was correct, the possibility of bias in the study was the least (grade A). If any one or more of the quality evaluation criteria were only partially satisfied (if the method was not clear), then the study had a moderate possibility of corresponding bias (grade B). If any one or more of the quality evaluation criteria were not met at all (the method was incorrect or not used), the study was highly likely to be biased (grade C). If no relevant information was provided in the study, we would try to contact the original author.
2.4Data extraction
The title and abstract of each article were read independently by two researchers, and the appropriate studies were selected according to the above inclusion criteria and exclusion criteria. Any study that may be included in the meta-analysis should be read the full text and be translated if necessary. If the two researchers disagree on the literature evaluation, it can be settled through discussion and negotiation. Observation indicators were as follows: average operation time, intraoperative blood loss, postoperative drainage, postoperative landing time, VAS score of waist and leg before and after operation, ODI score and JOA score. The postoperative waist and leg VAS score, ODI score and JOA score were limited to 6 months after operation, and those less than 6 months were subject to the last follow-up.
Table 1
The basic characteristics of inclusion in the literature
| Study | Year | Country | Ages (MIS-TLIF/ open-TLIF) (years) | Cases (MIS-TLIF/ open-TLIF) | Main index |
|---|---|---|---|---|---|
| Ding RH [14] | 2013 | China | 51.4 | 20/20 | Average operation time, Intraoperative bleeding volume, Postoperative drainage, VAS, JOA |
| Miao J [15] | 2014 | China | 48.7 | 53/62 | Intraoperative bleeding volume, Postoperative drainage, Postoperative landing time |
| Wen TL [16] | 2014 | China | 50.02 | 20/27 | Average operation time, Intraoperative bleeding volume, VAS, ODI |
| Guo ZP [17] | 2016 | China | 36.7 | 80/80 | Average operation time, Intraoperative bleeding volume, Postoperative drainage, Postoperative landing time, VAS, ODI |
| Zhang W [18] | 2016 | China | 15 | 102/84 | Average operation time, Intraoperative bleeding volume, ODI |
| Liu YB [20] | 2017 | China | 45.0 | 100/86 | Average operation time, Intraoperative bleeding volume, Postoperative drainage, VAS, ODI |
| Wang G [21] | 2017 | China | 53.82 | 27/27 | Average operation time Intraoperative bleeding volume Postoperative drainage, Postoperative landing time |
| Lv Y [19] | 2017 | China | NR | 50/56 | Average operation time, Intraoperative bleeding volume, VAS, ODI |
| Liu JB [23] | 2018 | China | 54.45 | 50/50 | Average operation time, Intraoperative bleeding volume, Postoperative drainage, Postoperative landing time, VAS, JOA, ODI |
| Zhao JQ [22] | 2018 | China | 46.12 | 17/20 | Average operation time, Intraoperative bleeding volume, Postoperative drainage, VAS, ODI |
| Zhao HE [24] | 2019 | China | 57.3 | 52/49 | Average operation time, Intraoperative bleeding volume, JOA |
VAS: Visual Analogue Scale; ODI: Oswestry Disability Index; JOA: Japanese orthopaedic association; NR: Not reported.
2.5Statistical analysis
The data were analyzed by Stata 15.0 statistical software. The heterogeneity among studies was evaluated by inconsistency index (I
3.Results
3.1Literature retrieval and quality evaluation
After a preliminary search, a total of 380 relevant literature were retrieved. A totlal of 333 articles were excluded by reading titles and abstracts, and 36 articles were excluded after careful reading of the full text. Finally, eleven studies [14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24] were included (Table 1). There were 1132 patients with LDH, including 571 patients in the MIS-TLIF group and 561 patients in the O-TLIF group. The specific screening flow diagram was shown in Fig. 1. According to the evaluation criteria of literature quality, 3 articles in this study were grade A, 5 articles were grade B, and 3 articles were grade C (Table 2).
Figure 1.
Flow diagram of the study.
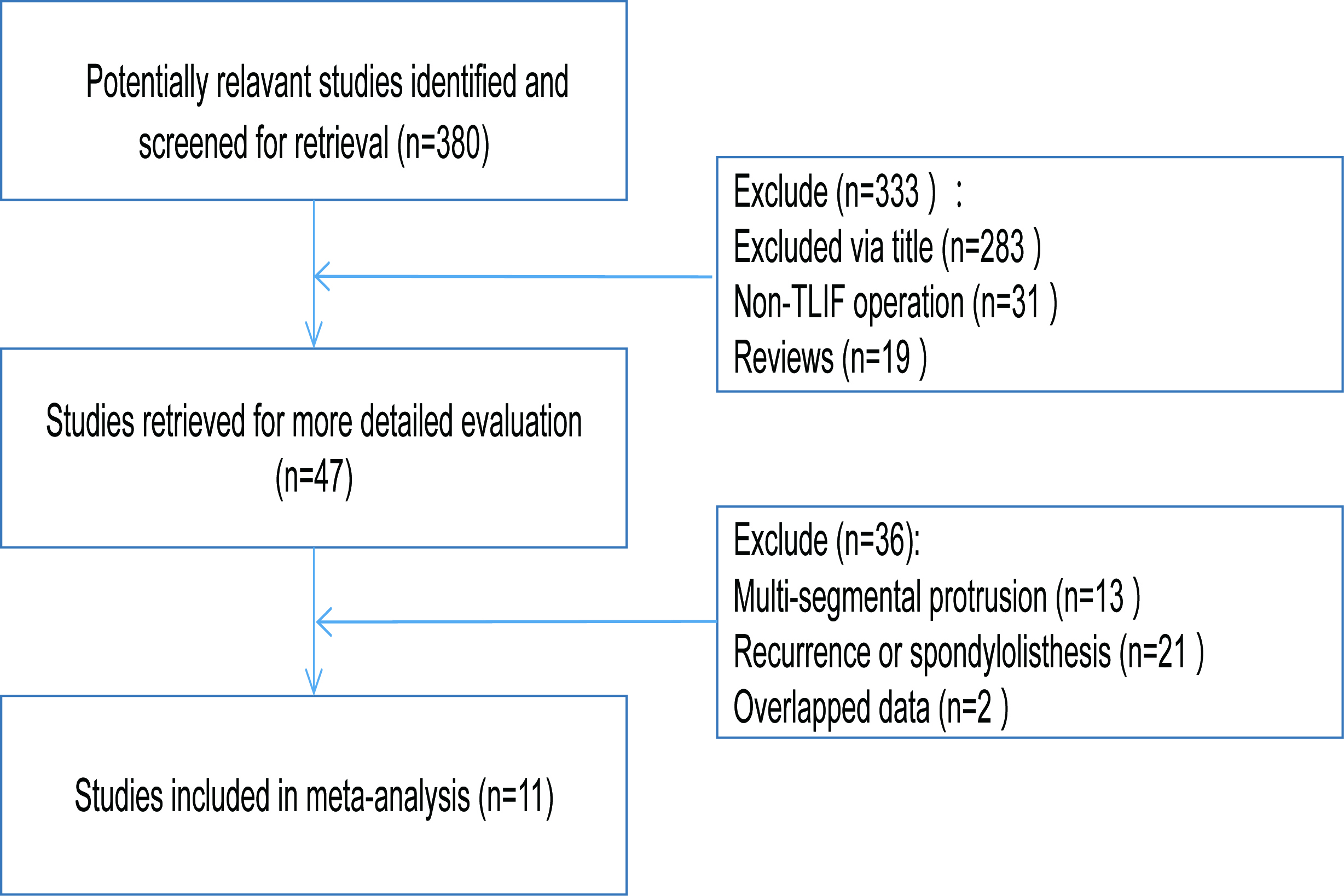
Table 2
Quality evaluation of the included literature
| First author | Random | Allocation hiding | Evaluator blind method | Loss of follow-up | Baseline situation | Methodological quality level |
|---|---|---|---|---|---|---|
| Ding RH [14] | Sufficient | Insufficient | Unclear | No | Comparable | B |
| Miao J [15] | Insufficient | Insufficient | Unclear | No | Comparable | C |
| Wen TL [16] | Insufficient | Insufficient | Unclear | No | Comparable | C |
| Guo ZP [17] | Sufficient | Insufficient | Unclear | No | Comparable | B |
| Zhang W [18] | Insufficient | Insufficient | Unclear | No | Comparable | C |
| Liu YB [20] | Sufficient | Insufficient | Unclear | Yes | Comparable | B |
| Wang G [21] | Sufficient | Insufficient | Unclear | No | Comparable | B |
| Lv Y [19] | Sufficient | Sufficient | Sufficient | No | Comparable | A |
| Liu JB [23] | Sufficient | Insufficient | Unclear | No | Comparable | B |
| Zhao JQ [22] | Sufficient | Sufficient | Sufficient | No | Comparable | A |
| Zhao HE [24] | Sufficient | Sufficient | Sufficient | No | Comparable | A |
Figure 2.
Forest plots with effect index of MD (A: average operation time; B: intraoperative blood loss; C: postoperative drainage; D: postoperative ground movement time).
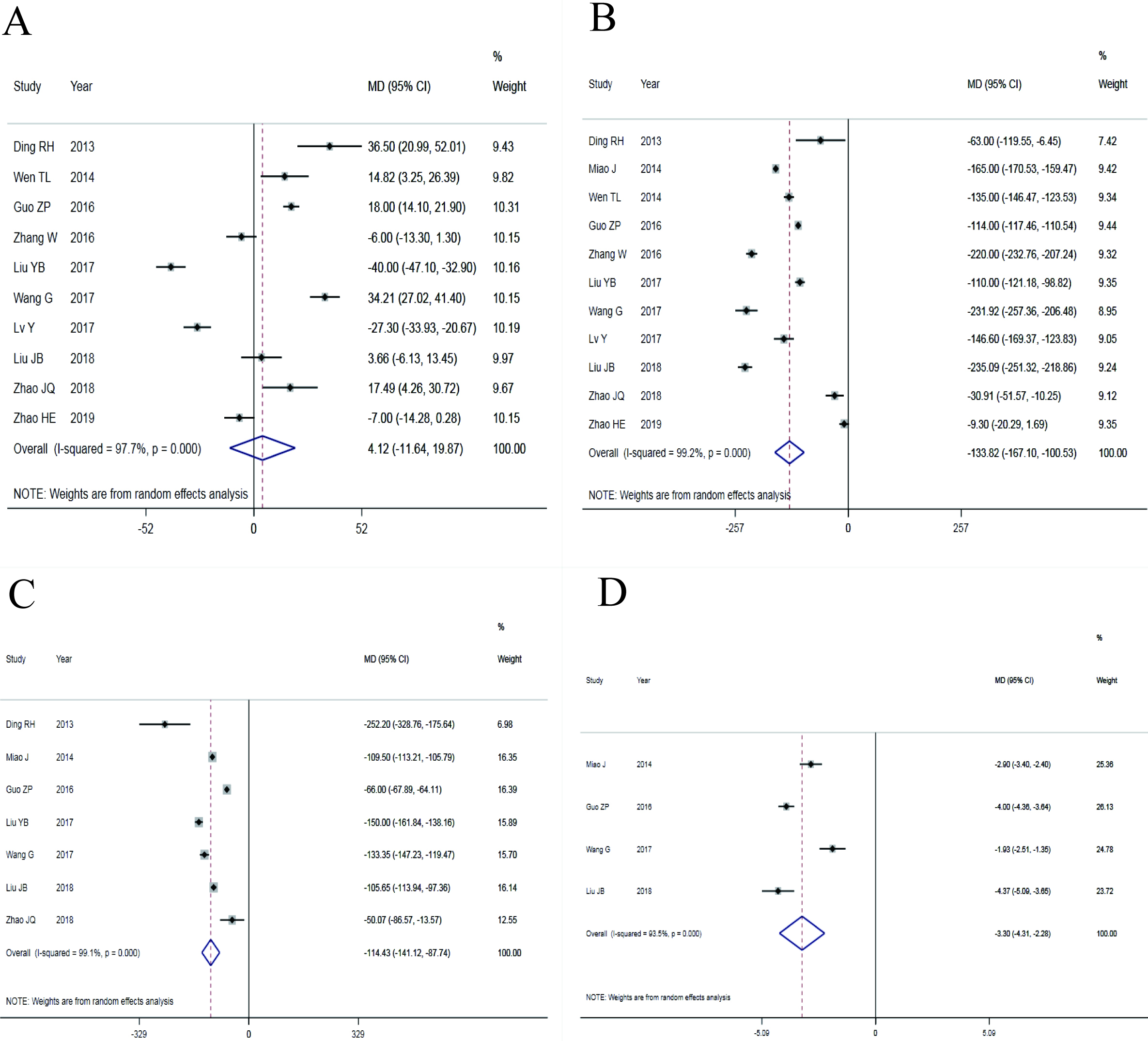
Table 3
Main results of the meta-analysis
| Indicators |
| MD | SMD | 95% CI | I | Model | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Average operation time | 10 | 4.12 | NA | 0.609 | 97.7 | 0.000 | REM | 0.863 | ||
| Intraoperative bleeding volume | 11 | NA | 0.000 | 99.2 | 0.000 | REM | 0.724 | |||
| Postoperative drainage | 7 | NA | 0.000 | 99.1 | 0.000 | REM | 0.122 | |||
| Postoperative landing time | 4 | NA | 0.000 | 93.5 | 0.000 | REM | 0.625 | |||
| Postoperative back VAS | 6 | NA | 0.010 | 96.4 | 0.000 | REM | 0.591 | |||
| Postoperative leg VAS | 4 | NA | 0.00 | 0.998 | 64.5 | 0.000 | REM | 0.098 | ||
| Postoperative ODI | 7 | NA | 0.063 | 94.2 | 0.000 | REM | 0.935 | |||
| Postoperative JOA | 3 | NA | 0.41 | 0.15 | 0.002 | 13.1 | 0.316 | FEM | 0.707 | |
MD: Mean difference; SMD: Standard mean difference; CI: Confidence internal; REM: Random effect model; FEM: Fixed effect model.
Figure 3.
Forest plots with effect index of SMD (A: postoperative low back pain VAS score; B: postoperative leg pain VAS score; C: postoperative ODI score; D: postoperative JOA score).
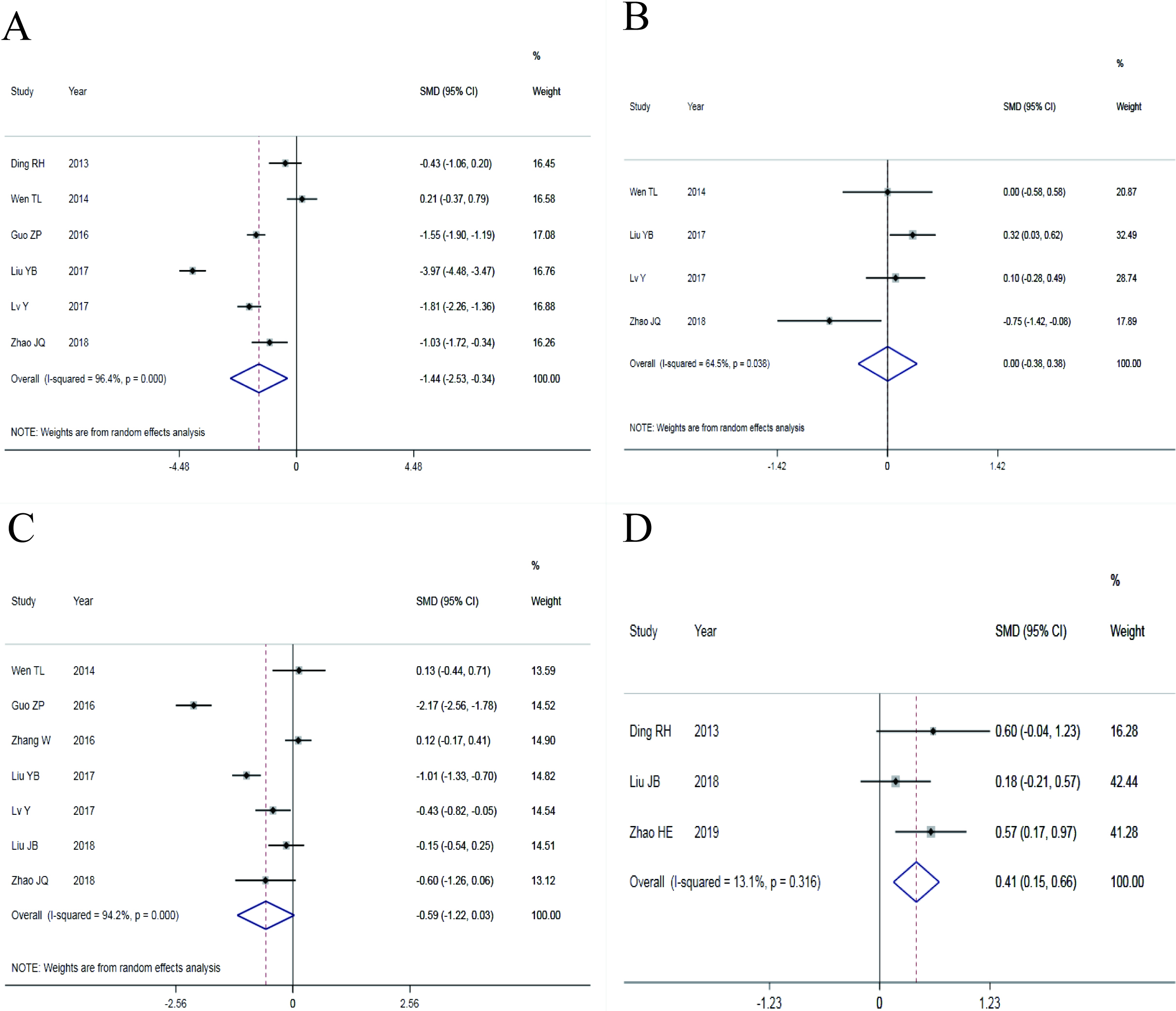
Figure 4.
Funnel plots with effect index of MD (A: average operation time; B: intraoperative blood loss; C: postoperative drainage; D: postoperative ground movement time).
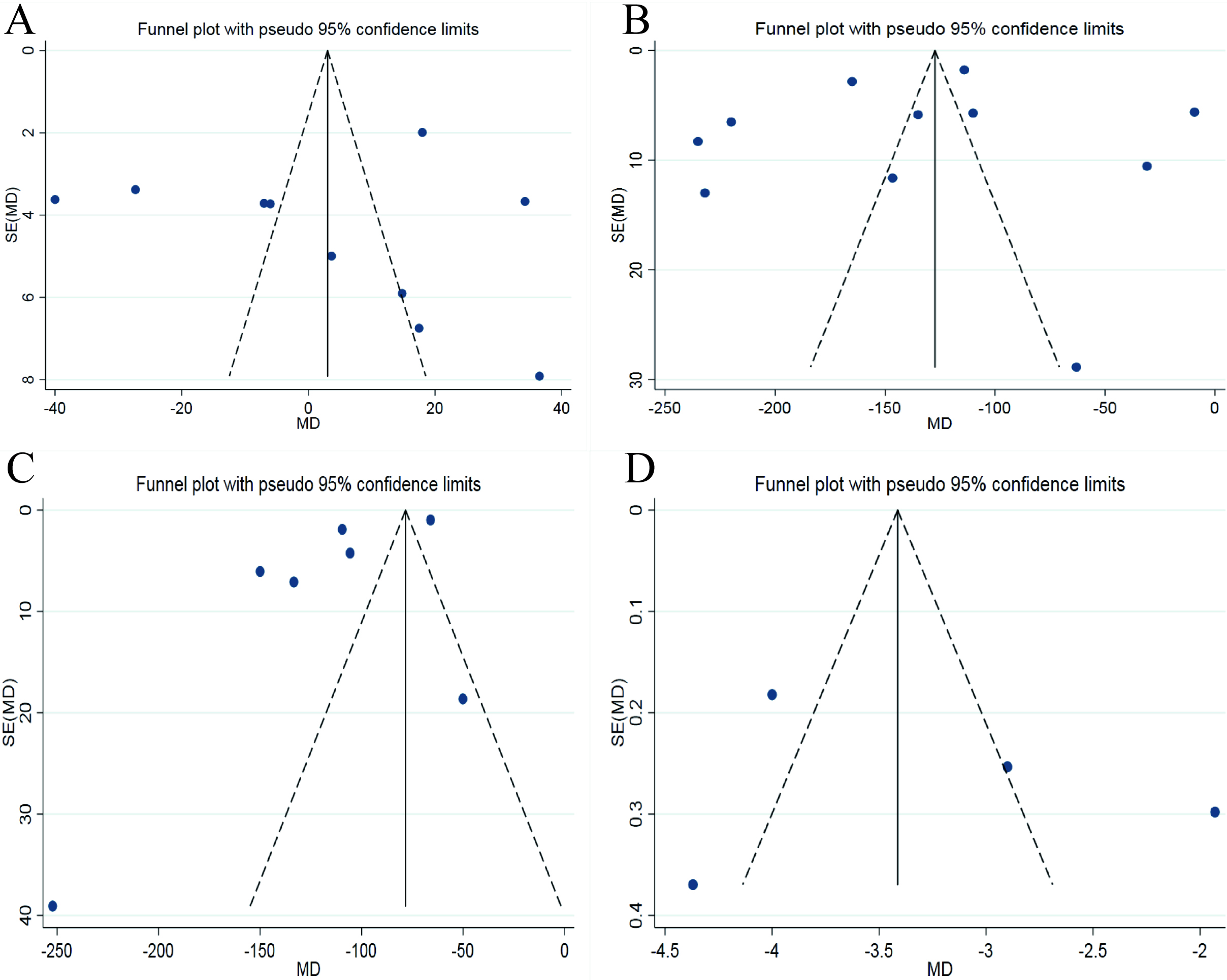
Figure 5.
Funnel plots with the effect index of SMD (A: VAS score of postoperative low back pain; B: VAS score of postoperative leg pain; C: postoperative ODI score).
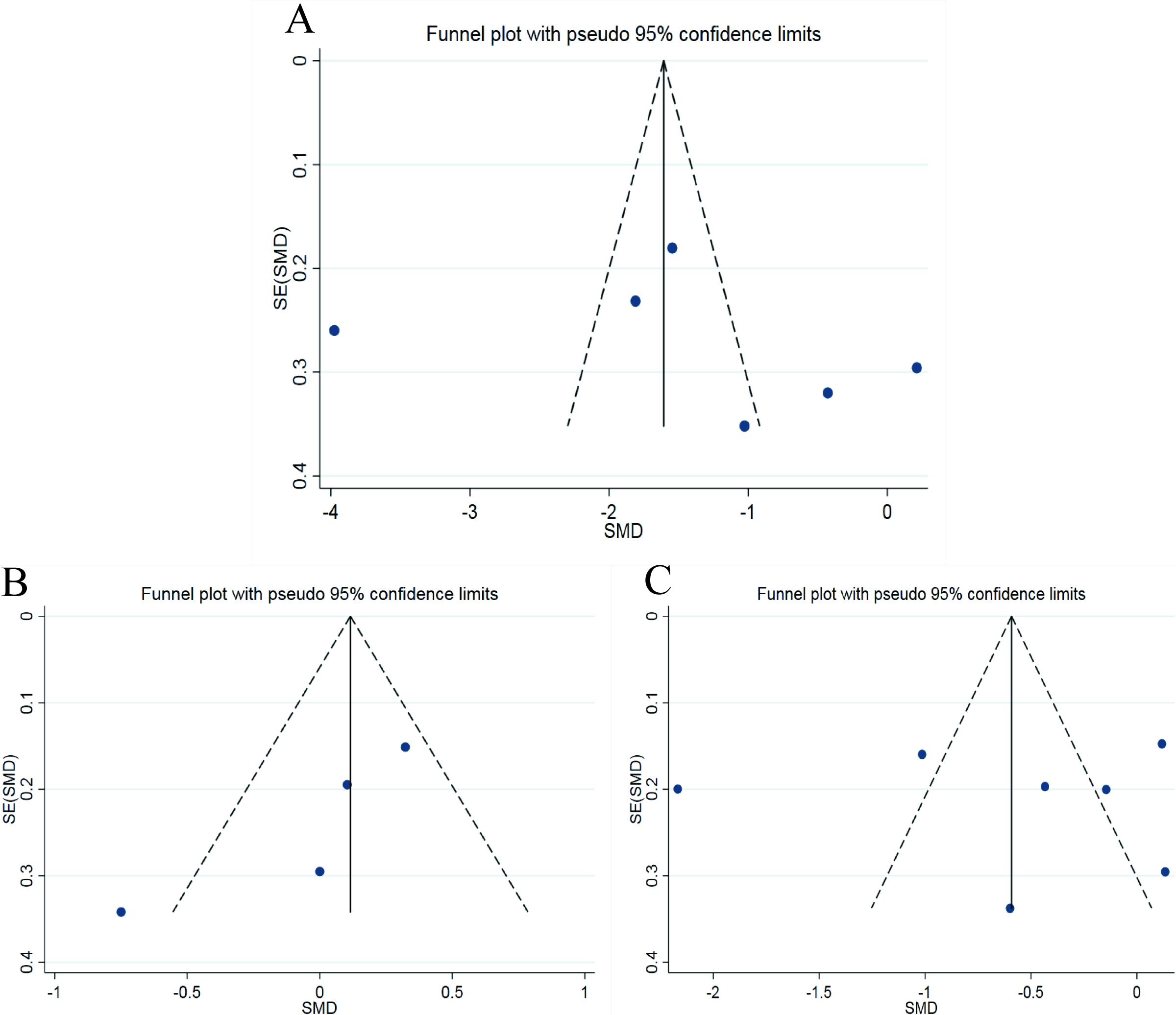
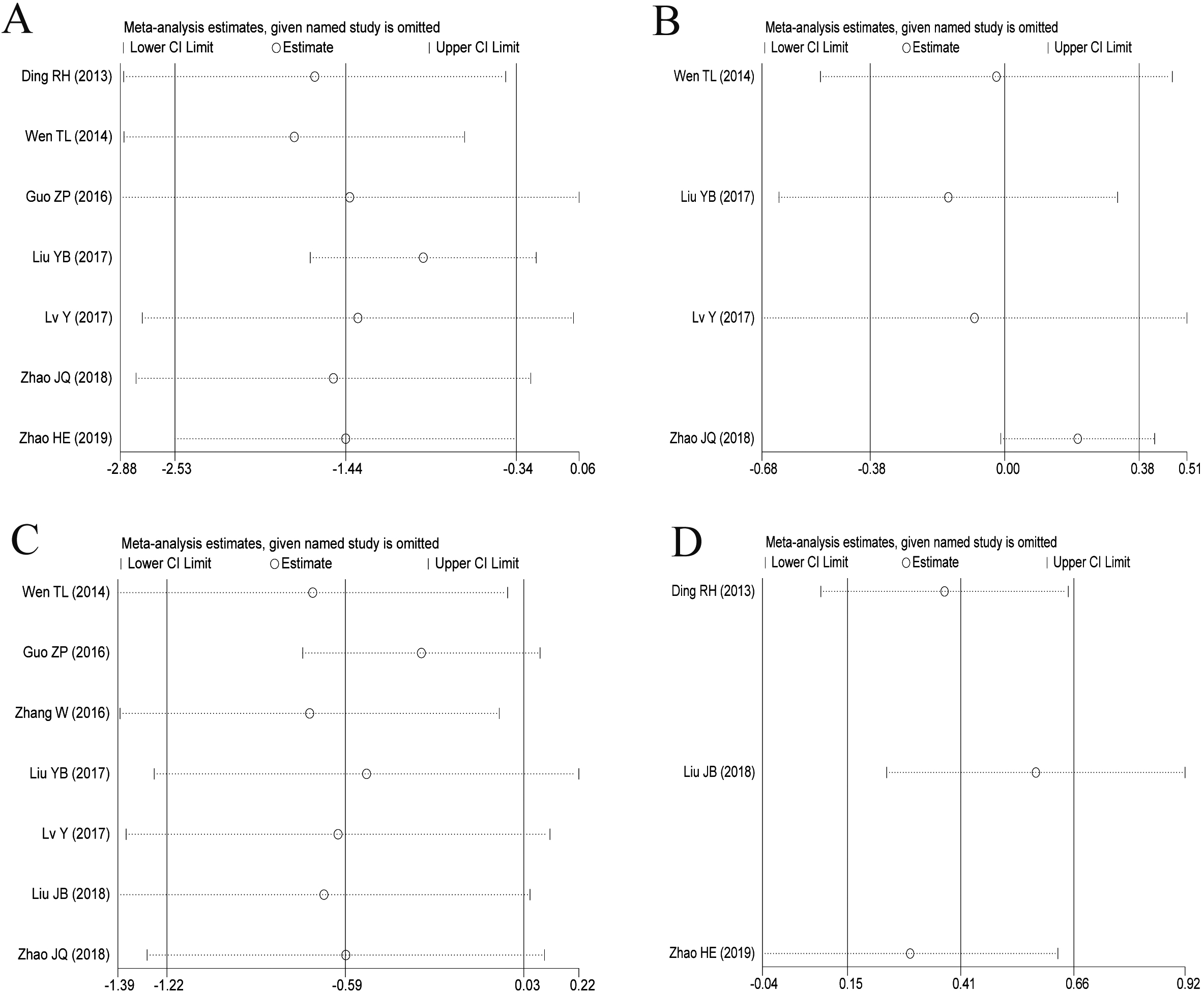
Figure 6.
The results of sensitivity analysis with effect index of MD (A: average operation time; B: intraoperative blood loss; C: postoperative drainage; D: postoperative ground movement time).
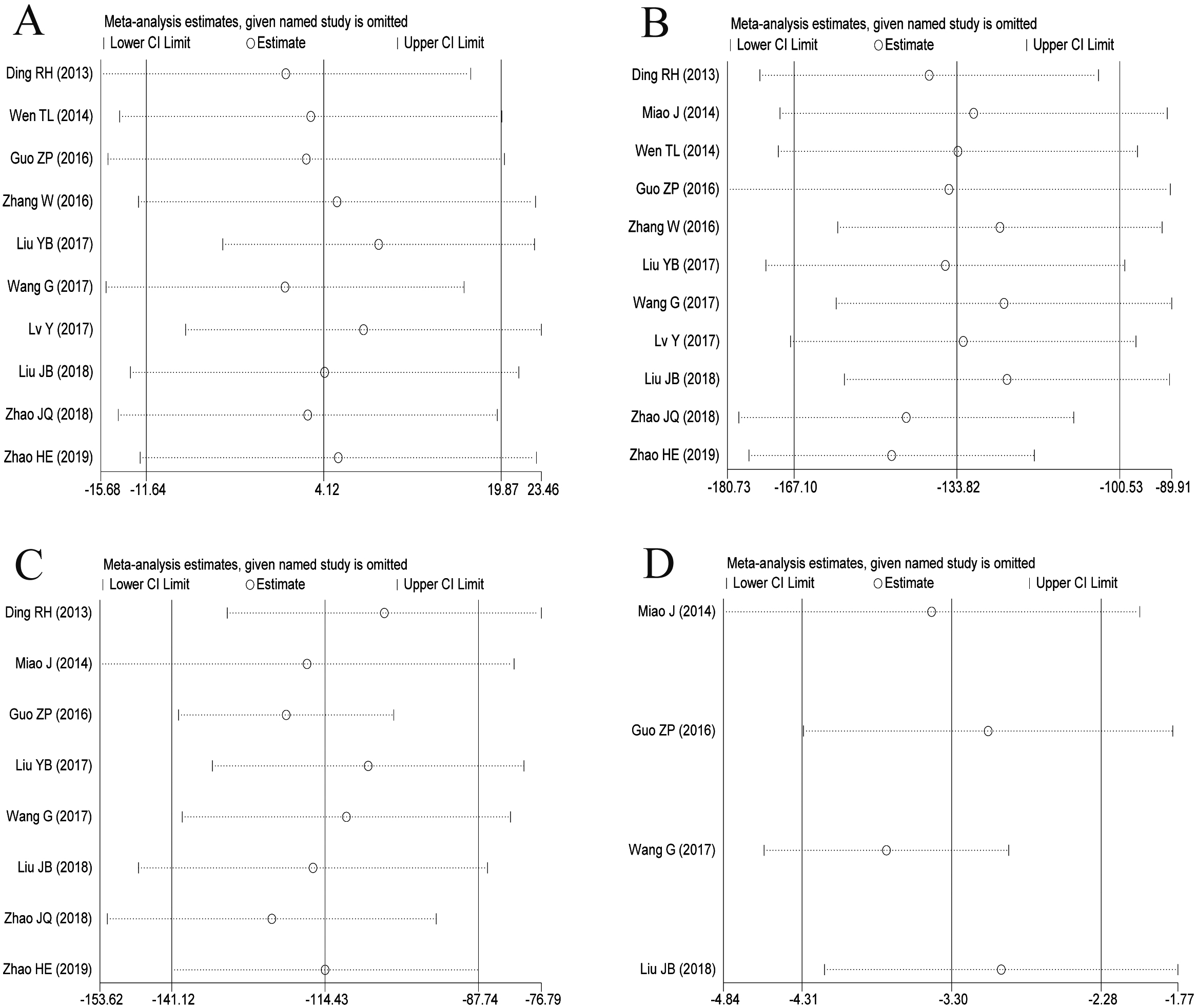
Figure 7.
Sensitivity analysis with the effect index of SMD (A: postoperative low back pain VAS score; B: postoperative leg pain VAS score; C: postoperative ODI score; D: postoperative JOA score).
3.2Results of meta-analysis
3.2.1Results with the effect index of MD
The main results of the meta-analysis are shown in Table 3. The four indexes of average operation time, intraoperative blood loss, postoperative drainage and postoperative ground activity time were combined using effect index MD, and 10, 11, 7, 4 studies were separately included in the analysis. There was statistical heterogeneity among the studies in four indicators, so the random effect models were used. The results showed that the average operation time was shorter (MD
3.2.2Results with the effect index of SMD
Postoperative low back pain VAS score, postoperative leg pain VAS score, postoperative ODI score and postoperative JOA score were combined with the effect index of SMD, and 6, 4, 7 and 3 studies were separately included in the analysis. There was statistical heterogeneity among the four indicators, so the REM were used. The results showed that there were significant differences in postoperative low back pain VAS score (SMD
3.3Publication bias
The funnel plots of average operation time and intraoperative blood loss, postoperative drainage volume and postoperative ground movement time are shown in Fig. 4A–D. The funnel plots of postoperative waist and leg VAS score and ODI score was shown in Fig. 5A–C. For there were only three studies on postoperative JOA score, the funnel plot was not drawn. The Egger’s Test results of these indicators are shown in Table 3. As can be seen from the funnel plots, the graphic symmetry was good, and from the results of Egger’s Test,
3.4Sensitivity analysis
The sensitivity analysis of average operation time, intraoperative blood loss, postoperative drainage and postoperative ground movement time was found in Fig. 6A–D. The sensitivity analysis of VAS score and ODI score of waist and leg after operation was shown in Fig. 7A–D. The results showed that the findings were robust in the average operation time, intraoperative blood loss, postoperative drainage, postoperative ground movement time, postoperative leg pain VAS score and postoperative ODI score. After two studies were eliminated in the VAS score of postoperative low back pain, the results had no statistical significance, while there was no statistical significance after the elimination of one study in the postoperative JOA score. Therefore, the conclusions of VAS score and JOA score for low back pain should still be cautious.
4.Discussion
To investigate the advantages and disadvantages of MIS-TLIF compared with O-TLIF in the treatment of LDH in the Chinese population, we conducted this meta-analysis. The results showed that, compared with O-TLIF, MIS-TLIF could significantly reduce intraoperative blood loss, postoperative drainage volume, postoperative time out of bed, and improve postoperative VAS score.
At present, there is still some controversy about the specific mechanism of low back pain caused by LDH, and the theories with more consistent views are as follows: 1) Mechanical compression: according to this point of view, the acute mechanical compression of the nucleus pulposus protruding into the spinal canal leads to symptoms such as low back pain and radiation pain of the lower extremities, and the size of the protrusion directly affects the degree of pain of the patients. However, this point of view cannot explain some clinical phenomena, e.g. the imaging examination of some patients shows that the protrusions are large, but the symptoms of low back pain are not obvious, while the protrusions of some patients are not large, but the symptoms of low back pain are very serious. 2) Inflammatory reaction: it is believed that the protruding nucleus pulposus can be used as a biochemical and immunological stimulant to cause inflammation of nerve roots, which may be the cause of low back pain in patients [25, 26]. In recent years, minimally invasive surgery is the development trend of surgery, as well as the direction of continuous efforts and pursuit of surgeons, which is the gospel of the majority of patients. Minimally invasive surgery requires less trauma, quick recovery and good effect. Minimally invasive surgery is also the main development direction of spinal surgery in recent years, that all hospitals all over the country with conditions and ability are making great efforts to develop minimally invasive surgery technology. Minimally invasive not only refers to the small incision, but also refers to the maximum clinical treatment effect while minimizing the injury [27, 28].
All the 11 studies included in this meta-analysis had clear inclusion and exclusion criteria, of which 8 studies described random methods, 3 studies described distributive concealment, 3 studies described blind methods, 10 studies reported no loss of follow-up cases, and 8 studies were of high qualities. The inclusion studies had the possibility of selective bias, implementation bias and moderate measurement bias, and the included literatures were both in English and Chinese. From the Egger’s test, the publication bias was low, so the conclusion of this study had a certain reference value. The results showed that there was no difference in operation time between MIS-TLIF and O-TLIF. Compared with O-TLIF, MIS-TLIF could significantly reduce intraoperative blood loss, postoperative drainage volume, and postoperative landing time in LDH patients. Within half a year after operation, the comparison of postoperative low back pain VAS score and limb JOA score showed that the minimally invasive group was superior to the standard open group in the improvement of low back pain. However, the results of sensitivity analysis showed that these two indicators were unstable to a certain extent, so this conclusion still needs to be taken with precaution. There was no statistical difference between VAS score and ODI score of leg pain. It may be that leg pain was caused by sciatica nerve root compression. After relieving nerve root compression, leg pain will be relieved naturally. Therefore, both MIS-TLIF and O-TLIF can achieve good results in the treatment of LDH. Minimally invasive surgery can reduce intraoperative blood loss, reduce postoperative drainage, shorten postoperative bed rest time, to a certain extent, the improvement of postoperative low back pain is better than standard open surgery, and there is no difference in operation time.
MIS-TLIF has been used in clinic for more than 10 years since it was first used in clinic. The advantage of innovation has been recognized by the majority of orthopedic surgeons and patients. Foley [13] reported that the operation was performed under the working channel by using the MIS-TLIF operation technique and the tubular channel technique, which reduced the injury to the soft tissue such as the posterior lumbar muscle, and obtained a good surgical effect. Some studies have shown that MIS-TLIF technology can achieve the same purpose of decompression and fusion as conventional open surgery, and reduce the damage to muscle and other soft tissue to a certain extent [29]. Sun [30] made a meta-analysis of the efficacy of MIS-TLIF and O-TLIF surgery in the treatment of lumbar degenerative diseases concluded that there was no significant difference in clinical efficacy between the two surgical methods. MIS-TLIF surgery reduces the injury and destruction of lumbar posterior soft tissue to a certain extent, retains the biomechanical characteristics of normal spine to the greatest extent, and achieves the purpose of full decompression, internal fixation and interbody fusion of spinal canal. Patients with mild low back pain can get out of bed early for exercise, short hospital stay and rapid recovery, reflecting the concept of modern minimally invasive surgery [31]. The expandable channel used by the MIS-TLIF can be extended to a certain extent according to the needs of the operation, and the visual field of the operation can be expanded. At the same time, the expandable channel equipment is provided with a cold light source, which can provide sufficient lighting for the visual field of the operation. The visual field of the operation is clear, which effectively solves the problem that sometimes the shadowless operating lamp is difficult to project to the part needed by the main surgeon due to occlusion. At the same time, the expandable channel does not need an assistant to pull the hook manually, which saves manpower.
This study is not without limitations. 1) This study was basically a study of Chinese people, lacking of studies in Europe, the United States or African countries, Therefore, it is not known whether the conclusion is applicable to other countries; 2) In the VAS score and JOA score of postoperative low back pain, the sensitivity analysis showed a robust deviation; 3) The follow-up time included in the study was less than half a year, which made this study lack the evaluation of the long-term efficacy and complications of MIS-TLIF and O-TLIF in the treatment of LDH. 4) Except for postoperative JOA, all the other indexes have certain heterogeneity. Due to the limited information provided in the original literature, it is impossible for us to make a further analysis of the sources of heterogeneity.
5.Conclusion
The two surgical methods could achieve good effects in the treatment of LDH, but MIS-TLIF had advantages in reducing intraoperative blood loss, postoperative drainage, postoperative low back pain, and shortening postoperative recovery time, so it was an effective minimally invasive technique for the treatment of LDH in Chinese population. However, due to the above limitations of this study, it still needs to be verified by more randomized controlled trials with better quality, longer follow-up period and larger sample size.
Declarations
All authors have read and approved this version of the article. The authors claim that none of the material in the paper has been published or is under consideration for publication elsewhere.
Funding
The authors have no support or funding to report.
Conflict of interest
The authors declare that they have no conflict of interest.
References
[1] | Lee JH, Lee SH. Clinical usefulness of electrodiagnostic study to predict surgical outcomes in lumbosacral disc herniation or spinal stenosis. Eur Spine J. (2015) ; 24: (10): 2276-80. |
[2] | Qu Y, Cheng M, Dong R, Kang M, Zhou H, Zhao J. K-rod dynamic internal fixation versus microendoscopic discectomy for the treatment of single-segment lumbar disc herniation. J Orthop Surg (Hong Kong). (2017) ; 25: (3): 2309499017742740. |
[3] | Chadha M, Sharma G, Arora SS, Kochar V. Association of facet tropism with lumbar disc herniation. Eur Spine J. (2013) ; 22: (5): 1045-52. |
[4] | Strömqvist F, Strömqvist B, Jönsson B, Karlsson MK. Surgical treatment of lumbar disc herniation in different ages-evaluation of 11,237 patients. Spine J. (2017) ; 17: (11): 1577-1585. |
[5] | Strömqvist F, Strömqvist B, Jönsson B, Gerdhem P, Karlsson MK. Predictive outcome factors in the young patient treated with lumbar disc herniation surgery. J Neurosurg Spine. (2016) ; 25: (4): 448-455. |
[6] | Fakouri B, Nnadi C, Boszczyk B, Kunsky A, Cacciola F. When is the appropriate time for surgical intervention of the herniated lumbar disc in the adolescent? J Clin Neurosci. (2009) ; 16: (9): 1153-6. |
[7] | Mixter WJ, Barr JS. Rupture of the intervertebral disc with involvement of spinal canal. New Engl J Med. (1934) ; 211: (5): 210-215. |
[8] | Gugliotta M, da Costa BR, Dabis E, Theiler R, Jüni P, Reichenbach S, et al. Surgical versus conservative treatment for lumbar disc herniation: a prospective cohort study. BMJ Open. (2016) 21; 6: (12): e012938. |
[9] | Harms J, Rolinger H. Die operative behandlung der spondylolisthese durch dorsale aufrichtung und ventrale verblockung [A one-stager procedure in operative treatment of spondylolistheses: Dorsal traction-reposition and anterior fusion (author’s transl)]. Z Orthop Ihre Grenzgeb. (1982) ; 120: (3): 343-7 (in German). |
[10] | Mroz TE, Lubelski D, Williams SK, O’Rourke C, Obuchowski NA, Wang JC, et al. Differences in the surgical treatment of recurrent lumbar disc herniation among spine surgeons in the United States. Spine J. (2014) ; 14: (10): 2334-43. |
[11] | Goz V, Weinreb JH, Schwab F, Lafage V, Errico TJ. Comparison of complications, costs, and length of stay of three different lumbar interbody fusion techniques: An analysis of the Nationwide Inpatient Sample database. Spine J. (2014) ; 14: (9): 2019-27. |
[12] | Wiltse LL, Bateman JG, Hutchinson RH, Nelson WE. The paraspinal sacrospinalis-splitting approach to the lumbar spine. J Bone Joint Surg Am. (1968) ; 50: (5): 919-26. |
[13] | Foley KT, Holly LT, Schwender JD. Minimally invasive lumbar fusion. Spine (Phila Pa 1976). (2003) ; 28: (15 Suppl): S26-35. |
[14] | Ding RH, Liu B, Zhang B, Wang YQ, Xiao B, Su HT. Comparism of minimally invasinve and open transforaminal lumbar lumbar interbody fusion in the treatment of single-level lumbar disc herniation. Journal of Practical Orthopaedics. (2013) ; 19: (11): 969-75 (in chinese). |
[15] | Miao J, Zhao JC, An YH, He LY, Zhang Y, Wang DS, et al. Comparison of efficacy between minimally invasive surgery and open surgery in the treatment of lumbar disc herniation and nursing for complication. Chinese Journal of Modern Nursing. (2014) ; 20: (13): 1541-1543 (in chinese). |
[16] | Wen TL, Liu XM, Zhang TY, Et Al. Effect of minimally invasive transformational lumbar interbody fusion in treatment of far lateral lumbar disc herniation. Medical & Pharmaceutical Journal of Chinese People’s Liberation Army. (2014) ; 26: (10): 4-8 (in chinese). |
[17] | Guo ZP, Wen GH, Shang H, Wu YP, Guo XP, Li BK. Effect comparison of quadrant TLIF channel system and traditional TLIF method in treatment of lumbar intervertebrai disc protrusion. Chin Med Herald. (2016) ; 13: (12): 97-100 (in chinese). |
[18] | Zhang W, Gao D, Gao HR, Gao QY, Han K, Wang YD, et al.Comparison of Mini-TLIF using quadrant minimally invasive system and open-TLIF in treatment of lumbar disc herniation. Chinese Journal of General Practice. (2016) ; 14: (3): 346-348 (in chinese). |
[19] | Lv Y, Chen J, Chen J, Wu Y, Chen X, Liu Y, et al. Three-year postoperative outcomes between MIS and conventional TLIF in1-segment lumbar disc herniation. Minim Invasive Ther Allied Technol. (2017) ; 26: (3): 168-176. |
[20] | Liu YB, Sun XZ, Gong R, Yu JH, Hou SB, Gu ZF, et al. The analysis of therapeutic effects of two different surgical methods in the treatment of lumbar disc herniation. Journal of Clinical Orthopaedics. (2017) ; 26: (1): 13-16 (in chinese). |
[21] | Wang G, Yang K, Mei QA, Zhang Q. Comparison of the curative effect of Quadrant minimally invasive therapy and transforaminal lumbar interbody fusion in the treatment of lumbar disc herniation. Modern Journal of Integrated Traditional Chinese and Western Medicine. (2017) ; 26: (7): 701-707 (in chinese). |
[22] | Zhao J, Zhang S, Li X, He B, Ou Y, Jiang D. Comparison of minimally invasive and open transforaminal lumbar interbody fusion for lumbar disc herniation: A retrospective cohort study. Med Sci Monit. (2018) ; 24: : 8693-8698. |
[23] | Liu JB, Li JL, Xie DW, Zhou P, Xiong FL, Gong GY. Clinical comparison of two kinds of operation schemes in treatment of lumbar disc herniation combined with lumbar instability. China Journal of Modern Medicine. (2018) ; 28: (19): 107-11 (in chinese). |
[24] | Zhao H, Gao H, Zhou C, Qian S, Yuan Y, Xue W, et al. A randomized controlled trial with ⩾5 years of follow-up comparing minimally invasive and open transforaminal lumbar interbody fusion in disc herniation at single level. Exp Ther Med. (2019) ; 17: (5): 3614-3620. |
[25] | Moen GH, Moen A, Schistad EI, Gjerstad J. Local up-regulation of interferon-γ (IFN-γ) following disc herniation is involved in the inflammatory response underlying acute lumbar radicular pain. Cytokine. (2017) ; 97: : 181-186. |
[26] | Cunha C, Silva AJ, Pereira P, Vaz R, Gonçalves RM, Barbosa MA. The inflammatory response in the regression of lumbar disc herniation. Arthritis Res Ther. (2018) ; 20: (1): 251. |
[27] | Hawasli AH, Khalifeh JM, Chatrath A, Yarbrough CK, Ray WZ. Minimally invasive transforaminal lumbar interbody fusion with expandable versus static interbody devices: Radiographic assessment of sagittal segmental and pelvic parameters. Neurosurg Focus. (2017) ; 43: (2): E10. |
[28] | McClelland S 3rd, Goldstein JA. Minimally invasive versus open spine surgery: What does the best evidence tell us? J Neurosci Rural Pract. (2017) ; 8: (2): 194-198. |
[29] | Park P, Foley KT. Minimally invasive transforaminal lumbar interbody fusion with reduction of spondylolisthesis: Technique and outcomes after a minimum of 2 years’ follow-up. Neurosurg Focus. (2008) ; 25: (2): E16. |
[30] | Sun ZJ, Li WJ, Zhao Y, Qiu GX. Comparing minimally invasive and open transforaminal lumbar interbody fusion for treatment of degenerative lumbar disease: A meta-analysis. Chin Med J (Engl). (2013) ; 126: (20): 3962-71. |
[31] | Wang J, Zhou Y, Zhang ZF, Li CQ, Zheng WJ, Liu J. Comparison of one-level minimally invasive and open transforaminal lumbar interbody fusion in degenerative and isthmic spondylolisthesis grades 1 and 2. Eur Spine J. (2010) ; 19: (10): 1780-4. |




